Abstract
Background
Identifying the factors influencing mental health of mothers at critical stages of childrearing is significant for the implementation of effective promotion policies and counselling activities.
Objective
This study aimed to investigate the relationships between children's feeding difficulties, marital quality, parenting quality and maternal mental health risks amidst Chinese mothers with high and low social support using a multi-group structural equation modelling approach.
Participants
A cross-sectional study was conducted in Wenzhou, China and a total of 772 mothers with children aged 0–3 were surveyed by using purposive sampling.
Findings
Results showed that of the 772 participants, 23.6 % reported anxiety, 50.1 % reported depression, 91.2 % reported insomnia, and 24 % reported feeding difficulties. The joint occurrence of multiple forms of mental problems is the most commonly reported features of mental health risks among mothers. The positive association between feeding difficulties of children and mental health risks of mothers was mediated by marital quality and parenting quality. In addition, feeding difficulties were not related to mental health risks in high social support group but all the relationships were significant in low social support group.
Conclusions
These findings highlight the importance of the specific interventions to enhance social support, marital quality and parenting quality for improving mental health of mothers of children with feeding difficulties.
Keywords: Feeding difficulties, Mental health, Marital quality, Parenting quality, Structural equation model
1. Introduction
Feeding difficulties (FDs) in children refers to a condition in which a child has weight loss or no weight gain without an obvious physiological disease [1]. It is remarkably prevalent in children aged 0–36 months, which is a critical period in child rearing. In China, an epidemiological survey found that the incidence of FDs in children aged 0–36 months was 10.5 % [2]. FDs in early childhood may not only lead to impaired growth and low nutrient intake in children, but also to mental health problems in caregivers, such as depression, anxiety and insomnia [3], especially in mothers who are often considered the primary parent responsible for feeding their children [4]. Diathesis-stress theory [5] and family systems theory [6] provide a framework for understanding the impact of children's FDs on mental health of mothers. Specifically, life stressors (children's FDs) can trigger the deterioration of the family relationship in the marital subsystem (marital quality) and the parental subsystem (parenting quality), which are significantly related to the development of a family member's mental health risk. Furthermore, based on the buffering theory of social support [7], the effect of children's FDs on mothers' mental health risks might be buffered by social support. Therefore, in the light of the above theories, the current study aims to examine the prevalence and characteristics of mothers' mental health at critical stages of childrearing, to explore the mediating role of marital quality and parenting quality in the association between children's FDs and mothers' mental health risks; and to try to understand the buffering role of social support.
1.1. FDs of children and mental health of mothers
FDs are characterized by food selectivity, problematic eating behavior and oral/motor difficulties [8], are significant contributors to low immunity and impaired physical, brain, and intellectual development in children [9]. Recent research has expanded the focus from the children themselves to their caregivers, particularly mothers, who are the primary caregivers during early childhood [10]. Based on the diathesis-stress theory [5], the interaction between a biological predisposition and psychosocial stress triggers pathological symptoms. In this context, children's FDs (stressful life events) combine with maternal postpartum hormonal imbalance (diathesis) to disrupt the mother's psychological equilibrium and produce psychological problems [11]. Furthermore, empirical studies have provided evidence that mothers of children with FDs tend to experience frustration and lower parenting self-efficacy, followed by the emergence of mental health symptoms [[12], [13], [14]]. These mothers may also neglect their own health to focus on their children, contributing to poorer health and well-being compared to mothers of children without FDs [15]. For example, Azhari et al. (2020) found that mothers of children with FDs reported more challenges with daily activities and psychological problems, including insomnia, irritability, depression and anxiety.
Furthermore, while the majority of relevant research has focused primarily on the first year postpartum, very few studies have explored this issue up to three years postpartum, which is the critical period for both mothers and offspring. For children, the 0–3 years period is an extremely critical stage in their physical and mental development in the life cycle. However, children's digestive systems are still developing and are susceptible to adverse physiological, environmental, and psychological conditions, that can lead to FDs [16]. For mothers, the three years after childbirth is a stressful and challenging time. During this period, due to their new roles and responsibilities as mothers, women experienced major physiological, psychological and maternal behavioural changes [17]. Especially in China, mothers usually take on most of the childcare before their children enter kindergarten, which further adds to their stress and burden. In the current study, we have therefore defined 0–3 years as a “critical parenting period". This study explores the impact of children's FDs on maternal mental health during this critical parenting period.
1.2. Marital quality and parenting quality as mediators
Marital quality is significantly associated with their mental health through direct and indirect path [18,19]. Specifically, couples with positive marital interaction or high marital satisfaction tend to use effective communication strategies to resolve marital conflict, which in turn may improve their mental health level [20]. Conversely, negative aspects of marital quality often lead to various behavioral and psychological problems, including depression, hostility, and anger [21].
Further, marital quality of young parents is usually influenced by the parenting difficulties of their children (eg. their children's FDs). According to the role conflict theory [22], a woman's roles as a spouse and a mother often overlap and conflict during the critical parenting period. Mothers of children with FDs often exhausted from parenting duties, which can lead to neglecting their husbands' feelings and a subsequent decline in marital quality. Empirical studies have found that families with children of FDs often report lower marital satisfaction [23]. Specifically, parents with children of FDs frequently experience high levels of negative emotions in parenting and may express these emotions towards their spouses, affecting their marital relationship [24]. This phenomenon is observed even in same-sex couples, where the addition of a newborn can reduce couple time, alter employment and household dynamics, and increase conflict and stress in romantic relationships [25].
Parenting quality refers to the quality and level of cooperation between caregivers responsible for raising children, typically encompassing parent-child relationships and parenting competence [26]. Empirical research found that parenting quality is significantly related to parent's mental health, particularly for mothers [[27], [28], [29]]. For example, a clinical study of 121 mothers found that mothers with poor parent-child relationships were less interested in their child's health and more likely to engage in negative health behaviours [30].
Additionally, FDs can compromise parenting quality, leading to negative mother-child interactions, increased parenting pressure, and decreased parenting efficacy [31,32],.Thus, FDs are significantly associated with parenting quality, which in turn affects maternal mental health. Evidence also suggests a strong link between marital quality and parenting quality According to Family System Spillover Theory [33], the positive or negative experiences in the marriage system can spill over into parenting system [34]. For example, a longitudinal study of 1604 preschool children showed that marital conflict will spill over into parent-child relationships, which is characterized by more hostile, harsh, emotionally neglectful parenting, and less warmth [35]. Thus, marital quality is crucial for parenting quality, and both are influenced by the stress factor of children's FDs.
1.3. Group difference by social support
The stress-buffering model [36] and empirical research suggest that social support can mitigate the adverse effects of stressful events (e.g., children's FDs) on mothers' mental health (e.g., depression, insomnia). For example, Ajdukovic, Rajter [37] found that support from family and friends can alleviate the pressures associated with child-rearing. However, early relative studies mainly emphasised the role of social support in a single pathway from stressful events to mental health. There is a lack of studies examining the effect of social support within a structural equation model framework.
1.4. The present study
In order to synthesize findings from existing literature and identify pathways to the onset of mental health risk in Chinese mothers, it is necessary to consider the variables above synchronously. In this study, we evaluate the prevalence of mental health risk, examine how FDs of children are associated with mental health risks among mothers at critical stages of childrearing, and hypothesize that marital quality and parenting quality act as mediators of this relationship, and social support plays a moderating role.
2. Methods
2.1. Participants
Mothers with children aged 0–3 years were selected for the study. They were recruited from 10 community immunisation centres in Wenzhou, Zhejiang Province, China, between March 2021 and September 2021. Wenzhou is one of the most economically developed cities in China, with a population of 9.19 million. Inclusion criteria were: female, age ≥18 years, no history of depression or other psychiatric problems before delivery, and children's age ≤3 years.
The study was approved by the Institutional ReviewBoard (IRB) of Wenzhou Medical University, with the IRB approval number: [2021-K-23-02]. All procedures performed in this study were in accordance with the 1964 Helsinki declaration. Data collection procedures were as follows. First, the investigator introduced a detailed description of the study to the mothers while they were waiting in the quiet observation room for 30 min to check whether their children had any adverse reactions after vaccination. Second, written informed consent was obtained prior to data collection (98.89 % agreed to participate in our study). Finally, the participants completed the questionnaire. A total of 772 valid samples were collected (response rate = 96 %).
Of these, mothers' ages ranged from 18 to 50 years (M = 32.18, SD = 5.89), 47.3 % of them had an undergraduate degree, while 46.0 % were junior college and below. A majority (95.3 %) of participants were first marriage and 58.5 % of them delivered the baby by eutocia. The family annual income of 79.0 % participants was within 8–30 thousand RMB or below. This study included a sample of childrens ranging in age from 0 to 36 months (M = 18.08, SD = 9.88), male childrens accounted for 50.7 % of the total sample, 99.3 % of the childrens were not born prematurely, and 99.6 % of the childrens were in good health.
2.2. Measures
2.2.1. Socio-demographics
A demographic questionnaire was used to collect maternal variables, including mother's age, level of education, marital status, annual family income and occupation, and children variables, including children's age, sex and birth.
2.2.2. FDs of children
The Chinese version [38] of the revised Montreal Children's Hospital Feeding Scale (MCH-FS) was used to assess FDs, which included fourteen items grated from 1 (strongly disagree) to 7 (strongly agree). Four types of FDs (infant growth, infant oral motor function, parental feeding behavior and infant eating behavior) were assessed using the MCH-FS infant growth subscale (e.g., “How is your child's growth?”), infant oral motor function subscale (e.g., “How well your child chews (or sucks)”), parental feeding behavior subscale (e.g., “How does the child's eating affect relationships between family members?”), and infant eating behavior subscale (e.g., “How is your child's appetite?”). Higher scores indicate more serious the feeding problem. In our study, the alpha for the scale was .87.
2.2.3. Marital quality
Marital quality was evaluated from two aspects: marital happiness and marital interaction.
The Marital Happiness scale [39] was utilized to evaluate marital happiness. It consisted of twelve items (e.g., “Spouse's care for your family”) scored from 0 (very dissatisfied) to 4 (very satisfied). Higher scores indicate more marital happiness. In our study, the alpha for the scale was .96.
The Chinese version [40] of the revised marital interaction scale [41] was used to measure marital interaction. It consisted of eight items (e.g., “Couples discuss the big things in life”) scored from 0 (never) to 4 (almost always). Higher scores indicate more marital interaction. In our study, the alpha for the scale was .93.
2.2.4. Parenting quality
Parenting quality was evaluated from two aspects: parent child relationship and parenting sense of competence.
Five items were used to assess the parent child relationship (1) I get along well with my children; (2) I can keep a happy mood with my children; (3) I hug and kiss my children; (4) My children like me very much; (5) My child is very happy to be with me. Responses were recorded on a 5-point scale ranging from “never" to “almost always." Higher score indicated better relationship. We constructed an indicator of parent child relationship using confirmatory factor analysis (CFA) and it showed an acceptable model fit (RMSEA = .07 < .08, NFI = .92 > .90, CFI = .93 > .90, GFI = .96 > .90). The corresponding factor loadings range from .87 to .91. The alpha was .93 and the overall Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy was .85.
The Chinese version of the short form [42] of 17-items Parenting Sense of Competence Scale (PSCS) [43] was utilized to evaluate parenting sense of competence. Two types of PSCS (parenting satisfaction and self-efficacy) were assessed using the PSCS parenting satisfaction subscale (e.g., “Although motherhood is a joy, caring for a child of this age at this time is discouraging.”), and self-efficacy subscale (e.g., “Being a good mother is a reward in itself”.). The items in two subscales were responded on a 4-point Likert scale (from 1 = absolutely disagree to 4 = absolutely agree). High scores indicate high levels of parenting satisfaction and self-efficacy. In our study, the alpha for the scale was .74.
2.2.5. Social support
Six items assessing participants' perceptions of support from (1) husband, (2) mother, (3) mother-in-law, (4) father-in-law, (5) father, and (6) friends were used as indicators of social support. Responses were recorded on a 5-point scale ranging from “not at all" to “extremely strong. For example, “the level of support from your husband during the postpartum three years”. Higher score indicated stronger social support. The results of CFA showed an acceptable model fit (RMSEA = .07 < .08, NFI = .98 > .90, CFI = .99 > .90, GFI = .96 > .90). The corresponding factor loadings ranged from .70 to .82. The alpha was .84 and the KMO was .74.
2.2.6. Mental health risk of mothers
Mental health risks of mothers were evaluated from three aspects: anxiety, depression and insomnia.
Anxiety: Anxiety symptom was measured by the Self-Rating Anxiety Scale (SAS) [44], which consisted of twenty items scored from 1 (never) to 4 (almost always). For example, “I think I get nervous and anxious more easily than usual.” In our study, the alpha for the scale was .81.
Depression: Depression symptom severity was measured by the Chinese version [45] of the revised Edinburgh Postnatal Depression Scale (EPDS) [46], which consisted of ten items scored from 0 (never) to 3 (almost always). For example, “I'm so unhappy that I can't sleep.” In our study, the alpha for the scale was .86.
Insomnia: Sleep quality was measured by the Chinese version of the revised Insomnia Severity Index (ISI) [47], which consisted of seven items scored from 0 (never) to 4 (almost always). For example, “The extent to which you are anxious and annoyed about your current sleep problems.” In our study, the alpha for the scale was .86.
2.3. Data analysis
Firstly, a preliminary description of all variables was carried out using bivariate correlations and independent samples t-test. Secondly, structural equation modelling (SEM) with maximum likelihood method was performed in AMOS 26.0 to test the hypothetical model. First, a measurement model was tested using CFA. Then, the direct and indirect effects of children's FDs were tested in the structural model. Finally, multi-group SEM was used to examine the moderator of social support. Various goodness of fit tests were used, including chi-squared statistic (χ2), root mean square error of approximation (RMSEA), comparative fit index (CFI), Tucker-Lewis fit index (TLI) and standardised root mean square residual (SRMR). Acceptable values were as follows: CFI and TLI greater than .9; SRMR and RMSEA greater than .08 [48].
2.4. Common method biases detection
Deviation from common method bias was controlled by the process control method of reversing some projects and anonymous questionnaires. Harman's one-way analysis was performed using SPSS 26.0. According to Podsakoff, MacKenzie [49], the explanation rate of the cumulative one-way variance below 40 % was acceptable. The result showed that the variation of the explanation of the first factor obtained by the unrotated factor was 34.56 %, which did not exceed 40 %. Therefore, it has a minor impact on our result.
3. Results
3.1. Prevalence and characteristics of mental health risk
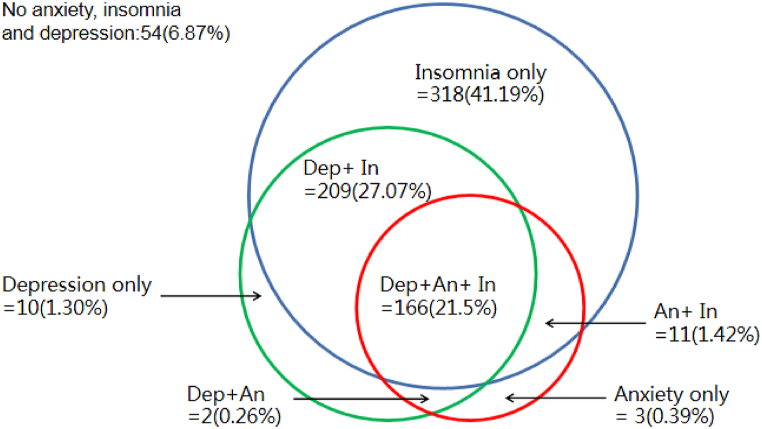
In general, out of 772 mothers, 183 (23.6 %) participants reported anxiety symptoms(M = 43.48, SD = 10.25). Specifically, 132 (17 %) had mild anxiety, 45 (5.8 %) had moderate anxiety, and 6 (.8 %) had severe anxiety. A total of 387 (50.1 %) participants reported depressive symptoms (M = 9.64, SD = 4.99). Specifically, 221 (28.6 %) had mild and moderate depression, and 166 (21.5 %) had moderately severe or severe depression. 704 (91.2 %) participants had symptoms of insomnia (M = 13.96, SD = 5.14). Specifically, 436 (56.5 %) had mild insomnia, 226 (29.3 %) had moderate insomnia, and 42 (5.4 %) had severe insomnia.
The different patterns of anxiety, depression and insomnia and their overlap are shown in the Venn diagrams in Fig. 1. Overall, only 6.87 % had none of the above symptoms. The most common form of mental health problem was insomnia (318; 41.19 %) alone compared to depression alone and anxiety alone. Furthermore, more than half of them experienced multiple forms of mental health problems including comorbidities of anxiety and depression (2; .26 %), insomnia and depression (209; 27.07 %) and anxiety, depression and insomnia in particular (166; 21.5 %).
Fig. 1.
Comorbidity rates of mental health risks among mothers with children aged 0–3 years in Wenzhou, China (March–September 2021).
Note. An anxiety, Dep depression, In insomnia.
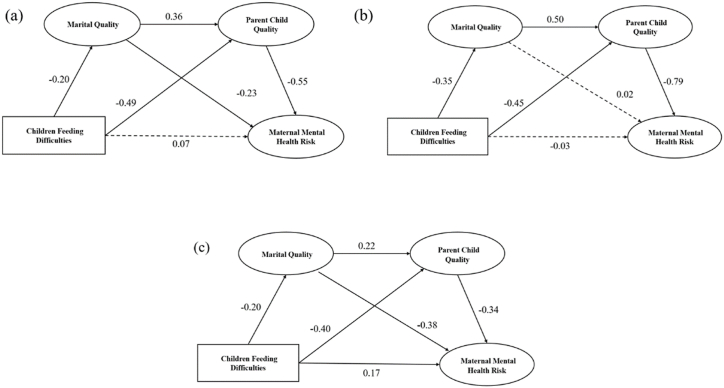
3.2. Preliminary analyses
Means, standard deviations, and bivariate correlations among FDs of children, marital quality, parenting quality and mental health risks of mothers are summarized in Table 1. As shown in Fig. 2(a), FDs of children were significantly positively correlated with mental health (depression, anxiety and insomnia) (rs = .22 - .38, ps < .01), and negatively correlated with marital quality, and parenting quality (rs = - .42 − - .34, ps < .01). Mental health (anxiety, depression and insomnia) was significantly positively correlated with FDs of children (rs = .21 − .38, ps < .01), and negatively correlated with marital quality and parenting quality (rs = - .47 − - .17, ps < .01).
Table 1.
Correlations and descriptive statistics for the main study variables (N = 772).
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1.FDC | 1 | ||||||||
| 2.MH | −.176∗∗ | 1 | |||||||
| 3.MI | −.172∗∗ | .740∗∗ | 1 | ||||||
| 4.PCR | −.365∗∗ | .233∗∗ | .239∗∗ | 1 | |||||
| 5.CC | −.415∗∗ | .320∗∗ | .295∗∗ | .465∗∗ | 1 | ||||
| 6.D | .354∗∗ | −.426∗∗ | −.361∗∗ | −.345∗∗ | −.478∗∗ | 1 | |||
| 7.A | .380∗∗ | −.321∗∗ | −.278∗∗ | −.342∗∗ | −.452∗∗ | .684∗∗ | 1 | ||
| 8.I | .216∗∗ | −.318∗∗ | −.259∗∗ | −.173∗∗ | −.315∗∗ | .536∗∗ | .571∗∗ | 1 | |
| 9.SS | −.110∗∗ | .483∗∗ | .478∗∗ | .234∗∗ | .273∗∗ | −.313∗∗ | −.246∗∗ | −.244∗∗ | 1 |
| M | 39.510 | 38.150 | 21.570 | 22.370 | 48.010 | 9.640 | 43.480 | 13.960 | 31.370 |
| SD | 13.278 | 6.470 | 4.835 | 2.825 | 6.428 | 4.996 | 10.25 | 5.138 | 7.643 |
Note. ∗p .05; ∗∗p .01; ∗∗∗p 0001. FDC feeding difficulties of children; MH Marital happiness; MI Marital interaction; PCR parent-child relationship; CC Childcare competence; D Depression; A Anxiety; I Insomnia; SS social support.
Fig. 2.
The chain mediated model of feeding difficulties of children. (a) Full model; (b) High social support group model; (c) Low social support group model.
The results of the independent sample t-test indicate that high social support groups scored significantly higher on marital quality (marital happiness: t = −12.465, p < .001; marital interaction: t = −11.711, p < .001), parenting quality (parent child relationship: t = −3.964, p < .001; childcare competence: t = −5.268, p < .001), as well as less mental health problems (depression: t = 7.138, p < .001; anxiety: t = 4.573, p < .001; insomnia: t = 5.926, p < .001) than low social support groups (see Table 2).
Table 2.
Differences in Key variables between high and low social support groups.
| variables |
M ± SD |
t | |
|---|---|---|---|
| Low social support (n = 202) | High social support (n = 253) | ||
| FDC | 39.23 ± 13.97 | 37.32 ± 12.56 | 1.516 |
| MH | 34.60 ± 6.13 | 41.63 ± 5.79 | −12.465∗∗∗ |
| MI | 19.13 ± 4.35 | 24.15 ± 4.69 | −11.711∗∗∗ |
| PCR | 22.09 ± 2.89 | 23.09 ± 2.47 | −3.964∗∗∗ |
| CC | 46.95 ± 6.00 | 50.15 ± 6.92 | −5.268∗∗∗ |
| D | 11.19 ± 5.21 | 7.91 ± 4.59 | 7.138∗∗∗ |
| A | 45.26 ± 10.30 | 40.83 ± 10.23 | 4.573∗∗∗ |
| I | 15.14 ± 5.35 | 12.36 ± 4.47 | 5.926∗∗∗ |
Note. ∗p.05; ∗∗p.01; ∗∗∗p.001. FDC feeding difficulties of children; MH Marital happiness; MI Marital interaction; PCR parent-child relationship; CC Childcare competence; D Depression; A Anxiety; I Insomnia.
3.3. Test of the measurement model
The results demonstrated good model fit indices: (χ2 = 40.759, df = 11, p < .001, CFI = .986, TLI = .973, RMSEA = .059 (95%CI = .036, .69); SRMR = .027). The factor loadings of three latent variables (marital quality, parenting quality, and mental health risk) ranged from .81 to .92, .77-.80, and .65-.84, respectively, suggesting that latent variables well represented the observed variables well.
3.4. Test of the structural model
Fig. 2 presents the standardized coefficient of the indirect effect model, which revealed good fit statistics: χ2 = 50.069, df = 15, χ2/df = 3.336, RMSEA = .055 (95%CI = .039, .072), CFI = .985, TLI = .971, SRMR = .028. All path coefficients were significant (βs > .012 or < −.197, ps < .05) except for the direct path (β = .074, p > .05).
The mediating effects of marital quality and parenting quality are shown in Table 3. The 95 % confidence interval for the standardized indirect effect did not include zero, indicating significant mediating effects. Specifically, FDs of children had significant indirect effect on mental health risk via marital quality (β = .014, SE = .005, BC95%CI [.007, .025]) or parenting quality (β = .084, SE = .014, BC95%CI [.060, .116]), and both marital quality and parenting quality (β = .012, SE = .004, BC95%CI [.006, .021]). These results indicated that marital quality and parenting quality fully mediated the relationship between FDs of children and mental health risk of mothers.
Table 3.
The bootstrap confidence interval and effect size of the mediation model.
| Mediation paths | Effect | SE |
bias-corrected 95%CI |
||
|---|---|---|---|---|---|
| Lower | Upper | P | |||
| Direct effects | |||||
| FDC -MQ | −.197 | .040 | −.275 | −.121 | .000 |
| FDC -PCR | −.486 | .039 | −.560 | −.405 | .000 |
| MQ -PCR | .356 | .046 | .269 | .448 | .000 |
| MQ -MHR | −.231 | .049 | −.324 | −.131 | .000 |
| PCR -MHR | −.548 | .068 | −.688 | −.417 | .000 |
| FDC -MHR | .074 | .053 | −.035 | .172 | .178 |
| Indirect effects | |||||
| FDC - MQ -MHR | .014 | .005 | .007 | .025 | .000 |
| FDC -PCQ-MHR | .084 | .014 | .060 | .116 | .000 |
| FDC - MQ -PCR-MHR | .012 | .004 | .006 | .021 | .000 |
Note. FDC feeding difficulties of children; PCR parent-child relationship; MQ marital quality; MHR mental health risk.
3.5. Test of group differences
Group differences by social support were tested using multi-group analysis in SEM. Firstly, according to the high-low grouping method of Kelley [50], the top 27 % of the participants with a total score of social support are classified as the high social support group, and the bottom 27%are classified as the low social support group.
Firstly, the indirect effects model was verified in two levels of social support prior to multi-group analysis (high social support as shown in Fig. 2(b): χ2 = 23.410, df = 15, χ2/df = 1.561, RMSEA = .047, CFI = .989, TLI = .979, NFI = .969, SRMR = .032; low social support as shown in Fig. 2(c): χ2 = 28.165, df = 15, χ2/df = 1.878, RMSEA = .066, CFI = .976, NFI = .952, TLI = .956, SRMR = .038). All of the above models showed good indices of fit.
Secondly, as presented in Table 4, Model 1 is unconstrained baseline model, Model 2 constrains the factor loadings to be equal across groups, and Model 3 constrains the factor loadings, item intercepts, and latent means to be equal across groups. The model fit index indicates that one unconstrained baseline model and two constrained models fit well (CFIs > .90, NFIs > .90, RMSEAs < .05, see Table 5). There is a significant difference between model 1 and model 2, Δχ2 = 11.441, p = .034. Furthermore, the differences in the χ2 values between Model 1 and Model 3 were significant (Δχ2 = 25.027, p = .008), indicating that at least one of the parameters was different across two levels of social support. Although all three models provided adequate data-model fit, we selected the measurement residuals constrained model as the final model according to χ2, AIC, and ECVI indexes.
Table 4.
The fitting index of multiple-group analysis model.
| Model | χ2 | df | χ2/df | Δχ2 | p | RMSEA | CFI | NFI | AIC | ECVI |
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | 50.589 | 58 | 1.720 | (--) | .040 | .983 | .962 | 167.589 | .370 | |
| Model 2 | 62.030 | 54 | 1.824 | 11.441 | .034 | .043 | .978 | .954 | 170.030 | .375 |
| Model 3 | 75.616 | 48 | 1.890 | 25.027 | .008 | .044 | .973 | .944 | 171.616 | .379 |
Table 5.
The critical ratios of path coefficient in the multiple-group analysis model.
| Path | path coefficient |
CRD | |
|---|---|---|---|
| 1 | 2 | ||
| MQ-MHR | −.378∗∗∗ | .020 | −2.181∗ |
| PQ-MHR | −.341∗∗∗ | −.793∗∗∗ | 2.297∗ |
Note. PQ parenting quality; MQ marital quality; MHR mental health risk; 1 low social support group; 2.
Thirdly, we utilized critical ratios of differences (CRDs) as an index to examine the differences in the structure path coefficients between two groups. If the CRD was larger than 1.96, then the associations between these two variables would demonstrate a significant difference as p < .05. Table 5 illustrates the results of CRD of path coefficient in the multiple-group analysis model. Specifically, the path coefficient from marital quality to mental health risk in the model of the low social support group (β = −.378, p < .001) was significantly but not in high social support group (β = .020, p > .05), furthermore, the CRD test showed that the path coefficient in high subjective social status and was significantly higher than that in low subjective social status (CRD = -2.181, p < .05). Meanwhile, the path coefficient from parenting quality to mental health risk in the model of the high social support group (β = −.793, p < .001) was significantly lower than the low social support group (β = −.341, p < .001; CRD = 2.297, p < .05). These results demonstrated that social support moderated the relationships between FDs of children and mental health risk of mothers, and marital quality had a more significant effect on the mental health risk in low social support groups.
4. Discussion
Extending previous research on mental health of mother at critical stages of childrearing, this study estimated the prevalence of anxiety, insomnia and depression in a large sample of typical Chinese mother with children 0–3 years, examined the mediating role of marital quality and parenting quality in the link between FDs of children and maternal mental health risk of mothers and assessed the moderating role of social support.
4.1. Prevalence and characteristics of mental health risk
The first finding of the study is that the prevalence of anxiety, depression, and insomnia symptoms was 23.6 %, 50.1 %, and 91.2 % respectively. Although this result is within the estimated range of maternal mental health problems [51,52], it is inconsistent with previous studies [53,54]. For example, Ding, Wang [55] surveyed 214 mothers during hospitalization and found that the prevalence of depression was 24.3 %, which is much lower than this study. Another study reported that a total of 34 % of ordinary residents in six cities in China experienced sleep disorders, which is lower than this study [56]. This discrepancy could be due to the different rating scales used, the different samples selected and the different ways of analysing the data. In addition, up to 90 % of mothers experienced at least one mental health problem, and more than half of them experienced multiple forms of mental health problems, especially three overlapping patterns. It suggests that the critical period of child rearing is a particularly high-risk period for maternal mental health in China. Early parenthood is a difficult and vulnerable period for the majority of mothers, and maternal role stress may trigger acute psychiatric symptoms that surface for the first time [57]. Therefore, it highlights the need to extend to screen probable maternal mental problems from one-year postpartum to three-year postpartum.
4.2. FDs of children and mental health risks of mothers
The second important finding of the study is that FDs of children was found to be significantly associated with mental health risk of mothers. This finding is in line with the second hypothesis and consistent with results of previous studies [58]. Based on the Psychological Stress Theory [59], mothers of children with FDs may experience chronic stress, invest more time and energy into feeding [60], be less inclined to socialize which then may increase their propensity for mental health risks (i.e., anxiety, insomnia and depression) in life [61].
4.3. The mediating effects of marital quality and the parenting quality
The third important finding of the study is that children's FDs had an indirect effect on maternal mental health risks through the mediation of marital quality and parenting quality. This supports the third, fourth and fifth hypotheses.
For the wife role of the marital quality pathway, we found a significant correlation between feeding difficulties and marital quality. And marital quality was negatively correlated with maternal psychological distress. According to role conflict theory [21], a woman's roles as wife and mother often overlap during the critical child-rearing period, creating marital conflict [62], especially when the woman has to deal with the children's feeding difficulties. The frustrated marital interaction would indeed lead to the high levels of negative emotions (i.e. depression, anxiety and insomnia) among mothers [63]. These findings are in line with previous research showing the importance of a good quality relationship for mothers' mental health during the period when children are highly dependent on parental care [64].
For the maternal role of the parenting quality pathway, children's FDs were strongly negatively correlated with parenting quality, and then lower levels of parenting quality would lead to a higher risk of mental health problems. These findings were consistent with the previous research [65]. Based on the stress coping theory [66], FDs of children can be seen as a stressor that would trigger negative appraisals due to overload stress or imbalanced stress. Such appraisals may reduce the quality of parenting. Furthermore, if the stress cannot be resolved for a long time, the parenting quality would be reduced and let mothers might engage in avoidance behaviors and even feel helpless, which would generate mental health risks.
There was also a chain mediating effect of marital quality and parenting quality on the relationship. This suggests that women with lower marital quality are more likely to have lower parenting quality. It supports the family systems theory [6] that family subsystems (e.g. parent-child, marriage) should be understood as interdependent units that influence each other in their emotions, thoughts and behaviour. Thus, our study provides new evidence for the spillover effect between the marriage subsystem and the parent-child subsystem. It can also be speculated that women with a healthy marital relationship are more likely to have a good relationship with their children, which in turn plays a role in promoting maternal mental health throughout life.
4.4. Group comparison by social support
The final important finding of the study is that the moderating effect of social support in the relationships and marital quality had a more significant effect on the mental health risk in low social support groups. This supports the last hypothesis and provides new evidence for the buffering function of social support. Furthermore, the results indicated that the mediating effect significantly varies with high and low levels of social support. Specifically, FDs of children impairs the marital quality or parenting quality, which subsequently weaken mental health in low social support, but not in high social support. It means that the risk of maternal mental health caused by FDs of children can be buffered or reduced by high support from their families or friends.
5. Conclusion
This study investigated the prevalence of mental health risks among Chinese mothers during critical stages of childrearing and the association between feeding difficulties (FDs) of children and these risks. Our findings highlight that feeding difficulties significantly impact the mental health of mothers, influencing anxiety, depression, and insomnia. We also examined the mediating roles of marital quality and parenting quality, revealing that these factors significantly modulate the impact of feeding difficulties on maternal mental health. Additionally, our research explored the moderating effect of social support, underscoring the crucial role of robust social support systems in mitigating the adverse effects of feeding difficulties on maternal well-being. In conclusion, the study underscores the complex interplay between child feeding difficulties, marital quality, parenting quality, and social support in shaping maternal mental health outcomes, emphasizing the need for comprehensive interventions that address both child-related challenges and support systems to promote overall maternal mental health during critical stages of childrearing.
Funding
This work was supported by the Zhejiang Provincial Health Science and Technology Plan Clinical Research Application Project (Grant No. 2022KY1198). The funding body had no role in the design of the study, data collection, analysis, interpretation of data, or writing the manuscript.
Data availability
The data supporting the findings of this study are not public but can be made available upon reasonable request to the corresponding author.
CRediT authorship contribution statement
Qi Liang: Writing – original draft. Zixin Ye: Conceptualization. Chunchan Han: Data curation. Liuzhi Hong: Data curation. Juan Fang: Resources. Jiahui Huang: Data curation. Jiayi Tang: Data curation. Zhaohong Cai: Data curation. Ruiliang Wang: Data curation. Yanlong Liu: Writing – review & editing. Shaochang Wu: Writing – review & editing, Conceptualization. Li Chen: Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Shaochang Wu, Email: lseywsc@163.com.
Li Chen, Email: psychologychenli@163.com.
References
- 1.Hasbani E.C., et al. How parents' feeding styles, attitudes, and multifactorial aspects are associated with feeding difficulties in children. BMC Pediatr. 2023;23(1):543. doi: 10.1186/s12887-023-04369-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Su S., Yan M. Advances in support strategies for preterm infants with oral feeding difficulties. China Nurs. Manag. 2022;22:1569–1573. [Google Scholar]
- 3.Augustin M., et al. Effects of a mobile-based intervention for parents of children with crying, sleeping, and feeding problems: randomized controlled trial. JMIR Mhealth Uhealth. 2023;11 doi: 10.2196/41804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elliott S., Bowen S. Defending motherhood: morality, responsibility, and double binds in feeding children. J. Marriage Fam. 2018;80(2):499–520. doi: 10.1111/jomf.12465. [DOI] [Google Scholar]
- 5.Broerman R. Diathesis-stress model. Encyclopedia of personality and individual differences. 2020:1107–1109. [Google Scholar]
- 6.Becvar R.J., Becvar D.S., Reif L.V. Rowman & Littlefield; 2023. Systems Theory and Family Therapy: A Primer. [Google Scholar]
- 7.Bekiros S., Jahanshahi H., Munoz-Pacheco J.M. A new buffering theory of social support and psychological stress. PLoS One. 2022;17(10) doi: 10.1371/journal.pone.0275364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peverill S., et al. Developmental trajectories of feeding problems in children with autism spectrum disorder. J. Pediatr. Psychol. 2019;44(8):988–998. doi: 10.1093/jpepsy/jsz033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goday P.S., et al. Pediatric feeding disorder: consensus definition and conceptual framework. J. Pediatr. Gastroenterol. Nutr. 2019;68(1):124–129. doi: 10.1097/MPG.0000000000002188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Love P., Walsh M., Campbell K.J. Knowledge, attitudes and practices of australian trainee childcare educators regarding their role in the feeding behaviours of young children. Int. J. Environ. Res. Publ. Health. 2020;17(10) doi: 10.3390/ijerph17103712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meyer I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jackson L., et al. Guilt, shame, and postpartum infant feeding outcomes: a systematic review. Matern. Child Nutr. 2021;17(3) doi: 10.1111/mcn.13141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vizzari G., et al. Feeding difficulties in late preterm infants and their impact on maternal mental health and the mother–infant relationship: a literature review. Nutrients. 2023;15(9) doi: 10.3390/nu15092180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cimino S., Almenara C.A., Cerniglia L. A study on online intervention for early childhood eating disorders during covid-19. Int. J. Environ. Res. Publ. Health. 2022;19(6) doi: 10.3390/ijerph19063696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones C.J., Bryant-Waugh R. Development and pilot of a group skills-and-support intervention for mothers of children with feeding problems. Appetite. 2012;58(2):450–456. doi: 10.1016/j.appet.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 16.Goudet S., et al. Effectiveness of programme approaches to improve the coverage of maternal nutrition interventions in South Asia. Matern. Child Nutr. 2018;14 doi: 10.1111/mcn.12699. Suppl 4 (Suppl 4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duarte-Guterman P., Leuner B., Galea L.A.M. The long and short term effects of motherhood on the brain. Front. Neuroendocrinol. 2019;53 doi: 10.1016/j.yfrne.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Kealy-Bateman W., Pryor L. Marriage equality is a mental health issue. Australas. Psychiatr. 2015;23(5):540–543. doi: 10.1177/1039856215592318. [DOI] [PubMed] [Google Scholar]
- 19.Huntington C., et al. Happy, healthy, and wedded? How the transition to marriage affects mental and physical health. J. Fam. Psychol. 2022;36(4):608–617. doi: 10.1037/fam0000913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zineldin M. TCS is to blame: the impact of divorce on physical and mental health. Int. J. Prev. Med. 2019;10:141. doi: 10.4103/ijpvm.IJPVM_472_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng G., et al. The role conflict-burnout-depression link among Chinese female health care and social service providers: the moderating effect of marriage and motherhood. BMC Publ. Health. 2022;22(1):230. doi: 10.1186/s12889-022-12641-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stryker S., Macke A.S. Status inconsistency and role conflict. Annu. Rev. Sociol. 1978;4(1):57–90. [Google Scholar]
- 23.Abuhammad S., et al. Factors that predict infant temperament: a jordanian study. J. Pediatr. Nurs. 2020;51:e45–e49. doi: 10.1016/j.pedn.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 24.Crenshaw A.O., Leo K., Baucom B.R.W. The effect of stress on empathic accuracy in romantic couples. J. Fam. Psychol. 2019;33(3):327–337. doi: 10.1037/fam0000508. [DOI] [PubMed] [Google Scholar]
- 25.Farr R.H., Tornello S.L. Contemporary Issues in Perinatal Education. Routledge; 2022. The transition to parenthood and early child development in families with LGBTQ+ parents; pp. 92–101. [Google Scholar]
- 26.Feinberg M.E., Kan M.L., Goslin M.C. Enhancing coparenting, parenting, and child self-regulation: effects of family foundations 1 year after birth. Prev. Sci. 2009;10(3):276–285. doi: 10.1007/s11121-009-0130-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris R., et al. Maternal mental health during the neonatal period: relationships to the occupation of parenting. Early Hum. Dev. 2018;120:31–39. doi: 10.1016/j.earlhumdev.2018.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rubio B., et al. Transition to parenthood and quality of parenting among gay, lesbian and heterosexual couples who conceived through assisted reproduction. J. Fam. Stud. 2020;26(3):422–440. [Google Scholar]
- 29.Waldrop J., et al. Parenting interventions and secondary outcomes related to maternal mental health: a systematic review. Matern. Child Health J. 2021;25(6):870–880. doi: 10.1007/s10995-021-03130-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallegos M.L., Segrin C., Thompson A. Parent-child relationships and the health of incarcerated mothers: exploring the mediating role of loneliness. Health Commun. 2021:1–12. doi: 10.1080/10410236.2021.2012014. [DOI] [PubMed] [Google Scholar]
- 31.Arianas E.A., et al. Maternal weight status and responsiveness to preterm infant behavioral cues during feeding. Bmc Pregnancy Childb. 2017;17(1):113. doi: 10.1186/s12884-017-1298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Piro S.S., Ahmed H.M. Impacts of antenatal nursing interventions on mothers' breastfeeding self-efficacy: an experimental study. Bmc Pregnancy Childb. 2020;20(1):19. doi: 10.1186/s12884-019-2701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Don B.P., et al. Interparental positivity spillover theory: how parents' positive relational interactions influence children. Perspect. Psychol. Sci. 2024 doi: 10.1177/17456916231220626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwok S.Y.C.L., et al. The spillover effect of parenting on marital satisfaction among Chinese mothers. J. Child Fam. Stud. 2015;24(3):772–783. [Google Scholar]
- 35.Hosokawa R., Katsura T. A longitudinal study of socioeconomic status, family processes, and child adjustment from preschool until early elementary school: the role of social competence. Child Adolesc Psychiatry Ment Health. 2017;11:62. doi: 10.1186/s13034-017-0206-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valikhani A., et al. Examining the mediating role of perceived stress in the relationship between mindfulness and quality of life and mental health: testing the mindfulness stress buffering model. Anxiety Stress Copin. 2020;33(3):311–325. doi: 10.1080/10615806.2020.1723006. [DOI] [PubMed] [Google Scholar]
- 37.Ajdukovic M., Rajter M., Rezo I. Individual and contextual factors for the child abuse potential of Croatian mothers: the role of social support in times of economic hardship. Child Abuse Negl. 2018;78:60–70. doi: 10.1016/j.chiabu.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 38.Dai Q., et al. Standardized research of Chinese version of the montreal children hospital feeding scale (MCH-FS) Chin J Woman Child Health Res. 2011;22:258–259. [Google Scholar]
- 39.Zhang H. Family income and marital happiness among urban women: mediating of positive marital interaction. Chin. J. Clin. Psychol. 2013;21(2):268–271. [Google Scholar]
- 40.Xu X. Measuring the concept of marital quality as social indicators in urban China. Soc. Indicat. Res. 1996;37:189–206. [Google Scholar]
- 41.Gottman J.M. The roles of conflict engagement, escalation, and avoidance in marital interaction: a longitudinal view of five types of couples. J. Consult. Clin. Psychol. 1993;61(1):6–15. doi: 10.1037//0022-006x.61.1.6. [DOI] [PubMed] [Google Scholar]
- 42.Yang X., et al. The reliability and validity of the Chinese version of parenting sense of competence scale. Chin. J. Nurs. 2014;49(7):881–885. [Google Scholar]
- 43.Johnston C., Mash E.J. A measure of parenting satisfaction and efficacy. J. Clin. Child Psychol. 1989;18(2):167–175. [Google Scholar]
- 44.Zung W.W. The differentiation of anxiety and depressive disorders: a biometric approach. Psychosomatics. 1971;12(6):380–384. doi: 10.1016/S0033-3182(71)71480-7. [DOI] [PubMed] [Google Scholar]
- 45.Lee D.T., et al. Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh Postnatal Depression Scale. Br. J. Psychiatry. 1998;172:433–437. doi: 10.1192/bjp.172.5.433. [DOI] [PubMed] [Google Scholar]
- 46.Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 47.Morin C.M., et al. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hu L.t., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 49.Podsakoff P.M., et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 50.Kelley T.L. The selection of upper and lower groups for the validation of test Items. J. Educ. Psychol. 1939;30(1):17–24. [Google Scholar]
- 51.Rampono J., et al. Transfer of escitalopram and its metabolite demethylescitalopram into breastmilk. Br. J. Clin. Pharmacol. 2006;62(3):316–322. doi: 10.1111/j.1365-2125.2006.02659.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Turgunova L., et al. The incidence of depression among the population of central Kazakhstan and its relationship with sociodemographic characteristics. Behav. Neurol. 2017;2017 doi: 10.1155/2017/2584187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Premji S.S., et al. What stakeholders think: perceptions of perinatal depression and screening in China's primary care system. Bmc Pregnancy Childb. 2021;21(1):15. doi: 10.1186/s12884-020-03473-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Duan G., et al. Patient-controlled intravenous tramadol versus patient-controlled intravenous hydromorphone for analgesia after secondary cesarean delivery: a randomized controlled trial to compare analgesic, anti-anxiety and anti-depression effects. J. Pain Res. 2019;12:49–59. doi: 10.2147/JPR.S184782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ding T., et al. Epidural labor analgesia is associated with a decreased risk of postpartum depression: a prospective cohort study. Anesth. Analg. 2014;119(2):383–392. doi: 10.1213/ANE.0000000000000107. [DOI] [PubMed] [Google Scholar]
- 56.Deng J., et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 2021;1486(1):90–111. doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goco D.E.B., Diliman Q.C. Eexperiences of mothers from dual-career families on child-rearing of their preschool-aged children. Signature. 2019 [Google Scholar]
- 58.Hart S.L., Jackson S.C., Boylan L.M. Compromised weight gain, milk intake, and feeding behavior in breastfed newborns of depressive mothers. J. Pediatr. Psychol. 2011;36(8):942–950. doi: 10.1093/jpepsy/jsr031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Biggs A., Brough P., Drummond S. Lazarus and Folkman's psychological stress and coping theory. The handbook of stress and health: A guide to research and practice. 2017:349–364. [Google Scholar]
- 60.Qin Y., et al. The relationship between social capital and postpartum depression symptoms of lactating women in minority areas—a cross-sectional study from Guangxi, China. Front. Psychol. 2022;13 doi: 10.3389/fpsyg.2022.905028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ruggiero C.F., et al. A mixed methods study of siblings' roles in maternal feeding practices in early childhood: an application of the learning from experience process. Int J Behav Nutr Phy. 2022;19(1):64. doi: 10.1186/s12966-022-01302-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Maman R., Rand D., Avrech Bar M. A scoping review of the maternal role at older age; Perceptions and occupations. Int J Env Res Pub He. 2022;19(1):492. doi: 10.3390/ijerph19010492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kızılırmak A., et al. Correlation between postpartum depression and spousal support and factors affecting postpartum depression. Health Care Women Int. 2021;42(12):1325–1339. doi: 10.1080/07399332.2020.1764562. [DOI] [PubMed] [Google Scholar]
- 64.Bidzan M., Lutkiewicz K. Perceived stress as a predictor of partnership relation quality in polish mothers of preterm-born children. Int. J. Environ. Res. Publ. Health. 2019;16(3) doi: 10.3390/ijerph16030355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chrzan-Detkos M., et al. Improvement of the breastfeeding self-efficacy and postpartum mental health after lactation consultations - observational study. Midwifery. 2021;94 doi: 10.1016/j.midw.2020.102905. [DOI] [PubMed] [Google Scholar]
- 66.Lazarus R.S. Toward better research on stress and coping. Am. Psychol. 2000;55(6):665–673. doi: 10.1037//0003-066x.55.6.665. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are not public but can be made available upon reasonable request to the corresponding author.