Abstract
Auricular acupuncture (AA) is effective in treating various pain conditions, but there have been no analyses of AA for the treatment of pain after ambulatory knee surgery. We assessed the range of analgesic requirements under AA after ambulatory knee arthroscopy. Twenty patients randomly received a true AA procedure (Lung, Shenmen and Knee points) or sham procedure (three non-acupuncture points on the auricular helix) before ambulatory knee arthroscopy. Permanent press AA needles were retained in situ for one day after surgery. Post-operative pain was treated with non-steroidal anti-inflammatory ibuprofen, and weak oral opioid tramadol was used for rescue analgesic medication. The quantity of post-operative analgesics and pain intensity were used to assess the effect of AA. The incidence of analgesia-related side effects, time to discharge from the anesthesia recovery room, heart rate and blood pressure were also recorded. Ibuprofen consumption after surgery in the AA group was lower than in the control group: median 500 versus 800 mg, P = 0.043. Pain intensity on a 100 mm visual analogue scale for pain measurement and other parameters were similar in both groups. Thus AA might be useful in reducing the post-operative analgesic requirement after ambulatory knee arthroscopy.
Keywords: ambulatory surgery, auricular acupuncture, post-operative pain
Introduction
Despite recent advances in therapy for acute post-operative pain, >80% of patients continue to experience distressing pain after ambulatory surgery (1). In order to achieve better post-operative pain relief, improve cost-effectiveness and enhance patient satisfaction, an integrative approach combining pharmacological methods and various complementary non-pharmacological analgesic techniques has been recommended (2). Auricular acupuncture (AA) is effective in treating pain syndromes from various origins (3–5). To our knowledge, there has been no randomized controlled trial (RCT) assessing the effectiveness of AA as a complementary therapy for the relief of acute pain in patients following ambulatory surgery. Therefore, before conducting a large RCT, we performed this study to assess analgesic requirements in patients who received real and sham AA after ambulatory knee arthroscopy (AKA). The results from this analysis could provide the power analysis for a subsequent RCT.
Methods
Patients and Design
After approval from the ethics committee, 20 patients consecutively scheduled for AKA under standardized general anesthesia without premedication were enrolled. Patients were not included if they had a history of opioid medication; were unable to understand the consent form or how to use a 100 mm visual analogue scale for pain measurement (VAS-100, where 0 mm = no pain, 100 mm = the worst pain imaginable); had a history of alcohol abuse, psychiatric disease, or both; had local auricular infection or significant auricular deformation; or had prosthetic cardiac valves. Patients were withdrawn from the study when surgery time exceeded 90 min, arthroscopy was limited to a diagnostic procedure or turned into open surgery, or the expected post-operative pain intensity owing to the type of surgery assessed a priori according to the post-operative pain score was >5 (6).
Patients were informed that they would receive acupuncture at specific points or non-acupuncture points in addition to standard post-operative analgesia. They were divided into two groups by means of sealed envelopes on the day of surgery. Immediately after this, the acupuncturist performed AA of specific points (AA group) or a sham procedure (control group) according to allocation. Only the acupuncturist was aware of patients' allocation between the study groups and had no further personal contact with them after acupuncture. The patients' grouping was un-blinded after all data analysis had been completed.
Auricular Acupuncture
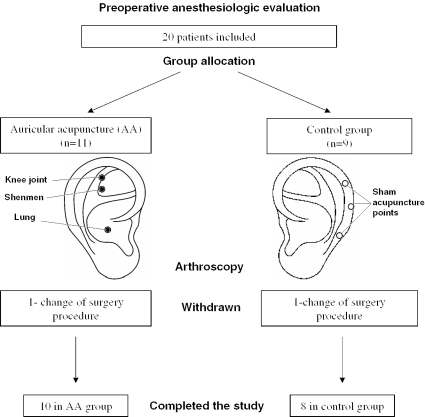
AA was performed by two certified and experienced acupuncturists. Disposable permanent press steel ‘Vinco’ AA needles (Helio Medical Supplies, USA) were inserted before surgery, fixed with flesh-colored adhesive tape and retained in situ after surgery until the following morning. The needles had a diameter of 0.22 mm and were 1.5 mm long. The AA group received acupuncture at three specific acupuncture points ipsilateral to the surgery site: Knee joint, Shenmen and Lung (Figure 1). Non-acupuncture points of the helix ipsilateral to the site of surgery were used for the control procedure. The choice of the specific and sham AA points was based on principles described previously (5). The AA needles were kept in place until the following morning because this is the usual period of maximal post-operative pain after AKA. Localization of both the specific acupuncture points and the non-acupuncture points was confirmed using an electrodermal point finder (Neuralstift SVESA 1070, SVESA, Munich, Germany). This device detects zones of low skin resistance that correspond to acupuncture points (7).
Figure 1.
Flow diagram showing specific and sham auricular acupuncture points (non-acupuncture points of the helix) used in the study.
General Anesthesia and Post-operative Care
Operations were conducted in the mornings and anesthesia was induced intravenously with propofol (1.5–2 mg kg−1) and continuous infusion of remifentanil (0.2 μg kg−1 min−1). Cis-atracurium (0.1 mg kg−1) was used to facilitate tracheal intubation. Lung ventilation with 40% oxygen–air mixture was mechanically controlled to keep end-tidal carbon dioxide at 4.5–5.3 kPa throughout the surgery. Anesthesia was maintained by continuous infusions of propofol (4–8 mg kg−1 h−1) to prevent spontaneous movements during surgery and to ensure that heart rate and mean arterial pressure were within 20% of baseline values. Anesthesiologists performing general anesthesia had no previous AA expertise but were instructed in how to stimulate AA needle sites. Stimulation was manually performed for 5 min by massaging the AA needles before tracheal intubation, during the most painful phase of the surgery (intra-articular installation of the arthroscope) and before extubation. Post-operative analgesia was provided on demand in the anesthesia recovery room using incremental boluses of weak opioid agonist piritramide 0.02 mg kg−1. We aimed at maintaining the patient's pain intensity at <40 mm on VAS-100.
Patients were discharged from the recovery room according to standard discharge criteria after ambulatory surgery (8) and were instructed how to stimulate the AA needles at home by means of massage. They were encouraged to stimulate the needles for 5 min every time they experienced pain >40 mm (VAS-100) and to take oral ibuprofen only 10 min after, if pain persisted. Ibuprofen was titrated in single 200 mg doses at intervals of at least 1 h, to a maximum of 1000 mg, until the follow-up examination. If, after receiving the maximum dose, the patients still experienced pain with intensity VAS >40 mm, oral tramadol 50 mg at 1 h intervals, to a maximum of 200 mg, was allowed as rescue medication. The AA needles were withdrawn during the follow-up examination the next morning and the amount of ibuprofen and tramadol used (self-reported tablet count) was registered. The physicians from the orthopedic surgery department involved in the patient management and data collection were blinded to group allocation and had no previous AA expertise.
Measures of Outcome
The primary endpoint consisted of the tablet count of post-operative ibuprofen taken between surgery and the follow-up examination self-reported by the patients the next morning. The secondary endpoints were pain intensity assessed by the patients on VAS-100 at rest before acupuncture, 30 min after tracheal extubation, on discharge from the anesthesia recovery room and during the follow-up examination; total piritramide requirement in the anesthesia recovery room between surgery and discharge; duration of general anesthesia, time from tracheal extubation to discharge and duration of night's sleep after surgery (in hours) self-reported during the follow-up examination; and the incidence of analgesia-related side effects (nausea and vomiting, sedation and pruritus). Heart rate and blood pressure were taken before and after the AA procedure, 30 min after tracheal intubation, 30 min after tracheal extubation and just before discharge.
Statistical Analysis
Statistical analysis was performed using the SPSS 11.0 statistic package for Mac OS X (SPSS Inc., Chicago, IL USA). Normally distributed continuous data (patient characteristics, pain intensity on VAS-100, duration of general anesthesia and night's sleep, time to discharge, heart rate and blood pressure) were compared using the unpaired Student's t-test. Skewed data (total ibuprofen consumption, total piritramide requirement) were compared using the Mann–Whitney test. The Chi-square test was used to analyze the incidence of analgesia-related side effects. P < 0.05 was considered statistically significant.
Results
Characteristics of Subjects
All patients were Caucasians who had never previously received AA. The data for two patients were withdrawn from the final analysis because the arthroscopic procedure turned into open knee surgery and both were admitted to the in-patient orthopedic surgery department. Eighteen patients completed the study: 10 in the AA group and 8 in the control group. Their results were used for the final assessment (Figure 1). The differences between the groups in terms of age, weight, withdrawal rate and type of surgery were not significant. Sex distribution differed in the two groups: there were more women in the AA group and more men in the control group. A priori assessed intensity of post-operative pain according to the type of surgery during arthroscopy was similar in both groups (Table 1).
Table 1.
Patient characteristics
| AA group (n = 10) | Control group (n = 8) | |
|---|---|---|
| Age (years)* | 33 ± 13 | 45 ± 15 |
| Weight (kg)* | 79 ± 19 | 89 ± 17 |
| Body-mass index (kg m 2)* | 27.1 ± 6.1 | 28.1 ± 6.4 |
| Sex, male/female† | 4/6 | 5/3 |
| Withdrawn from study† | 1 | 1 |
| Type of surgery | ||
| Partial synovectomy | 2 | 2 |
| Meniscus resection | 3 | 3 |
| Lateral release | 4 | 3 |
| Debridement | 1 | |
| A priori assessed pain score+ | 4 (3–5) | 4 (3–4) |
AA = auricular acupuncture.
*Mean 6 standard deviation.
†Number of patients.
+Median (interquartile range).
Comparison of AA and Control Groups
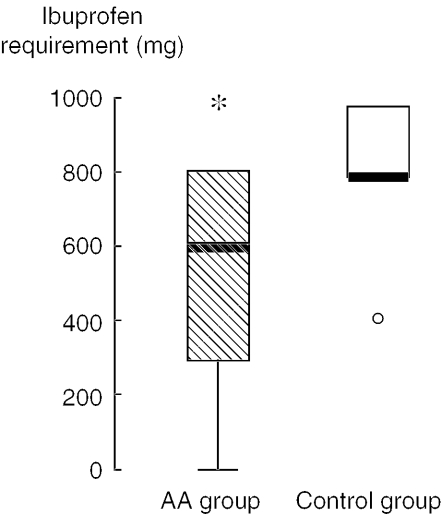
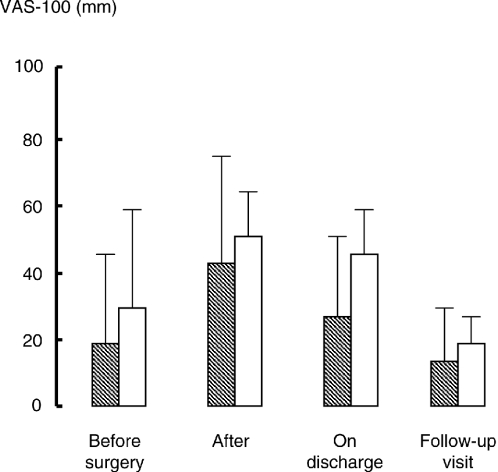
The AA group required less ibuprofen than the control group during the period between surgery and the following morning: median 500 versus 800 mg, P = 0.043 (Figure 2). Two patients from the control group who reached the maximum daily ibuprofen dose used tramadol in addition as a rescue analgesic. No patient from the AA group required rescue tramadol. The total amount of piritramide required by patients after surgery in the anesthesia recovery room before discharge was similar in both the AA and the control groups: median 3.75 versus 3.5 mg, P = 0.696. Pain intensity on VAS-100 was comparable in both groups, showing a trend toward being less in the AA group at all time-points registered (Figure 3). The duration of general anesthesia, the length of night's sleep and the time to discharge were similar in both groups (Table 2). Heart rate and blood pressure were similar in both groups during the course of monitoring (data not shown). Two patients from the AA group and two from the control group required a single dose of atropine (0.5–1 mg) because of hemodynamically relevant bradycardia. No patient reported side effects from pharmacological analgesia or AA.
Figure 2.
Post-operative ibuprofen requirement between surgery and the follow-up examination the next morning, as a box plot. The thick horizontal lines are median values. The outlier represents the patient from the control group who required only 400 mg ibuprofen. *P = 0.043.
Figure 3.
Pain intensity on a visual analogue scale (VAS-100) measured before and after surgery, on discharge from the anesthesia recovery room and during the follow-up examination the next morning. Hatched bars: patients who received true auricular acupuncture; empty bars: control group with sham acupuncture as mean ± standard deviation. The differences are not significant.
Table 2.
Main results
| Outcome measures | AA group (n = 10) | Control group (n = 8) | P |
|---|---|---|---|
| Duration of anesthesia (min)* | 68 ± 12 | 62 ± 11 | n.s. |
| Time to discharge (min)* | 122 ± 65 | 120 ± 53 | n.s. |
| Night sleep (h)* | 5.8 ± 1.6 | 6.3 ± 2.8 | n.s. |
| Piritramide requirement (mg)† | 3.75 (0–7) | 3.5 (0–5) | n.s. |
| Total ibuprofen (mg)† | 500 (200–800) | 800 (800–1000) | 0.043 |
| Tramadol+ | 0 | 2 | n.s. |
| Pain intensity (VAS-100) at follow-up† | 4 (0–25) | 25 (19–29) | n.s. |
AA = auricular acupuncture.
*Mean 6 standard deviation.
†Median (interquartile range).
+Number of patients.
n.s. = not significant.
Discussion
We assessed post-operative analgesic requirements after AKA in patients who received AA applied to specific acupuncture points and in control patients, in whom acupuncture needles were inserted in non-acupuncture sites. In order to obtain reliable results in pain measurement using analgesic requirement as the primary endpoint, the titration of ibuprofen in 200 mg doses was used to achieve similar pain values on VAS-100 in both groups, as had been earlier recommended (9). A uniform general anesthesia scheme was run to exclude potential intra-operative confounding factors for the post-operative analgesic requirement. Reduced post-operative ibuprofen requirement and the decreasing trend of pain intensity the day following surgery compared with the sham procedure suggest an analgesic effect of AA applied to specific acupuncture points. The unequal sex distribution between the two groups (female prevalence in the AA group and male prevalence in the control group) might only have diminished the difference between the groups in terms of ibuprofen requirement (suggested analgesic effect of AA), since women experience more acute pain than men and they also require more non-steroidal anti-inflammatory drugs (10,11). We hesitate to make a final conclusion concerning the analgesic effects of AA based on the widely spread data of this initial study (Figure 2). Nevertheless, these findings will assist in designing a large-scale RCT, in which groups will be balanced with regard to sex and age.
The AA procedure was safe. Some patients had transitory circulatory complications. We are reluctant to explain the cases of bradycardia with the auricular needle insertion, at least in patients from the control group. Vagal stimulation could have been produced only from the acupoint Lung, situated in the middle of the Concha, a well-known innervation zone of the vagal nerve (12). AA was easy to perform under peri-operative clinical conditions using permanent press needles, which were retained in situ for 24 h after surgery.
Our protocol was based on experts' recommendations for acupuncture RCT, which follow CONSORT (Consolidated Standards of Reporting Trials) guidelines for the specific requirements of acupuncture studies (13,14). The homogeneous group of patients and comparable nociceptive field of AKA, supported by a priori assessed expected post-operative pain intensity, were well suited to so-called formulaic AA. Using a particular pattern (prescription) of acupuncture points for all patients with a certain disease, formulaic acupuncture assures the methodological quality of the trial (15).
The choice of sham acupuncture (needling of non-acupuncture points) as a control procedure in our study is based on the fact that the cutaneous penetration of the needles always causes a physiological reaction, e.g. the triggering of neural pathways resulting in diffuse noxious inhibitory control (16). Indeed, it is well known that sham acupuncture produces an analgesic effect in 40–50% of patients, compared with 70% for true acupuncture (17). Clearly, this weak analgesic effect of sham acupuncture may diminish the comparative effect of AA applied to specific points when only two groups (real AA and sham) are compared. In order to estimate the genuine clinical effect of true acupuncture and the placebo effect of sham acupuncture, a third group with standard therapy (without acupuncture) is needed.
To strengthen the reliability of the data, the success of the blinding of patients should be tested in further studies. We presumed that the evaluator in our study was successfully blinded since the pattern of specific AA points could not be distinguished from the sham pattern on the auricular helix. The tape used to attach the AA needles was flesh colored and was barely noticeable on the auricular surface. Nevertheless, we believe that in order to increase the quality and data reliability of future studies, evaluator blinding should also be tested. In order to minimize the influence of intra-operative factors on the post-operative analgesic requirement, the depth of general anesthesia should be monitored and corrected using the measurement of bispectral index and patients' core temperatures (18,19). The findings of our study suggest that AA shows promise for reducing analgesic requirement after AKA. Large-scale randomized investigation of this treatment modality will follow. As recently emphasized for this approach and others, there is still a need for more in-depth analyses that document a biological basis for acupuncture analgesia (20,21).
Acknowledgments
The authors thank Dr. M. Groth for discussing the study design, the personnel of the Polyclinic for Orthopedic Surgery, University Hospital of Greifswald and the patients who participated.
References
- 1.McHugh GA, Thoms GM. The management of pain following day-case surgery. Anaesthesia. 2002;57:270–5. doi: 10.1046/j.1365-2044.2002.2366_2.x. [DOI] [PubMed] [Google Scholar]
- 2.Shang AB, Gan TJ. Optimising postoperative pain management in the ambulatory patient. Drugs. 2003;63:855–67. doi: 10.2165/00003495-200363090-00002. [DOI] [PubMed] [Google Scholar]
- 3.Simmons M, Oleson T. Auricular electrical stimulation and dental pain threshold. Anesth Prog. 1993;40:14–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Vorobiev VV, Dymnikov AA. The effectiveness of auricular microneedle acupuncture at the early postoperative period under conditions of the day surgical department. Vestn Khir im II Grek. 2000;159:48–50. [PubMed] [Google Scholar]
- 5.Usichenko TI, Dinse M, Hermsen M, Witstruck T, Pavlovic D, Lehmann C. Auricular acupuncture for pain relief after total hip arthroplasty—a randomized controlled study. Pain. 2005;114:320–7. doi: 10.1016/j.pain.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 6.Csongradi JJ, Goodman SB, Mihm FG. Surgery of the lower extremities. In: Jaffe RA, Samuels SI, editors. Anesthesiologist's Manual of Surgical Procedures. Philadelphia, PA: Lippincott Williams & Wilkins; 1999. pp. 757–758. [Google Scholar]
- 7.Usichenko TI, Lysenjuk VP, Groth M, Pavlovic D. Detection of ear acupuncture points by measuring the electrical skin resistance in patients before, during and after orthopedic surgery performed under general anesthesia. Acupunct Electrother Res. 2003;28:167–73. doi: 10.3727/036012903815901606. [DOI] [PubMed] [Google Scholar]
- 8.Chung F, Chan VW, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth. 1995;7:500–6. doi: 10.1016/0952-8180(95)00130-a. [DOI] [PubMed] [Google Scholar]
- 9.McQuay HJ, Moore RA. Methods of therapeutic trials. In: Wall PD, Melzack R, editors. Textbook of Pain. Edinburgh: Churchill Livingstone; 1999. pp. 1125–38. [Google Scholar]
- 10.Walker JS, Carmody JJ. Experimental pain in healthy human subjects: gender differences in nociception and in response to ibuprofen. Anesth Analg. 1998;86:1257–62. doi: 10.1097/00000539-199806000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Taenzer AH, Clark C, Curry CS. Gender affects report of pain and function after arthroscopic anterior cruciate ligament reconstruction. Anesthesiology. 2000;93:670–5. doi: 10.1097/00000542-200009000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Peuker ET, Filler TJ. The nerve supply of the human auricle. Clin Anat. 2002;15:35–7. doi: 10.1002/ca.1089. [DOI] [PubMed] [Google Scholar]
- 13.MacPherson H, White A, Cummings M, Jobst K, Rose K, Niemtzow R. Standards for reporting interventions in controlled trials of acupuncture: the STRICTA recommendations. Complement Ther Med. 2001;9:246–9. doi: 10.1054/ctim.2001.0488. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Schulz KF, Altman DG CONSORT GROUP (Consolidated Standards of Reporting Trials) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Intern Med. 2001;134:657–62. doi: 10.7326/0003-4819-134-8-200104170-00011. [DOI] [PubMed] [Google Scholar]
- 15.Patel M, Gutzwiller F, Paccaud F, Marazzi A. A meta-analysis of acupuncture for chronic pain. Int J Epidemiol. 1989;18:900–6. doi: 10.1093/ije/18.4.900. [DOI] [PubMed] [Google Scholar]
- 16.Le Bars D, Dickenson AH, Besson JM. Diffuse noxious inhibitory controls (DNIC). I. Effects on dorsal horn convergent neurones in the rat. Pain. 1979;6:283–304. doi: 10.1016/0304-3959(79)90049-6. [DOI] [PubMed] [Google Scholar]
- 17.Lewith GT, Machin D. On the evaluation of the clinical effects of acupuncture. Pain. 1983;16:111–27. doi: 10.1016/0304-3959(83)90202-6. [DOI] [PubMed] [Google Scholar]
- 18.Sebel PS, Lang E, Rampil IJ, White PF, Cork R, Jopling M, et al. A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg. 1997;84:891–9. doi: 10.1097/00000539-199704000-00035. [DOI] [PubMed] [Google Scholar]
- 19.Doufas AG. Consequences of inadvertent perioperative hypothermia. Best Pract Res Clin Anaesthesiol. 2003;17:535–49. doi: 10.1016/s1521-6896(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 20.Ma SX. Neurobiology of acupuncture: toward CAM. Evid Based Complement Alternat Med. 2004;1:41–7. doi: 10.1093/ecam/neh017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Usichenko TI, Ma SX. Basic science meets clinical research: 10th North American Symposium on Acupuncture. Evid Based Complement Alternat Med. 2004;1:343–4. [Google Scholar]