The implication of neuroinflammatory processes, including blood–brain barrier (BBB) impairment, in psychiatric disorders is gaining more and more attention [1]. So far numerous studies have suggested a disruption of the BBB in schizophrenia, major depression, and bipolar disorder [1, 2]. The blood–cerebrospinal fluid (CSF) barrier on the other hand is greatly understudied, but this picture might be prone to bias due to the use of an inconsistent terminology. While both barriers ensure a stable milieu, which is indispensable for neuronal function, the differentiation between BBB and blood–cerebrospinal fluid barrier (BCB) is of pivotal importance due to substantial differences in morphology and physiology [3]. Many research papers have been published regarding this topic and there is justified hope that this research will improve our mechanistic understanding of neuropsychiatric disorders and foster the development of novel treatments. However, we believe that in the last years, the terminology and the interpretation of findings was subject to a relevant inaccuracy.
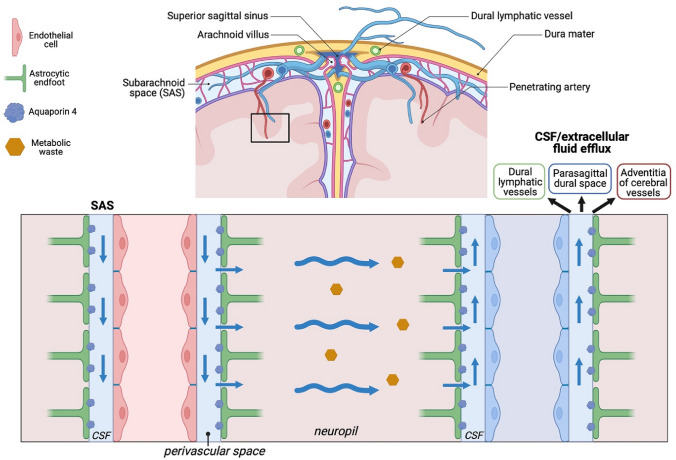
The BBB mainly consists of vascular endothelial cells with tight junctions, basal lamina, pericytes and perivascular space surrounded by astrocytic endfeet (Fig. 1) and is located throughout the brain [3]. The BCB is mainly formed by epithelial cells of the choroid plexus, interconnected by tight junctions, fenestrated blood vessels and subarachnoid epithelial cells facing the CSF [3]. The morphological differences imply variation in transport and permeability of both barriers in health and disease, stressing the importance of accurate distinction between the two.
Fig. 1.
Cerebrospinal fluid flow in the central nervous system. Adapted from [7], created with BioRender
CSF-to-serum albumin ratio (Qalb) has been widely, but wrongfully used as an indirect marker for BBB integrity in psychiatry [1, 2, 4, 5] and neurology [6], since albumin is exclusively produced in the liver and not by the nervous system [3]. The CSF is produced mainly in the choroid plexus, located in brain ventricles, and flows into the subarachnoid space, extending all over the brain and spinal cord, via the lateral and median apertures [7]. Part of the CSF flows in an anterograde manner along the penetrating arteries in the so-called perivascular space and enters the neuropil, supported by the pulsations of the vessels and aquaporin 4 (AQP4) water channels (Fig. 1) [7]. Importantly, the perivascular spaces around penetrating vessels in the brain are the only site, where the CSF borders the BBB. The extracellular fluid (previously CSF) is drained into perivenous spaces. CSF from subarachnoid space and extracellular fluid then leave the intracranial compartment by several different routes including (1) dural lymphatics, (2) parasagittal dural spaces via arachnoid granulations and (3) adventitia of large cerebral vessels (Fig. 1) [7]. Considering the CSF circulation in the brain and the fact that CSF from perivascular spaces (bordering the BBB) eventually leaves the intracranium (hence not proceeding to the lumbar area), it is extremely unlikely that increased Qalb in lumbar CSF results from a BBB disruption [3, 7]. Thus, Qalb should be considered an indirect measure of BCB and not BBB integrity, although other factors such as subarachnoid flow and CSF production might also be relevant [1].
To err is human and in that regard recent biomarker studies [1, 2, 5, 6], including from our working group [8] used and continue to use Qalb as a measure of BBB impairment, drawing inaccurate conclusions regarding the pathophysiology of neuropsychiatric disorders. Even though there is evidence pointing to BBB disruption in neuropsychiatric disorders [1], we argue that this misconception has led to overestimation of the role of BBB and underestimation of the role of BCB, significantly overlooking regions such as the choroid plexus in neuropsychiatric research. Interestingly, choroid plexus epithelium possesses secretory activities that might be relevant in the context of cerebral drug delivery [9]. Given the fact that BBB and BCB differ in antipsychotic in- and efflux, it remains to be investigated how alterations in each barrier impact efficacy and adverse effects of different drugs [1]. In order to specifically investigate the BBB and its implications in neuropsychiatric disorders, novel methods, such as dynamic contrast-enhanced magnetic resonance imaging should find more attention [1].
To facilitate a precise and fruitful discussion and avoid inaccurate conclusions, we strongly encourage the correct, physiology-informed use of terminology on BCB and BBB in neuropsychiatric research.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Footnotes
Vladislav Yakimov and Joanna Moussiopoulou have shared the first authorship.
References
- 1.Pollak TA, Drndarski S, Stone JM, David AS, McGuire P, Abbott NJ (2018) The blood-brain barrier in psychosis. Lancet Psychiatry 5(1):79–92 [DOI] [PubMed] [Google Scholar]
- 2.Orlovska-Waast S, Köhler-Forsberg O, Brix SW, Nordentoft M, Kondziella D, Krogh J et al (2019) Cerebrospinal fluid markers of inflammation and infections in schizophrenia and affective disorders: a systematic review and meta-analysis. Mol Psychiatry 24(6):869–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tumani H, Huss A, Bachhuber F (2017) The cerebrospinal fluid and barriers - anatomic and physiologic considerations. Handb Clin Neurol 146:21–32 [DOI] [PubMed] [Google Scholar]
- 4.Futtrup J, Margolinsky R, Benros ME, Moos T, Routhe LJ, Rungby J et al (2020) Blood-brain barrier pathology in patients with severe mental disorders: a systematic review and meta-analysis of biomarkers in case-control studies. Brain Behav Immun Health 6:100102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rømer TB, Jeppesen R, Christensen RHB, Benros ME (2023) Biomarkers in the cerebrospinal fluid of patients with psychotic disorders compared to healthy controls: a systematic review and meta-analysis. Mol Psychiatry 28(6):2277–2290 [DOI] [PubMed] [Google Scholar]
- 6.Olsson B, Lautner R, Andreasson U, Öhrfelt A, Portelius E, Bjerke M et al (2016) CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol 15(7):673–684 [DOI] [PubMed] [Google Scholar]
- 7.Rasmussen MK, Mestre H, Nedergaard M (2022) Fluid transport in the brain. Physiol Rev 102(2):1025–1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maurus I, Wagner S, Campana M, Roell L, Strauss J, Fernando P et al (2023) The relationship between blood-brain barrier dysfunction and neurocognitive impairments in first-episode psychosis: findings from a retrospective chart analysis. BJPsych Open 9(3):e60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strazielle N, Ghersi-Egea JF (2016) Potential pathways for CNS drug delivery across the blood-cerebrospinal fluid barrier. Curr Pharm Des 22(35):5463–5476 [DOI] [PMC free article] [PubMed] [Google Scholar]