Abstract
Lipoleiomyosarcoma is a malignant tumor of both mesenchymal and smooth muscle origin. Lipoleiomyosarcoma is a very rare type of retroperitoneal sarcoma, which by itself is a rare type of soft tissue sarcoma. Lipoleiomyosarcoma is a very rare subtype of liposarcoma, which is the most common type of retroperitoneal sarcoma. To our best review of available literature, this was the first case of lipoleiomyosarcoma presenting as a massive retroperitoneal mass of size 50 × 50 × 30 cm, managed with multi-visceral R0 resection. The computed tomography of the abdomen showed a massive fat density lesion with internal soft density lesions and internal calcifications. Multivisceral resection was planned and executed and achieved R0 resection. We suggest that lipoleiomyosarcoma should be included in differential diagnosis of retroperitoneal tumors, and multi-visceral R0 resection should be considered as an option for lipoleiomyosarcoma, as these tumors have very good prognosis with R0 resection.
Keywords: Lipoleiomyosarcoma, Retroperitoneal sarcoma, Soft tissue sarcoma, Multivisceral resection
Introduction
Lipoleiomyosarcoma is a malignant tumor of both mesenchymal and smooth muscle origin [1]. Retroperitoneal sarcomas are rare tumors, which account for around 15% of all soft tissue sarcomas [2]. Lipoleiomyosarcoma is a very rare neoplasm with very few case reports and one study reported in history [1, 3, 4]. We present a case report of a case of massive retroperitoneal sarcoma which was unusually very large, of size 50 cm, which was managed surgically.
Case Report
A 35-year-old male presented with complaints of abdominal distension and vague abdominal pain for the past 3 months. He had no altered bladder or bowel habits. A clinical image of the patient with abdominal distension is shown in Fig. 1.
Fig. 1.
Clinical image of the patient with abdominal distension
Contrast enhanced computed tomography (CECT) of the abdomen was done and found to have 31 × 38 × 39 cm fat density lesion with internal soft density lesions and internal calcification. Lesion abuts the pancreas, abdominal wall, aorta, inferior vena cava, psoas muscle, and urinary bladder as shown in Fig. 2.
Fig. 2.
Contrast Enhanced Computed Tomography abdomen showing massive retroperitoneal mass abutting pancreas, abdominal wall, aorta, inferior vena cava, psoas muscle, and urinary bladder
Ultrasonography-guided biopsy of the abdominal mass was done, and the report came negative for malignancy. As the imaging features suggest high suspicion of malignancy, surgery was planned. According to NCCN guidelines, if imaging is suggestive of liposarcoma, surgery can be proceeded, even with a negative biopsy report.
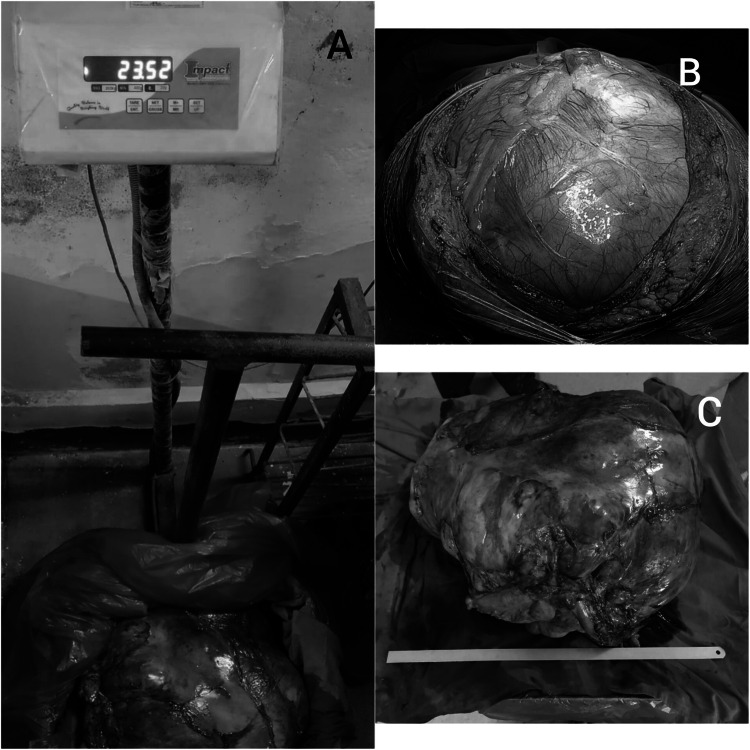
Intraoperatively, a mass of size 50 × 50 × 30 cm was found and was adherent to the left kidney and descending colon. Mass excision in toto with left kidney, left adrenal gland, and descending colon segmental resection was done. Intraoperative image and postoperative specimen are shown in Fig. 3.
Fig. 3.
A) post-operative specimen with weight of 23 kg is shown in the picture. B) intra-operative image of the mass to be resected C) post operative specimen of multivisceral resection for lipoleiomyosarcoma. Mass excised in toto with left kidney, left adrenal gland and a small segment of descending colon
The postoperative biopsy report was suggestive of well-differentiated liposarcoma. The immunohistochemistry report came as lipoleiomyosarcoma. The histological images are shown in Fig. 4.
Fig. 4.
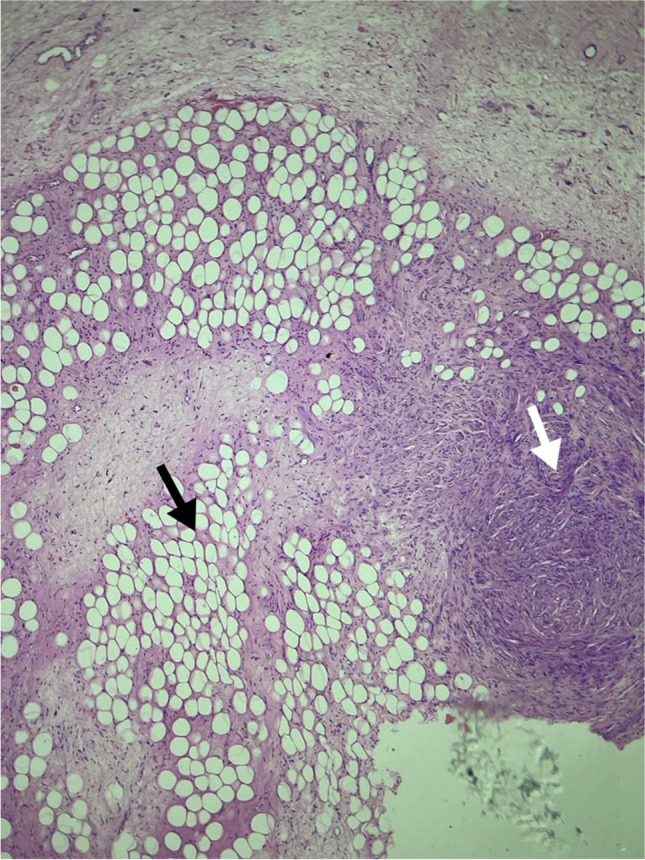
Histopathological image of lipoleiomyosarcoma. White arrow shows leiomyosarcomatous component. Black arrow shows lipomatous component of the tumor
The postoperative period was uneventful. The patient recovered well and was discharged on the 7th postoperative day. The patient was followed up for one and a half years till now, and a recent computed CECT abdomen showed no evidence of recurrence.
Discussion
Lipoleiomyosarcoma is a rare malignant neoplasm; its first case was reported by Evans in 1990 [5]. Since then, very few case reports and one clinicopathological study have been published in the literature as shown in Table 1.
Table 1.
Case reports and clinicopathological studies published in the literature
| S. no | Reference | Number of cases | Location (number of cases) |
|---|---|---|---|
| 1 | Evans(1990) [5] | 3 | Scrotum (1), mediastinum (1), abdomen (1) |
| 2 | Talini et al. (1993) [9] | 2 | Retroperitoneum (2) |
| 3 | Suster et al. (1993) [10] | 2 | Scrotum (1), retroperitoneum (1) |
| 4 | Evans et al.(1994) [11] | 1 | Abdomen (1) |
| 5 | Gomez- Roman et al. (1997) [12] | 1 | Mediastinum (1) |
| 6 | Andrew L Folpe et al. (2002) [1] | 9 | Popliteal fossa (1), mediastinum (1), retroperitoneum (2), lung (1), abdomen (1), scrotum (1), inguinal (2) |
| 7 | Jha et al. (2007) [13] | 1 | Uterus (1) |
| 8 | Hwang et al. (2010) [14] | 1 | Uterus (1) |
| 9 | Lee et al. (2012) [15] | 2 | Uterus(2) |
| 10 | Veronique Drapeau-Zgoralski (2017) [16] | 1 | Uterus (1) |
| 11 | J-J Tong (2018) [3] | 1 | Posterior mediastinum (1) |
| 12 | Wasim Firoz Khan (2019) [4] | 1 | Spermatic cord (1) |
| 13 | Present study | 1 | Retroperitoneal (1) |
Malignant lesions are four times more common than benign lesions in the retroperitoneum, unlike elsewhere in the body [6]. Nearly more than 50% of retroperitoneal tumors are more than 20 cm at presentation [7]. Liposarcoma and leiomyosarcoma are the most common types of retroperitoneal sarcoma [8]. Liposarcoma has three biological groups: atypical lipomatous tumor/well-differentiated and dedifferentiated, myxoid round cell, and the pleomorphic type. The most common is the well-differentiated and dedifferentiated category [8]. Lipoleiomyosarcoma is a rare tumor that is found to have smooth muscle components within liposarcoma. It seems that the smooth muscle component originates from the vessels in the tumor and its typically low grade, and the behavior of the tumor is very similar to well-differentiated liposarcoma [1].
These tumors histologically have well-differentiated smooth muscle with no nuclear atypia [1]. According to the NCCN guidelines, Soft Tissue Sarcoma, Version 1.2023, in these types of tumors, R0 resection is the mainstay of treatment. A preoperative biopsy is not mandatory unless neoadjuvant therapy is planned.
The other important differential diagnosis for lipoleiomyosarcoma is dedifferentiated liposarcoma which has a leiomyosarcoma component in the dedifferentiated part of liposarcoma. These are high-grade sarcoma with a bad prognosis [1].
L Folpe et al. presented in 2002 a retrospective case series of nine cases of lipoleiomyosarcoma and concluded that these tumors also have significant local recurrence risk and have advised R0 resection as the mainstay of treatment [1]. A total of only around 25 cases were reported in the literature as shown in Table 1.
We present this case, in which we did multi-visceral R0 resection and managed this rare case of lipoleiomyosarcoma of size 50 × 50 × 30 cm, which was a great surgical adventure and test for a surgeon’s skill.
Conclusion
A multi-visceral resection is a feasible option that can be tried by doing exploratory laparotomy for patients who have a mass with multi-organ involvement. Lipoleiomyosarcoma has a good prognosis with R0 resection, even if it is done by doing a multi-visceral resection.
Acknowledgements
I would like to express my gratitude for my fellow colleagues and my professors for guiding me to write this report.
Declarations
Competing Interests
The authors declare no competing interests.
Patient ‘s Consent Statement
Patient’s identity is not exposed in this article, and permission was taken from the patient regarding publication. Institute committee clearance for publication was obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Folpe AL, Weiss SW (2002) Lipoleiomyosarcoma (well-differentiated liposarcoma with leiomyosarcomatous differentiation): a clinicopathologic study of nine cases including one with dedifferentiation. Am J Surg Pathol 26(6):742–749. 10.1097/00000478-200206000-00007 [DOI] [PubMed] [Google Scholar]
- 2.Pisters PWT, Weiss M, Maki R. Soft-Tissue Sarcomas. https://pdfs.semanticscholar.org/61b9/cfc10b9c36dbb931aa95e3fea0b81d9b5018.pdf
- 3.Tong JJ, Li XJ, Li GX, Qian GQ (2018) Lipoleiomyosarcoma of the posterior mediastinum. QJM 111(3):191–192. 10.1093/qjmed/hcx256 [DOI] [PubMed] [Google Scholar]
- 4.Khan WF, Rathore YS, Aduri RS, Mridha AR (2019) Lipoleiomyosarcoma of spermatic cord: an unusual presentation. BMJ Case Rep 12(8):e228952. 10.1136/bcr-2018-228952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans HL (1990) Smooth muscle in atypical lipomatous tumors. A report of three cases. Am J Surg Pathol 14(8):714–8. 10.1097/00000478-199008000-00002 [DOI] [PubMed] [Google Scholar]
- 6.Van Roggen JF, Hogendoorn PC (2000) Soft tissue tumours of the retroperitoneum. Sarcoma 4(1–2):17–26. 10.1155/S1357714X00000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cormier JN, Pollock RE (2004) Soft tissue sarcomas. CA Cancer J Clin 54(2):94–109. 10.3322/canjclin.54.2.94 [DOI] [PubMed] [Google Scholar]
- 8.Choi JH, Ro JY (2020) Retroperitoneal sarcomas: an update on the diagnostic pathology approach. Diagnostics (Basel) 10(9):642. 10.3390/diagnostics10090642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tallini G, Erlandson RA, Brennan MF, Woodruff JM (1993) Divergent myosarcomatous differentiation in retroperitoneal liposarcoma. Am J Surg Pathol 17(6):546–556. 10.1097/00000478-199306000-00002 [DOI] [PubMed] [Google Scholar]
- 10.Suster S, Wong TY, Moran CA (1993) Sarcomas with combined features of liposarcoma and leiomyosarcoma. Study of two cases of an unusual soft-tissue tumor showing dual lineage differentiation. Am J Surg Pathol 17(9):905–11. 10.1097/00000478-199309000-00006 [DOI] [PubMed] [Google Scholar]
- 11.Evans HL, Khurana KK, Kemp BL, Ayala AG (1994) Heterologous elements in the dedifferentiated component of dedifferentiated liposarcoma. Am J Surg Pathol 18(11):1150–1157. 10.1097/00000478-199411000-00009 [DOI] [PubMed] [Google Scholar]
- 12.Gómez-Román JJ, Val-Bernal JF (1997) Lipoleiomyosarcoma of the mediastinum. Pathology 29(4):428–430. 10.1080/00313029700169475 [DOI] [PubMed] [Google Scholar]
- 13.Jha A, Sayami G, Adhikari D (2007) Lipoleiomyosarcoma an extremely unusual sarcoma of uterus: a case report. Nepal J Obstetrics Gynaecol 2(1):67–70. 10.3126/njog.v2i1.1482 [Google Scholar]
- 14.Hwang EJ, Lim MC, Kim EN, Kwon Y, Hong EK, Jung DC et al (2010) Lipoleiomyosarcoma of the uterus: a case report and review. Korean J Obstetrics Gynecol 53(11):1019–1023. 10.5468/kjog.2010.53.11.1019 [Google Scholar]
- 15.Lee HP, Tseng HH, Hsieh PP, Shih TF (2012) Uterine lipoleiomyosarcoma: report of 2 cases and review of the literature. Int J Gynecol Pathol 31(4):358. 10.1097/PGP.0b013e31823f841f [DOI] [PubMed] [Google Scholar]
- 16.Drapeau-Zgoralski V, Doyon J, Berthiaume MJ, Mottard S (2017) Uterine lipoleiomyosarcoma: complete medullary compression as presentation of a solitary metastasis. Gynecol Oncol Rep 25(21):7–9. 10.1016/j.gore.2017.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]