Abstract
Background:
Ocular trauma is the leading cause of monocular blindness in children. This study aimed to identify and compare pediatric ocular injuries at two national university hospitals: Benha University Hospital (BUH) and South Valley University Hospital (SVUH) while evaluating the predictive utility of the Ocular Trauma Score (OTS) for post-traumatic permanent visual infirmity.
Design and methods:
This multicenter observational study enrolled children under 18 years at BUH and SVUH Ophthalmology Departments from May 31 to December 31, 2022. Comprehensive medical histories and detailed data on eye trauma were obtained, with each undergoing thorough eye examinations at the initial presentation and during the 6-month follow-up period. The final visual outcome was permanent visual infirmity that was defined as the Best Corrected Visual Acuity in the better eye worse than 3/60 or near vision worse than N6 according to the International Classification of Diseases 11.
Results:
The study included 120 cases evenly distributed between the two hospitals, with a mean age of 10.03 (±3.30) years, 74.17% male and 51.67% urban residents. Blunt, sharp, and foreign objects were the most common causes (39.17%, 33.33%, and 11.67%, respectively). Closed-globe injuries prevailed at BUH (83.33%) than SVUH (40.0%). Most injuries were accidental and outdoors, with an average interval of 9.93 (±23.57) hours to seek medical care. Lack of education, open-globe injuries, poor initial visual acuity, longer intervals from admission to intervention, and lower OTS were associated with visual impairment.
Keywords: Eye trauma, pediatric, upper and lower Egypt, medicolegal, ocular trauma score
Introduction
Ocular trauma (OT) is any injury to the eye or its surrounding structures that is caused by blunt force impact, sharp objects, chemicals, or thermal burns. 1 Ocular trauma can lead to many complications owing to the delicate nature of ocular tissues. A range of ocular complications based on the causative agent including, but is not limited to, corneal damage, lens opacities, lens dislocation, glaucoma, vitreous hemorrhage, retinal tears, retinal detachment, and traumatic optic neuropathies. 2
Ocular trauma remains a major public health concern, particularly among males and young adults. 3 Even minor ones, can result in a high economic burden to both families and countries due to factors including the absence time from work or schools, burden of hospital stays, cost of investigations, medications, interventions required, follow up, and the rehabilitation needed afterward. 4 Medicolegal cases usually do not present immediately after trauma. They present over varying periods of trauma, which may be weeks or days. 5 Early and accurate recording of medicolegal aspects such as the causative agent and the circumstances of injury are essential for possible litigations as well as for further clinical evaluation and prognosis of ocular trauma. 6
Ocular injuries can be divided into open globe or closed globe injuries based on a standardized ocular trauma classification system. When there is a full thickness injury of the cornea and/or sclera it is defined as an open globe injury, whereas the closed globe injury represents an ocular contusion or partial thickness injury of cornea and/or sclera.7,8 It is also important to report the factors that can lead to increased likelihood of visual infirmity at final follow-up, including severity of trauma, pattern of globe injury (open or closed), zone affected by injury, time delay in seeking medical care, timing of delivering medical and/or surgical care, and the presence or absence of infection. 9
An Ocular Trauma Score (OTS) was developed by the Ocular Trauma Classification Group to provide a systematic method for describing mechanical eye trauma, guide the perspectives of patients and their families, help decision-making by physicians, and predict visual outcomes at a 6-month period. The score ranges from 1 (corresponding to the worst prognosis) to 5 (corresponding to the least poor prognosis). An 80% predictive accuracy has been linked to OTS in relation to open-globe injuries. 10 A Pediatric OTS (POTS) was developed as a prognostic tool in penetrating eye injuries in children. However, it showed an underestimation of final visual acuity due to lower scores given for initial visual acuity and more scores given for associated ocular tissue injuries, which did not appear to indicate a poor visual prognosis.11,12 Thus, in our study, the use of OTS was used as a universal prognostic tool.
Pediatric ocular injuries are of specific concern due to more difficult treatment and serious complications. 13 Eye trauma represents the most common cause of unilateral blindness especially in developing countries. 14 About 3.3–5.7 million pediatric eye injuries occur annually worldwide with the majority of these occurring in rural areas. About half of these cases necessitate inpatient care. 15 In developing countries, ocular trauma is more prevalent and causes more serious complications. 16 Pediatric eye injuries carry a major socioeconomic and psychological impact.
In Egypt, there are limited reports on the incidence of ocular trauma and its impacts. However, about a 50% increase in pediatric ocular trauma has been reported. 17 Thus, this study aimed to identify the patterns, risk factors, and visual outcomes of ocular trauma after a 6-month follow up period in children below 18 years of age, at two national university hospitals: Benha University Hospital (BUH) and South Valley University Hospital (SVUH). This study also aimed to evaluate the role of OTS in the prediction of post-traumatic visual outcomes in children. The findings will be used to develop recommendations to reduce the incidence of ocular trauma and improve emergency department management.
Patients and methods
Study design and ethical concern
This study is a prospective observational multicenter hospital-based study conducted in the Departments of Ophthalmology of two university hospitals in Egypt which are: Benha University Hospital, Qalyubia Governorate, representing Lower Egypt, and South Valley University Hospital, Qena Governorate, representing Upper Egypt. Enrollment of patients took a period of 6-month period (May 31 to December 31, 2022), and patients were followed for 6 months.
The study was approved by the Scientific Research Ethics Committee of the Faculty of Medicine, South Valley University “SvuMEDOPH026/4/22/3/363,” and the study was conducted in accordance with the ethical standards laid down by the Declaration of Helsinki. A written informed consent was obtained from the legal guardian for each participating subject and confidentiality of the data was considered.
Study settings
The study was conducted at two national tertiary hospitals in Egypt. Benha University Hospital, Benha City, the Capital of Qalyubia Governorate, one of the Greater Cairo governorates, with a population of about 6 million people. BUH has highly qualified medical staff and good equipment and facilities. BUH provides outpatient and inpatient services, emergency service, and receives referrals from other hospitals and health centers in a wide geographic region extending to neighboring governorates due to its strategic location in the Nile Delta region. The other is South Valley University Hospital, one of the largest hospitals in Upper Egypt, located in Qena Governorate on the eastern bank of the Nile river, which is inhabited by more than 3.5 million people. SVUH provides a wide range of medical services to the southern region of the country, including emergency care, specialized treatment, and advanced surgeries.
In Egypt, children start kindergarten (preschool stage) at the age of four, move to primary school at age of six, then the preparatory school at the age of 12, and start high school at the age of 15 years.
Patient eligibility criteria
The study enrolled pediatric patients 18 years old and younger who had experienced ocular trauma, including injuries to the eye and/or ocular adnexa, and presented to the emergency section of the Ophthalmology Department of the two previously mentioned hospitals. Exclusion criteria were patients whose parent or legal guardian did not consent to their enrollment in the study, patients with previous eye diseases affecting visual acuity, patients with previous ocular trauma, or previous ocular surgery in the studied eye.
Study participants
The study included a total of 120 cases with pediatric ocular trauma. Half of them were recruited from each hospital upon admission. Cases were enrolled sequentially from each hospital till the target sample was achieved, which took a period of 6 months.
Data collection
History: On hospital admission, a full history was taken from patients or their guardians. Information about patients’ sociodemographic characteristics, including age, gender, residence (rural or urban), educational level, and occupation (if applicable), were obtained. History of ocular or systemic diseases, surgical procedures, any known drug or food allergies, trauma, glasses wearing or known amblyopia, habits, and family history of eye and systemic diseases was also obtained. Medicolegal aspects of ocular trauma were collected including: (i) the etiology of ocular injury that was classified into mechanical agents (such as blunt objects, sharp objects, road traffic injuries, fall from height, fall on the ground, animal origin, plant origin, fight, foreign body, and gunshot pellets), and non-mechanical (such as thermal injuries and chemical injuries), (ii) the manner of ocular trauma whether accidental, homicidal, or suicidal, (iii) whether the injury affects the globe, adnexa, or both, (iv) laterality of eye injury, and (v) the place of eye trauma (whether indoor or outdoor). The time of injury (by day or night), time lapse to presentation to healthcare, and time from presentation to intervention were also recorded.
Eye examination: Every patient had a full eye examination of admission, including assessment of visual acuity, slit lamp examination, fundus examination, intraocular pressure measurement, and gonioscopy, as applicable. B-scan and Computerized Tomography (CT) scan of the eye were also carried out when indicated. The zone of ocular injury was described as external (limited to bulbar conjunctiva, sclera, and cornea), anterior segment (includes structures of the anterior segment and the pars plicata), posterior segment (all internal structures posterior to the posterior lens capsule), and mixed.18,19 The ocular injury was classified at initial presentation into Open Globe Injuries (OGIs) and Closed Globe Injuries (CGIs) according to the ocular trauma classification group system. 19 OTS was calculated for each patient at the time of start of management as described in Table 1. 10 The outcome of ocular trauma was defined as permanent visual infirmity or no permanent visual infirmity after 6 months. The Best Corrected Visual Acuity (BCVA) was recorded at the initial visit and on every follow up visit whenever possible. BCVA was obtained using the appropriate method according to the age of patient. BCVA was classified according to the International Classification of Diseases 11 (ICD11) for vision impairment. No impairment was considered at BCVA better than 6/12 in better eye. Mild, moderate, and severe visual impairment were corresponding to BCVA in better eye worse than 6/12, 6/18, and 6/60, respectively. Blindness (the working definition of visual infirmity) was defined as BCVA in the better eye worse than 3/60 or near vision worse than N6.20,21
Table 1.
Calculating the OTS: variables and raw points.
| Variables | Raw points |
|---|---|
| Initial vision | |
| NLP | 60 |
| LP/HM | 70 |
| 1/200–19/200 | 80 |
| 20/200–20/50 | 90 |
| ≥ 20/40 | 100 |
| Rupture | −23 |
| Endophthalmitis | −17 |
| Perforating injury | −14 |
| Retinal detachment | −11 |
| Afferent pupillary defect | −10 |
NLP: no light perception; LP: light perception; HM: Hand motion (Scott, 2015).
Patients were managed at presentation as follows: Cases presented with open globe injury in the form of corneal lacerations underwent corneal suturing using 10/0 Nylon sutures under general anesthetic. Patients with scleral lacerations underwent surgical repair of the sclera using 8/0 virgin silk sutures. No patients with hyphaema had corneal bloodstaining or glaucoma. Patients with intraocular foreign body had uneventful vitrectomy operations. All patients with OGI in the study underwent primary repair only. No further procedures were needed for any patient during the study period. We did not encounter any intraoperative or postoperative complications during the study including postoperative corneal leak, wound gaping, wound infection, dehiscence, endophthalmitis, post-operative hypotony, surgical-induced glaucoma, steroid-induced glaucoma, choroidal detachment, or suprachoroidal hemorrhage. No patients had any allergic reaction from any postoperative treatment given. No patients had to return to the theater for revision of their procedures.
Patients were followed up on the first day, first week, first month, third month, and at sixth month. At each visit, BCVA, slit lamp examination, fundus examination, and intraocular pressure check were carried out when applicable. Only (82.5%) 99/120 patients completed 6-months follow up, and were considered for final visual outcome analysis.
Statistical analysis
Statistical analyses were carried out using MS Excel and STATA/SE version 11.2 for Windows (STATA Corporation, College Station, Texas). Descriptive statistics such as mean, Standard Deviation (SD), range, and frequency were used as appropriate. Univariate tests such as the Chi-square test (X2), Fisher Exact Test (FET), Student t-test (t), Mann-Whitney test (z), One-way Analysis of Variance (ANOVA; F), and Kruskal Wallis test (kX2) were used to compare data between the different study groups as appropriate. The prediction of final visual infirmity conditioned on OTS was examined using the Receiver Operator Characteristic ROC curve to estimate the best cut-off value and the corresponding sensitivity, specificity, predictive value positive, and predictive value negative. A two-way p-value < 0.05 was considered statistically significant.
Results
The study recruited 120 cases with eye injuries presented to BUH and SVUH. Males constituted 74.17% (n = 89) of them. The age of cases ranged from 3 to 18 years with an average of 10.03 (±3.30) years. About 51.67% of participants were from urban areas, the majority were school students (77.50%, n = 93), and 14 cases were illiterate and all were admitted to SVUH. Table 2 shows the sociodemographic characteristics of cases recruited from the two hospitals. Most injuries were due to accidents (85.83%; n = 103) that occurred outdoors (70.00%; n = 84), and at night (54.17%; n = 65).
Table 2.
Sociodemographic characteristics and ocular injury context in the studied children.
| Variable | BUH (n = 60) | SVUH (n = 60) | Test | p | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Gender | Female | 11 | 18.33 | 20 | 33.33 | X2 = 3.52 | 0.06 |
| Male | 49 | 81.67 | 40 | 66.67 | |||
| Age (years) | Mean ± SD Range |
9.55 ± 4.11 3–18 |
10.52 ± 2.15 5–15 |
t = 1.61 | 0.11 | ||
| 0–4 | 7 | 11.67 | 0 | 0.00 | FET | <0.001 | |
| 5–9 | 25 | 41.67 | 15 | 25.00 | |||
| 10–14 | 16 | 26.67 | 44 | 73.33 | |||
| 15–18 | 12 | 20.00 | 1 | 1.67 | |||
| Residence | Rural | 29 | 48.33 | 29 | 48.33 | X2 = 000 | 1.00 |
| Urban | 31 | 51.67 | 31 | 51.67 | |||
| Occupation | None | 0 | 0.00 | 13 | 21.67 | FET | <0.001 |
| Preschool/kindergarten | 7 | 11.67 | 0 | 0.00 | |||
| Student | 53 | 88.33 | 42 | 70.00 | |||
| Worker | 0 | 0.00 | 5 | 8.33 | |||
| Educational level | Under school age a | 12 | 20.00 | 1 | 1.67 | FET | <0.001 |
| Illiterate b | 0 | 0.00 | 14 | 23.33 | |||
| Primary/read & write | 32 | 53.33 | 39 | 65.00 | |||
| Preparatory | 10 | 16.67 | 6 | 10.00 | |||
| Secondary | 6 | 10.00 | 0 | 0.00 | |||
| Place of injury | Indoor | 18 | 30.00 | 18 | 30.00 | X2 = 0.00 | 1.00 |
| Outdoor | 42 | 70.00 | 42 | 70.00 | |||
| Time of injury | Day | 35 | 58.33 | 20 | 33.33 | X2 = 7.55 | 0.006 |
| Night | 25 | 41.67 | 40 | 66.67 | |||
| Manner of injury | Accidental | 54 | 90.00 | 49 | 81.67 | X2 = 1.71 | 0.19 |
| Homicidal | 6 | 10.00 | 11 | 18.33 | |||
BUH: Benha University Hospital; SVUH: South Valley University Hospital; X2: Chi-square test; FET: Fisher Exact Test; t: Student t-test.
p < 0.05 was considered statistically significant.
<6 years of age.
Children who did not have school education, or early dropped out of school.
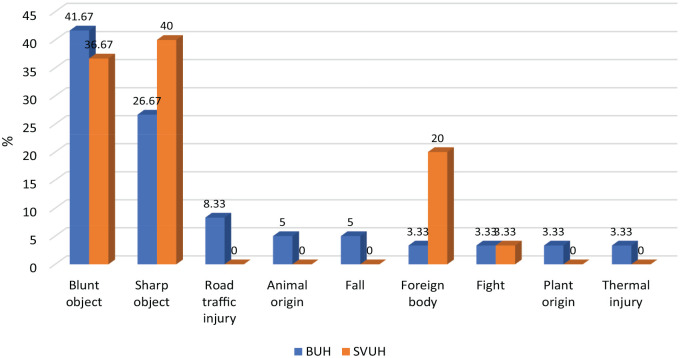
The frequency distribution of the different causes of eye injuries is demonstrated in Figure 1. Blunt objects, sharp objects, and foreign bodies were the most frequent causes (39.17%, 33.33%, and 11.67%, respectively). Road traffic injuries and fights were the cause of 4.17% and 3.33% of injuries, respectively. Eye injuries caused by animals and falls were 2.50%, and thermal eye injuries and injuries of plant origin were 1.67%. Foreign bodies-induced eye injuries were more frequent in cases admitted to SVUH than BUH (p = 0.004). While road traffic injuries were more frequent in BUH (p = 0.02).
Figure 1.
Causes of studied pediatric eye injuries by region.
BUH: Benha University Hospital; SVUH: South Valley University Hospital.
The majority of eye injuries were Closed Globe Injuries (CGIs; 61.67%). CGIs were more frequent among cases admitted to BUH (83.33%), compared to 40.0% among cases admitted to SVUH (p < 0.001). External and anterior zone eye injuries were the most prevalent forms of eye injuries (p = 0.001), as shown in Table 3.
Table 3.
Types of pediatric eye injuries.
| Variable | BUH (n = 60) | SVUH (n = 60) | Test | p | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Type of injury | CGI | 50 | 83.33 | 24 | 40.00 | X2 = 23.83 | <0.001 |
| OGI | 10 | 16.67 | 36 | 60.00 | |||
| Zone of eye injury | External | 21 | 35.00 | 14 | 23.33 | FET | 0.001 |
| Anterior | 31 | 51.67 | 30 | 50.00 | |||
| Anterior + posterior | 3 | 5.00 | 16 | 26.67 | |||
| Posterior | 5 | 8.33 | 0 | 0.00 | |||
BUH: Benha University Hospital; SVUH: South Valley University Hospital; CGI: Closed Globe Injury; OGI: Open Globe Injury; X2: Chi-square test; FET: Fisher Exact Test.
p < 0.05 was considered statistically significant.
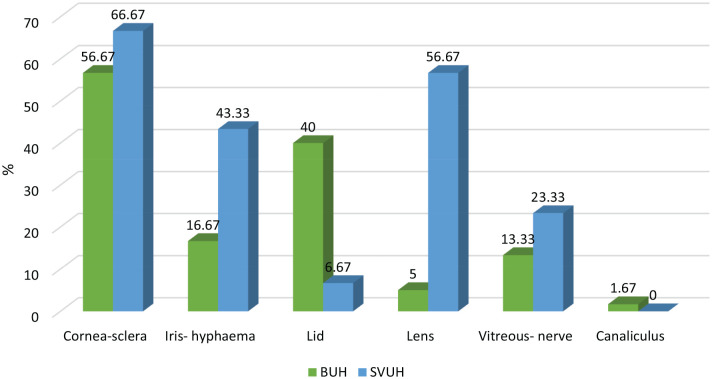
Figure 2 demonstrates the frequency distribution of tissues affected in eye injuries among cases admitted to BUH and SVUH. Cornea-scleral injuries were affected most frequently (61.67%; n = 74) followed by lens (30.83%; n = 37), iris-hyphaema (30.00%; n = 36), lid injuries (23.33%; n = 28), vitreous-nerve injuries (18.33%; n = 22), and canaliculus injuries (0.83%; n = 1). The iris and lens were more frequently affected in SVUH (p = 0.001 and p < 0.001, respectively), while eyelid injuries were more frequent in BUH (p < 0.001).
Figure 2.
Tissues affected in eye injuries in the studied cases.
BUH: Benha University Hospital; SVUH: South Valley University Hospital.
Table 4 shows the medicolegal classification and clinical aspects of eye injuries in the studied cases. Only five cases had bilateral eye injuries. The time interval to seek medical advice ranged from zero (immediate) to 120 h, with an average of 9.93 (±23.57) hours. The average time from admission to intervention was 1.63 (±2.77) hours and ranged from zero to 15 h. A total of 55 cases presented with blindness/ near vision impairment on admission, 29 cases presented with moderate visual impairment, and 29 cases with no or mild visual impairment. There were significant differences in visual impairment between cases admitted to each hospital upon admission (p < 0.001). The mean Ocular Trauma Score (OTS) in the studied cases was 3.20 (±1.65). Cases attended to BUH had higher OTS than those attended to SVUH (p < 0.001).
Table 4.
Medicolegal and clinical aspects of studied pediatric eye injuries.
| Variable | BUH (no.= 60) | SVUH (no.= 60) | Test | p | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Laterality | Unilateral | 57 | 95.00 | 58 | 96.67 | FET | 1.00 |
| Bilateral | 3 | 5.00 | 2 | 3.33 | |||
| Vision impairment at admission a | Near vision impairment | 13 | 21.67 | 26 | 43.33 | FET | <0.001 |
| Blindness | 2 | 3.33 | 14 | 23.33 | |||
| Moderate | 27 | 45.00 | 2 | 3.33 | |||
| No/ mild | 17 | 27.33 | 12 | 20.00 | |||
| Not available | 1 | 1.67 | 6 | 10.00 | |||
| OTS | Mean ± SD Range |
4.04 ± 1.33 1–5 (n = 59) |
2.44 ± 1.56 1–5 (n = 54) |
Z = 5.26 | <0.001 | ||
| Time delay to seek advice (h) | ≤24 | 56 | 93.33 | 50 | 83.33 | X2 = 2.91 | 0.09 |
| >24 | 4 | 6.67 | 10 | 16.67 | |||
| Mean ± SD Range |
5.34 ± 11.58 0.33–72 |
14.52 ± 30.72 0–120 |
Z = 0.55 | 0.58 | |||
| Presentation-intervention interval (h) | ≤6 | 55 | 91.67 | 60 | 100.00 | FET | 0.06 |
| >6 | 5 | 8.33 | 0 | 0.00 | |||
| Mean ± SD Range |
1.55 ± 3.50 0–15 |
1.72 ± 1.78 0–5 |
Z = 0.28 | 0.78 | |||
BUH: Benha University Hospital; SVUH: South Valley University Hospital; OTS: Ocular Trauma Score; X2: Chi-square test; FET: Fisher Exact Test; Z: Mann Whitney test.
p < 0.05 was considered statistically significant.
According to the International Classification of Diseases 11 (2023) for vision impairment; no- visual acuity is better than 6/12, mild- visual acuity worse than 6/12 to 6/18, moderate – visual acuity worse than 6/18 to 6/60, severe – visual acuity worse than 6/60 to 3/60, blindness – visual acuity worse than 3/60, or near vision worse than N6.
Final visual acuity was available for only 99 cases. Of these, 40 cases had improved final visual acuity compared to the initial condition. Forty-seven cases remained the same, while 8 cases worsened during follow-up. Lastly, four cases did not have an initial visual acuity assessment.
Table 5 shows comparisons between OGI and CGI regarding ocular injury description and educational level. Sharp object and blunt object accounted for the highest proportion of OGI and CGI, respectively (58.7% and 47.3%, p < 0.001). The majority of OGI involved the anterior and posterior eye zones, while most CGIs were in the external and anterior eye zones (p < 0.001). Injuries of cornea-sclera, iris-hyphaema, lens, and vitreous-nerve were more frequent in OGI compared to CGI (p < 0.05). There were significant differences in educational level between OGI and CGI with 30.43% of OGIs were in illiterate children, while 64.86% of CGIs were in children who had primary/ read and write education (p < 0.001). Children with OGI had longer time interval from admission to intervention then those with CGI (p = 0.001).
Table 5.
Injury description and educational level in relation to the type of eye injury.
| Variable | CGI (n = 74) | OGI (n.= 46) | Test | p | |||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Laterality | Unilateral | 69 | 93.24 | 46 | 100.00 | FET | 0.15 |
| Bilateral | 5 | 6.76 | 0 | 0.00 | |||
| Cause of eye injury | Blunt object | 35 | 47.30 | 12 | 26.09 | FET | <0.001 |
| Sharp object | 13 | 17.57 | 27 | 58.70 | |||
| Foreign body | 10 | 13.51 | 4 | 8.70 | |||
| Road traffic accident | 4 | 5.41 | 1 | 2.17 | |||
| Animal origin | 2 | 2.70 | 1 | 2.17 | |||
| Plant origin | 1 | 1.35 | 1 | 2.17 | |||
| Fall | 3 | 4.05 | 0 | 0.00 | |||
| Fight | 4 | 5.41 | 0 | 0.00 | |||
| Thermal injury | 2 | 2.70 | 0 | 0.00 | |||
| Zone of eye injury | External | 35 | 47.30 | 0 | 0.00 | FET | <0.001 |
| Anterior | 32 | 43.24 | 29 | 63.04 | |||
| Anterior + posterior | 5 | 6.76 | 14 | 30.43 | |||
| Posterior | 2 | 2.70 | 3 | 6.52 | |||
| Eye tissues affected | Cornea-sclera | 33 | 44.59 | 41 | 89.13 | X2 = 23.80 | <0.001 |
| Iris-hyphaema | 16 | 21.62 | 20 | 43.48 | X2 = 6.45 | 0.01 | |
| Lid | 28 | 37.84 | 0 | 0.00 | X2 = 22.70 | <0.001 | |
| Lens | 8 | 10.81 | 29 | 63.04 | X2 = 36.29 | <0.001 | |
| Vitreous-nerve | 7 | 9.46 | 15 | 32.61 | X2 = 10.15 | 0.001 | |
| Canaliculus | 1 | 1.35 | 0 | 0.00 | FET | 1.00 | |
| Time delay to seek advice (h) | ≤24 | 70 | 94.59 | 39 | 84.78 | FET | 0.10 |
| >24 | 4 | 5.41 | 7 | 15.22 | |||
| Mean ± SD Range |
6.33 ± 15.20 0–72 |
15.70 ± 32.24 0–120 |
Z = 1.33 | 0.18 | |||
| Presentation-intervention interval (h) | ≤6 | 72 | 97.30 | 43 | 93.48 | FET | 0.37 |
| >6 | 2 | 2.70 | 3 | 6.52 | |||
| Mean ± SD Range |
0.89 ± 2.40 0–15 |
2.82 ± 2.92 0–12 |
Z = 3.17 | 0.001 | |||
| Educational level | Under school age | 10 | 13.51 | 3 | 6.52 | FET | <0.001 |
| Illiterate | 0 | 0.00 | 14 | 30.43 | |||
| Primary/read & write | 48 | 64.86 | 23 | 50.00 | |||
| Preparatory | 10 | 13.51 | 6 | 13.04 | |||
| Secondary | 6 | 8.11 | 0 | 0.00 | |||
CGI: Closed Globe Injury; OGI: Open Globe Injury; X2: Chi-square test; FET: Fisher Exact Test; z: Mann-Whitney test.
p < 0.05 was considered statistically significant.
Fifteen cases had permanent infirmity at the end of the follow-up period. The relationship between permanent infirmity and sociodemographic data and characteristics of eye injuries in studied cases are demonstrated in Table 6. Permanent infirmity was more likely in uneducated cases with open globe injury (p < 0.001). Cases with external and anterior eye zone injuries were less likely to have permanent infirmity (p < 0.001). All cases with final permanent infirmity had initial near vision impairment. Most cases without permanent infirmity (95.24%) sought medical care within the first 24 h of eye trauma compared to 66.67% of those with permanent visual infirmity (p = 0.004). Permanent infirmity was more likely in cases with longer interval from admission to intervention than those with short admission to intervention interval (5.53 ± 3.36 vs 1 ± 1.86 h; p < 0.001). Lower OTS was associated with an increased risk of permanent infirmity (1.27 ± 0.59 vs 3.66 ± 1.54; p < 0.001).
Table 6.
Relationship between final visual acuity and sociodemographic data and characteristics of pediatric eye injuries.
| Variable | Final Visual Acuity | Test | p | ||||
|---|---|---|---|---|---|---|---|
| No infirmity (no = 84) | Infirmity a (no = 15) | ||||||
| No. | % | No. | % | ||||
| Gender | Female | 21 | 25.00 | 6 | 40.00 | FET | 0.34 |
| Male | 63 | 75.00 | 9 | 60.00 | |||
| Age (years) | Mean ± SD; (range) | 10.49 ± 2.99;(4–18) | 11.47 ± 2.39; (5–15) | t = 1.12 | 0.23 | ||
| 0–4 | 1 | 1.19 | 0 | 0.00 | FET | 0.06 | |
| 5–9 | 29 | 34.52 | 1 | 6.67 | |||
| 10–14 | 44 | 52.38 | 13 | 86.67 | |||
| 15–18 | 10 | 11.90 | 1 | 6.67 | |||
| Residence | Rural | 40 | 47.62 | 9 | 60.00 | X2 = 0.78 | 0.38 |
| Urban | 44 | 52.38 | 6 | 40.00 | |||
| Occupation | None | 4 | 4.76 | 9 | 60.00 | FET | <0.001 |
| Preschool | 1 | 1.19 | 0 | 0.00 | |||
| Student | 77 | 91.67 | 3 | 20.00 | |||
| Worker | 2 | 2.38 | 3 | 20.00 | |||
| Educational level | Under school age | 5 | 5.95 | 1 | 6.67 | FET | <0.001 |
| Illiterate | 4 | 4.76 | 10 | 66.67 | |||
| Primary/read & write | 55 | 65.48 | 4 | 26.67 | |||
| Preparatory | 14 | 16.67 | 0 | 0.00 | |||
| Secondary | 6 | 7.14 | 0 | 0.00 | |||
| Type of injury | CGI | 61 | 72.62 | 1 | 6.67 | X2 = 23.65 | <0.001 |
| OGI | 23 | 27.38 | 14 | 93.33 | |||
| Zone of eye injury | External | 30 | 35.71 | 0 | 0.00 | FET | <0.001 |
| Anterior | 43 | 52.19 | 7 | 46.67 | |||
| Posterior | 2 | 2.38 | 1 | 6.67 | |||
| Anterior + posterior | 9 | 10.71 | 7 | 46.67 | |||
| Place of injury | Indoor | 26 | 30.95 | 1 | 6.67 | FET | 0.06 |
| Outdoor | 58 | 69.05 | 14 | 93.33 | |||
| Time of injury | Day | 40 | 47.62 | 5 | 33.33 | X2 = 1.05 | 0.31 |
| Night | 44 | 52.38 | 10 | 66.67 | |||
| Manner of injury | Accidental | 69 | 82.14 | 14 | 93.33 | FET | 0.45 |
| Homicidal | 15 | 17.86 | 1 | 6.67 | |||
| Laterality | Unilateral | 81 | 96.43 | 15 | 100.00 | FET | 1.00 |
| Bilateral | 3 | 3.57 | 0 | 0.00 | |||
| Time delay to seek advice (h) | ≤24 | 80 | 95.24 | 10 | 66.67 | FET | 0.004 |
| >24 | 4 | 4.76 | 5 | 33.33 | |||
| Mean ± SD; (range) | 5.72 ± 14.13;(0–72) | 27.53 ± 35.87;(0–96) | Z = 0.64 | 0.52 | |||
| Presentation-intervention interval (h) | ≤6 | 83 | 98.81 | 13 | 86.67 | FET | 0.06 |
| >6 | 1 | 1.19 | 2 | 13.33 | |||
| Mean ± SD; (range) | 1 ± 1.86;(0–12) | 5.53 ± 3.36;(3–15) | Z = 5.63 | <0.001 | |||
| Vision impairment at admission a | No/ mild | 20 | 25.00 | 0 | 0.00 | FET | <0.001 |
| Moderate | 28 | 35.00 | 0 | 0.00 | |||
| Blindness | 16 | 20.00 | 0 | 0.00 | |||
| Near vision impairment | 16 | 20.00 | 15 | 100.00 | |||
| OTS | Mean ± SD; (range) | 3.66 ± 1.54; (1–5) | 1.27 ± 0.59;(1–3) | Z = 5.18 | <0.001 | ||
CGI: Closed Globe Injury; OGI: Open Globe Injury; OTS: Ocular Trauma Score; X2: Chi-square test; FET: Fisher Exact Test; t: Student t-test; z: Mann-Whitney test.
p < 0.05 was considered statistically significant.
According to the International Classification of Diseases 11 (ICD 11) for vision impairment; no- visual acuity is better than 6/12, mild-visual acuity worse than 6/12 to 6/18, moderate – visual acuity worse than 6/18 to 6/60, severe – visual acuity worse than 6/60 to 3/60, blindness – visual acuity worse than 3/60, or near vision worse than N6.
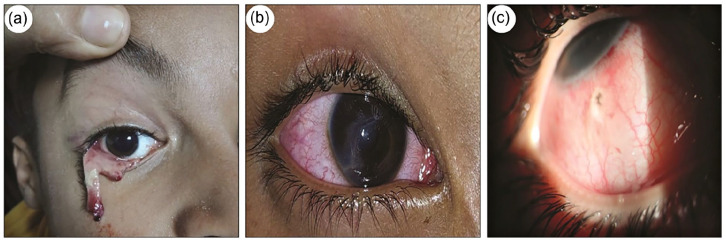
An OTS of less than two could predict 86.73% of cases with final permanent infirmity, with sensitivity, specificity, positive predictive value, and negative predictive value rates of 80.0%, 87.95%, 54.55%, and 96.05%, respectively (Figure 3). Figure 4 shows some examples of eye injuries involved in the study.
Figure 3.
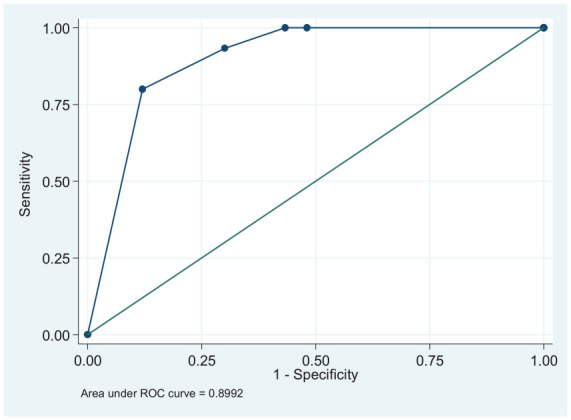
Receiver Operator Characteristic Curve (ROC) for the prediction of final permanent infirmity based on Ocular Trauma Score (OTS).
Figure 4.
(a) Full thickness lower eyelid laceration in a 7-year-old male child, (b) corneal laceration in right eye in a 5-year-old female patient, and (c) 5-year-old male child with penetrating scleral wound by a steel wire.
Discussion
This pioneering study represents the first investigation in Egypt to compare patterns and outcomes of ocular trauma in children across upper and lower regions of the country. The study included 120 pediatric patients with ocular trauma who were presented or were referred to the ophthalmology departments of two university hospitals in Egypt; South Vally University Hospital located in Upper Egypt and Benha University Hospital representing Lower Egypt. The study also examined potential factors affecting outcomes and searched for an association between ocular trauma and permanent infirmity.
Age
Children are vulnerable to injuries due to immature motor skills, curiosity, risk-taking, and poor decision-making. 22 Older children face higher risk due to increased activities like school, sports, and outdoor play. The studied patients’ age range was 3–18 years, averaging 10.03 (±3.30) years, higher than previous Egyptian studies. In Upper Egypt (2009–2010), the mean age was 7.37 (±3.42) years, with most injuries in the 2–7 years group. 23 In Assuit, it was 7.42 (±4.5) years, and over a third of children under five. 24 Another Upper Egypt study reported an average age of 8.23 (±4.55) years, with the highest incidence in the 6–10 years group. 25 In Cairo, injuries ranged from 5 months to 15 years, mostly in children aged five and above. 17 Similar patterns are observed globally, such as in Qatar, where the mean age was 6.63 years, mostly in children aged five and older. 26 Childhood ocular trauma is generally centered around 9 years, with frequent cases in the 6–11 years group27 –29 and the 9–15 years group.30,31
Gender
Males are more prone to injuries due to engaging in risky behaviors and less supervision. 32 In this study, male patients comprised 81.67% and 66, 67% of cases at BUH and SVUH, respectively. Similarly, at Kasr El Aini Hospital, Cairo, males accounted for 64% of pediatric ocular trauma cases, 17 and in Upper Egypt, they comprised 58.34%–70.7% of cases.23 –25 These variations may stem from different numbers of participants and study designs. A male predominance in pediatric ocular trauma was also observed in tertiary hospitals in India,33,34 Croatia, 22 the US, 35 Colombia, 27 Indonesia, 36 Turkey, 28 and Nigeria. 29 This trend may be due to social and environmental factors, with males being more often allowed outdoors and involved in physically demanding jobs, as well as their generally more aggressive nature. 22
Education
Most recruited patients were school students (77.5%): 59.17% in primary, 13.33% in preparatory, and 5.0% in secondary schools; 10.83% were pre-school aged. Additionally, 11.67% were illiterate, and 4.17% were workers from Qena in Upper Egypt. The high illiteracy rate in Upper Egypt is attributed to poverty and a lack of schools, leading to school dropouts and child labor. In Cairo, 63% of children with eye injuries were students, 34.0% were pre-school aged, and 2.7% were working. 17 An Upper Egypt study reported 42.2% of eye injuries in preschool children, 54.7% in students (25.0% primary, 20.3% preparatory, and 9.4% secondary), and 3.1% were illiterate. 24 Likewise, more than half of the cases in the current study were from urban areas. Likewise, 58.91% of ocular injuries in children between 2016 and 2020 were from urban areas. 28 In India, the urban areas percentage of children exposed to ocular trauma was 69.9%. 33 The frequency distribution of rural and urban cases can be affected by the restricted access to health facilities in rural areas. 28
Place
Outdoor injuries were prevalent in our sample. Two-thirds of cases admitted to SVUH happened at night compared to 41.67% at BUH. In Upper Egypt, 54.7% of pediatric ocular trauma occurred on the street, with 46.7% at midday, 39.3% in the morning, and 14% in the evening. 23 In Cairo, 54.67% of children’s eye injuries occurred outside the home, mostly between 12:00 and 6:00 PM. 17 In Upper Egypt, 53.1% of penetrating eye injuries in children were home accidents, 39.1% occurred on the street, and 7.8% were workplace accidents, likely due to younger children staying at home. 24 Globally, 53.9% of open globe injuries in children under 16 happened outdoors. 37 In addition, the highest proportion (44.3%) of ocular trauma in children occurred on the street, 42.5% at home, 12.3% at school, and 5.7% on sports fields. 26 Bućan et al. reported that 70% of childhood ocular trauma occurred outdoors. 22 Whereas, other studies showed 32.79% of ocular trauma occurred on the street. 27 In India, the home was the most frequent location for ocular trauma. 33 The place of injury varies with age; younger children are more likely to be injured at home, while older children are injured at school, playing, or in the street.22,37 Increased outdoor injuries may be due to less supervision. Ensuring safety at home, school, and sports areas by keeping hazardous agents out of children’s reach and increasing supervision is crucial. 33
Trauma
This study showed a high frequency of blunt trauma (39.17%), sharp trauma (33.33%), and foreign body-induced trauma (11.67%), with fewer cases from road traffic accidents (4.17%) and fights (3.33%). Similar results in Egypt reported blunt trauma, sharp trauma, and projectile injuries as the most frequent causes of ocular trauma in children (44%, 39%, and 15%, respectively). 17 In Upper Egypt, 43.06% of ocular injuries in children were caused by blunt trauma, 40.28% by penetrating trauma, and 16.67% by foreign bodies. 25 Another study in Upper Egypt found wood, stones, and toy guns to be the most frequent agents of pediatric eye injuries (20%, 17.3%, and 15.3%, respectively). 23 Blows were the leading cause of eye injuries (63.93%) in children under 15, followed by foreign bodies (19.67%). 27 In India, penetrating injuries accounted for two-thirds of open globe injuries 15 and sports-related injuries were common during summer vacations. 34 The causes of eye injuries varied with age: toys in preschoolers, pencils in the 7–12 age group, and sports activities in the 13–18 age group. 28 Injury mechanisms depend on the availability of objects within children’s reach. 27 Family and community education about safety precautions to prevent injuries by household hazards and during recreational activities is recommended. 28
Type of injury
In studied patients, most eye injuries were CGI (61.67%). There was a higher prevalence of CGI at BUH (83.33%) compared to SVUH (40.0%), likely due to more penetrating trauma at SVUH leading to more OGI. More than half of the cases had anterior zone eye injuries followed by external zone eye injuries (29.17%). CGI represented 52.78% of pediatric eye injuries in Upper Egypt. 25 Previous studies in Egypt reported higher OGI rates in children.17,23 In Upper Egypt, OGI accounted for two-thirds of injuries, often in children under 7 years. 23 In Cairo, 83.75% of ocular injuries were OGI, attributed to increased gunshot injuries post-2011 revolution, with 62.5% affecting the anterior segment. 17 In Saudi Arabia, 72.6% of pediatric eye trauma between 1998 and 2019 was OGI. 38 Additionally, 63.9% of pediatric eye injuries were OGI, as severely injured eyes were more likely to seek hospital care. 34 Consistent with our results, 62.19% of eye injuries in Indian children were CGI 33 as well as 59.4% in Qatar, 26 70.2% in Indonesia, 36 and 73.4% in Nigeria. 29 CGI, such as contusions, were more common in older children due to their ability to protect themselves. 39
Affected tissue
Cornea-scleral injuries were most frequent among collected cases at both BUH (56.67%) and SVUH (66.67%). This was followed by lid injuries at BUH (40.00%), and lens injuries and iris-hyphaema at SVUH (56.67% and 43.33%, respectively). The differences may be due to the higher prevalence of CGI at BUH and OGI at SVUH. Injured tissues depend on the trauma cause, leading to disfigurement, impaired vision or blindness. Previous studies in Upper Egypt found the cornea most frequently injured in pediatric eye trauma.23 –25 In 2011, more than half of pediatric eye injuries at Cairo University hospital were OGI with lacerated globes, followed by penetrating injuries (38.75%), and ruptured globes (30.0%). 17 Corneal perforations were also the most frequent pediatric eye injuries reported in India (47.5%). 34
In the present study, accidental injuries accounted for 82.14% and 93.33% of cases admitted to BUH and SVUH, respectively. Bilateral injuries were found in five cases only. Similarly, 97.24% of eye injuries in children were accidental and 2.78% were homicidal. 25 Bilateral eye injuries was reported in 22.9% of children. 34
Timing
Similarly to Soliman et al. 24 we found that 88.33 of cases were presented to hospital within 24 h of eye trauma, with an average admission to intervention time of 1.63 (±2.77) hours, ranging from zero to 15 h. In contrast, 43% of pediatric eye trauma cases in Cairo were presented after 24 h, likely because Kasr El Aini Hospital receives 50% of its cases from distant areas across Greater Cairo. 17 Globally, 86.5% and 69% of eye trauma cases were presented to pediatric emergency departments within 24 h in Spain and Iran, respectively.40,41 In China, 54% of children presented within 24 h, while 24.4% presented more than 7 days after eye trauma between 2008 and 2017 in China. 42 About 75% of children with eye trauma in another study were presented more than 1 day after the trauma. 43 Open globe injuries, such as penetrating and rupture injuries were associated with more rapid care-seeking compared to CGI, such as contusions. 42
Initial visual impairment
BCVA was used to monitor visual impairment, but it was not available for seven young, uncooperative cases. Upon admission, 55 cases (45.83%) had blindness or near vision impairment, mainly at SVUH (n = 40) and BUH (n = 15), likely due to more frequent OGI at SVUH, which is often linked to significant visual impairment. 8 In this study, 42 out of 55 cases with visual acuity less than 3/60 had OGI. Similarly, Abdellah et al. reported 44.44% of children with poor visual acuity (less than 1/60) following eye trauma, associated with OGI. 25 Additionally, 73.9% of children with OGI from mechanical injuries had initial visual acuity less than 6/60, 42 and 68% of cases with OGI had visual acuity less than 6/60 after eye trauma. 43 Visual acuity better than 6/60 was more frequent in CGI than in OGI cases (55.6% vs 37.3%). 26 However, there was no significant difference in the proportion of cases with poor vision (<20/400) at presentation between cases with OGI and CGI (40.1% vs 40%). 38 In Spain, acute vision loss was reported in 70.7% of children with eye trauma, associated with age ≥ 10 years, pre-existing refractive errors, OGI, and blunt object injuries. 41
Final visual impairment
After 6 months, BCVA was available for 99 cases, with 15 having permanent visual infirmity (BCVA worse than 3/60 or near vision worse than N6). All cases with permanent infirmity initially had poor visual acuity. Most of these cases (13/15) were managed at SVUH, with only two at BUH. The outcome was worse in OGI cases and those with delayed intervention, 42 making permanent infirmity more likely in Upper Egypt than in Benha. Al-Mahdi et al. reported 11.6% and 4.7% of children with OGI had severe visual impairment and blindness, respectively. 26 More than half of children with ocular injuries had a final visual acuity less than 6/60.42,43
OTS
This study calculated OTS for (94.17%) 113/120 cases, with missing results due to uncooperative children or young age. BUH patients had higher OTS compared to SVUH patients (4.04 ± 1.33 vs 2.44 ± 1.56; p< 0.001), likely due to the higher prevalence of CGI at BUH and OGI at SVUH, as OGI is linked to poor visual outcomes. 34 OTS is a prognostic tool for eye injury management. Children with final permanent infirmity had significantly lower OTS. ROC analysis showed that an OTS ≤2 could predict 86.73% of permanent infirmity with (80.0%) sensitivity and (87.95%) specificity. Good OTS and initial visual acuity were correlated with favorable outcomes,36,42,44 as confirmed by this study. However, some patients had better final visual acuity than predicted by OTS,45,46 possibly due to initial assessment challenges. 45 Perez et al. found that OTS underestimated visual outcomes of OGI following secondary Pars Plana Vitrectomy (PPV).42,47
Limitation of the study
The primary drawbacks in this study were associated with the limited number of study participants, a deliberate choice made to ensure maximum participant retention over the study duration. Nonetheless, 21 cases (17.5%) did not complete the 6-month follow-up. Some parents opted for alternative medical advice, while others experienced improvement and chose not to continue with the follow-up. This limitation hinders the generalization of the results, which principally reflect the studied cases.
Recommendations
Our research outcomes hold the potential to contribute to the development of preventive programs aimed at reducing the incidence of eye trauma and its consequences. Emphasizing the right to education for all children, particularly underscoring this need in Upper Egypt, is crucial. Article 64 of the Egyptian Child Law No. 12 appropriately restricts child labor for those aged 15 years and above, thereby minimizing their exposure to potential hazards. Given the serious outcomes associated with eye injuries, there is a critical need to advocate for enhanced supervision at home, in schools, and during recreational activities such as sports and festivals. Taking preventive measures, such as keeping sharp and hazardous materials out of the reach of children, is paramount. Moreover, ensuring the availability of first aid facilities and raising public awareness about emergency hotline numbers can significantly contribute to early management and improved outcomes for traumatized children. The utilization of the OTS as a well-established prognostic tool holds significance, guiding both medical and medicolegal professionals in their approach to managing eye injuries and predicting their outcomes.
Conclusion
In summary, accidental eye injuries continue to be a significant contributor to visual impairment among children in both Upper and Lower Egypt. This study underscores that such injuries predominantly affect male children at school age, particularly in the outdoor settings. The primary causative agents were blunt objects and sharps, with a higher incidence of Closed Globe Injuries (CGI) in Benha and more frequent Open Globe Injuries (OGI) in Upper Egypt. The study highlights the correlation between initial visual acuity and the Ocular Trauma Score (OTS) with the final visual acuity, indicating that OTS serves as a valuable prognostic tool for cases resulting in permanent visual infirmity.
Acknowledgments
The authors are thankful to all children and their parents/guardians who agreed to participate in this study.
Footnotes
List of abbreviations: BCVA: Best Corrected Visual Acuity
BUH: Benha University Hospital
CGIs: Closed Globe Injuries
OGIs: Open Globe Injuries
OTS: Ocular Trauma Score
SVUH: South Vally University Hospital
Author’s contributions: All authors contributed to the study conception, design, and material preparation. Data collection and data entry were performed by [AA], [GHY], [NHFH]. Statistical analysis and interpretation were carried out by [HB], [AAF], [FAE], and [OMA]. The first draft of the manuscript was written by [HB], [AAF], [NHFH], and [NSI]. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript and this submission.
Availability of data and materials: The data that support the findings of this study are available from the corresponding author upon request.
Code availability: Not applicable.
Consent for publication: All involved legal guardians gave their informed written consent prior to study inclusion.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval and consent to participate: The study was approved by the Scientific Research Ethics Committee of the Faculty of Medicine, South Valley University “SvuMEDOPH026/4/22/3/363,” and the study was conducted in accordance with the ethical standards laid down by the Declaration of Helsinki. A written informed consent was obtained from the legal guardian for each participating subject and confidentiality of the data was considered.
ORCID iD: Hanaa E Bayomy  https://orcid.org/0000-0001-7273-7931
https://orcid.org/0000-0001-7273-7931
References
- 1. Heath Jeffery RC, Dobes J, Chen FK. Eye injuries: Understanding ocular trauma. Aust J Gen Pract 2022; 51(7): 476–482. [DOI] [PubMed] [Google Scholar]
- 2. Mohseni M, Blair K, Gurnani B, et al. Blunt eye trauma, https://www.ncbi.nlm.nih.gov/books/NBK470379/ (2023, accessed 9 September 2023). [PubMed]
- 3. Li C, Fu Y, Liu S, et al. The global incidence and disability of eye injury: an analysis from the Global Burden of Disease Study 2019. eClinicalMedicine 2023; 62: 102134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aghadoost D. Ocular trauma: an overview. Arch Trauma Res 2014; 3(2): e21639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rasool R, Shahid E, Ehsan R, et al. Visual outcome of ocular trauma and its medicolegal interpretation in a tertiary care hospital, Karachi. Ann ASH KMDC 2020; 25(3). [Google Scholar]
- 6. Tripathy K, Chawla R, Venkatesh P, et al. Clinical profile of medicolegal cases presenting to the eye casualty in a tertiary care center in India. Indian J Ophthalmol 2016; 64(6): 422–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kuhn FM, Witherspoon CDH, Jeffers JBT. Standardized classification of ocular trauma. Ophthalmology 1996; 103(2):240–243. [DOI] [PubMed] [Google Scholar]
- 8. Zhou Y, DiSclafani M, Jeang L, et al. Open globe injuries: review of evaluation, management, and surgical pearls. Clin Ophthalmol 2022; 16: 2545–2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Salama N, Badr El, Dine F. Ocular trauma characteristics in cases admitted to Alexandria University Main Hospital: a medicolegal study. Ain Shams J Forensic Med Clin Toxicol 2014; 23(2): 21–29. [Google Scholar]
- 10. Scott R. The ocular trauma score. Community Eye Health 2015; 28(91): 44–45. [PMC free article] [PubMed] [Google Scholar]
- 11. Pahor D, Gracner T. Comparison of the ocular trauma score and pediatric ocular trauma score as two prognostic models in pediatric open globe injuries. Klin Monatsbl Augenheilkd 2021; 238(1): 67–72. [DOI] [PubMed] [Google Scholar]
- 12. Chaudhary A, Singh R, Singh SP. Prognostic value of ocular trauma score and pediatric penetrating ocular trauma score in predicting the visual prognosis following ocular injury. Rom J Ophthalmol 2022; 66(2): 146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hoskin AK, Philip SS, Yardley AM, et al. Eye injury prevention for the pediatric population. Asia Pac J Ophthalmol 2016; 5(3): 202–211. [DOI] [PubMed] [Google Scholar]
- 14. Zungu T, Mdala S, Manda C, et al. Characteristics and visual outcome of ocular trauma patients at Queen Elizabeth Central Hospital in Malawi. PLoS One 2021; 16(3): e0246155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sharma B, Singh S, Kumar K, et al. Epidemiology, clinical profile and factors, predicting final visual outcome of pediatric ocular trauma in a tertiary eye care center of Central India. Indian J Ophthalmol 2017; 65(11): 1192–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jac-Okereke CC, Jac-Okereke CA, Ezegwui IR, et al. Current pattern of ocular trauma as seen in tertiary institutions in south-eastern Nigeria. BMC Ophthalmol 2021; 21(1): 420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Al Wadeai EA, Osman AA, Macky TA, et al. Epidemiological features of pediatric ocular trauma in Egypt. J Ophthalmol 2016; 2016: 7874084. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Knyazer B, Levy J, Rosen S, et al. Prognostic factors in posterior open globe injuries (zone-III injuries). Clin Exp Ophthalmol 2008; 36(9): 836–841. [DOI] [PubMed] [Google Scholar]
- 19. Pieramici DJ, Sternberg P, Aaberg TM, et al. A system for classifying mechanical injuries of the eye (globe). The ocular trauma classification group. Am J Ophthalmol 1997; 123(6): 820–831. [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization. ICD-11: International classification of diseases (11th revision) for mortality and morbidity statistics (Version:01/2023). https://icd.who.int/ (2022).
- 21. Kv V, Vijayalakshmi P. Understanding definitions of visual impairment and functional vision. Community Eye Health 2020; 33(110): S16–S17. [PMC free article] [PubMed] [Google Scholar]
- 22. Bućan K, Matas A, Lovrić JM, et al. Epidemiology of ocular trauma in children requiring hospital admission: a 16-year retrospective cohort study. J Glob Health 2017; 7(1): 010415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. El-Sebaity DM, Soliman W, Soliman AM, et al. Pediatric eye injuries in upper Egypt. Clin Ophthalmol 2011; 5: 1417–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Soliman K, Abdalla Mohamed A, Anwar Sayed M, et al. Pediatric Penetrating Eye Injuries at Assiut University Hospital, Assiut, Egypt. Asian J Res Rep Ophthalmol 2020; 2(1): 14–24. [Google Scholar]
- 25. Abdellah N, Shaltout E, Ebrahem N, et al. Pattern of childhood ophthalmic injuries in Upper Egypt. Ain Shams J Forensic Med Clin Toxicol 2022; 39(2): 30–38. [Google Scholar]
- 26. Al-Mahdi HS, Bener A, Hashim SP. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emerg Nurs 2011; 19(4): 186–191. [DOI] [PubMed] [Google Scholar]
- 27. D'Antone V, Flórez DCP, García CJL, et al. Epidemiological findings of childhood ocular trauma in a public hospital in Colombia. BMC Ophthalmol 2021; 21(1): 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kaçer EÖ, Kaçer İ. Ocular trauma in the pediatric age group: a systematic review. Egypt Pediatr Assoc Gazette 2022; 70(1): 28. [Google Scholar]
- 29. Ugalahi MO, Adebusoye SO, Olusanya BA, et al. Ocular injuries in a paediatric population at a child eye health tertiary facility, Ibadan, Nigeria. Injury 2023; 54(3): 917–923. [DOI] [PubMed] [Google Scholar]
- 30. Maurya R, kumar A, Singh V, et al. Pattern of pediatric ocular trauma in an Eastern Uttar Pradesh. Indian J Clin Exp Ophthalmol 2017; 3(3): 252–258. [Google Scholar]
- 31. Kadappu S, Silveira S, Martin F. Aetiology and outcome of open and closed globe eye injuries in children. Clin Experiment Ophthalmol 2013; 41(5): 427–434. [DOI] [PubMed] [Google Scholar]
- 32. Udry JR. Why are males injured more than females? Inj Prev 1998; 4(2): 94–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chakraborti C, Giri D, Choudhury K, et al. Paediatric ocular trauma in a tertiary eye care center in Eastern India. Indian J Public Health 2014; 58(4): 278–280. [DOI] [PubMed] [Google Scholar]
- 34. Madan AH, Joshi RS, Wadekar PD. Clin Ophthalmol 2020; 14: 1003–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schneider K, Nguyen-Tran H, Segura BJ, et al. Ocular injury presenting to a level-III pediatric trauma center. Pediatr Emerg Care 2020; 36(11): e606–e609. [DOI] [PubMed] [Google Scholar]
- 36. Irawati Y, Ardiani LS, Gondhowiardjo TD, et al. Predictive value and applicability of ocular trauma scores and pediatric ocular trauma scores in pediatric globe injuries. Int J Ophthalmol 2022; 15(8): 1352–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ilhan HD, Bilgin AB, Cetinkaya A, et al. Epidemiological and clinical features of paediatric open globe injuries in southwestern Turkey. Int J Ophthalmol 2013; 6(6): 855–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. AlGhadeer H, Khandekar R. Clinical profile, etiology, and management outcomes of pediatric ocular trauma in Saudi Arabia. Pediatr Emerg Care 2022; 38(10): e1626–e1630. [DOI] [PubMed] [Google Scholar]
- 39. Haavisto A, Sahraravand A, Holopainen JM, et al. Paediatric eye injuries in Finland – Helsinki eye trauma study. Acta Ophthalmol 2017; 95(4): 392–399. [DOI] [PubMed] [Google Scholar]
- 40. Aghadoost D, Fazel MR, Aghadoost HR. Pattern of pediatric ocular trauma in kashan. Arch Trauma Res 2012; 1(1): 35–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. García Mancebo J, Ferrero García-Loygorri C, Romero AI, et al. [Ocular trauma in the pediatric emergency departments, characteristics and risk factors of immediate sequelae]. An Pediatr 2021; 94(3): 161–172. [DOI] [PubMed] [Google Scholar]
- 42. Li C, Lin Y, Xiao H, et al. Epidemiology of pediatric eye injuries requiring hospitalization in rural areas of Wenzhou and Changsha, China: a 10-year retrospective study. BMC Ophthalmol 2020; 20(1): 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Minderhoud J, van Nispen RM, Heijthuijsen AA, et al. Epidemiology and aetiology of childhood ocular trauma in the Republic of Suriname. Acta Ophthalmol 2016; 94(5): 479–484. [DOI] [PubMed] [Google Scholar]
- 44. Wang W, Zhou Y, Zeng J, et al. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in south-central China. Acta Ophthalmol 2017; 95(6): e503–e510. [DOI] [PubMed] [Google Scholar]
- 45. Oiticica-Barbosa MM, Kasahara N. Eye trauma in children and adolescents: Perspectives from a developing country and validation of the ocular trauma score. J Trop Pediatr 2015; 61(4): 238–243. [DOI] [PubMed] [Google Scholar]
- 46. Morgan AM, Kasahara N. Comparative evaluation of the prognostic value between the ocular trauma score and the pediatric penetrating ocular trauma score. J Craniofac Surg 2018; 29(7): 1776–1779. [DOI] [PubMed] [Google Scholar]
- 47. Perez EA, Ramirez DA, Peterson JD, et al. The ocular trauma score underestimates visual recovery for the most severe open-globe injuries. Ophthalmol Retina 2023; 7(7): 612–619. [DOI] [PubMed] [Google Scholar]