Abstract
Objectives
To evaluate the longitudinal impact of introducing a national, direct access physiotherapy model of care on the rates of primary and secondary care consultations for musculoskeletal (MSK) conditions.
Design
Interrupted time series analysis using segmented linear regression.
Setting
Norway primary care
Participants
A cohort of 82 072 participants was derived from 3 population-based health surveys conducted across separate geographical regions in Norway. All participants surveyed were eligible for inclusion as a national representative sample of the Norwegian population. Registered MSK consultations were linked to the Norwegian Control and Payment of Health Reimbursement database and the Norwegian Patient Register using the International Classification of Primary Care diagnostic medical codes L-chapter for MSK conditions and spine related International Classification of Diseases, 10th Revision, codes.
Intervention
Direct access to physiotherapy model of care introduced nationally in Norway in 2018. This model allowed Norwegians to consult directly with qualified physiotherapists for MSK conditions (eg, back pain, knee osteoarthritis) without the need for a medical referral in order to claim a social security reimbursement.
Main outcomes measured
Rates of primary care consultations per 10 000 population (general practitioner (GP) and physiotherapist consultations) and secondary care (specialist consultations and surgical procedures) measured from 2014 to 2021.
Results
The introduction of the direct access physiotherapy model was associated with an immediate stepped reduction of 391 general practice consultations per 10 000 population, (95% CI: −564 to −216), without an associated change in physiotherapy consultations. Subgroup analyses suggested there was an associated reduction in physiotherapy consultations for those in the lowest education group of 150 consultations per quarter (95% CI:−203 to −97), 70 consultations per quarter in the intermediate education group (95% CI:−115 to −27) and a stepped reduction of 2 spinal surgical procedures per 10 000 population, for those aged between 40 and 60 years (95% CI: −3 to −1) following the introduction of the direct access physiotherapy model.
Conclusion
The national introduction of a direct access to physiotherapy model of care was associated with a reduction in the workload of GPs for the management of MSK conditions. The use of physiotherapists in direct contact roles is a potential strategic model to reduce the burden on the GP workforce in primary care worldwide.
Keywords: Primary Health Care, Health Services, Health Policy
WHAT IS ALREADY KNOWN ON THE TOPIC
Direct access physiotherapy offers a safe alternative model to manage musculoskeletal (MSK) conditions in primary care, with evidence reporting it can reduce healthcare utilisation (eg, medication prescription and imaging referral) but the impact at a healthcare system level is unknown.
WHAT THIS STUDY ADDS
This study is the first to examine the longitudinal impact of a direct access physiotherapy model of care on general practitioners (GP) MSK workload at a national level.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Results from this study provide evidence that a direct access physiotherapy model of care can reduce strain on primary care systems by reducing GP workload.
Introduction
Musculoskeletal (MSK) conditions are a leading cause of disability burden worldwide.1 Not only is this burden reflected in reduced participation in the workforce and community2 but also in the increasing costs and strain placed on healthcare systems worldwide.3 4
In the US alone, the estimated cost attributed to treating MSK conditions (eg, low back pain, knee osteoarthritis) is over US$180 billion and represents the greatest healthcare spending.5 The clinical management of MSK conditions largely occurs in primary healthcare systems and is typically initiated by general practitioners (GPs) or physicians, who guide ongoing management and act as gatekeepers for access to other healthcare services. While the recruitment and retention of GPs is in decline, the prevalence of MSK and other conditions being managed in primary care is increasing,6 creating a shortfall of GPs in the workforce to meet current care demands.7 8 With MSK conditions representing approximately 20% of GP’s workload,9 10 models of care capable of redirecting management of these conditions at the point of entry are urgently needed to reduce strain on primary healthcare systems.
Direct access to physiotherapy is a model of care that allows patients to refer themselves for physiotherapy management without the need to see a GP first. With a large established workforce in most developed healthcare systems, and expertise aligned with guideline recommendations, physiotherapy offers an alternative to GP-led care for the management of MSK conditions.11 While direct access to physiotherapy is reported to be safe,12 recent systematic reviews suggest that it does not result in superior patient reported outcomes compared with GP-led care.11 13 Instead, the benefits of this model of care largely result from reduced delivery of ineffective or harmful interventions14 (eg, opioid prescription), reduced sick leave or work absence15 and decreased healthcare utilisation13 (eg, imaging and specialist referrals).
Comparison of the impact of direct access physiotherapy across various healthcare systems must be made cautiously due to differences in the populations and settings investigated, as well as the study designs employed. Yet, pooled mean differences from a range of healthcare systems and settings indicate direct access physiotherapy consistently results in a reduction in average imaging rates by 28%, and medication prescription rates by 42% compared with the traditional medical models of care.11 Additionally, meta-analysis from five studies conducted in the USA estimate a reduced total healthcare cost of US$1828 (95% CI 673 to 3079) per patient in favour of direct access physiotherapy compared with GP-led care.16 Favourable findings have been reported in economic evaluations conducted on direct access models of care in the UK,12 and a cost-effectiveness evaluation in Sweden showing physiotherapy-led care was likely to be cost-effective at a societal level (when incorporating indirect costs such as loss of productivity).17
Despite the existence of this model of care in several healthcare systems worldwide, the measured impact of direct access to physiotherapy on other healthcare outcomes such as GP workload and secondary care referral (eg, specialist consultation or surgical referral) is inconsistent and primarily derived from case–control15 and service evaluation studies over a limited time period,18 non-experimental observational cohorts19 and pilot randomised control trial across a small number of practices.20 The long-term impact of the introduction of the direct access physiotherapy model of care on GP and physiotherapy workload, at a healthcare system level, is still unknown.
Norway, a country with a population of approximately 5.4 million, has an MSK prevalence and burden reflective of global trends.21 MSK conditions are a leading causes of disability,21 with an estimated annual prevalence of 26% (among all age groups) in Norwegian primary care.22 Norway, presents a unique case study to evaluate the long-term impact of the introduction of direct access physiotherapy in the healthcare system. This is because while Norway has offered a limited version of direct access physiotherapy since 2006 (restricted to specialised manual therapists), it was not until January 2018 that direct access to a physiotherapist, without the need of a referral in order to claim a social security refund, was introduced. Using an interrupted time series design, the primary aim of this study was to investigate the longitudinal impact of the introduction of direct access physiotherapy on the rates of GP and physiotherapist consultations in primary care for MSK conditions, as well as the rates of specialist consultations and surgical procedures in those with spinal (back or neck) conditions. The secondary aims were to explore whether there was a change in rates of consultation across age, education level and the most common MSK conditions (back, neck, shoulder and knee). We hypothesised that the national introduction of a direct access physiotherapy would reduce GP consultations without an immediate impact on physiotherapy rates in primary care. For secondary outcomes, we hypothesised that direct access physiotherapy would have an immediate impact on reducing specialist spinal consultations and a lagged effect on reducing surgical spinal procedures.
Method
Design, participants and setting
An interrupted time series quasiexperimental design was used to retrospectively evaluate the longitudinal effectiveness of the introduction of direct access to physiotherapy in Norway in 2018, on the rate of healthcare consultations for participants with MSK conditions. Where randomisation or parallel controlled designs are not possible, this model provides an effective approach for evaluating interventions at a population level.23 This study is reported in accordance with methodological and reporting recommendations for studies conducted using observational routinely-collected health data24 and interrupted time series studies.25
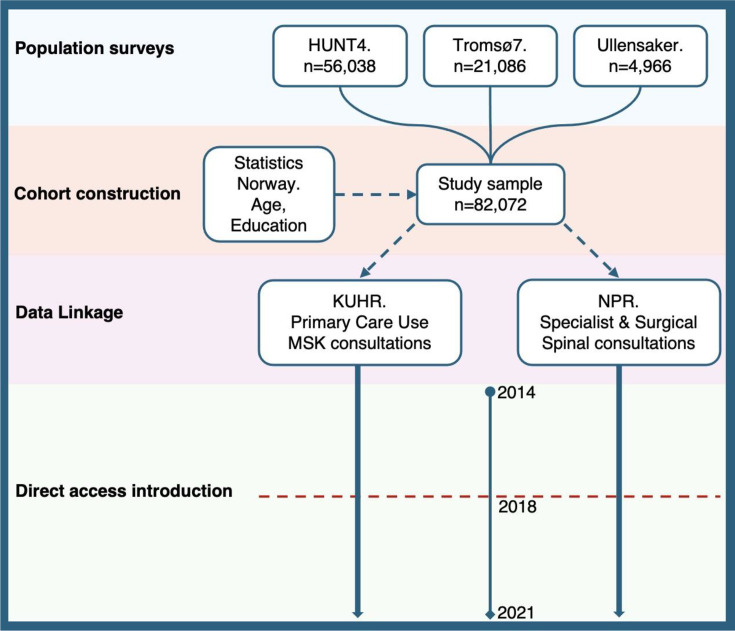
To generate an unbiased cohort of participants, that is, participants with and without exposure to primary care attendance for an MSK complaint, we used three large population-based health surveys that are independently and routinely conducted to collect a range of data for public health research in Norway. The three surveys were chosen to ensure a cohort of participants representative of a broad age group and to reflect three distinct geographical regions in Norway, which could capture regional variation in healthcare utilisation. The HUNT4 Survey (central Norway) was conducted in 2017–2019 and included participation population from the age of 20 years. The seventh survey of the Tromsø Study (northern Norway) was conducted between 2015 and 2016 and included adults from the age of 40 years. The fourth survey of the Musculoskeletal pain in Ullensaker Study (MUST) (municipality in southern Norway) was conducted in 2010–2011 and included adults from the age of 18 years. All participants that completed the surveys were included in our cohort to provide a nationally representative sample of the Norwegian population. No further exclusion criteria were applied. Only the unique patient identifiers were extracted from the survey data to create the baseline cohort, data extraction on healthcare outcomes were collected via data linkage as outlined below. We obtained data on age and education level at the beginning of our observation period (1 January 2014) from Statistics Norway. See figure 1 for study flow diagram.
Figure 1. Study flow diagram. HUNT4, The HUNT4 Survey; KUHR, Norwegian Control and Payment of Health Reimbursement database; MSK, musculoskeletal; NPR, Norwegian Patient Register.
All registered MSK consultations with physiotherapists and GPs in primary care were determined for the study cohort. This was calculated with unique participant identifiers linked with The Norwegian Control and Payment of Health Reimbursement database (KUHR) and the Norwegian Patient Register (NPR) using the International Classification of Primary Care (ICPC-2) diagnostic medical codes26 L-chapter for MSK conditions and spine related International Classification of Diseases 10th Revision, codes (ICD-10). GP consultations included face to face and indirect contacts such as telephone conversations and communication through the public health communication portal (HelseNorge.no). The KUHR registry contained data on physiotherapists with municipality operating agreements only, representing government funded healthcare that would be directly impacted by direct access physiotherapy intervention. For specialist consultations and surgical procedures, only cohort participants with a spinal-related diagnostic code were available and identified using ICD-10 codes27 from the NPR registry for specialist consultations and a combination of ICD-10 and the Nordic Medico-Statistical Committee (NOMESCO) Classification of Surgical Procedures codes for surgical procedures.28 For details on included ICD-10 codes, see online supplemental table 1. Data quality checks were conducted during data cleaning and linkage, including assessing potential duplicate entries and cross-referencing participant identifiers across the population-based health surveys to ensure each participant was unique to a single survey. No observations were missing for linkage data, as we used administrative registry data routinely collected when participants were in contact with health services.29
Intervention
Direct access to physiotherapy was introduced in Norway on 1 January 2018. This allowed Norwegians to consult directly with qualified physiotherapists for certain conditions, without the need to see their GP first for a referral in order to claim a social security reimbursement. Prior to this, there was limited access to compensable physiotherapy available through manual therapists.
Primary outcomes
The primary outcomes of this study were (1) the rate per 10 000 participants of GP and physiotherapy consultations for MSK conditions in primary care and (2) the rate per 10 000 participants of specialist consultations (eg, consultations with rheumatologists, pain specialists, rehabilitation physicians) and surgical procedures for back and neck conditions. Data were analysed for a preintervention period of 4 years 2014–2017 (inclusive) and postintervention period of 4 years 2018–2021 (inclusive).
Secondary outcomes
Rates of consultations were analysed across prespecified subgroups, age, education level and MSK diagnosis. Subgroups were selected from the existing literature indicating that patients who use direct access physiotherapy are often slightly younger, and more educated than those who use GP care.13 30 Previous qualitative research has reported older patients may be reluctant to directly access physiotherapy without seeing their GP first, due to self-perceived complexity of their condition and presence of multimorbidties.31 Ageing has also been associated with increasing primary physician utilisation in Norway, with substantial increases in costs after age 40 years and again after age 60 years.32 Additionally, higher education has been consistently associated with higher specialist healthcare utilisation,33 and this relationship has been reflected in higher uptakes of self-referral to new direct access physiotherapy pathways.19 To the authors’ knowledge, no studies have investigated the influence of pain location/MSK diagnosis on the uptake of direct access physiotherapy. However, it is plausible that patients’ choice of provider may be related to the perceived ability of physiotherapists or GPs to manage particular pain presentations. Age was categorised into three groups (18–39 years, 40–60 years and >60 years). Education was categorised into four levels: lower education (comprising no education/preschool education, primary and lower secondary education), intermediate education (comprising upper secondary and postsecondary non-tertial education), undergraduate (comprising first stage of tertiary education at an undergraduate level) and postgraduate education (comprising secondary stage tertiary education). MSK conditions were categorised into shoulder (ICPC-2 L08 and L92 codes), knee (ICPC-2 L15, L78 and L90), neck (ICPC-2 L01 and L83 codes) and back (ICPC-2 L02, L03, L84, L85 and L86) pain.
Data collection and primary analyses
All registry recorded GP and physiotherapy consultations for MSK conditions and back or neck specialist or surgical care were collected from the beginning of 2014 until the end of 2021. Consultations were totalled by quarter, converted to a rate per 10 000 participants and age standardised to the year of inclusion (2014), to account for the influence of the increasing age of participants each year. Visual exploration of data of participants from each survey confirmed no significant longitudinal variation in primary outcomes between survey groups, so data was combined for all participants. Graphical representations of the interrupted time series were constructed in accordance with guideline recommendations.34
Statistical analysis
Exploratory analysis of all outcomes was conducted to inspect visual trends, stationarity and seasonality. Where non-stationarity was suspected, an augmented Dickey-Fuller test was conducted to determine if transformation of data was needed.35 Seasonality was accounted for using ‘dummy’ variable for the summer months, where consultation rates were consistently lower.
To estimate the effect of the introduction of direct access physiotherapy on rates of consultations for primary outcomes, a segmented regression using a Poisson or negative binomial model was used. The negative binomial model was chosen if the initial analysis indicated overdispersion in the data. Specification of the estimated impact of direct access on the immediate (step change) or change in trend (slope change) in rates of consultations was determined using knowledge from existing evidence19 and visual trends in exploratory data analysis. For GP and specialist consultations, an immediate and trend change in the number of consultations following the intervention was modelled. For physiotherapy consultations, a possible trend rather than stepped change was modelled, and an estimated lag effect of two quarters (6 months) was anticipated for surgical procedures. For all outcomes, sensitivity analyses using different assumptions were conducted to assess the robustness of results (see below). Newey-West standard errors were used to accommodate for residual autocorrelation and heteroskedasticity. Autocorrelation and partial autocorrelation correlograms, along with residual plots, were inspected to evaluate the validity of statistical models. These findings were combined with a comparison of Akaike Information Criteria and Bayesian Information Criterion between models, and visual inspection of the model fit to the data, to find a balance between parsimony and structure of modelled data for final model selection.
Subgroup and sensitivity analyses
Separate segmented regression models were estimated for age, education and MSK subgroups for each primary outcome. Several sensitivity analyses were conducted using altered assumptions of step and/or slope change and methods to deseasonalise trends, for example, using Fourier terms or spline functions36 to model non-linear trends. Different lagged effects of the intervention, for example, no delayed effect of the intervention on surgical consults, and for the timing of the intervention for MSK diagnosis subgroup were conducted. An additional sensitivity analysis was conducted by restricting data analyses prior to 2020 to remove the potential time confounding effect of the COVID-19 on rates of consultations. All analyses were performed using Stata V.17 software package (StataCorp LLC, Texas, USA).
Patient and public involvement
Aims and designs of the study were discussed with a patient/user representative who regularly attends research meetings as part of the AID-Spine project. Data linkage and data protection restriction prevented greater involvement in study analyses. Patient representatives will provide guidance on dissemination of the results in lay language for distribution in user organisations.
Results
Characteristics of the participant sample of 82 072 Norwegians were similar across the 3 health surveys (table 1). Only a small percentage of data (<0.6%) was missing for education status. Given the small impact on sample size, complete cases were used for the subgroup analyses by education level.37 Exploratory analysis of longitudinal trends for all outcomes demonstrated stationarity, therefore no transformation of data was performed.
Table 1. Characteristics of included participants from three Norwegian Health surveys.
| Survey | HUNT 4(n=56 038) | Tromso7(n=21 068) | MUST(n=4966) |
| Characteristic | |||
| Age average (year 2014) | 55 (SD 15.3) | 56 (SD 11.5) | 59 (10.2) |
| Education (%) | |||
| Lower | 18 | 17 | 21 |
| Intermediate | 50 | 41 | 52 |
| Undergraduate | 26 | 28 | 21 |
| Postgraduate | 6 | 14 | 6 |
| Sex (%) | |||
| Male | 45 | 48 | 45 |
| Female | 55 | 52 | 55 |
| Healthcare provider seen (2014–2021) (% total consultations) | |||
| Physical therapist | 55 | 45 | 49 |
| Chiropractor | 13 | 10 | 14 |
| Medical doctor | 32 | 45 | 37 |
HUNT4The HUNT4 SurveyMUSTMusculoskeletal pain in Ullensaker Studynnumber of participants
Primary outcomes
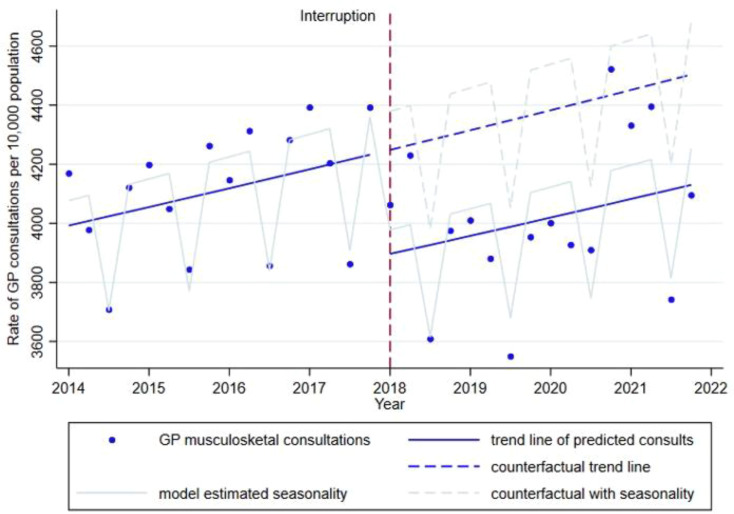
The mean quarterly rate of GP consultations for MSK conditions was 4061 per 10 000 participants, with a minimum of 3550 consultations occurring quarter 3 in 2019 and maximum of 4522 consultations occurring quarter 4 in 2020 (figure 2). The primary segmented regression model estimated an immediate stepped reduction of 391 GP consultations per 10 000 participants, (95% CI: −564 to −216) associated with the introduction of direct access physiotherapy in Norway. Model estimates suggested an average increase of 18 GP consultations each quarter (95% CI: 9 to 27) from 2014. There was no significant difference in the slope of the quarterly trend (p=0.938) before, compared with after the introduction of direct access physiotherapy after accounting for the stepped reduction in consultations, and this was removed from the final model. (See table 2 for model estimates for primary outcomes).
Figure 2. 2014 age-standardised rates of general practitioner (GP) musculoskeletal (MSK) consultations before and after the introduction of direct access physiotherapy in Norway.
Table 2. Results of segmented regression models, reported in consultation/procedure rates per 10 000 population, (2014 age standardised).
| GP consultations | Physiotherapy consultations | Specialist consultations | Surgical procedures | |||||
| Value (CI 95%) | P value | Value (CI 95%) | P value | Value (CI 95%) | P value | Value (CI 95%) | P value | |
| Variable | ||||||||
| Trend over time | 18.17 (8.99 to 27.35) | P<0.000 | −48.73 (−67.23 to −30.22) | P<0.000 | 0.43 (0.15 to 0.71) | P=0.003 | −0.01 (−0.08 to 0.01) | P=0.871 |
| Immediate intervention effect | −390.79 (−564.73 to −216.86) | P<0.000 | n/a | n/a | −3.95 (−9.88 to 1.98) | P=0.192 | −0.001 (−0.01 to 0.01) | P=0.653 |
| Trend change pre intervention/post intervention | n/a | n/a | 0.47 (−0.62 to 1.58) | P=0.477 | −0.16 (−0.76 to 0.45) | P=0.656 | n/a | n/a |
| Seasonal change | −413.39 (−474.56 to −352.41) | P<0.000 | −1403.56 (−1674.24 to −1132.88) | P<0.000 | −17.10 (−20.53 to −13.67) | P<0.000 | −1.41 (−2.35 to −0.48) | P<0.000 |
| Constant | 4061.99 (4045.01 to 4078.97) | P<0.000 | 5965.44 (5830.41 to 6100.47) | P<0.000 | 83.75 (81.65 to 85.86) | P<0.000 | 7.59 (7.19 to 8.00) | P<0.000 |
Value=model estimated consultations/procedures per 10 000 population.
GPgeneral practitioner
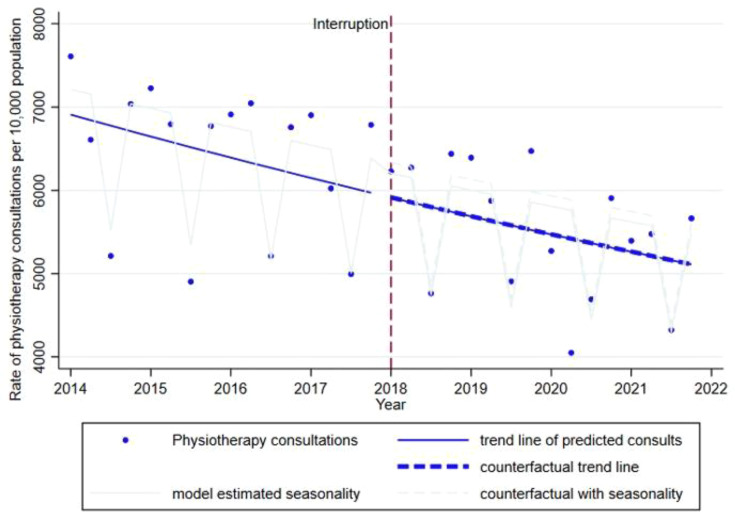
The mean quarterly rate of physiotherapy consultations for MSK conditions was 5966 per 10 000 participants, with a minimum of 4049 consultations in quarter 2 in 2020 and maximum of 7608 in quarter 1, 2014. There was a steady decline in physiotherapy consultations from 2014 through to 2021, with a model estimated decrease of 48 physiotherapy consultations per 10 000 participants per quarter (figure 3). This steady decline did not change with the introduction of direct access physiotherapy, with model estimated change in slope 0.5 (95% CI: −0.6 to 1.6).
Figure 3. 2014 age-standardised rates of physiotherapy musculoskeletal (MSK) consultations before and after the introduction of direct access physiotherapy in Norway.
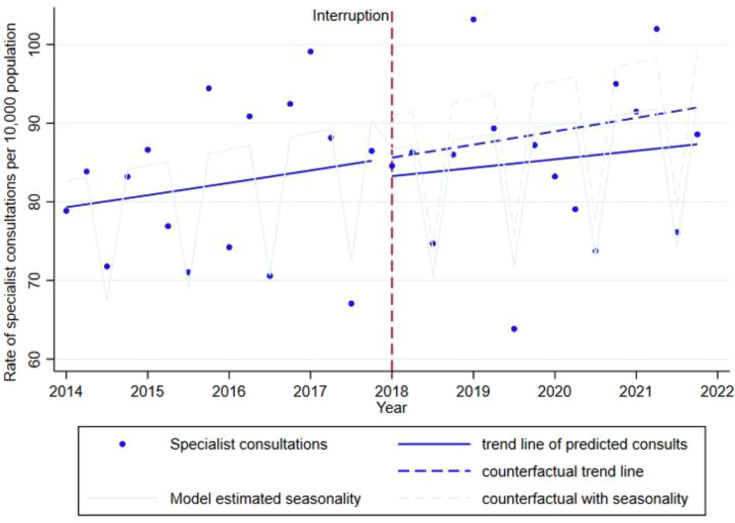
The mean quarterly rate of specialist consultations for back or neck conditions was 84 per 10 000 participants, with a minimum of 64 consultations in quarter 3 in 2019 and a maximum of 103 in quarter 1, 2019 (figure 4). Rates of specialist consultations increased at a low rate of 0.4 consultations per quarter (95% CI: 0.2 to 0.7). There was no associated effect of the introduction of direct access physiotherapy on specialist consultations either immediately (B= −4, 95% CI: −10 to 2) or on the trend in consultations (B=−0.2, 95% CI: −0.8 to 0.4) each quarter.
Figure 4. 2014 age-standardised rates of specialist spinal consultations before and after the introduction of direct access physiotherapy in Norway.
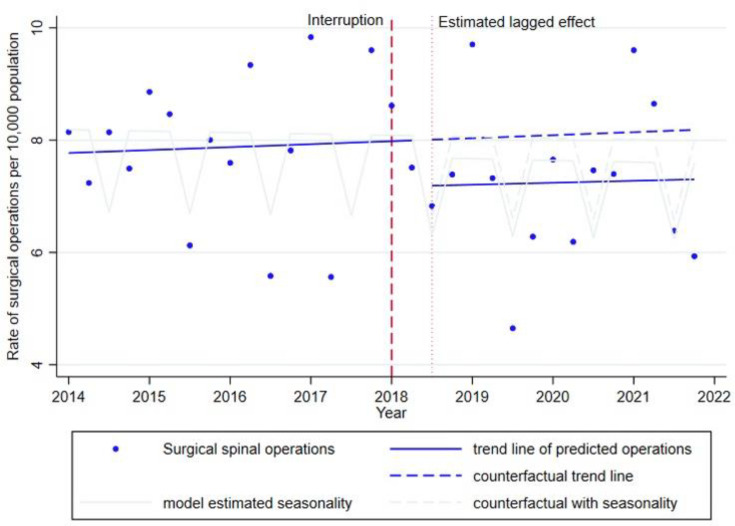
The mean quarterly rate of surgical operations for back or neck conditions was 8 per 10 000 participants, with a minimum of 5 operations in quarter 3 in 2019 and maximum of 10 in quarter 1, 2017 (figure 5). There was no change in surgical procedures over the analysed time period (B=−0.006, 95% CI: −0.08 to 0.07). There was no associated effect of the introduction of direct access physiotherapy on the rate of surgical consultations demonstrated (B=−0.001, 95% CI: −0.01 to 0.007).
Figure 5. 2014 age-standardised rates of spinal operations before and after the introduction of direct access physiotherapy in Norway.
Subgroup analyses
Following separate segmented regression for each subgroup, three subgroups demonstrated trends that were not in accordance with primary outcomes. The trend in quarterly rates of physiotherapy consultations reduced for those in the lower education group by 150 consultations per quarter (95% CI: −203 to −97) and intermediate education group by 70 consultations (95% CI: −115 to −27) associated with the introduction of direct access physiotherapy. For those aged between 40 and 60 years, there was an estimated stepped reduction of two surgical procedures (95% CI: −3 to −1) associated with a predetermined lagged effect of two quarters following the introduction of direct access physiotherapy (see online supplemental figures 1–3 and online supplemental tables 2–4 for regression plots and model estimates).
Sensitivity analyses
Divergence of GP consults from a seasonal trend after 2020, resulted in some variance in residuals using the modelled seasonality adjustment. A sensitivity analysis removing the seasonal dummy variable, improved the residual variance after 2020, resulting in a slightly smaller step change, estimating a reduction of 351 GP consultations (95% CI: −582 to −122) associated with the intervention. A secondary sensitivity analysis using spline functions to model seasonality indicated a slightly higher step change for GP consultations, estimating a reduction of 417 consultations (95% CI: −570 to −237, p≤0.000) following the introduction of direct access physiotherapy. Due to potential underfitting (without seasonality) and overfitting (using spline functions), the original model was chosen for primary analysis. Sensitivity analyses, using models for physiotherapy consultations including an estimated step change, did not alter the reported findings from primary models. Removing the lagged effect of direct access physiotherapy on surgical operations did not alter findings (B=0.001, 95% CI: −0.078 to 0.006). Limiting analyses to exclude data after the year 2020 (after the first recorded COVID-19 cases in Norway) did not impact the direction of effect for any primary outcomes but resulted in a slight reduction in the size of the stepped effect on GP consultations (−348 consultations, 95% CI: −483 to −213, p<0.000).
Discussion
The findings from this study demonstrate a stepped reduction of approximately 10%, in the rates of GP consultations for MSK conditions in Norway primary care, associated with the introduction of a direct access physiotherapy model of care in 2018. The introduction of this model of care was not associated with a change in rates of physiotherapy consultations for MSK conditions, nor the rates of specialist consultations or surgery for spinal conditions. Exploratory analysis of subgroups indicated an associated reduction in the quarterly rates of physiotherapy MSK consultations for those in the lower and intermediate education groups following the introduction of the direct access to physiotherapy model. Additionally, a stepped reduction of spinal operations was observed in those aged between 40 and 60 years, 6 months after the introduction of the model of care. We did not observe any association between the introduction of the direct access to physiotherapy model of care and primary outcome measures for different MSK conditions (back, neck, shoulder and knee).
The demonstration of an immediate reduction in the number of GP consultations associated with the introduction of a direct access to physiotherapy model, is a novel finding. While no previous research has used an interrupted time series design to evaluate the impact of introducing this intervention at a specific time point, at a healthcare system level, there is evidence that direct access to physiotherapy can reduce GP MSK workload. A national 1-year trial, conducted across 26 clinics in Scotland, observed those who directly accessed physiotherapy spent 50% less time consulting with GPs compared with those who first consulted with their GP.38 While not directly comparable to our results, the authors extrapolated this would equate to 400 weeks of freed GP appointment time in Scotland each year, based on an estimated 22% of patients self-referring directly to physio for MSK management. In contrast, a 5-year longitudinal evaluation of the national introduction of direct access physiotherapy model of care in the Netherlands, did not report a reduction in GP workload.19 However, the evaluation did not investigate total GP MSK consultations prior to the introduction of the service, relying on incidence rates of the top five MSK conditions as an indication of GP workload. One proposed mechanism by which direct access physiotherapy can reduce GP workload is through a reduction in repeat visits to GPs.38 Not including this may have led to an under-reporting on the impact of direct access physiotherapy on GP workload following the introduction of this pathway in the Netherlands.
A concern raised in opposition to direct access physiotherapy models of care is the prospect of an overwhelming increase in physiotherapy consultations following the removal of the GP gatekeeper role. Results of the current study do not support this. The data showed a steady declining rate of consultations with physiotherapist in Norway that remained unaffected by the introduction of direct access to physiotherapy care in 2018. This finding was also reported following Scotland’s national trial, and in the 1-year follow-up of the national introduction of direct access physiotherapy in the Netherlands, where overall physiotherapy consultations did not increase after the introduction of the new model of care.30 38
It is plausible that introducing a direct access pathway to physiotherapy care in Norway, simply removed the unnecessary step of having to see the GP first (prior to referral), resulting in a drop in GP consultations for those who self-referred to a physiotherapist. This may also partly explain why physiotherapy consultations did not increase. Rather than a new group of patients accessing physiotherapy care, it could be hypothesised that consultations consisted of those who were referred by GPs and those who self-referred (who would previously been referred by their GP).30
In addition, direct access physiotherapy was not associated with a change in the rates of specialist consultations or surgical procedures for spinal conditions. While little is known about the impact on rates of surgery associated with this model in primary care, previous evaluation of direct triage to physiotherapy services, at a clinic level, has demonstrated a reduction in specialist referrals associated with physiotherapy led care.15 18 Non-experimental studies conducted in primary care in Sweden and the UK observed a 61%15 reduction in specialist referrals (ie, rheumatologists, orthopaedics, pain physicians, neurologists) and up to 64%18 reduction in orthopaedic referrals, respectively, when patients initiated care with a physiotherapist compared with a GP. The contrasting findings between these results, and the findings observed in the current study, might be explained by a smaller percentage of those whose who used the direct access pathway. Unlike these service evaluations, the direct access model of care in Norway permits patients to choose their initial provider. While the numbers of those self-referring to physiotherapy were not measured in the current study, the estimated 10% decrease in GP consultations would suggest a significant proportion of patients still initiated care with their GP, potentially reducing the impact on specialist referral rates. Supporting this idea, Holdsworth et al38 observed that rates of specialist referrals were doubled for those patients who started care with their GP compared with those who self-referred to physiotherapy. These results underline the importance of uptake of this direct access service by self-referrers, and perhaps emphasise the need for public awareness and education to support this model of care.30 39
We found exploratory evidence to suggest that the introduction of direct access physiotherapy model was associated with a reduction in physiotherapy consultations in the intermediate and lower education groups. The differences in characteristics of patients self-referring for physiotherapy compared with those who use GP-led care, provides a possible explanation for this finding. Although this study did not collect patient level characteristics, recent systematic reviews suggest those who access physiotherapy directly may be more educated (younger and with a short duration of symptoms) than those who use GP-led care.13 40 It is possible that a higher proportion of physiotherapy consultations were used by those more highly educated patients who self-directed to physiotherapy following the introduction of this service, reducing the availability for those in lower educations groups who might be more likely to rely on a GP referral.
The associated reduction in spinal surgery for those aged 40–60 years is intriguing. While age-standardised rates of spinal surgery in Norway are typically highest in those aged 60–74 years, spinal surgery for those aged 40–60 years typically accounts for the largest proportion of procedures performed.41 With surgical procedures lowest in those aged 18–39 years, and older patients often preferring to see their GP to initiate care,30 it is perhaps surgical rates in the ‘middle-age’ bracket that are likely to reflect divergent treatment pathways affected by GPs and physiotherapists as initial care providers. For example, sciatic pain, with an incidence highest in this age group,42 is frequently managed surgically, though evidence suggests it can be adequately managed with conservative care.43 It is possible that direct access to physiotherapy in this subgroup of patients might offer improved earlier management of symptoms, reducing the need for escalated care (eg, surgery). An alternate mechanism of effect might be altered referral patterns, with physiotherapists less frequently referring for surgical consultations when managing patients with sciatic symptoms compared with GPs. The lack of participant-level data collected in this study, and the exploratory nature of the subgroup analysis (using separate segmented regressions for each group), precludes strong conclusions being interpreted from subgroup findings.
Strengths and limitations
The main strengths of the current study are the longitudinal analysis, large patient sample broadly representative of Norwegian population, and the use of routinely collected registry data to evaluate time series trends in healthcare utilisation, associated with the nationwide introduction of direct access physiotherapy in Norway. Although variability in MSK and diagnostic coding is a limitation of registry based studies, it is not expected this changed systematically across the time period analysed. Interrupted time series analyses are susceptible to time-varying confounders, and the variability seen in GP consultations after 2020 might reflect consultation changes with the impact of COVID-19. In Norway, stringent measures were introduced in March 2020 to control the spread of the COVID-19 pandemic including the closure of schools, universities and reduction in sporting events which may have impacted primary care consultation rates. Mean daily number of healthcare contacts for common MSK injuries (ie, dislocations, sprains and strains) reduced by 55% during the lockdown period between 13 March and 2 April, compared with the preceding month.44 While there are several explanations for this reduction in healthcare contacts (eg, reduced injury exposure or redistribution of healthcare resources limiting access to care), it appears trends normalised by June 2020. Similarly, a 50% reduction in GP consultations for MSK conditions reported between March and May in 2020 in Norway, reduced to an 8% difference by November 2020, compared with the referenced 5-year average.45 These findings suggest the lower rates of GP MSK consultations we observed in the first two quarters of 2020 might partly reflect changes in COVID-19-related healthcare use. What is less clear is how this might have influenced the following time period and potential increased usage of primary care services because of delayed access to care. Nonetheless, sensitivity analysis excluding years affected by COVID-19 disease did not meaningfully alter our results.
It is acknowledged that differences in the time frames of when surveys were administered may introduce selection bias if there are systemic differences in the cohort of participants responding to the early versus later surveys. However, baseline statistics across the three surveys demonstrated that characteristics were balanced for measured variables, and visual exploration of outcomes stratified by early survey responders (Ullensaker study) through to the late survey responders (The HUNT4 Survey) did not demonstrate differences in healthcare utilisation rates over the analysed time period. A further limitation of this study is the lack of patient-level data, preventing strong conclusions explaining healthcare utilisation rates associated with the direct access model of care. Finally, the reliability of the results in this study are based on the underlying assumptions of the segmented regression analyses being met. While Newey-West standard errors provide some accommodation for residual autocorrelation and heteroskedasticity, there was some variability of residuals in the GP regression model after the year 2020. Additionally, a lagged effect for the intervention on surgical procedures was based on field expertise, given a lack of prior evidence in the literature to inform the modelling. However, sensitivity analyses conducted demonstrated that our results were robust to altered assumptions and our conclusions would not be altered.
Clinical and policy implications
This study provides evidence that a nationwide introduction of direct access physiotherapy is associated with a reduction in GP workload. While this change may not be felt at the clinic,46 it may have implications at a healthcare system level. With an estimated 10% reduction in GP MSK consultations, an average GP consultation time in Norway of 18 minutes47 and a conservative total of 1 000 000 MSK consultations nationally,48 this could be extrapolated to represent over 900 weeks of freed GP time in Norway each year, based on an average of 33 hours of direct patient contact time.49 Given direct access was available to manual therapists since 2006, and they accounted for 10% of recorded MSK consultations in this cohort, the impact of GP workload when implementing this model of care, may be more pronounced in healthcare systems without a history of direct access physiotherapy. Current evidence suggests the wider impact of this model of care is largely dependent on the proportion of patients who choose to self-refer,38 39 the level of public awareness/education on how or why to directly access physiotherapy care,30 39 and the availability of physiotherapy services to support the model.50
The context of the healthcare system is also an important consideration. Norway is a high-income country with a well-established healthcare system. In Norway, GP funding is a mixed payment model, constituting payments from the municipality, fee for service and out-of-pocket payments from patients. Patients’ maximum out-of-pocket payments are also capped by the Norwegian government. The effectiveness of direct access physiotherapy in other healthcare systems is likely dependent on service accessibility and reach, funding for primary care service delivery and use, resource availability and population health profile.46 For example, in the absence of publicly funded physiotherapy services or capped out-of-pocket costs, self-referral to physiotherapy services is likely to be low and unlikely to impact GP workloads. In addition, the level of centralisation within healthcare systems is likely to impact widespread policy implementation of a direct access physiotherapy service. While our findings revealed consistent healthcare utilisation rates across geographical regions, it is possible that regional variation (eg, characteristics of the population distribution of primary care services) could influence the generalisability of these results. Collectively, these characteristics might limit the applicability of our findings in middle-income and lower-income countries. Future research evaluating this model of care should employ a broad range of effectiveness measures at a healthcare system level (eg, GP workload, cost-effectiveness), service (eg, medication prescription and imagine referral) and patient level outcomes (eg, pain and function). Consideration of these key factors in the context of other healthcare systems is needed before wider adoption can be promoted .
Conclusion
This is the first study to evaluate the longitudinal impact of the introduction of direct access physiotherapy on healthcare utilisation for MSK conditions, using an interrupted time series design. Results showed a 10% reduction in the rates of GP MSK consultations associated with the introduction of direct access physiotherapy, without an associated change in rates of physiotherapy consultations in Norwegian primary care. No change was observed in the rates of specialist consultations or surgical procedures for spinal pain, in the primary analysis. The associated reduction in GP workload, highlights the potential benefits of optimising healthcare resources and patient access to appropriate care, by offering direct access to physiotherapy at a healthcare system level. These findings build on existing knowledge demonstrating this model of care is safe and effective at a clinic level, strengthening support for the consideration of the implementation of direct access physiotherapy in similar healthcare systems.
supplementary material
Acknowledgements
We would like to acknowledge the curators and participants of The Tromsø Study, The Ullensaker Study and The Trøndelag Health Study (HUNT) Study. The HUNT is a collaboration between HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology), Trøndelag County Council, Central Norway Regional Health Authority and the Norwegian Institute of Public Health.
Footnotes
Funding: This study was funded by Norwegian Research Council (324915).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by Health Region of South-East Norway (2022/371282) and the Data Protection Authority of Norway has approved the registry protocol (Sikt ref no 558480). Written informed consent was obtained from all participants in the three surveys forming the basis for the sample of this study (HUNT4, Tromsø7 and Ullensaker4), including the consent to let the data be linked to public Norwegian health and welfare registers. The AID-Spine protocol has been registered in the ClinicalTrials.gov (Identifier: NCT05745129). Participants gave informed consent to participate in the study before taking part.
Data availability free text: Access to Norwegian public health and welfare registers and population survey data (HUNT4, Tromsø7 and Ullensaker4), including consent for data linkage, must be obtained from third parties and are not publicly available.
Patient and public involvement: Aims and designs of the study were discussed with a patient/user representative who regularly attends research meetings as part of the AID-Spine project. Data linkage and data protection restriction prevented greater involvement in study analyses. Patient representatives will provide guidance on dissemination of the results in lay language for distribution in user organisations.
Contributor Information
James Henry Zouch, Email: jzou3929@uni.sydney.edu.au.
Bjørnar Berg, Email: bjornarb@oslomet.no.
Are Hugo Pripp, Email: apripp@oslomet.no.
Kjersti Storheim, Email: kjersti.storheim@ous-research.no.
Claire E Ashton-James, Email: claire.ashton-james@sydney.edu.au.
Manuela L Ferreira, Email: mferreira@georgeinstitute.org.au.
Margreth Grotle, Email: mgrotle@oslomet.no.
Paulo H Ferreira, Email: paulo.ferreira@sydney.edu.au.
Data availability statement
Data may be obtained from a third party and are not publicly available.
References
- 1.Liu S, Wang B, Fan S, et al. Global burden of musculoskeletal disorders and attributable factors in 204 countries and territories: a secondary analysis of the Global Burden of Disease 2019 study. BMJ Open. 2022;12:e062183. doi: 10.1136/bmjopen-2022-062183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nicolson PJA, Williamson E, Morris A, et al. Musculoskeletal pain and loneliness, social support and social engagement among older adults: Analysis of the Oxford Pain, Activity and Lifestyle cohort. Musculoskeletal Care. 2021;19:269–77. doi: 10.1002/msc.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agarwal SD, Pabo E, Rozenblum R, et al. Professional Dissonance and Burnout in Primary Care: A Qualitative Study. JAMA Intern Med. 2020;180:395–401. doi: 10.1001/jamainternmed.2019.6326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearson WS, Bhat-Schelbert K, Probst JC. Multiple chronic conditions and the aging of America: challenge for primary care physicians. J Prim Care Community Heal. 2012;3:51–6. doi: 10.1177/2150131911414577. [DOI] [PubMed] [Google Scholar]
- 5.Dieleman JL, Baral R, Birger M, et al. US Spending on Personal Health Care and Public Health, 1996-2013. JAMA. 2016;316:2627–46. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li K, Frumkin A, Bi WG, et al. Biopsy of Canada’s family physician shortage. Fam Med Community Health. 2023;11:e002236. doi: 10.1136/fmch-2023-002236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kringos D, Boerma W, Hutchinson A, et al. Building primary care in a changing Europe. Eur Obs Heal Syst Policies. 2015:172. [PubMed] [Google Scholar]
- 9.Keavy R, Horton R, Al-Dadah O. The prevalence of musculoskeletal presentations in general practice: an epidemiological study. Fam Pract. 2023;40:68–74. doi: 10.1093/fampra/cmac055. [DOI] [PubMed] [Google Scholar]
- 10.Haas R, Gorelik A, Busija L, et al. Prevalence and characteristics of musculoskeletal complaints in primary care: an analysis from the population level and analysis reporting (POLAR) database. BMC Prim Care. 2023;24:40. doi: 10.1186/s12875-023-01976-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallotti M, Campagnola B, Cocchieri A, et al. Effectiveness and Consequences of Direct Access in Physiotherapy: A Systematic Review. J Clin Med. 2023;12:5832. doi: 10.3390/jcm12185832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodwin RW, Hendrick PA. Physiotherapy as a first point of contact in general practice: a solution to a growing problem? Prim Health Care Res Dev. 2016;17:489–502. doi: 10.1017/S1463423616000189. [DOI] [PubMed] [Google Scholar]
- 13.Babatunde OO, Bishop A, Cottrell E, et al. A systematic review and evidence synthesis of non-medical triage, self-referral and direct access services for patients with musculoskeletal pain. PLoS One. 2020;15:e0235364. doi: 10.1371/journal.pone.0235364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zouch J, Comachio J, Bussières A, et al. Influence of Initial Health Care Provider on Subsequent Health Care Utilization for Patients With a New Onset of Low Back Pain: A Scoping Review. Phys Ther. 2022;102:pzac150. doi: 10.1093/ptj/pzac150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bornhöft L, Larsson MEH, Thorn J. Physiotherapy in Primary Care Triage - the effects on utilization of medical services at primary health care clinics by patients and sub-groups of patients with musculoskeletal disorders: a case-control study. Physiother Theory Pract. 2015;31:45–52. doi: 10.3109/09593985.2014.932035. [DOI] [PubMed] [Google Scholar]
- 16.Hon S, Ritter R, Allen DD. Cost-Effectiveness and Outcomes of Direct Access to Physical Therapy for Musculoskeletal Disorders Compared to Physician-First Access in the United States: Systematic Review and Meta-Analysis. Phys Ther. 2021;101:1–11. doi: 10.1093/ptj/pzaa201. [DOI] [PubMed] [Google Scholar]
- 17.Bornhöft L, Thorn J, Svensson M, et al. More cost-effective management of patients with musculoskeletal disorders in primary care after direct triaging to physiotherapists for initial assessment compared to initial general practitioner assessment. BMC Musculoskelet Disord. 2019;20:186. doi: 10.1186/s12891-019-2553-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Downie F, McRitchie C, Monteith W, et al. Physiotherapist as an alternative to a GP for musculoskeletal conditions. Br J Gen Pract. 2019;69:E314–20. doi: 10.3399/bjgp19X702245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swinkels ICS, Kooijman MK, Spreeuwenberg PM, et al. An overview of 5 years of patient self-referral for physical therapy in the Netherlands. Phys Ther. 2014;94:1785–95. doi: 10.2522/ptj.20130309. [DOI] [PubMed] [Google Scholar]
- 20.Bishop A, Ogollah RO, Jowett S, et al. STEMS pilot trial: a pilot cluster randomised controlled trial to investigate the addition of patient direct access to physiotherapy to usual GP-led primary care for adults with musculoskeletal pain. BMJ Open. 2017;7:e012987. doi: 10.1136/bmjopen-2016-012987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kinge JM, Knudsen AK, Skirbekk V, et al. Musculoskeletal disorders in Norway: prevalence of chronicity and use of primary and specialist health care services. BMC Musculoskelet Disord. 2015;16:75. doi: 10.1186/s12891-015-0536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tyrdal MK, Perrier F, Røe C, et al. Musculoskeletal disorders in Norway: trends in health care utilization and patient pathways: a nationwide register study. Scand J Prim Health Care. 2024:1–11. doi: 10.1080/02813432.2024.2368848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. doi: 10.1136/bmj.h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jandoc R, Burden AM, Mamdani M, et al. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol. 2015;68:950–6. doi: 10.1016/j.jclinepi.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 26.WONCA Classification Committee CW . International classification of primary care, second edition (ICPC-2) Oxford University Press; 1998. www.globalfamilydoctor.com Available. [Google Scholar]
- 27.World Health Organization(WHO) International classification of diseases, 10th revision. Vol. 2. 2016
- 28.Nordic Medico-Statistical Committee NOMESCO classification of surgical procedures (NCSP). Vol. 1.15. 2011
- 29.Bakken IJ, Ariansen AMS, Knudsen GP, et al. The Norwegian Patient Registry and the Norwegian Registry for Primary Health Care: Research potential of two nationwide health-care registries. Scand J Public Health. 2020;48:49–55. doi: 10.1177/1403494819859737. [DOI] [PubMed] [Google Scholar]
- 30.Leemrijse CJ, Swinkels ICS, Veenhof C. Direct access to physical therapy in the Netherlands: results from the first year in community-based physical therapy. Phys Ther. 2008;88:936–46. doi: 10.2522/ptj.20070308. [DOI] [PubMed] [Google Scholar]
- 31.Igwesi-Chidobe CN, Bishop A, Humphreys K, et al. Implementing patient direct access to musculoskeletal physiotherapy in primary care: views of patients, general practitioners, physiotherapists and clinical commissioners in England. Physiotherapy. 2021;111:31–9. doi: 10.1016/j.physio.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalseth J, Halvorsen T. Health and care service utilisation and cost over the life-span: a descriptive analysis of population data. BMC Health Serv Res. 2020;20:435. doi: 10.1186/s12913-020-05295-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terraneo M. Inequities in health care utilization by people aged 50+: evidence from 12 European countries. Soc Sci Med. 2015;126:154–63. doi: 10.1016/j.socscimed.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 34.Turner SL, Karahalios A, Forbes AB, et al. Creating effective interrupted time series graphs: Review and recommendations. Res Synth Methods. 2021;12:106–17. doi: 10.1002/jrsm.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hategeka C, Ruton H, Karamouzian M, et al. Use of interrupted time series methods in the evaluation of health system quality improvement interventions: a methodological systematic review. BMJ Glob Health. 2020;5:e003567. doi: 10.1136/bmjgh-2020-003567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhaskaran K, Gasparrini A, Hajat S, et al. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42:1187–95. doi: 10.1093/ije/dyt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hughes RA, Heron J, Sterne JAC, et al. Accounting for missing data in statistical analyses: multiple imputation is not always the answer. Int J Epidemiol. 2019;48:1294–304. doi: 10.1093/ije/dyz032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holdsworth LK, Webster VS, McFadyen AK. What are the costs to NHS Scotland of self-referral to physiotherapy? Results of a national trial. Physiotherapy. 2007;93:3–11. doi: 10.1016/j.physio.2006.05.005. [DOI] [Google Scholar]
- 39.Bishop A, Chen Y, Protheroe J, et al. Providing patients with direct access to musculoskeletal physiotherapy: the impact on general practice musculoskeletal workload and resource use. The STEMS-2 study. Physiotherapy. 2021;111:48–56. doi: 10.1016/j.physio.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Demont A, Bourmaud A, Kechichian A, et al. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: a systematic review of the literature. Disabil Rehabil. 2021;43:1637–48. doi: 10.1080/09638288.2019.1674388. [DOI] [PubMed] [Google Scholar]
- 41.Grotle M, Småstuen MC, Fjeld O, et al. Lumbar spine surgery across 15 years: trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open. 2019;9:e028743. doi: 10.1136/bmjopen-2018-028743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007;99:461–73. doi: 10.1093/bja/aem238. [DOI] [PubMed] [Google Scholar]
- 43.Konstantinou K, Lewis M, Dunn KM, et al. Stratified care versus usual care for management of patients presenting with sciatica in primary care (SCOPiC): a randomised controlled trial. Lancet Rheumatol. 2020;2:e401–11. doi: 10.1016/S2665-9913(20)30099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ohm E, Hauge LJ, Madsen C, et al. Impact of the COVID-19 pandemic on the treatment of injuries during lockdown in Norway. Scand J Public Health. 2021;49:689–96. doi: 10.1177/1403494821993725. [DOI] [PubMed] [Google Scholar]
- 45.Velek P, de Schepper E, Schiphof D, et al. Changes to consultations and diagnosis of osteoarthritis in primary care during the COVID-19 pandemic. Osteoarthr Cartil. 2023;31:829–38. doi: 10.1016/j.joca.2023.02.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ojha HA, Snyder RS, Davenport TE. Direct access compared with referred physical therapy episodes of care: a systematic review. Phys Ther. 2014;94:14–30. doi: 10.2522/ptj.20130096. [DOI] [PubMed] [Google Scholar]
- 47.Irving G, Neves AL, Dambha-Miller H, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7:e017902. doi: 10.1136/bmjopen-2017-017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Statistics Norway GPs and emergency primary health care. 2024. https://www.ssb.no/en Available.
- 49.Rosta J, Rø KI. Changes in weekly working hours, proportion of doctors with hours above the limitations of European Working Time Directive (EWTD) and time spent on direct patient care for doctors in Norway from 2016 to 2019: a study based on repeated surveys. BMJ Open. 2023;13:e069331. doi: 10.1136/bmjopen-2022-069331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang M, Bishop A, Sussex J, et al. Economic evaluation of patient direct access to NHS physiotherapy services. Physiotherapy. 2021;111:40–7. doi: 10.1016/j.physio.2020.12.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data may be obtained from a third party and are not publicly available.