Abstract
Introduction
Postoperative pancreatic fistula (POPF) occurs in 25% of patients undergoing a high-risk pancreatoduodenectomy (PD) and is a driving cause of major morbidity, mortality, prolonged hospital stay and increased costs after PD. There is a need for perioperative methods to decrease these risks. In recent studies, preoperative chemoradiotherapy in patients with pancreatic ductal adenocarcinoma (PDAC) reduced the rate of POPF seemingly due to radiation-induced pancreatic fibrosis. However, patients with a high risk of POPF mostly have a non-pancreatic periampullary tumour and do not receive radiotherapy. Prospective studies using radiotherapy specifically to reduce the risk of POPF have not been performed. We aim to assess the safety, feasibility and preliminary efficacy of preoperative stereotactic radiotherapy on the future pancreatic neck transection margin to reduce the rate of POPF.
Methods and analysis
In this multicentre, single-arm, phase II trial, we aim to assess the feasibility and safety of a single fraction of preoperative stereotactic radiotherapy (12 Gy) to a 4 cm area around the future pancreatic neck transection margin in patients at high risk of developing POPF after PD aimed to reduce the risk of grade B/C POPF. Adult patients scheduled for PD for malignant and premalignant periampullary tumours, excluding PDAC, with a pancreatic duct diameter ≤3 mm will be included in centres participating in the Dutch Pancreatic Cancer Group. The primary outcome is the safety and feasibility of single-dose preoperative stereotactic radiotherapy before PD. The most relevant secondary outcomes are grade B/C POPF and the difference in the extent of fibrosis between the radiated and non-radiated (uncinate margin) pancreas. Evaluation of endpoints will be performed after inclusion of 33 eligible patients.
Ethics and dissemination
Ethical approval was obtained by the Amsterdam UMC’s accredited Medical Research Ethics Committee (METC). All included patients are required to have provided written informed consent. The results of this trial will be used to determine the need for a randomised controlled phase III trial and submitted to a high-impact peer-reviewed medical journal regardless of the study outcome.
Trial registration number
NL72913 (Central Committee on Research involving Human Subjects Registry) and NCT05641233 (ClinicalTrials).
Keywords: pancreatic surgery, radiotherapy, clinical trials, hepatobiliary disease, pancreatic disease
Strengths and limitations of this study.
FIBROPANC trial is a phase II trial designed to assess safety, feasibility and preliminary efficacy of preoperative stereotactic radiotherapy at the future pancreatic neck transection margin to reduce the risk of postoperative pancreatic fistula (POPF) after high-risk pancreatoduodenectomy (PD) for a non-pancreatic ductal adenocarcinoma (PDAC) indication.
The FIBROPANC study intervention may be practice-changing as POPF remains the primary driver of morbidity and early mortality after PD.
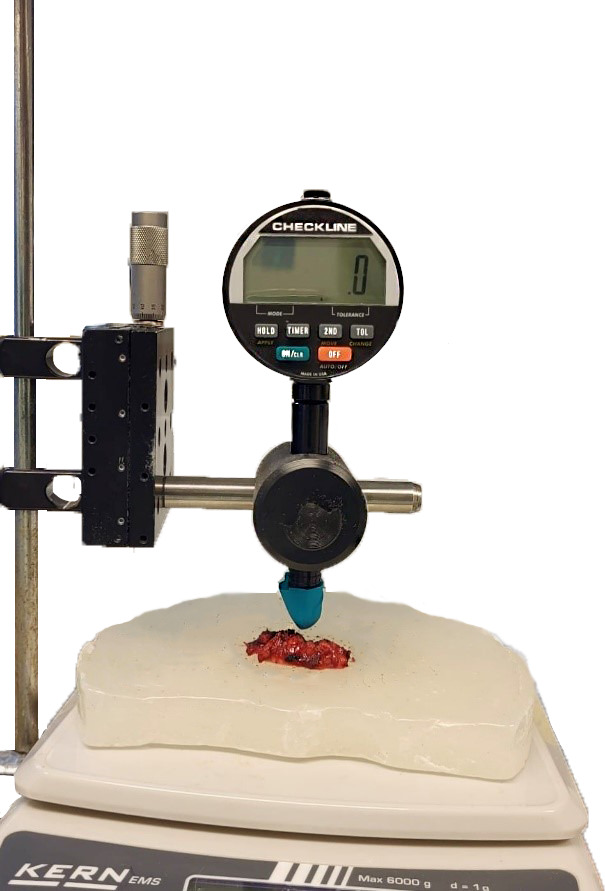
Radiation-induced pancreatic fibrosis is quantified by using the Rex Gauge Durometer and histopathological measurements.
All patients will receive a single fraction of 12 Gy preoperative stereotactic radiotherapy; dose escalation will not be investigated.
The primary focus of this trial is to assess the safety and feasibility of the study intervention; depending on the results, a randomised controlled phase III trial may be be initiated to draw a definite conclusion regarding efficacy.
Introduction
Postoperative pancreatic fistula (POPF) is a potentially life-threatening complication after pancreatoduodenectomy (PD) associated with a prolonged hospital stay, radiological and surgical interventions, higher readmission rates, higher costs and mortality.1,3 Although outcomes for pancreatic surgery improved in recent years, the rate of POPF has not decreased and occurs in up to 19% after PD.4 5 Soft pancreatic texture, small pancreatic duct diameter (≤3 mm), high body mass index and male sex are well-known risk factors for developing POPF.6 7 Furthermore, patients undergoing PD for diagnoses other than pancreatic ductal adenocarcinoma (PDAC) or chronic pancreatitis have a higher risk of POPF.8 9 These diagnoses include (pre)malignant tumours in the periampullary region, pancreatic neuroendocrine tumours and intraductal papillary mucinous neoplasm. Patients scheduled for PD for another diagnosis than PDAC or chronic pancreatitis with a non-dilated pancreatic duct (≤3 mm) have a risk of developing POPD of more than 25%, as identified by the nationwide, mandatory Dutch Pancreatic Cancer Audit (DPCA) 2014–2018 (table 1).10
Table 1. POPF after pancreatoduodenectomy in the mandatory Dutch Pancreatic Cancer Audit in the period 2014–2018.
| Total, n | POPF grade B/C, n (%) | |
| Diagnosis | ||
| PDAC | 1453 | 113 (7.8) |
| Cholangiocarcinoma | 452 | 107 (23.7) |
| Papillary carcinoma | 443 | 85 (19.2) |
| Duodenal carcinoma | 214 | 45 (21.0) |
| NET | 170 | 42 (24.7) |
| IPMN, SPN, MCN | 276 | 42 (15.2) |
| Chronic pancreatitis | 110 | 7 (6.4) |
| Other, unknown | 359 | 66 (18.4) |
| Main pancreatic duct diameter | ||
| MPD ≤3 mm | 892 | 209 (23.4) |
| MPD >3 mm | 1232 | 86 (7.0) |
| Risk categories | ||
| PDAC and MPD >3 mm | 681 | 26 (3.8) |
| PDAC and MPD ≤3 mm | 297 | 47 (15.8) |
| Non-PDAC* and MPD >3 mm | 538 | 60 (11.2) |
| Non-PDAC* and MPD ≤3 mm | 590 | 162 (27.5) |
Non-PDAC: cholangiocarcinoma, papillary/ampullary carcinoma, duodenal carcinoma, NET, IPMN, SPN, MCN.
IPMN, intraductal papillary mucinous neoplasm (all types, including invasive IPMN); MCN, mucinous cystic neoplasm; MPD, main pancreatic duct diameterPDAC, pancreatic ductal adenocarcinoma; POPF, postoperative pancreatic fistula according to the ISGPS 2016 criteria; SPN, solid-pseudopapillary neoplasm
Multiple studies reported a very low rate of grade B/C POPF of 0%–3.5% after PD in patients with PDAC who had preoperative chemoradiotherapy, compared with 8%–11% in patients after upfront surgery (pooled OR: 0.46, 96% CI: 0.29 to 0.73).11,14 This difference was not observed in studies with preoperative chemotherapy alone (without radiotherapy) compared with upfront surgery (pooled OR: 0.83, 95% CI: 0.59 to 1.16).12 The Dutch PREOPANC trial investigated the effect of neoadjuvant chemoradiotherapy in 246 patients with pancreatic cancer, using 15 fractions of 2.4 Gy in 3 weeks. In that study, a remarkably low POPF rate of 0% was observed in the chemoradiotherapy group, compared with 9.2% in the upfront surgery group (p=0.011).13 15 Changes in acinar cell function and pancreatic texture caused by radiotherapy may play a role in the declined risk of POPF after chemoradiotherapy. Radiation-induced fibrosis is characterised by tissue reorganisation and immune response modulation due to the accumulation of various cells (ie, fibroblasts and inflammatory cells) and extracellular matrix proteins, such as collagen, resulting in scar formation, possibly creating support at the site of the pancreatic enteral anastomosis.16 Additionally, histological evaluation of irradiated pancreatic tissue shows atrophy and distortion of the lobular structure with a decreased volume of acinar cells.17 Decreased exocrine secretion due to loss of acinar cells is suggested to have a positive effect on postoperative leakage.18 19 Currently, preoperative chemoradiotherapy is only indicated for patients undergoing PD for PDAC. In contrast, patients with periampullary tumours are at much higher risk for developing POPF.
In the current feasibility, safety and preliminary efficacy study, we assess the hypothesis that a single dose of preoperative radiotherapy of 12 Gy targeted at 4 cm centred around the future pancreatic transection margin may induce local fibrosis, thereby reducing the risk of POPF in patients at high risk of developing POPF (>25%) after PD.
Methods and analysis
Study design
In this single-arm, multicentre, open-label, phase II trial, patients planned for a PD at high risk for developing POPF who give informed consent undergo preoperative single fraction radiotherapy around the future transection margin of the pancreas. Given the yearly number of patients eligible for this study in the participating Dutch Pancreatic Cancer Group (DPCG) centres, the expected inclusion period will be 3–4 years, followed by analyses and assessments to evaluate radiation-induced firmness and fibrosis of pancreatic tissue. Patient recruitment started March 2021. The first part of the study will be performed to establish the safety and feasibility of the radiotherapy administration before PD. When the criteria for safety and feasibility are met, the second part of the study will start to provide a reliable estimate of the rate of grade B/C POPF (according to the International Study Group for Pancreatic Surgery, 20161) following the study intervention. The latter will be used to determine the need for a multicentre randomised controlled trial.
Patient and public involvement
Members of the patient platform ‘Living with Hope Foundation’ for patients and their relatives affected by pancreatic cancer were involved in the design of this research during the national multidisciplinary DPCG meetings.
Study population
The study population includes patients scheduled to undergo PD with a pancreatic duct diameter of ≤3 mm and diagnosis other than PDAC, thereby at high risk for developing POPF, as identified in the DPCA (table 1).
Eligibility criteria
Inclusion criteria
In order to be eligible to participate in this study, a patient must meet all of the following criteria:
Scheduled to undergo PD;
Pancreatic duct diameter ≤3 mm, measured on the diagnostic CT scan (at the level of the portomesenteric vein, at the pancreatic neck, the future anastomotic site);
WHO-ECOG performance status≤2;
Ability to undergo stereotactic radiotherapy and surgery;
Age≥18 years;
Good understanding of the oral and written patient information provided;
Written informed consent.
Exclusion criteria
Patients with any of the following criteria will be excluded:
Patients undergoing PD for (suspected) PDAC, chronic pancreatitis, or benign neoplasms (eg, serous cyst);
Patients with (a history of) chronic pancreatitis;
Contraindications for MRI.
Intervention
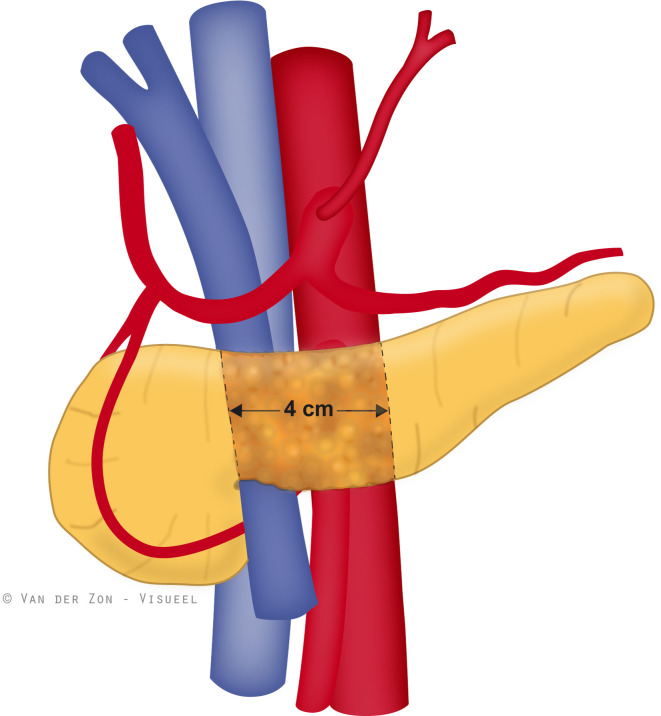
All patients will receive a preoperative single fraction stereotactic ablative radiotherapy (SABR) targeted at 4 cm around the future pancreatic neck transection margin, as shown in figure 1. The radiotherapy dose was calculated based on the dose given in the PREOPANC randomised trial (15 fractions of 2.4 Gy, delivered in 3 weeks) since a POPF rate of 0% was observed in the chemoradiotherapy group of that trial.13 To lower patient burden and the number of visits for study participants, the dose was converted to a single fraction of 12 Gy. Additionally, hypofractionation (increased dose per fraction) correlates directly with the degree of radiation-induced fibrosis in other tissue types.20 In preparation for treatment delivery, all patients will undergo MRI for MR-guided stereotactic radiotherapy. When CyberKnife stereotactic radiotherapy is used, a fiducial marker is placed endoscopically in the pancreatic tissue. However, after one serious adverse event (AE) (pancreatitis) following endoscopic fiducial marker placement, the CyberKnife radiotherapy approach was adapted to the internal target volume (ITV), without a fiducial marker using a planning CT scan. Patients are treated in a supine position. Radiotherapy treatment is performed in hospitals using SABR.
Figure 1. Single fraction stereotactic ablative radiotherapy will be targeted at 4 cm around the future pancreatic neck transection margin.
Target volumes, treatment planning, and dose prescription
The gross target volume (GTV) includes the middle of the pancreatic corpus, covering the intended location of the pancreatic-enteric anastomosis of the pancreas: from the right-sided border of the portal vein 4 cm to the left (ie, towards the spleen) (figure 1). Depending on institutional protocols, the planning target volume (PTV) margin will be generated by adding a 3–5 mm margin around the GTV. The dose prescription is 12 Gy in 1 fraction of the outline of the PTV, a cylinder encompassing the pancreatic duct and surrounding circumferential pancreatic tissue. Dosing constraints are D95%≥95% of the prescribed dose (95% of the PTV receives at least 95% of the prescribed dose), and D2%≤110% of the prescribed dose (2% of the PTV receives a maximum dose of 110% of the prescribed dose), meaning homogenous planning. Technologies used in this study to deliver SABR are MRI-guided intensity-modulated radiotherapy and CyberKnife technology. MRI-guided radiotherapy (MRgRT) enables real-time online adaptive planning. During MRgRT, before treatment, a new MR scan is acquired during a 17 s breath-hold in shallow inspiration. The PTV is generated from the GTV plus an isotropic 3 mm margin. Treatment is performed under breath-hold conditions. When treating using the CyberKnife (adapted procedure), an ITV is created based on the patient’s free breathing motion. The ITV will be made of different breathing phases on the in0% (beginning of inhalation), in50% (middle of inhalation), in100% (end of inhalation) and ex50 (middle of exhalation) (ITV=GTVin0%+GTV in50%+GTVin100%+GTVex50). The margin from ITV to PTV is 5 mm.
Durometer measurements
Several Durometers have been evaluated to quantify pancreatic hardness.21,23 The Rex Gauge Durometer (Rex Gauge Company, USA) outcomes range from 0 to 100 (Shore OO) and correlate well with the surgeon’s evaluation and the apparent diffusion coefficient values measured in MRI.21 Durometer outcomes were significantly lower in soft pancreatic tissue (median: 11, IQR: 8–13) compared with hard pancreatic tissue (median: 25, IQR: 21–28) (p<0.001).20 Therefore, the Rex Gauge Durometer Shore OO is used to assess pancreatic texture in the current study. In the current study, two samples of the resection specimen are derived at the pathology department for durometer measurements:
Sample of radiated tissue: the pancreatic transection plane, taken parallel to the transection plane;
Sample of non-radiated tissue: the uncinate process, taken as a cross-sectional horizontal section of at most caudal part.
To perform a robust measurement, the durometer is secured in the operating stand (figure 2), and a minimum sample thickness of 6 mm is required. First, the sample will be positioned under the durometer and pinned to paraffin to immobilise. The measurement is performed by pressing 500 g on the sample. To increase internal validity, these measurements will also be performed in controls (eligible patients who did not receive the study intervention). The average result of three repeated measurements on the exact location will be taken. After the measurements are completed, the samples are returned to the pathologist for regular diagnostics and preserved for further analysis.
Figure 2. Durometer (Rex Gauge Company, USA) set up to assess firmness of radiated and non-radiated pancreatic tissue.
Histopathological measurements
Another way to quantify fibrosis is via digital image analysis of the histological slide, determining the area of collagen using Sirius red staining.24 The samples from the pancreatic resection margin and uncinate process are separately submitted, and formalin-fixed, paraffin-embedded blocks are stored following the standard protocol. At the end of the study, blocks and/or unstained sections of the pancreatic resection plane and uncinate process are requested and stained with Sirius red at Amsterdam UMC. Through image analysis, the percentage of collagen per sample will be determined.
Endpoints
The primary objective is the safety and feasibility of single-dose preoperative radiotherapy prior to PD. All toxicities grade 3–5 potentially related to the preparation (eg, endoscopic fiducial marker placement) or administration of radiotherapy will be considered events for this endpoint. The intervention is defined as safe when ≤15% of patients experience grade 3–5 radiation toxicity. The AE rate should not be higher than the intended benefit. Feasibility is reached if a significant difference is measured in the hardness of the radiated part of the pancreas (resection margin), as compared with the non-radiated part of the pancreas within the same patient (the uncinate process of the pancreas) using the digital Rex Gauge Durometer, Model DD-4 Digital Durometer Type Shore OO.21 The Durometer measurement will be obtained via ex vivo measurements.
Secondary endpoints
POPF grade B/C1;
Histopathological assessment of fibrosis measured as the percentage of collagen in the pancreatic resection margin (radiated part) as compared with the uncinate process (non-radiated part);
Pancreatic texture, determined intraoperatively by the pancreatic surgeon;
Length of hospital stay in days;
Unplanned hospital admission after endoscopy, radiotherapy or surgery;
30-day mortality and in-hospital mortality;
Postoperative pancreatic function (exocrine or endocrine insufficiency) is determined by measuring faecal elastase and using antidiabetics and pancreatic enzyme replacement therapy.
Surgical techniques
Somatostatin analogues, for example, Pasireotide, will be administered perioperatively according to the institutional protocols for each centre. PD and anastomotic technique will be performed per the institutional standard. Both open and minimal invasive PD are included.
Study procedures
Patient screening and informed consent
Eligible patients will be identified at the outpatient clinic and informed about the trial. After 48 hours of consideration, additional questions can be answered, and informed consent will be obtained. The patient informed consent form can be found in online supplemental material 1. This includes consent for publication. After written informed consent, patients will be scheduled for an intake with the responsible radiotherapist, who will plan imaging and radiotherapy. After the single fraction radiotherapy, PD will follow after 4–6 weeks. A minimum period of 4 weeks is considered to allow fibrosis to develop. Radiation-induced injury is divided into an early inflammatory phase, which typically occurs directly after radiation exposure, and a late fibroproliferative phase, occurring after months.25 Although maintaining a longer period after radiotherapy might benefit fibrosis, postponing surgery for several months in patients with (pre-)malignant disease is not desirable. Patients in whom surgery is ultimately performed within this 4-week window are replaced.
Data collection
All measurements, methods and/or tests used to assess the defined study parameters/endpoints are collected within standard postoperative care. Data management is conducted using Castor Electronic Data Capture system. Personal information will be securely managed to preserve confidentiality. Access to the dataset will be restricted to authorised personnel only.
Withdrawal of individual patients
Patients can withdraw consent to the study at any time for any reason if they wish to do so without any consequences. The investigator can withdraw a patient from the study for urgent medical reasons. Follow-up of patients withdrawn from treatment is following usual care.
Replacement of individual patients
Patients who drop out of the study before receiving the intervention (ie, radiotherapy) or patients who undergo PD within 4 weeks after radiotherapy will be replaced.
Safety reporting
Under section 10, subsection 1, of the Medical Research Involving Human Subjects Act (WMO), the investigator will inform the patients and the reviewing accredited MEC if anything occurs, based on which it appears that the disadvantages of participation may be significantly greater than was foreseen in the research proposal. The study will be suspended pending further review by the accredited METC, except insofar as suspension would jeopardise the patient’s health. The investigator will take care that all patients are kept informed. The sponsor has an insurance that provides cover for injury or death caused by the study.
Adverse events
AEs are any undesirable experience occurring to a patient during the study, whether or not considered related to fiducial marker placement or stereotactic radiotherapy. All AEs classified as Common Terminology Criteria for Adverse Events (CTCAE) V.5.0 grade 3 or higher reported spontaneously by the patient or observed by the investigator or his staff will be recorded. All episodes of those mentioned above acute and late AEs from fiducial marker placement will be reported and scored for severity using the NCI CTCAE V.5.0.
Radiation-induced AEs include fatigue, loss of appetite, nausea/vomiting, stomach ulcers and diarrhoea. All episodes of those as mentioned earlier acute and late AEs from stereotactic radiation therapy will be reported and scored for severity using the NCI CTCAE V.5.0. All patients receive acid blockers and analgesics as standard of postoperative care after PD.
Serious adverse events (SAEs)
A SAE is any untoward medical occurrence or effect that
Results in death;
Is life-threatening (at the time of the event);
Requires hospitalisation or prolongation of existing inpatients' hospitalisation;
Results in persistent or significant disability or incapacity;
Is a congenital anomaly or defect;
Any other important medical event, based on appropriate judgement by the investigator.
The sponsor will report all grade 4 events (possibly related to stereotactic radiotherapy or surgery) and all deaths (regardless of attribution) occurring until 30 days after surgery. These SAEs will be reported through the preferred web portal to the accredited MEC that approved the protocol within 15 days after the sponsor knows the SAE. Only hospitalisations that prolong an existing hospitalisation of >10 days will be reported. All SAEs will be reported until the end of the study. All participating physicians involved in the FIBROPANC trial must brief the study coordinator in case of mortality or any unexpected event that prolongs hospitalisation or leads to readmission.
Follow-up of AE
All AEs will be followed until they have abated or a stable situation has been reached. Depending on the event, follow-up may require additional tests or medical procedures as indicated and/or referral to the general physician or a medical specialist. SAEs will be reported until the end of the study.
Data safety monitoring
Since this feasibility study included a small number of patients (n=33), no Data Safety Monitoring Board (DSMB) was installed.
Study monitoring
A clinical research associate will monitor the study. All monitoring visits will be scheduled at mutually agreeable times, periodically during the study at an appropriate frequency. These visits will be conducted to evaluate the progress of the study, to ensure that the rights and well-being of the patients are protected, to check that the reported clinical study data are accurate, complete and verifiable from source documents, and if the conduct of the study complies with the approved protocol and amendments, good clinical practice and applicable national regulatory requirements. A monitoring visit will include a review of the essential clinical study documents (regulatory documents, case report forms, source documents, patient informed consent forms, etc) and a discussion on the conduct of the study with the investigators. The investigators should be available during these visits to facilitate the review of the clinical study records and to discuss, resolve and document any discrepancies found during the visit.
Protocol amendments
Amendments are changes made to the research protocol after a favourable opinion by the accredited METC has been given. All amendments will be notified to the METC that gave a favourable opinion, the most recent version (V.3, dd 11 August 2022) was approved on 13 May 2024 and can be found in online supplemental material 2.
Sample size and analyses
With a sample size of 20 eligible patients and an expected reduction of 15% in POPF, a maximum of 3 (<15%) patients with grade 3–4 toxicity related to the intervention (stereotactic radiotherapy) is accepted. Furthermore, for feasibility in 20 patients, a one-sample t-test with a 5% one-sided significance level will have 80% power to detect the difference between a null hypothesis mean of 11 and an alternative mean of 25 (on Durometer measurements), assuming that the SD is 21.198 as based on a recent publication.21 For the second part, focusing on clinical assessment to provide a reliable estimate of the rate of grade B/C POPF following the study intervention, an additional 13 patients are needed to calculate a reduction in POPF from the baseline risk of >25% to 10% (alpha=0.05, power 0.80), intended 15% reduction. A complete analysis of all endpoints (safety, feasibility and POPF) is required in 33 eligible patients to prevent Type II errors.
Suppose an endpoint cannot be evaluated due to unforeseen circumstances (eg, a patient does not undergo resection due to the discovery of metastases during exploratory laparotomy or withdrawal of informed consent before the intervention). In that case, an additional patient will be included. All patients who received the intervention will remain in the study for follow-up. The expected risk of unforeseen circumstances in the study population is low.
Ethics and dissemination
Ethical approval in the Amsterdam UMC was received on 20 July 2020. The trial was registered on 23 February 2021 on the Central Committee on Research involving Human Subjects Register Central Committee on Research involving Human Subjects Registerwith trial number NL72913, and on ClinicalTrials.govClinicalTrials.gov with trial number NCT05641233 on 07 December 2022 . This study will be conducted according to the principles of the Declaration of Helsinki (version October 2013) and the Dutch WMO. The treating physician will inform eligible patients about the study and will explain the aims, methods, anticipated benefits and potential hazards. Also, this information will be provided in print. Written informed consent is required before any study-related procedures take place.
The results of this trial will be submitted to a high-impact peer-reviewed medical journal regardless of the study outcome. Authorship eligibility will be determined according to the current International Committee of Medical Journal Editors guidelines and data will be shared on reasonable request.
The Standard Protocol Items: Recommendations for Interventional Trials checklist can be found in online supplemental material 3.
supplementary material
Acknowledgements
The authors would like to thank the patients who will participate in the study.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-087193).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Collaborators: for the Dutch Pancreatic Cancer Group (DPCG).
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
J. Annelie Suurmeijer, Email: j.a.suurmeijer@amsterdamumc.nl.
Leonoor V. Wismans, Email: l.wismans@erasmusmc.nl.
Tessa E. Hendriks, Email: t.hendriks@dica.nl.
Anna M. Bruynzeel, Email: ame.bruynzeel@amsterdamumc.nl.
Joost J. Nuyttens, Email: j.nuyttens@erasmusmc.nl.
Martijn P.W. Intven, Email: M.Intven@umcutrecht.nl.
Lydi M.J.W. van Driel, Email: l.m.j.w.vandriel@erasmusmc.nl.
Bas Groot Koerkamp, Email: b.grootkoerkamp@erasmusmc.nl.
Olivier R. Busch, Email: o.r.busch@amsterdamumc.nl.
Jaap J. Stoker, Email: j.stoker@amsterdamumc.nl.
Joanne Verheij, Email: j.verheij@amsterdamumc.nl.
Arantza Farina, Email: a.farina@amsterdamumc.nl.
Michail Doukas, Email: m.doukas@erasmusmc.nl.
Ignace H.J. de Hingh, Email: ignace.d.hingh@catharinaziekenhuis.nl.
Daan J. Lips, Email: d.lips@mst.nl.
Erwin van der Harst, Email: harste@maasstadziekenhuis.nl.
Geertjan van Tienhoven, Email: g.vantienhoven@amsterdamumc.nl.
Marc G. Besselink, Email: m.g.besselink@amsterdamumc.nl.
Casper H.J. van Eijck, Email: c.vaneijck@erasmusmc.nl.
References
- 1.Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584–91. doi: 10.1016/j.surg.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 2.Wang J, Ma R, Churilov L, et al. The cost of perioperative complications following pancreaticoduodenectomy: A systematic review. Pancreatology. 2018;18:208–20. doi: 10.1016/j.pan.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Mackay TM, Wellner UF, van Rijssen LB, et al. Variation in pancreatoduodenectomy as delivered in two national audits. Br J Surg. 2019;106:747–55. doi: 10.1002/bjs.11085. [DOI] [PubMed] [Google Scholar]
- 4.Smits FJ, Henry AC, Besselink MG, et al. Algorithm-based care versus usual care for the early recognition and management of complications after pancreatic resection in the Netherlands: an open-label, nationwide, stepped-wedge cluster-randomised trial. Lancet. 2022;399:1867–75. doi: 10.1016/S0140-6736(22)00182-9. [DOI] [PubMed] [Google Scholar]
- 5.Suurmeijer JA, Henry AC, Bonsing BA, et al. Outcome of Pancreatic Surgery During the First 6 Years of a Mandatory Audit Within the Dutch Pancreatic Cancer Group. Ann Surg. 2023;278:260–6. doi: 10.1097/SLA.0000000000005628. [DOI] [PubMed] [Google Scholar]
- 6.Mungroop TH, Klompmaker S, Wellner UF, et al. Updated Alternative Fistula Risk Score (ua-FRS) to Include Minimally Invasive Pancreatoduodenectomy: Pan-European Validation. Ann Surg. 2021;273:334–40. doi: 10.1097/SLA.0000000000003234. [DOI] [PubMed] [Google Scholar]
- 7.Schuh F, Mihaljevic AL, Probst P, et al. A Simple Classification of Pancreatic Duct Size and Texture Predicts Postoperative Pancreatic Fistula: A classification of the International Study Group of Pancreatic Surgery. Ann Surg. 2023;277:e597–608. doi: 10.1097/SLA.0000000000004855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Roessel S, Mackay TM, van Dieren S, et al. Textbook Outcome: Nationwide Analysis of a Novel Quality Measure in Pancreatic Surgery. Ann Surg. 2020;271:155–62. doi: 10.1097/SLA.0000000000003451. [DOI] [PubMed] [Google Scholar]
- 9.van Dam JL, Bonsing BA, van Santvoort HC, et al. The influence of diagnosis on complications after pancreatoduodenectomy: results from a nationwide audit. HPB (Oxford) 2021;23:S272. doi: 10.1016/j.hpb.2020.11.687. [DOI] [Google Scholar]
- 10.van Rijssen LB, Koerkamp BG, Zwart MJ, et al. Nationwide prospective audit of pancreatic surgery: design, accuracy, and outcomes of the Dutch Pancreatic Cancer Audit. HPB (Oxf) 2017;19:919–26. doi: 10.1016/j.hpb.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Cooper AB, Parmar AD, Riall TS, et al. Does the use of neoadjuvant therapy for pancreatic adenocarcinoma increase postoperative morbidity and mortality rates? J Gastrointest Surg. 2015;19:80–6. doi: 10.1007/s11605-014-2620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Dongen JC, Wismans LV, Suurmeijer JA, et al. The effect of preoperative chemotherapy and chemoradiotherapy on pancreatic fistula and other surgical complications after pancreatic resection: a systematic review and meta-analysis of comparative studies. HPB (Oxf) 2021;23:1321–31. doi: 10.1016/j.hpb.2021.04.027. [DOI] [PubMed] [Google Scholar]
- 13.van Dongen JC, Suker M, Versteijne E, et al. Surgical Complications in a Multicenter Randomized Trial Comparing Preoperative Chemoradiotherapy and Immediate Surgery in Patients With Resectable and Borderline Resectable Pancreatic Cancer (PREOPANC Trial) Ann Surg. 2022;275:979–84. doi: 10.1097/SLA.0000000000004313. [DOI] [PubMed] [Google Scholar]
- 14.Wismans LV, Suurmeijer JA, van Dongen JC, et al. Preoperative chemoradiotherapy but not chemotherapy is associated with reduced risk of postoperative pancreatic fistula after pancreatoduodenectomy for pancreatic ductal adenocarcinoma: a nationwide analysis. Surgery. 2024;175:1580–6. doi: 10.1016/j.surg.2024.01.029. [DOI] [PubMed] [Google Scholar]
- 15.Versteijne E, Suker M, Groothuis K, et al. Preoperative Chemoradiotherapy Versus Immediate Surgery for Resectable and Borderline Resectable Pancreatic Cancer: Results of the Dutch Randomized Phase III PREOPANC Trial. J Clin Oncol. 2020;38:1763–73. doi: 10.1200/JCO.19.02274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ding NH, Li JJ, Sun LQ. Molecular mechanisms and treatment of radiation-induced lung fibrosis. Curr Drug Targets. 2013;14:1347–56. doi: 10.2174/13894501113149990198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Takahashi H, Ogawa H, Ohigashi H, et al. Preoperative chemoradiation reduces the risk of pancreatic fistula after distal pancreatectomy for pancreatic adenocarcinoma. Surgery. 2011;150:547–56. doi: 10.1016/j.surg.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 18.Uchida E, Tajiri T, Nakamura Y, et al. Relationship between grade of fibrosis in pancreatic stump and postoperative pancreatic exocrine activity after pancreaticoduodenectomy: with special reference to insufficiency of pancreaticointestinal anastomosis. J Nippon Med Sch. 2002;69:549–56. doi: 10.1272/jnms.69.549. [DOI] [PubMed] [Google Scholar]
- 19.Gurusamy KS, Koti R, Fusai G, et al. Somatostatin analogues for pancreatic surgery. Cochrane Database Syst Rev. 2013;2013:Cd008370. doi: 10.1002/14651858.CD008370.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Straub JM, New J, Hamilton CD, et al. Radiation-induced fibrosis: mechanisms and implications for therapy. J Cancer Res Clin Oncol. 2015;141:1985–94. doi: 10.1007/s00432-015-1974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong TH, Choi J-I, Park MY, et al. Pancreatic hardness: Correlation of surgeon’s palpation, durometer measurement and preoperative magnetic resonance imaging features. World J Gastroenterol. 2017;23:2044–51. doi: 10.3748/wjg.v23.i11.2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marchegiani G, Ballarin R, Malleo G, et al. Quantitative Assessment of Pancreatic Texture Using a Durometer: A New Tool to Predict the Risk of Developing a Postoperative Fistula. World J Surg. 2017;41:2876–83. doi: 10.1007/s00268-017-4073-9. [DOI] [PubMed] [Google Scholar]
- 23.Belyaev O, Herden H, Meier JJ, et al. Assessment of pancreatic hardness-surgeon versus durometer. J Surg Res. 2010;158:53–60. doi: 10.1016/j.jss.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 24.Huang Y, de Boer WB, Adams LA, et al. Image analysis of liver collagen using sirius red is more accurate and correlates better with serum fibrosis markers than trichrome. Liver Int. 2013;33:1249–56. doi: 10.1111/liv.12184. [DOI] [PubMed] [Google Scholar]
- 25.Fijardo M, Kwan JYY, Bissey P-A, et al. The clinical manifestations and molecular pathogenesis of radiation fibrosis. EBioMedicine. 2024;103:105089. doi: 10.1016/j.ebiom.2024.105089. [DOI] [PMC free article] [PubMed] [Google Scholar]