Abstract
Background:
Nighttime aircraft noise may affect people’s sleep, yet large-scale evidence using objective and subjective measures remains limited.
Objective:
Our aim was to investigate associations between nighttime aircraft noise exposure and objectively measured sleep disturbance using a large UK cohort.
Methods:
We used data from 105,770 UK Biobank cohort participants exposed and unexposed to aircraft noise who lived in 44 local authority districts near 4 international airports in England. We used a generalized linear regression model to examine cross-sectional associations between aircraft noise (23:00 hours–07:00 hours) and 7-d actimetric measures collected 2013–2015 (). We also used Logit and generalized estimating equations models to examine associations between and self-reported sleep measures at enrollment (2006–2010) and follow-up (2012–2013). This approach allowed us to compare and contrast the results and support potential future meta-analyses on noise-related sleep disturbance.
Results:
Cross-sectional analyses of actimetric data suggested sleep disturbance associated with , showing higher level of movements during the least active continuous 8-h time period [: 0.12 milligravitational units; 95% confidence interval (CI): 0.013, 0.23]. We also saw disrupted sleep–wake cycles as indicated by index scores of lower relative amplitude (: ; 95% CI: , ), poorer interdaily stability (: ; 95% CI: , ), and greater intradaily variability (: 0.021; 95% CI: 0.019, 0.023), comparing dB with dB. Repeated cross-sectional analyses found a 52% higher odds of more frequent daytime dozing [odds ratio (OR) ; 95% CI: 1.32, 1.75] for dB in comparison with dB, whereas the likelihood for more frequent sleeplessness was more uncertain (; 95% CI: 0.92, 1.39). Higher effect sizes were seen in preidentified vulnerable groups, including individuals of age and those with diabetes or dementia.
Conclusion:
Individuals exposed to higher levels of aircraft noise experienced objectively higher levels of sleep disturbance and changes in sleep–wake cycle. https://doi.org/10.1289/EHP14156
Introduction
The World Health Organization (WHO) Environmental Noise Guidelines for the European Region published in 2018 recommended reducing the noise levels produced by aircraft during nighttime to below 40 dB [A-weighted equivalent noise level () over the 8-h night period of 23:00 hours–07:00 hours] because nighttime aircraft noise above this level is associated with adverse effects on sleep.1 In the United Kingdom alone, nearly 1 million people ( of the UK population) were affected by aircraft noise greater than 55 dB, according to the most recently published government noise action plan in 2017.2
Aircraft noise at night can disrupt sleep by evoking physiological signals in the auditory system, because the sleeping body continues to react to environmental stimuli.3 This disruption potentially results in shortened sleep, sleep awakenings, stage modifications, and autonomic responses.4 The 2018 WHO Environmental Noise Guidelines for the European Region used self-reported percentage of the population to be highly sleep-disturbed (%HSD) as the outcome for sleep disturbance.1 Highly sleep-disturbed people were typically those who chose scale points close to the top of the scale (worst sleep quality) on the sleep quality questionnaires.5,6 The guidelines synthesized the findings of three studies that used nonnoise specified questionnaires and identified a 17% [odds ratio (OR) ; 95% confidence interval (CI): 0.54, 2.53] higher odds of self-reported high sleep disturbance for every 10 dB increase in nighttime aircraft noise.7 Nonnoise-specified questionnaires refer to those in which participants were asked how often they had disturbed sleep, without specifically mentioning any cause of disturbance such as noise. An update to this review using the same nonnoise-specific questionnaire approach found the odds of experiencing sleep disturbance because of aircraft noise higher by 52% (; 95% CI: 1.20, 1.93; based on eight studies) per 10-dB increase in the average nighttime outdoor noise, based on eight studies.8
Sleep, being an unconscious process, means that self-reported sleep disturbance may be subject to recall bias.8 However, evidence from large-scale studies using more objective methods to evaluate sleep disturbances has been limited to date. Polysomnography (PSG), although considered the gold standard in sleep research,7 is relatively inconvenient and labor-intensive. The 2018 literature review for the WHO Environmental Noise Guidelines identified only four studies using PSG. One study, which was rated as moderate quality, found an association between aircraft noise and polysomnography-measured probability of additional awakenings, with an OR of 1.35 (95% CI: 1.22, 1.50) per 10 dB increase in indoor LAS, max.7,9 However, it was not possible to estimate a pooled effect due to design variability and small sample sizes.7 Actimetry, a less inconvenient and labor-intensive but still relatively objective method involving wrist-worn devices to track sleep–wake cycles, has been widely used and validated.10 Most published studies using actimetric measures have relatively small sample sizes. In a study in Switzerland, 105 subjects with actimetric data were included,11 and in France, 112 participants with actimetric data were involved.12 There has still been very limited large-scale evidence on aircraft noise and sleep studies using actimetric measures, which was an important motivation for this study.
The objective of our study was to investigate the association between nighttime aircraft noise exposure and actigraphy-generated sleep disturbance outcomes. We also included self-reported sleep outcomes, as the inclusion of both objective and subjective measures to study the association between aircraft noise and sleep disturbance in the same cohort may help better understand the strengths and limitations of actimetric measures and support potential future meta-analyses on noise-related sleep disturbance. We focused on a subset of individuals living near four major airports, obtained from the UK Biobank, a large, broadly population-based, biomedical cohort study database. Our study serves both a hypothesis-testing study to examine the association between nighttime aircraft noise exposure and sleep disturbance as well as a hypothesis-generating one to explore potential actimetric outcomes that could act as proxies for sleep disturbance in noise studies.
Methods
Study Population
Our study analyzed data from participants in the UK Biobank cohort study, which has collected comprehensive health, lifestyle, and genetic information from 502,413 volunteer participants 40–69 y of age at recruitment between 2006 and 2010. A subset of 105,770 participants from UK Biobank were included in our study, all of whom resided in one of the 44 Local Authority Districts (LADs; as per the boundary May 2020), wholly or partially encompassed within Civil Aviation Authority (CAA) (Day–evening–night noise level) noise contours of four major international airports [London Heathrow (LHR), London Gatwick (LGW), Birmingham (BHX), and Manchester (MAN)] in England. The participants who lived inside the noise contours within the 44 LADs are in the exposed group, whereas those living outside contour but still within the 44 LADs are comparators. The CAA and noise contours and 44 Local Authority Districts are presented in Figure 1.
Figure 1.
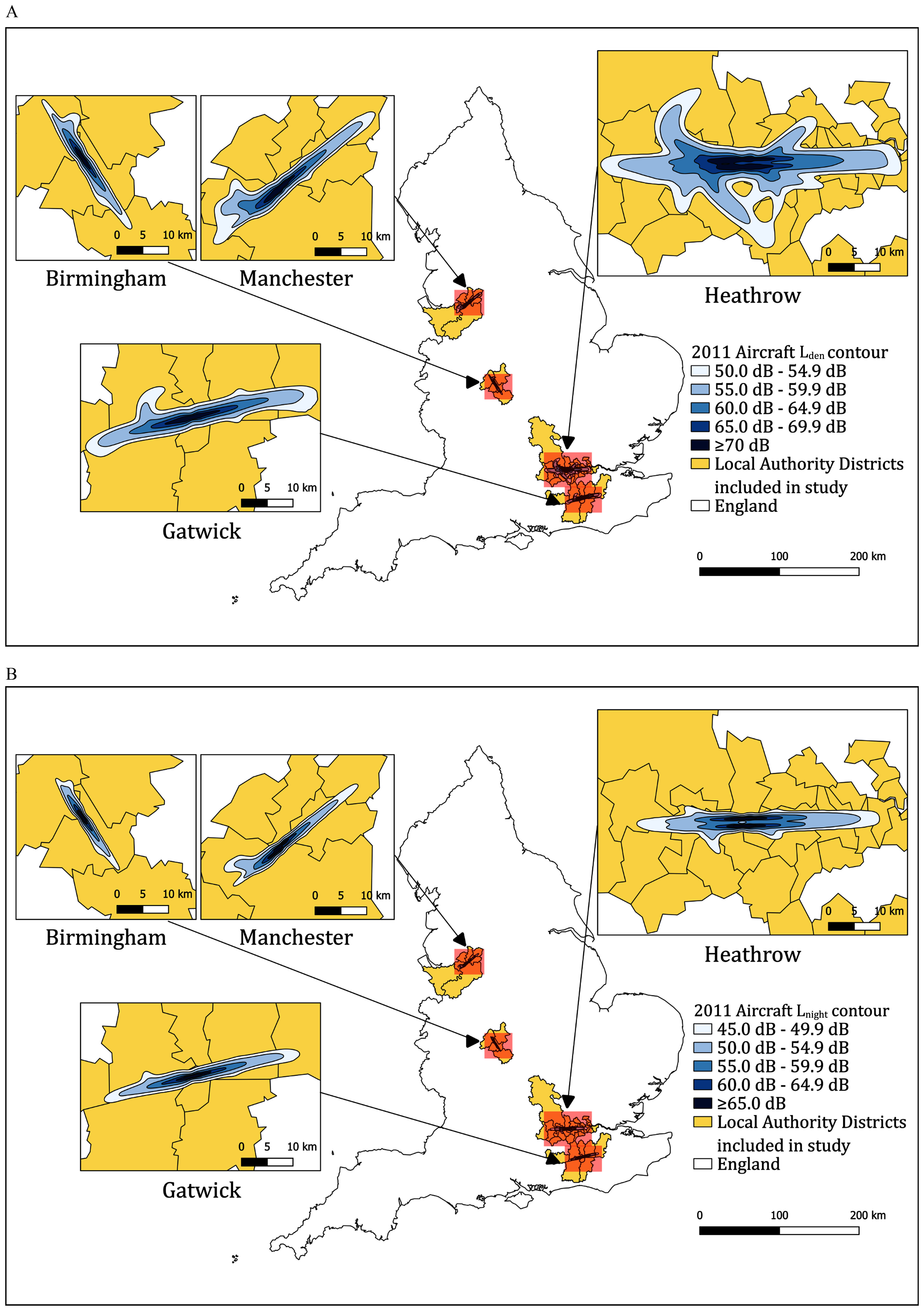
Maps of England showing Civil Aviation Authority noise contours for the four airports and the 44 local authorities included in the study. (A) noise contour. (B) noise contour. Note: represents the day–evening–night noise level, and refers to the A-weighted equivalent noise level () measured in decibels (dB) over the 8-h night period from 23:00 hours to 07:00 hours. The Local Authority District shapefile was obtained as open-source data from https://geoportal.statistics.gov.uk/. The package used to create Figures 1A and 1B was QGIS.
UK Biobank has conducted baseline and multiple follow-up assessment visits. The baseline assessment (instance 0; 2006–2010) includes extensive data collected at the time of recruitment, such as information on demographics, lifestyle factors, medical history, physical measurements, and biological samples, etc. The first follow-up visit (instance 1) was conducted in the period 2012–2013. During that period, a total of 103,514 participants were invited to participate, and of those, 20,345 participants attended further assessments.13 For our study, we used instance 0 (2006–2010) and follow-up instance 1 (2012–2013) data.
UK Biobank has ethical approval to function as a Research Tissue Bank (RTB) from the North West Multi-Centre Research Ethics Committee (MREC) under the current REC approval number (2021, 5-y cycle): 21/NW/0157. Approval for this specific research project application was covered by UK Biobank project approval number 59129. Under RTB approval, our study does not require separate ethical clearance.14
Outcomes
Because sleep disturbance has multiple aspects, we adopted an approach using multiple actimetric measures, some of which are novel. We additionally used self-reported measures to compare and contrast their results with those obtained from objective measures and to aid future meta-analyses that rely on self-reported data. Table S1 provides detailed definitions, data descriptions, and interpretations for each actimetric outcome, along with the questions, response options, and categorizations for each self-reported outcome.
Actimetric measures.
Our actimetric measures include accelerometer derived average movements during the least active periods, time spent on sleep or in bed, and a relatively overlooked sleep aspect: the sleep–wake cycle.
A total of 236,519 participants from the UK Biobank were invited to measure their physical activity using the Axivity AX3 wrist-worn triaxial accelerometer between 1 June 2013 and 23 December 2015.15 Of those invited, 106,053 participants agreed to wear the monitor, resulting in a response rate of 44.8%.15 Among the participants who wore the monitor, 103,712 had complete actimetric data, with a median wear-time of 6.9 d (interquartile range: 6.5–7.0 d). For each participant, accelerometer data (5-s epoch time series) were extracted from UK Biobank15 and converted to R-format for processing and analysis with GGIR (version 1.11-0; http://cran.r-project.org).16 Participants were excluded if they failed calibration, had fewer than 3 d of valid wear (defined as per day), or wear-data were not present for each 15 min period of the 24-h cycle. Valid physical activity data [valid days, ()] were obtained from 96,600 participants (93.3%),15 of whom 22,101 (for the proportion of time spent on sleep or in bed within 7 d) and 22,102 (for other actimetric measures) participants were living in any of the 44 LADs included in this study. These valid physical activity data were then previously processed to derive outcomes used in this study.
The first outcome is average acceleration during the least active 8-h period, measured in milligravitational units (mg), which provides an indication of overall activity during the rest period.17 This outcome may be used as a proxy for participant movement or arousal during their least active rest windows of time.18,19 The 8-h period (average from 23:06 to 07:06 in our data) was chosen because it aligns well with the 8-h window (23:00 hours to 07:00 hours) used in the noise exposure metric we used in our study.
We used the overall average proportion of time spent on sleep or in bed (defined as nonwaking time20) during the monitoring 7 d, which was previously derived using a published machine-learning methodology.20 We name this outcome as time spent on sleep or in bed to aid interpretation.
We also looked at three previously derived outcomes related to a participant’s sleep–wake cycle: relative amplitude (RA), intradaily variability (IV), and interdaily stability (IS).21 RA measures the contrast in activity levels between the most active 10 h and the least active 5 h within a 24-h period. IV measures the fragmentation of the 24-h rest–activity rhythm, whereas IS measures the stability of the rest–activity rhythm.
All actimetric outcomes were measured at one time point (in 2013–2015). Baseline UK Biobank covariate data were used in the models of actimetric measures for the 22,102 participants.
Self-reported measures.
The first self-reported outcome was related to sleeplessness/insomnia and was obtained through responses to the question, “Do you have trouble falling asleep at night or do you wake up in the middle of the night?” The second outcome was daytime dozing/sleeping, which we obtained through responses to the question “How likely are you to doze off or fall asleep during the daytime when you don’t mean to? (e.g., when working, reading or driving)?” Last, we extracted sleep duration as the final self-reported outcome, which was obtained through responses to the question, “About how many hours sleep do you get in every 24 h? (please include naps).” These questions were measured at baseline (instance 0) and had a repeated measurement (instance 1). Any responses indicating “prefer not to say” or “do not know” were treated as missing data and excluded from the regression.
To facilitate analysis, interpretation, and to ensure comparability with other studies on the same topic, we grouped responses for self-reported sleeplessness and daytime dozing. Both questions have verbal answers with various frequencies. For example, sleeplessness has response options: “never/rarely,” “sometimes,” and “usually,” whereas response options for daytime dozing include “never/rarely,” “sometimes,” “often,” and “all of the time.” We selected the two responses indicating the highest frequency for each question; i.e., “sometimes” and “usually” were chosen as the exposure group for sleeplessness, whereas “often” and “all of the time” were selected to represent the exposure group for daytime dozing.
Aircraft Noise Exposure
The Civil Aviation Authority (CAA) provided aircraft noise surfaces (measured in and ) for four airports—LHR, LGW, BHX, and MAN—for 2006 and for 2011. The noise contours are shown in Figure 1. These contours were modeled using ANCON version 2, taking into account variables such as height, speed profile, takeoff/landing weights, and aircraft performance data.22 Noise levels modeled by using the ANCON model have shown significant similarities with US Federal Aviation Administration’s Integrated Noise Model (INM) and have been validated by comparing sound exposure level noise calculations at grid points with noise measurements made at equivalent distances from the airport.23 For instance, the largest variation from predicted levels, when compared with measured levels for a Boeing 747-400, was just over 2 dB.23
Our study focused on nighttime noise, using the metric, which is the A-weighted equivalent noise level () over the 8-h night period of 23:00 hours–07:00 hours. The CAA provided data truncated to a lower level of 45 dB; levels below this specific noise exposure level are not provided.
We determined each participant’s residential noise levels by overlaying postcode centroid points onto the CAA’s noise contours. We divided the nighttime aircraft noise exposure of the participants into four categories based on a 5-dB increment: dB, dB, dB, and dB. The 5-dB difference was chosen because a minimal 3–5 dB difference may be needed for people to detect a change in noise level.24 Approximately 5% of people in the sample were exposed to noise above 50 dB.
Covariates
The covariates used were selected based on a directed acyclic graph (DAG), as depicted in Figure S1. The DAG graph was plotted based on reviews of the mechanisms of the health impacts of noise exposure1,25 and other related studies.12,26,27
The demographic variables in this study consist of sex (male or female), age in 2006 (the time point of the first nighttime aircraft noise exposure measurement) and 2011 (the time point of the second nighttime aircraft noise exposure measurement), as well as body mass index (BMI) (continuous). We controlled for self-reported ethnicity (White, Mixed, Asian or Asian British, Black or Black British, Chinese or others). Ethnicity may be associated with important aspects of disadvantage, including employment and earnings disparities,28 as well as experiences of racism and discrimination in the United Kingdom.29 The categories of ethnicity used in our study followed those of the UK Biobank dataset.30
The Hedonic price model suggests an inverse association between noise exposure and house prices,31–33 implying a link between aircraft noise exposure and deprivation. We therefore controlled for socioeconomic factors. These include self-reported average yearly household income before tax (, £18,000–£30,999, £31,000–51,999, £52,000–£100,000, or ), and calculated Townsend deprivation index (continuous) at the output area (a small census area) in which participants’ postcode was located at recruitment. Townsend index is an area-based score of social deprivation (accounting for unemployment, overcrowding, noncar ownership, and nonhome ownership).34
Self-reported mental health or lifestyle factors include “ever seen a psychiatrist or doctor (GP) for nerves, anxiety, tension, or depression” (yes or no), smoking status (never, previous or current), and alcohol consumption (daily or almost daily, 3–4 times a week, 1–2 times a week, 1–3 times a month, special occasions only or never). We also incorporated the total number of vigorous or moderate physical activities (in days) reported by each participant per week. In cases where a participant engaged in both vigorous and moderate activities on a single day, we counted that day as 1.
Environmental covariates included modeled nighttime road traffic noise ( dB, dB, dB, and dB), nighttime rail traffic noise ( dB, dB, dB, and dB), average annual nitrogen dioxide () concentration(continuous), average annual particulate matter with aerodynamic diameter () concentration (continuous) and greenspace percentage within a buffer of (continuous). Nighttime road noise at participants’ home postcodes was calculated using the CNOSSOS-EU framework using 2013 data such as traffic counts, speeds, surface roughness, building heights, wind profiles, and temperatures.35,36 Rail noise levels were extracted from 2011 noise maps created by Extrium on behalf of the Department for Environment, Food and Rural Affairs (DEFRA).37 concentrations for 2009 were modeled using UK-specific Land Use Regression (LUR) model.38 concentrations were modeled using LUR for the European Study of Cohorts for Air Pollution Effects (ESCAPE).39 We used the percentage of greenspace within a radius of each participant calculated by Wheeler et al.40
We additionally used the number of years a participant had lived at current address (continuous).
Field IDs or return IDs of all variables used in our study and their description can be found in Table S2.
Statistical Analysis
Descriptive statistics were used to provide a summary of the sleep outcomes, environmental variables, and covariates.
For actimetric data that only had one measurement, we used a cross-sectional design with baseline instance and 2011 aircraft noise data. We employed generalized linear regression models with a gamma distribution and identity link to investigate the association of noise exposure with actimetric sleep measures, accounting for all covariates. A gamma distribution was chosen due to its suitability for modeling positive values, whereas the identity link function was used so that the coefficient can be interpreted as the incremental change in the outcome per noise category in comparison with the reference group ( dB).
We employed a repeated cross-sectional design to examine the association between nighttime aircraft noise and self-reported sleep outcomes using instance 0 (2006–2010) and instance 1 (2012–2013). We used 2006 aircraft noise levels with UK Biobank instance 0 and 2011 noise levels with instance 1. We used a random-effects logit model, adjusting for all covariates, to analyze the association between nighttime aircraft noise and self-reported sleeplessness and daytime dozing, considering both sleeplessness and daytime dozing are binary. We employed a generalized estimating equations (GEE) model with random effects, adjusting for all covariates, to examine the association between nighttime aircraft noise and self-reported sleep duration. Some covariates like sex, ethnicity, household income, and some environmental variables (road noise levels, rail noise levels, , , and greenspace proportion) were only available at baseline and thus baseline covariate values were used for the follow-up instance.
To account for potential differences in the noise characters across four airports, we clustered variance by four airports (LHR, LGW, BHX, and MAN), except for self-reported sleep duration as the GEE model did not support cluster robust variance.
To check the robustness of our findings, we conducted multiple sensitivity analyses. We performed regression analyses while excluding subgroups of participants susceptible to misclassification with noise exposure levels. For each sensitivity analysis, we excluded one subgroup at a time. These include participants with hearing difficulty, those who have moved homes since recruitment, and those who engaged in night-shift work.
To examine for interactions, we stratified our data based on various sociodemographic factors, including sex (male or female), ethnicity (White or non-White), age (), and low and high household income groups. The national median was between £29,073 and £32,000 between 2006 and 2022.41 We thus defined incomes and £18,000–£30,999 as the low household income group and categorized the remaining income levels as the high household income group. Some home/family caregivers had considerable caregiving burden,42 leading to experiences of stress,42 distress,43 depressive symptoms,44 and/or sleep disturbances.45 We stratified our data based on participants’ involvement in home/family caregiving.
The relationship between sleep and health conditions is complex. Poor sleep can be associated with higher blood pressure,46 mental health,47 as well as neurological conditions.48 There is a bidirectional relationship between sleep and diabetes. Poor sleep can be linked to a higher risk of developing type 2 diabetes,49 whereas diabetes can also negatively impact sleep quality through symptoms such as nocturia and restless legs syndrome.50 We therefore examined associations in participants with certain health conditions known to be linked to sleep problems: diabetes (self-reported doctor-diagnosed at baseline), hypertension (based on self-reported doctor-diagnosed cases at baseline, self-reported use of medication to treat hypertension at baseline, or recorded blood pressure readings showing systolic blood pressure or diastolic blood pressure at baseline), high BMI (greater than median 26.64 or less than median, measured at baseline), dementia (diagnosis up to 2020 using multiple ascertainment sources), mental health issues [defined as having seen a psychiatrist or doctor (GP) for nerves, anxiety, tension, or depression at baseline], and sleep disorder (self-reported, primary care–diagnosed or hospital diagnosed up to 2023).
We employed a complete case approach to analyze the data. Any observations with missing values in any of the variables included in the regression analysis were excluded.
All statistical analyses were conducted using Stata software (version 18; STATA Corp.), and the significance level was set at .
Results
Descriptive Summary
The descriptive summary of sleep outcomes, socio-economic variables, environmental variables, mediators and moderators can be found in Table 1. We had a total of 105,770 participants, with 57,381 (54.3%) identifying as female. Ethnicity information was available for 104,739 individuals, with 91,251 (86.3%) identifying as White, 5,194 (4.9%) as Asian, and 4,386 (4.1%) as Black. Participants were recruited at ages 40–70 y when attending the baseline assessment. In 2006 the mean age of participants stood at 53.7 y [standard deviation ], spanning an age range from 35 to 72 y of age.
Table 1.
Descriptive summary of UK Biobank data sleep variables, socioeconomic variables, and environmental variables used in study of airport noise and sleep [for continuous variables: (min-max) (, % of ), or for categorical variables: (% of )].
| Variable name | Baseline (instance 0: 2006–2010) |
First follow-up (instance 1: 2012–2013) |
|---|---|---|
| Sleep variables | ||
| Average acceleration over least-active continuous 8 h (mg) (Baseline , 20.9%) |
(1.6–39.2) | — |
| Proportion of time spent on sleep or in bed (7-d average) (Baseline , 20.9%) |
(0.02–0.73) | — |
| Relative amplitude (unitless) (Baseline , 20.9%) |
(0.28–0.97) | — |
| Intra-daily variability (unitless) (Baseline , 20.9%) |
(0.22–2.04) | — |
| Interdaily stability (unitless) (Baseline , 20.9%) |
(0.04–0.98) | — |
| Sleep duration [decimal time (24-h clock)] (Baseline , 20.9%; first follow-up , 100%) |
07 h::06 (1 h–23 h) | 07 h::06 (1 h–16 h) |
| Sleeplessness/insomnia | ||
| Never or rarely | 27,308 (25.8%) | 1,403 (22.8%) |
| Sometimes or usually | 77,806 (73.6%) | 4,737 (77.1%) |
| Missing | 656 (0.6%) | 3 (0.0%) |
| Self-reported daytime dozing | ||
| Never, rarely or sometimes | 101,179 (95.7%) | 5,984 (97.4%) |
| Often or all of the time | 3,213 (3.0%) | 145 (2.4%) |
| Missing | 1,378 (1.3%) | 14 (0.2%) |
| Social demographic variables | ||
| Sex | ||
| Female | 57,381 (54.3%) | 3,286 (53.5%) |
| Male | 48,387 (45.7%) | 2,857 (46.5%) |
| Missing | 2 (0.0%) | 0 (0.0%) |
| Ethnicity | ||
| White | 91,251 (86.3%) | 5,929 (96.5%) |
| Mixed | 1,120 (1.1%) | 34 (0.6%) |
| Asian or Asian British | 5,194 (4.9%) | 56 (0.9%) |
| Black or Black British | 4,386 (4.1%) | 49 (0.8%) |
| Chinese | 612 (0.6%) | 22 (0.4%) |
| Other | 2,176 (2.1%) | 34 (0.6%) |
| Missing | 1,031 (1.0%) | 19 (0.3%) |
| Average household income before tax | ||
| 17,083 (16.2%) | 1,076 (17.5%) | |
| £18,000–£30,999 | 19,213 (18.2%) | 1,638 (26.7%) |
| £31,000–£51,999 | 21,678 (20.5%) | 1,497 (24.4%) |
| £52,000–£100,000 | 20,328 (19.2%) | 1,042 (17.0%) |
| 7,941 (7.5%) | 307 (5.0%) | |
| Missing | 19,527 (18.5%) | 583 (9.5%) |
| Age in 2006 (baseline) and 2011 (first follow-up) (y) | (35.0–72.0) | (44.0–78.0) |
| Townsend deprivation index at recruitment (Baseline , 99.9%; first follow-up , 99.9%) |
(–10.2) | (–9.2) |
| Environmental variables | ||
| Nighttime aircraft noise 2006 (dB) | ||
| 92,367 (87.3%) | — | |
| 7,829 (7.4%) | — | |
| 3,841 (3.6%) | — | |
| 1,733 (1.6%) | — | |
| Nighttime aircraft noise 2011 (dB) | ||
| 93,492 (88.4%) | 5,904 (96.1%) | |
| 7,383 (7.0%) | 190 (3.1%) | |
| 3,491 (3.3%) | 39 (0.6%) | |
| 1,404 (1.3%) | 10 (0.2%) | |
| Nighttime road traffic noise (dB) | ||
| 44,474 (42.1%) | 2,889 (47.0%) | |
| 38,046 (36.0%) | 2,172 (35.4%) | |
| 13,434 (12.7%) | 669 (10.9%) | |
| 9,809 (9.3%) | 413 (6.7%) | |
| Missing | 5 (0.0%) | 0 (0.0%) |
| Nighttime rail traffic noise (dB) | ||
| 102,627 (97.0%) | 6,020 (98.0%) | |
| 1,672 (1.6%) | 54 (0.9%) | |
| 882 (0.8%) | 48 (0.8%) | |
| 589 (0.6%) | 21 (0.3%) | |
| Average annual concentration () (Baseline , 98.6%; first follow-up , 99.7%) |
(8.2–20.7) | (8.2–18.9) |
| Average annual concentration () | (4.5–79.2) | (5.3–61.8) |
| Greenspace percentage, buffer (%) (Baseline , 99.1%; first follow-up , 99.4%) |
(4.4–98.1) | (8.0–98.1) |
| Covariates | ||
| Ever seen a psychiatrist or doctor (GP) for nerves, anxiety, tension or depression | ||
| No | 69,598 (65.8%) | 4,057 (66.0%) |
| Yes | 34,223 (32.4%) | 2,042 (33.2%) |
| Missing | 1,949 (1.8%) | 44 (0.7%) |
| Smoking | ||
| Never | 56,981 (53.9%) | 3,616 (58.9%) |
| Previous | 35,914 (34.0%) | 2,189 (35.6%) |
| Current | 11,917 (11.3%) | 324 (5.3%) |
| Missing | 958 (0.9%) | 14 (0.2%) |
| Alcohol consumption | ||
| Daily or almost daily | 23,671 (22.4%) | 1,185 (19.3%) |
| 3 or 4 times a week | 22,887 (21.6%) | 1,594 (25.9%) |
| Once or twice a week | 23,862 (22.6%) | 1,566 (25.5%) |
| 1–3 times a month | 11,164 (10.6%) | 676 (11.0%) |
| Special occasions only | 13,104 (12.4%) | 682 (11.1%) |
| Never | 10,437 (9.9%) | 439 (7.1%) |
| Missing | 645 (0.6%) | 1 (0.0%) |
| Vigorous or moderate physical activity per week (in days, range) (Baseline ; 97.1%; first follow-up ; 99.0%) |
(0.0–7.0) | (0.0–7.0) |
| Time at current address (years) (Baseline ; 96.5%; first follow-up ; 98.4%) |
(1.0–70.0) | (1.0–79.0) |
| Body mass index () (Baseline ; 99.0%; first follow-up ; 99.7%) |
(12.6–68.1) | (14.9–58.9) |
| Moderators or mediators | ||
| Presence of hearing difficulties | ||
| No | 73,468 (69.5%) | 3,899 (63.5%) |
| Having hearing difficulties or completely deaf | 23,524 (22.2%) | 1,916 (31.2%) |
| Missing | 54 (0.1%) | 4 (0.1%) |
| Nightshift work | ||
| Sometimes, usually or always | 5,393 (5.1%) | 163 (2.7%) |
| Never/rarely, do not know, prefer not to answer, did not answer or | 100,377 (94.9%) | 5,980 (97.3%) |
| Never moved since recruitment | ||
| Yes | 76,883 (72.7%) | 4,660 (75.9%) |
| No | 28,880 (27.3%) | 1,483 (24.1%) |
| Missing | 7 (0.0%) | 0 (0.0%) |
| Looking after home/familya | ||
| Yes | 6,025 (5.7%) | 234 (3.8%) |
| No or missing | 99,745 (94.3%) | 5,909 (96.2%) |
| Diabetesb | ||
| Yes | 6,278 (5.9%) | 394 (6.4%) |
| No | 98,492 (93.1%) | 5,742 (93.5%) |
| Missing | 1,000 (0.9%) | 7 (0.1%) |
| Hypertensionc | ||
| Yes | 53,690 (50.8%) | 3,562 (58.0%) |
| No | 51,949 (49.1%) | 2,581 (42.0%) |
| Missing | 131 (0.1%) | 0 (0.0%) |
| Dementiad | ||
| Yes | 1,605 (1.5%) | 91 (1.5%) |
| No or missing | 104,165 (98.5%) | 6,052 (98.5%) |
| Sleep disordere | ||
| Yes | 4,028 (3.8%) | 129 (2.1%) |
| No or missing | 101,742 (96.2%) | 6,014 (97.9%) |
Note: This table displays (min-max) [, % of ] for continuous variables, or (% of ) for categorical variables. All actimetric outcomes were measured at one time point (2013–2015) and are presented in the baseline column, as they were linked to the baseline UK Biobank assessments. Aircraft noise levels for 2006 are also in the baseline column because they were only used with baseline data. Aircraft noise levels for 2011 are included in both baseline and first follow-up columns, because they were used with baseline for actimetric measures and with first follow-up for self-reported measures. —, no data; dB, decibel; , nitrogen dioxide; , fine particulate matter with aerodynamic diameter ; SD, standard deviation.
Looking after home/family is a labor market status. It means the participant who were neither employed nor unemployed due to home/family responsibilities.
Diabetes was self-reported at baseline based on doctor diagnosis.
Hypertension was based on self-reported doctor-diagnosed cases at baseline, self-reported use of medication to treat hypertension at baseline, or recorded blood pressure readings showing systolic blood pressure or diastolic blood pressure at baseline.
Dementia was identified using multiple ascertainment sources from baseline through 2020.
Sleep disorders were based on self-report, primary care diagnosis or hospital diagnosis up to 2023.
Descriptive analysis of sleep variables.
We present a Venn diagram to show the number of participants who lived near the four airports and had valid responses to the outcomes included in our study in Figure 2. Among the 105,770 participants, 22,101 had actimetric-generated average proportions of time spent on sleep or in bed (7-d average; defined as nonwaking behavior20) using the variable ID 40046 in the UK Biobank. Actimetry identified that they spent an average of 36% ( of their time on sleep or in bed. This is equivalent to 8 h and 38 min per day on average. A few individuals had actimetric data that passed the quality control as outlined in a previous paper20 but had either a very low or very high number of hours spent sleeping or in bed according to the algorithm. These include a total of 3, 5, 6, and 17 participants who had less than a 2-h, 2–3-h, 3–4-h, or 4–5-h period asleep or in bed, respectively. In addition, one participant spent more than 18 h sleeping or in bed.
Figure 2.
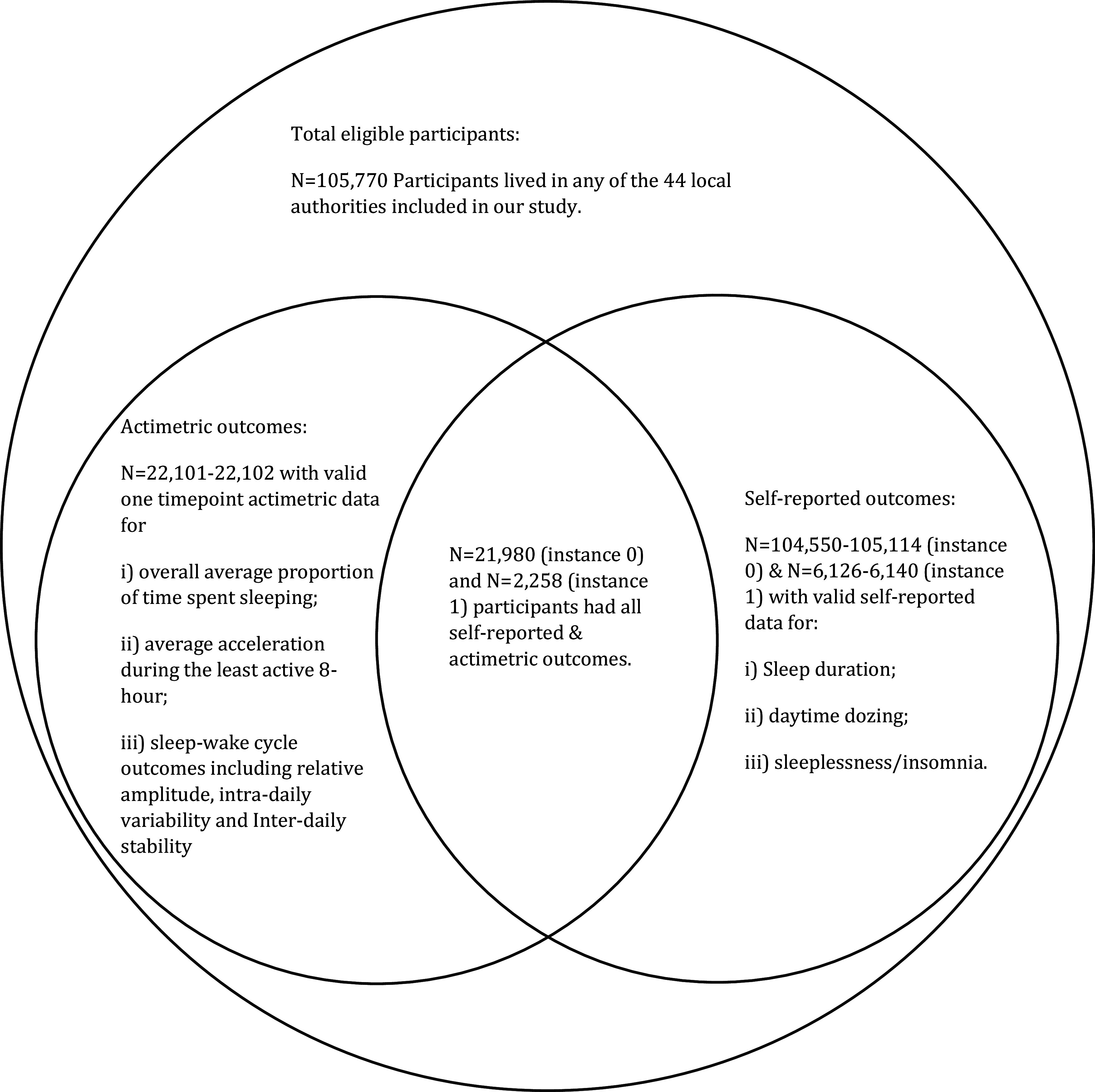
Venn diagram depicting the number of UK Biobank participants with valid values for each outcome.
A total of 22,102 participants had actimetric variables relating to average acceleration during the least active 8-h period and sleep-wake cycle. The average acceleration was (). The mean relative amplitude, intradaily variability and interdaily stability were 0.88 (), 0.66 (), and 0.66 (), respectively.
When looking at self-reported data, respondents reported an average of 7 h and 6 min (; h and 6 min) of sleep per day in the baseline survey and 7 h and 12 min (; h and 6 min) in the follow-up survey. A total of 73.6% () in instance 0 and 77.1% () in instance 1 reported that they “sometimes” or “usually” experienced sleeplessness. However, most respondents in both instances indicated that they “never/rarely” or “sometimes” experienced daytime dozing [95.7% () in instance 0 and 97.4% () in instance 1]. Almost identical results on self-reported sleeplessness, daytime dozing, and sleep duration were seen when restricted to the of the participants in our sample with actimetric data.
Descriptive analysis of aircraft noise variables.
Nighttime aircraft noise data () for all four airports considered were available for 2006 and 2011. In 2006, 7,829 (7.4%), 3,841 (3.6%), and 1,733 (1.6%) participants experienced levels of dB, dB, and dB, respectively. By 2011, these numbers had slightly decreased to 7,383 (7.0%), 3,491 (3.3%), and 1,404 (1.3%), respectively.
Nighttime road noise levels were available for 2013 for 105,763 participants: 44,474 (42.1%) experienced nighttime road noise levels dB; 38,046 (36.0%) at dB; 13,434 (12.7%) at dB; and 9,809 (9.3%) at dB, respectively. For railway noise (available for 2011), 102,627 (97.0%) participants were exposed to levels dB. A total of 1,672 (1.6%), 882 (0.8%), and 589 (0.6%) participants experienced noise levels of dB, dB, and dB, respectively.
Analytic Results
Actimetric measured outcomes.
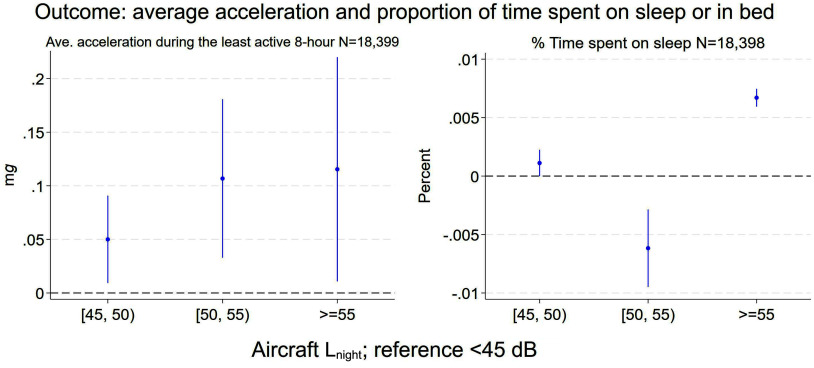
The final number of participants involved in regressions using actimetric outcomes was 18,398–18,399. The loss of participants is due to missing covariates. Figure 3 (Table S4) shows that individuals exposed to dB exhibited (95% CI: 0.013, 0.23) higher average acceleration during the least active 8-h period than those exposed to dB. A similar pattern of association was seen when looking at dB to dB or dB to dB. These overall findings present a gradient, indicating that risks rose with increasing noise level.
Figure 3.
Cross-sectional association between nighttime aircraft noise and actimetry data on average acceleration, measured in milligravitational units (mg) during the least active 8 h, and percentage of time spent on sleep or in bed using UK Biobank cohort (–18,399). Note: The figures display the point estimate (), and 95% CIs. represents the increment in the absolute value of the outcome when exposed to higher aircraft noise categories, in comparison with those exposed to dB. refers to the A-weighted equivalent noise level () measured in decibels (dB) over the 8-h night period from 23:00 hours to 07:00 hours. All models have been adjusted for sex; ethnicity; age in 2006; BMI; ever seen a psychiatrist or doctor (GP) for nerves, anxiety, tension, or depression; smoking status; alcohol consumption; total number of vigorous or moderate physical activities (in days) a participant typically reported doing in a week; average yearly household income before tax; Townsend deprivation index at recruitment by place of residence; nighttime road traffic noise; nighttime rail traffic noise; concentration; concentration; and greenspace percentage within a buffer of . The numeric results can be found in Excel Tables S1 and S2. BMI, body mass index; CI, confidence interval; GP, general practitioner.
From actimetry data, individuals exposed to noise levels dB spent (95% CI: 0.6%, 0.7%) more time on average on sleep or in bed, equivalent to min per day in comparison with those exposed to dB (Table S5). Conversely, for those exposed to noise levels dB to dB, there was an approximate 0.6% lower () in average sleep or bed time (95% CI: , ).
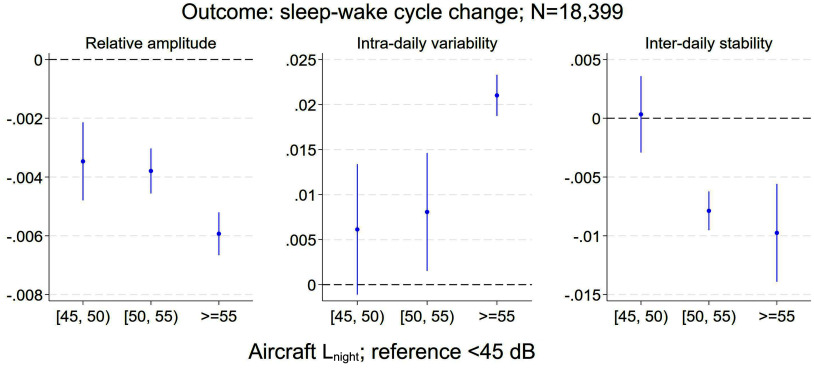
Figure 4 presents sleep–wake cycle results. Gradients with increasing noise levels were seen for all three sleep–wake cycle outcomes. For relative amplitude (Table S6), when compared with participants exposed to dB, higher was associated with a lower RA by (95% CI: , ; dB to dB), (95% CI: , ; dB to dB), and (95% CI: , ; dB), respectively, where negative values indicate higher levels of activity during sleep and/or lower activity during the day.
Figure 4.
Cross-sectional association between nighttime aircraft noise and sleep–wake cycle using UK Biobank cohort (). Note: Sleep–wake cycle outcomes including RA, IV, and IS, all unitless. A higher RA value indicates greater activity during the day and reduced activity during sleep. A high IV suggests a more fragmented rhythm indicative of circadian dysfunction. A higher IS score indicates a strong alignment with light and other environmental cues that regulate the biological clock. The figures display the point estimate () and 95% CIs. represents the increment in the absolute value of the outcome when exposed to higher aircraft noise categories, in comparison with those exposed to dB. refers to the A-weighted equivalent noise level () measured in decibels (dB) over the 8-h night period from 23:00 hours to 07:00 hours. All models have been adjusted for sex; ethnicity; age in 2006; BMI; ever seen a psychiatrist or doctor (GP) for nerves, anxiety, tension, or depression; smoking status; alcohol consumption; total number of vigorous or moderate physical activities (in days) a participant typically reported doing in a week; average yearly household income before tax; Townsend deprivation index at the time of recruitment from the national census output areas associated with the participant’s place of residence; nighttime road traffic noise; nighttime rail traffic noise; concentration; concentration; and greenspace percentage within a buffer of . The numeric results can be found in Excel Tables S3, S4, and S5. BMI, body mass index; CI, confidence interval; GP, general practitioner; IS, interdaily stability; IV, intradaily variability; RA, relative amplitude.
Moreover, intradaily variability (IV) measures were higher by 0.006 (95% CI: , 0.013; dB to dB), 0.008 (95% CI: 0.002, 0.015; dB to dB), and 0.021 (95% CI: 0.019, 0.023; dB), respectively, where positive values indicate a more fragmented sleep–wake rhythm indicative of circadian dysfunction (Table S7).
Interdaily stability (Table S8) had a lower level by (95% CI: , ; dB to dB), and (95% CI: ; dB), respectively, where negative values indicate weaker alignment with light and other environmental cues that regulate the biological clock.
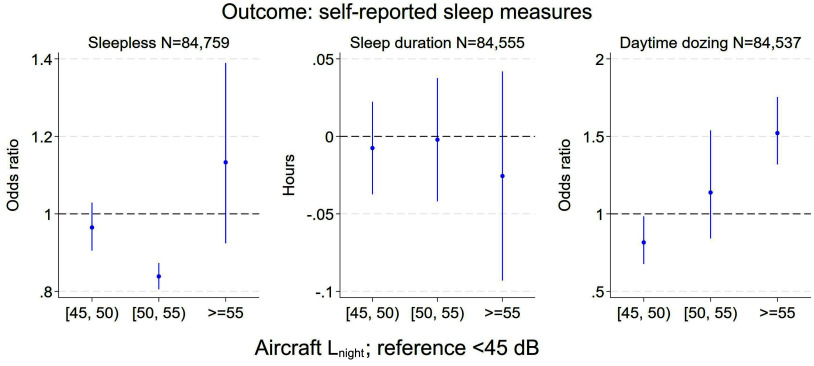
Self-reported outcomes.
A total of 84,537 to 84,759 participants had full observations and were involved in regressions using self-reported outcomes. Results from repeated cross-sectional analysis (Figure 5; Table S9) shows among participants exposed to noise levels of 55 dB or higher nighttime aircraft noise, there was a 13% higher likelihood of reporting sleeplessness sometimes or usually (; 95% CI: 0.92, 1.39) in comparison with individuals exposed to noise levels below 45 dB, albeit with wide confidence intervals. When looking at daytime dozing reported by of the study population (Table 1; Table S10), those exposed to noise levels of 55 dB or higher had an higher likelihood (; 95% CI: 1.32, 1.75). No association was found between nighttime noise and self-reported sleep duration (Table S11) due to large uncertainty.
Figure 5.
Repeated cross-sectional association between nighttime aircraft noise and self-reported sleep outcomes using UK Biobank cohort (–84,759). Note: The figures “Sleepless” (left) and “Daytime Dozing” (right) illustrate the ORs and 95% CIs, whereas the “Sleep Duration” (middle) figure presents the point estimate () and 95% CIs. The OR represents the likelihood of someone reporting more severe sleep disturbance outcomes when exposed to noise levels dB in comparison with those exposed to dB; represents the increment in the absolute value of the outcome when exposed to higher aircraft noise categories, in comparison with those exposed to dB. refers to the A-weighted equivalent noise level () measured in decibels (dB) over the 8-h night period from 23:00 hours to 07:00 hours. All models have been adjusted for sex; ethnicity; age in 2006 and 2011; BMI; ever seen a psychiatrist or doctor (GP) for nerves, anxiety, tension, or depression; smoking status; alcohol consumption; total number of vigorous or moderate physical activities (in days) a participant typically reported doing in a week; average yearly household income before tax; Townsend deprivation index at the time of recruitment from the national census output areas associated with the participant’s place of residence; nighttime road traffic noise; nighttime rail traffic noise; concentration; concentration; and greenspace percentage within a buffer of . The numeric results can be found in Excel Tables S6, S7, and S8. BMI, body mass index; CI, confidence interval; GP, general practitioner; OR, odds ratio.
Sensitivity analysis.
We performed analyses on subsets of the sample that excluded individuals prone to noise misclassification. The results are presented in Figures S2–S9 (Table S4–S11), with each graph including the previously presented results from the full sample as a reference. The findings from these sensitivity analyses remain consistent with the main results, suggesting our conclusions are robust to different types of potential exposure misclassification.
In subset analyses considering demographic and sociodemographic factors that might influence susceptibility to sleep disturbances, the results are presented in Figures S10–S17 (Table S4–S11). Most subgroups showed broadly similar patterns of associations with actimetric data as those in main results, but with varying coefficient sizes and less clear patterns, likely related to smaller sample size. There was no evidence that those with lower income or in non-White ethnic groups were experiencing disproportionate impacts. However, we did find that elderly individuals exposed to dB had an approximate 5.4% higher ( and 8 min within a 24-h period on average) actigraphy-measured sleep duration.
In the third set of sensitivity analyses (Figures S18–S25; Table S4–S11), we examined participants reporting health conditions known to be linked to sleep problems. Analyses of actimetric data suggested potential vulnerabilities among participants with diabetes, dementia, or sleep disorder, although based on smaller numbers with wide confidence intervals. We found people with diabetes or dementia exposed to noise levels dB (in comparison with dB) exhibited significantly lower relative amplitude, with associations being and 17 times higher than those found in the entire sample. Diabetic participants exposed to aircraft dB also demonstrated the highest intradaily variability and lowest interdaily stability, with effect sizes estimate1d between 6 and 10 times greater than the pooled effects when all participants were included. The odds for participants with a sleep disorder who were exposed to dB, in comparison with those with a sleep disorder but exposed to dB, was 300% higher. They also spent nearly 24 min (longest among all subgroups) more in sleep or in bed.
Discussion
Many studies relying on subjective reports of sleep quality have found that aircraft noise is associated with disturbed sleep. This study is one of the first to provide objective evidence of impacts of aircraft noise on sleep using actimetry data, with particular strengths of a very large sample size and recruitment being independent of interest in aircraft noise.
Specifically, we observed a higher level of average acceleration during the least active 8-h period in individuals exposed to the highest levels of aircraft noise in comparison with those in the lowest noise group. We also saw sleep–wake cycle changes. Participants exposed to higher nighttime aircraft noise experienced a diminished contrast between daytime activity and nighttime rest (as measured by relative amplitude).51 Their rest–activity rhythm was less stable and less synchronized with the 24-h light–dark cycle (as measured by interdaily stability).21,52 They also showed fragmented rest–activity rhythm (as measured by intradaily variability).52,53 However, we found aircraft noise had no clear impact on objectively measured length of time on sleep or in bed, which agrees with findings on noise exposure and self-reported sleep length in our and other studies.12
Our results on self-reported outcomes suggest mixed results. We noted that nighttime aircraft noise was associated with daytime dozing, with a substantial association size, which again suggests some evidence of poor nighttime sleep among people exposed to high level of aircraft noise at night.27,54 However, although we found a slightly higher likelihood of self-reported sleeplessness among people exposed to higher levels of aircraft noise, such an association was not statistically significant. Furthermore, self-reported shorter hours of sleep were observed among those exposed to high noise levels, which contrasts with our previous evidence of a slightly longer time sleep or in bed measured actimetrically.
Several factors could contribute to differing results from actimetric and self-reported outcomes. Sleep is an unconscious process, and its subjective evaluation can be challenging.8 The potential for recall bias in self-reported sleep measures may account for the contrasting evidence observed. In particular, when looking at self-reported sleep duration, people may not estimate their sleep well and/or estimate it to whole numbers (e.g., 7 h, 8 h), and some may have included daytime naps in the total reported sleep duration. The algorithm used for actimetric defined sleep duration from an Oxford group20 may include time in bed and is less strict than some algorithms.55,56 This approach may lead to a classification bias: an individual who is immobile yet awake can be inaccurately categorized as being in a sleep phase.12 Some studies have found substantial differences between self-reported and physiologically derived measures of sleep, including those related to noise-induced sleep disturbance.8,57 For example, a 2017 study (DEBATS Study) conducted in France with 1,244 participants living near three airports discovered that an increase of 10 dB(A) in aircraft noise level at night was associated with an OR of 1.63 (95% CI: 1.15, 2.32) for self-report of sleeping during the sleeping period of the day.26 However, a subset of 112 individuals with actimetric data showed longer total sleep time (TST) and time in bed (TB) among those exposed to high levels of aircraft noise.12
Given the more objective nature of actimetric measures, evidence of aircraft noise association with actigraphy-derived sleep measures based on a large-scale cohort can complement current studies that predominantly use subjective measures. We showed that actigraphy provides detailed and subtle sleep measures that are not captured by questionnaires. Future research is recommended to examine the association between noise exposure from not only aircraft but also road and railway sources and actimetric measures of sleep disturbance, sleep efficiency, and staging in large cohorts.
Our findings may have a broader health implication. Nighttime exposure to aircraft noise was associated with a slightly higher average acceleration, indicating a higher level of participant movement during rest periods.18,19 We observed a difference in those exposed to higher aircraft noise over the least active 8 h, which compares to an average acceleration in the least active 8 h in the UK Biobank cohort of . The differences are small, and, at present, it is unclear how meaningful they may be, because little research has been conducted on this measure to date.
However, one previous study found that a higher level of participant movement during rest periods of was linked to a higher risk of adverse outcomes from COVID-19.18 A increase in acceleration (the SD difference) was associated with a increase in waist circumference adiposity, a 0.9% increase in % fat, a 0.2-point decrease in fitness as measured by the Short Physical Performance Battery (SPPB) score, a reduction of 1.4 repetitions in the sit-to-stand test, and an increase of 1.5 bpm in resting heart rate.58
To interpret findings on RA, we looked at previous studies. One study using UK Biobank data (91,105 participants) found that a one-quintile reduction ( to difference in absolute value) was associated with increased risks of lifetime major depressive disorder (; 95% CI: 1.04, 1.08), lifetime bipolar disorder (; 95% CI: 1.03, 1.20) and greater mood instability (; 95% CI: 1.01, 1.04).59 A pooled analysis across three studies involving 578 healthy participants showed individuals with the least robust 24-h rest–activity pattern (bottom quintile of relative amplitude) had a BMI that was higher than those with the most robust pattern (top quintile).60,61 Another UK Biobank study found that RA 1 SD higher than the mean () was associated with lower waist circumference.58 If these results can be directly compared with our findings, our identified differences () in RA would correspond to an approximate increase of in waist circumference among individuals exposed to noise levels dB in comparison with those exposed to levels dB. Specific subgroups like individuals with diabetes () and those who look after home/family () showed greater differences in RA when exposed to nighttime aircraft noise, which are in the range previously associated with mental health effects.59
With respect to interdaily stability/intra-daily variability, a study from the United States that focused on 1,734 elderly individuals ( y of age) found a more stable 24-h activity rhythm (as measured by interdaily stability) was associated with a lower mortality risk [hazard ratio (HR) ; 95% CI: 0.71, 0.96] per 1 SD (approximately 0.1), whereas a more fragmented rhythm as measured by IV was associated with a higher mortality risk (; 95% CI: 1.04, 1.44) per 1 SD (around 0.1).62 We found in our study that elderly participants ( y of age), exposed to aircraft noise dB , had an associated 0.08 increase in IV. If results can be directly compared and associations are causal, our results might imply a comparable increase in mortality ratio related to fragmented activity rhythms. This implication needs to be investigated in follow-up studies.
Interdaily stability values are also associated with metabolic health. A 2020 literature review reported that among a subgroup of 1,137 older individuals, higher interdaily stability values (suggesting greater stability of 24-h rest–activity patterns), were associated with 31%, 27%, and 24% lower odds of having metabolic syndrome, type-2 diabetes, and obesity, respectively.61,62
Disruption of circadian rhythms is of concern because of the potential for wider health impacts.63 There is robust evidence derived from both animal models and human epidemiological research that demonstrates circadian disruption to be significant risk factors for cardiovascular disease,64 and growing interest in the relationship between environmental noise and cancer, particularly breast cancer.65,66 One theory for this link is the reduction in melatonin levels caused by disrupted circadian rhythm, which may subsequently contribute to an increased cancer risk.65,67 Circadian misalignment and diminished amplitude of rhythms have been demonstrated to predict the onset of neurodegenerative diseases.68 This pathway could again potentially explain the largely unknown mechanisms underlying the association between noise exposure and neurodegenerative disorders such as dementia, a topic that has attracted increasing attention in recent years.69–72 Additional studies are needed to establish whether nighttime aircraft noise may be impacting on melatonin levels, and circadian rhythm.
A key strength of our paper lies in the large sample size, which, to the best of our knowledge, is the largest to date to look at aircraft noise and device-based measures of sleep disturbance. Although a large sample size can raise concerns about overpowered statistical analysis, we conducted multiple sensitivity analyses on subsamples with smaller sample sizes, and our results remained largely consistent. The research design involving self-reported outcomes is repeated cross-sectional, which is another strength. Furthermore, actimetry has been widely used and validated10 and provides rich outcomes that may not be available through questionnaires. Our study serves as a hypothesis-generating investigation to explore potential actimetric derived outcomes that could be used as proxies for sleep disturbance in future noise studies.
Our paper has some limitations. First, there may be misclassification of noise levels, which could affect the accuracy of our findings. In particular, the noise contours used were assessed for 2011, whereas actimetric data were measured between 2013 and 2015. In addition, building sound-proofing is likely to vary and create differences in individual exposures.8 We adopted a complete case approach to analyze the data, which could introduce bias.73 Some unmeasured health or disease variables might have influenced the sleep outcomes, which we were unable to adjust for in our study. Our sleep outcomes may be subject to biases. Different devices and algorithms used to process actigraphy data could introduce bias. An individual who was immobile may be classified as being in a sleep phase even when they were awake, or conversely, someone with a sleep disorder could be classified as awake, due to movement, despite being asleep.12,15 There was uncertainty about how to address negative values during the gravity removal process, as well as the best method to identify nonwear episodes.15 However, actigraphy has the advantage of being easily performed in larger samples while preserving participants’ natural sleep habits in their homes.12 Some studies, including a retrospective analysis involving 27 patients, have shown that actigraphy and ambulatory polysomnography can yield comparable results in assessing chronic insomnia.74 In a meta-analysis of eight studies that compared sleep architecture estimates between wrist-worn actigraphy and polysomnography, authors found that actigraphy-based sleep staging had some ability to classify different sleep stages in comparison with polysomnography.75,76
We note that flight activity at all the airports in our study is increasing, so consideration will need to be given to potential for increased noise exposure and associated public health impacts. Heathrow, Gatwick, Birmingham, and Manchester, among many other major airports in Europe, are set to expand to accommodate an anticipated increase in passenger numbers by nearly 42% from 2017 to 2040, as projected by the European Environmental Agency.77 Heathrow is planning to build a third runway, supported by the UK government through the Airports National Policy Statement.78 Gatwick plans to make more regular use of its Northern Runway,79 and Manchester and Birmingham airports are considering transforming or expanding their terminals.80,81
Conclusion
We know from many studies relying on subjective report of sleep quality that aircraft noise is associated with disturbed sleep. This study is one of the first to provide evidence on the association between aircraft noise and objective measures of sleep using actimetry data from a large sample near four major international airports in England. Aircraft noise at night was associated with increased movement during the least active continuous 8-h periods (a proxy for sleep) and a disrupted sleep–wake cycle, which has been associated with wider health impacts including mental health, BMI, diabetes, and mortality risk. However, we found aircraft noise had minimal impact on objectively measured length of time in bed, which agrees with self-reported sleep length in our and other studies. Our results have significant policy implications, highlighting the necessity for authorities to formulate strategies that mitigate sleep disturbances caused by aircraft noise.
Supplementary Material
Acknowledgments
The authors thank Enock Havyarimana for help with data preparation. The authors also thank members of the RISTANCO advisory board for their input on the methodological aspects of this study. The advisory board includes representation from relevant government departments and agencies, community groups, nongovernmental organizations, and industry. The views expressed in this paper are those of the author(s) and may not reflect those of the advisory board members or their respective organizations.
The research was funded by the National Institute for Health and Care Research (NIHR) Leicester Biomedical Research Centre (BRC). Additional funding support came from the NIHR Health Protection Research Unit (HPRU) in Environmental Exposures and Health, a partnership between the UK Health Security Agency (UKHSA), the Health and Safety Executive (HSE), and the University of Leicester (Grant number: NIHR200901). The views expressed are those of the author(s) and not necessarily those of the NIHR, Department of Health and Social Care, UKHSA, HSE or University of Leicester.
This research has been conducted using the UK Biobank Resource under Application Number 59129.
The authors gratefully acknowledge the UK Civil Aviation Authority who provided aircraft noise data, calculated using the UK Civil Aircraft Noise Model, ANCON, and the Noise and Statutory Nuisance Team at the Department for Environment, Food & Rural Affairs (DEFRA), for the creation and provision of the Environmental Noise (England) Regulations Round 2 exposure surfaces of rail transport in England.
Funder acknowledgment for NIHR HPRU: The research was supported by the NIHR HPRU in Environmental Exposures and Health, a partnership between the UKHSA, the HSE, and the University of Leicester. The views expressed are those of the author(s) and not necessarily those of the NIHR, UKHSA, HSE, or University of Leicester. [Grant number NIHR200901]
Funder acknowledgment for NIHR BRC: This study/project is funded by/supported by the NIHR Leicester Biomedical Research Centre (BRC). The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health and Care Research or the Department of Health and Social Care.
Data acknowledgment for aircraft noise: The authors acknowledge the UK Civil Aviation Authority, who provided aircraft noise data, calculated using the UK Civil Aircraft Noise Model, ANCON.
Data acknowledgment for railway noise: The authors gratefully acknowledge the Noise and Statutory Nuisance Team at the DEFRA, for the creation and provision of the Environmental Noise (England) Regulations Round 2 exposure surfaces of rail transport in England.
A.L.H. conceived the study. A.L.H. and X.G. developed the study design. J.G., C.J., and K.A. prepared the exposure data and the environmental confounder data. G.A., K.E., and X.G. prepared and manipulated the UK Biobank data with advice from A.R. on sleep and actimetric data. X.G. ran the analyses and wrote the initial draft with input from A.L.H. All authors contributed to interpretation of the results and provided comments on subsequent drafts.
Conclusions and opinions are those of the individual authors and do not necessarily reflect the policies or views of EHP Publishing or the National Institute of Environmental Health Sciences.
References
- 1.World Health Organization Regional Office for Europe. 2018. Environmental Noise Guidelines for the European Region. https://www.who.int/europe/publications/i/item/9789289053563 [accessed 16 August 2024].
- 2.Grollman C, Martin I, Mhonda J. 2020. Aviation Noise and Public Health Rapid Evidence Assessment. https://www.hacan.org.uk/wp-content/uploads/2021/06/Grollman-et-al-2020-Noise-Health.pdf [accessed 16 May 2024].
- 3.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. 2014. Auditory and non-auditory effects of noise on health. Lancet 383(9925):1325–1332, PMID: 24183105, 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muzet A. 2007. Environmental noise, sleep and health. Sleep Med Rev 11(2):135–142, PMID: 17317241, 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Brink M, Schäffer B, Vienneau D, Pieren R, Foraster M, Eze IC, et al. 2019. Self-reported sleep disturbance from road, rail and aircraft noise: exposure–response relationships and effect modifiers in the SiRENE study. Int J Environ Res Public Health 16(21):4186, PMID: 31671890, 10.3390/ijerph16214186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schubert M, Romero Starke K, Gerlach J, Reusche M, Kaboth P, Schmidt W, et al. 2023. Traffic-related high sleep disturbance in the LIFE-Adult cohort study: a comparison to the WHO exposure–response–curves. Int J Environ Res Public Health 20(6):4903, PMID: 36981810, 10.3390/ijerph20064903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basner M, McGuire S. 2018. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health 15(3):519, PMID: 29538344, 10.3390/ijerph15030519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith MG, Cordoza M, Basner M. 2022. Environmental noise and effects on sleep: an update to the WHO systematic review and meta-analysis. Environ Health Perspect 130(7):076001, PMID: 35857401, 10.1289/EHP10197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basner M, Samel A, Isermann U. 2006. Aircraft noise effects on sleep: application of the results of a large polysomnographic field study. J Acoust Soc Am 119(5 pt 1):2772–2784, PMID: 16708935, 10.1121/1.2184247. [DOI] [PubMed] [Google Scholar]
- 10.Van de Water AT, Holmes A, Hurley DA. 2011. Objective measurements of sleep for non-laboratory settings as alternatives to polysomnography–a systematic review. J Sleep Res 20(1 pt 2):183–200, PMID: 20374444, 10.1111/j.1365-2869.2009.00814.x. [DOI] [PubMed] [Google Scholar]
- 11.Röösli M, Brink M, Rudzik F, Cajochen C, Ragettli MS, Flückiger B, et al. 2019. Associations of various nighttime noise exposure indicators with objective sleep efficiency and self-reported sleep quality: a field study. Int J Environ Res Public Health 16(20):3790, PMID: 31600891, 10.3390/ijerph16203790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nassur A-M, Léger D, Lefèvre M, Elbaz M, Mietlicki F, Nguyen P, et al. 2019. The impact of aircraft noise exposure on objective parameters of sleep quality: results of the DEBATS study in France. Sleep Med 54:70–77, PMID: 30529780, 10.1016/j.sleep.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 13.UK Biobank. 2014. Repeat Assessment: participant Characteristics of Responders vs. Non-Responders. https://biobank.ndph.ox.ac.uk/∼bbdatan/repeat_assessment_characteristics_v1.pdf [accessed 19 December 2023].
- 14.UK Biobank. 2007. UK Biobank Ethics and Governance Framework. https://www.ukbiobank.ac.uk/media/0xsbmfmw/egf.pdf [accessed 16 May 2024].
- 15.Doherty A, Jackson D, Hammerla N, Plötz T, Olivier P, Granat MH, et al. 2017. Large scale population assessment of physical activity using wrist worn accelerometers: the UK Biobank study. PLoS One 12(2):e0169649, PMID: 28146576, 10.1371/journal.pone.0169649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Migueles JH, Rowlands AV, Huber F, Sabia S, van Hees VT. 2019. GGIR: a research community–driven open source R package for generating physical activity and sleep outcomes from multi-day raw accelerometer data. J Meas Phys Behav 2(3):188–196, 10.1123/jmpb.2018-0063. [DOI] [Google Scholar]
- 17.Rowlands A, Davies M, Dempsey P, Edwardson C, Razieh C, Yates T. 2021. Wrist-worn accelerometers: recommending ∼1.0 mg as the minimum clinically important difference (MCID) in daily average acceleration for inactive adults. Br J Sports Med 55(14):814–815, PMID: 32928741, 10.1136/bjsports-2020-102293. [DOI] [PubMed] [Google Scholar]
- 18.Rowlands AV, Kloecker DE, Chudasama Y, Davies MJ, Dawkins NP, Edwardson CL, et al. 2021. Association of timing and balance of physical activity and rest/sleep with risk of COVID-19: a UK Biobank study. Mayo Clin Proc 96(1):156–164, PMID: 33413813, 10.1016/j.mayocp.2020.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dawkins NP, Yates T, Razieh C, Edwardson CL, Maylor B, Zaccardi F, et al. 2021. Differences in accelerometer-measured patterns of physical activity and sleep/rest between ethnic groups and age: an analysis of UK Biobank. J Phys Act Health 19(1):37–46, PMID: 34826803, 10.1123/jpah.2021-0334. [DOI] [PubMed] [Google Scholar]
- 20.Walmsley R, Chan S, Smith-Byrne K, Ramakrishnan R, Woodward M, Rahimi K, et al. 2022. Reallocation of time between device-measured movement behaviours and risk of incident cardiovascular disease. Br J Sports Med 56(18):1008–1017, PMID: 34489241, 10.1136/bjsports-2021-104050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitchell JA, Quante M, Godbole S, James P, Hipp JA, Marinac CR, et al. 2017. Variation in actigraphy-estimated rest-activity patterns by demographic factors. Chronobiol Int 34(8):1042–1056, PMID: 28650674, 10.1080/07420528.2017.1337032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ollerhead J, Rhodes D, Viinikainen M, Monkman D, Woodley A. 1999. R&D Report 9842: The UK Civil Aircraft Noise Contour Model ANCON: Improvements in Version 2. https://www.caa.co.uk/publication/download/12420 [accessed 16 May 2024].
- 23.Rhodes D, White S, Havelock P. 2001. Validating the CAA Aircraft Noise Model with Noise Measurements. https://wp-noise-management.s3-eu-west-1.amazonaws.com/2018/06/VALIDATING-THE-CAA-AIRCRAFT-NOISE-MODEL-WITH-NOISE-MEASUREMENTS.pdf [accessed 16 May 2024].
- 24.Heathrow Airport Limite.. 2022. Respite Research. https://www.heathrow.com/company/local-community/noise/making-heathrow-quieter/respite-research [accessed 23 November 2022].
- 25.Eriksson C, Pershagen G, Nilsson M. 2018. Biological Mechanisms Related to Cardiovascular and Metabolic Effects by Environmental Noise. https://iris.who.int/bitstream/handle/10665/346548/WHO-EURO-2018-3009-42767-59666-eng.pdf?sequence=3&isAllowed=y#:∼:text=Environmental%20noise%20may%20induce%20acute,pressure%20elevations%20caused%20by%20vasoconstriction [accessed 16 May 2024].
- 26.Nassur A-M, Lefèvre M, Laumon B, Léger D, Evrard A-S. 2019. Aircraft noise exposure and subjective sleep quality: the results of the DEBATS study in France. Behav Sleep Med 17(4):502–513, PMID: 29172716, 10.1080/15402002.2017.1409224. [DOI] [PubMed] [Google Scholar]
- 27.Basner M. 2008. Nocturnal aircraft noise exposure increases objectively assessed daytime sleepiness. Somnologie 12(2):110–117, 10.1007/s11818-008-0338-8. [DOI] [Google Scholar]
- 28.Li Y, Heath A. 2020. Persisting disadvantages: a study of labour market dynamics of ethnic unemployment and earnings in the UK (2009–2015). J Ethn Migr Stud 46(5):857–878, 10.1080/1369183X.2018.1539241. [DOI] [Google Scholar]
- 29.Smith GD, Chaturvedi N, Harding S, Nazroo J, Williams R. 2000. Ethnic inequalities in health: a review of UK epidemiological evidence. Crit Public Health 10(4):375–408, 10.1080/09581590010005331. [DOI] [Google Scholar]
- 30.Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. 2017. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol 186(9):1026–1034, PMID: 28641372, 10.1093/aje/kwx246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malpezzi S. 2003. Hedonic pricing models: a selective and applied review. In: Housing Economics and Public Policy. O’Sullivan T, Gibb K, eds. Oxford, UK: Blackwell Publishing, 67–89, 10.1002/9780470690680.ch5. [DOI] [Google Scholar]
- 32.Kim KS, Park SJ, Kweon Y-J. 2007. Highway traffic noise effects on land price in an urban area. Transp Res D Transp Environ 12(4):275–280, 10.1016/j.trd.2007.03.002. [DOI] [Google Scholar]
- 33.Blanco JC, Flindell I. 2011. Property prices in urban areas affected by road traffic noise. Appl Acoust 72(4):133–141, 10.1016/j.apacoust.2010.11.004. [DOI] [Google Scholar]
- 34.Woodward M, Peters SA, Harris K. 2021. Social deprivation as a risk factor for COVID-19 mortality among women and men in the UK Biobank: nature of risk and context suggests that social interventions are essential to mitigate the effects of future pandemics. J Epidemiol Community Health 75(11):1050–1055, PMID: 33906905, 10.1136/jech-2020-215810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gulliver J, Morley D, Vienneau D, Fabbri F, Bell M, Goodman P, et al. 2015. Development of an open-source road traffic noise model for exposure assessment. Environ Model Softw 74:183–193, 10.1016/j.envsoft.2014.12.022. [DOI] [Google Scholar]
- 36.Morley DW, de Hoogh K, Fecht D, Fabbri F, Bell M, Goodman PS, et al. 2015. International scale implementation of the CNOSSOS-EU road traffic noise prediction model for epidemiological studies. Environ Pollut 206:332–341, PMID: 26232738, 10.1016/j.envpol.2015.07.031. [DOI] [PubMed] [Google Scholar]
- 37.Extrium. England Noise and Air Quality Viewer. http://extrium.co.uk/noiseviewer.html [accessed 20 May 2024].
- 38.Gulliver J, de Hoogh K, Hansell A, Vienneau D. 2013. Development and back-extrapolation of NO2 land use regression models for historic exposure assessment in Great Britain. Environ Sci Technol 47(14):7804–7811, PMID: 23763440, 10.1021/es4008849. [DOI] [PubMed] [Google Scholar]
- 39.Eeftens M, Beelen R, de Hoogh K, Bellander T, Cesaroni G, Cirach M, et al. 2012. Development of land use regression models for PM(2.5), PM(2.5) absorbance, PM(10) and PM(coarse) in 20 European study areas; results of the ESCAPE project. Environ Sci Technol 46(20):11195–11205, PMID: 22963366, 10.1021/es301948k. [DOI] [PubMed] [Google Scholar]
- 40.Wheeler B. 2017. Documentation of Environmental Indicators Attributed to Participants Based on Home Location Grid References. https://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/App15374Docs.pdf [accessed 3 February 2024].
- 41.Office for National Statistics. 2023. Average Household Income, UK: Financial Year Ending 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/bulletins/householddisposableincomeandinequality/financialyearending2022 [accessed 16 May 2024].
- 42.Cohen M, Katz D, Baruch Y. 2007. Stress among the family caregivers of liver transplant recipients. Prog Transplant 17(1):48–53, PMID: 17484245, 10.1177/152692480701700107. [DOI] [PubMed] [Google Scholar]
- 43.Matthews B, Baker F, Spillers R. 2003. Family caregivers and indicators of cancer-related distress. Psychol Health Med 8(1):46–56, PMID: 21888488, 10.1080/1354850021000059250. [DOI] [PubMed] [Google Scholar]
- 44.Papastavrou E, Kalokerinou A, Papacostas SS, Tsangari H, Sourtzi P. 2007. Caring for a relative with dementia: family caregiver burden. J Adv Nurs 58(5):446–457, PMID: 17442030, 10.1111/j.1365-2648.2007.04250.x. [DOI] [PubMed] [Google Scholar]
- 45.Keilty K, Cohen E, Ho M, Spalding K, Stremler R. 2015. Sleep disturbance in family caregivers of children who depend on medical technology: a systematic review. J Pediatr Rehabil Med 8(2):113–130, PMID: 26409865, 10.3233/PRM-150325. [DOI] [PubMed] [Google Scholar]
- 46.Wang Q, Xi B, Liu M, Zhang Y, Fu M. 2012. Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertens Res 35(10):1012–1018, PMID: 22763475, 10.1038/hr.2012.91. [DOI] [PubMed] [Google Scholar]
- 47.Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. 2021. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev 60:101556, PMID: 34607184, 10.1016/j.smrv.2021.101556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palagini L, Hertenstein E, Riemann D, Nissen C. 2022. Sleep, insomnia and mental health. J Sleep Res 31(4):e13628, PMID: 35506356, 10.1111/jsr.13628. [DOI] [PubMed] [Google Scholar]
- 49.Nôga DA, Meth EdMeS, Pacheco AP, Tan X, Cedernaes J, van Egmond LT, et al. 2024. Habitual short sleep duration, diet, and development of type 2 diabetes in adults. JAMA Netw Open 7(3):e241147, PMID: 38441893, 10.1001/jamanetworkopen.2024.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Surani S, Brito V, Surani A, Ghamande S. 2015. Effect of diabetes mellitus on sleep quality. World J Diabetes 6(6):868–873, 10.4239/wjd.v6.i6.868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McGowan NM, Goodwin GM, Bilderbeck AC, Saunders KE. 2020. Actigraphic patterns, impulsivity and mood instability in bipolar disorder, borderline personality disorder and healthy controls. Acta Psychiatr Scand 141(4):374–384, PMID: 31916240, 10.1111/acps.13148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gonçalves BS, Cavalcanti PR, Tavares GR, Campos TF, Araujo JF. 2014. Nonparametric methods in actigraphy: an update. Sleep Sci 7(3):158–164, PMID: 26483921, 10.1016/j.slsci.2014.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Luik AI, Zuurbier LA, Hofman A, Van Someren EJ, Tiemeier H. 2013. Stability and fragmentation of the activity rhythm across the sleep-wake cycle: the importance of age, lifestyle, and mental health. Chronobiol Int 30(10):1223–1230, PMID: 23971909, 10.3109/07420528.2013.813528. [DOI] [PubMed] [Google Scholar]
- 54.Pérez-Carbonell L, Mignot E, Leschziner G, Dauvilliers Y. 2022. Understanding and approaching excessive daytime sleepiness. Lancet 400(10357):1033–1046, PMID: 36115367, 10.1016/S0140-6736(22)01018-2. [DOI] [PubMed] [Google Scholar]
- 55.van Hees VT, Sabia S, Anderson KN, Denton SJ, Oliver J, Catt M, et al. 2015. A novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS One 10(11):e0142533, PMID: 26569414, 10.1371/journal.pone.0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhu G, Catt M, Cassidy S, Birch-Machin M, Trenell M, Hiden H, et al. 2019. Objective sleep assessment in > 80,000 UK mid-life adults: associations with sociodemographic characteristics, physical activity and caffeine. PLoS One 14(12):e0226220, PMID: 31881028, 10.1371/journal.pone.0226220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silva GE, Goodwin JL, Sherrill DL, Arnold JL, Bootzin RR, Smith T, et al. 2007. Relationship between reported and measured sleep times: the Sleep Heart Health Study (SHHS). J Clin Sleep Med 3(6):622–630, PMID: 17993045. [PMC free article] [PubMed] [Google Scholar]
- 58.Rowlands AV, van Hees VT, Dawkins NP, Maylor BD, Plekhanova T, Henson J, et al. 2023. Accelerometer-assessed physical activity in people with type 2 diabetes: accounting for sleep when determining associations with markers of health. Sensors (Basel) 23(12):5382, PMID: 37420551, 10.3390/s23125382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lyall LM, Wyse CA, Graham N, Ferguson A, Lyall DM, Cullen B, et al. 2018. Association of disrupted circadian rhythmicity with mood disorders, subjective wellbeing, and cognitive function: a cross-sectional study of 91,105 participants from the UK Biobank. Lancet Psychiatry 5(6):507–514, PMID: 29776774, 10.1016/S2215-0366(18)30139-1. [DOI] [PubMed] [Google Scholar]
- 60.Cespedes Feliciano EM, Quante M, Weng J, Mitchell JA, James P, Marinac CR, et al. 2017. Actigraphy-derived daily rest–activity patterns and body mass index in community-dwelling adults. Sleep 40(12):zsx168, PMID: 29029250, 10.1093/sleep/zsx168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zuraikat FM, Makarem N, Redline S, Aggarwal B, Jelic S, St-Onge M-P. 2020. Sleep regularity and cardiometabolic heath: is variability in sleep patterns a risk factor for excess adiposity and glycemic dysregulation? Curr Diab Rep 20(8):1–9, 10.1007/s11892-020-01324-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sohail S, Yu L, Bennett DA, Buchman AS, Lim AS. 2015. Irregular 24-hour activity rhythms and the metabolic syndrome in older adults. Chronobiol Int 32(6):802–813, PMID: 26061588, 10.3109/07420528.2015.1041597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang L, Feng H, Chen J, Kwok Wing Y, Benedict C, Tan X, et al. 2023. Association of circadian rest-activity rhythms with cardiovascular disease and mortality in type 2 diabetes. Diabetes Res Clin Pract 197:110262, PMID: 36690211, 10.1016/j.diabres.2023.110262. [DOI] [PubMed] [Google Scholar]
- 64.Thosar SS, Butler MP, Shea SA. 2018. Role of the circadian system in cardiovascular disease. J Clin Invest 128(6):2157–2167, PMID: 29856365, 10.1172/JCI80590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hansen J. 2017. Environmental noise and breast cancer risk? Scand J Work Environ Health 43(6):505–508, PMID: 29043372, 10.5271/sjweh.3681. [DOI] [PubMed] [Google Scholar]
- 66.Hegewald J, Schubert M, Wagner M, Dröge P, Prote U, Swart E, et al. 2017. Breast cancer and exposure to aircraft, road, and railway noise: a case–control study based on health insurance records. Scand J Work Environ Health 43(6):509–518, PMID: 28813586, 10.5271/sjweh.3665. [DOI] [PubMed] [Google Scholar]
- 67.Stevens RG. 2005. Circadian disruption and breast cancer: from melatonin to clock genes. Epidemiology 16(2):254–258, PMID: 15703542, 10.1097/01.ede.0000152525.21924.54. [DOI] [PubMed] [Google Scholar]
- 68.Fishbein AB, Knutson KL, Zee PC. 2021. Circadian disruption and human health. J Clin Invest 131(19):, PMID: 34596053, 10.1172/JCI148286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen H, Kwong JC, Copes R, Tu K, Villeneuve PJ, van Donkelaar A, et al. 2017. Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: a population-based cohort study. Lancet 389(10070):718–726, PMID: 28063597, 10.1016/S0140-6736(16)32399-6. [DOI] [PubMed] [Google Scholar]
- 70.Carey IM, Anderson HR, Atkinson RW, Beevers SD, Cook DG, Strachan DP, et al. 2018. Are noise and air pollution related to the incidence of dementia? A cohort study in London, England. BMJ Open 8(9):e022404, PMID: 30206085, 10.1136/bmjopen-2018-022404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yu Y, Mayeda ER, Paul KC, Lee E, Jerrett M, Su J, et al. 2020. Traffic-related noise exposure and late-life dementia and cognitive impairment in Mexican-Americans. Epidemiology 31(6):771–778, PMID: 33555809, 10.1097/EDE.0000000000001249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cantuaria ML, Waldorff FB, Wermuth L, Pedersen ER, Poulsen AH, Thacher JD, et al. 2021. Residential exposure to transportation noise in Denmark and incidence of dementia: national cohort study. BMJ 374:n1954, PMID: 34497091, 10.1136/bmj.n1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hughes RA, Heron J, Sterne JA, Tilling K. 2019. Accounting for missing data in statistical analyses: multiple imputation is not always the answer. Int J Epidemiol 48(4):1294–1304, PMID: 30879056, 10.1093/ije/dyz032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martoni M, Bayon V, Elbaz M, Léger D. 2012. Using actigraphy versus polysomnography in the clinical assessment of chronic insomnia (retrospective analysis of 27 patients). Presse Med 41(3 pt 1):e95–e100, PMID: 22104484, 10.1016/j.lpm.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 75.Yuan H, Hill EA, Kyle SD, Doherty A. 2023. A systematic review of the performance of actigraphy in measuring sleep stages. J Sleep Res e14143, PMID: 38384163, 10.1111/jsr.14143. [DOI] [PubMed] [Google Scholar]
- 76.Yuan H, Hill EA, Kyle SD, Doherty A. 2023. A systematic review of the performance of actigraphy in measuring sleep stages. Medrxiv. Preprint posted online August 2023. 10.1101/2023.08.01.23293507. [DOI] [PubMed] [Google Scholar]
- 77.European Environmental Agency. 2019. European Aviation Environmental Report 2019. https://www.eurocontrol.int/publication/european-aviation-environmental-report-2019 [accessed 16 May 2024].
- 78.Heathrow Airport Limited. 2023. Heathrow Expansion. https://www.heathrow.com/company/about-heathrow/expansion [accessed 16 May 2024].
- 79.London Gatwick. 2023. Future Plans. https://www.gatwickairport.com/business-community/future-plans/ [accessed 16 May 2024].
- 80.MAG Manchester Airport. 2023. MAG Announces £440m Investment in Final Phase of £1.3bn Manchester Airport Transformation Programme. https://mediacentre.manchesterairport.co.uk/mag-announces-440m-investment-in-final-phase-of-13bn-manchester-airport-transformation-programme/ [accessed 16 May 2024].
- 81.Birmingham Airport. 2023. Master Plan 2018. https://www.birminghamairport.co.uk/about-us/planning-and-development/airport-strategy/master-plan-2018/ [accessed 16 May 2024].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.