Abstract
Objectives. To compare the incidence, case-hospitalization rates, and vaccination rates of COVID-19 between people experiencing sheltered homelessness (PESH) and the broader community in Chicago, Illinois, and describe the impact of a whole community approach to disease mitigation during the public health emergency.
Methods. Incidence of COVID-19 among PESH was compared with community-wide incidence using case-based surveillance data from March 1, 2020, to May 11, 2023. Seven-day rolling means of COVID-19 incidence were assessed for the overall study period and for each of 6 distinct waves of COVID-19 transmission.
Results. A total of 774 009 cases of COVID-19 were detected: 2579 among PESH and 771 430 in the broader community. Incidence and hospitalization rates per 100 000 in PESH were more than 5 times higher (99.84 vs 13.94 and 16.88 vs 2.14) than the community at large in wave 1 (March 1, 2020–October 3, 2020). This difference decreased through wave 3 (March 7, 2021–June 26, 2021), with PESH having a lower incidence rate per 100 000 than the wider community (8.02 vs 13.03). Incidence and hospitalization of PESH rose again to rates higher than the broader community in waves 4 through 6 but never returned to wave 1 levels. Throughout the study period, COVID-19 incidence among PESH was 2.88 times higher than that of the community (70.90 vs 24.65), and hospitalization was 4.56 times higher among PESH (7.51 vs 1.65).
Conclusions. Our findings suggest that whole-community approaches can minimize disparities in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission between vulnerable populations and the broader community, and reinforce the benefits of a shared approach that include multiple partners when addressing public health emergencies in special populations. (Am J Public Health. 2024;114(S7):S590–S598. https://doi.org/10.2105/AJPH.2024.307801)
People experiencing sheltered homelessness (PESH) in Chicago, Illinois, are at increased risk for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, especially in congregate shelters.1 PESH may also have an increased risk of severe illness with COVID-19 because of underlying medical conditions and systemic health and social inequities. Many urban centers2–4 have experienced large outbreaks of COVID-19 among PESH, with high rates of morbidity and mortality. In Chicago, an early study noted that among 1435 shelter residents tested between March 1 and May 1, 2020, the overall prevalence of infection was 30%.1
In March 2020, the Chicago Department of Public Health (CDPH) responded to COVID-19 among PESH by partnering with the Department of Family and Support Services, homeless service providers, advocacy groups, academic medical centers, and federally qualified health centers (FQHCs) to initiate a whole-community approach5 to COVID-19 mitigation among PESH. In alignment with the Centers for Disease Control and Prevention’s (CDC’s) and Federal Emergency Management Agency’s (FEMA’s) definition and principles of a whole-community approach,5 these strategies included changes to housing services, infection prevention and control interventions, and outbreak detection and response protocols.
Outbreak reports6,7 have detailed strategies used to interrupt SARS-CoV-2 transmission within individual shelters. Additionally, local, national, and global public health agencies have produced guidance aimed at mitigating COVID-19 transmission risk within congregate settings. However, to date, no published reports to our knowledge have detailed citywide, holistic strategies to mitigate the impact of COVID-19 among PESH or have described the impact of these mitigation strategies.
This study used case-based surveillance data to compare the incidence, case-hospitalization rates, and vaccination rates of COVID-19 between PESH and the broader community in Chicago, Illinois, for the duration of the public health emergency (PHE). These data span successive transmission waves and are in the context of holistic, citywide COVID-19 mitigation efforts. We hypothesized that the difference between PESH and community-wide incidence and case-hospitalization for COVID-19 decreased as focused mitigation efforts among PESH were implemented.
METHODS
Chicago, Illinois, is one of the most populous cities in the United States, with a population of 2 693 959.8 Throughout the COVID-19 PHE (January 31, 2020–May 11, 2023) an average estimated 4426 PESH resided in Chicago city limits, with the majority (70.4%) living in homeless shelters and the remainder living unsheltered. This was estimated by averaging the point-in-time (PIT) counts from 2020 to 2023. The PIT count captures an annual sample of people experiencing homelessness on a single night of the year and represents a limited understanding of the total number of people experiencing homelessness. During the PHE, Chicago experienced 6 waves of COVID-19 transmission. A new wave of COVID-19 transmission was defined as a 10% increase in weekly case incidence rate per 100 000 for 2 consecutive weeks in which the increase lasted at least 3 total weeks; if the increase in weekly case counts lasted 2 weeks or less, it was considered a spike and incorporated into the previous wave. The first wave of infection began on March 1, 2020; the start dates of the second through sixth waves of infection are listed in Table 1.
TABLE 1—
COVID-19 Cases, Hospitalizations, and Deaths Among PESH vs Community by Wave and Overall: Chicago, IL, March 1, 2020–May 11, 2023
| COVID-19 Incidence (per 100 000/Day) | COVID-19 Hospitalizations (per 100 000/Day) | Deaths, No. | |||
| Meana | RR (95% CI) | Meana | RR (95% CI) | ||
| Wave 1 (Mar 1, 2020–Oct 3, 2020) | |||||
| PESH | 99.8 | 7.1 (4.2, 13.0) | 16.9 | 8.5 (2.3, 54.4) | 5 |
| Community | 13.9 | 1 (Ref) | 2.1 | 1 (Ref) | 2991 |
| Wave 2 (Oct 4, 2020–Mar 6, 2021) | |||||
| PESH | 63.6 | 1.6 (1.1, 2.5) | 5.0 | 1.7 (0.4, 8.5) | 3 |
| Community | 39.7 | 1 (Ref) | 2.5 | 1 (Ref) | 2096 |
| Wave 3 (Mar 7, 2021–Jun 26, 2021) | |||||
| PESH | 8.0 | 0.6 (0.2, 1.5) | 1.4 | 0.5 (0.02, 6.6) | 2 |
| Community | 13.0 | 1 (Ref) | 1.3 | 1 (Ref) | 595 |
| Wave 4 (Jun 27, 2021–Oct 23, 2021) | |||||
| PESH | 23.0 | 1.9 (1.0, 4.0) | 4.4 | 4.0 (0.5, 99.0) | 1 |
| Community | 12.1 | 1 (Ref) | 0.9 | 1 (Ref) | 404 |
| Wave 5 (Oct 24, 2021–Mar 12, 2022) | |||||
| PESH | 165.7 | 2.7 (2.0, 3.6) | 13.1 | 4.3 (1.3, 19.0) | 6 |
| Community | 62.6 | 1 (Ref) | 2.8 | 1 (Ref) | 1573 |
| Wave 6 (Mar 13, 2022–May 11, 2023) | |||||
| PESH | 57.5 | 3.2 (1.9, 5.6) | 4.3 | 4.0 (0.5, 99.0) | 0 |
| Community | 18.7 | 1 (Ref) | 1.0 | 1 (Ref) | 465 |
| Entire PHE (Mar 1, 2020–May, 11, 2023) | |||||
| PESH | 70.9 | 2.8 (1.8, 4.6) | 7.5 | 8.0 (1.3, 178.9) | 17 |
| Community | 24.6 | 1 (Ref) | 1.6 | 1 (Ref) | 8124 |
Note. CI = confidence interval; PESH = people experiencing sheltered homelessness; PHE = public health emergency; RR = rate ratio.
7-day rolling means.
Data Sources and Main Measures
Case-based surveillance data were obtained through the Illinois National Electronic Disease Surveillance System (I-NEDSS). COVID-19 cases were positive tests for SARS-CoV-2 by any diagnostic assay with US Food and Drug Administration emergency use authorization, including molecular and rapid antigen tests; health care providers and laboratories are required to report all COVID-19 cases to CDPH through I-NEDSS.
COVID-19 cases among PESH were identified via (1) matching addresses of reported cases in I-NEDSS to those of homeless shelters or (2) identifying cases in I-NEDSS that were categorized as residing in a homeless shelter. Cases reported to I-NEDSS not identified as PESH through these methods were defined as broader community cases. Interventions were primarily targeted toward sheltered individuals because of low testing and vaccination uptake in encampment residents. COVID-19 hospitalizations and deaths among both PESH and the community were identified through provider and laboratory reporting in I-NEDSS.
Vaccination data were obtained from the City of Chicago Data Portal of COVID-19 Daily Vaccinations.9 For vaccination among PESH, shelter-based and mobile or street outreach events serving PESH were reported to CDPH in aggregate by lead coordinating organizations. Totals were reported by date of vaccination event, vaccine brand, shelter name, program type, address, the vaccine recipient’s role (resident/attendee, staff, or other), age group, and race/ethnicity by dose type. Housing status was not verified, and only doses administered to residents and attendees of vaccination events were included. “Staff” or “other” attendees of these vaccination events were excluded to help approximate the number of PESH receiving vaccination.
Vaccination coverage was categorized into people who received (1) at least 1 vaccine dose (1 dose of any COVID-19 vaccine, including the single-dose Johnson & Johnson [J&J, Janssen] COVID-19 vaccine), (2) a completed vaccine series (1 dose of J&J or both doses of a 2-dose vaccine such as Pfizer or Moderna), and (3) received at least 1 dose of any booster vaccine. No patient-level identifiers were provided by the lead coordinating organizations. As a result, doses among PESH could not be de-duplicated by individual.
Multiple mitigation strategies were implemented by the City of Chicago to reduce the spread of COVID-19, including domestic and international travel restrictions, closure of nonessential businesses, stay-at-home orders, limited gatherings, mask mandates, and more. CDPH established a COVID-19 Response Bureau for the investigation and surveillance of COVID-19 cases and outbreaks across all settings. The COVID-19 Response Bureau also supported community mitigation efforts that ranged from early detection and prevention measures to follow-up of COVID-19-positive individuals to reduce transmission and to relay public health guidance.
The study period encompasses Chicago’s announcement of its first COVID-19 case and the launch of the COVID-19 response center website on January 24, 2020, through the end of the PHE on May 11, 2023, and includes notable events aimed at preventing COVID-19 transmission. A federal travel restriction was placed on February 3, 2020, and less than 2 weeks later Chicago secured a contract for short-term housing to serve as a quarantine facility. On March 14, 2020, a stay-at-home order was issued, and on March 16, 2020, an executive order was released by the Governor prohibiting all gatherings of 50 people or more, including the suspension of services for on-premises consumption of food and beverages. On April 30, 2020, a mandatory face covering order was issued. An Emergency Travel Order was issued on July 2, 2020, directing travelers entering or returning to Chicago from states experiencing a surge in new COVID-19 cases to quarantine for a period of 14 days.
Several measures were implemented for PESH to reduce transmission following the whole-community approach as recommended by the CDC and FEMA,5 which is characterized not by specific actions taken, but by a collaboration between multiple sectors. The response included the following:
-
1.
Organizing a dedicated CDPH team for infection prevention and control in shelters (March 2020);
-
2.
Convening a coalition of public, academic, and clinical partners providing infection prevention and control training to housing service providers (mid-March 2020);
-
3.
Distributing personal protective equipment to shelters and allocating small grants for facility adjustments to reduce the risk of SARS-CoV-2 transmission (March 18, 2020);
-
4.
Opening decompression shelters to reduce crowding, including 1 hotel space with individual rooms for PESH at the highest risk of severe COVID-1910 (March 22–26, 2020);
-
5.
Establishing an isolation facility for PESH with SARS-CoV-2 infection (April 2, 2020);
-
6.
Partnering with academic medical centers to provide widespread testing in response to detected cases (April 3, 2020);
-
7.
Partnering with FQHCs to provide on-site primary and behavioral health care and infection prevention and control services through Shelter-Based Service Teams (SBSTs; October 20, 2020); and
-
8.
Prioritizing PESH for COVID-19 vaccination (January 25, 2021).
The SBST program was initiated on October 20, 2020, when CDPH contracted 2 FQHCs with experience serving PESH to provide infection prevention services in Chicago shelters. Shelters were assigned to the FQHCs based on the organization’s geographic area of operation and operational capacity. The goal of the program was to reduce health disparities for PESH by (1) reducing transmission of COVID-19 and other infectious diseases in homeless shelters, (2) mitigating the severity of COVID-19 in shelter residents, (3) containing COVID-19 outbreaks in shelters, and (4) improving the long-term health of PESH.
COVID-19 Vaccination
In Chicago, phase 1a vaccination of health care workers and those living in residential health care facilities began on December 15, 2020. Phase 1b vaccination (individuals aged 65 years and older, those living in non-health care residential facilities, and frontline essential workers) began on January 25, 2021; and phase 1c vaccination (those with underlying medical conditions and other essential workers) began March 29, 2021. Phase 2 (all Chicagoans aged 16 years and older) began on April 19, 2021.
In late February 2021, the city launched Protect Chicago Plus, an initiative to deploy resources to communities with the highest need for COVID-19 mitigation. Fifteen high-need communities were prioritized for vaccination using tailored engagement strategies, vaccine clinics, and door-to-door teams to reach residents disconnected from more traditional channels, based on the city’s COVID-19 vulnerability index.
Based on Advisory Committee on Immunization Practices guidance, CDPH included frontline essential workers in homeless shelters and encampments in phase 1b of Chicago’s vaccination program. CDPH also vaccinated residents of congregate settings in phase 1b given that they shared the same level of risk. SBSTs began administering vaccinations in shelters on January 20, 2021. Prior to vaccination visits, SBSTs and CDPH staff provided on-site education and listening sessions around COVID-19 vaccines in the largest shelter sites. Each of the 70 shelters received at least 1 on-site visit by SBST staff by February 15th. Mobile health care teams visited other homeless service sites outside of traditional shelters. Vaccine providers predominantly administered Moderna vaccines, and administered the J&J vaccine after it became authorized for emergency use on February 27, 2021. Individual vaccination records were reported to the Illinois Comprehensive Automated Immunization Registry Exchange (I-CARE), and facility-level vaccine administration data were reported to CDPH.
We calculated 7-day rolling means of COVID-19 incidence among PESH and in the broader community. For incidence calculations among PESH, the PIT estimate (average of 2020–2023 PIT estimates) of the number of PESH in Chicago shelters was used as the denominator (n = 3117). The population of Chicago was estimated from the United States Census Bureau American Community Survey from 2019 (population = 2 693 959). Incidence of COVID-19 and hospitalization among PESH and the broader community were compared using rate ratios (RRs) and 95% confidence intervals (CIs). COVID-19 deaths were rare events among PESH; descriptive statistics are provided in Table 1.
COVID-19 vaccination coverage was defined as the number of COVID-19 vaccines administered over previously mentioned estimates of PESH and community denominators; coverage was compared among PESH and the community using the 2-sample t-test with unequal variance (Welch test) for each wave, as well as the overall study period.
Analyses were conducted in Microsoft Excel (2020), SAS version 9.4 (SAS Institute, Cary, NC) and R version 4.0.3 (The R Foundation, Vienna, Austria). This activity was reviewed by the CDC and determined to be nonresearch.
An independent evaluation of the SBST program was conducted to assess effectiveness and make recommendations to improve its impact and quality. CDPH consulted with the Evaluation, Data Integration, and Technical Assistance (EDIT) Program at Northwestern University. The EDIT team interviewed SBST staff to assess stakeholder perspectives, measure outcomes, provide evidence, explore unanticipated outcomes, and evaluate program implementation. Interviews were transcribed, reviewed for accuracy, and analyzed using a reflexive thematic analysis approach.
Throughout the analytic process, the qualitative research team met to discuss transcripts, noting key themes and ideas in participant responses. Key themes were grouped together to form codes, which were applied to the transcripts in Dedoose. Consensus was reached by the EDIT team when disagreements about code application were identified.
RESULTS
In March 2020, the first laboratory-confirmed case of COVID-19 among PESH in Chicago was reported to CDPH. During the study period (March 1, 2020–May 11, 2023), 774 009 cases of COVID-19 were detected in Chicago; 2579 were detected in PESH compared with 771 430 in the broader community. The characteristics of people testing positive among PESH and the broader community are provided in Table 1.
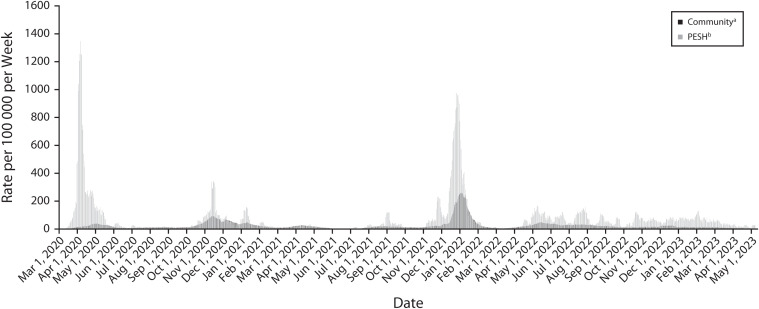
During the overall study period, the average weekly case incidence rate was 2.8 (95% CI = 1.8, 4.6) times higher among PESH compared with the broader community; however, the difference in observed cases varied across waves (Figure 1). Throughout the PHE, the incidence rate in PESH was significantly higher than that of the community in waves 1, 2, 5, and 6, and ranged from 7.1 to 1.6 times higher (Table 2). During wave 3 (March 7, 2021–June 26, 2021) the incidence rate among PESH was lower than that of the wider community (RR = 0.6; 95% CI = 0.2, 1.5).
FIGURE 1—
Seven-Day Rolling Means of COVID-19 Incidence Among People Experiencing Sheltered Homelessness (PESH) and the Community: Chicago, IL, March 1, 2020–May 11, 2023
aThe community comprised the 2019 citywide population estimate of 2 693 959 according to the American Communities Survey.
bPESH comprised 2579 total cases according to the Illinois National Electronic Disease Surveillance System Address Match.
TABLE 2—
Characteristics of People Testing Positive for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Among People Experiencing Sheltered Homelessness and the Community: Chicago, IL, March 1, 2020–May 11, 2023
| Chicago Community, No. (%) | People Experiencing Sheltered Homelessness, No. (%) | |||
| Cases (n = 771 430) | Overall (n = 2 693 959) | Cases (n = 2 579) | Overall (n = 3 117)a | |
| Gender | ||||
| Male | 335 602 (43.5) | 1 311 431 (48.7) | 1 638 (63.5) | 1 836 (58.9) |
| Female | 416 668 (54.0) | 1 382 528 (51.3) | 890 (34.5) | 1 278 (41.0) |
| Unknown | 1 739 (0.2) | … | 51 (2.0) | … |
| Other | … | … | … | 12 (0.4) |
| Age group, y | ||||
| 0–17 | 127 917 (16.6) | 555 424 (20.6) | 202 (7.8) | 842 (27.0) |
| 18–59 | 525 590 (68.1) | 1 631 171 (60.5) | 2 583 (100.2) | 1 951 (62.6)b |
| ≥ 60 | 120 398 (15.6) | 507 364 (18.8) | 507 (19.7) | 324 (10.4) |
| Unknown | 104 (0.0) | … | 3 (0.1) | … |
| Race/ethnicity | ||||
| Non-Latinx Asian | 32 429 (4.2) | 184 768 (6.9) | 32 (1.2) | 33 (1.05) |
| Non-Latinx Black | 172 563 (22.4) | 768 524 (28.5) | 1 310 (50.8) | 2 360 (75.7) |
| Latinx | 207 075 (26.8) | 776 290 (28.8) | 267 (10.4) | 323 (10.36) |
| Non-Latinx Other | 42 899 (5.6) | 62 436 (2.3) | 16 (0.6) | 50 (1.6) |
| Non-Latinx White | 185 831 (24.1) | 901 941 (33.5) | 330 (12.8) | 650 (20.85) |
| Unknown | 133 212 (17.3) | … | 624 (24.2) | … |
This is an average calculated using point-in-time counts from 2020 to 2023 and 2023. All statistics in this column are reflective of this average. Percentages may not equal 100% because of rounding.
Ages 18–59 years had to be estimated from the point-in-time count because of age ranges inconsistent with other data sources and a change of age ranges in 2023 based on Housing and Urban Development guidance.
Across the 6 waves, 51 957 Chicago residents were hospitalized with COVID-19, of which 273 (0.53%) were PESH; 8141 COVID-19-related deaths were detected, of which 17 (0.21%) were PESH. Differences across waves in the incidence of hospitalization among PESH compared with the broader community are provided in Table 2. Across the entire PHE, the hospitalization rate per 100 000 among PESH was significantly higher than that among the wider community (RR = 8.0; 95% CI = 1.3, 178.9), ranging from 8.5 to 1.7 times higher across waves. This theme is reflected across all waves except wave 3, where the hospitalization rate among PESH was lower than that of the community (RR = 0.5; 95% CI = 0.02, 6.6).
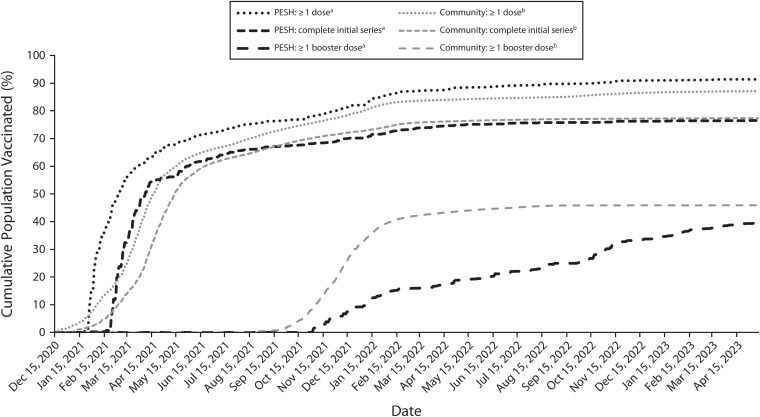
During the study period, 1 863 856 (87.16%) of an estimated 2 138 535 people aged 18 years and older in Chicago received at least 1 dose of any COVID-19 vaccine, 1 654 509 (77.37%) completed a vaccination series, and 981 541 (45.9%) received at least 1 booster vaccine. Among PESH, 2224 (91.37%) of an estimated 2434 sheltered PESH aged 18 years and older received at least 1 dose of any COVID-19 vaccine, 1862 (76.5%) completed a vaccination series, and 959 (39.42%) received at least 1 dose of any booster vaccine.
While vaccination coverage during the study period was similar among PESH and the broader community (Figure 2), uptake of the vaccine among PESH occurred and plateaued earlier relative to the community, consistent with initiating vaccination among PESH during phase 1b. Vaccination coverage at the end of the study period was higher among PESH relative to the wider community for 1 dose (76.8% vs 70.9%; P < .001). There was no significant difference between the 2 groups when assessing those who had received a completed initial vaccine series (63.8% vs 63.1%; P = .468). J&J vaccine doses (n = 285) were counted in both primary vaccine series categories but only account for 12.8% of first doses received and 15% of completed vaccine series. The broader community had a significantly higher booster dose uptake compared with PESH (26.6% vs 15.1%; P < .001).
FIGURE 2—
Percent of Population That Had Received at Least 1 Dose of a COVID-19 Vaccine or Were Fully Vaccinated Among People Experiencing Sheltered Homelessness (PESH) and the Community: Chicago, IL, March 1, 2020–May 11, 2023
aPESH comprised a mean population estimate of 2433 sheltered individuals aged 18 years and older, averaged from the 2020–2023 point-in-time count.
bThe community comprised the 2019 citywide aged 18 years and older population estimate of 2 138 535 according to the American Communities Survey.
Several themes emerged through the evaluation relating to strong relationship building, advocacy, and staffing. On the theme of relationship building, SBST staff felt like peers and collaborators with CDPH, rather than simply staff funded to perform a service. These relationships promoted communication between CDPH, SBSTs, and shelters, fostering the sharing of pertinent information related to COVID-19 transmission risk and prevention. These relationships between the SBSTs and shelters built trust between the shelters and their clients. Relationship-building was further enhanced by the perception that CDPH was advocating for expanded focus and resources for PESH. As service teams hired additional behavioral health staff, clients experienced better care, and service teams benefited from greater professional collaboration. This expansion of internal expertise was key to bringing access to care directly to PESH with groups already experienced with the needs of this population. Respondents also noted that the expansion of services allowed them to build infection control expertise within shelter settings. Expanded services, enhanced client-provider relationships, and information sessions on the COVID-19 vaccine were frequently named as key factors in encouraging PESH to be vaccinated against COVID-19.
Although most themes were positive, interviewees reported that challenges locating and contracting suitable space for isolation led to difficulty isolating patients as a consequence of the nature of available space and other logistical issues.
DISCUSSION
In this study, we found that focused mitigation strategies among PESH were associated with reductions in COVID-19 disparities across 6 waves. In wave 1, we observed an initial 7.1-fold disparity in the average incidence of COVID-19 among PESH relative to the broader community. In waves 2 and 3, PESH saw a large reduction in COVID-19 incidence and hospitalizations, with incidence dropping lower in PESH than the community in wave 3. Incidence and hospitalization rates in PESH rose again in waves 4 to 6 in comparison with the wider community but never returned to wave 1 disparity levels. These data demonstrate the high risk of COVID-19 among PESH and the potential for successful implementation of whole-community approaches to reduce the impact of COVID-19 in this population. After prioritizing multiple layered mitigation strategies among PESH in early waves, COVID-19 incidence during wave 3 was substantially lower among PESH than in the community; this disparity remained reduced throughout the PHE.
It is possible that the reduction in COVID-19 disparities between PESH and the community can be attributed to the prioritization of vaccination for sheltered individuals. More than 75% of the sheltered homeless population received at least 1 dose of the primary vaccine series, and more than 60% received the full primary series during initial vaccine rollout. Despite the low booster uptake in PESH (39.4%), uptake gradually increased through the end of the study period. In contrast, the broader community experienced a plateau in booster vaccination around the fall of 2022. PESH may have had a continuous interest in vaccination strengthened by CDPH-led involvement in shelters.
Limitations
These findings are subject to several limitations. First, the incidence rates reported among PESH and in the broader community are strongly impacted by the availability of diagnostic testing and quality of reporting, which may have differed at times between groups. For example, during Chicago’s first wave of COVID-19 transmission, access to diagnostic testing in the community was limited, particularly for people without symptoms, while testing in congregate settings was prioritized and offered to anyone who had potentially been exposed to the virus. Additionally, much of the diagnostic testing among PESH was conducted by academic medical partners contracted by CDPH, with multiple mechanisms to ensure complete reporting, while the broader community ascertainment of cases was dependent on individual clinical providers and self-reporting of home tests. Despite the more reliable reports from CDPH’s medical partners, cases, hospitalizations, and deaths are still likely to be underreported due to challenges categorizing individuals as homeless in I-NEDSS. Furthermore, unsheltered individuals could not be separated from the broader community and are counted among wider community cases in this analysis, artificially inflating the number of community cases. Sheltered PESH with inaccurate address data or an indication that they resided in a shelter were also included in the broader community case counts. The lack of this information highlights a need for improved case reporting among providers and laboratories.
Second, the extent to which the interventions described are causally linked with reductions in COVID-19 is uncertain; other factors might have contributed, including some level of herd immunity, especially among subpopulations (e.g., specific shelters that experienced large outbreaks during the first wave). Further work should be done to compare mitigation strategies between jurisdictions to more clearly describe this causal relationship.
Third, incidence, hospitalization, and vaccination rates are likely overestimated in PESH in this analysis. This is attributable to the use of PIT count data as an estimate of the true size of the homeless population in Chicago. The PIT methods do not account for movement into or out of this population, or variation through seasons and economic circumstances. The true number of PESH in Chicago throughout the year is likely higher than what is estimated, which would result in an overestimate of rates among PESH. Disparities between PESH and the broader community in incidence and hospitalization may be less pronounced, and vaccination rates are likely lower than estimated in PESH. We chose to use an average of the PIT count estimates from 2020 to 2023 instead of yearly counts for each pandemic year to account for undercounting during the pandemic because of shelter decompression and changes to the PIT count methodology during the pandemic.
Finally, estimates of vaccines given to sheltered PESH may be underreported. Shelter providers reported total doses by event in aggregate, and patient-level data were not available. As such, patient-level housing and vaccine-eligibility could not be confirmed. Moreover, state immunization records (i.e., I-CARE) of vaccination events among PESH appear to be incomplete. Furthermore, the number of PESH vaccinated could not reliably be removed from the number of those in the wider community who were vaccinated, thus PESH are nested within the community estimates.
Public Health Implications
Programming targeted at infection prevention in homeless shelters with a whole-community approach-style collaboration between the health department, partner agencies, and shelter staff builds relationships and service capacity. The SBST program evaluation highlights the importance of continued funding for programs that bring resources directly to PESH. Future evaluations of similar programs should aim to incorporate client feedback alongside providers and shelter staff.
This report underscores the high risk of SARS-CoV-2 infection among PESH during community spread. Originally articulated by FEMA and CDC, a “whole-community approach” became the de facto organizing structure for the COVID-19 national response and appears to be associated with a reduction in incident cases, hospitalizations, and deaths among PESH. Whole-community approaches may be valuable in mitigating SARS-CoV-2 transmission in other populations disproportionately affected by COVID-19.
ACKNOWLEDGMENTS
This work was funded by the Centers for Disease Control and Prevention of the US Department of Health and Human Services (HHS) as part of Epidemiology and Laboratory Capacity Grant 19NU50CK000556.
We would like to thank the residents and staff of all the Chicago homeless shelters, as well as the Chicago Department of Family and Support Services, for their support during the COVID-19 public health emergency and their support as we continue our work in these spaces.
Note. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS, or the US government.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose
HUMAN PARTICIPANT PROTECTION
This study was exempt from institutional review board review because it was conducted for public health surveillance purposes in accordance with federal regulations (45 CFR 46.102(l)(2)). All data were collected and analyzed in a manner ensuring confidentiality and privacy, adhering to ethical standards.
REFERENCES
- 1.Ghinai I, Davis ES, Mayer S, et al. Risk factors for severe acute respiratory syndrome coronavirus 2 infection in homeless shelters in Chicago, Illinois: March-May, 2020. Open Forum Infect Dis. 2020;7(11): ofaa477. 10.1093/ofid/ofaa477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baggett TP, Keyes H, Sporn N, Gaeta JM. Prevalence of SARS-CoV-2 infection in residents of a large homeless shelter in Boston. JAMA. 2020; 323(21):2191–2192. 10.1001/jama.2020.6887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mosites E, Parker EM, Clarke KE, et al. Assessment of SARS-CoV-2 infection prevalence in homeless shelters—four US cities, March 27–April 15, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(17):521–522. 10.15585/mmwr.mm6917e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roederer T, Mollo B, Vincent C, et al. Seroprevalence and risk factors of exposure to COVID-19 in homeless people in Paris, France: a cross-sectional study. Lancet Public Health. 2021;6(4): e202–e209. 10.1016/S2468-2667(21)00001-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Federal Emergency Management Agency. A whole community approach to emergency management: principles, themes, and pathways for action . 2011. . Available at: https://www.fema.gov/sites/default/files/2020-07/whole_community_dec20112.pdf . Accessed October 1, 2023.
- 6.Hsu YT, Lan FY, Wei CF, et al. Comparison of COVID-19 mitigation and decompression strategies among homeless shelters: a prospective cohort study. Ann Epidemiol. 2021;64:96–101. 10.1016/j.annepidem.2021.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montgomery MP, Paulin HN, Morris A, et al. Establishment of isolation and noncongregate hotels during COVID-19 and symptom evolution among people experiencing homelessness-Atlanta, Georgia, 2020. J Public Health Manag Pract. 2021;27(3):285-294. doi: 10.1097/PHH.0000000000001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Census Bureau. American community survey 5-year estimates, 2019. Available at https://www.data.census.gov. Accessed October 1, 2023.
- 9.City of Chicago. COVID-19 daily vaccinations - Chicago residents. 2021. Available at: https://data.cityofchicago.org/Health-Human-Services/COVID-19-Daily-Vaccinations-Chicago-Residents-Hist/2vhs-cf6b/about_data. Accessed October 1, 2023.
- 10.Huggett TD, Tung EL, Cunningham M, et al. Assessment of a hotel-based protective housing program for incidence of SARS-CoV-2 infection and management of chronic illness among persons experiencing homelessness. JAMA Netw Open. 2021;4(12):e2138464. 10.1001/jamanetworkopen.2021.38464 [DOI] [PMC free article] [PubMed] [Google Scholar]