Highlights
-
•
Exercise and education programs can address some barriers to physical activity.
-
•
Continuing to manage persistent knee pain and comorbidities is important.
-
•
Reinforcing pain management strategies may improve physical activity participation.
-
•
Clinicians could facilitate physical activity by referring to community groups.
-
•
Improved funding may be required to support exercise and physical activity initiatives.
Keywords: Arthritis, Knee, Physical therapy, Physiotherapy, Qualitative research rehabilitation
Abstract
Background
A mixed methods study which aimed to evaluate the influence of Good Life with osteoArthritis Denmark (GLA:D®) on physical activity participation, including perceived capability, barriers, and facilitators in people with knee osteoarthritis.
Objective
Quantify changes in physical activity participation at 3- and 12-months for people with knee osteoarthritis who participated in an education and exercise-therapy program (GLA:D®).
Methods
A mixed-methods study involving 44 participants with knee osteoarthritis who completed GLA:D®. Guided by the Theoretical Domains Framework, 19 were interviewed, with transcripts analysed using reflexive thematic analysis. University of California Los Angeles physical activity scores were dichotomised as ‘more’ (≥7) or ‘less’ active (≤6), and compared between baseline and 3- and 12-months using McNemar's test. Motivation and confidence to exercise (0–10 scale); fear of knee joint damage with exercise (yes/no); and Knee Osteoarthritis Outcome Scores (KOOS) were evaluated.
Results
Four overarching themes were identified: prior to GLA:D® 1) fear of knee joint damage, and scarcity of exercise and physical activity information prior to GLA:D®; and following GLA:D® 2) varied exercise-therapy and physical activity participation; 3) facilitators including reduced fear of knee damage, increased confidence, routine, strategies, and support; and 4) ongoing barriers including persistent knee pain, comorbidities, cost, and lack of opportunity and motivation. There was no difference in the proportion of ‘more’ active participants between baseline (41%) and at 3-months (37%, p = 0.774) or 12-months (35%, p = 0.375). The proportion with fear of damage reduced from baseline (50%) to 3-months (5%) and 12-months (21%). Self-reported motivation (9.1/10) and confidence (9.1/10) to exercise at 3-months were high, and all KOOS subscales improved from baseline to 3-months (effect sizes = 0.41–0.58) and 12-months (effect sizes = 0.29–0.66).
Conclusion
Varied and often inadequate physical activity participation following GLA:D® indicates more targeted interventions to address ongoing barriers may be required.
Introduction
Knee osteoarthritis negatively impacts quality of life (QoL),1 community and social participation,2 and occupational capacity.3 Just 13%4 of people with knee osteoarthritis are estimated to meet the physical activity guidelines,5 increasing their risk of comorbidities.6,7 Therefore, increasing physical activity is important for people with knee osteoarthritis due to their increased risk of comorbidities and low levels of physical activity.8 Major international guidelines consistently recommend exercise-therapy, education, and weight management when needed as first-line treatment for knee osteoarthritis.9, 10, 11 Exercise-therapy and education are safe and effectively improve knee pain, physical function, and QoL.12, 13, 14 However, findings related to changes in physical activity following exercise-therapy in controlled clinical trials are mixed.8 While exercise-therapy programs focused on walking or other aerobic exercise4,15, 16, 17 may increase physical activity compared to control interventions, resistance-training alone does not seem to have the same effect.18, 19, 20 Additionally, exercise-therapy may not alter physical activity participation in the medium- (6–12 months) or long-term (>12-months) compared to control interventions.18,19,21, 22, 23 When education focused on pain coping skills is combined with resistance-training, it provides moderate increases to physical activity in the medium-term compared to exercise-therapy alone.8,18,19
The Good Life with osteoArthritis from Denmark (GLA:D®) is an education and exercise-therapy program developed for people with knee or hip osteoarthritis.24,25 It includes education about the importance of physical activity to osteoarthritis management and general health, and is now implemented in at least seven countries, including Australia.26 Outcomes reported at 3- and 12-months include improved pain, joint- and health-related QoL, and functional capacity in people with knee osteoarthritis.25,27, 28, 29 Evaluation of GLA:D® in Denmark indicates that the program may slightly increase the proportion of people who regularly report being more physically active at 3-months, but may have limited influence at 12-months (odds ratio 1.18 and 1.10 respectively, compared to baseline).27
Barriers to physical activity participation for people with knee osteoarthritis include lack of knowledge about benefits, fear of pain and damage with exercise, beliefs and attitudes towards physical activity, environmental constraints, and social influences.30,31 Some barriers may be addressed through education and exercise-therapy provided in programs such as GLA:D®. However, beyond initial quantitative data provided by an initial program evaluation in Denmark, the influence of GLA:D® on physical activity participation has not been explored with qualitative methods. Also, it is not known how capable and motivated participants are to increase their physical activity following GLA:D®. We believe this study will identify important participant perspectives about why their physical activity did or didn't change following a structured education and exercise-therapy program like GLA:D®.
For people with knee osteoarthritis who participated in an education and exercise-therapy program, (GLA:D®), our aim was to use mixed methods to quantify changes in physical activity participation at 3- and 12-months. Additionally, we aimed to explore their perceived capability (motivation, confidence, fear of damage), barriers, and facilitators to increasing their physical activity at 3-months. We aimed to use knee-related patient reported outcome measures (PROMs) for our cohort to compare our findings with the overall GLA:D® population.
Methods
Design
We used a concurrent triangulation design, whereby, separate but complementary qualitative and quantitative methods were used concurrently to collect data, and both contributed to the interpretation of findings. Reporting was guided by Good Reporting of A Mixed Methods Study checklist (GRAMMS)32 and the consolidated criterion for reporting qualitative research checklist (COREQ).33 GLA:D® provides two group education sessions, and 12 supervised group exercise-therapy sessions involving neuromuscular, functional, and resistance-training exercises.28 Education delivered over two sessions, focuses on osteoarthritis, its treatment options, self-management, and exercise and physical activity.28 Further details about the program can be found in the original Danish,27 and subsequent Australian,28 evaluations. Ethics approval for this study was provided by La Trobe University's Human Ethics Research Committee (#HEC18500). All participants provided written informed consent.
Setting
We recruited participants from an existing prospective non-inferiority randomised controlled trial comparing GLA:D® delivered in person or via telehealth (ACTRN12619000235101), as a supplementary study. For our quantitative analysis, data were pooled from both groups to create a prospective cohort study design. We invited 19 participants to interview sequentially from both arms, via email before attending their 3-month follow-up assessment for the existing trial (Supplementary material 1). Following qualitative interviews, quantitative data were included for the full set of recruited participants from the main trial (n = 44).
Participants
Knee osteoarthritis clinical diagnosis was guided by NICE guidelines.10 We included participants if they: i) were aged >40 years, ii) had activity-related knee pain, and iii) had morning stiffness of the knee which lasts less than 30-minutes or no knee stiffness. We selected participants for this secondary analysis consecutively via convenience sampling at the conclusion of the education and exercise-therapy intervention.
Qualitative
A descriptive phenomenology approach was used, whereby semi-structured interviews explored perspectives of people with knee osteoarthritis completing GLA:D® in Australia regarding physical activity participation including perceived capability, barriers, and facilitators. Interviews and qualitative data analysis were led by a female physical therapist (ECB), who was a PhD candidate with previous qualitative research experience34 and three years clinical experience at the time. ECB was supported by three experienced qualitative researchers (CJB, PO, JAW).
Data collection
Semi-structured interviews were guided by a topic guide (Supplementary material 2), developed based on the theoretical domains framework,35 and informed by the clinical and research experience of physical therapists (ECB, CJB, JAW) and a psychologist (PO). Examples were placed as a semi-structured prompt for the interviewer and were offered when participants could not come up with their own examples. This was done so that if participants couldn't think of an example, they may be prompted and able to expand or report that something was not relevant for them. Questions were not pilot tested prior to the first interview. Questions explored participant physical activity participation before and after GLA:D®; perceived capability, confidence, and motivation to participate in physical activity; and barriers and facilitators to physical activity participation. All interviews were conducted individually, in person at a university or via Zoom, audio recorded with verbal consent, and conducted within one-week after the 3-month follow-up from commencement of GLA:D®. Interviews were intended to be conducted on the day of quantitative data collection, and thus designed to be 20- to 30-minutes in duration so they did not overburden participants. Seven of the participants were known to the interviewer (ECB) through her involvement as a treating clinician in the GLA:D® trial, and were instructed to answer all questions, regardless of the nature of responses being positive or negative. One repeat interview was conducted due to a recording failure. Interview field notes were not collected. Participants were recruited until authors (ECB and CJB) felt they were no longer identifying new information. Analysis took place in batches in line with 3-month assessments. Whether new information was identified was carefully considered after each interview. Interviews were transcribed verbatim by a third-party transcription service (Transcription Australia). Participants were provided with a copy of their transcripts and the opportunity to correct any inaccuracies and provide further comments within a four-week period. Feedback was planned to be included in the analysis phase. No participants responded with specific feedback.
Data analysis
Reflexive thematic analysis36 was supported by NVivo software (QSR International Pty Ltd, Melbourne, Australia). Analysis commenced with a close review of each transcript by two researchers (ECB, CJB) to gain an overall picture of the data and a meeting to discuss potential codes. To establish a thematic framework, one researcher assigned codes to each key issue identified, with similar codes being grouped to form subthemes, and subthemes being grouped to form overarching themes. All transcripts contributed to the thematic framework, and themes identified were not predetermined. A random sample of 50% of interviews were coded independently by a third researcher (PO) and compared with the initial analysis. Identified themes were discussed and refined between researchers (ECB, PO, JAW, CJB) at four meetings, until consensus was reached.
Quantitative
Data collection
Except for motivation and confidence ratings collected during interviews, quantitative data were collected via the secure online Research Electronic Data Capture (REDCap) system hosted by La Trobe University. Data were collected at baseline and 3-months on site at La Trobe University by a blinded assessor. An automatic survey was emailed to participants at 12-months, with email reminders every three days for two-weeks then up to three phone calls made to non-respondents.
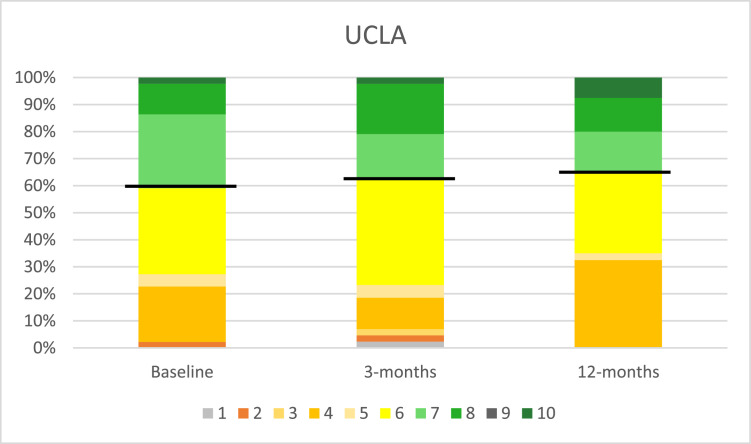
Physical activity was assessed using the University of California, Los Angeles (UCLA) physical activity scale (1–10), which is recommended for observing physical activity participation of osteoarthritis populations (Supplementary material 3).37 The UCLA has established construct validity and reliability.37 Fear of physical activity and exercise was measured by participants answering ‘yes’ or ‘no’ to the question “Are you afraid that your joints will be damaged from physical activity and exercise”. Adherence to GLA:D® exercise-therapy classes, GLA:D® education sessions and home exercise-therapy sessions were also reported by participants at 3-months.
The Knee injury and Osteoarthritis Outcome Score (KOOS) was used to measure sport and recreation participation, pain, symptoms, function, and knee-related QoL (0–100). Higher scores indicate a more positive outcome.38 Each subscale of KOOS has high test-retest reliability.39
During interviews, participants were also asked to provide a numerical value from 0 to 10 (0 being not at all and 10 being maximal) to rate their motivation and confidence (Supplementary material 2).
Data analysis
Statistical analysis was performed using SPSS version 28 (SPSS, Inc, Chicago, IL, USA). Minimal important change has not been defined for the UCLA physical activity scale. Median (interquartile range [IQR]) were calculated for the UCLA physical activity scale. We also dichotomised UCLA data as participants being (i) ‘more’ (≥7= “Regularly participates in active events, such as bicycling” or higher) or (ii) ‘less’ active (≤6= “Regularly participates in moderate activities, such as swimming and unlimited housework or shopping” or lower) (Supplementary material 3). Changes in the number of participants who were physically more active from baseline to 3-months and baseline to 12-months were determined using McNemar's test. The proportion of participants who answered “yes” to fear of damage with physical activity and exercise were presented at baseline and 3- and 12-months. Changes in the number of participants who reported fear from baseline to 3-months and baseline to 12-months were determined using McNemar's test. Mean (standard deviation (SD), range) were calculated for confidence and motivation at 3-months.
Independent one-way ANOVAs were performed to evaluate the changes following GLA:D® on all KOOS subscales. Significance level set at p < 0.05, and Bonferroni's post-hoc test was applied for multiple pairwise comparisons when appropriate. Effect sizes were calculated using Cohen's d, and classified as negligible (<0.10), small (≥0.10), moderate (≥0.30), or large (≥0.50).40 The minimally important change values set for KOOS subscales were 20 for sport and recreation,41 13 for pain,41 16 for symptoms,41 15 for function,41 and 15 for QoL.42 Comparisons of 3- and 12-month outcomes for each KOOS subscale were made with normative values from people without knee injury of similar age (55–74 years).43
To aid clinical interpretation, we compared our KOOS findings at 3- and 12-months to normative values43 to determine whether our participants outcomes were within normal limits, defined as within one standard deviation (SD) from the mean of normative values. Normative means (SDs) used were 67 (33) for sport & recreation, 83 (21) for pain, 83 (21) for symptoms, 82 (22) for function, and 78 (28) for QoL.43
Data synthesis
Triangulation and synthesis of the qualitative and quantitative findings was facilitated by presenting a side-by-side table with an additional column added covering implications for practice generated by the research team and informed by current literature and practice. Findings were considered convergent where qualitative findings aligned with relevant quantitative data. Findings were considered divergent if qualitative findings conflicted with relevant quantitative data.
Results
Nineteen participants were interviewed (in-person=16, Zoom=3) at 3-months following commencement of GLA:D® between September 2019 and January 2020. No invited participants refused participation. Demographics of included participants are provided in Table 1.
Table 1.
Demographics of included participants.
| Qualitative group (n = 19) | All participants (n = 44) | |
|---|---|---|
| Sex (female) | 12 (63 %) | 26 (59 %) |
| Age (years) | 62 (7) | 63 (9) |
| BMI (kg/m2) | 30.9 (6.3) | 30.5 (5.2) |
| Marital status | ||
| Married/de-facto | 15 (79 %) | 34 (77 %) |
| Single | 2 (11 %) | 5 (11 %) |
| Divorced | 1 (5 %) | 3 (7 %) |
| Widowed | 0 (0 %) | 1 (2 %) |
| Separated | 1 (5 %) | 1 (2 %) |
| Education level | ||
| High school | 0 (0 %) | 1 (2 %) |
| Apprenticeship | 1 (5 %) | 2 (5 %) |
| Certificate | 4 (21 %) | 5 (11 %) |
| Diploma | 3 (16 %) | 8 (18 %) |
| Undergraduate | 5 (26 %) | 12 (27 %) |
| Postgraduate | 6 (32 %) | 16 (36 %) |
| Comorbidities | ||
| High blood pressure | 4 (21 %) | 16 (36 %) |
| High cholesterol | 3 (16 %) | 14 (32 %) |
| Chronic lung disease | 4 (21 %) | 8 (18 %) |
| Depression | 2 (11 %) | 3 (7 %) |
| Number of comorbidities | ||
| 0 | 6 (32 %) | 15 (34 %) |
| 1 | 6 (32 %) | 10 (23 %) |
| 2 | 7 (37 %) | 19 (43 %) |
| Adherence to GLA:D® | ||
| Exercise sessions | 11.1 (1.7) | 9.3 (3.7) |
| Education sessions | 1.7 (0.5) | 1.6 (0.6) |
Data are mean (standard deviation) and frequency (proportion). BMI, body mass index; kg, kilogram; m, metres; GLA:D®, Good Life with osteoarthritis.
Qualitative findings
Interviews lasted between 11 and 40 min (mean= 24 min), no participants made changes to their transcripts. Four overarching themes were identified (Tables 2 - 4): 1) fear of knee joint damage, and scarcity of exercise and physical activity information for osteoarthritis prior to GLA:D®; 2) varied exercise-therapy and physical activity participation following GLA:D®; 3) facilitators following GLA:D® included reduced fear of knee damage, increased confidence, routine, strategies, and support; and 4) barriers following GLA:D® included persistent knee pain, comorbidities, cost, and lack of opportunity and motivation. A qualitative matrix with all overarching themes, subthemes, and quotes related to each subtheme is provided in Supplementary material 4, with key illustrative quotes provided in Table 2, Table 3, Table 4.
Table 2.
Theme extracted from qualitative interviews about participants’ views before GLA:D®.
|
Theme 1: fear of knee joint damage, and scarcity of exercise and physical activity information for osteoarthritis prior to GLA:D® | |
|---|---|
| Subthemes | Illustrative quotes |
| Participants report fear of pain and damage to the knee | “I wasn't attempting any exercise on my legs. I wasn't even going there because I was just too worried about incurring more damage.” – P8 “I was cautious. My knee hurt, it was pretty stiff, and I was incapacitated but I was now used to it.” – P18 “I was a bit hesitant and reluctant too because, of course, my pain I was worried, I'd cause myself an injury.” – P12 |
| Previous experience and beliefs about physical activity reduces willingness to participate in physical activity | “I had no problem with doing any exercise and it I was sort of physically active anyway that [GLA:D®] was just an add-on to what I was already doing.” – P10 “I was always keen on exercise and physical activity. I just thought I would have to greatly reduce it because of my knees.” – P17 “I felt like I wanted to do it but couldn't. So I felt limited by my body rather than attitude. I felt a high degree of frustration with my inability to do things that I wanted to do.” – P6 “I wouldn't even have considered the daily exercise routine.” - P5 |
| Health professional education rarely included information about exercise-therapy | “I had very little from GPs [general practitioner] or any other professionals. I'd only had a GP do couple of scans or x-rays… and that's it. No treatment, no exercises, no referrals.” – P10 “I probably haven't received any education [about exercises]. I mean the only thing the surgeon ever said to me was, “I'll see you when you're ready.” -P14 “The knee surgeon I saw said… you can take a few pain killers, but that's not gonna get rid all of the pain totally…Get a new knee.” – P18 “I mean I went to see a knee surgeon and he was the one that suggested I did the GLA:D program.” – P4 “I'd seen physios over the years and got fairly general advice. But I didn't know it was general advice until I started doing [GLA:D®].” – P2 “One other physio who'd said to me, “You cannot exercise if it hurts.”” – P1 “I was already going to the chiro and he recommended a physio.” – P9 |
| Uncertainty of quality of online information and bias towards surgical intervention | “I was looking for information about knee replacements. So, I didn't find a lot about exercise. However, on one Australian site … there was stuff about general exercise being good to keep – especially if you suffer from osteoarthritis, to keep the joints sort of moving. But when I was looking at that stage, I was getting pain in my knee at times… I wasn't taking notice of the exercise suggestions. And there was nothing specific – was like walking, swimming, bike riding… Nothing with dosages, nothing to help explain…the problem is a lot of it is American stuff and it seems to be connected to a place or sponsored by people trying to get you to have knee replacements…” – P2 “I think I always remember what reading about and bringing up on the surgery I suppose, yeah, a little bit. I can't remember [exercise] stuff from the website.” – P17 “Online is very confusing. There's too much information…. Then you work out whether you trust what they say.” – P18 |
Table 3.
Theme extracted about the influence of GLA:D® on physical activity.
|
Theme 2: varied exercise-therapy and physical activity participation following GLA:D® | |
|---|---|
| Subthemes | Illustrative quotes |
| Engagement in varied exercise-therapy following GLA:D® | “I've gone back to the gym and hopefully talking to the physiologist so I can incorporate some of GLA:D® into it.” - P3 “And in doing the GLAD® program, it made me more aware of what I might be doing in my Pilates and Barre classes and RPM [cycling] classes and things like that…” – P19 “I was sort of physically active anyway that it was just an add-on to what I was already doing.” - P10 “… going for walks with my husband, the dogs, on the weekend. I can't walk too fast. But now, we will walk a long way. I was also going back to the gym doing circuit classes, doing the weights.” - P13 |
| Varied physical activity participation following GLA:D® | “Probably just doing more activity, not being sedentary so much, making sure that I get up and move more often than what I was doing….” - P3 “I now attempt stairs where I never used to. I used to avoid the stairs and use the lift. If I'm sore at the end of a shift at work, I will use the lift, but I try to use the stairs more frequently… It made me much more active.” - P9 “It hasn't changed my physical activity, unfortunately, I suppose. But maybe in my physical activity, I feel freer walking, etcetera.” - P14 “I haven't changed and I think cause I was already doing cycling and hockey… I plan to increase it and introduce running back in.” - P17 “I've actually had to decrease… it hasn't improved my ability to walk… The discomfort hasn't changed.” – P1 |
Table 4.
Themes extracted relating to facilitators and barriers to physical activity participation following GLA:D®.
|
Theme 3: physical activity participation facilitators following GLA:D® included reduced fear of knee damage, increased confidence, routine, strategies and support | |
|---|---|
| Subthemes | Illustrative quotes |
| Changes in knowledge and beliefs about physical activity following GLA:D® | “Made me realise I have to be more active and more specifically active… do things that are going to help strengthen the knee as well as improve my cardio activity…….. The knowledge I gained from the program… a) that may not fix things anyway and b) I can actually strengthen the knee…….. Knowledge – most important thing is knowledge and the fact that I was doing exercise regularly because of the sessions, which I wasn't doing without the sessions…” - P2 “I think it showed me why – what happens in your knee with the theoretical part of and then with the exercise program developing the “why” after learning about it in theory, the “why” and how it's going to affect your knee and how it's going to strengthen it and the benefits follow.” – P10 “I think it was just realising that the more you move, the better off you're going to be, long term.” - P3 |
| Reduced fear of knee pain and damage and improved confidence with exercise-therapy and physical activity | “I just feel fitter and stronger and more confident in everything I do.” – P12 “Certainly, the fear of the pain has changed. I don't have that anymore. I'm more confident of what I can do with it now, without damaging it.” – P2 “If we continue on with that sort of exercise regime there is no need for surgery.” – P7 “And that confidence has made a hell of a difference because it's not just someone telling me, it's – I've experienced how I can actually learn to strengthen it.” - P2 “Yes, the program did help me. The benefits are mobility, more confidence in trusting my leg, and as I said before, the understanding that exercise is not to be shied away from.” - P18 “I feel more confident, especially going up again the stairs… it has given me the extra confidence to just try things… I'm much more confident to doing more walking now.” - P3 “It gave me more confidence to go to some of the other classes at the gym that I wouldn't have gone to, I thought there's no way I'll be able to go to those because I can't squat or I can't lunge. Where now I have been known to them, so that's really improved my confidence to go to those other classes.” - P13 “…I was told I have to stop running… I suppose [I've got] confidence in getting back into running.” – P17 |
| Routine, strategies and support facilitate opportunities to remain physically active | “I need to do it early in the morning… It just made me more regimented in what I do and get back to exercise.” - P5 “I'm gonna be happy to pay to do another 12 sessions just to try and create that habit. I think it's definitely stuff that I can do at home… I did like that they tailor it specifically for me.” – P15 “Maybe a little nudgy every now and again… Something like a booster session or a follow-up session or a check-in and are you still doing things right kind of thing would be good… Maybe twice a year.” – P6 “…I'm going to have to make that time and book it in. So I'm committed. It's that accountability stuff.” – P14 “It's up to the individual to apply yourself.” – P11 “… So anything I can do in order to keep myself mobile is going to work for me.” – P14 |
| Impact of external supports (including technology, subsidised activities and social interaction) on physical activity participation | “I mean I've got access to the videos too if I get a little bit stuck.” – P3 “I guess the ease of having a physio, supervising in your own home – that's a big positive for me, if you're time-poor. I guess having it evaluated is important too, there was a 30 percent improvement in that getting up out of a chair- that's significant.” – P14 “A phone application…” – P3 “A little text to remind you every now and again doesn't hurt.” – P6 “Yeah, being able to track [physical activity].” – P18 “…if the government, if it could be subsidised, the money is saved in knee replacements and lack of productivity, and people being on disability pensions and all of those things would be enormous…” – P13 “…There's also a social aspect to it so then we go and have a cup of coffee after and I think that's quite nice.” – P1 |
|
Theme 4: physical activity participation barriers following GLA:D® included persistent knee pain, comorbidities, cost, lack of opportunity, and lack of motivation | |
|---|---|
| Subthemes | Illustrative quotes |
| Impact of ongoing knee pain and comorbidities on physical activity participation | “…still just knee pain.” – P7 “… The inflammatory conditions that I've had with hyperthyroid, the whole package of things that had slowed me down tremendously over the last three or four years…hopefully if my hip settles down…That's the limiting factor with that now, not my knees…” – P6 “Pain and discomfort.” – P4 |
| Lack of motivation as a barrier to ongoing physical activity | “I've never been a person just to do specific exercises like that on my own. I'm a shocker when it comes to self-motivation.” – P1 “[The barrier is] basically my motivation – my starting, my doing something. There's no physical barrier as such.” – P2 |
| Impact of cost of exercise-therapy and physical activity programs on opportunity to participate | “I guess what would hold a lot of people back is the cost. A lot of people just don't see that as an important thing. I mean they might spend money going out to the pictures every week but a lot of people have a lot of trouble spending on their health, whether it would be buying good healthy food or preventative things and so you try and educate people that, yes, it might cost $500 for the program but the benefits you'll get.”…” – P13 …”there's got to be some sort of other way that they could package it because, otherwise, that will be too financially… if I was paying for it, I would say, I can't do that.” – P8 |
| Impact of social and physical environment on opportunity for physical activity participation | “…There's a whole lot of stuff going on at work, which makes it really difficult …” – P14 “…You get a bit busy doing other things and you don't actually do specific physical exercise, and because I do nana duty, I stopped playing tennis.” – P5 “It just hasn't occurred yet and with Christmas, it's chaotic at the moment.” – P5 “I used to do a lot of bike riding, rode thousands of kilometre and whatnot but, unfortunately, the reason I gave that up more to do with safety and more accidents riding a bicycle than I have in my life and that's disappointing…” – P1 “…I'm troubled by things like weather and that sort of thing.” – P6 |
Quantitative findings
Quantitative data were collected for 44 participants at baseline, 43 at 3-months, and 40 at 12-months. There was no difference in the proportion of participants who were ‘more’ active (UCLA score of at least 7) between baseline (41%), 3-months (37%), and 12-months (35%) (McNemar's test 3-months p = 0.774; 12-months p = 0.375). Median [IQR] for UCLA at baseline and 3- and 12-months were 6 [5 to 7], 6 [5 to 6] and 5 [3 to 6], respectively. Detailed results from the UCLA scale are shown in Fig. 1. The proportion of participants reporting fear of knee damage from physical activity and exercise at baseline and 3- and 12-months was 50% (22), 5% (2), and 22.5% (9), respectively (McNemar's test 3-months p=<0.001; 12-months p = 0.013). Mean (SD, range) for confidence and motivation to participate in regular physical activities among interview participants (n = 19) at 3-months were 9.1 (1, 6 to 10) and 9.1 (1, 6 to 10), respectively. Table 5 contains one-way ANOVA results for all subscales of the KOOS.
Fig. 1.
Physical activity for baseline and 3- and 12-months. Figure legend: UCLA= University of Los Angeles Physical Activity Scale, 1=“Wholly inactive: dependent on others; cannot leave residence”, 2=”Mostly inactive: restricted to minimal activities of daily living”, 3="Sometimes participate in mild activities", 4="Regularly participate in mild activities, such as walking, limited housework, and limited shopping", 5="Sometimes participate in moderate activities", 6="Regularly participate in moderate activities, such as swimming and unlimited housework or shopping", 7="Regularly participate in active events, such as bicycling", 8="Regularly participate in very active events, such as bowling or golf", 9="Sometimes participate in impact sports" 10="Regularly participate in impact sports such as jogging, tennis, skiing, acrobatics, ballet, heavy labour, or back packing", solid black line between green and yellow indicates the distinction between ‘more’ and ‘less’ active.
Table 5.
ANOVA for KOOS.
| Baseline vs. 3-months |
Baseline vs. 12-months |
3-months vs. 12-months |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | Pre-GLA:D® | 3-month follow-up | 12-month follow-up | Mean difference | Effect size | Mean difference | Effect size | Mean difference | Effect size |
| KOOS function sport and recreation | 42 (22) | 56 (24) | 53 (26) | 14 (1, 27) | 0.41 | 10 (−3, 23) | 0.29 | −4 (−17, 9) | 0.12 |
| KOOS pain | 63 (16) | 76 (15) | 75 (18) | 13 (4, 21) | 0.58 | 12 (3, 20) | 0.53 | −1 (−10, 8) | −0.04 |
| KOOS symptoms | 57 (20) | 67 (16) | 68 (18) | 11 (1, 19) | 0.44 | 11 (1, 20) | 0.43 | 0 (−9, 10) | 0.00 |
| KOOS function daily activities | 70 (18) | 81 (13) | 81 (17) | 11 (3, 20) | 0.49 | 11 (2, 19) | 0.48 | −1 (−9, 8) | −0.04 |
| KOOS quality of life | 43 (15) | 56 (15) | 57 (18) | 13 (5, 22) | 0.58 | 15* (6, 23) | 0.66 | 1 (−7, 10) | 0.04 |
Data are mean (standard deviation) and mean difference (95 % confidence interval). GLA:D®, Good Life with osteoArthritis from Denmark; KOOS, Knee injury and Osteoarthritis Outcome Score.
Bold values denote p < 0.05.
denotes reaching minimal important change threshold.
All KOOS subscales improved from baseline to 3- and 12-months (Table 5). All KOOS subscales at 3- and 12-months were within normal limits (i.e. within one SD of normative means) (Supplementary material 5). All KOOS subscales except KOOS symptoms (3-months) and KOOS QoL (3- and 12-months) exceeded a value within one minimal important change below the normative mean (Supplementary material 5).
One participant (5%) underwent total knee replacement (TKR) 10-months following commencing GLA:D®. Their UCLA physical activity scale score (3: ‘sometimes participates in mild activities’) remained unchanged at 3- and 12-month follow-ups.
Table 6 contains a synthesis of qualitative and quantitative results, including implications for practice.
Table 6.
Synthesis of qualitative and quantitative data.
| Qualitative findings | Quantitative findings | Convergent or divergent | Implications |
|---|---|---|---|
| Theme 1: Prior to GLA:D®, participants limited physical activity participation due to fear of pain and damage, and education and advice about physical activity and exercise-therapy provided by health professionals was inconsistent. Online information about physical activity was considered unclear, and some participants felt that surgery was overrepresented online. | Prior to GLA:D®, the proportion of participants with fear of damaging their knee through physical activity and exercise was 50% (n = 22/44). | Convergent | Reducing fear of pain and damage with physical activity and exercise may improve willingness to increase or maintain physical activity participation. Initiatives including patient education resource development, increased uptake of existing resources and health professional education and training are needed to improve the consistency of information provided about physical activity and exercise-therapy for osteoarthritis. |
| Theme 2: Following GLA:D®, participants reported inconsistent changes in, and varied participation in, exercise-therapy and physical activity participation. | Proportion of participants who are more active at baseline, 3- and 12-months was 41%, 37% and 35% respectively. | Convergent | Additional intervention following GLA:D® may be needed to improve physical activity participation. Possible interventions need to be explored in detail. Initial suggestions may include tailored physical activity plans and motivational interviewing to address individual barriers and promote individual facilitators. |
| Theme 3: Following GLA:D®, physical activity participation facilitators included improved understanding of the value and benefits of exercise, reduced fear of knee pain and damage, and increased confidence. Suggested strategies to increase or maintain physical activity participation included external supports (technology, subsidised activities and social interaction) and routine. | Compared to baseline (50%), fewer participants reported fear of damage from physical activity and exercise at 3-months (5%) and 12-months (22.5%). Following GLA:D®, average confidence of participants to manage their knee condition was typically high (9.1/10). All KOOS subscales, including sport and recreation, and function, improved at 3- and 12-months to within normal limits. | Convergent | Exercise-therapy and education programs such as GLA:D® can address some barriers to physical activity participation including knowledge about the benefits and safety of exercise, and confidence to manage symptoms and participate in exercise and physical activity. Referral to existing community exercise programs and services (e.g. community walking groups, YMCA gyms), improved access to subsidised exercise support (e.g. gym membership), technology (telehealth or tracking devices) may help to increase physical activity participation. |
| Theme 4: Following GLA:D®, ongoing barriers to physical activity participation included persistent knee pain symptoms and comorbidities. Lack of motivation was frequently an ongoing barrier to physical activity participation following GLA:D®. Other barriers to exercise and physical activity participation following GLA:D® included out-of-pocket costs associated with exercise-therapy and physical activity programs, and inadequate social and physical environment opportunity. |
KOOS symptoms improved at 3-months (67 points) and 12-months (68 points) but remained one MIC below normative values (83 points). Motivation to continue to be physically active was generally high (9.1/10) at 3-months. N/A |
Convergent Divergent N/A |
Following GLA:D®, additional guideline supported interventions to address persistent knee symptoms to increase physical activity participation. For some participants, weight loss may be indicated. Following all first-line management options, participants may benefit from second-line management including pharmacological options, aids and passive treatments. The impact of comorbidities should be evaluated on an individual basis and should be addressed with a multidisciplinary approach as required. Mismatch between quantitative and qualitative findings related to motivation indicate detailed subjective assessment of motivation should be undertaken clinically. Additional behaviour change strategies (e.g. motivational interviewing) targeting motivation may help to increase physical activity participation. In addition to encouraging clinicians to refer to community exercise programs and services, social and environmental factors also need be considered. Physical activity participation may be facilitated through improved funding of exercise and physical activity support including social initiatives, and environmental planning (exercise paths, supporting active transport, etc.) |
Legend: GLA:D®= Good Life with osteoArthritis from Denmark, KOOS = Knee injury and Osteoarthritis Outcome Score, QoL= quality of life, YMCA= Young Men's Christian Association, Theme 1= fear of knee joint damage, and scarcity exercise and physical activity information for osteoarthritis prior to GLA:D®, Theme 2= varied exercise-therapy and physical activity participation following GLA:D®, Theme 3= physical activity participation facilitators following GLA:D® included reduced fear of knee damage, increased confidence, routine, strategies and support, Theme 4= physical activity participation barriers following GLA:D® included persistent knee pain, comorbidities, cost, lack of opportunity, and lack of motivation, MIC= minimal important change.
Discussion
Our mixed methods study provides unique insight into the influence of group education and exercise-therapy programs such as GLA:D® on physical activity participation in people with knee osteoarthritis. Convergent qualitative and quantitative findings indicate a lack of clear or consistent increases to physical activity participation among our cohort. This finding is consistent with previous evaluation of GLA:D® in Denmark over 12-months,27 and most other clinical trials evaluating the effects of exercise-therapy on physical activity, indicating a need for additional interventions beyond GLA:D® to increase physical activity participation in the longer term.8
Following GLA:D® in this study, participants reported greater confidence to engage in exercise and physical activity, alongside improved knowledge about how to manage their knee condition, along with the benefits and safety of exercise. Convergent findings also indicated that fear of knee pain and damage during physical activity participation, which is common in people with knee osteoarthritis,44 was also reduced following GLA:D®. The potential importance of addressing this psychological barrier to physical activity participation is highlighted by the association between lower fear of movement with more steps per day in people with knee osteoarthritis.45 However, lack of consistent increases to physical activity participation in this study despite apparent improvements in knee joint confidence suggests that additional barriers need to be considered and addressed.
Our qualitative findings provide key insights which may help explain the absence of clear or consistent increases to physical activity participation in the longer term following exercise-therapy.8 Firstly, some participants continued to describe lack of motivation as a barrier to physical activity participation following GLA:D®, despite quantitative findings indicating that participants’ motivation was typically high. The divergence between qualitative and quantitative findings may suggest social desirability bias,46 where participants feel that they should be motivated to be physically active following GLA:D®, due to the education they received, rather than actual motivation to be more physically active. Considering this, careful subjective assessment to identify true motivation to increase physical activity participation is encouraged. For those lacking motivation to increase physical activity participation, additional evidence-based behaviour change interventions such as motivational interviewing may help.47,48 Future research to explore this is encouraged.
Beyond motivation, we identified other key ongoing intrinsic barriers to physical activity participation following GLA:D®, including persistent knee pain and comorbidities. Despite all KOOS subscales improving to within normal limits at 3-months, only knee-related QoL was associated with a minimally important change. Medium to large effect increases were achieved by all KOOS subscales from baseline to both 3- and 12-months (except sport and recreation from baseline to 12-months). Additionally our participants remained more than one minimal important change score below aged matched norms for KOOS symptoms (67 vs 83) and KOOS QoL (56 vs 74).43 This suggests that although knee-related health improved following GLA:D®, ongoing difficulties with knee-related symptoms and QoL remained, meaning they were “better” but not necessarily “good”.49 Awareness and consideration of comorbidities such as other medical conditions, additional musculoskeletal conditions, or persistent knee pain are important for clinicians wanting to support people with knee osteoarthritis to increase physical activity participation.50,51
Key ongoing extrinsic barriers to physical activity participation identified following GLA:D® included out-of-pocket costs associated with physical activity programs, safety and physical environment, and inadequate social opportunity. Therefore, publicly funded physical activity programs, community supported activities (such as walking groups), and subsidised gymnasium memberships are encouraged to provide opportunity to participate in physical activity. Importantly, people with knee osteoarthritis may want health professionals to educate them about whether they can participate in more physical activity and where they can join others to participate in exercise following supervised exercise-therapy programs.52 This highlights an opportunity for physical therapists and other health professionals more broadly, to improve their knowledge of, and referral practices to, existing community programs such as walking or running groups (e.g. Parkrun),53 local exercise facilities or community exercise groups. Facilitators identified in this study also warrant consideration. Our participants reported that forming a routine for physical activity may help to keep them on track. Additionally, strategies including booster sessions54 and technology55 including telehealth or activity tracking devices, which can increase adherence to exercise-therapy in knee osteoarthritis were also considered by our participants as potential facilitators to increase physical activity participation.
Prior to GLA:D®, interactions with health professionals were reported to be inconsistent, and often lacked detailed exercise-therapy or physical activity prescription, with seemingly more emphasis on a potential need for surgery. This finding may reflect the common impairment discourse about osteoarthritis, leading people to believe their knee will eventually wear out and that surgery is inevitable.51 Some participants reported difficulty recalling specific physical activity or exercise-therapy information from online searching, while having better recall of surgical information, consistent with reports that only 31% of the commonly accessed knee osteoarthritis websites contain accurate and clear information about exercise-therapy and just 20% for physical activity.56 Collectively, these findings highlight an opportunity for health professionals to discuss and promote physical activity as part of regular practice,57 along with development and dissemination of more online resources promoting the safety and benefits of exercise for knee osteoarthritis.
Our study's findings should be considered in the context of its limitations. Participants were willing to participate in a clinical trial of education and exercise-therapy for their knee osteoarthritis, without any ‘out of pocket’ expenses. Therefore, qualitative findings may not reflect the attitudes of all people with knee osteoarthritis regarding willingness to participate in exercise-therapy and physical activity. Seven interview participants were known to the interviewer (ECB), which may have biased accounts of their experiences with GLA:D®. However, qualitative and quantitative findings mostly converged suggesting this is unlikely to have occurred. The average length of interviews was slightly shorter than some recommendations,58 which is a result of methodological design to not overburden participants. However, our qualitative data set was rich, identifying 4 themes and 14 subthemes to further strengthen our quantitative data. The interviewer did not record notes during interviews, which may mean that reactions were not recorded, however, audio files were able to be used for changes in tone, laughs, etc.
The UCLA physical activity scale has good construct validity and has been widely used in osteoarthritis.59,60 A limitation of this scale is that it combines one item to measure intensity, frequency, difficulty, and duration, potentially limiting sensitivity to change.61,62 Additionally, it is a self-reported measure, creating risk for recall and responder bias. However, our qualitative and quantitative findings related to physical activity participation generally converged, increasing the trustworthiness of quantitative findings. We used a cut-off to determine ‘more’ and ‘less’ active based on the UCLA deemed most likely to correlate with participants who meet physical activity guidelines. However, this cut off is arbitrary, and other cut points may change our findings. Future studies should look to measure physical activity changes following GLA:D® using activity monitoring devices. Some outcome measures used in this study are not well validated in this population, including fear, confidence, and motivation. However, they provide additional information related to barriers and facilitators of physical activity.
Conclusion
Education and exercise-therapy programs such as GLA:D® may address several intrinsic barriers to physical activity, including fear of damage, and knee-related symptoms and confidence. However, despite apparent improvements in knee joint confidence, physical activity participation does not appear to clearly, or consistently, increase at 3- or 12-months following GLA:D®. Further research should evaluate additional interventions beyond commonly implemented education and exercise-therapy programs to address ongoing barriers to increasing physical activity participation in people with knee osteoarthritis.
Author contributions
Conceptualisation: ECB, PO, JAW, KMC, CJB
Participant recruitment: CJB, ZP, ECB, MFP
Project administration: All
Interviews: ECB
Qualitative analysis: ECB, PO, JAW, CJB
Quantitative analysis: ECB, MFP, CJB
First draft: ECB, MFP, PO, JAW, CJB
Final draft: All
Conflicts of interest
Three authors (KMC, JLK, CJB) are program leads of GLA:D® Australia, which is a not-for-profit implementation initiative. Their institution has received payment for training GLA:D® practitioners.
Acknowledgments
Acknowledgements
We would like to thank the physical therapists for providing telehealth GLA:D®, and private physical therapy clinics and their physical therapists for providing in-person GLA:D® to participants in this study, including Complete Sports Care (Hawthorn), Clifton Hill Physiotherapy, Lifecare (Croydon, Prahran), Mill Park Physiotherapy, and Total Physiocare (Heidelberg, Reservoir). This study is supported by a La Trobe University Postgraduate Stipend. One author was supported by an MRFF TRIP Fellowship (APP1150439). This study was funded by a La Trobe University Sport and Exercise Rehabilitation Research Focus Area grant, with additional in-kind support provided by the not-for-profit GLA:D® Australia program.
Data sharing
Data may be made available upon reasonable request from Associate Professor Barton (c.barton@latrobe.edu.au). This includes de-identified quantitative outcomes which are available for 7 years for use before they are destroyed according to ethics requirements. Data may be used for systematic reviews or secondary analyses. Qualitative data are included in supplementary material 4.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.bjpt.2024.101113.
Appendix. Supplementary materials
References
- 1.Desmeules F., Dionne C., Belzile É., Boubonnais R., Frémont P. Waiting for total knee replacement surgery: factors associated with pain, stiffness, function and quality of life. BMC Musculoskelet Disord. 2009;10(52) doi: 10.1186/1471-2474-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallis J.A., Taylor N.F., Bunzli S.N.S. Experience of living with knee osteoarthritis: a systematic review of qualitative studies. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-030060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palmer K. Occupational activities and osteoarthritis of the knee. Br Med Bull. 2012;102(1):147–170. doi: 10.1093/bmb/lds012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallis J.A., Webster K.E., Levinger P., Taylor N.F. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthr Cartil. 2013;21(11):1648–1659. doi: 10.1016/j.joca.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Physical activity. 2023. https://www.who.int/news-room/fact-sheets/detail/physical-activity#:∼:text=Physical%20inactivity%20is%20one%20of,people%20who%20are%20sufficiently%20active.
- 6.Booth F., CK R., Laye M. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–1211. doi: 10.1002/cphy.c110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skou S.T., Pedersen B.K., Abbott J.H., Patterson B., Barton C. Physical activity and exercise therapy benefits more than just symptoms and impairments in people with hip and knee osteoarthritis. JOSPT. 2018;48(6):439–447. doi: 10.2519/jospt.2018.7877. [DOI] [PubMed] [Google Scholar]
- 8.Bell E., Wallis J., Goff A., Crossley K., O'Halloran P., Barton C. Does land-based exercise-therapy improve physical activity in people with knee osteoarthritis? A systematic review with meta-analyses. Osteoarthr Cartil. 2022;30(11):1420–1433. doi: 10.1016/j.joca.2022.07.008. [DOI] [PubMed] [Google Scholar]
- 9.McAlindon T.E., Bannuru R.R., Sullivan M.C., et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil. 2014;22(3):363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Health and Clinical Excellence. NICE guideline on osteoarthritis: the care and management of osteoarthritis in adults. 2014.
- 11.The Royal Australian College of General Practitioners. Guideline for the management of knee and hip osteoarthritis. 2023.https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/knee-and-hip-osteoarthritis
- 12.Fransen M., McConnell S., Harmer A.R., Van der Esch M., Simic M., Bennell K.L. Exercise for osteoarthritis of the knee: a Cochrane systematic review. BMJ. 2015;49(24) doi: 10.1136/bjsports-2015-095424. [DOI] [PubMed] [Google Scholar]
- 13.Briani R., Ferreira A., Pazzinatto M., Pappas E., De Oliveria Silva D., de Azevedo F. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med. 2018;52(16):1031–1038. doi: 10.1136/bjsports-2017-098099. [DOI] [PubMed] [Google Scholar]
- 14.Goff A., De Oliveria Silva D., Merolli M., Bell E., Crossley K., Barton C. Patient education improves pain and function in people with knee osteoarthritis with better effects when combined with exercise therapy: a systematic review. J Physiother. 2021;67(3):177–189. doi: 10.1016/j.jphys.2021.06.011. [DOI] [PubMed] [Google Scholar]
- 15.Shahine N., El Ashri N., Senna M., Elhameed S. Effect of a pedometer based aerobic walking program on pain and function among elderly patients with knee osteoarthritis. Eur J Mol Clin Med. 2020;7(9):790–799. [Google Scholar]
- 16.Yip Y., Sit J., Fung K., et al. Effects of a self-management arthritis programme with an added exercise component for osteoarthritic knee: randomized controlled trial. J Adv Nurs. 2007;59(1):20–28. doi: 10.1111/j.1365-2648.2007.04292.x. [DOI] [PubMed] [Google Scholar]
- 17.Talbot L., Gaines J., Huynh T., Metter E. A home-based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee: a preliminary study. J Am Geriatr Soc. 2003;51(3):387–392. doi: 10.1046/j.1532-5415.2003.51113.x. [DOI] [PubMed] [Google Scholar]
- 18.Bennell K., Ahamed Y., Jull G., et al. Physical therapist-delivered pain coping skills training and exercise for knee osteoarthritis: randomized controlled trial. Arthritis Care Res. 2016;68(5):590–602. doi: 10.1002/acr.22744. [DOI] [PubMed] [Google Scholar]
- 19.Farr J., Going S., McKnight P., Kasle S., Cussler E., M C. Progressive resistance training improves overall physical activity levels in patients with early osteoarthritis of the knee: a randomized controlled trial. Phys The. 2010;90(3):356–366. doi: 10.2522/ptj.20090041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Callahan L., Mielenz T., Freburger J., et al. A randomized controlled trial of the people with arthritis can exercise program: symptoms, function, physical activity, and psychosocial outcomes. Arthritis Rheum. 2008;59(1):92–101. doi: 10.1002/art.23239. [DOI] [PubMed] [Google Scholar]
- 21.Brosseau L., Wells G., Kenny G., et al. The implementation of a community-based aerobic walking program for mild to moderate knee osteoarthritis: a knowledge translation randomized controlled trial: part II: clinical outcomes. BMC Public Health. 2012;12:1073. doi: 10.1186/1471-2458-12-1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schlenk E., Fitzgerald G., Rogers J., Kwoh C., Sereika S. Promoting physical activity in older adults with knee osteoarthritis and hypertension: a randomized controlled trial. J Aging Phys Act. 2021;29(2):207–218. doi: 10.1123/japa.2019-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilcox S., McClenaghan B., Sharpe P., et al. The steps to health randomized trial for arthritis: a self-directed exercise versus nutrition control program. Am J Prev Med. 2015;48(1):1–12. doi: 10.1016/j.amepre.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roos E., Barton C., Davis A., et al. GLA:D to have a high-value option for patients with knee and hip arthritis across four continents: good Life with osteoArthritis from Denmark. Br J Sports Med. 2018;52:1544–1545. doi: 10.1136/bjsports-2017-098904. [DOI] [PubMed] [Google Scholar]
- 25.Roos E., Grønne D., Skou S., et al. Immediate outcomes following the GLA:D® program in Denmark, Canada and Australia. A longitudinal analysis including 28,370 patients with symptomatic knee or hip osteoarthritis. Osteoarthr Cartil. 2021;29(4):502–506. doi: 10.1016/j.joca.2020.12.024. [DOI] [PubMed] [Google Scholar]
- 26.Grønne D., Hansen I., Kongsted A., Roos E., Hartvigsen J., Skou S. GLA:D® Denmark Annual Report 2020. 2021. https://www.glaid.dk/pdf/GLAD_Denmark_annual_report_2020_f.pdf
- 27.Skou S., Roos E. Good Life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord. 2017;18(72) doi: 10.1186/s12891-017-1439-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barton C., Kemp J., Roos E., et al. Program evaluation of GLA:D® Australia: physiotherapist training outcomes and effectiveness of implementation for people with knee osteoarthritis. Osteoarthr Cartil Open. 2021;3(3) doi: 10.1016/j.ocarto.2021.100175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davis A., Kennedy D., Wong R., et al. Cross-cultural adaptation and implementation of Good Life with osteoarthritis in Denmark (GLA:D™): group education and exercise for hip and knee osteoarthritis is feasible in Canada. Osteoarthr Cartil. 2018;26(2):211–219. doi: 10.1016/j.joca.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Dobson F., Bennell K., French S., et al. Barriers and facilitators to exercise participation in people with hip and/or knee osteoarthritis: synthesis of the literature using behavior change theory. Am J Phys Med Rehabil. 2016;95(5):372–389. doi: 10.1097/PHM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 31.Wallis J., Ackerman I., Brusco N., et al. Barriers and enablers to uptake of a contemporary guideline-based management program for hip and knee osteoarthritis: a qualitative study. Osteoarthr Cartil Open. 2020;2(4) doi: 10.1016/j.ocarto.2020.100095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Cathain A., Murphy E., Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy. 2008;13(2):92–98. doi: 10.1258/jhsrp.2007.007074. [DOI] [PubMed] [Google Scholar]
- 33.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32 item checklist for interview and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 34.Barton C., Ezzat A., Bell E., et al. Knowledge, confidence and learning needs of physiotherapists treating persistent knee pain in Australia and Canada: a mixed-methods study. Physiother Theory Pract. 2021;38(12):2073–2085. doi: 10.1080/09593985.2021.1906805. [DOI] [PubMed] [Google Scholar]
- 35.Atkins L., Francis J., Islam R., et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(77):1–18. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Braun V., Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11(4):589–597. doi: 10.1080/2159676X.2019.1628806. [DOI] [Google Scholar]
- 37.Terwee C., Bouwmeester W., van Elslan S., de Vet H., Dekker J. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthr Cartil. 2011;19(6):620–633. doi: 10.1016/j.joca.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 38.Roos E.M., Lohmander L.S. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;64(1) doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alviar M., Olver J., Brand C., Hale T., Khan F. Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med. 2011;43:374–381. doi: 10.2340/16501977-0801. [DOI] [PubMed] [Google Scholar]
- 40.Cohen J. 2nd ed. Taylor & Francis; 1988. Statistical Power Analysis for the Behavioural Sciences. [Google Scholar]
- 41.Collins N., Prinsen C., Christensen R., Bartels E., Terwee C., Roos E. Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthr Cartil. 2016;24(8):1317–1329. doi: 10.1016/j.joca.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 42.Monticone M., Ferrante S., Salvaderi S., Motta L., Cerri C. Responsiveness and minimal important changes for the knee injury and osteoarthritis outcome score in subjects undergoing rehabilitation after total knee arthroplasty. Phys Med Rehabil. 2013;92(10):864–870. doi: 10.1097/PHM.0b013e31829f19d8. [DOI] [PubMed] [Google Scholar]
- 43.Paradowski P., Bergman S., Sundén-Lundius A., Lohmander L., Roos E. Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS) BMC Musculoskelet Disord. 2006;7:38. doi: 10.1186/1471-2474-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gunn A., Schwartz T., Arbeeva L., et al. Fear of movement and associated factors among adults with symptomatic knee osteoarthritis. Arthritis Care Res. 2018;69(12):1826–1833. doi: 10.1002/acr.23226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Uritani D., Kasza J., PK C., Metcalf B., Egerton T. The association between psychological characteristics and physical activity levels in people with knee osteoarthritis: a crosssectional analysis. BMC Musculoskelet Disord. 2020;21:269. doi: 10.1186/s12891-020-03305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Furnham A. Response bias, social desirability and dissumulation. Pers Individ Dif. 1986;7(3):385–400. doi: 10.1016/0191-8869(86)90014-0. [DOI] [Google Scholar]
- 47.O'Halloran P., Blackstock F., Shields N., et al. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin Rehabil. 2014;28(12):1159. doi: 10.1177/0269215514536210. [DOI] [PubMed] [Google Scholar]
- 48.Bell E., O'Halloran P., Wallis J., et al. Using SUpported Motivational InTerviewing (SUMIT) to improve physical activity for people with knee osteoarthritis. A pilot, feasibility randomised controlled trial. BMJ Open. 2023;13(11) doi: 10.1136/bmjopen-2023-075014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roos E., Boyle E., Frobell R., Lohmander L., Ingelsrud L. It is good to feel better, but better to feel good: whether a patient finds treatment ‘successful’ or not depends on the questions researchers ask. BJSM. 2019;53(23) doi: 10.1136/bjsports-2018-100260. [DOI] [PubMed] [Google Scholar]
- 50.Skou S., Mair F., Fortin M., et al. Multimorbidity. Nat Rev Dis Prim. 2022;8(48) doi: 10.1038/s41572-022-00376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bunzli S., Taylor N., O'Brien P., et al. How do people communicate about knee osteoarthritis? A discourse analysis. Pain Med. 2021;22(5):1127–1148. doi: 10.1093/pm/pnab012. [DOI] [PubMed] [Google Scholar]
- 52.Goff A., Donaldson A., De Oliveria Silva D., Crossley K., Barton C. Physical therapists prioritize providing education about exercise therapy and to dispel misconceptions about radiology for people with knee osteoarthritis: a concept mapping study. J Orthop Sports Phys Ther. 2022;52(9):607–619. doi: 10.2519/jospt.2022.11090. [DOI] [PubMed] [Google Scholar]
- 53.Sutton L., Lahham A., Jose K., et al. Feasibility of ‘parkrun’ for people with knee osteoarthritis: a mixed methods pilot study. Osteoarthr Cartil Open. 2022;4(2) doi: 10.1016/j.ocarto.2022.100269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bove A., Smith K., Bise C., et al. Exercise, manual therapy, and booster sessions in knee osteoarthritis: cost-effectiveness analysis from a multicenter randomized controlled trial. Phys Ther. 2018;98(1):16–27. doi: 10.1093/ptj/pzx104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bennell K., Nelligan R., Schwartz S., et al. Behavior change text messages for home exercise adherence in knee osteoarthritis: randomized trial. J Med Internet Res. 2020;22(9):e21749. doi: 10.2196/21749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goff A., Barton C., Merolli M., Quah A., Hoe C., De Oliveira Silva D. Comprehensiveness, accuracy, quality, credibility and readability of online information about knee osteoarthritis. Health Inf Manage J. 2022 doi: 10.1177/18333583221090579. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 57.Cunningham C., O'Sullivan R. Healthcare professionals promotion of physical activity with older adults: a survey of knowledge and routine practice. Int J Environ Res Public Health. 2021;18(11):6064. doi: 10.3390/ijerph18116064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jamshed S. Qualitative research method-interviewing and observation. J Basic Clin Pharm. 2014;5(4):87–88. doi: 10.4103/0976-0105.141942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Holsgaard-Larsen A., Christensen R., Clausen B., Søndergaard J., Andriacchi T., Roos E. One year effectiveness of neuromuscular exercise compared with instruction in analgesic use on knee function in patients with early knee osteoarthritis: the EXERPHARMA randomized trial. Osteoarthr Cartil. 2018;26(1):28–33. doi: 10.1016/j.joca.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 60.Rolfson O., Bohm E., Franklin P., et al. Patient-reported outcome measures in arthroplasty registries. Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries. Part II. Recommendations for selection, administration, and analysis. Atca Orthopaedica. 2016;87:9–32. doi: 10.1080/17453674.2016.1181816. (eSuppl 362) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mørup-Petersen A., Skou S., Holm C., et al. Measurement properties of UCLA Activity Scale for hip and knee arthroplasty patients and translation and cultural adaptation into Danish. Acta Orthop. 2021;96(6):681–688. doi: 10.1080/17453674.2021.1977533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zahiri C., Schmalzried T., Szuszczewicz E., Amstrtz H. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/s0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.