Abstract
Extra-medullary plasmacytoma (EMP) is a rare tumor that most frequently occur in the head and neck region, with the paranasal sinuses, nasopharynx and tonsils being the most common sites. Diagnostic criteria for EMP include histological confirmation of a solitary plasma cell lesion, the presence of fewer than 5% plasma cells in the bone marrow, and the absence of end-organ damage commonly associated with multiple myeloma. CT scans and MRI features are nonspecific and can mimic those of other conditions. EMP of the nasopharynx presents as a slow-growing, radiosensitive mass with a favorable prognosis.
We present the case of a 55-year-old male patient who sought medical attention for recurrent epistaxis. An endoscopic examination revealed a tumor located in the nasopharynx, which was confirmed by MRI as a confined nasopharyngeal mass. Subsequent pathology studies, laboratory results, and bone marrow biopsy were consistent with a solitary EMP of the nasopharynx.
Keywords: Extra-medullary plasmacytoma, Nasopharynx, Diagnosis, Treatment, MRI
Introduction
Plasmacytoma is an exceptionally rare solitary tumor composed of neoplastic monoclonal plasma cells, first described by Schridde in 1905. Extramedullary plasmacytoma (EMP) is infrequently reported and constitutes approximately 4% of all nonepithelial tumors of the upper respiratory tract [1]. It most commonly occurs in the head and neck region. Symptoms are nonspecific and typically result from the local mass effect and compression of adjacent structures [2]. CT and MRI findings are nonspecific and may mimic those of other conditions. Diagnosis is confirmed through histological and immunohistochemical analysis. EMP of the head and neck is radiosensitive, and in most cases, radiation therapy alone with a dose of approximately 40-50 Gy is curative [3].
Case presentation
This case describes a 55-year-old man with no known medical comorbidities who has been suffering from repeated episodes of mild to moderate grade epistaxis during the preceding 6 months. This issue then prompted a visit to an Otolaryngologist. An endoscopic test showed a tumor in the nasopharynx, as well as biopsies were later done
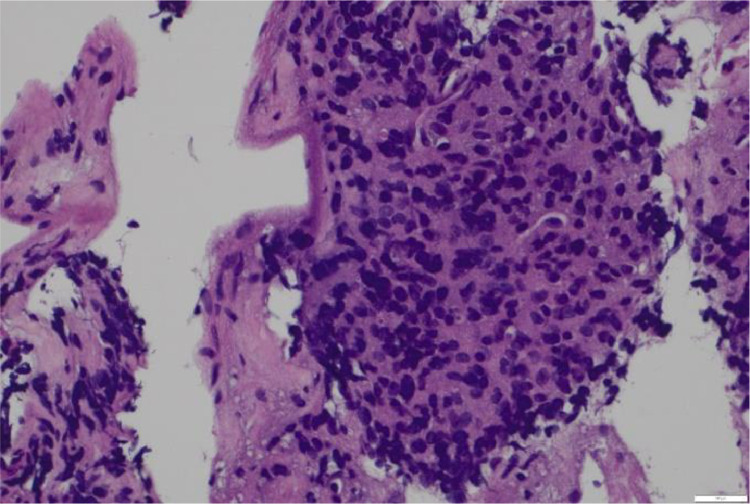
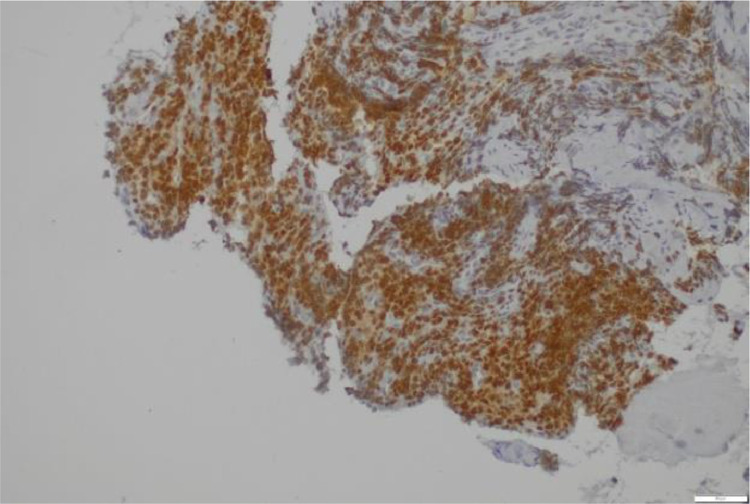
Pathological study revealed monomorphic round to oval cells with eccentric nuclei and immunoblastoid plasmacytoid infiltrate (Fig. 1). Immunohistochemically, the tumor cells were positive for kappa light chain and CD183 (Fig. 2). These pathological findings were consistent with plasmacytoma.
Fig. 1.
Microscopically, the tumor showed sheets of monomorphic round-to-oval cells with nuclear plemorphism (hematoxylin and eosin).
Fig. 2.
Positive immunohistochemical staining for kappa light chains and CD138 antibody.
The laboratory results were as follows: calcium level was 9.7 mg/dL, the albumin-to-globulin ratio was within the normal range, and both serum and 24-hour urine immunofixation electrophoresis were negative. A bone marrow biopsy was performed, and there was no evidence of plasma cell infiltration.
The diagnosis of solitary extramedullary plasmocytoma was made.
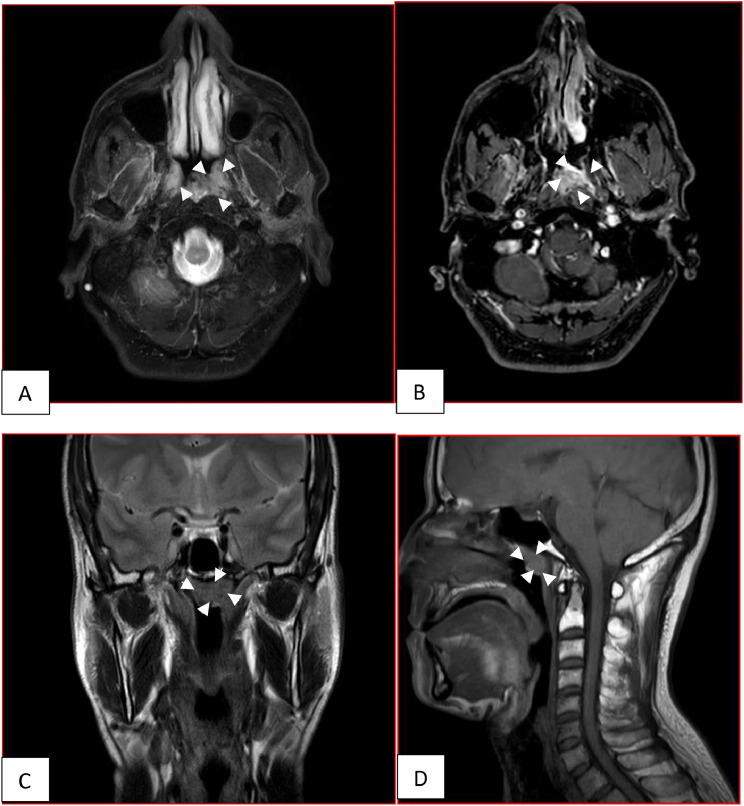
MRI of the nasopharynx revealed a confined nasopharyngeal mass centered in the left Rosenmüller fossa with intermediate signal on T1,T2 weighted images and high signal intensity on Fat-satT2-weighted image, it presented intense and homogeneous enhancement on Fat-sat T1-weighted images (Fig. 3).
Fig. 3.
(A) and (B) Axial fat-sat T2 weighted and axial fat-sat postgadolinium T1-weighted images, (C) Coronal T2 weighted image, (D) Sagittal T1 weighted image. Confined nasopharyngeal mass centered in left Rosenmüller fossa with high signal intensity on T2, It demonstrated intense and homogeneous enhancement (arrowhead).
The patient received exclusive radiotherapy, with a total dose of 50 Gy delivered in 25 fractions of 2 Gy each.
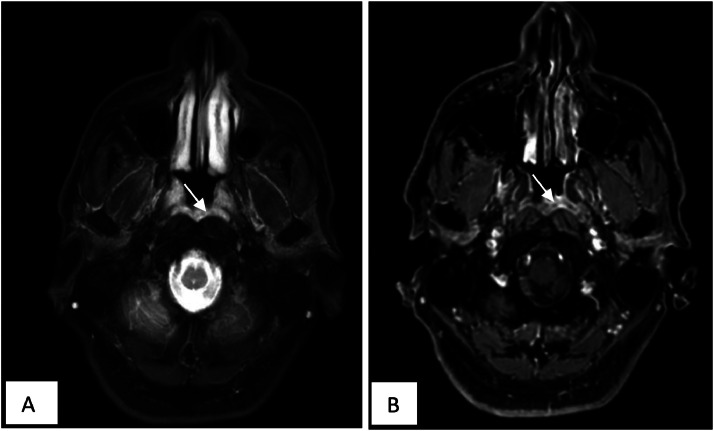
Postradiotherapy MRI findings confirmed optimal control (Fig. 4).
Fig. 4.
(A) and (B) Axial fat-sat T2 weighted and axial fat-sat postgadolinium T1-weighted images. Optimal control after radiotherapy (arrow).
Discussion
Extramedullary plasmacytoma (EMP) represents a rare type of plasma cell dyscrasia characterized by the localized proliferation of monoclonal plasma cells in a single site, such as bone or soft tissue, without evidence of bone marrow or systemic involvement. EMP account for only 2%-5% of all plasma cell dyscrasias, with EMP being even rarer, constituting just 3%-4% of all SP cases. Additionally, some reports indicate that the incidence of solitary bone plasmacytomas is approximately 40% higher than that of EMPs [3].
EMP most frequently occur in the head and neck region, with the paranasal sinuses, nasopharynx, and tonsils being the most common sites. Other less frequent locations include the stomach, intestines, and skin.
EMP exhibits a marked predominance in males, with a male-to-female ratio of approximately 3:1. These lesions most frequently present in individuals during their 60s to 80s. When located in the nasal region, EMPs typically manifest with symptoms such as nasal obstruction, epistaxis, rhinorrhea, and dysphonia [4].
EMP of the nasopharynx present as slow-growing mass and is associated with a favorable prognosis.
EMP shares similarities in cell type, morphology, and pathology with multiple myeloma (MM) but does not exhibit the systemic manifestations associated with the more advanced condition. To diagnose a solitary EMP, it is crucial to rule out multiple myeloma. This differentiation is significant because more than 60% of patients with solitary plasmacytoma are effectively treated with local therapies alone, whereas the 5-year survival rate for multiple myeloma patients is approximately 35% [5].
The diagnostic criteria for solitary EMP include a histologically confirmed solitary plasma cell lesion, less than 5% plasma cells in a bone marrow biopsy from a separate site, absence of end-organ damage typical of multiple myeloma, and a comprehensive skeletal survey to rule out intramedullary involvement [6,7]. In cases of solitary EMP, laboratory tests should be normal except for potential monoclonal gammopathies. Relevant tests include immunoglobulin levels, blood counts, electrolytes, serum-free light chains, and serum protein electrophoresis [6].
CT imaging reveals a homogeneous mass of medium density with homogeneous and significant enhancement following contrast injection. MRI shows a homogeneous mass with slightly hypointense to intermediate signal on T1-weighted images, isointense signal on T2-weighted images, restricted diffusion, and low apparent diffusion coefficient (ADC) values, with notable enhancement after gadolinium administration [8].
These imaging features are nonspecific and may mimic other conditions, such as undifferentiated nasopharyngeal carcinoma, lymphoma, and nasopharyngeal squamous cell carcinoma.
CT scan and MRI are both valuable tools for the initial staging of solitary EMP of the nasopharynx [4].
Whole-body PET-CT is crucial for assessing disease dissemination to additional sites and is also valuable in evaluating treatment response [4].
Management of head and neck EMP typically involves tumor resection, radiation therapy alone, or a combination of surgery followed by radiation. In cases of high-grade or large tumors, chemotherapy may be considered due to the increased risk of recurrence associated with high-grade ESP when treated with RT alone [3].
Conclusion
Though rare, EMP of the nasopharynx must be considered in differential diagnosis of lesions arising from the nasopharyngeal mucosa especially for appropriate treatment. An accurate diagnosis is achieved through detailed work-up. In the present case, after 1 year follow up patient was free from sign of recurrence and successful cured by radiotherapy. Nevertheless, the incidences of local and systemic relapse as well as multiple myeloma transformation emphasize that surveillance is absolutely necessary. Close collaboration between clinicians and radiologists is essential to implement optimal patient management.
Patient consent
The authors of this manuscript declare that an informed consent for publication of this case was obtained from the patient.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Nolan KD, Mone MC, Nelson EW. Plasma cell neoplasms: review of disease progression and report of a new variant. Surg Oncol. 2005;14:85–90. doi: 10.1016/j.suronc.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Wang J, Li J, Zhang F, Zhang P. Retroperitoneal extramedullary plasmacytoma: a case report and review of the literature. Medicine (Baltimore) 2018;97(46) doi: 10.1097/MD.0000000000013281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Padhi P, El-Beheiry R. Extramedullary solitary plasmacytoma with anaplastic features of the nasopharynx. Case Rep Hematol. 2020;2020 doi: 10.1155/2020/8845546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raghuram S, Faizal B, Sanjeevan KV, Eapen M, Nair IR, Philip A, et al. Recurrent extramedullary plasmacytomas without multiple myeloma: a case report with review of the literature. Cancer Treat Res Commun. 2022;31:100550. doi: 10.1016/j.ctarc.2022.100550. [DOI] [PubMed] [Google Scholar]
- 5.Haloui A, Karich N, Akouh N, Seghrouchni N, Najioui Y, Aissaoui A, et al. Ovarian plasmacytoma: a case report. Pan Afr Med J. 2023;44(1) doi: 10.11604/pamj.2023.44.108.37603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gouiaa N, Ellouze S, Bellaaj H, Louati D, Abid H, Mnif H, et al. Plasmocytome ovarien bilatéral: une observation. Imagerie Femme. 2011;21(3):111–114. [Google Scholar]
- 7.Andze G, Pagbe JJ, Edzoa T, Tchokoteu P, Mbakop A, Yomi J. Le plasmocytome solitaire extraosseux ovarien: à propos d’un cas exceptionnel chez une enfant de 12 ans. J Chir (Paris) 1993;130(3):137–140. [PubMed] [Google Scholar]
- 8.El Abbassi I, Elhodaigui N, Boufettal H, Mahdaoui S, Samouh N. Solitary ovarian plasmacytoma: about a rare entity of extramedullary plasma cell tumor. Int J Surg Case Rep. 2024;116:109096. doi: 10.1016/j.ijscr.2023.109096. [DOI] [PMC free article] [PubMed] [Google Scholar]