Abstract
Carotid body tumors (CBTs) are rare, hypervascular neuroendocrine neoplasms that can lead to significant complications during surgical resection due to the high risk of bleeding. We present the case of a 64-year-old male with a palpable neck mass on the left side, diagnosed as a CBT through imaging studies. Given the tumor's increasing size and rich vascularization, percutaneous preoperative embolization with Onyx under ultrasound and angiographic guide, was performed to minimize intraoperative complications. Forty-eight hours later, the tumor was surgically resected with minimal blood loss and no injury to cranial nerves or the carotid bifurcation.
Keywords: Carotid body tumor, Embolization, Onyx, Paraganglioma, Preoperative embolization
Introduction
Carotid body tumors (CBTs), alternatively termed paragangliomas or chemodectomas, are uncommon, con hypervascular neuroendocrine neoplasms arising from the chemoreceptor of the carotid body. The reported incidence of CBTs is approximately 1-2 cases per 100.000; 94% of them are benign and represents about 0.6% of all head and neck tumors. They occur at any age but the mean patient age is 30-40 years, with slightly higher prevalence in women than men (M/F ratio of 1/1.9) [1].
The majority of CBTs do not present with symptoms, often being discovered incidentally during physical examinations or radiological imaging studies. Nonetheless, in symptomatic cases, common symptoms include pain, dysphagia and autonomic dysfunction. The tumor is laterally mobile but not vertically (Fontaine's sign) [2].
Eco-color-doppler ultrasonography is the ideal screening test for CBTs. These tumors typically appear as a well-defined hypoechoic mass that splays the carotid bifurcation. Color Doppler imaging reveals a hypervascular appearance with a low-resistance flow pattern. This lesion has a soft tissue density and intense enhancement on CT. On MRI, the mass has a slightly high signal on T2W, slightly low signal on non‐contrast-enhanced T1W, strong enhancement on contrast-enhanced T1W and restricted diffusion in DWI. On MRI, CBTs often exhibit a distinctive "salt and pepper" appearance, where "salt" refers to hyperintense areas indicative of hemorrhage, and "pepper" indicates hypointense flow voids from prominent blood vessels. The splaying of the internal carotid artery (ICA) and external carotid artery (ECA) by the tumor, known as the "Lyre sign," is characteristic of a CBT [3].
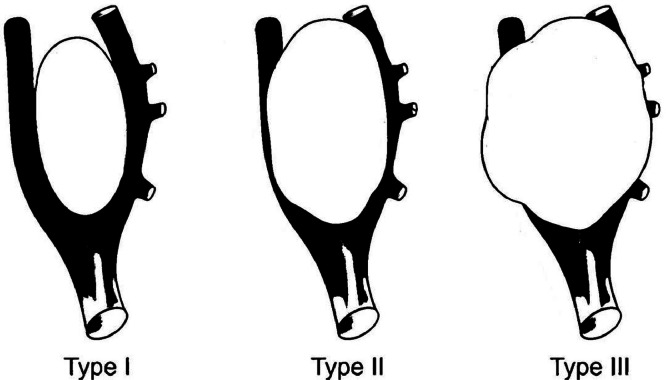
In 1971, Shamblin introduced a classification system based on the relationship with the carotid arteries to determine the respectability of these tumors (Fig. 1).
Fig. 1.
Circumferential angle of contact of tumor with ICA can be categorized under the Shamblin group system as type I with <180° of encasement, type II with 180°-270° of encasement, type III with >270° of encasement.
Surgical excision continues to be the gold standard therapeutic modality and the most effective treatment for CBTs.
To optimize the outcomes of surgical intervention, preoperative selective embolization is often performed 24-48 hours before surgery, to shrink the tumor, minimize intraoperative blood loss, and reduce the risk of cranial nerve (CN) injury [4].
Case report
A 64-year-old, hypertensive male patient presented for a palpable mass in the left side of the neck, with palpitations since a few days, as associated symptomatology. The patient reported that the mass has gradually increased in size over the last year.
The clinical examination revealed a firm, painless mass localized behind the left sternocleidomastoid muscle with positive Fontaine's sign. There were no palpable lymph nodes.
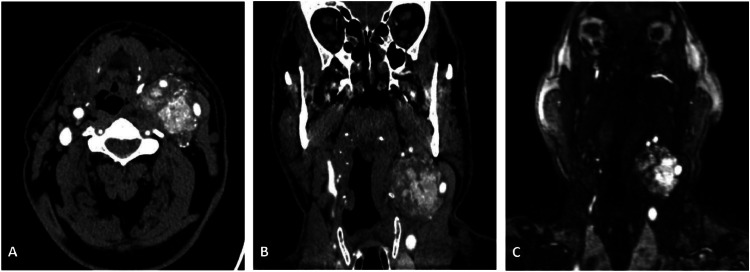
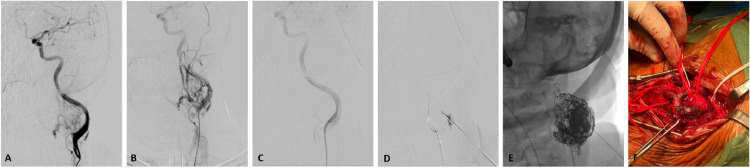
CT of the neck showed an oval mass measuring 5×4 cm, with soft tissue density and high contrast enhancement, localized next to the left carotid bifurcation. The characteristic “lyre sign” was described: the mass displaced the left ICA posteriorly and the left ECA anteriorly. In further Magnetic Resonance Angiography (MRA), the lesion presented hypointense signal in T1 and heterogeneously hyperintense signal in T2 (a "salt and pepper" appearance), as well as significant enhancement after gadolinium administration (Fig. 2); thus supporting the diagnosis of carotid glomus tumor. However, due to the observed increase in tumor volume and the presence of rich vascularization, we collegially opted to conduct preoperative embolization. Transarterial access was obtained through the right common femoral artery. DSA were performed from ICA and ECA; the characteristic splaying of the 2 main left carotid branches (lyre sign) was confirmed; the mass showed a rich blood supply from feeding vessels originating primarily from left ascending pharyngeal artery. After a carotid balloon test occlusion, selective catheterization of the left ECA was performed, followed by super-selective catheterization of the tumor-feeding vessels. The ECA was temporarily occluded with Eclipse micro-balloon catheter, to prevent the reflux of embolic material. The CBT was punctured percutaneously, under ultrasound guidance, for the intralesional injection of the embolic material Onyx. The injection of Onyx was completed when the previously visualized portion of the tumor supplied by the given vascular territory was occluded. The final angiographic assessment showed a complete and successful elimination of the uptake of contrast agents in the mass. The patency of the carotid bifurcation was confirmed by the passage of a contrast agent at the 2 main left carotid branches at the end of the procedure (Fig. 3). Forty-eight hours later, the surgical resection of the tumor was carried out. During the entire operation, less than 100 mL of blood was lost and no injuries to the carotid bifurcation or CN were observed.
Fig. 2.
Axial (A), coronal (B) CT scans and coronal MRA (C), demonstrate a mass with significant contrast enhancement located adjacent to the left carotid bifurcation. The mass displaces the left ICA posteriorly and the left ECA anteriorly, creating the characteristic "lyre sign."
Fig. 3.
DSA was performed from CCA, the characteristic splaying of the 2 main left carotid branches (lyre sign) was confirmed; the mass showed a rich blood supply from feeding vessels originating primarily from left ascending pharyngeal artery (A and B). The ECA was temporarily occluded with Eclipse micro-balloon catheter, to prevent the reflux of embolic material (C). The CBT was punctured percutaneously, under ultrasound guidance, for the intralesional injection of the embolic material Onyx (D). The final angiographic assessment showed a complete and successful elimination of the uptake of contrast agents in the mass (E). Forty-eight hours later, the surgical resection of the tumor was carried out without complications (F).
Histopathological examination confirmed the initial diagnosis of CBT. The patient was instructed to follow-up.
Discussion
Paragangliomas are highly vascularized tumors, which might lead to a considerable blood loss during surgical extirpation.
Preoperative embolization of CBTs has been proposed by Shick et al. in 1980 as a technique to reduce operative blood loss and perioperative complications [5].
Casasco, et al. first described direct devascularization of head and neck tumors in 1994, as a suitable solution allowing for the obliteration of the entire CBT tumor bed [6]; prior to this, transarterial embolization was the favored treatment modality.
Initial reports employed n-butyl cyanoacrylate (n-BCA), though delayed migration of n-BCA has been described [7].
More recently, Onyx, which has more uniform and consistent composition and facilitates a safer and more controlled intralesional injection, has been successfully used.
Although no direct comparative studies for these 2 embolic agents are available. Onyx has slower precipitation, enabling deeper penetration into the tumor bed and facilitating more controlled injection [8]. Despite that, there is a certain but relatively small risk of Onyx deviation into the ECA, thus, we inserted and temporarily inflated a nondetachable micro-balloon in the proximal ECA.
Further documentation is necessary to prove the higher grade of devascularization of paragangliomas with Onyx compared with conventional glue.
Recent recommendations in the literature advocate that preoperative embolization should precede the surgical procedure for 24-48 hours to reduce local edema and inflammation associated with embolization procedures [4].
Although a large metanalysis [9] showed no reduction in vascular injury in surgical resection performed without preoperative embolization, several studies have demonstrated benefits from preoperative embolization in terms of minimizing intraoperative complications [4,6]. According to Garg et al. [10] the preference and experience of the senior surgeon should be the factors that guide the decision.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Berger G, Łukasiewicz A, Grinevych V, et al. Carotid body tumor - radiological imaging and genetic assessment. Pol Przegl Chir. 2020;92:39–44. doi: 10.5604/01.3001.0014.4872. [DOI] [PubMed] [Google Scholar]
- 2.Butt N, Baek WK, Lachkar S, et al. The carotid body and associated tumors: updated review with clinical/surgical significance. Br J Neurosurg. 2019;33:500–503. doi: 10.1080/02688697.2019.1617404. [DOI] [PubMed] [Google Scholar]
- 3.Yuan Y, Shi H, Tao X. Head and neck paragangliomas: diffusion weighted and dynamic contrast enhanced magnetic resonance imaging characteristics. BMC medical imaging. 2016;16(12):1–6. doi: 10.1186/s12880-016-0114-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore MG, Netterville JL, Mendenhall WM, Isaacson B, Nussenbaum B. Head and neck paragangliomas: an update on evaluation and management. Otolaryngol Head Neck Surg. 2016;154:597–605. doi: 10.1177/0194599815627667. [DOI] [PubMed] [Google Scholar]
- 5.Schick PM, Hieshima GB, White RA, et al. Arterial catheter embolization followed by surgery for large chemodectoma. Surgery. 1980;87:459–464. [PubMed] [Google Scholar]
- 6.Casasco A, Herbreteau D, Houdart E, George B, Tran Ba Huy P, Deffresne D, et al. Devascularization of craniofacial tumors by percutaneous tumor puncture. AJNR Am J Neuroradiol. 1994;15:1233–1239. [PMC free article] [PubMed] [Google Scholar]
- 7.Krishnamoorthy T, Gupta AK, Rajan JE, et al. Stroke from delayed embolization of polymerized glue following percutaneous direct injection of a carotid body tumor. Korean J Radiol. 2007;8:249–253. doi: 10.3348/kjr.2007.8.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ierardi AM. Glue or onyx: a guide to choice – tips and techniques. J Endovasc Resusc Trauma Manag. 2020;4:33–39. doi: 10.26676/jevtm.v4i1.114. [DOI] [Google Scholar]
- 9.Robertson V, Poli F, Hobson B, Saratzis A, Ross Naylor A. A systematic review and meta-analysis of the presentation and surgical management of patients with carotid body tumours. Eur J Vasc Endovasc Surg. 2019;57:477–486. doi: 10.1016/j.ejvs.2018.10.038. [DOI] [PubMed] [Google Scholar]
- 10.Garg T, Shrigiriwar A, Garg V. Pre-operative embolization for carotid body tumors. Br J Neurosurg. 2023;37:1425. doi: 10.1080/02688697.2021.1879012. [DOI] [PubMed] [Google Scholar]