Abstract
Background:
Although many studies have focused on the degenerative changes of the ulnohumeral and radiohumeral joints in osteoarthritis (OA) of the elbow, the proximal radioulnar joint (PRUJ), which facilitates the pronation and supination motions of the forearm, has not been comprehensively evaluated.
Purpose:
To assess the prevalence of PRUJ OA in patients diagnosed with OA of the elbow using computed tomography (CT) images and to establish an association between the CT findings and clinical manifestations.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Between 2010 and 2022, a total of 85 consecutive patients who were scheduled to undergo osteocapsular arthroplasty for OA of the elbow and had undergone preoperative CT imaging were included in the study. As a control group, 85 patients who underwent CT scans of the elbow for reasons other than OA of the elbow were selected and matched to patients in the OA group. CT findings of OA in the PRUJ, including osteophytes, joint space narrowing, subchondral cysts, and loose bodies, were evaluated. Inter- and intraobserver agreement analyses for CT findings were performed. The relationship between the CT findings of OA in the PRUJ and OA of the elbow classification systems (Broberg-Morrey, Hasting-Rettig, and Kwak) as well as clinical manifestations (range of motion [ROM], Mayo Elbow Performance Score, and visual analog scale for pain) were evaluated.
Results:
Patients in the OA group showed osteophytes in the radial notch (81.2%), osteophytes in the radial head (45.9%), joint space narrowing (54.1%), loose bodies (25.9%), and subchondral cysts (23.5%) involving the PRUJ. Both the interobserver (κ = 0.866) and intraobserver agreements (κ = 0.933) for CT findings of PRUJ OA were almost perfect. The CT findings of PRUJ OA were associated with the severity of OA of the elbow in Cochran-Armitage Trend analysis (with Brogberg-Morray, r = -2.624, P = .011; with Hasting-Rettig, r = -3.421, P = .002; with Kwak, r = -2.266, P = .032). The presence of radial notch osteophytes restricted ROM in the flexion-extension arc and pronation-supination arc (P = .009 and P < .001, respectively).
Conclusion:
PRUJ OA could be identified using CT imaging and showed radial notch osteophytes, joint space narrowing, loose bodies within the joint space, and subchondral cysts. PRUJ OA was related to overall OA of the elbow and may contribute to reduced ROM in the elbow joint. Therefore, preoperative evaluation of PRUJ OA can aid in the surgical planning of osteocapsular arthroplasty for OA of the elbow.
Keywords: computed tomography, elbow, imaging, osteoarthritis, pronation-supination, proximal radioulnar joint
Osteoarthritis (OA) of the elbow is a relatively rare condition compared to OA of other joints. The reported incidence of this condition is approximately 2%, and its development is typically associated with overuse of the upper extremities by individuals such as throwing athletes, manual laborers, and wheelchair users.10,13,20 Pain during terminal flexion and extension, along with a restricted range of motion (ROM) and difficulty in performing daily activities, are common complaints in individuals with symptomatic OA of the elbow.5,9
The proximal radioulnar joint (PRUJ), one of the joints that constitute the elbow, facilitates the pronation and supination motions of the forearm in coordination with the distal radioulnar joint.1,8,17,19,25,28 Past radiographic studies regarding characteristic radiographic features of OA include the formation of osteophytes, subchondral cysts, loose bodies in the joint space, and narrowing of the joint space and have mainly focused on the ulnohumeral and capituloradial joints in patients with OA of the elbow. ‖ To date, no radiographic study of OA in the PRUJ has been conducted. Therefore, the aim of the present study was to investigate the radiological characteristics of PRUJs in individuals with and without OA using computed tomography (CT) imaging. A secondary aim of the study was to evaluate the relationship between radiologic findings and existing systems for classifying OA of the elbow. We also assessed associations with clinical findings, including the visual analog scale for pain (VAS-P), the Mayo Elbow Performance Score (MEPS), and ROM measurements.
Methods
Patients and Evaluations
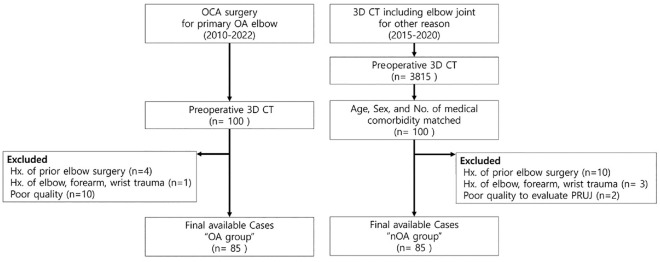
Our institutional review board approved the study protocol (approval No. 2022-1575). We identified 100 consecutive patients who underwent scheduled osteocapsular arthroplasty for primary OA (excluding secondary OA due to rheumatoid arthritis) of the elbow and who underwent preoperative CT imaging at our center between 2010 and 2022. Of the 100 patients, we excluded those with unsuitable imaging quality for PRUJ evaluation (n = 10), a history of elbow surgery (n = 4), or a history of trauma to the elbow, forearm, or wrist (n = 1). The remaining 85 patients were analyzed as the “OA group.” For the comparison of the radiologic features of arthritic and nonarthritic PRUJs on CT imaging, we also included patients who underwent upper extremity CT (including the elbow) for reasons other than OA of the elbow at our center between 2015 and 2020. Of them, 100 were matched with patients in the OA group based on age, sex, and medical comorbidities to minimize the influence of factors other than OA that could potentially impact the radiologic characteristics of the elbow. Of the 100 patients in the non-OA group, we excluded those who had a history of elbow surgery (n = 10) or trauma to the elbow, forearm, or wrist (n = 3), as well as those whose imaging quality was unsuitable for PRUJ evaluation (n = 2) (Figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart of the participants included in the study groups. 3D CT, 3-dimensional computed tomography; Hx, history; nOA, nonosteoarthritis; OA, osteoarthritis; OCA, osteocapsular arthroplasty; PRUJ, proximal radioulnar joint.
CT Features of PRUJ OA
CT imaging was performed using 3 CT machines (SOMATOM Definition AS, SOMATOM Definition AS+, and SOMATOM Definition Edge; Siemens Healthcare). The CT protocol included 120 kV, 305 to 373 mA, field of view of 160 to 219 mm, thickness acquisition of 1 mm, and 2-mm thickness overlapping reconstruction at intervals of 1.7 mm using the B30f reconstruction kernel.
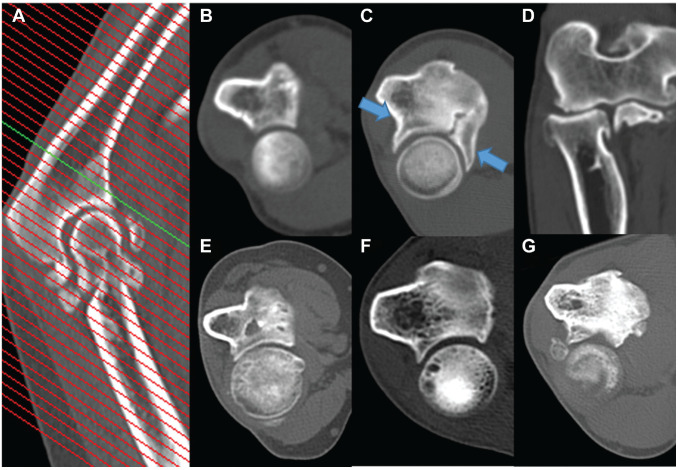
PRUJ OA was evaluated based on a middle axial view of the joint (Figure 2A). Radiological features, including osteophytes in the radial notch, joint space narrowing, subchondral cysts, and loose bodies in the joint space (Figure 2C, E -G), as well as radial head osteophytes in the coronal or sagittal plane (Figure 2D) were evaluated in both study groups. The frequency of radiological features was compared between the 2 groups. All radiological assessments were conducted by 2 orthopaedic surgeons (J.B.L. and H.B.) who had completed fellowships in shoulder and elbow surgery. Any disagreements were resolved through blind consensus. The PRUJ OA was determined by OA findings on the CT scans in the PRUJ.
Figure 2.
Radiologic features of proximal radioulnar joint (PRUJ) osteoarthritis on computed tomography images. (A) Level of the cut used to obtain a middle axial view of the PRUJ. (B) PRUJ without osteoarthritic change. (C) Radial notch osteophytes (blue arrows). (D) Radial head osteophyte in coronal view. (E) Joint space narrowing. (F) Subchondral cyst of the radial head. (G) Presence of a loose body.
Intra- and Interobserver Agreement Analyses
To evaluate the reliability of the PRUJ CT findings, intra- and interobserver reliability analyses were performed. Two investigators (J.B.L. and H.B.), who are orthopaedic surgeons with specialized training via shoulder and elbow fellowships, participated in the reproducibility assessment of PRUJ OA twice, with an interval of at least 4 weeks.
Association Between Radiologic OA of the Elbow and PRUJ OA
Anteroposterior and lateral radiographic views of the elbow were reviewed to classify PRUJ OA based on published classification systems.3,11,15 In the Broberg-Morrey (B-M) classification, grade 1 indicates slight joint space narrowing with minimal osteophyte formation, grade 2 indicates moderate joint space narrowing with moderate osteophyte formation, and grade 3 indicates severe degenerative change with significant joint destruction. In the Hasting-Rettig (H-R) classification, class 1 indicates degeneration in the margins of the ulnotrochlear joint, with the presence of coronoid and olecranon spurs and an absence of degenerative changes in the capituloradial joint; class 2 includes all the characteristics of class 1 and also involves joint space narrowing within the capituloradial joint, without radial head subluxation; and class 3 includes all the characteristics of class 2 and also involves capituloradial joint subluxation. For the Kwak classification, the middle of a sagittal CT image of the ulnotrochlear joint was used. In the Kwak system, grade 0 indicates the absence of osteophytes in the coronoid and olecranon fossae, grade 1 indicates the involvement of either the coronoid or the olecranon fossa, grade 2 indicates the involvement of both fossae, and grade 3 indicates joint space narrowing with or without fossae involvement. Associations between the different radiologic classifications of OA of the elbow were determined, along with the radiologic assessments of PRUJ OA.
Clinical Findings and PRUJ Radiologic Features
Patient information, such as age, sex, underlying disease, and history of previous surgeries, was collected by reviewing electronic medical records. Clinical data, including ROM, flexion-extension, pronation-supination measurements, VAS-P, and MEPS, were retrieved from medical records. A manual goniometer was used to evaluate the ROM for elbow flexion-extension. The elbow pronation-supination arc was measured using a manual goniometer with the elbow flexed at a 90° angle and the vertical stick grasped in hand. An independent examiner (S.P.S.) not involved in the study conducted the clinical assessments. Associations between the clinical findings (flexion-extension, pronation-supination, VAS-P, MEPS) and the CT-based radiologic findings (PRUJ OA features) were determined.
Statistical Analysis
Quantitative data are presented as mean values with standard deviations, while qualitative data are presented as numbers and frequencies. The measured parameters in the study groups were compared using the independent Student t test or the Mann–Whitney U test for continuous data and the chi-square or Fisher exact test for categorical data. A comparison of the OA classification between the OA group and non-OA group was carried out using the Fisher exact test, and comparison of the incidence CT findings between the OA and non-OA group was carried out using a chi-square test or Fisher exact test. Inter- and intraobserver reliability were evaluated using the Cohen kappa coefficient. Interpretation of the Cohen kappa was performed as described by Landis and Koch 16 : <0, no agreement; 0 to 0.20, slight agreement; 0.21 to 0.40, fair agreement; 0.41 to 0.60, moderate agreement; 0.60 to 0.80, substantial agreement; and 0.81 to 1, almost perfect agreement. A Cochran-Armitage trend analysis was conducted to examine the relationship between PRUJ OA CT findings and the severity of OA of the elbow assessed by previously published OA of the elbow classifications. A multiple linear regression test was performed to analyze the relationship between PRUJ OA CT findings and clinical manifestations. The significance level for all statistical tests was set at P < .05. All statistical analyses were conducted using SAS Version 9.4 (SAS Institute).
The OA group was analyzed to determine the association between the OA of the elbow classification determined through published methods and the observed PRUJ OA. In a second analysis, we evaluated the associations between the observed PRUJ OA and clinical findings, including the total range of flexion-extension, total range of pronation-supination, VAS-P, and MEPS.
Results
Of the 85 patients in the OA group (mean age, 56.8 ± 8.8 years), 69 (81.2%) were men. The patient characteristics are provided in Table 1.
Table 1.
Comparison of Clinical Findings in Patients With and Without Elbow OA a
| Characteristic | OA | Non-OA | P Value |
|---|---|---|---|
| Patients | 85 | 85 | — |
| Age, y | 56.8 ± 8.8 | 53.8 ± 10.2 | .832 |
| Men:women | 69:16 | 45:40 | .457 |
| Right:left elbow | 58:27 | 52:33 | .875 |
| Medical comorbidities | 15 (17.6) | 10 (11.8) | .731 |
| Elbow diagnosis | <.001 | ||
| OA of the elbow | 85 | 0 | |
| Humeral shaft fracture | 0 | 49 | |
| Humerus tumor | 0 | 36 | |
| OA of the elbow grade | |||
| B-M classification (0:1:2:3) | 0:18:47:20 | 85:0:0:0 | <.001 |
| H-R classification (0:1:2:3) | 0:11:24:50 | 85:0:0:0 | <.001 |
| Kwak classification (0:1:2:3) | 0:16:42:27 | 85:0:0:0 | <.001 |
Data are presented as n, n (%), or mean ± SD unless otherwise indicated. Boldface type indicates statistical significance. B-M, Broberg-Morrey; H-R, Hasting-Rettig; OA, osteoarthritis. Dash indicates not applicable.
CT Features of PRUJs in the OA and Non-OA Patient Groups
On CT images, 79 of 85 patients in the OA group and 12 of 85 patients in the non-OA group (92.9% vs 14.1%; P < .001) had PRUJ OA features. Radial notch osteophytes were the most common finding (81.2%), followed by joint space narrowing (54.1%), radial head osteophyte (45.9%), loose bodies in the joint space (25.9%), and subchondral cyst (23.5%) (Table 2).
Table 2.
Comparison of CT Findings of the PRUJ OA in Patients With and Without OA of the Elbow a
| Feature | OA (n = 85) | Non-OA (n = 85) | P Value |
|---|---|---|---|
| Any PRUJ OA feature | 79 (92.9) | 12 (14.1) | <.001 |
| Radial notch osteophyte | 69 (81.2) | 10 (11.8) | <.001 |
| Radial head osteophyte | 39 (45.9) | 0 (0) | <.001 |
| Joint space narrowing | 46 (54.1) | 3 (3.5) | <.001 |
| Subchondral cyst | 20 (23.5) | 1 (1.2) | <.001 |
| Loose bodies | 22 (25.9) | 0 (0) | <.001 |
Data are presented as n (%). Boldface P values indicate statistical significance. CT, computed tomography; OA, osteoarthritis; PRUJ, proximal radioulnar joint.
Intra- and Interobserver Agreement
The intraobserver agreement for the assessments of the radiographic features of PRUJ OA was almost perfect, with mean κ coefficients of 0.933 and 0.898 for the 2 investigators. The interobserver agreement was also excellent, with a mean κ coefficient of 0.866 (Table 3).
Table 3.
Intraobserver and Interobserver Agreement for CT Findings of PRUJ OA a
| Feature | Intraobserver (κ) | Interobserver (κ) | ||
|---|---|---|---|---|
| Any PRUJ OA | 0.933 | Almost perfect | 0.866 | Almost perfect |
| Radial notch osteophyte | 0.860 | Almost perfect | 0.849 | Almost perfect |
| Radial head osteophyte | 0.642 | Substantial | 0.811 | Almost perfect |
| Joint space narrowing | 0.761 | Substantial | 0.622 | Substantial |
| Subchondral cyst | 0.909 | Almost perfect | 0.804 | Almost perfect |
| Loose bodies | 0.849 | Almost perfect | 0.702 | Substantial |
CT, computed tomography; OA, osteoarthritis; PRUJ, proximal radioulnar joint.
Association Between OA of the Elbow Classification Systems and PRUJ OA
PRUJ OA features were related to the severity of OA of the elbow assessed by previously reported classifications (any PRUJ OA feature vs B-M, P = .011; vs H-R, P = .002; vs Kwak, P = .032). Radial notch osteophytes were significantly associated with the assessed B-M and Kwak classifications (P = .037 and P < .001, respectively). Radial head osteophytes were also significantly associated with all assessed OA of the elbow classifications (radial head osteophyte vs B-M, P < .001; vs H-R, P = .002; vs Kwak, P = .005). Joint space narrowing was significantly associated with all assessed OA of the elbow classifications (joint space narrowing vs B-M, P = .002; vs H-R, P = .047; vs Kwak, P = .031) (Table 4, Supplementary Figure 1).
Table 4.
Association of Radiologic Features with Assessments Based on Published Elbow OA Classification Systems a
| Feature | Statistical Test | Classification System | ||
|---|---|---|---|---|
| B-M | H-R | Kwak | ||
| Any PRUJ OA feature | Cochran-Armitage trend test | -2.624 | -3.421 | -2.266 |
| P value | .011 | .002 | .032 | |
| Radial notch osteophyte | Cochran-Armitage trend test | -2.232 | -2.081 | -3.598 |
| P value | .037 | .051 | <.001 | |
| Radial head osteophyte | Cochran-Armitage trend test | -3.883 | -3.159 | -2.851 |
| P value | <.001 | .002 | .005 | |
| Joint space narrowing | Cochran-Armitage trend test | -3.230 | -2.107 | -2.193 |
| P value | .002 | .047 | .031 | |
| Subchondral cyst | Cochran-Armitage trend test | -1.350 | -1.372 | -1.247 |
| P value | .189 | .213 | .275 | |
| Loose bodies | Cochran-Armitage trend test | -1.290 | -1.010 | -1.470 |
| P value | .268 | .389 | .161 | |
Boldface type indicates statistical significance. B-M, Broberg-Morrey; H-R, Hasting-Rettig; OA, osteoarthritis; PRUJ, proximal radioulnar joint.
Clinical Findings and PRUJ Radiologic Features
In patients with the radiologic features of PRUJ OA, the total arc of flexion-extension (P = .016) and the total arc of pronation-supination (P = .001) were reduced compared to those without such findings. Radial notch osteophytes were significantly associated with the total arc of flexion-extension (P = .009) and the total arc of pronation-supination (P < .001) (Table 5). In the multiple linear regression analysis, radial notch osteophyte was the only CT finding associated with the elbow flexion-extension (β = -11.276, SE = 4.620, P = .017). In addition, radial notch osteophyte was associated with elbow pronation-supination limitation (β = -34.1, SE = 4.95, P < .0001) (Table 6).
Table 5.
Comparison of ROM, VAS-P, and MEPS Between Patients a
| Radiologic Feature | + or − | Clinical Finding | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Flexion-Extension | P | Pronation-Supination | P | VAS-P | P | MEPS | P | ||
| Any PRUJ OA feature | + | 128.7 ± 16.2 | .016 | 136.4 ± 20.2 | .001 | 5.4 ± 1.7 | .950 | 63.9 ± 14.0 | .922 |
| − | 142.5 ± 9.9 | 170.0 ± 12.6 | 5.3 ± 2.3 | 63.3 ± 12.1 | |||||
| Radial notch osteophyte | + | 127.6 ± 16.1 | .009 | 132.5 ± 17.6 | <.001 | 5.3 ± 1.7 | .611 | 63.3 ± 13.7 | .465 |
| − | 138.8 ± 13.6 | 167.3 ± 14.4 | 5.6 ± 2.1 | 66.3 ± 14.7 | |||||
| Radial head osteophyte | + | 131.5 ± 16.5 | .341 | 141.6 ± 21.2 | .285 | 5.3 ± 1.7 | .665 | 64.6 ± 11.7 | .621 |
| − | 128.2 ± 15.9 | 136.5 ± 21.7 | 5.5 ± 1.8 | 63.2 ± 15.5 | |||||
| Joint space narrowing | + | 129.7 ± 16.5 | .984 | 137.0 ± 18.5 | .423 | 5.4 ± 1.7 | .926 | 64.6 ± 14.3 | .594 |
| − | 129.7 ± 16.0 | 140.9 ± 24.7 | 5.4 ± 1.9 | 62.9 ± 13.4 | |||||
| Subchondral cyst | + | 127.0 ± 15.5 | .385 | 137.3 ± 18.0 | .682 | 5.2 ± 1.8 | .645 | 60.0 ± 13.4 | .157 |
| − | 130.5 ± 16.4 | 139.3 ± 22.6 | 5.4 ± 1.8 | 65.0 ± 13.8 | |||||
| Loose bodies | + | 128.2 ± 13.7 | .573 | 139.3 ± 27.4 | .911 | 5.4 ± 1.9 | .949 | 65.0 ± 16.0 | .678 |
| − | 130.2 ± 17.0 | 138.6 ± 19.2 | 5.4 ± 1.7 | 63.4 ± 13.1 | |||||
Data are presented as mean ± SD unless otherwise indicated. Boldface type indicates statistical significance. MEPS, Mayo Elbow Performance Score; PRUJ, proximal radioulnar joint; ROM, range of motion; VAS-P, visual analog scale for pain.
Table 6.
Multiple Linear Regression Analysis of PRUJ OA Radiologic Features and Elbow ROM a
| Estimate (β) | Standard Error | P | ||
|---|---|---|---|---|
| Flexion-extension | Intercept | 140.17 | 4.361 | <.0001 |
| Radial notch osteophyte | -11.276 | 4.620 | .017 | |
| Radial head osteophyte | -3.4192 | 3.499 | .331 | |
| Joint space narrowing | 3.1714 | 3.649 | .387 | |
| Subchondral cyst | -2.9427 | 4.05 | .470 | |
| Loose bodies | -2.0364 | 3.986 | .610 | |
| Pronation-supination | Intercept | 166.92 | 4.67 | <.0001 |
| Radial notch osteophyte | -34.1 | 4.95 | <.0001 | |
| Radial head osteophyte | -5.0871 | 3.75 | .179 | |
| Joint space narrowing | 4.0402 | 3.91 | .305 | |
| Subchondral cyst | -0.5497 | 4.34 | .899 | |
| Loose bodies | 1.762 | 4.27 | .681 |
Boldface type indicates statistical significance. OA, osteoarthritis; PRUJ, proximal radioulnar joint; ROM, range of motion.
Discussion
To the best of our knowledge, the present study is the first to conduct a CT-based assessment of the radiological characteristics of PRUJ OA. CT imaging of PRUJs revealed radiologic findings of osteophyte formation, joint space narrowing, loose bodies in the joint space, and subchondral cysts, all indicative of OA. The prevalence of PRUJ OA increased with the severity of OA of the elbow. In addition, PRUJ OA was associated with limited elbow ROM, including flexion-extension and pronation-supination. The results of this study could provide guidance for clinical and radiological approaches to treating OA of the elbow with accompanying PRUJ OA.
OA occurs less frequently in the elbow than in any other joint.10,20 The majority of previous studies have focused on limitations in flexion-extension and pain during terminal flexion and extension.3,5,9,22 Given the frequent use of multiple electronic devices today, limitations in pronation-supination could significantly affect the quality of life. 12 In cases where there are limitations in pronation, compensatory movements of the shoulder joint may be necessary to use a keyboard at a desk.7,21,24 Limitations in supination could affect the use of smartphones.23,24 Thus, the finding of this study that PRUJ OA may increase the risk of limited pronation-supination is significant in the clinical assessment of patients with OA of the elbow.
In this study, radial notch osteophytes were the most common finding in PRUJ OA, followed by joint space narrowing, radial head osteophytes, loose bodies in the joint space, and subchondral cysts. These findings were significantly more prevalent in patients with than in those without OA of the elbow, indicating that degenerative changes in the PRUJ are associated with OA of the elbow. The significance of these differences suggests that the radiologic findings on CT imaging mentioned earlier may be specific to pathologic PRUJ OA. Our evaluation of the inter- and intraobserver reproducibility and reliability of PRUJ OA CT findings demonstrated almost perfect agreement.
The classification systems for OA of the elbow – B-M, H-R, and Kwak 15 – focus on the ulnohumeral and radiohumeral joints, which primarily affect the flexion-extension arc of the elbow. These classification systems are therefore limited in their ability to assess the state of PRUJ OA. In the present study, we observed that as the grade of OA of the elbow increases, the frequency of PRUJ OA also increases. Thus, as OA of the elbow progresses, the PRUJ, which is a component of the elbow joint, also undergoes degenerative changes. As a result, in advanced OA, the PRUJ OA status should be evaluated along with classification of OA of the elbow.
The results of the present study demonstrate that PRUJ OA can impact the arc of forearm pronation-supination. Radial notch and radial head osteophytes were found to be related. In a previous study on OA of the elbow, osteophytes were found to be the most significant factor associated with pain during terminal elbow motion and motion limitations.14,15 Radial notch osteophytes in PRUJ OA can affect the total pronation-supination arc. However, the mechanism behind the limitation of motion was not fully evaluated in this study. Further research on this topic could be valuable.
Our results suggest that PRUJ OA, especially with radial notch osteophytes, was related to a decrease in flexion-extension motion. However, it remains unclear whether this limitation in motion is a direct consequence of PRUJ OA or radial notch osteophytes or an indirect effect resulting from the overall status of OA of the elbow, particularly in the ulnohumeral joint. However, since joints are closely related to each other in every motion, it is impossible to evaluate them completely separately. Therefore, it should be considered that the analysis results related to motion associated with PRUJ OA may be related to overall OA of the elbow. In addition, future study on this topic is deemed necessary.
There was no difference in VAS-P and MEPS when comparing patients with and without PRUJ OA. Pain in the elbow of patients with OA is primarily reported during flexion and extension, with midrange pain occurring in the advanced stages of the disease. Although pronation-supination is often associated with pain, it appears to cause relatively minimal discomfort. MEPS is largely determined by the ROM of elbow flexion-extension and VAS-P. Therefore, in this study, the association between OA in the PRUJ and MEPS was limited. This implies that MEPS has limitations in assessing the degree of OA in the PRUJ or evaluating the limitation of pronation-supination in patients. Therefore, further research is needed on clinical scores for OA in the PRUJ and pronation-supination.
In this study, we observed a higher incidence of PRUJ OA in patients with advanced OA of the elbow. This finding emphasizes the importance of considering PRUJ OA during surgical planning for OA of the elbow. Although further studies are needed to fully understand the implications for patients with PRUJ OA in OA of the elbow, it is important to recognize that it may result in limitations in the pronation-supination arc. Therefore, clinicians should be aware of this possibility and conduct additional examinations for PRUJ OA during osteocapsular arthroplasty for OA of the elbow. In addition, bony spurs in PRUJ OA may restrict flexion and extension, which can be resolved by spur resection during osteocapsular arthroplasty to improve the flexion-extension arc. Further research is needed to determine the effects of osteophyte resection on PRUJ OA.
This study has several strengths. First, the CT findings for PRUJ OA are well described through clear imaging, with all radiologic assessments being supported by strong reproducibility and reliability analyses. Furthermore, it was demonstrated that the radiologic features of PRUJ OA are associated with existing OA of the elbow classifications. The presence of radiologic features of PRUJ OA restricts ROM. such as in the flexion-extension arc and pronation-supination arc.
However, the present study has some limitations. First, it was a retrospective study and the number of patients analyzed was relatively small, which limits the generalizability of our findings. Second, we were unable to account for selection bias in this study population. Moreover, the use of 3 different CT machines during the study period may have introduced a factor that could have affected the analysis of images due to potential variations in spatial resolution. This is a limitation inherent in retrospective studies. Conducting additional studies using a single CT machine could be helpful in addressing this limitation.
Conclusion
PRUJ OA could be identified using CT imaging, which can reveal specific findings such as radial notch osteophytes, joint space narrowing, loose bodies within the joint space, and subchondral cysts. PRUJ OA status was associated with the severity of OA of the elbow. PRUJ OA was associated with overall OA of the elbow and may contribute to reduced mobility in the elbow joint. Preoperative assessment of PRUJ OA can help determine the appropriate surgical plan.
Supplemental Material
Supplemental material, sj-docx-1-ojs-10.1177_23259671241255354 for Osteoarthritis of Proximal Radioulnar Joint: Computed Tomography–Based Assessment and Associations with Clinical Findings by Jun-Bum Lee, Hui Ben, Sang-Pil So, Hood Alsaqri, Hyun June Lee, Kyoung-Hwan Koh and In-Ho Jeon in The Orthopaedic Journal of Sports Medicine
Footnotes
Final revision submitted November 8, 2023; accepted December 5, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Asan Medical Center (ref No. 2022-1575).
ORCID iD: Kyoung-Hwan Koh  https://orcid.org/0000-0002-6181-9621
https://orcid.org/0000-0002-6181-9621
Supplemental Material: Supplemental Material for this article is available at https://journals.sagepub.com/doi/full/10.1177/23259671241255354#supplementary-materials.
References
- 1. Adams JE. Forearm instability: anatomy, biomechanics, and treatment options. J Hand Surg Am. 2017;42(1):47-52. [DOI] [PubMed] [Google Scholar]
- 2. Biswas D, Wysocki RW, Cohen MS. Primary and posttraumatic arthritis of the elbow. Arthritis. 2013;2013:473259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68(5):669-674. [PubMed] [Google Scholar]
- 4. Carlier Y, Desmoineaux P, Lenoir H, Vidil A. Prospective comparative analysis of arthroscopic debridement for primary and post-traumatic elbow osteoarthritis. Orthop Traumatol Surg Res. 2019;105(8S):S217-S220. [DOI] [PubMed] [Google Scholar]
- 5. Cheung EV, Adams R, Morrey BF. Primary osteoarthritis of the elbow: current treatment options. J Am Acad Orthop Surg. 2008;16(2):77-87. [DOI] [PubMed] [Google Scholar]
- 6. Dalal S, Bull M, Stanley D. Radiographic changes at the elbow in primary osteoarthritis: a comparison with normal aging of the elbow joint. J Shoulder Elbow Surg. 2007;16(3):358-361. [DOI] [PubMed] [Google Scholar]
- 7. DeDeugd CM, Shin AY, Shaughnessy WJ. Derotational pronation-producing osteotomy of the radius and biceps tendon rerouting for supination contractures in neonatal brachial plexus palsy patients: a review of 20 cases. J Pediatr Orthop. 2019;39(5):e366-e372. [DOI] [PubMed] [Google Scholar]
- 8. Ehman EC, Felmlee JP, Frick MA. Imaging of the proximal and distal radioulnar joints. Magn Reson Imaging Clin N Am. 2015;23(3):417-425. [DOI] [PubMed] [Google Scholar]
- 9. Galle SE, Beck JD, Burchette RJ, Harness NG. Outcomes of elbow arthroscopic osteocapsular arthroplasty. J Hand Surg. 2016;41(2):184-191. [DOI] [PubMed] [Google Scholar]
- 10. Gramstad GD, Galatz LM. Management of elbow osteoarthritis. J Bone Joint Surg Am. 2006;88(2):421-430. [DOI] [PubMed] [Google Scholar]
- 11. Hart DJ, Spector TD. The classification and assessment of osteoarthritis. Baillieres Clin Rheumatol. 1995;9(2):407-432. [DOI] [PubMed] [Google Scholar]
- 12. Haverstock JP, King GJW, Athwal GS, Johnson JA, Langohr GDG. Elbow motion patterns during daily activity. J Shoulder Elbow Surg. 2020;29(10):2007-2014. [DOI] [PubMed] [Google Scholar]
- 13. Kroonen LT, Piper SL, Ghatan AC. Arthroscopic management of elbow osteoarthritis. J Hand Surg. 2017;42(8):640-650. [DOI] [PubMed] [Google Scholar]
- 14. Kwak JM, Kholinne E, Sun Y, et al. Clinical outcome of osteocapsular arthroplasty for primary osteoarthritis of the elbow: comparison of arthroscopic and open procedure. Arthroscopy. 2019;35(4):1083-1089. [DOI] [PubMed] [Google Scholar]
- 15. Kwak JM, Kim H, Sun Y, et al. Arthroscopic osteocapsular arthroplasty for advanced-stage primary osteoarthritis of the elbow using a computed tomography-based classification. J Shoulder Elbow Surg. 2020;29(5):989-995. [DOI] [PubMed] [Google Scholar]
- 16. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. [PubMed] [Google Scholar]
- 17. Lees VC. The functional anatomy of forearm rotation. J Hand Microsurg. 2009;1(2):92-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lim YW, van Riet RP, Mittal R, Bain GI. Pattern of osteophyte distribution in primary osteoarthritis of the elbow. J Shoulder Elbow Surg. 2008;17(6):963-966. [DOI] [PubMed] [Google Scholar]
- 19. Malone PS, Shaw OG, Lees VC. Anatomic relationships of the distal and proximal radioulnar joints articulating surface areas and of the radius and ulna bone volumes - implications for biomechanical studies of the distal and proximal radioulnar joints and forearm bones. Front Bioeng Biotechnol. 2016;4:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Papatheodorou LK, Baratz ME, Sotereanos DG. Elbow arthritis: current concepts. J Hand Surg. 2013;38(3):605-613. [DOI] [PubMed] [Google Scholar]
- 21. Pottorf OA, Lee DJ, Czujko PN. Reliability and concurrent validity of mobile health technology for patient self-monitoring in physical rehabilitation. JSES Int. 2022;6(3):506-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rettig LA, Hastings H II, Feinberg JR. Primary osteoarthritis of the elbow: lack of radiographic evidence for morphologic predisposition, results of operative debridement at intermediate follow-up, and basis for a new radiographic classification system. J Shoulder Elbow Surg. 2008;17(1):97-105. [DOI] [PubMed] [Google Scholar]
- 23. Santos C, Pauchard N, Guilloteau A. Reliability assessment of measuring active wrist pronation and supination range of motion with a smartphone. Hand Surg Rehabil. 2017;36(5):338-345. [DOI] [PubMed] [Google Scholar]
- 24. Sardelli M, Tashjian RZ, MacWilliams BA. Functional elbow range of motion for contemporary tasks. J Bone Joint Surg Am. 2011;93(5):471-477. [DOI] [PubMed] [Google Scholar]
- 25. Soubeyrand M, Assabah B, Bégin M, et al. Pronation and supination of the hand: anatomy and biomechanics. Hand Surg Rehabil. 2017;36(1):2-11. [DOI] [PubMed] [Google Scholar]
- 26. Turmezei TD, Treece GM, Gee AH, Fotiadou AF, Poole KE. Quantitative 3D analysis of bone in hip osteoarthritis using clinical computed tomography. Eur Radiol. 2016;26(7):2047-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wysocki RW, Cohen MS. Primary osteoarthritis and posttraumatic arthritis of the elbow. Hand Clin. 2011;27(2):131-137, v. [DOI] [PubMed] [Google Scholar]
- 28. Xiao K, Zhang J, Li T, Dong YL, Weng XS. Anatomy, definition, and treatment of the “terrible triad of the elbow” and contemplation of the rationality of this designation. Orthop Surg. 2015;7(1):13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ojs-10.1177_23259671241255354 for Osteoarthritis of Proximal Radioulnar Joint: Computed Tomography–Based Assessment and Associations with Clinical Findings by Jun-Bum Lee, Hui Ben, Sang-Pil So, Hood Alsaqri, Hyun June Lee, Kyoung-Hwan Koh and In-Ho Jeon in The Orthopaedic Journal of Sports Medicine