Abstract
Objective
Despite growing numbers of initiatives designed to address increasing diabetes prevalence in the U.S., the need remains for effective programs. Because family history is a diabetes risk factor, family focused programs may be a potential strategy to improve the health of the entire family. We present the development process and pretest results of a lifestyle change program for rural-dwelling mothers at risk for diabetes and their children.
Methods
We completed semistructured interviews with mothers (N = 17) focusing on program content and activities. Findings informed program development by identifying specific barriers motivators and potential leverage points such as focusing on the intrinsic incentives of health activities. The resulting program was pretested with rural-dwelling mothers (N = 5) who completed program activities with their families and provided feedback via semistructured interviews. All interviews were audio-recorded, transcribed, and analyzed using thematic analysis.
Results
While pretest results showed that the program was generally acceptable and feasible, feedback was used to further refine the program. The revised program consists of 8 group sessions with family focused content around physical activity, healthy eating, and making connections while engaging in health activities. Between sessions, mothers tracked the family goals, activity levels, and mood, and documented barriers to discuss during the sessions.
Conclusions
Our development process engaged intended program users to codesign a program that focuses on wellness and intrinsic incentives of engaging in health-enhancing activities as a family. By providing strategies to change behaviors as a family, this program aims to improve the mother's health while developing healthy habits in their children.
Keywords: formative evaluation, health promotion, lifestyle change, program development, rural health
Diabetes is an ongoing public health issue that negatively impacts multiple dimensions of health. 1 As of 2021, approximately 11% of the U.S. population lives with type 2 diabetes (T2DM). 2 Furthermore, rates of T2DM in youth continue to rise.2‐4 This is concerning as T2DM onset earlier in life is associated with greater mortality, more severe complications, and a higher risk for cardiovascular disease (CVD) in adulthood.5,6
Despite the number of initiatives addressing T2DM, efforts to reduce modifiable risk factors, such as obesity, have been largely ineffective. 7 A report regarding youth-onset T2DM noted that individual-level interventions are unable to address the complexity of family dynamics and environmental factors that influence behaviors.8,9 However, there is limited data on effective and sustainable strategies to engage families in changing children's behaviors, although studies suggest that strategies with indirect engagement (ie, sending information) are less effective than strategies requiring direct engagement (ie, facilitating supportive environments).10‐12 Moreover, parents play a critical role in developing youth health beliefs and behaviors.13,14 Behavior change in adult family members with diabetes can have positive effects on the entire household. 15 For adults, family support is equally important in successfully engaging in self-management activities. 16
Furthermore, families in rural communities are often in geographically and socially isolated areas with fewer health resources compared to nonrural areas.17,18 Significant disparities in diabetes risk factors prevalence and access to screening and treatment persist in rural communities. 19 And, the need remains to better understand how health decisions are impacted by sociocultural and physical environments of rural communities to improve the feasibility and acceptability of health promotion efforts.20‐22
These reasons highlight the need for diabetes prevention efforts designed for rural communities. Because family history is a risk factor for T2DM,23,24 family focused programs may be a strategy to improve health outcomes for the entire family.25,26 Therefore, in this report, we present the development process and pretest results of a lifestyle change program focusing on improving self-care activities in rural-dwelling mothers at risk for diabetes and developing healthy habits in their children.
Methods
This report follows guidelines outlined by the Standards for Reporting Qualitative Research. 27 The university institutional review board approved all study activities.
Formative Work to Develop the Initial Program
Community need for lifestyle change programs that focused on diabetes prevention was identified during the development of a separate T2DM self-management program for adults in rural Alabama.28,29 To better understand this need, discussion groups were completed with rural-dwelling adults with diabetes and children with a parent with diabetes. While findings were presented elsewhere,30,31 briefly, the results showed that an individual's diabetes management often impacted their family emotionally and in activities of daily living. Youth discussions highlighted parental modeling as an important source of health learning. For example, youth reported that they had never spoken directly to their parents about diabetes and had learned about diabetes by watching family members manage their condition. Finally, there was an interest in T2DM prevention programs that included younger family members. The results of this work, completed between 2016 and 2018, were combined with a review of the literature to inform the initial draft of the program.
In 2018, the project moved to Wisconsin. While many rural residents report similar health barriers such as access to fewer opportunities and resources, challenges around caregiving, and the lack of time and energy, research shows that individual rural communities are distinct and impacted differently by determinants of health.21,32 Likewise, significant sociodemographic differences exist between rural Alabama and Wisconsin. Thus, we completed semistructured interviews with rural-dwelling Wisconsin mothers that explored the feasibility and acceptability of the draft program content, materials, and activities.
Caregiver Semistructured Interview Recruitment, Enrollment, and Data Collection
Semistructured telephone interviews were completed during April–August 2021. Eligible participants were adults, primary caregivers of children living in the home, and willing to participate in telephone interviews. Participants were recruited from the Survey of the Health of Wisconsin, a representative cohort of Wisconsin.33,34 Recruitment letters were mailed to rural-dwelling participants as defined by the 2010 Census Urban and Rural Classification. 35 Participants received $20 for participation in these interviews.
Informed consent was completed before the interview. Interviews lasted an average of 45 min. An interviewer guide structured using constructs of social cognitive theory (SCT)36,37 and self-determination theory (SDT)38,39 was used to maintain consistency over the interviews. Interviews began with a discussion of a common definition of family health and leisure-time physical activity. Interviews then explored factors that influenced the participants and their family's decisions to engage or not engage in health-enhancing behaviors, including motivations, barriers and facilitators, behavioral capability and efficacy, and social support and norms. Interviews concluded with a discussion around activities and supports that would be important to include in a lifestyle change program.
After each interview, the interviewer completed field notes and a debriefing meeting to reflect on the interview's tone, flow, and emerging findings. 40 Interviews were audio-recorded and transcribed verbatim. Transcriptions were checked for accuracy by comparing the transcript to the audio recordings and de-identified.
Coding occurred concurrently as the interviews were being conducted by SA and research assistants in teams of 3 using thematic analysis. 41 Data were organized in NVivo 12. 42 A coding team (SA and a research assistant) developed the initial codes and definitions by working independently to code the first 2 transcripts. The team then met to discuss the codes and definitions. Any differences were reviewed and resolved through group consensus. This codebook was used to code the remaining transcripts. The remaining transcripts were analyzed by coding teams of 2 coders. After independently coding each transcript, the 2 coders met to review the application of codes. Reliability was assessed during the meetings by identifying coding discrepancies. Disagreements were discussed as a team and a group consensus was reached by the coders in consultation with a third coder. After the meetings, the codebook was updated, and recoding was performed to ensure consistent application of the codes.
The coded data were reviewed to identify patterns, similarities, and differences. 41 Codes were grouped into broad categories that reflected a common idea or similar phenomena. Themes were defined, and example quotes were selected. Multiple independent coders were used to ensure consistent application of codes 43 and an audit trail tracked the coding process. 44
Integration of Semistructured Interview Findings Into the Program
Results of the semistructured interviews were used to further develop the program, particularly highlighting the importance of focusing on the intrinsic incentive of activities. Thus, messaging focused on the positive consequences and immediate benefits of health actions. Discussion prompts used during sessions focused on barriers, facilitators, and motivators identified during the interviews. Finally, feedback regarding session formats and data collection procedures was integrated into the study protocols. With program materials in advanced draft stages, we conducted a pretest to obtain feedback on the protocols and key program materials, messages, and activities. 45
Program Pretest Recruitment, Data Collection, and Study Measures
Pretest activities were completed during the summer of 2022. Eligible participants were primary caregivers of a child and had a family history of T2DM. Participants were recruited using chain-referral sampling where enrolled participants were asked to refer potential participants within their social networks. Enrolled participants completed 2 study visits and pretest activities. Participants received $40 for study participation. While the primary outcomes for the pretest were program acceptability and feasibility obtained using semistructured interviews, measures were included that may be used to assess program effectiveness in subsequent evaluations such as physical activity, 46 social support, 47 exercise self-regulation, 48 and perceived stress. 49 Semistructured interviews also included discussions around the acceptability of the selected measures.
Descriptive analysis was conducted by creating frequency distributions of categorical variables and means and standard deviations of continuous variables. Semistructured interviews were audio-recorded, and summary reports of program feasibility and acceptability were generated based on recurring themes found in the transcripts by using a similar process as described above.
Study Visits and Pretest Activities
At the first study visit, participants met with study staff to complete assessments and to review program content and materials. After this visit, participants were asked to complete program activities with their families and to note their experiences over 3 weeks. Participants also tracked their family's physical activity levels, mood, and the number of program activities completed each day. Then, a second visit was completed during which semistructured interviews were conducted to better understand participant experiences around completing the program activities and using the materials, focusing on readability, appropriateness, attractiveness, enjoyment, and helpfulness of the activities.45,50
Results
Results of the Caregiver Semistructured Interviews
Semistructured interview participants (N = 17) had an average of 2 children in the home (range = 1–5), were white, and on average 41 years old (SD = 7.4). Most had graduated from college (14, 82%), annual income of $40 000 (12, 71%), married (13, 77%), and employed full or part-time (14, 82%). Mothers discussed their motivations and challenges around engaging in health behaviors as a family and the acceptability of program components. Participants identified several leverage points that could potentially be used to develop strategies to enable physical activity participation as a family. Participants discussed their preference for engaging in physical activities as a family, even though this was often logistically challenging. A significant barrier was identifying enjoyable and age-appropriate activities for all family members. However, mothers wanted to develop healthy habits in their children, and being active together provided this opportunity. Moreover, mothers noted that spending family time to be physically active would potentially overcome other barriers such as not having enough time for exercise.
When asked about past experiences of being physically active as a family, mothers focused on positive, enjoyable social interactions. Although organizing family time often took additional effort, enjoying being together helped motivate them. In addition, participants discussed barriers such as lack of time, stress from school or work, and lack of resources. Mothers discussed preference for activities such as walking that were low cost, not requiring equipment or training, and easy for different skills and fitness levels. Furthermore, mothers noted that a positive of engaging their children was that they often encouraged new or different activities as a family. Finally, mothers discussed the tendency of caregivers to prioritize their own health below their family's health. Thus, participants wanted strategies to help balance family time with time for self-care. Table 1 provides a summary of key findings that informed program development.
Table 1.
Summary of Semistructured Interview Findings.
| Participating in physical activity as a family |
|
| Barriers for participants as a family |
|
Results of the Pretest
Pretest participants were on average 41 (SD = 8.0) years old, graduated from college, married, employed part- or full-time, had an income >$40,000, and on average 2 children at home. Three participants reported meeting weekly activity levels of 150 min and all reported low perceived stress levels (Table 2).
Table 2.
Pretest Participant Characteristics.
| Characteristic | N = 5 |
|---|---|
| Mothers age, mean ± SD | 41.4 ± 8.0 |
| Education (n, %) | |
| College graduate | 5 |
| Income (n) | |
| 40 000 or greater | 5 |
| Employment (n) | |
| Full-time | 3 |
| Part-time | 2 |
| Marital status (n) | |
| Married | 5 |
| Number of children in the home, mean ± SD | 2.4 ± 1.14 |
| Physical activity levels1 (n) | |
| Inactive | 2 |
| Minimally active | 2 |
| Highly active | 1 |
| Perceived stress,2 mean ± SD | 12.7 ± 0.9 |
IPAQ-categorical scores: inactive, minimally active (achieves minimum recommended levels), and highly active (exceeds minimum physical activity recommendations).
Perceived stress scale, range 0–40, high scores mean higher perceived stress.
Overall, the pretest semistructured interviews showed that the program components were acceptable and feasible with families completing and enjoying most activities. One participant described,
…[the] program was nice because it gave us more fun things to do. Like the kids, they're not always excited. When we make them go out, [laughs] they're like, we already went outside today? But, I think, they were actually exercising. It was actually really fun to do as a family.
Participants liked that program activities were developed to be adaptable to better fit into families’ daily routines,
…a couple of days, we kind of added our own things to do…it was fun ideas. And I felt like it was a nice way to work on the emotional aspect of the family, you know? Like the connection side of things. So, I think that was like, an unexpected bonus where [it] gave us a reason and ideas, something to talk about, something to do.
Additionally, participants gave feedback on how they modified specific activities to be age-appropriate for younger versus older children.
Moreover, participants noted that in addition to the physical activity, an unexpected positive was the emotional connections made during the activities,
…it was somewhat folded into the regular routine and then a little bit [more]. To me, it was more of the emotional connection. A little bit more [of a] focus on doing the activity with the kids, rather than just mindlessly walking along to try to get to the next stop, to get to the next thing. It caused me…to slow down a little bit and think about spending the time.
Based on pretest results, revisions were made to make the materials more usable, incorporated activity modification suggestions, and added new activity ideas. Short videos with key health information were added so mothers could revisit them as needed. Session discussion prompts were revised to include additional barriers, a sleep health session was added, and an asset mapping activity was added to help identify local resources.
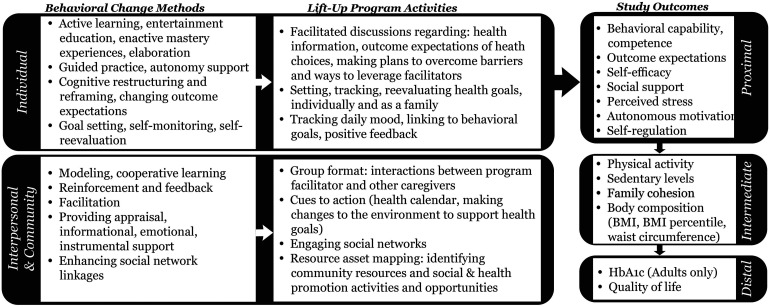
The final program consists of 8 group sessions with topics including physical activity basics and benefits, reducing sedentary behaviors, healthy eating, and sleep health. Figure 1 presents our intervention's proposed conceptual framework including behavioral change methods based on SCT and SDT, practical application of the methods, and study outcomes.
Figure 1.
Intervention conceptual framework.
Participants receive an activity book and a family health calendar. The 3-month program consists of an intensive phase of 4 weekly 30 min sessions followed by maintenance-focused sessions meeting bi-weekly and then monthly. During the intensive phase, families watch a health education video. Sessions then reinforce the video content using discussions and activities. Participants set and then reevaluate individual and family goals to improve physical activity, sedentary levels, and healthy eating. The activity book contains 3 types of games based on physical activity, healthy eating, and connecting and talking. Between sessions, families use a health calendar to track goals, activity levels, and moods, and to document barriers and facilitators. The calendar will be reviewed during sessions to emphasize the impact of health actions on changes in wellness, mood, and anxiety or stress levels.
Discussion
T2DM prevention programs often focus on supporting individuals in making behavior changes. However, individual-level health programs often do not fully address the complexity of family dynamics and environmental factors that influence behaviors. 9 Because family history is a T2DM risk factor, engaging the family in these efforts is a potentially cost-efficient strategy to improve the health of the entire family.51,52 Our intervention development process engaged intended program users to codesign a family centered lifestyle change program. The resulting program focuses on health, wellness, and intrinsic incentives of engaging in health-enhancing activities as a family.
During program development, we found that youth who have family members with T2DM had some awareness and knowledge of T2DM even without explicit education. And like previous studies, we found that parental modeling is a significant source of health learning.53,54 Previous studies have found that youth and their families with higher T2DM risk often lack knowledge regarding risk and prevention. 55 This is true for other chronic conditions such as CVD. A survey of high school students found they lacked knowledge of CVD and had low levels of perceived susceptibility to CVD. 56 Early interventions for at-risk children built behavioral capacity, boosted confidence, and improved health outcomes. 57 For example, Melnyk et al 57 found that youth who had higher self-esteem and stronger beliefs about their ability to engage in healthy behaviors made healthier choices. Furthermore, health behaviors developed early in life are often associated with behaviors in adulthood.58,59
Finally, behaviors are more likely to be sustained if they are self-regulated and motivated by intrinsic incentives driven by enjoyment and interest. 60 Similarly, our study participants prioritized activities that enabled family members to make meaningful connections and learn about each other's motivations while meeting health goals. Thus, our program included activities that facilitated reframing physical activity requirements as an opportunity to connect with family by incorporating active times into the family's daily routines.
This study had several limitations including a small sample size and the use of convenience sampling for recruitment. Enrolled mothers had higher education and income levels compared to rural Wisconsin communities. Therefore, additional community-specific tailoring may be needed for future program implementation. Furthermore, because of the nature of qualitative data, our findings are not generalizable. Rather, the experiences shared by our participants may represent the experiences of other community members in similar contexts. Despite these limitations, this study engaged intended program users to guide program development and to provide insights into the feasibility and acceptability of the lifestyle change program. These insights will support the next phase of this study to evaluate the impact of the program on health outcomes.
Conclusions
In collaboration with intended program users, our team developed and pretested a program for mothers and children with a family history of T2DM. Better understanding the factors that impact families in engaging in physical activity and other health-enhancing behaviors can help identify feasible strategies that support behavior change as a family. A family centered program that focuses both on the children and mothers has the potential to impact not only the health habits of youth at higher risk for developing T2DM but also improve outcomes in adults.
Acknowledgments
Thank you to the participants who volunteered for this research and the graduate and undergraduate student researchers who contributed to this study. The authors would also like to thank the University of Wisconsin Survey Center, SHOW administrative, field, and scientific staff, as well as all the SHOW participants for their contributions to this study.
Author Biographies
Susan J. Andreae is an assistant professor in the Department of Kinesiology, University of Wisconsin-Madison.
Anna Lindberg is an undergraduate student researcher in the Department of Kinesiology, University of Wisconsin-Madison.
Thomas Casey is a graduate student researcher in the Department of Kinesiology, University of Wisconsin-Madison.
Kristen A. Pickett is an associate professor in the Program in Occupational Therapy in the Department of Kinesiology, University of Wisconsin-Madison.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval: The study was reviewed and approved by the Institutional Review Board at the University of Wisconsin-Madison (2019-0556).
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported in part by the Virginia Horne Henry Fund for Women's Physical Education, School of Education, UW-Madison, University of Wisconsin-Madison, Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation (WARF), and the Eunice Kennedy Shriver National Institute of Child Health & Human Development, the Office of Research on Women's Health, Building Interdisciplinary Research Careers in Women's Health (BIRCWH) program, the Office of The Director, National Institutes of Health and the National Cancer Institute, under Award Number K12HD101368. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Funding for the Survey of the Health of Wisconsin (SHOW) was provided by the Wisconsin Partnership Program PERC Award (No. AAL2297).
ORCID iD: Susan J. Andreae https://orcid.org/0000-0002-1336-7720
Data Availability Statement: The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
- 1.American Diabetes A. Economic costs of diabetes in the U.S. In 2017. Diabetes Care. 2018;41(5):917‐928. doi: 10.2337/dci18-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Diabetes Statistics Report. CDC, National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. Updated May 15, 2024. Accessed July 26, 2024. https://www.cdc.gov/diabetes/php/data-research/index.html
- 3.Imperatore G, Boyle JP, Thompson TJ, et al. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35(12):2515‐2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778‐1786. doi: 10.1001/jama.2014.3201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Constantino MI, Molyneaux L, Limacher-Gisler F, et al. Long-term complications and mortality in young-onset diabetes: type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care. 2013;36(12):3863‐3869. doi: 10.2337/dc12-2455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viigimaa M, Sachinidis A, Toumpourleka M, Koutsampasopoulos K, Alliksoo S, Titma T. Macrovascular complications of type 2 diabetes Mellitus. Curr Vasc Pharmacol. 2020;18(2):110‐116. doi: 10.2174/1570161117666190405165151 [DOI] [PubMed] [Google Scholar]
- 7.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3). doi: 10.1542/peds.2017-3459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nadeau KJ, Anderson BJ, Berg EG, et al. Youth-onset type 2 diabetes consensus report: current status, challenges, and priorities. Diabetes Care. 2016;39(9):1635‐1642. doi: 10.2337/dc16-1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ball K, Carver A, Downing K, Jackson M, O'Rourke K. Addressing the social determinants of inequities in physical activity and sedentary behaviours. Health Promot Int. 2015;30(Suppl 2):ii8-. doi: 10.1093/heapro/dav022 [DOI] [PubMed] [Google Scholar]
- 10.Schlechter CR, Rosenkranz RR, Guagliano JM, Dzewaltowski DA. A systematic review of children's dietary interventions with parents as change agents: Application of the RE-AIM framework. Prev Med. 2016;91:233‐243. doi: 10.1016/j.ypmed.2016.08.030 [DOI] [PubMed] [Google Scholar]
- 11.Park J, Woo S, Ju YS, et al. Factors associated with dropout in a lifestyle modification program for weight management in children and adolescents. Obes Res Clin Pract. 2020;14(6):566‐572. doi: 10.1016/j.orcp.2020.09.002 [DOI] [PubMed] [Google Scholar]
- 12.Schmied EA, Madanat H, Chuang E, et al. Factors predicting parent engagement in a family-based childhood obesity prevention and control program. BMC Public Health. 2023;23(1):457. doi: 10.1186/s12889-023-15359-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lau RR, Quadrel MJ, Hartman KA. Development and change of young adults’ preventive health beliefs and behavior: Influence from parents and peers. J Health Soc Behav. 1990;31(3):240‐259. [PubMed] [Google Scholar]
- 14.Hesketh KR, Goodfellow L, Ekelund U, et al. Activity levels in mothers and their preschool children. Pediatrics. 2014;133(4):e973‐e980. doi: 10.1542/peds.2013-3153 [DOI] [PubMed] [Google Scholar]
- 15.Laroche HH, Heisler M, Forman J, Anderson M, Davis MM. When adults with diabetes attempt to drink less soda: Resulting adult-child interactions and household changes. J Natl Med Assoc. 2008;100(9):1004‐1011. [DOI] [PubMed] [Google Scholar]
- 16.Pamungkas RA, Chamroonsawasdi K, Vatanasomboon P. A systematic review: family support integrated with diabetes self-management among uncontrolled type II diabetes Mellitus patients. Behav Sci (Basel). 2017;7(3):62. doi: 10.3390/bs7030062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia MC, Faul M, Massetti G, et al. Reducing potentially excess deaths from the five leading causes of death in the rural United States. MMWR Surveill Summ. 2017;66(2):1‐7. doi: 10.15585/mmwr.ss6602a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holmes M, Thompson KW. Risk factors and potentially preventable deaths in rural communities. In: NC rural health research program. Cecil G. Sheps Center for Health Services Research, UNC-CH; 2019: 2-4 [Google Scholar]
- 19.Dugani SB, Wood-Wentz CM, Mielke MM, Bailey KR, Vella A. Assessment of disparities in diabetes mortality in adults in US rural vs nonrural counties, 1999-2018. JAMA Netw Open. 2022;5(9):e2232318. doi: 10.1001/jamanetworkopen.2022.32318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frost SS, Goins RT, Hunter RH, et al. Effects of the built environment on physical activity of adults living in rural settings. Am J Health Promot. 2010;24(4):267‐283. doi: 10.4278/ajhp.08040532 [DOI] [PubMed] [Google Scholar]
- 21.Whitfield GP, Carlson SA, Ussery EN, Watson KB, Berrigan D, Fulton JE. National-level environmental perceptions and walking among urban and rural residents: informing surveillance of walkability. Prev Med. 2019;123:101‐108. doi: 10.1016/j.ypmed.2019.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosputni C, Short E, Rahim-Sepulveda M, et al. Diabetes prevention programs in rural North America: a systematic scoping review. Curr Diab Rep. 2019;19(7):43. doi: 10.1007/s11892-019-1160-3 [DOI] [PubMed] [Google Scholar]
- 23.Moonesinghe R, Beckles GLA, Liu T, Khoury MJ. The contribution of family history to the burden of diagnosed diabetes, undiagnosed diabetes, and prediabetes in the United States: analysis of the national health and nutrition examination survey, 2009–2014. Genet Med. 2018;20(10):1159‐1166. doi: 10.1038/gim.2017.238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papazafiropoulou AK, Papanas N, Melidonis A, Maltezos E. Family history of type 2 diabetes: does having a diabetic parent increase the risk? Curr Diabetes Rev. 2017;13(1):19‐25. doi: 10.2174/1573399812666151022143502 [DOI] [PubMed] [Google Scholar]
- 25.Smith J, Ali P, Birks Y, et al. Umbrella review of family-focused care interventions supporting families where a family member has a long-term condition. J Adv Nurs. 2020;76(8):1911‐1923. doi: 10.1111/jan.14367 [DOI] [PubMed] [Google Scholar]
- 26.Nur A, Chua JYX, Shorey S. Effectiveness of community-based family-focused interventions on family functioning among families of children with chronic health conditions: a systematic review and meta-analysis. Fam Process. 2023;62(4):1408‐1422. doi: 10.1111/famp.12930 [DOI] [PubMed] [Google Scholar]
- 27.O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245‐1251. doi: 10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- 28.Andreae SJ, Andreae LJ, Cherrington AL, et al. Peer coach delivered storytelling program improved diabetes medication adherence: a cluster randomized trial. Contemp Clin Trials. 2021;104:106358. doi: 10.1016/j.cct.2021.106358 [DOI] [PubMed] [Google Scholar]
- 29.Andreae SJ, Andreae LJ, Cherrington A, Richman J, Safford M. Peer coach delivered storytelling program for diabetes medication adherence: intervention development and process outcomes. Contemp Clin Trials Commun. 2020;20:100653. doi: 10.1016/j.conctc.2020.100653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khodadadi A, Andreae S, Cherrington A. Assessing community members’ preferences of a family-based diabetes prevention program in rural Alabama. Ann Behav Med. 2017;51(suppl_1):s120. doi: 10.1007/s12160-017-9903-3 [DOI] [Google Scholar]
- 31.Andreae S, Andreae L, Safford M, Dutton G, Davies S, Cherrington A. Assessing youth perceptions and awareness of diabetes in rural Alabama. APHA; 2017:
- 32.Peterson J, Schmer C, Ward-Smith P. Perceptions of Midwest rural women related to their physical activity and eating behaviors. J Community Health Nurs. 2013;30(2):72‐82. doi: 10.1080/07370016.2013.778722 [DOI] [PubMed] [Google Scholar]
- 33.Malecki KMC, Nikodemova M, Schultz AA, et al. The survey of the health of Wisconsin (SHOW) program: an infrastructure for advancing population health. Front Public Health. 2022;10:818777. doi: 10.3389/fpubh.2022.818777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nieto FJ, Peppard PE, Engelman CD, et al. The survey of the health of Wisconsin (SHOW), a novel infrastructure for population health research: rationale and methods. BMC Public Health. 2010;10:785. doi: 10.1186/1471-2458-10-785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.United States Census Bureau. 2010 census urban and rural classification and urban area criteria. U.S. Department of Commerce. Updated October 28, 2021. Accessed December 18, 2023. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html
- 36.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191‐215. doi: 10.1037//0033-295x.84.2.191 [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143‐164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 38.Ng JY, Ntoumanis N, Thogersen-Ntoumani C, et al. Self-determination theory applied to health contexts: a meta-analysis. Perspect Psychol Sci. 2012;7(4):325‐340. doi: 10.1177/1745691612447309 [DOI] [PubMed] [Google Scholar]
- 39.Deci EL, Ryan RM. The “what” and “why” of goal pursuits: human needs and the self-determination of behavior. Psychol Inq. 2000;11(4):227‐268. doi: 10.1207/S15327965PLI1104_01 [DOI] [Google Scholar]
- 40.McMahon SA, Winch PJ. Systematic debriefing after qualitative encounters: an essential analysis step in applied qualitative research. BMJ Global Health. 2018;3(5):e000837. doi: 10.1136/bmjgh-2018-000837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Braun V, Clarke V. Thematic analysis. In: Cooper H, ed. APA handbook of research methods in psychology vol. 2, research designs. American Psychological Association; 2012:57‐71. Chap 4. [Google Scholar]
- 42.NVivo qualitative data analysis software. QSR International, Version 12; 2018.
- 43.O’Connor C, Joffe H. Intercoder reliability in qualitative research: debates and practical guidelines. Int J Qual Methods. 2020;19:1‐13. doi: 10.1177/1609406919899220 [DOI] [Google Scholar]
- 44.Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16:1‐16. doi: 10.1177/1609406917733847 [DOI] [Google Scholar]
- 45.Whittingham JR, Ruiter RA, Castermans D, Huiberts A, Kok G. Designing effective health education materials: experimental pre-testing of a theory-based brochure to increase knowledge. Health Educ Res. 2008;23(3):414‐426. doi: 10.1093/her/cym018 [DOI] [PubMed] [Google Scholar]
- 46.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3-4):610‐617. doi: 10.1080/00223891.1990.9674095 [DOI] [PubMed] [Google Scholar]
- 48.Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the treatment self-regulation questionnaire (TSRQ) across three different health behaviors. Health Educ Res. 2006;22(5):691‐702. doi: 10.1093/her/cyl148 [DOI] [PubMed] [Google Scholar]
- 49.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385‐396. [PubMed] [Google Scholar]
- 50.Brown KM, Lindenberger JH, Bryant CA. Using pretesting to ensure your messages and materials are on strategy. Health Promot Pract. 2008;9(2):116‐122. doi: 10.1177/1524839908315134 [DOI] [PubMed] [Google Scholar]
- 51.Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115(4):e443‐e449. doi: 10.1542/peds.2004-2172 [DOI] [PubMed] [Google Scholar]
- 52.Brown HE, Atkin AJ, Panter J, Wong G, Chinapaw MJ, van Sluijs EM. Family-based interventions to increase physical activity in children: a systematic review, meta-analysis and realist synthesis. Obes Rev. 2016;17(4):345‐360. doi: 10.1111/obr.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Patrick H, Nicklas TA. A review of family and social determinants of children's eating patterns and diet quality. J Am Coll Nutr. 2005;24(2):83‐92. [DOI] [PubMed] [Google Scholar]
- 54.Beets MW, Cardinal BJ, Alderman BL. Parental social support and the physical activity-related behaviors of youth: a review. Health Educ Behav. 2010;37(5):621‐644. doi: 10.1177/1090198110363884 [DOI] [PubMed] [Google Scholar]
- 55.Amuta AO, Barry AE, McKyer ELJ. Risk perceptions for developing type 2 diabetes among overweight and obese adolescents with and without a family history of type 2 diabetes. Am J Health Behav. 2015;39(6):786‐793. doi: 10.5993/AJHB.39.6.6 [DOI] [PubMed] [Google Scholar]
- 56.Vanhecke TE, Miller WM, Franklin BA, Weber JE, McCullough PA. Awareness, knowledge, and perception of heart disease among adolescents. Eur J Cardiovasc Prev Rehabil. 2006;13(5):718‐723. doi: 10.1097/01.hjr.0000214611.91490.5e [DOI] [PubMed] [Google Scholar]
- 57.Melnyk BM, Small L, Morrison-Beedy D, et al. Mental health correlates of healthy lifestyle attitudes, beliefs, choices, and behaviors in overweight adolescents. J Pediatr Health Care. 2006;20(6):401‐406. doi: 10.1016/j.pedhc.2006.03.004 [DOI] [PubMed] [Google Scholar]
- 58.Hallal PC, Wells JC, Reichert FF, Anselmi L, Victora CG. Early determinants of physical activity in adolescence: prospective birth cohort study. Research support, non-U.S. Govt. Br Med J. 2006;332(7548):1002‐1007. doi: 10.1136/bmj.38776.434560.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hearst MO, Patnode CD, Sirard JR, Farbakhsh K, Lytle LA. Multilevel predictors of adolescent physical activity: a longitudinal analysis. Research support, N.I.H., extramural. Int J Behav Nutr Phys Act. 2012;9:8. doi: 10.1186/1479-5868-9-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cobb-Clark DA, Kassenboehmer SC, Schurer S. Healthy habits: The connection between diet, exercise, and locus of control. J Econ Behav Organ. 2014;98:1‐28. doi: 10.1016/j.jebo.2013.10.011 [DOI] [Google Scholar]