Abstract
Background
One of the reasons for the high rates of maternal and child morbidity and mortality in Sub-Saharan Africa is the rising proportion of teenage pregnancy. Preventing teenage pregnancy is critical to meeting sustainable development goal number three which aims to reduce the global maternal mortality ratio to less than 70 per 100,000 live births. To support the achievement of this goal, this study aimed to assess the spatial variation and factors associated with teenage pregnancy in Ethiopia using the recent nationally representative data.
Methods
A secondary data analysis of the 2019 Ethiopian mini Demographic and Health Survey was conducted with a total weighted sample of 2211 (unweighted 2100) teenagers. The Bernoulli model was fitted using SaTScan version 9.6 to identify hotspot areas and the geospatial pattern and prediction of teenage pregnancy were mapped using ArcGIS version 10.7. A multilevel logistic regression model was fitted to identify factors associated with teenage pregnancy among teenagers. Adjusted OR with 95% CI was calculated and variables having a p-value less than 0.05 were statistically significant factors of teenage pregnancy.
Result
The prevalence of teenage pregnancy among adolescents aged 15–19 years in Ethiopia was 12.89% (95% CI: 11.56%, 14.36%). The SaTScan analysis identified a primary cluster in the Gambella region of Ethiopia (log-likelihood ratio = 14.02, p < 0.001). A high prevalence of teenage pregnancy was observed in Somalia, Afar, Gambella, and the southern part of the Oromia regions of Ethiopia. Age, educational status- primary and secondary, religion- protestant, having television, contraceptive knowledge, household head-female, and region- Small peripheral were significant determinants of teenage pregnancy.
Conclusion
The spatial distribution of teenage pregnancy in Ethiopia was nonrandom. Age, educational status, religion, having television, contraceptive knowledge, sex of household head, and region were significant determinants of teenage pregnancy. Therefore, concerned government bodies and other stakeholders should organize periodic educational campaigns and youth-friendly reproductive health services. Collaboration between healthcare professionals, and religious and community leaders could also form a strategic partnership that makes interventions more comprehensive, culturally sensitive, and effective in reducing teenage pregnancy.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13690-024-01380-8.
Keywords: Teenage pregnancy, Spatial analysis, Multilevel analysis, EDHS, Ethiopia
| Text box 1. Contributions to the literature |
|---|
| • The study pinpointed geographical areas in Ethiopia with higher rate of teenage pregnancy, providing targeted areas for intervention and adding valuable information to the existing literature. |
| • The study provides a strong empirical foundation for advocacy groups working on teenage pregnancy, promoting community-driven initiatives and advocacy with robust data. |
| • The study sheds light on regional disparities in teenage pregnancy rates, highlighting areas where specific socio-demographic, cultural, or healthcare factors are contributing more significantly. |
Introduction
Teenage pregnancy is a global problem with serious health, social, and economic consequences including death among adolescents and their children [1, 2]. Although adolescent motherhood continues to be a significant public health issue in both developed and developing countries, it is much more common in low and middle-income countries(LMICs), particularly in Sub-Saharan Africa [3, 4]. According to the World Health Organization, nearly 21 million teenage girls aged 15 to 19 become pregnant each year in LMICs [5]. According to a meta-analysis conducted in Africa, the overall prevalence of teenage pregnancies was 18.8% in Africa and 19.3% in Sub-Saharan Africa, respectively [6]. Teenage pregnancy is more prevalent in LMICs, where access to education, information, and healthcare services is limited [7, 8].
One of the reasons for the high rates of maternal and child morbidity and mortality in Africa is the rising proportion of teenage pregnancy [9]. Also, teenage pregnancy plays a significant role in the intergenerational cycle of poverty in LMICs because of its impact on the economic status of adolescents, their families, and their communities as a whole [5, 6, 10, 11].
Evidence indicates that half of the pregnancies among teenage women in developing countries are unwanted [12], and more than half result in abortions [13]. Teenage pregnancy is linked to many adverse complications, including preterm labor [14], low birth weight, intrauterine growth retardation, neonatal death, [15–17], obstructed labor, fistula, and eclampsia [18], premature rupture of the membranes, stillbirths, unsafe abortion, sexually transmitted infections and increased maternal mortality and morbidity [17, 19, 20].
The most frequently cited risk factors for teenage pregnancy are older teenagers [21], low educational attainment [22–24], residence [9], marital status [23, 24], ethnicity [24], working status [21, 24], contraceptive use [21, 25], exposure to media [4, 21, 26], household wealth, peer pressure [27], living in a neighborhood where fewer people use birth control [28], gender inequality [29], and physical or sexual violence [29].
The public health burden of teenage pregnancy in Ethiopia is considerable. According to the 2016 Ethiopian Demographic and Health Survey (EDHS), its prevalence rate was approximately 13%. There is substantial geographic variation in its distribution, with higher rates observed in rural areas of Ethiopia compared to urban centers. Factors such as limited access to education, healthcare services, and contraceptive use are what influence the within-country variation. Apart from its direct health impacts, managing complications associated with teenage pregnancies such as pre-eclampsia and anemia is straining the healthcare system. In addition, teenagers who get pregnant frequently drop out of school, limiting their future employment opportunities and perpetuating cycles of poverty. It also contributes to a higher dependency ratio, straining family resources and reducing overall community productivity. Hence, it is causing a substantial economic burden on the healthcare system and the country in general. In some regions of the country, teenage pregnancy is related to cultural norms that support early marriage and childbearing. This highlights that efforts to address this critical issue in Ethiopia require multifaceted interventions including the need for evidence-based information regarding the geographical variation, community engagement, improved access to reproductive health services, and strong public health policies [30, 31].
Preventing teenage pregnancy is critical to meeting the sustainable development goal (SDGs) for maternal and newborn health [1]. Although the Ethiopian government’s many attempts to decrease teenage pregnancy, such as laws prohibiting early marriage, teenage pregnancy remains a public health issue in Ethiopia [32, 33]. Assessing the spatial variation and determinants of teenage pregnancy using the most recent nationally representative data (2019 EDHS) and robust modeling techniques such as the multilevel model is essential for several reasons. First, unlike traditional models like logistic regression which assumes all individuals are independent, multilevel models can properly account for the hierarchical and clustered nature of the EDHS data. Because this model explicitly accounts for this intra-cluster correlation by including random effects at the cluster level, it provides more accurate estimates of standard errors and regression coefficients than the conventional regression models. The multilevel model also allows for the modeling of variability of multiple levels and thus can improve the validity of statistical inferences [34]. Furthermore, conducting spatial analysis helps to consider geographical variations of teenage pregnancy within the country. This is critical to reduce wastage of public health resources and to improve socioeconomic equality in public health resource allocation and policy design through the identification of areas with a high prevalence of teenage pregnancy and guiding geographically targeted interventions [35]. Hence this study aimed to assess the spatial variation and factors associated with teenage pregnancy in Ethiopia.
Methods
Data sources, sampling procedure, and populations
The study was conducted based on the secondary data from the mini-2019 Ethiopian Demography and Health (EDHS), which was a cross-sectional community-based study design. Administratively, Ethiopia is divided into nine regions (Afar, Amhara, Benishangul-Gumuz, Gambella, Harari, Oromia, Somali, Southern Nations Nationalities and People’s Region, and Tigray) and two city administrations (Addis Ababa and Dire Dawa) at the time of the survey. The survey design employed a multi-staged stratified sampling technique. Each region was divided into urban and rural areas, resulting in 21 different sampling strata. Firstly, a total of 305 EAs (93 in urban, 212 in rural) were chosen independently with a probability proportional to each EA. The list of households in all selected EAs was recorded after the EAs were chosen. Household listing in EAs with more than 300 households was done after segmenting the EA and selecting only one segment for the survey, to minimize the task of listing households for the data frame. This makes the cluster in 2019 EMDHS either an EA (when the households in EA are less than 300) or a segment of EA (when households in EA are greater than 300). Second, from the newly formed household listing, a fixed number of 30 households/clusters were selected with an equal probability of systematic selection. Detailed sampling procedures are available on the measure DHS website [36, 37]. Adolescents aged 15–19 in Ethiopia were the source of the population whereas those found in the selected enumeration areas or clusters were the study population. The individual record dataset was used for this analysis. A total weighted sample of 2211 teenagers aged 15–19 years was included in this study. Regarding consent, before each DHS interview is conducted, an informed consent statement is read to the respondent, who may accept or decline to participate. A parent or guardian provides consent before participation by a child or adolescent. The informed consent statement emphasizes that participation is voluntary; that the respondent may refuse to answer any question or terminate participation at any time, and that the respondent’s identity and information will be kept strictly confidential [38].
Variables of the study
The outcome variable for this study was teenage pregnancy. A woman was considered as experiencing teenage pregnancy if her age was from 15 to 19 and had a birth or was pregnant at the time of the interview and recoded as “yes” and otherwise recoded as “no” [39]. Teenagers with a history of stillbirth or abortions were also considered as having ‘teenage pregnancy’.
The individual-level independent variables included in this study were age (maternal age was categorized as less than 17 years old, and greater than or equal to 17 years old), woman’s level of education (no education, primary education, secondary, and higher education), Religion(orthodox, protestant, Muslim and other (Catholic and Traditional/Indigenous Beliefs)), head of the household (male, and female), having a television (yes or no- was measured by asking respondents ‘does your household have a television?’), household size (less than six, greater than or equal to six) [40], contraceptive knowledge(yes or no), and wealth index (poor, middle, rich) which was measured by data on a household’s ownership of selected assets, such as television and bicycles, materials used for housing construction, and types of water access and sanitation facilities [36]. Community-level factors included residence, community-level poverty, community level of women’s education, and region. Since the data were not normally distributed, community poverty and literacy levels were classified as high or low, by using the median value as the classification cut-off point. The poverty level in a community was classified as high if the proportion of households in the two lowest wealth quintiles was greater than the median value, and low if the proportion was less than the median value [41]. The community level of teenagers’ education was classified as high if the proportion of teenagers with at least a primary level of education was greater than the median value, and low if it was less than the median value [42]. Regarding the measurement of variable ‘contraceptive knowledge’, the 2019 mEDHS classifies respondents who answered affirmatively to the question, indicating that they know at least one method of contraception, categorized as having contraceptive knowledge (Yes). Respondents who did not know any method of contraception were categorized as not having contraceptive knowledge (No).
Data management and analysis
The independent variables were extracted, cleaned, and recorded using STATA version 14 software. The data were weighted using sampling weight to restore the representativeness of the survey. Weighting was done according to the DHS’s recommendation. First, the weight variable for the used data (individual data) was identified. Then the weight variable was adjusted by scaling it with a factor of 1,000,000, as suggested by the DHS. Since the number of independent variables in this study was < 16, variables with a p-value of 0.2 from the bivariable multilevel logistic regression analysis were included in the multivariable multilevel logistic regression analysis. This was important to avoid missing potentially important predictors. It also allows for a more comprehensive initial model which was then refined through further analysis using a multivariable multilevel model. In the EDHS data, since teenagers are nested within a cluster, teenagers within the same cluster were more similar to each other than within different clusters, which violates the assumptions of the classic logistic regression analysis, which are independence of observation and equal variance across the cluster. Multilevel models explicitly account for this intra-cluster correlation by including random effects at the cluster level. Random effects in turn capture unobserved heterogeneity at different levels, which leads to more accurate and interpretable estimates of standard errors and fixed effects. In addition, multilevel models can include different levels of hierarchy. This allows for the modeling of variability at each level and thus provides a more nuanced understanding of the data. As a result, we estimated a fixed effect for both individual and community level factors, as well as a random effect for cluster variation, using a multilevel random intercept logistic regression model analysis which, with each community assumed to have a different intercept and fixed coefficients, and a random effect applied at the cluster level [34, 43, 44]. Fixed-effect results are reported as adjusted odds ratios with 95% confidence intervals, and variables with p-values ≤ 0.05 were considered statistically significant factors. Random effects (a measure of variation) were estimated by the intra-class correlation coefficient (ICC), which indicates the degree of heterogeneity of teenage pregnancy among clusters. The model’s fitness was evaluated using deviance, and the model with the lowest deviance value was selected as the best-fit model. Multicollinearity was also tested using the variance inflation factor (VIF) by performing a pseudo-linear regression analysis. In a multilevel model, predictors are at different levels (i.e., individual and community levels). Hence, mean VIF is the average of VIF values across all predictors. A mean VIF value ≤ 5 generally indicates that multicollinearity is not a major issue. Although multicollinearity was not an issue in this study, the literature suggests that there are various steps to handle high multicollinearity. Examining the VIF values of individual predictors to identify which variables are contributing most to multicollinearity is the first step, followed by calculating pairwise correlations among predictors to identify highly correlated pairs, and finally making model adjustments such as dropping one of the correlated predictors or combining predictors [45].
In multilevel analysis, four models were fitted. The first was a null model with no independent variables, which is fitted to assess the variability of teenage pregnancy in the community. The second (model I) hierarchical models contain individual-level variables whereas the third (model II) contains community-level variables. In the fourth model (model III) both individual and community-level variables were fitted simultaneously.
Spatial analysis
Spatial analysis was used to assess the geographic variations in teenage pregnancy cases among EDHS clusters. We calculated the proportions of teenage pregnancy cases in the survey for each cluster and then appended the latitude and longitude coordinates of the chosen EAS in the 2019 EDHS survey.
The spatial autocorrelation (Global Moran’s Index) statistic was used to determine whether teenage pregnancy was dispersed, clustered, or randomly distributed among teenagers in the study area [35, 46]. Moran’s I statistics gives a value between − 1 and + 1. A Global Moran’s I value approaching + 1 suggests a spatially clustered teenage pregnancy distribution. A Global Moran’s I value approaching − 1 indicates a dispersed spatial distribution, while a Global Moran’s I value 0 indicates a dispersed spatial distribution of teenage pregnancy. A significant spatial autocorrelation is indicated by a statistically significant Global Moran’s’ I test, p-value < 0.05. The maximum peak distance at which teenage pregnancy becomes more prominent was determined using incremental spatial autocorrelation [46].
Hot Spot analysis (the Getis-Ord Gi * statistic) of the z-scores and significant p-values defines the hot spot or cold spot values for the clusters spatially [47]. A statistical output with a high GI* indicates a “hotspot,” whereas one with a low GI* indicates a “cold spot.” [48]. A “hotspot” area indicates a high proportion of teenage pregnancy while a “cold spot” area indicates a low proportion of teenage pregnancy.
The spatial interpolation technique is employed to predict teenage pregnancy for areas that were not sampled based on sampled clusters [49]. We used deterministic and geostatistical ordinary kriging interpolation techniques. Spatial interpolation was conducted on the assumption that objects that are spatially distributed are spatially correlated, and that objects that are close together are more likely to have similar properties [50, 51].
The SaTScan software (Spatial and Temporal Scan Statistics) was used to identify significant spatial widows of teenage pregnancy. SaTScan uses a scanning window that moves over the study region. The input data used were case and controls. After that, the analysis model was selected, which was the Bernoulli-based model of spatial scan statistics. The Bernoulli model was used by applying Kuldorff’s method for purely spatial analysis, as the outcome variable has a Bernoulli distribution. To determine whether the number of observed teenage pregnancies within the potential cluster was significantly higher than expected, a likelihood ratio test statistic and the p-value were used. Information on detected clusters, their location, size, and statistical significance was obtained and was visualized using ArcGIS software to mat the clusters.
Ethical consideration
Our study was based on secondary data from the Ethiopian Demographic and Health Survey and we have secured a permission letter from the main Demographic Health and Survey to download the dataset after explaining the purpose of our study. The original EDHS data were collected following international and national ethical guidelines. The dataset was not shared or passed on to other bodies and has maintained its confidentiality.
Patient and public involvement
There was no patient or public involvement in this study because it was a secondary data analysis based on previously collected DHS data to provide estimates of common health and health-related indicators.
Results
Characteristics of the study participants
A total weighted sample of 2,211 (unweighted sample, 2,100) women aged 15–19 was included in this study. The mean (± SD) age of the participants was 16.88 ± 1.38 years. Most of the study participants 1,470 (66.52%) live in rural areas. Around 235 (10.65%) of the study participants have no education. The prevalence of teenage pregnancy among adolescents aged 15–19 years in Ethiopia was 12.89% (95% CI: 11.56%, 14.36%) (Table 1).
Table 1.
Individual and community level characteristics of the teenagers in Ethiopia, 2019 mini EDHS (n = 2,211)
| Variables | Categories | Weighted frequency | Percentage(%) |
|---|---|---|---|
| Women education status | No education | 235 | 10.65 |
| Primary | 1,462 | 66.18 | |
| Secondary and higher | 511 | 23.16 | |
| Religion | Orthodox | 948 | 42.92 |
| Muslim | 633 | 28.66 | |
| Protestant | 594 | 26.88 | |
| Othera | 34 | 1.54 | |
| Household size | Less than six | 1,018 | 46.09 |
| Greater than or equal to six | 1,191 | 53.91 | |
| Sex of household head | Male | 1,696 | 76.76 |
| Female | 513 | 23.24 | |
| Have television | Yes | 365 | 16.52 |
| No | 1,844 | 83.48 | |
| Contraceptive knowledge | Yes | 2,052 | 92.89 |
| No | 157 | 7.11 | |
| Wealth index | Poor | 732 | 33.13 |
| Middle | 446 | 20.21 | |
| Rich | 1,031 | 46.66 | |
| Residence | Urban | 739 | 33.48 |
| Rural | 1,470 | 66.52 | |
| Community level poverty | Low | 1,277 | 57.79 |
| High | 932 | 42.21 | |
| Community level of women’s education | Low | 728 | 34.67 |
| High | 1,372 | 65.33 | |
| Region | larger central | 1,931 | 87.40 |
| small peripherals | 162 | 7.34 | |
| metropolis | 116 | 5.25 |
a = Catholic and Traditional/Indigenous Beliefs
Spatial analysis of teenage pregnancy in Ethiopia
Spatial autocorrelation (Global Moran’s I) analysis
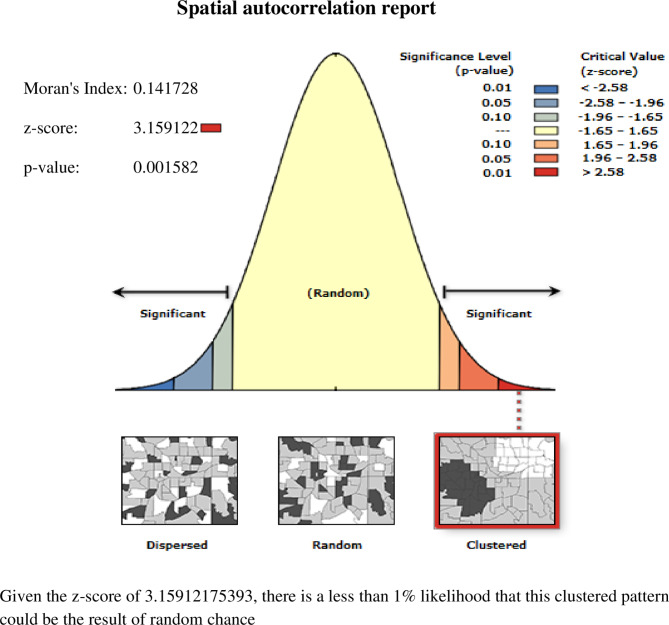
The global spatial autocorrelation analysis showed a clustering pattern of teenage pregnancy in Ethiopia (Global Moran’s I = 0.141, p value = 0.001582) (Fig. 1). The incremental autocorrelation result revealed statistically significant z-scores at a peak distance of 253.944 km 2.73 (distances; Z-score) for teenage pregnancy.
Fig. 1.
Spatial autocorrelation of teenage pregnancy across regions in Ethiopia, EMDHS 2019
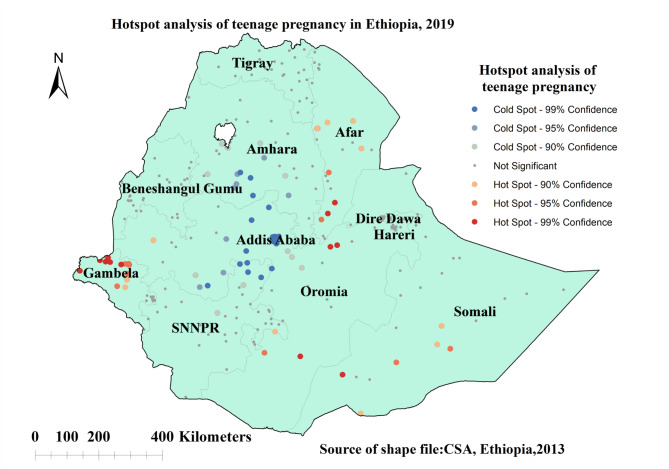
Hotspot analysis
We observed significant spatial variability in the distribution of teenage pregnancy among adolescent Ethiopian women, with significant hotspots found in Somalia, Afar, Gambella, and the southern part of the Oromia regions of Ethiopia. The significant cold spot regions of teenage pregnancy among teenagers were detected in Addis Ababa, the Northern part of SNNPR, and the Southern Amhara regions of Ethiopia (Fig. 2).
Fig. 2.
Spatial patterns of hotspots and cold spots of teenage pregnancy across regions in Ethiopia, EMDHS 2019
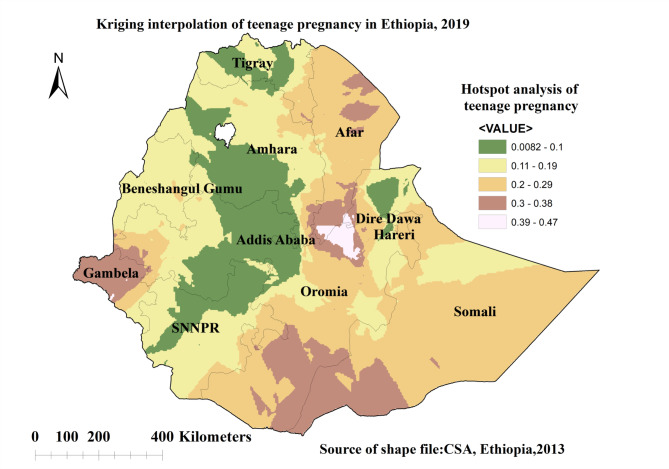
Spatial interpolation
The highest predicted proportion of teenage pregnancy among teenagers was detected in Somalia, Afar, Gambella, Oromia, and the Southeastern part of Diredawa and Harari regions of Ethiopia. The lowest predicted proportion of teenage pregnancy among teenagers was detected in the Addis Ababa, Dire Dawa, Harari, Amhara, Tigray, and SNNPR regions of Ethiopia (Fig. 3).
Fig. 3.
Kriging Interpolation of teenage pregnancy across regions in Ethiopia, 2019 EMDHS
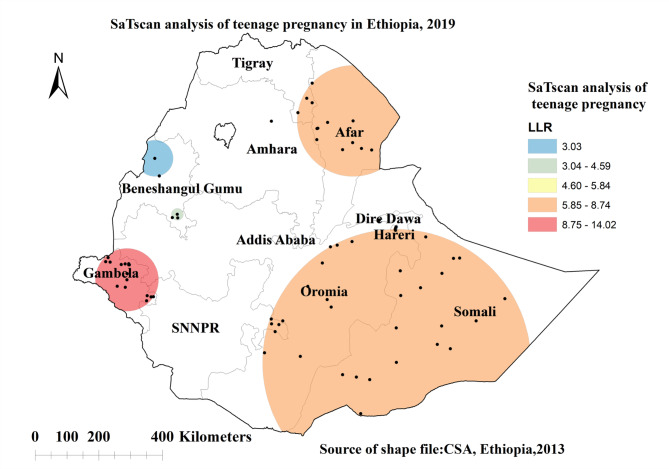
Spatial scan statistical analysis
The SaTScan analysis result identified a total of 64 statistically significant clusters of which primary clusters of teenage pregnancy were detected in the Gambella regions of Ethiopia. The spatial window was located at 7.813123 N, 34.536369 E with a 98.81 km radius, with a relative risk of 2.46 and log-likelihood ratio (LLR) of 14.02 at a p-value of 0.0003. Teenagers who lived within the spatial window had a 2.46 times higher chance of experiencing teenage pregnancy as compared to those teenagers outside the spatial window (Fig. 4).
Fig. 4.
Significant primary and secondary windows of teenage pregnancy across regions in Ethiopia, EMDHS 2019
Factors associated with teenage pregnancy
Variance inflation factor (VIF) was used to test multicollinearity and rule out the presence of a significant correlation between variables. The mean VIF of < 5, indicates that there was no multicollinearity. The ICC value in the null model indicated that cluster/EA variability accounted for 29% of the overall teenage pregnancy distribution variability, while individual differences accounted for the remaining 71% of the variability. The variation in teenage pregnancy distribution remained significant after accounting for individual and community-level factors. Across the communities, 30% of the chances of variations in teenage pregnancy were detected in the final model (Model III). s.
The final model (model III) with the lowest deviance value (1242) is the best-fit model. In the final model Age, educational status, religion, having television, contraceptive knowledge, sex of household head, and region were significant predictors of teenage pregnancy. A woman who was less than 17 years old had 93% [AOR = 0.07; 95%CI: 0.04, 0.11] less likely to experience teenage pregnancy compared with those aged greater than 17 years old. The odds of experiencing teenage pregnancy among teenagers who have primary education was 44% (AOR = 0.56: 95% CI: 0.35, 0.88) less as compared to those who have no education. The odds of experiencing teenage pregnancy among teenagers who have secondary and higher education was 81% (AOR = 0.19: 95% CI: 0.10, 0.36) less as compared to those who have no education.
The odds of experiencing teenage pregnancy among Protestants was 1.87 (AOR: 1.87:95% CI 1.11, 3.14) times higher as compared to orthodox religion followers. Teenagers who had television had 76% [AOR = 0.24; 95%CI: 0.10, 0.56] times lower odds of experiencing teenage pregnancy as compared with teenagers who had no television. Teenagers with a female household head were 59% [AOR = 0.41; 95%CI: 0.26, 0.65] less likely to experience teenage pregnancy as compared with teenagers with a male household head.
Teenagers who have contraceptive knowledge were 2.88 [AOR = 2.88; 95%CI: 1.32, 6.30] times higher odds of experiencing teenage pregnancy compared with teenagers with no contraceptive knowledge. Teenagers who live in small peripheral regions were 4.40 [AOR = 4.40; 95%CI: 1.91, 10.14] times higher odds of experiencing teenage pregnancy compared with a woman who was living in a large central region (Table 2).
Table 2.
Multivariable multilevel analysis for assessing the determinants of teenage pregnancy in Ethiopia, 2019 mini EDHS
| Variables | Categories | Null model | Model I | Model II | Model III | ||
|---|---|---|---|---|---|---|---|
| AOR [95% CI] | AOR [95% CI] | AOR [95% CI] | |||||
| Age | < 17 | 0.07 [0.04, 0.11] | 0.07 [0.04, 0.11]*** | ||||

|
1.00 | 1.00 | |||||
| Women education status | No education | 1.00 | 1.00 | ||||
| Primary | 0.46 [0.29, 0.71] | 0.56 [0.35, 0.88]*** | |||||
| Secondary and higher | 0.15 [0.08, 0.29] | 0.19 [0.10, 0.36]*** | |||||
| Religion | Orthodox | 1.00 | 1.00 | ||||
| Muslim | 1.03 [0.58, 1.82] | 0.58 [0.30, 1.12] | |||||
| Protestant | 1.84 [1.10, 3.09] | 1.87 [1.11, 3.14]* | |||||
| Othera | 0.29 [0.04, 1.78] | 0.28 [0.04, 1.81] | |||||
| Have television | No | 1.00 | 1.00 | ||||
| Yes | 0.29 [0.13, 0.61] | 0.24 [0.10, 0.56]*** | |||||
| Contraceptive knowledge | No | 1.00 | 1.00 | ||||
| Yes | 2.00 [0.94, 4.25] | 2.88 [1.32, 6.30]*** | |||||
| Sex of the household | Male | 1.00 | 1.00 | ||||
| Female | 0.49 [0.31, 0.76] | 0.41 [0.26, 0.65]** | |||||
| Wealth index | Poor | 1.00 | 1.00 | ||||
| Middle | 1.11 [0.72, 1.72] | 1.31 [0.83, 2.05] | |||||
| Rich | 0.63 [0.39, 0.99] | 0.77 [0.46, 1.27] | |||||
| Community level variables | |||||||
| Residence | Rural | 1.92 [0.98, 3.79] | 1.23 [0.54, 2.76] | ||||
| Urban | 1.00 | 1.00 | |||||
| Community level poverty | Low | 1.00 | 1.00 | ||||
| High | 1.39 [0.78, 2.49] | 1.42 [0.72, 2.82] | |||||
| Community level of women’s education | Low | 1.00 | 1.00 | ||||
| High | 0.50 [0.29, 0.85] | 0.65 [0.34, 1.21] | |||||
| Region | Large central | 1.00 | 1.00 | ||||
| Small peripheral | 1.53 [0.79, 2.95] | 4.40 [1.91, 10.14]** | |||||
| Metropolitans | 0.78 [0.27, 2.22] | 2.50 [0.71, 8.76] | |||||
| * = P-value < 0.05, ** = Pvalue < 0.01, *** = Pvalue < 0.001 | |||||||
| AOR = adjusted odds ratio; CI = confidence interval. | |||||||
| Random effect & comparison | |||||||
| ICC | 0.29 | 0.29 | 0.24 | 0.30 | |||
| Deviance | 1562 | 1265 | 1531 | 1242 | |||
| Mean VIF | 1.51 | 1.51 | 1.86 | ||||
ICC = Inter cluster correlation coefficient, VIF = Variance inflation factor, a = Catholic and Traditional/Indigenous Beliefs
Discussion
This study was aimed at assessing the spatial distribution and determinant factors of teenage pregnancy in Ethiopia. Our spatial analysis indicated that there is significant spatial heterogeneity in teenage pregnancy across regions of Ethiopia. The Getis-Ord Gi* analysis showed that a significant teenage pregnancy was highly clustered in Somalia, Afar, Gambella, and the southern part of the Oromia regions of Ethiopia. Spatial Kuldorff’s scan statistics analysis revealed that a total of 64 statistically significant clusters were identified with primary clusters observed in the Gambella region of Ethiopia. Previous studies have also shown the presence of geographical differences in teenage pregnancy [24]. The multilevel analysis also supported that teenagers who lived in small peripheral regions have more than four times higher chance of experiencing teenage pregnancy as compared to teenagers living in metropolis regions. The possible reason for the high prevalence of teenage pregnancy in these small peripherals, inhabitants living in small peripheral regions are pastoralists who have limited access to health information and family planning services due to their high mobility and a strong commitment to cultural and religious values [52–54]. Evidence also suggests that access to healthcare in Ethiopia’s small peripheral regions is a challenge that may affect adolescents’ access to reproductive health services [55]. Improving targeted interventions such as promoting healthcare access, particularly reproductive health services, organizing periodic awareness campaigns, and facilitating youth-friendly service events in those hotspot areas could play a significant role in reducing teenage pregnancy and its consequences. Collaborative work between healthcare professionals and other stakeholders like women and children affairs could play significant role in realizing interventions like youth-friendly service events.
The odds of teenage pregnancy were higher among adolescents in the age range of greater than 17 years old. The finding is consistent with a study done in Ethiopia [23, 56], and East Africa [21]. The possible reason for the higher pregnancy rate among older teenagers might be due to older teens may have been exposed to more sex and may have been more likely to marry [57]. The other possible reason could be that older teenagers had more autonomy and opportunities to live independently and away from their parents because it signifies the end of their high school education and the beginning of their University journey.
Women with higher educational status (secondary and higher education) were less likely to experience teenage pregnancy as compared to those who had no education. The finding is similar to a study done in Ethiopia [58, 59], East Africa [21], Africa [9], Nigeria [60], and Japan [61]. This could be because educated adolescents have better access to reproductive health information and services, reducing the risk of teenage pregnancy. Another possible explanation is that higher-educated females were more likely to marry at an older age, lowering the risk of teenage pregnancy [23].
Teenagers who live in a household with a television are less likely to become pregnant than teenagers who live in a household without a television. The finding is consistent with other studies done in Zambia [4, 26], and East Africa [21]. The possible reason might be those teenagers who have television may have a chance to be exposed to information that will enhance the utilization of reproductive health services including contraception [62]. Teenagers who live in a female household head are less likely to experience teenage pregnancy than teenagers who live in a male household head. The possible reason might be those women who live in a female household head may have the autonomy to decide for their age at first birth and other social and economic issues.
Protestant religious followers were more likely to have teenage pregnancies than teenagers who were orthodox religious followers. The result is consistent with a study conducted in Ethiopia [59]. This could be explained by religious differences in attitudes, norms, and beliefs about using contraception [63, 64]. The other possible reason for the increased risk of teenage pregnancy could be the liberal attitude of the protestant religion towards sexual activity, leading to premarital sex and pregnancy [65].
Teenagers with contraceptive knowledge were more likely to become pregnant than those with no contraceptive knowledge. The finding is similar to a study done in Sub-Saharan Africa [66]. There are several alternative explanations for this counterintuitive finding. First, even if teenagers know about contraception, they might not use it effectively or consistently. This could be due to a lack of service availability and accessibility, or incorrect use. Second, there are persisting myths, misconceptions, and cultural and social norms about contraceptives in the country. Some beliefs and attitudes say using contraceptive methods is a sin and even if used, some methods are unreliable. These beliefs and attitudes are highly circulated in the community and are often associated with stigma or disapproval of individuals who utilize the service, particularly in areas that this study found as hotspots. Consequently, these societal pressures might make teenagers worried about societal judgment and lack of privacy if using contraception. Third, even with knowledge and access, teenagers may face barriers to practicing contraceptives. Due to restrictions from their sexual partner or family, they may lack the autonomy or confidence to insist on contraceptive use within their relationships [67]. Furthermore, evidence suggests that greater knowledge of contraceptive methods does not guarantee contraceptive use [68]. Understanding and addressing these factors can help bridge the gap between knowledge and practice, leading to more effective service utilization strategies.
The study’s strengths included the use of a nationally representative dataset and a combination of statistical methods (spatial analysis and multilevel logistics analysis) was used, allowing for a better understanding of the role of contextual and geographical factors in the occurrence of teenage pregnancy. As a limitation, the geographical coordinates of clusters were displaced up to 2 km in urban areas, 5 km for most clusters in rural areas, and 10 km for 1% of clusters in rural areas. This was done by the EDHS before making the dataset public for potential identification of survey participants. This could affect the estimated cluster effects and must be accounted for when utilizing the findings of this study. In addition, since the data used is secondary, important predictors such as occupational status and peer pressure were not included in the analysis.
Conclusion and recommendation
The spatial distribution of teenage pregnancy in Ethiopia was nonrandom. Age, educational status, religion, having television, contraceptive knowledge, sex of household head, and region were significant determinants of teenage pregnancy. Therefore, Improving targeted interventions such as promoting healthcare availability and accessibility, particularly reproductive health services, organizing periodic educational campaigns, and facilitating youth-friendly reproductive health services in the identified hotspot areas could play a significant role in reducing teenage pregnancy and its consequences. Collaborative work between healthcare professionals and other stakeholders like women and children affairs could play a significant role in realizing interventions like youth-friendly reproductive health services.
What’s more, concerned government bodies and health facilities should form strategic partnerships with religious and community leaders to collaborate and support initiatives aimed at reducing teenage pregnancy. These initiatives can be organizing joint taskforces, and co-hosting community workshops, health fairs, and events that address teenage pregnancy and sexual health. This helps to ensure a unified approach in designing government health strategies, to show respect and integrate religious values into health interventions, and to establish referral systems where religious and community leaders can direct individuals to appropriate health services and support programs. Religious organizations should also support health programs to integrate faith-based perspectives into public health programs. These collaborative approaches ensure that interventions are comprehensive, culturally sensitive, and effective in reducing teenage pregnancy. This study recommends further qualitative or mixed-method studies to be conducted by researchers to explore uncovered cultural and religious drives associated with teenage pregnancy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to acknowledge the MEASURE DHS program for allowing us to access and use the 2019 mini EDHS data set.
Abbreviations
- AOR
Adjusted Odd Ratio
- EDHS
Ethiopian Demography and Health Survey
- ICC
Intra-class Correlation Coefficient
- LMICs
Low and middle-income countries
- MOR
Median odds ratio
- PCV
Proportional Change in Variance
- SSA
Sub-Saharan Africa
- SDG
Sustainable Development Goal
- WHO
World Health Organization
Author contributions
The conception of the work and design of the work was done by FMA. Data analysis and interpretation, drafting of the article, revising it critically for intellectual content, validation, and final approval of the version to be published were done by MAA, FMA, ALB, MTA, WMT, WNA, AKY, MCA, TKT, and MNA.
Funding
No funding was obtained for this study.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Our study was based on secondary data from the Ethiopian Demographic and Health Survey and we have secured a permission letter from the main Demographic Health and Survey to download the dataset after explaining the purpose of our study. The original EDHS data were collected following international and national ethical guidelines. The dataset was not shared or passed on to other bodies and has maintained its confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Organization WH, Adolscent pregnancy. 2022 [cited 2023 January 26]; https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy
- 2.Moshi FV, Tilisho OJRH. The magnitude of teenage pregnancy and its associated factors among teenagers in Dodoma Tanzania: a community-based analytical cross-sectional study. 2023. 20(1): pp. 1–13. [DOI] [PMC free article] [PubMed]
- 3.Neal S, et al. Childbearing in adolescents aged 12–15 years in low resource countries: a neglected issue. New estimates from demographic and household surveys in 42 countries. Acta Obstet Gynecol Scand. 2012;91(9):1114–8. [DOI] [PubMed] [Google Scholar]
- 4.Phiri M et al. A multilevel analysis of trends and predictors associated with teenage pregnancy in Zambia (2001–2018). 2023. 20(1): pp. 1–13. [DOI] [PMC free article] [PubMed]
- 5.WHO. Adolescent pregnancy. 2022.
- 6.Kassa GM, et al. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and meta-analysis. Reproductive Health. 2018;15(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed S et al. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. 2010. 5(6): p. e11190. [DOI] [PMC free article] [PubMed]
- 8.Sas M et al. The role of education in the prevention of radicalization and violent extremism in developing countries. 2020. 12(6): p. 2320.
- 9.Kassa GM et al. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and meta-analysis. 2018. 15(1): pp. 1–17. [DOI] [PMC free article] [PubMed]
- 10.Kawakita T et al. Adverse maternal and neonatal outcomes in adolescent pregnancy. 2016. 29(2): pp. 130–6. [DOI] [PMC free article] [PubMed]
- 11.Organization WH. World health statistics 2016: monitoring health for the SDGs sustainable development goals. World Health Organization; 2016.
- 12.Alabi O, I.O.J.I.J.o.A.R.i.B., Oni, Sciences S. Teenage pregnancy in Nigeria: Causes, effect and control. 2017. 7(2): pp. 17–32.
- 13.Mezmur H, Assefa N, Alemayehu T. Teenage pregnancy and its associated factors in eastern Ethiopia: a community-based study. Int J Women’s Health, 2021: pp. 267–78. [DOI] [PMC free article] [PubMed]
- 14.Rasheed S, Abdelmonem A, Amin M. Adolescent pregnancy in upper Egypt. Int J Gynecol Obstet. 2011;112(1):21–4. [DOI] [PubMed] [Google Scholar]
- 15.Wu W-Y, et al. The growth and development of children born to adolescent mothers in Taiwan. Ital J Pediatr. 2016;42(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar A, et al. Outcome of teenage pregnancy. Indian J Pediatr. 2007;74:927–31. [DOI] [PubMed] [Google Scholar]
- 17.Indarti J et al. Teenage pregnancy: obstetric and perinatal outcome in a tertiary centre in Indonesia. Obstetrics and gynecology international, 2020. 2020. [DOI] [PMC free article] [PubMed]
- 18.Ayuba II, Gani O. Outcome of teenage pregnancy in the Niger Delta of Nigeria. Ethiop J Health Sci. 2012;22(1):45–50. [PMC free article] [PubMed] [Google Scholar]
- 19.Bateman BT, Simpson LL. Higher rate of stillbirth at the extremes of reproductive age: a large nationwide sample of deliveries in the United States. Am J Obstet Gynecol. 2006;194(3):840–5. [DOI] [PubMed] [Google Scholar]
- 20.Pergialiotis V, et al. Teenage pregnancy antenatal and perinatal morbidity: results from a tertiary centre in Greece. J Obstet Gynaecol. 2015;35(6):595–9. [DOI] [PubMed] [Google Scholar]
- 21.Worku MG et al. Prevalence and associated factors of adolescent pregnancy (15–19 years) in East Africa: a multilevel analysis. 2021. 21: pp. 1–8. [DOI] [PMC free article] [PubMed]
- 22.Were M. Determinants of teenage pregnancies: the case of Busia District in Kenya. Econ Hum Biology. 2007;5(2):322–39. [DOI] [PubMed] [Google Scholar]
- 23.Kefale B et al. A multilevel analysis of factors associated with teenage pregnancy in Ethiopia. 2020: pp. 785–93. [DOI] [PMC free article] [PubMed]
- 24.Bolarinwa OA et al. Spatial distribution and factors associated with adolescent pregnancy in Nigeria: a multi-level analysis. 2022. 80(1): p. 43. [DOI] [PMC free article] [PubMed]
- 25.Bitew DA, et al. Predictors of underage pregnancy among women aged 15–19 in highly prevalent regions of Ethiopia: a multilevel analysis based on EDHS, 2016. Sci Rep. 2023;13(1):857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sserwanja Q et al. Access to mass media and teenage pregnancy among adolescents in Zambia: a national cross-sectional survey. 2022. 12(6): p. e052684. [DOI] [PMC free article] [PubMed]
- 27.Yakubu I, Salisu WJ. Determinants of adolescent pregnancy in sub-saharan Africa: a systematic review. Reproductive Health. 2018;15(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Asmamaw DB, Tafere TZ, Negash WD. Prevalence of teenage pregnancy and its associated factors in high fertility sub-saharan Africa countries: a multilevel analysis. BMC Womens Health. 2023;23(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Negriff S, Schneiderman JU, Trickett PK. Child maltreatment and sexual risk behavior: maltreatment types and gender differences. J Dev Behav Pediatrics: JDBP. 2015;36(9):708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abate K, Assefa N, Tesfaye B, et al. Teenage pregnancy in Ethiopia: prevalence, determinants, and outcomes. Reprod Health. 2021;18(1):100. 10.1186/s12978-021-01156-0.34020669 [Google Scholar]
- 31.Gebremariam A, Abreha S, Aemero M, et al. The prevalence and determinants of teenage pregnancy in Ethiopia: a systematic review and meta-analysis. BMC Public Health. 2020;20:1584. 10.1186/s12889-020-09588-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ayele BGk et al. Determinants of teenage pregnancy in Degua Tembien District, Tigray, Northern Ethiopia: a community-based case-control study. 2018. 13(7): p. e0200898. [DOI] [PMC free article] [PubMed]
- 33.Pati RN, Tekie S. Biocultural dynamics of teenage pregnancies in Ethiopia: medico anthropological appraisal. Int J Social Sci Manage. 2016;3(1):68–77. [Google Scholar]
- 34.Snijders TA, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. sage; 2011.
- 35.Fischer MM, Getis A. Handbook of applied spatial analysis: software tools, methods and applications. Berlin: Springer; 2010. [Google Scholar]
- 36.Croft TN et al. Guide to DHS statistics. 2018. 645.
- 37.Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. 2021. Ethiopia Mini Demographic and Health Survey 2019: Final Report. Rockville, Maryland, USA: EPHI and ICF. https://dhsprogram.com/pubs/pdf/FR363/FR363.pdf
- 38.DHS Program. Protecting the privacy of DHS (Demographic and Health Surveys) survey respondents [Internet]. https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm
- 39.Tigabu S, Liyew AM. and B.M.J.B.W.s.H. Geremew, modeling spatial determinates of teenage pregnancy in Ethiopia; geographically weighted regression. 2021. 21(1): p. 254. [DOI] [PMC free article] [PubMed]
- 40.United Nations Department of Economic and Social Affairs, Population Division. Household Size and Composition Around the World 2017. New York: United Nations. 2017. https://www.un.org/en/development/desa/population/publications/pdf/ageing/household_size_and_composition_around_the_world_2017_data_booklet.pdf
- 41.Liyew AM, A.B.J.B.P H, Teshale. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016; a multilevel analysis. BMC Public Health. 2020;20(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sisay D et al. Spatial Distribution and Associated Factors of Institutional Delivery among Reproductive-Age Women in Ethiopia: The Case of Ethiopia Demographic and Health Survey. 2022. 2022. [DOI] [PMC free article] [PubMed]
- 43.Goldstein H. Multilevel statistical models. Volume 922. Wiley; 2011.
- 44.Wong GY, W.M.J.J.o.t.A SA, Mason. The hierarchical logistic regression model for multilevel analysis. 1985. 80(391): pp. 513–24.
- 45.Shieh Y-Y, Fouladi R. The Effect of Multicollinearity on Multilevel modeling parameter estimates and standard errors. Volume 63. Educational and Psychological Measurement - EDUC PSYCHOL MEAS; 2003. pp. 951–85.
- 46.Waldhör TJSiM. The spatial autocorrelation coefficient Moran’s I under heteroscedasticity. Stat Med. 1996;15(7–9):887–92. [DOI] [PubMed] [Google Scholar]
- 47.Wulder M, B.J.I.J.o.R S, Boots. Local spatial autocorrelation characteristics of remotely sensed imagery assessed with the Getis statistic. 1998. 19(11): pp. 2223–31.
- 48.Tsai P-J, et al. Spatial autocorrelation analysis of health care hotspots in Taiwan in 2006. BMC Public Health. 2009;9(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krivoruchko, K., Empirical bayesian kriging. ESRI: Redlands, CA. 2012, California: USA. Available online at: http://www.esri.com/news/arcuser
- 50.Franklin J. Mapping species distributions: spatial inference and prediction. Cambridge University Press; 2010.
- 51.Le ND, J.V.J.J.o.M A, Zidek. Interpolation with uncertain spatial covariances: a bayesian alternative to kriging. J Multivar Anal. 1992;43(2):351–74. [Google Scholar]
- 52.Kahsay ZH et al. Application of individual behavioral models to predict willingness to use modern contraceptives among pastoralist women in Afar region, Northern Ethiopia. 2018. 13(5): p. e0197366. [DOI] [PMC free article] [PubMed]
- 53.Belda SS, et al. Modern contraceptive utilization and associated factors among married pastoralist women in Bale eco-region, Bale Zone. South East Ethiopia. 2017;17(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Henok A. and E.J.E.j.o.h.s. Takele, Assessment of barriers to reproductive health service utilization among Bench Maji Zone Pastoralist communities. 2017. 27(5): pp. 523–30. [DOI] [PMC free article] [PubMed]
- 55.Tesema GA, Tessema ZT, S.J.B.H.S K. Decomposition and spatio-temporal analysis of health care access challenges among reproductive age women in Ethiopia, 2005–2016. 2020. 20: pp. 1–23. [DOI] [PMC free article] [PubMed]
- 56.Kassa GM et al. Trends and determinants of teenage childbearing in Ethiopia: evidence from the 2000 to 2016 demographic and health surveys. 2019. 45(1): pp. 1–13. [DOI] [PMC free article] [PubMed]
- 57.Ayanaw Habitu Y. A. Yalew, and T.J.J.o.p. Azale Bisetegn, Prevalence and factors associated with teenage pregnancy, Northeast Ethiopia, 2017: a cross-sectional study. 2018. 2018. [DOI] [PMC free article] [PubMed]
- 58.Mezmur H, Assefa N, T.J.I. .J.o.W.s.H. Alemayehu, teenage pregnancy and its associated factors in eastern Ethiopia: a community-based study. 2021: pp. 267–78. [DOI] [PMC free article] [PubMed]
- 59.Bitew DA et al. Predictors of underage pregnancy among women aged 15–19 in highly prevalent regions of Ethiopia: a multilevel analysis based on EDHS, 2016. 2023. 13(1): p. 857. [DOI] [PMC free article] [PubMed]
- 60.Nwosu U, Health P. Contemporary factors of teenage pregnancy in rural communities of Abia state. Nigeria. 2017;4(2):588–92. [Google Scholar]
- 61.Baba S, Iso H, Fujiwara TJPo. Area-level and individual-level factors for teenage motherhood: a multilevel analysis in Japan. 2016. 11(11): p. e0166345. [DOI] [PMC free article] [PubMed]
- 62.Fatema K, J.T.J.S.-P H, Lariscy. Mass media exposure and maternal healthcare utilization in South Asia. 2020. 11: p. 100614. [DOI] [PMC free article] [PubMed]
- 63.Obeng Gyimah S.J.P.R. A cohort analysis of the timing of first birth and fertility in Ghana. Review. 2003;22:251–66. [Google Scholar]
- 64.Taggart T et al. The role of religious socialization and religiosity in African American and Caribbean black adolescents’ sexual initiation. 2018. 57: pp. 1889–904. [DOI] [PMC free article] [PubMed]
- 65.Addai. I.J.R.o.r.r., Religious affiliation and sexual initiation among Ghanaian women. 2000: pp. 328–343.
- 66.Asmamaw DB, Tafere TZ. and W.D.J.B.W.s.H. Negash, Prevalence of teenage pregnancy and its associated factors in high fertility sub-saharan Africa countries: a multilevel analysis. 2023. 23(1): pp. 1–10. [DOI] [PMC free article] [PubMed]
- 67.McQueston K, Silverman R. and A.J.C.f.G.D.W.P. Glassman, Adolescent fertility in low-and middle-income countries: effects and solutions. 2012. 295.
- 68.Ochako R et al. Barriers to modern contraceptive methods uptake among young women in Kenya: a qualitative study. 2015. 15(1): pp. 1–9. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.