Abstract
Propagation of the flavivirus tick-borne encephalitis virus in BHK-21 cells selected for mutations within the large surface glycoprotein E that increased the net positive charge of the protein. In the course of 16 independent experiments, 12 different protein E mutation patterns were identified. These were located in all three of the structural domains and distributed over almost the entire upper and lateral surface of protein E. The mutations resulted in the formation of local patches of predominantly positive surface charge. Recombinant viruses carrying some of these mutations in a defined genetic backbone showed heparan sulfate (HS)-dependent phenotypes, resulting in an increased specific infectivity and binding affinity for BHK-21 cells, small plaque formation in porcine kidney cells, and significant attenuation of neuroinvasiveness in adult mice. Our results corroborate the notion that the selection of attenuated HS binding mutants is a common and frequent phenomenon during the propagation of viruses in cell culture and suggest a major role for HS dependence in flavivirus attenuation. Recognition of this principle may be of practical value for designing attenuated flavivirus strains in the future.
RNA viruses are capable of rapid adaptation to alterations in their growth environment. This has historically been exploited to generate viruses with desired biological properties, such as attenuated viral strains to be used as live vaccines (1). On the other hand, unrecognized adaptive mutations occurring during propagation of viruses in the laboratory can be a source of misleading results and erroneous conclusions regarding the viral life cycle in the natural host (4). It is therefore of fundamental importance to understand the molecular processes underlying virus adaptation to particular host cells.
Recently, much attention has been given to the interaction of viral surface proteins with glycosaminoglycans (GAGs), which are present almost ubiquitously on cell surfaces but vary with respect to their composition and quantity among different cell types, tissues, and cellular developmental stages (6, 64). Although the overall picture is still far from being complete, it has become clear during the past few years that viruses from many different families interact with GAGs, in most cases heparan sulfate (HS) (7, 8, 11, 12, 14, 15, 18, 20, 34, 35, 38, 40, 50, 59, 61, 62, 63, 67, 70), and it has been proposed that the affinity of the viral surface for HS may be an important determinant of tissue tropism and pathogenicity (5, 9, 17, 30, 48, 65). In most cases the affinity of the virus for HS seems to be relatively low and may serve the purpose of concentrating the virus on the cell surface to facilitate subsequent binding to one or more high-affinity receptors (6, 21, 33, 53, 58). In some cases, however, the interaction may be more specific, such as in the case of herpes simplex virus type 1, for which interaction with an HS carrying a specific sulfation pattern can functionally substitute for a protein receptor (60). For a number of viruses, including alphaviruses (5, 37), pestiviruses (32), picornaviruses (17, 56), and retroviruses (47, 50), it has been demonstrated that adaptation to certain cell lines results in the selection of mutants that bind HS with high affinity. Although the increased affinity for HS was apparently favorable for growth in cell culture, GAG-adapted viruses in several cases were found to have reduced virulence in animals (5, 9, 36, 37, 39, 48, 56).
In this study we investigated the adaptation of a flavivirus, tick-borne encephalitis (TBE) virus, to BHK-21 cells and the involvement of HS binding in this process. Members of the genus Flavivirus, family Flaviviridae, are mostly arthropod-borne viruses and include, in addition to TBE virus, human pathogens such as yellow fever virus, West Nile virus, Japanese encephalitis virus, and the dengue viruses (66). They are spherical, small (approximately 50 nm in diameter), enveloped particles with a positive-stranded RNA genome that encodes all of the viral proteins in a single long open reading frame. Mature virus particles carry two membrane-associated proteins designated M (7 to 8 kDa) and E (50 to 60 kDa). The latter mediates both receptor binding and fusion, and its atomic structure has been solved by X-ray diffraction analysis for TBE virus (55). Protein E forms an elongated structure and is present on mature virus particles as head-to-tail homodimers. As a distinctive feature that is different from many other enveloped viruses, these dimers are oriented parallel rather than perpendicular to the viral membrane. The surface of the virion therefore does not contain protruding spikes but is fairly smooth. Based on structural studies with recombinant subviral particles, virions are predicted to contain 90 protein E dimers, which are organized in a regular icosahedral lattice by lateral interactions (19). The X-ray structure further indicates that protein E consists of three distinct structural domains. One of these, domain II, contains a short amino acid sequence that is highly conserved among all flaviviruses and acts as an internal fusion peptide which, in the course of a low pH-triggered conformational change, is involved in the fusion of the viral envelope to a cellular membrane (2, 24). Domain III, which has the typical fold of an immunoglobulin constant domain, has been proposed to contain a receptor binding site (39, 41, 55). However, despite a number of reports in which different potential flavivirus receptor molecules have been identified, the initial stages of attachment and uptake of flaviviruses remain largely unresolved (reference 39 and references therein; reference 41 and references therein). In two cases, HS was reported to play a role in this process. In the case of dengue virus type 2, HS was shown to be required for virus infectivity (11, 30), and mutants of Murray Valley encephalitis virus, another member of the genus carrying an amino acid substitution within a putative receptor binding motif, were found to have an increased dependence on GAGs (39). Here we report the emergence of multiple potential HS binding sites distributed over the surface of protein E of TBE virus as a result of adaptation to growth in BHK-21 cells. Using the infectious cDNA clone of TBE virus (42), we investigated some of these mutations in detail with respect to their effect on specific infectivity, growth, binding, and HS dependence in cell culture as well as virulence in the mouse model.
MATERIALS AND METHODS
Virus and infectious cDNA clone.
Experiments were performed with Western subtype TBE virus prototypic strain Neudoerfl or its derivatives. Strain Neudoerfl is a tick isolate with a very short passage history (26) and has been previously characterized in detail, including its virulence and infectivity in the mouse model (44). The complete genomic sequence of this strain is available under GenBank accession no. U27495. Infectious RNA was transcribed in vitro either from a full-length infectious cDNA clone (plasmid pTNd/c) or after ligation of two partial clones (plasmids pTNd/5′ and pTNd/3′) which contain the 5′ one-third and the 3′ two-thirds of the genome of TBE virus strain Neudoerfl (42).
For virus binding assays (see below) wild-type and mutant viruses were grown in primary chicken embryo (CE) cells and purified as follows. Supernatants were cleared from cell debris by centrifugation (Sorvall F16/250 rotor; 10,000 rpm, 30 min, 4°C) and virus was harvested by precipitation with 7% polyethylene glycol 6000 for 2 h at 4°C and subsequent centrifugation at 10,000 rpm for 30 min at 4°C. Virus pellets were resuspended in 1/100 of the original volume of TAN buffer (0.05 M triethanolamine [pH 8.0], 0.1 M NaCl, 0.1% bovine serum albumin [BSA] [essentially fatty acid free]), and insoluble fragments were removed by centrifugation in an Eppendorf microcentrifuge (10,000 rpm, 10 min, 4°C). Then the preparation was subjected to centrifugation through a sucrose gradient (10 to 50% [wt/wt] sucrose in TAN buffer, pH 8.0) for 3 h at 38,000 rpm and 4°C in a Beckman SW-40 rotor. Gradients were fractionated using an ISCO 640 density gradient fractionator. Virus was detected by hemagglutination activity at pH 6.4 with goose erythrocytes (13) and was quantified by four-layer enzyme-linked immunosorbent assay (ELISA) after sodium dodecyl sulfate treatment (27).
Serial passages in BHK-21 cells.
Two different experimental schemes involving infections at either a low or high multiplicity of infection (MOI) were applied to passage TBE virus in BHK-21 cells. In order to passage TBE virus at a low MOI, a log10 dilution series of virus was prepared and used to infect the cells. Virus production was monitored by a four-layer ELISA (28), and the supernatant from the culture infected with the highest dilution that still scored positive in the ELISA was again diluted in log10 steps and used for the next round of infection. This procedure was repeated three times, and then undiluted supernatant was used to infect a large tissue culture flask of BHK-21 cells in order to produce sufficient amounts of virus for the subsequent characterization. In passaging experiments that involved a high MOI, supernatants of infected cells were used without dilution for the next round of infection and this procedure was repeated up to 28 times.
The passaged viruses that were analyzed included not only wild-type strain Neudoerfl but also a number of recombinant derivatives of strain Neudoerfl that carried additional mutations that are not directly relevant to this study (e.g., deletions in the 3′ noncoding region) and have been described in part elsewhere (44).
Sequence analysis.
Virus was concentrated from cell culture supernatants by ultracentrifugation, and the pellets were used to prepare genomic RNA, which was sequenced by reverse transcription-PCR (RT-PCR) by standard methods as described previously (68). PCR-derived fragments were sequenced directly on both strands. The sequence analysis always included the entire protein E coding region and, in some cases, also included the region encoding the other structural proteins and parts of NS5 and the 3′ noncoding region. New plasmid constructions were checked by sequencing the entire protein E coding region and the regions containing the restriction sites used for cloning. Stocks of recombinant mutant viruses were checked prior to their biological characterization by RT-PCR sequence analysis of the structural protein coding region and parts of the noncoding regions and the nonstructural protein coding region. Sequencing was performed using an automated DNA sequencing system (Applied Biosystems).
Protein structure graphics.
The X-ray crystal structure of a soluble ectodomain fragment of the TBE virus protein E (55) (Protein Data Base [PDB] entry 1SVB) was used for depictions of wild-type protein E and was the basis for models of the mutants. Protein structure graphics were made using the molecular visualization program Insight II, version 95.0 (Biosym/MSI, San Diego, Calif.). The homology module of this program was used for making amino acid replacements and finding plausible side chain conformations using the “auto rotamer” search function. The main peptide chain conformation was kept constant in all models, but in order to avoid steric collisions it was necessary to change the original side chain orientation of the mutated residues in the S158R/G159R and E201K models. In the latter case the conformation of the side chain of Tyr 281 was also changed. Electrostatic potentials were calculated using the DelPhi module (protein dielectric, 2.0; solvent dielectric, 80; solvent radius, 1.4 Å; ionic strength, 0.145 M; ionic radius, 2.0 Å) and displayed on a solid Connolly surface generated by Insight II.
Construction and derivation of recombinant viruses.
The protein E mutations were introduced into plasmid pTNd/5′ by swapping a 640-bp-long AgeI-BstXI fragment with the corresponding fragment derived by RT-PCR from the passaged virus containing the desired mutations(s). AgeI and BstXI have unique cutting sites in this plasmid, at positions 960 and 1600, respectively, of the strain Neudoerfl genome. Infectious RNA was transcribed from the mutated plasmids after in vitro ligation with plasmid pTNd/3′, taking advantage of the unique ClaI restriction site, and was transfected into BHK-21 cells by electroporation as described previously (42). Cell supernatants containing recombinant virus were harvested after 2 to 3 days and used to infect litters of suckling mice for the preparation of high-titer virus stocks as described in previous studies (41, 44).
Plaque assay and determination of infectivity titers in cell cultures.
BHK-21 cells, primary CE cells, and porcine kidney (PS) cells were grown under standard conditions (31, 42). Plaque assays were performed on PS cells as described previously (31). Infectivity titers on BHK-21 and CE cells (for both of which there is no plaque assay available) were determined by endpoint dilution infection experiments. Virus preparations were diluted in 0.5-log steps and used to infect cells in 24-well culture plates. The culture medium was checked for virus production at 3 and 6 days postinfection by a four-layer ELISA (28).
Inhibition of virus growth by heparin or sulfate depletion.
Growth curves for BHK-21 cells were created by infecting cells grown in 24-well cluster plates with a low dose of virus in order to amplify possible effects of mutations (10 infectious units, as previously determined by endpoint titration on BHK-21 cells, per well). For infection, virus was added to the cells in 200 μl of medium (Earle's minimal essential medium containing 1% fetal calf serum) and incubated for 1 h at 37°C. The inoculum was then removed by washing and replaced by fresh growth medium. Virus release was monitored in aliquots of the supernatant harvested at various time points ranging from 24 to 108 h postinfection by a protein E ELISA (28). For heparin inhibition assays, the same procedure was used, but the virus was first incubated for 10 min with various concentrations (between 0 and 500 μg/ml) of heparin (from bovine lung; Sigma) prior to infection and the same concentrations of heparin were maintained during infection and viral growth. Growth curves for sulfate-depleted BHK-21 cells were created essentially as described by Chen et al. (11) using chlorate as an inhibitor of sulfation (3, 22). Briefly, BHK-21 cells were cultivated for at least four passages in sulfate-free medium (Earle's minimal essential medium lacking MgSO4, supplemented with 0.811 mM MgCl2, 2.4 mg of cysteine per liter, 1.5 mg of methionine per liter, and 5% dialyzed fetal calf serum), and 20 mM sodium chlorate was added 48 h before infection. Infection and monitoring of growth were then performed as described above.
Cell binding assay.
BHK-21 cells were rinsed twice with phosphate-buffered saline, pH 7.4, containing 0.3 mM EDTA and were harvested by scraping. Cells were suspended in a 50 mM HEPES buffer (pH 7.4, containing 100 mM NaCl, 0.4% BSA, 3 mM KCl, 0.5 mM MgCl2, 1 mM CaCl2) and washed once in this buffer. After counting of the cells with a CASY1 TT cell counter (Schärfe System, Reutlingen, Germany), aliquots of 105 cells were incubated in a final volume of 50 μl for 1 h at 37°C with gentle constant agitation with a GAG-digesting enzyme (heparinase III from Flavobacterium heparinum or chondroitinase ABC from Proteus vulgaris; Sigma) or without enzyme for the undigested cell control. After washing the cells three times with 50 mM HEPES buffer (pH 7.4, 100 mM NaCl, 0.2% BSA), cells were resuspended in 50 μl of this buffer chilled to 4°C, and 500 ng of purified wild-type or mutant virus was added and incubated for 1 h at 4°C with gentle constant agitation. Unbound virus was then removed by washing cells twice with the same buffer (4°C), and bound virus was detected by two successive incubation steps at 4°C for 30 min in approximately 50 μl with the protein E-specific monoclonal antibody B2 (23) in a concentration of 4.35 μg/ml and a commercial fluorescein-conjugated goat anti-mouse immunoglobulin G1 (Jackson ImmunoResearch Laboratories, Inc.) at a concentration of 7 μg/ml. Cell-associated fluorescence was then quantified in a FACSCalibur flow cytometer (Becton Dickinson; 15 mW argon laser, 488 nm) with a 530/30 nm band-pass filter analyzing 10,000 events per sample. Median fluorescence activities were calculated using CellQuest software and used as a parameter for virus binding.
Animal model.
Characterization of mutant viruses in the animal model was performed as described in previous studies (41, 44). Briefly, groups of 10 5-week-old (body weight, approximately 20 g) outbred Swiss albino mice were inoculated subcutaneously, and survival was recorded for 28 days. Then mice were bled, and seroconversion was detected by a TBE-antibody ELISA (25). For the determination of the 50% lethal dose (LD50) and the 50% infectious dose (ID50), mice were inoculated with sequential 10-fold dilutions of virus ranging from 1 to 106 PFU. The calculation of LD50s and ID50s was performed by the method of Reed and Muench (54). For ID50 calculations, the number of infected mice was taken to be the total of mice killed plus surviving mice with detectable seroconversion. Surviving mice without detectable serum antibody were scored as uninfected. To test whether seroconverted mice had developed a protective immunity, mice were inoculated with a challenge dose of 100 LD50s of the highly virulent TBE virus strain Hypr (69).
RESULTS
Gain of net positive charge in protein E during growth in BHK-21 cells.
In the course of our studies with TBE virus we observed that the virus often exhibited altered properties after a few passages in BHK-21 cells. To investigate this phenomenon in more detail we analyzed TBE virus that had been passaged in BHK-21 cells at a high or low MOI. Sequence analysis of viruses obtained from a total of 16 passaging experiments revealed that each of the viruses had acquired one or two amino acid mutations within protein E, as summarized in Table 1. Remarkably, all but one of these (the Leu-to-Phe mutation in experiment 3) were nonconservative substitutions, and there were no silent nucleotide changes except for two that arose at higher passage numbers in experiments with a high MOI (experiments 12 and 14). This strongly suggests that the observed mutations did not occur randomly but instead were the result of a specific selection pressure. Only 12 different mutation patterns were obtained because in some cases identical mutations arose in separate experiments. A striking common feature of all of the nonconservative substitutions was that they caused an increase in the net positive charge of protein E. This was achieved either by a gain of basic Arg or Lys residues or by the replacement of acidic Asp or Glu residues. In some cases a net gain of two positive charges occurred by the addition of two Arg residues (experiment 5), the loss of two Asp residues (experiment 15), or single mutations from a negatively charged amino acid to a positively charged residue (experiments 7, 9, 10, 11, 13, and 14).
TABLE 1.
Mutations in protein E resulting from BHK-21 cell adaptation
| Experiment no. | Passage
|
Mutation (position no.)
|
||
|---|---|---|---|---|
| No.a | MOIb | Nucleotidec | Amino acidd | |
| 1 | 4 | Low | A→G (1337) | Glu→Gly (122) |
| 2 | 4 | Low | A→G (1232) | Gln→Arg (87) |
| 3 | 4 | Low | G→A (1339) | Ala→Lys (123) |
| C→A (1340) | ||||
| C→T (1576) | Leu→Phe (202) | |||
| 4 | 4 | Low | C→A (1901) | Thr→Lys (310) |
| 5 | 4 | Low | T→A (1446) | Ser→Arg (158) |
| G→A (1447) | Gly→Arg (159) | |||
| 6 | 4 | Low | C→A (1901) | Thr→Lys (310) |
| 7 | 4 | Low | G→A (1222) | Glu→Lys (84) |
| 8 | 4 | Low | C→A (1669) | Gln→Lys (233) |
| 9 | 4 | Low | G→A (2131) | Glu→Lys (387) |
| 10 | 4 | Low | G→A (1123) | Glu→Lys (51) |
| 11 | 4 | Low | G→A (1855) | Glu→Lys (295) |
| 12 | 8 | High | A→G (1337) | Glu→Gly (122) |
| 28 | High | G→A (1338) | Silent | |
| 13 | 8 | High | G→A (1573) | Glu→Lys (201) |
| 14 | 18 | High | G→A (1573) | Glu→Lys (201) |
| T→C (2247) | Silent | |||
| 15 | 14 | High | A→G (1580) | Asp→Gly (203) |
| G→A (1729) | Asp→Asn (253) | |||
| 16 | 10 | High | A→G (1337) | Glu→Gly (122) |
Passage number after which sequence analysis was performed. At the indicated passage number the wild-type sequence was no longer detectable at the mutated positions.
Low and high MOI passaging experiments were performed as described in Materials and Methods.
Numbers are according to the TBE virus genomic sequence (GenBank accession no. U27495).
Numbers start from the amino terminus of protein E.
The rate of replacement of the wild-type by the mutant sequence depended on the passage conditions. As indicated in Table 1, the majority of our experiments were performed at a low MOI. Under these conditions, each mutant had completely displaced the wild type within four passages. Using a high MOI resulted in a lower rate of replacement. For example, in experiment 12 it took eight passages to completely abolish the wild-type signal from the sequencing reaction although the mutant sequence was already detectable after the first passage and accounted for approximately 50% of the virus population after three passages (data not shown). In the same experiment, no reversions or additional nucleotide changes were observed until the 23rd passage. At passage 28 an additional silent mutation was detected (Table 1). This mutation was in codon 122 (GGG to GGA), which had already undergone a primary change from Glu (GAG) to Gly (GGG). It is therefore likely that the additional mutation served to optimize the altered sequence at the RNA level. This example illustrates the high degree of genetic stability of the protein E coding sequence under the chosen experimental conditions and corroborates the idea that the mutations that had emerged during the first few passages were the result of selection pressure and were not random.
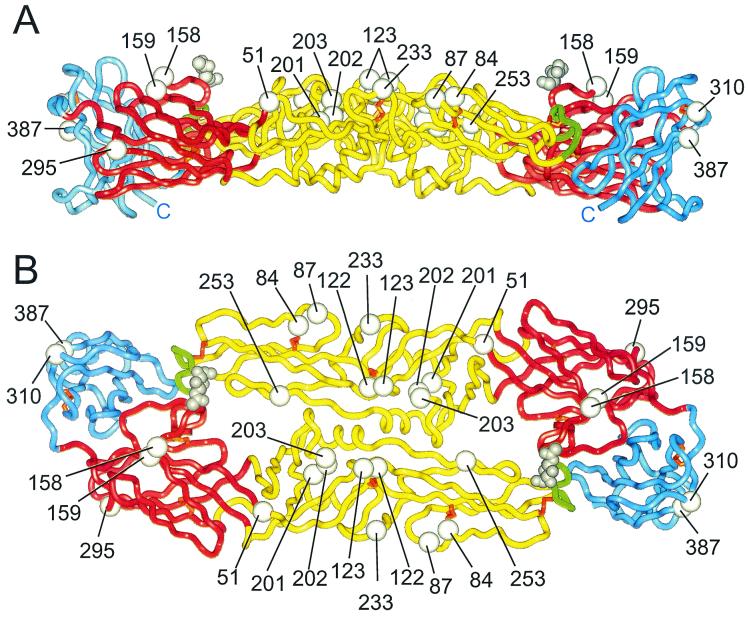
As shown in Fig. 1, the mutations were scattered over almost the entire upper and lateral surface of protein E and occurred in all three of the protein domains. Most of the mutations were located on crests or other protruding structural elements. An exception is the conservative mutation of Leu to Phe at residue 202, which is buried inside the molecule but is spatially close to Ala 123, which changed to a Lys in the same experiment (experiment 3). A close inspection of the mutations revealed that all of them (except for the conservative 202 mutation) were located in the vicinity of already existing positively charged surface residues. Since the mutations themselves contributed a net gain of positive charge, the result in each case was the formation of an expanded cluster of positive charge at the protein surface.
FIG. 1.
Ribbon diagram showing a side view (A) and a top view (B) of the ectodomain portion of the TBE virus protein E homodimer (55). The positions of mutations generated by passaging the virus in BHK-21 cells are shown by white spheres, with the amino acid numbers indicated. Domain I of each subunit is colored red, domain II is yellow, and domain III is blue. The fusion peptide (2) at the tip of domain II is colored green, and the disulfide bridges are orange. The first N-acetyl-glucosamine residue of the carbohydrate attached to Asn 154 is shown in gray, and the position where the peptide chain continues into the stem-anchor region at the carboxy terminus is indicated by a “C.”
Generation of recombinant viruses with altered surface charges.
To study the effects of individual mutations in a defined genetic background, we constructed recombinant virus mutants using the infectious cDNA clone of TBE virus strain Neudoerfl. Out of the 12 different mutation patterns that we obtained from the passaging experiments (Table 1) we selected the following three, each representing a different type of mutation, for the generation of recombinant viruses: (i) Glu 201→Lys, which caused a loss of a negative charge and a gain of a positive charge by a single mutation; (ii) Glu 122→Gly, which increased the net positive charge of protein E by the loss of an acidic residue (remarkably, this same mutation occurred in 3 out of 16 experiments); and (iii) Ser 158→Arg and Gly 159→Arg, which was unique in that it had acquired two positive charges in adjacent positions.
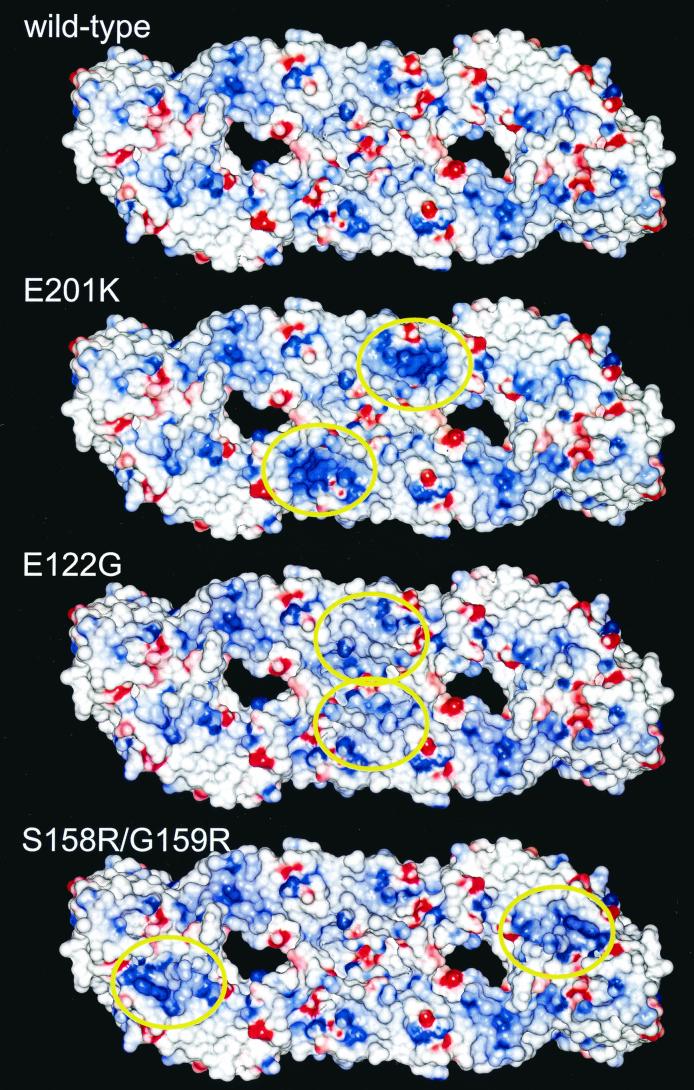
The effects of these three types of mutations on the surface charge distribution of protein E are shown in Fig. 2. Each of the mutations was found to have a strong effect on the local surface potential, creating a distinct patch of surface area that was predominantly positively charged. The location of the patch, however, was different for each mutation.
FIG. 2.
Surface models of wild-type and mutant E proteins colored by electrostatic potential. The viewing angle is the same as in Fig. 1B. Positively charged surfaces are shown in blue, and negatively charged surfaces are red. The yellow ovals indicate areas of increased positive charge relative to wild-type protein E.
The corresponding recombinant mutant viruses, designated E(E201K), E(E122G), and E(S158R/G159R), were readily obtained from the infectious cDNA clone, and high-titer stocks were prepared (Table 2). After their genetic identities had been confirmed by sequence analysis these virus stocks were used for all subsequent biological characterizations.
TABLE 2.
Recombinant viruses carrying protein E mutations
| Virus | Amino acid mutation (position no.)a | Infectivity titer of virus stock (log PFU/ml)b | Plaque size (mm) |
|---|---|---|---|
| Wild-type (strain Neudoerfl) | 8.0 ± 0.2 | 2.0–4.0 | |
| E(E201K) | Glu→Lys (201) | 8.7 ± 0.2 | <1.5 |
| E(E122G) | Glu→Gly (122) | 8.4 ± 0.3 | <1.5 |
| E(S158R/G159R) | Ser→Arg (158) | 7.3 ± 0.2 | <2.0 |
| Gly→Arg (159) |
Numbers start from the amino terminus of protein E.
Mean ± standard deviation determined from four experiments.
Plaque phenotypes and relative infectivity titers.
We started our characterization of the recombinant mutant viruses by determining how these mutations, which had originally arisen during adaptation to BHK-21 cells, influenced viral growth in these and other cultured cells. Plaque assays performed on PS cells revealed small plaque phenotypes for all three of the recombinant mutants. This property was more pronounced for mutants E(E201K) and E(E122G) than for mutant E(S158R/G159R) (Table 2).
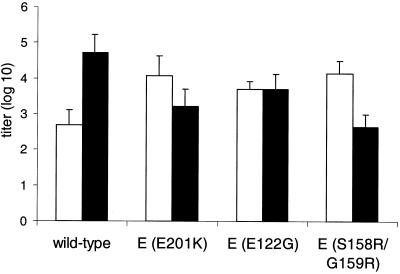
Another significant effect of the protein E mutations was found by comparing infectivity titers in BHK-21 cells and primary CE cells (Fig. 3). Starting with 104 PFU of each mutant and wild-type virus (as determined by plaque assays in PS cells) (Table 2), infectivity titers for these two cell types were determined by endpoint dilution experiments. The resulting values plotted in Fig. 3 demonstrate that the infectivity titer of parent strain Neudoerfl was significantly higher with CE cells than with BHK-21 cells. In contrast, all three of the mutants infected BHK-21 cells as well as or better than CE cells. These results show that the mutations increased the infectivity of TBE virus for BHK-21 cells relative to CE cells, and this may, at least in part, be the functional basis of adaptation to these cells.
FIG. 3.
Infectivity titers in BHK-21 (open bars) and CE (solid bars) cells. Titers were determined by endpoint dilution experiments (see Material and Methods), starting with 104 PFU of each virus. Values shown are the means of four independent experiments (with error bars representing standard deviations).
Growth in sulfate-depleted BHK-21 cells.
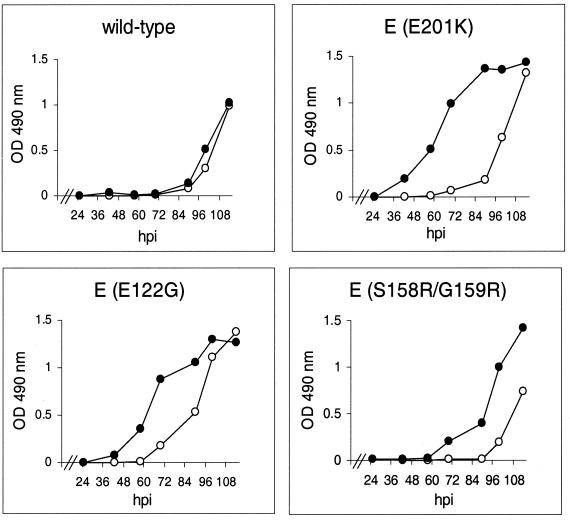
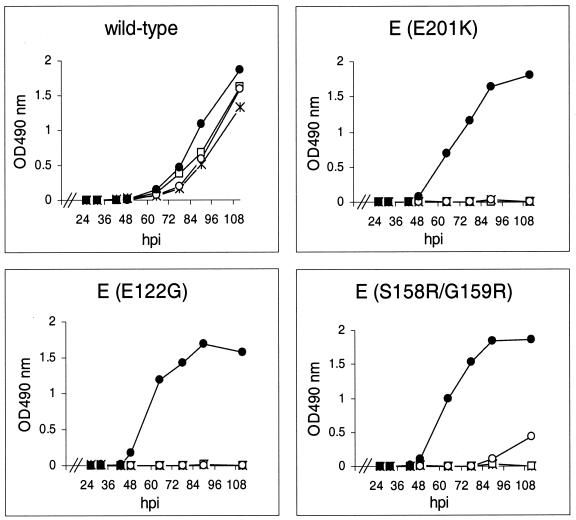
We hypothesized that the changes in infectivity titers described above might be due to more efficient attachment of the virus mutants to the cell surface. The nature of these mutations, which resulted in new clusters of positive surface charges (Fig. 2), suggested that these viral mutants might attach to negatively charged cell surface structures, in particular GAGs. To test a possible dependence on such highly sulfated cell surface polycarbohydrates, we infected BHK-21 cells grown under conditions that largely inhibited sulfation of GAGs (see Materials and Methods) and compared virus growth in these cells to that in normally grown BHK-21 cells. The resulting growth curves obtained for the three mutant viruses and the wild-type control are shown in Fig. 4. While the lack of sulfation had only a slight effect on the wild-type virus, the growth of the three recombinant mutants was significantly delayed by the inhibition of sulfation.
FIG. 4.
Growth curves obtained by infecting BHK-21 cells grown under normal conditions (●) or under conditions that prevent sulfation of proteoglycans (○). Cells were infected with 10 infectious units of wild-type or recombinant mutant virus, and release of virus into the supernatants was monitored by a protein E ELISA (for details, see Materials and Methods). A representative example of several experiments is shown. hpi, hours postinfection; OD, optical density.
Growth inhibition by heparin.
To confirm the dependence of the mutant viruses on GAGs, we used heparin, a soluble GAG structurally closely related to HS, as a potential inhibitor of virus growth. BHK-21 cells were infected as described above, but this time heparin was added at various concentrations to the cell culture medium. The resulting growth curves shown in Fig. 5 demonstrate that heparin very efficiently inhibited the growth of the three mutants, whereas the growth of the wild-type virus was only slightly delayed.
FIG. 5.
Inhibition of virus growth by soluble heparin. Heparin concentrations added to the virus and growth medium are as follows: ●, no heparin; ○, 50 μg/ml; □, 150 μg/ml; ∗, 500 μg/ml. Cells were infected with 10 infectious units of wild-type or recombinant mutant virus, and release of virus into the supernatants was monitored by a protein E ELISA (for details, see Materials and Methods). A representative example of several experiments is shown. hpi, hours postinfection; OD, optical density.
Binding to BHK-21 cells.
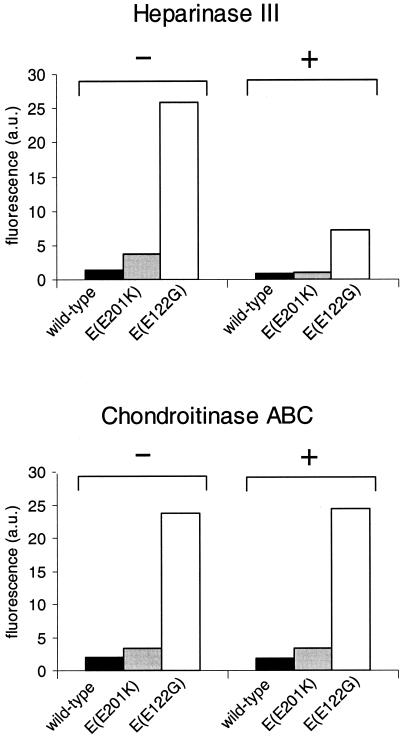
Finally, attachment of virus to the cell surface and its dependence on the presence of GAGs was assessed directly in a binding assay. After the addition of equal amounts of purified mutant or wild-type virus to identical aliquots of cells, binding was quantified by fluorescence-activated cell sorter analysis. As shown in Fig. 6, mutants E(E201K) and E(E122G) bound better to BHK-21 cells than did the wild-type virus. While the difference in binding was quite large for mutant E(E122G), it was less pronounced in the case of mutant E(E201K). Nevertheless, the difference was reproducible in several separate experiments and therefore is probably significant. Virions of mutant E(S158R/G159R) turned out to be too unstable to be purified in sufficient quantities and thus could not be subjected to this binding assay. Pretreatment of the cells with heparinase III strongly reduced the binding of the mutant viruses, whereas digestion of cells with chondroitinase ABC had no measurable influence on binding (Fig. 6), indicating that HS rather than chondroitin sulfate is the crucial GAG for the attachment of these TBE virus mutants.
FIG. 6.
Binding of wild-type and mutant viruses to BHK-21 cells. Equal amounts (500 ng) of purified virus were added to undigested BHK-21 cells (−) or cells that were predigested (+) with heparinase III (top) or chondroitinase ABC (bottom). The amount of cell-bound virus was quantified by fluorescence-activated cell sorter analysis (see Materials and Methods). Median fluorescence intensities are plotted as arbitrary units (a.u.). A representative example of several experiments is shown.
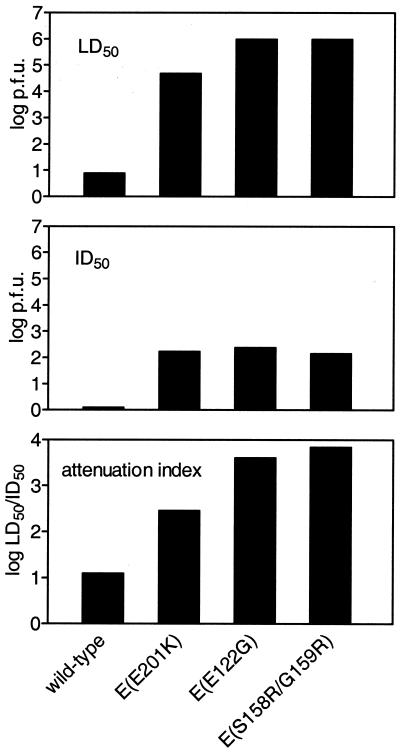
Virulence in the mouse model.
As shown in previous studies (41, 44), peripheral inoculation of adult mice with virulent TBE virus induces fatal encephalitis (neuroinvasiveness), whereas attenuated mutants do not kill mice but are still capable of replicating and inducing an antibody response (peripheral infectivity). After inoculation of mice with various doses of virus the LD50 and ID50 were determined as quantitative parameters of neuroinvasiveness and peripheral infectivity. The results are shown in Fig. 7. All three of the mutants exhibited a striking degree of attenuation compared to the wild-type virus. For mutants E(S158R/G159R) and E(E122G) the LD50 was as high as 106 PFU, i.e., approximately 100,000-fold higher than for the wild-type virus. All three mutants, however, also suffered a loss of peripheral infectivity (ID50) by a factor of approximately 100. The LD50/ID50 ratio, termed “attenuation index” (41), was determined to correct for these differences in the ID50 in order to reveal the degree to which neuroinvasiveness itself, rather than the overall infectivity, was reduced. As shown in Fig. 7, the attenuation indices of the three mutants ranged between 2.5 and 3.8, values indicative of strongly attenuated phenotypes in the adult mouse model. Infectivity calculations were based on the detection of seroconversion (see Materials and Methods). To determine whether seroconversion also conferred a protective immunity, mice were challenged with a lethal dose (100 LD50s) of the highly virulent TBE virus strain Hypr. All of the mice that had seroconverted were protected, and therefore the 50% protective dose was equal to the ID50 (Fig. 7). Thus, the attenuated mutants efficiently induced protective immunity in adult mice.
FIG. 7.
Virulence (neuroinvasiveness) and peripheral infectivity of wild-type and recombinant mutant viruses determined by subcutaneous inoculation of 5-week-old mice. LD50s (top) and ID50s (middle) were determined as described in Materials and Methods. The attenuation index (bottom) was calculated as the LD50/ID50 ratio.
DISCUSSION
During the past few years there has been a large accumulation of data from various fields of research, including both cell biology and the study of infectious agents, that illustrate the widespread biological importance of interactions of biomolecules with GAGs (6, 29, 51, 57). Since GAGs are almost ubiquitously and often abundantly present on cell surfaces, molecules approaching the cell are probably unable to avoid having to interact with them in one way or another. Although in the case of viruses the affinity and specificity of these interactions are usually low, the multiplicity of biochemical structures, including highly diverse sulfation patterns, also allows the creation of very specific binding sites that can serve to perform defined biological functions (60). High- and low-affinity interactions of viral proteins with GAGs may be important determinants of tropism, virus spread, or the establishment of latent infection (21, 35, 58, 60, 63, 64, 65). While the role of GAG binding of viruses in their natural hosts remains rather speculative, there is solid evidence from a number of quite diverse virus families that cell culture adaptation can result in the selection of mutants that exhibit a high affinity for binding to GAGs, in particular to HS (5, 17, 32, 37, 47, 50, 56). In this report, evidence for the selection of HS binding mutants in cell culture (BHK-21 cells) was obtained for a flavivirus, TBE virus.
One observation from this study that stands out very prominently is the large number of mutation patterns, all of which share the common property of increasing the net positive charge of protein E and being located within clusters of positively charged surface residues. All of these mutation patterns created local patches of surface area with increased positive surface charge similar to the three examples shown in Fig. 2. It is therefore likely that all of these mutations created HS binding sites. Characteristic primary sequence motifs of HS binding sites have been deduced from the analysis of known HS binding proteins (10, 29). In most of the sites created on the TBE virus E protein, however, inspection of the primary sequence alone would not allow them to be recognized as HS binding sites. In only one case (experiment 11; Glu 295→Lys) did the mutation create a sequence XBBXBX (where B is a basic amino acid and X is a hydrophobic amino acid) corresponding to one of the HS binding primary sequence motifs described by Cardin and Weintraub (10). In a few other cases, the mutations are next to or part of a cluster of three or four consecutive basic amino acids but do not match any of the classical binding motifs (10, 29). In the majority of cases, however, the basic amino acid residues are brought together only by the three-dimensional folding of the protein, demonstrating the limitations of predicting such functional sites from the primary sequence alone. Structural requirements for HS binding sites have been studied by solving the structures of protein-ligand complexes (29, 51, 57). In one case, such a study was performed with a virus, an HS binding strain of foot-and-mouth disease virus (21). In that report, the authors raised the question of whether the HS binding site had been created de novo by a particular mutation during cell culture adaptation or whether there was a structurally predisposed binding site that might have also been used during the natural infection of the host. Such preformed sites may play an important role for virus spread among different tissues and the establishment of persistent infection. Mutations occurring during infection could then modulate the tropism and pathogenicity of the virus. The large number of potential binding sites that we observed in protein E of TBE virus argues against the notion that the creation of such a site would require a very specific structural predisposition. It suggests instead that the structural requirements to create a binding site de novo are not very rigid. It remains to be investigated, however, to what extent the presence of existing mutations or the use of different passaging conditions influences the type and position of adaptive mutations that are favored. Although HS binding sites were formed almost everywhere on the TBE virus protein E surface, one region that remained free of mutations was the environment of the fusion peptide (2) located at the tip of domain II (Fig. 1). Interestingly, wild-type protein E already contains a predominantly positively charged surface around this area (Fig. 2) and one can speculate that a further increase of positive charge in this region might be structurally or functionally detrimental.
The biological characterization of the three recombinant mutants revealed that they shared a small plaque phenotype in PS cells and significant attenuation of their neuroinvasiveness in adult mice. Preliminary characterization of some of the other passaged mutants indicated that they also exhibited these characteristics (data not shown). Two of the mutations had been investigated previously in different contexts [mutation Ala 123→Lys in the monoclonal escape mutant VIE3 (31) and Thr 310→Lys as an engineered mutant, E(T310K) (41)] and were shown then to form small plaques and to be attenuated, which in the light of the results presented here can be interpreted as possibly being due to altered HS dependence. In fact, it seems likely that HS dependence could explain the attenuation of a considerable number of mutant flaviviruses described in the literature. A connection between HS dependence and attenuation in vivo was first recognized for Murray Valley encephalitis virus by Lee and Lobigs (39), who analyzed mutations specifically introduced into a putative receptor binding motif on the lateral surface of domain III. Inspection of previously described attenuated mutants of various flaviviruses carrying mutations within protein E (reviewed in reference 45) indicated that in a number of cases these mutations increased the net positive charge. Even widely used live vaccine strains of yellow fever virus (52) and Japanese encephalitis virus (49) exhibit, among other mutations elsewhere in the genome, this type of mutation in their protein E coding regions, suggesting that HS binding may be one of the attenuating principles of these vaccines.
The combination of HS binding with a small plaque phenotype and attenuation in vivo has also been observed for representatives of a growing number of other virus families (5, 9, 32, 36, 37, 39, 48, 56). The general conclusion arising from all of these studies is that attachment to HS provides a decisive selective advantage in cell culture but that in the natural host virus spread is impaired and clearance from the circulation is accelerated (5, 8, 9, 36). The available evidence from studies of very diverse virus families indicates that this is a very common mechanism of cell culture adaptation and attenuation which can be exploited for the design of nonpathogenic vaccine strains or vectors for gene delivery (16).
However, the fact that this adaptation is apparently common and occurs rapidly calls for attention to the possibility that laboratory strains might have suffered this kind of mutation during their original isolation and therefore could differ significantly in their biology from the virus populations circulating in nature. In the case of flaviviruses, dengue type 2 virus has been reported to utilize HS for infection (11). It is unclear whether the strain used in this study (a 1974 isolate from Tonga) had previously undergone an adaptive mutation or whether wild-type dengue virus in fact shows dependence on HS. TBE virus strain Neudoerfl, used as the wild-type strain in our study, has only a short passage history in baby mice and CE cells (26). The data presented here do not rule out the possibility that strain Neudoerfl interacts to some degree with HS, albeit with a lower affinity than that of the adapted mutants. Since attachment and uptake of TBE virus and other flaviviruses are still only poorly understood, a possible role for HS during entry of wild-type flaviviruses will deserve particular attention in future studies. The mutations identified in this study will aid to better define the structural requirements for interactions with HS and significantly increase our repertoire of molecular modifications that can be used to attenuate TBE virus as well as other flaviviruses.
ACKNOWLEDGMENTS
We gratefully acknowledge the excellent technical assistance of Heide Dippe, Silvia Röhnke, and Melby Wilfinger.
REFERENCES
- 1.Ada G. Overview of vaccines. Mol Biotechnol. 1997;8:123–134. doi: 10.1007/BF02752256. [DOI] [PubMed] [Google Scholar]
- 2.Allison S L, Schalich J, Stiasny K, Mandl C W, Heinz F X. Mutational evidence for an internal fusion peptide in flavivirus envelope protein E. J Virol. 2001;75:4268–4275. doi: 10.1128/JVI.75.9.4268-4275.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baeuerle P A, Huttner W B. Chlorate—a potent inhibitor of protein sulfation in intact cells. Biochem Biophys Res Commun. 1986;141:870–877. doi: 10.1016/s0006-291x(86)80253-4. [DOI] [PubMed] [Google Scholar]
- 4.Berger E A, Murphy P M, Farber J M. Chemokine receptors as HIV-1 coreceptors: roles in viral entry, tropism, and disease. Annu Rev Immunol. 1999;17:657–700. doi: 10.1146/annurev.immunol.17.1.657. [DOI] [PubMed] [Google Scholar]
- 5.Bernard K A, Klimstra W B, Johnston R E. Mutations in the E2 glycoprotein of Venezuelan equine encephalitis virus confer heparan sulfate interaction, low morbidity, and rapin clearance from blood of mice. Virology. 2000;276:93–103. doi: 10.1006/viro.2000.0546. [DOI] [PubMed] [Google Scholar]
- 6.Bernfield M, Götte M, Park P W, Reizes O, Fitzgerald M L, Lincecum J, Zako M. Functions of cell surface heparan sulfate proteoglycans. Annu Rev Biochem. 1999;68:729–777. doi: 10.1146/annurev.biochem.68.1.729. [DOI] [PubMed] [Google Scholar]
- 7.Bruett L, Barber S A, Clements J E. Characterization of a membrane-associated protein implicated in visna virus binding and infection. Virology. 2000;271:132–141. doi: 10.1006/viro.2000.0309. [DOI] [PubMed] [Google Scholar]
- 8.Byrnes A P, Griffin D E. Binding of Sindbis virus to cell surface heparan sulfate. J Virol. 1998;72:7349–7356. doi: 10.1128/jvi.72.9.7349-7356.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Byrnes A P, Griffin D E. Large-plaque mutants of Sindbis virus show reduced binding to heparan sulfate, heightened viremia, and slower clearance from the circulation. J Virol. 2000;74:644–651. doi: 10.1128/jvi.74.2.644-651.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cardin A D, Weintraub H J R. Molecular modeling of protein-glycosaminoglycan interactions. Arteriosclerosis. 1989;9:21–32. doi: 10.1161/01.atv.9.1.21. [DOI] [PubMed] [Google Scholar]
- 11.Chen Y, Maguire T, Hileman R E, Fromm J R, Esko J D, Linhardt R J, Marks R M. Dengue virus infectivity depends on envelope protein binding to target cell heparan sulfate. Nat Med. 1997;3:866–871. doi: 10.1038/nm0897-866. [DOI] [PubMed] [Google Scholar]
- 12.Chung C-S, Hsiao J-C, Chang Y-S, Chang W. A27L protein mediates vaccinia virus interaction with cell surface heparan sulfate. J Virol. 1998;72:1577–1585. doi: 10.1128/jvi.72.2.1577-1585.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clarke D H, Casals J. Techniques for hemagglutination and hemagglutination inhibition with arthropod-borne viruses. Am J Trop Med Hyg. 1958;7:561–573. doi: 10.4269/ajtmh.1958.7.561. [DOI] [PubMed] [Google Scholar]
- 14.Compton T, Nowlin D M, Cooper N R. Initiation of human cytomegalovirus infection requires initial interaction with cell surface heparan sulfate. Virology. 1993;193:834–841. doi: 10.1006/viro.1993.1192. [DOI] [PubMed] [Google Scholar]
- 15.Dechecchi M C, Tamanini A, Bonizzato A, Cabrini G. Heparan sulfate glycosaminoglycans are involved in adenovirus type 5 and type 2 host-cell interactions. Virology. 2000;268:382–390. doi: 10.1006/viro.1999.0171. [DOI] [PubMed] [Google Scholar]
- 16.Duisit G, Saleun S, Douthe S, Barsoum J, Chadeuf G, Moullier P. Baculovirus vector requires electrostatic interactions including heparan sulfate for efficient gene transfer in mammalian cells. J Gene Med. 1999;1:93–102. doi: 10.1002/(SICI)1521-2254(199903/04)1:2<93::AID-JGM19>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 17.Escarmis C, Carrillo E C, Ferrer M, Arriaza J F, Lopez N, Tami C, Verdaguer N, Domingo E, Franze-Fernandez M T. Rapid selection in modified BHK-21 cells of a foot-and-mouth disease virus variant showing alterations in cell tropism. J Virol. 1998;72:10171–10179. doi: 10.1128/jvi.72.12.10171-10179.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldmann S A, Hendry R M, Beeler J A. Identification of a linear heparin binding domain for human respiratory syncytial virus attachment glycoprotein G. J Virol. 1999;73:6610–6617. doi: 10.1128/jvi.73.8.6610-6617.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferlenghi I, Clarke M, Ruttan T, Allison S L, Schalich J, Heinz F X, Harrison S C, Rey F A, Fuller S O. Molecular organization of a recombinant subviral particle from tick-borne encephalitis virus. Mol Cell. 2000;7:593–602. doi: 10.1016/s1097-2765(01)00206-4. [DOI] [PubMed] [Google Scholar]
- 20.Flynn S J, Ryan P. A heterologous heparin-binding domain can promote functional attachment of a pseudorabies virus gC mutant to cell surfaces. J Virol. 1995;69:834–839. doi: 10.1128/jvi.69.2.834-839.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fry E E, Lea S M, Jackson T, Newman J W I, Ellard F M, Blakemore W E, Abu-Ghazaleh R, Samuel A, King A M Q, Stuart D I. The structure and function of a foot-and-mouth disease virus-oligosaccharide receptor complex. EMBO J. 1999;18:543–554. doi: 10.1093/emboj/18.3.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greve H, Cully Z, Blumberg P, Kresse H. Influence of chlorate on proteoglycan biosynthesis by cultured human fibroblasts. J Biol Chem. 1988;263:12886–12892. [PubMed] [Google Scholar]
- 23.Guirakhoo F, Heinz F X, Kunz C. Epitope model of tick-borne encephalitis virus envelope glycoprotein E: analysis of structural properties, role of carbohydrate side chain, and conformational changes occurring at acidic pH. Virology. 1989;169:90–99. doi: 10.1016/0042-6822(89)90044-5. [DOI] [PubMed] [Google Scholar]
- 24.Heinz F X, Allison S L. Structures and mechanisms in flavivirus fusion. Adv Virus Res. 2000;55:231–269. doi: 10.1016/S0065-3527(00)55005-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heinz F X, Berger R, Tuma W, Kunz C. A topological and functional model of epitopes on the structural glycoprotein of tick-borne encephalitis virus defined by monoclonal antibodies. Virology. 1983;126:525–537. doi: 10.1016/s0042-6822(83)80010-5. [DOI] [PubMed] [Google Scholar]
- 26.Heinz F X, Kunz C, Fauma H. Preparation of a highly purified vaccine against tick-borne encephalitis by continuous flow zonal ultracentrifugation. J Med Virol. 1980;6:213–221. doi: 10.1002/jmv.1890060304. [DOI] [PubMed] [Google Scholar]
- 27.Heinz F X, Stiasny K, Püschner-Auer G, Holzmann H, Allison S L, Mandl C W, Kunz C. Structural changes and functional control of the tick-borne encephalitis virus glycoprotein E by the heterodimeric association with protein prM. Virology. 1994;198:109–117. doi: 10.1006/viro.1994.1013. [DOI] [PubMed] [Google Scholar]
- 28.Heinz F X, Tuma W, Guirakhoo F, Kunz C. A model study of the use of monoclonal antibodies in capture enzyme immunoassays for antigen quantification exploiting the epitope map of tick-borne encephalitis virus. J Biol Stand. 1986;14:133–141. doi: 10.1016/0092-1157(86)90032-6. [DOI] [PubMed] [Google Scholar]
- 29.Hileman R E, Fromm J R, Weiler J M, Linhardt R J. Glycosaminoglycan-protein interactions: definition of consensus sites in glycosaminoglycan binding proteins. BioEssays. 1998;20:156–167. doi: 10.1002/(SICI)1521-1878(199802)20:2<156::AID-BIES8>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 30.Hilgard P, Stockert R. Heparan sulfate proteoglycans initiate dengue virus infection of hepatocytes. Hepatology. 2000;32:1069–1077. doi: 10.1053/jhep.2000.18713. [DOI] [PubMed] [Google Scholar]
- 31.Holzmann H, Stiasny K, Ecker M, Kunz C, Heinz F X. Characterization of monoclonal antibody-escape mutants of tick-borne encephalitis virus with reduced neuroinvasiveness in mice. J Gen Virol. 1997;78:31–37. doi: 10.1099/0022-1317-78-1-31. [DOI] [PubMed] [Google Scholar]
- 32.Hulst M M, van Gennip H G P, Moormann R J M. Passage of classical swine fever virus in cultured swine kidney cells selects virus variants that bind to heparan sulfate due to a single amino acid change in envelope protein Erns. J Virol. 2000;74:9553–9561. doi: 10.1128/jvi.74.20.9553-9561.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hung S-L, Lee P-L, Chen H-W, Chen L-K, Kao C-L, King C-C. Analysis of the steps involved in dengue virus entry into host cells. Virology. 1999;257:156–167. doi: 10.1006/viro.1999.9633. [DOI] [PubMed] [Google Scholar]
- 34.Jackson T, Ellard F M, Ghazaleh R A, Brookes S M, Blakemore W E, Corteyn A H, Stuart D I, Newman J W, King A M. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jan J T, Byrnes A P, Griffin D E. Characterization of a Chinese hamster ovary cell line developed by retroviral insertional mutagenesis that is resistant to Sindbis virus infection. J Virol. 1999;73:4919–4924. doi: 10.1128/jvi.73.6.4919-4924.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klimstra W B, Ryman K D, Bernard K A, Nguyen K B, Biron C A, Johnston R E. Infection of neonatal mice with Sindbis virus results in a systemic inflammatory response syndrome. J Virol. 1999;73:10387–10398. doi: 10.1128/jvi.73.12.10387-10398.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klimstra W B, Ryman K D, Johnston R E. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J Virol. 1998;72:7357–7366. doi: 10.1128/jvi.72.9.7357-7366.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krusat T, Streckert H J. Heparin-dependent attachment of respiratory syncytial virus (RSV) to host cells. Arch Virol. 1997;142:1247–1254. doi: 10.1007/s007050050156. [DOI] [PubMed] [Google Scholar]
- 39.Lee E, Lobigs M. Substitutions at the putative receptor-binding site of an encephalitic flavivirus alter virulence and host cell tropism and reveal a role for glycosaminoglycan in entry. J Virol. 2000;74:8867–8875. doi: 10.1128/jvi.74.19.8867-8875.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin C-L, Chung C-S, Heine H G, Chang W. Vaccinia virus envelope H3L protein binds to cell surface heparan sulfate and is important for intracellular mature virion morphogenesis and virus infection in vitro and in vivo. J Virol. 2000;74:3353–3365. doi: 10.1128/jvi.74.7.3353-3365.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mandl C W, Allison S L, Holzmann H, Meixner T, Heinz F X. Attenuation of tick-borne encephalitis virus by structure-based site-specific mutagenesis of a putative flavivirus receptor binding site. J Virol. 2000;74:9601–9609. doi: 10.1128/jvi.74.20.9601-9609.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mandl C W, Ecker M, Holzmann H, Kunz C, Heinz F X. Infectious cDNA clones of tick-borne encephalitis virus European subtype prototypic strain Neudoerfl and high virulence strain Hypr. J Gen Virol. 1997;78:1049–1057. doi: 10.1099/0022-1317-78-5-1049. [DOI] [PubMed] [Google Scholar]
- 43.Mandl C W, Guirakhoo F, Holzmann H, Heinz F X, Kunz C. Antigenic structure of the flavivirus envelope protein E at the molecular level, using tick-borne encephalitis virus as a model. J Virol. 1989;63:564–571. doi: 10.1128/jvi.63.2.564-571.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mandl C W, Holzmann H, Meixner T, Rauscher S, Stadler P F, Allison S L, Heinz F X. Spontaneous and engineered deletions in the 3′ noncoding region of tick-borne encephalitis virus: construction of highly attenuated mutants of a flavivirus. J Virol. 1998;72:2132–2140. doi: 10.1128/jvi.72.3.2132-2140.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McMinn P C. The molecular basis of virulence of the encephalitogenic flaviviruses. J Gen Virol. 1997;78:2711–2722. doi: 10.1099/0022-1317-78-11-2711. [DOI] [PubMed] [Google Scholar]
- 46.Mondor I, Ugolini S, Sattentau Q J. Human immunodeficiency virus type 1 attachment to HeLa CD4 cells is CD4 independent and gp120 dependent and requires cell surface heparans. J Virol. 1998;72:3623–3634. doi: 10.1128/jvi.72.5.3623-3634.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moulard M, Lortat-Jacob H, Mondor I, Roca G, Wyatt R, Sodroski J, Zhao L, Olson W, Kwong P D, Sattentau Q J. Selective interactions of polyanions with basic surfaces on human immunodeficiency virus type 1 gp120. J Virol. 2000;74:1948–1960. doi: 10.1128/jvi.74.4.1948-1960.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neff S, Sa-Carvalho D, Rieder E, Mason P W, Blystone S D, Brown E J, Baxt B. Foot-and-mouth disease virus virulent for cattle utilizes the integrin alpha(v)beta3 as its receptor. J Virol. 1998;72:3587–3594. doi: 10.1128/jvi.72.5.3587-3594.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nitayaphan S, Grant J A, Chang G-J J, Trent D W. Nucleotide sequence of the virulent SA-14 strain of Japanese encephalitis virus and its attenuated derivative, SA-14-14-2. Virology. 1990;177:541–552. doi: 10.1016/0042-6822(90)90519-w. [DOI] [PubMed] [Google Scholar]
- 50.Patel M, Yanagishita M, Roderiquez G, Bou-Habib D C, Oravecz T, Hascall V C, Norcross M A. Cell-surface heparan sulfate proteoglycan mediates HIV-1 infection of T-cell lines. AIDS Res Hum Retrovir. 1993;9:167–174. doi: 10.1089/aid.1993.9.167. [DOI] [PubMed] [Google Scholar]
- 51.Pellegrini L, Burke D F, von Delft F, Mulloy B, Blundell T L. Crystal structure of fibroblast growth factor receptor ectodomain bound to ligand and heparin. Nature. 2000;407:1029–1034. doi: 10.1038/35039551. [DOI] [PubMed] [Google Scholar]
- 52.Post P R, Santos C N D, Carvalho R, Cruz A C R, Rice C M, Galler R. Heterogeneity in envelope protein sequences and N-linked glycosylation among yellow fever virus vaccine strains. Virology. 1992;188:160–167. doi: 10.1016/0042-6822(92)90745-b. [DOI] [PubMed] [Google Scholar]
- 53.Qiu J, Handa A, Kirby M, Brown K E. The interaction of heparin sulfate and adeno-associated virus 2. Virology. 2000;269:137–147. doi: 10.1006/viro.2000.0205. [DOI] [PubMed] [Google Scholar]
- 54.Reed J L, Muench H. A simple method for estimating fifty percent endpoints. Am J Hyg. 1938;27:493. [Google Scholar]
- 55.Rey F A, Heinz F X, Mandl C, Kunz C, Harrison S C. The envelope glycoprotein from tick-borne encephalitis virus at 2 Å resolution. Nature. 1995;375:291–298. doi: 10.1038/375291a0. [DOI] [PubMed] [Google Scholar]
- 56.Sa-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P W. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schlessinger J, Plotnikov A N, Ibrahimi O A, Eliseenkova A V, Yeh B K, Yayon A, Linhardt R J, Mohammadi M. Crystal structure of a ternary FGF-FGFR-heparin complex reveals a dual role for heparin in FGFR binding and dimerization. Mol Cell. 2000;6:743–750. doi: 10.1016/s1097-2765(00)00073-3. [DOI] [PubMed] [Google Scholar]
- 58.Schneider-Schaulies J. Cellular receptors for viruses: links to tropism and pathogenesis. J Gen Virol. 2000;81:1413–1429. doi: 10.1099/0022-1317-81-6-1413. [DOI] [PubMed] [Google Scholar]
- 59.Secchiero P, Sund D, De Vico A L, Crowley R W, Reitz M S, Jr, Zauli G, Lusso P, Gallo R C. Role of the extracellular domain of human herpesvirus 7 glycoprotein B in virus binding to cell surface heparan sulfate proteoglycans. J Virol. 1997;71:4571–4580. doi: 10.1128/jvi.71.6.4571-4580.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shukla D, Liu J, Blaiklock P, Shworak N W, Bai X, Esko J D, Cohen G H, Eisenberg R J, Rosenberg R D, Spear P G. A novel role for 3-O-sulfated heparan sulfate in herpes simplex virus 1 entry. Cell. 1999;99:13–22. doi: 10.1016/s0092-8674(00)80058-6. [DOI] [PubMed] [Google Scholar]
- 61.Skrincosky D, Hocknell P, Whetter L, Secchiero P, Chandran B, Dewhurst S. Identification and analysis of a novel heparin-binding glycoprotein encoded by human herpesvirus 7. J Virol. 2000;74:4530–4540. doi: 10.1128/jvi.74.10.4530-4540.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Summerford C, Samulski R J. Membrane-associated heparan sulfate proteoglycan is a receptor for adeno-associated virus type 2 virions. J Virol. 1998;72:1438–1445. doi: 10.1128/jvi.72.2.1438-1445.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tufaro F. Virus entry: two receptors are better than one. Trends Microbiol. 1997;5:257–260. doi: 10.1016/S0966-842X(97)01057-3. [DOI] [PubMed] [Google Scholar]
- 64.Tumova S, Woods A, Couchman J R. Heparan sulfate proteoglycans on the cell surface: versatile coordinators of cellular functions. Int J Biochem Cell Biol. 2000;32:269–288. doi: 10.1016/s1357-2725(99)00116-8. [DOI] [PubMed] [Google Scholar]
- 65.Ugolini S, Mondor I, Sattentau Q J. HIV-1 attachment: a second look. Trends Microbiol. 1998;7:144–149. doi: 10.1016/s0966-842x(99)01474-2. [DOI] [PubMed] [Google Scholar]
- 66.van Regenmortel M H V, Fauquet C M, Bishop D H L, Carstens E B, Estes M K, Lemon S M, Maniloff J, Mayo M A, McGeoch D J, Pringle C R, Wickner R B, editors. Virus taxonomy: classification and nomenclature of viruses. London, England: Academic Press; 2000. pp. 859–878. [Google Scholar]
- 67.Vázquez M-I, Esteban M. Identification of functional domains in the 14-kilodalton envelope protein (A27L) of vaccinia virus. J Virol. 1999;73:9098–9109. doi: 10.1128/jvi.73.11.9098-9109.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wallner G, Mandl C W, Kunz C, Heinz F X. The flavivirus 3′-noncoding region: extensive size heterogeneity independent of evolutionary relationships among strains of tick-borne encephalitis virus. Virology. 1995;213:169–178. doi: 10.1006/viro.1995.1557. [DOI] [PubMed] [Google Scholar]
- 69.Wallner G, Mandl C W, Ecker M, Holzmann H, Stiasny K, Kunz C, Heinz F X. Characterization and complete genome sequences of high- and low-virulence variants of tick-borne encephalitis virus. J Gen Virol. 1996;77:1035–1042. doi: 10.1099/0022-1317-77-5-1035. [DOI] [PubMed] [Google Scholar]
- 70.WuDunn D, Spear D. Initial interaction of herpes simplex virus with cells is binding to heparan sulfate. J Virol. 1989;63:52–58. doi: 10.1128/jvi.63.1.52-58.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]