Abstract
Bariatric interventions, both surgical and medical, are increasingly employed by patients to achieve weight reduction and enhance overall health. However, there is growing concern about the associated changes in soft tissue facial aesthetics resulting from these interventions. In this systematic review, the authors aimed to analyze the existing literature regarding soft tissue facial changes after bariatric interventions, with a focus on the influence of massive weight loss on facial aging, attractiveness, and considerations for facial rejuvenation. A systematic review was conducted until February 10, 2024, using electronic databases such as PubMed, Scopus, Web of Science, Embase, and Google Scholar. This review was registered in the open science framework. The Covidence software (Melbourne, VIC, Australia) facilitates title, abstract, and full-text screening, as well as data extraction. In total, 309 papers were identified, 94 duplicates were removed, and 194 studies were excluded on the basis of inclusion criteria. Of the remaining 21 studies, 13 met the inclusion criteria with an additional single study from the conference abstract. Descriptive analysis was conducted. We observed a correlation between massive weight loss and facial aging. The most significant fat regional devolumization was observed along the mid-cheek region and with central neck skin laxity. The apparent age of patients was higher among those with massive weight loss. In our study, we demonstrated that massive weight loss causes accelerated facial aging, manifested through fat devolumization, and increased skin laxity. Further quantitative volumetric facial analyses postbariatric surgery would yield valuable results.
Level of Evidence: 3 (Therapeutic)

The number of patients who undergo bariatric surgery is increasing,1 and the pendulum has shifted toward less invasive bariatric inventions, including medical Glucagon-like peptide (GLP-1) agonists such as Ozempic (Novo Nordisk, Bagsværd, Denmark).2 In our practice of facial plastic and reconstructive surgery, an increasing number of patients are concerned about facial changes as a result of massive weight loss. Because GLP-1 agonists have become more popular among the general population, concerns regarding facial soft tissue changes have risen. Increasingly known as “Ozempic faces,”3 an increasing number of patients are presenting to various facial plastic surgery practices with displeasure over their facial changes following massive weight loss, which can have emotional and psychosocial sequel.4 There are few publications in the literature in which researchers highlight the facial changes that occur because of massive weight loss. In previous publications in plastic surgery, researchers focused on body contouring of the trunk and extremities, and there are very limited publications in the literature in which researchers highlight the facial changes that occur as a result of massive weight loss. Our primary objective in this scoping review is to highlight recent publications in the literature on facial changes following massive weight loss and illustrate any recommendations for facial rejuvenation with the secondary objective of identifying gaps in the literature for future research directions.
METHODS
A systematic scoping review based on the preferred reporting items for systematic reviews and meta-analysis scoping review (PRISMA-ScR) guidelines was performed on February 10, 2024, encompassing publications dating back to 2005. The research databases used included PubMed, Scopus, Web of Science, Embase, and Google Scholar. The search terms used were “weight loss or bariatric intervention or Ozempic or GLP-1 agonist” AND “facial changes or neck changes or facial aesthetics or facial cosmetics or facial ageing.” Inclusion criteria were text in English, full text, and primary original studies addressing facial changes following massive weight loss secondary to bariatric intervention from the year 2005 to February 10, 2024. Exclusion criteria were non-English studies, studies on bariatric intervention with body changes, and orthognathic changes. In addition to the peer-reviewed search, an online gray literature search was conducted, specifically looking at conference proceedings, abstracts, and published information from various medical online platforms. The Covidence (Melbourne, VIC, Australia) software was used to conveniently facilitate study screening and data extraction. Two reviewers (A.B.J. and J.J.) independently screened all abstracts to identify studies that fulfilled predetermined eligibility criteria. Any disagreements between reviewers were resolved by consensus. Qualitative data from each included study were extracted using standardized data from Covidence, as per our set data collection protocol. Two reviewers independently analyzed the data, and any discrepancies were resolved by consensus.
RESULTS
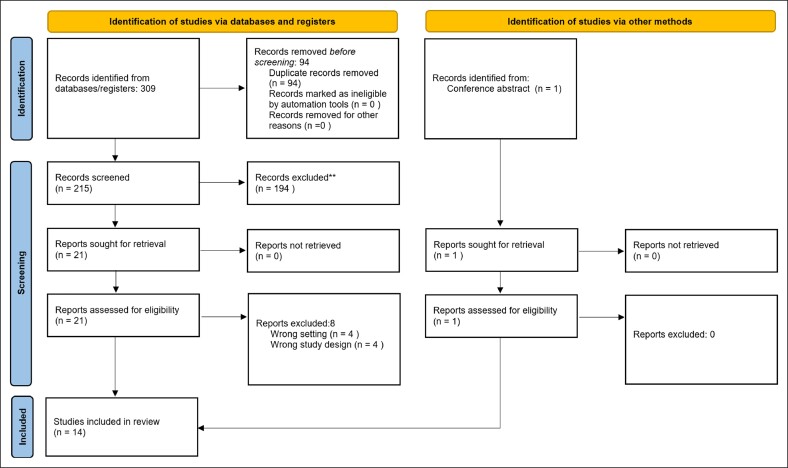
A total of 309 articles were identified, of which 184 were from PubMed, 42 from Embase, 39 from Web of Science, and 44 from Google Scholar. We identified 94 duplicates that were removed, leaving 215 abstract studies for screening. Of the 215 studies, 194 did not meet our inclusion criteria, 21 met the eligibility criteria, of those 21, 8 were excluded because of incorrect study design. A total of 13 studies underwent complete qualitative analysis with data extraction. Another study was included from a conference abstract presented at the annual 2023 AAFPRS meeting (Figure 1), outlining the 2020-PRISMA summary of our scoping review.
Figure 1.
A PRISMA 2020 flow diagram for new systematic reviews that included searches of databases, registers, and other sources. *Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools.5 For more information, visit: http://www.prisma-statement.org/.
Study Demographics
Of these 14 studies, 11 studies involved bariatric surgery as the main intervention for weight loss; however, only in 2 papers, opinions on the effect of Ozempic (GLP-1 agonist) on facial changes3,6 were provided and objective data on facial changes post-Ozempic use were provided in one.7 The majority of studies were conducted in the United States (n = 6),6-11 Europe (n = 4),3,12-14 with a minority in South America (n = 2)15,16 and Australia (n = 1).17 In all primary studies, patients with preoperative BMI >40 or BMI >35 with other medical comorbidities9,10,12,15 with an age range of >18 years and an average age of 40 were included. In the majority of studies, information on ethnicity was not included; in only 4 studies, the ethnicity of patients was reported, all of whom were Caucasian.7,9,15,17 The most common bariatric surgical intervention was the roux-En-y procedure, followed by gastric sleeve surgery and medical management, including Ozempic. A summary of studies outlining facial changes secondary to bariatric interventions causing weight loss is presented in Supplemental Tables 1 and 2.
Facial Volume Changes
In general, the authors of the majority of studies concluded qualitatively that, following bariatric intervention, massive weight loss results in significant facial volumetric changes that resemble facial aging. Midfacial volume loss is the most significant volumetric change noted by deep nasolabial folds and malar eminence flattening, followed by skin laxity in the submental region.8-11,17 In 3 studies, the authors evaluated the effects of Ozempic on facial changes and concluded that with the use of Ozempic, they noted volume changes along the midfacial region, periorbital region, temples, and an increased number of facial wrinkles.3,6 In 1 study, researchers showed that patients on Ozempic appeared 5 years older than those without.6 In only 1 study, authors performed objective volumetric facial analyses on 5 participants taking Ozempic and found a reduction in the superficial temporal fat pad by an average of 41.8% and a reduction in the cheek fat pad by an average of 69.9%.7
Facial Rejuvenation Procedures
In only 3 studies, the authors provided information on facial rejuvenation interventions after massive weight loss. Couto et al reported that among 7 patients with massive weight loss postbariatric surgery who experienced facial changes, 5 patients underwent an extended superficial musculoaponeurotic system facelift, whereas 1 patient underwent lateral SMAS sectomy and 1 SMAS plication.9 All 7 patients in their cohort underwent submental lipectomy and platysmaplasty. They concluded that patients with massive weight loss would require earlier and more frequent facelift revision because of marked skin excess.9 Narasimhan et al reported in their study of 22 patients that 91% underwent SMAS facelift, and all underwent fat augmentation. Their study also concluded that patients with massive weight loss required almost twice as much fat augmentation as patients with nonmassive weight loss.10 Humphrey et al provided opinion that in patients with massive weight loss, an extended facelift or deep plane technique would achieve more optimal results, because it addresses the neck region with more redundant skin laxity.6 In terms of nonsurgical interventions, Tay et al recommended hyaluronic acid dermal fillers as an effective treatment for enhancing the appearance of “Ozempic faces”.3
DISCUSSION
Apparent Age Changes and Facial Volume Differences in Massive Weight Loss Population Following Bariatric Surgeries
Bariatric surgery causes changes in facial appearance with a profound impact on regional facial fat loss.18 However, there are limited publications in the literature in which authors describe the quantity of facial fat loss and the regional distribution of loss. In some studies, authors compare facial changes after massive weight loss to facial aging; however, our understanding of the mechanics and pathophysiological differences is limited; thus, such comparative resemblance might not be precisely accurate.19 The dynamic changes in facial aesthetics after massive weight loss predominantly pertain to the loss of subcutaneous fat in a younger demographic, characterized by favorable skin texture and a robust facial musculoskeletal framework.20 Bariatric interventions lead to rapid weight loss over a short period, resulting in perceptible alterations in facial age perception.
Among the earliest investigations of facial age perception following bariatric surgery was a study involving 14 patients from bariatric clinics performed by Papoian et al.11 They utilized pre- and postweight loss photographs to assess perceived age and overall attractiveness. Although the results were heterogeneous, mild weight loss was associated with the perception of increased youthfulness but decreased attractiveness. In contrast, patients who showed substantial weight loss were perceived to look older postoperatively but were more attractive. However, the small sample size and short follow-up period are acknowledged as limitations of this study.11 In a subsequent study, Valente et al15 conducted a prospective cohort study that included a larger sample size and longer follow-up period to evaluate facial age perception among morbidly obese patients. The mean facial age perception before bariatric surgery was 40.8, whereas after bariatric surgery, the mean facial age increased to 43.7. In the study, the authors also observed that older people (>40 years) were more susceptible to changes in facial volume caused by weight loss compared with younger individuals. This can be explained by the fact that patients >40 years of age have already encountered facial aging in addition to changes after weight loss, which accelerates the process of facial aging with older perceived age.15
Although authors have addressed regional variations in facial fat loss postbariatric surgery, few have objectively documented these changes in their studies. Narasimhan et al10 examined 22 patients with an average initial BMI of 38 at the time of recruitment, and postbariatric surgery, the average BMI dropped to 26 to 27. The main facial regions that showed significant changes included 88% volume loss in the midface and nasolabial folds, followed by 82% platysma band formation. The authors observed excess skin and redundancy in the jowl and submental regions and noted ∼60% perioral volume loss.10 Biörserud et al13 performed a study in which excess skin was objectively measured in postbariatric surgery. The mean postoperative BMI difference was 44.7, and the patients had accompanying increased neck skin and chin ptosis.
The anatomical considerations of facial fat, as elucidated by Rohrich and Pessa's compartmentalization into superficial and deep layers, provide a basis for speculation of the differential effects of weight loss on these compartments.21 Although controversial among facial plastic surgeons, 1 argues that with massive weight loss, facial fat volume decreases in the superficial fat compartment before it does in the deep fat compartment, which could be a culprit for pseudoptosis and apparent aging among this population. However, there has not yet been a researcher who has quantitatively assessed this aspect in their study. We believe that this understanding will be important when it comes to facial rejuvenation procedures, and thus, further research is required. In addition, it has become apparent that certain regional areas of the face more readily lose fat than others, and such patterned topographical changes will appear in 1 area more than another. However, it remains to be studied whether certain facial fat compartments respond differently to massive weight loss, and whether GLP-1 agonists impact traditional bariatric surgical methods of weight loss differently; thus, direct comparisons are currently limited. Interestingly, the authors of many of the published studies identified in the literature evaluated massive weight loss that occurred at a rapid pace; however, there are no comparative studies in which authors assessed the impact of gradual weight loss on facial changes.
Furthermore, it is necessary to explore comparisons between age-related changes in the older population and the related apparent aging caused by volumetric facial fat loss in the younger population. Younger patients have more robust osteocutaneous and fasciocutaneous ligaments, and skin elasticity and integrity; thus, the mechanism of facial aesthetic changes might not resemble those of facial aging caused by loss of skin texture, effects of gravity, underlying muscular weakness, and bony resorption. For example, the buccal fat pad is considered a deep facial fat compartment. The volume is not affected by body habitus but has been shown to degenerate with age, resulting in “pseudoptosis.” However, some authors in their studies suggest that buccal fat pads appear to be more resistant to changes following weight loss because of robust blood supply. To date, no clinical study has been performed to address the changes in the buccal fat pad in younger patients who have undergone significant weight loss.
Scalafani et al8 noted that with massive weight loss, there is often excess loose skin, typically in the submental area, followed by jowl. Although platysmal bands are not typically seen as 1 would see in aging, the authors of this study concluded that preexisting pre- and postsubplatysmal fat accumulation leads to the stretching of the skin and that weight loss is associated with loose skin excess.8 They also noted that the perioral complex would generally need to be restored, because fat loss from the lips and cheeks after bariatric surgery accelerates lip atrophy and nasolabial folding. Furthermore, Peters et al12 evaluated morphological changes in the face of obese patients during massive weight loss who had undergone bariatric surgery (gastric sleeve technique or gastric bypass) and found that skin laxity and sagging of the face and neck in a vertical downward direction are the main findings in bariatric patients with massive weight loss as a result of underlying fat volume deflation.12
GLP-1 Agonist Medical Treatment for Weight Loss
GLP-1 agonists (eg, Ozempic and others) have grown in popularity as noninvasive, relatively affordable medical interventions for weight loss.22 These medications regulate weight loss by decreasing appetite and delay gastric emptying.23 Recently, various facial plastic surgeons have observed an increasing number of referrals for facial rejuvenation among younger patients who utilize GLP-1 agonists. The term “Ozempic faces” has been adopted by numerous facial aesthetic physicians and surgeons because these medications induce rapid fat loss in key areas, accentuating wrinkles and causing skin laxity in various facial regions. However, researchers of clinical trials rarely report facial fat loss as an adverse event, leading to under-recognition by providers and insufficient counseling for potential side effects. We found only 2 studies in the literature related to GLP-1 use and facial changes. The authors of both papers discuss Ozempic qualitatively, without an objective assessment. Tay et al discuss topographical facial changes following the use of Ozempic for weight loss.3 Loss of facial fat leads to the loss of volume and fullness in the cheeks, temples, chins, and periorbital area, resulting in a hollowed-out appearance that accentuates wrinkles and sagging skin. Furthermore, Humphrey et al published a report to express professional opinion in the literature.6 Dr Humphrey mentioned that with the rapid fat loss in patients taking Ozempic, wrinkles become more prominent and the skin begins to sag in areas such as temples, cheeks, tear troughs, jawline, marionette lines, and nasolabial folds. Ozempic can also cause lesser degree changes in the size of the lips, cheeks, and chin that disturb facial balance. Changes can occur in the facial skin, in which there is loss of collagen, elastin, and essential nutrients. Patients who experience massive weight loss appear up to 5 years older than those of similar ages without a history of extensive weight loss. Recently, a group from Upstate University Hospital led by the author Neal Deot et al published an abstract at the 2023 AAFPRS scientific meeting aimed at quantitatively examining volumetric changes of facial fat pads, especially temporal and buccal fat pads, among patients using Ozempic. A retrospective study was performed on 5 adult patients who used Ozempic, with multiple facial imaging scans obtained throughout the treatment period. A 3-dimensional slicer was used for volumetric analysis and segmentation was achieved by isolating the fat planes. The average loss of body weight was 21.1% over a mean follow-up time of 9.4 months. There was a decrease in superficial temporal fat pad volume by an average of 41.8% and a decrease of 69.9% in fat volume loss along the superficial cheek fat over the treatment period. However, this study had many limitations, which included only Caucasian patients, a 4:1 female-to-male ratio, and only 2 facial regions examined.
Facial Rejuvenation Following Massive Weight Loss
Following bariatric intervention, the researchers of many publications have observed that the most significant and common changes that occur following massive weight loss include midface fat loss, resulting in pseudoptosis and a deepening of the nasolabial folds as primary changes, excess skin laxity in the lower face and neck, and some perioral changes as secondary changes. Therefore, soft tissue augmentation, repositioning, and lifting are the key considerations for patients after significant weight loss. However, surgical interventions should be deferred until patients achieve weight stabilization, typically 3 to 6 months postbariatric surgery.24 Medical confounding factors, such as diabetes, anemia, and multivitamin deficiencies must be addressed preoperatively to optimize postoperative healing. Counseling is imperative, emphasizing realistic expectations and the potential need for multiple revision procedures. The preoperative counseling process should note areas of skin excess, especially in submental neck areas, facial fat loss or redistribution depicted by midface hollowness, pseudo-fat ptosis, increased nasolabial folds, jowling, and periorbital and perioral changes.
Couto et al9 conducted a compelling comparison between soft tissue facial changes and their correlation with actual vs apparent age among patients with massive vs nonmassive weight loss. Their findings revealed that patients in the massive weight loss group were 5.1 years older than the actual age, whereas those in the nonmassive weight loss group were 1.2 years older than the actual age following bariatric surgery. Most noteworthy, facial changes included deepened nasolabial folds, midface descent, and central neck laxity. Therefore, the authors recommend an extended SMAS face/neck lift. All patients with massive weight loss underwent lipectomy and platysmaplasty, with >85.7% receiving other adjuvant procedures. They concluded that patients with massive weight loss would require earlier and more frequent facelift revisions because of marked skin excess. These patients would also benefit from facelift with fat augmentation to provide a more youthful rejuvenated face. Narasimhan et al also investigated rejuvenative options.10 The authors considered SMAS facelift and fat augmentation as the treatment options for these patients. They also mentioned that almost twice as much autologous fat augmentation was required for massive weight loss patients compared with nonmassive weight loss patients to restore the volume loss. Humphrey et al provided a similar opinion with advocation for lower facelift to address the jowl and neck area.6 Noninvasive alternatives such as dermal fillers were recommended by Tay et al for postweight loss in the Ozempic population.3 Similarly, Humphrey recommended the use of noninvasive facial rejuvenation methods such as dermal fillers, calcium hydroxyapatite, Poly-L-Lactic acid (PLLA), or other radiofrequency (RF) energy–based devices.
Some considerations must be taken be into account while providing rejuvenation surgery (face/neck lift) for patients with weight loss postbariatric surgery. Postbariatric rhytidectomy patients are generally younger than traditional patients with aging faces. These patients are often reluctant to commit to a specific hairstyle to camouflage occipital scars. The vector of elevation in the neck can be mostly superior, and with care, incision across the mastoid skin and into the hairline can be avoided. Patients appreciate the absence of this obvious portion of the scar, especially when seeking to resume a more active and athletic lifestyle. Correction of the deformity requires significantly more skin undermining than does typical rhytidectomy. The inelasticity of the skin increases the chance of a “lateral sweep” and it is important that the skin flap be elevated and redraped in a smooth, tension-free manner. Although SMAS elevation and imbrication are performed in a standard fashion, they do not address the lift midface and nasolabial folds; thus, the counseling process of patients should include deep plane facelift to achieve satisfactory results. Fat reduction in the submental triangle and jowl areas can be judiciously performed to assist in creating a smooth, contoured, and sculpted neckline. In the midline, paramedian platysma bands are identified, and the edges are undermined from the submental crease inferiorly to the cricoid cartilage to provide adequate midline neck tightening.
Limitations and Future Directions
In spite of the fact that the authors of the present study offer valuable insights into facial changes following bariatric surgery, the study is not without its limitations. There is a tremendous paucity of quantitative studies in the literature in which authors evaluate the consequences of massive weight changes on facial volumetric differences. Further studies are recommended to evaluate the temporal relationships of the rapidity of facial volumetric changes following specific bariatric interventions. This would provide quantifiable outcomes that would help facial plastic surgeons and patients understand the changes and aid in better counseling. The relatively short follow-up periods in the majority of studies also limit our ability to discern the long-term effects of bariatric surgery on patients' facial morphology, because weight change can be dynamic among certain patients. Furthermore, the predominantly Caucasian representation of patients in some studies could skew the outcomes and underscore the broader ethnic diversity; thus, future studies are needed to better report different ethnic groups.
To date, there is a paucity of data to provide an objective evaluation of soft tissue facial changes following GLP-1 agonist administration despite its popularity among many patients. We suggest that the authors of any future study design should also bear in mind a longitudinal evaluation over varying doses of GLP-1 agonists, noting changes to soft tissue facial changes.
Lastly, seeking a consensus opinion from expert facial plastic surgeons in formulating a management algorithm for individuals experiencing facial changes postbariatric intervention is crucial, because it could enhance the clinical applicability and relevance of the study’s findings. In light of these limitations, researchers of future endeavors should address these gaps to further enrich our understanding of the complex relationship between bariatric interventions and facial morphology.
CONCLUSIONS
In our study, we provide compelling evidence that bariatric interventions can result in significant changes in facial appearance following massive weight loss. We observed accelerated facial aging because of fat devolumization and increased skin laxity. Given the paucity of literature on this topic, we advocate for further research depicting the longitudinal volumetric analysis of soft tissue facial changes following bariatric interventions. This is especially pertinent considering the increasing utilization of GLP-1 agonists in the general population.
Supplementary Material
Supplemental Material
This article contains supplemental material located online at https://doi.org/10.1093/asjof/ojae069.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1. Lazzati A. Epidemiology of the surgical management of obesity. J Visc Surg. 2023;160(2S):S3–S6. doi: 10.1016/j.jviscsurg.2022.12.004 [DOI] [PubMed] [Google Scholar]
- 2. Tan HC, Dampil OA, Marquez MM. Efficacy and safety of semaglutide for weight loss in obesity without diabetes: a systematic review and meta-analysis. J ASEAN Fed Endocr Soc. 2022;37(2):65–72. doi: 10.15605/jafes.037.02.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tay JQ. Ozempic face: a new challenge for facial plastic surgeons. J Plast Reconstr Aesthet Surg. 2023;81:97–98. doi: 10.1016/j.bjps.2023.04.057 [DOI] [PubMed] [Google Scholar]
- 4. Sarwer DB, Fabricatore AN. Psychiatric considerations of the massive weight loss patient. Clin Plast Surg. 2008;35(1):1–10. doi: 10.1016/j.cps.2007.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Humphrey CD, Lawrence AC. Implications of Ozempic and other semaglutide medications for facial plastic surgeons. Facial Plast Surg. 2023;39:719–721. doi: 10.1055/a-2148-6321 [DOI] [PubMed] [Google Scholar]
- 7. Neal Deot M, Hughes E, Hatala A, Debick N, Suryadevara A. AAFPRS Annual Meeting 2023, Las Vegas, NV: Upstate University; October 2023.
- 8. Sclafani AP. Restoration of the jawline and the neck after bariatric surgery. Facial Plast Surg. 2005;21(1):28–32. doi: 10.1055/s-2005-871760 [DOI] [PubMed] [Google Scholar]
- 9. Couto RA, Waltzman JT, Tadisina KK, et al. Objective assessment of facial rejuvenation after massive weight loss. Aesthet Plast Surg. 2015;39(6):847–855. doi: 10.1007/s00266-015-0540-6 [DOI] [PubMed] [Google Scholar]
- 10. Narasimhan K, Ramanadham S, Rohrich RJ. Face lifting in the massive weight loss patient: modifications of our technique for this population. Plast Reconstr Surg. 2015;135(2):397–405. doi: 10.1097/prs.0000000000000881 [DOI] [PubMed] [Google Scholar]
- 11. Papoian V, Mardirossian V, Hess DT, Spiegel JH. Effects of bariatric surgery on facial features. Arch Plast Surg. 2015;42(5):567–571. doi: 10.5999/aps.2015.42.5.567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peters F, Kroh A, Neumann UP, et al. Morphological changes of the human face after massive weight-loss due to bariatric surgery. J Craniomaxillofac Surg. 2020;48(7):694–699. doi: 10.1016/j.jcms.2020.05.010 [DOI] [PubMed] [Google Scholar]
- 13. Biörserud C, Fagevik Olsén M, Elander A, Wiklund M. Objective measurements of excess skin in post bariatric patients–inter-rater reliability. J Plast Surg Hand Surg. 2016;50(2):68–73. doi: 10.3109/2000656x.2015.1089876 [DOI] [PubMed] [Google Scholar]
- 14. Pokrowiecki R. Extended buccal lipectomy (bichectomy) for extreme cheek contouring. Int J Oral Maxillofac Surg. 2022;51(7):929–932. doi: 10.1016/j.ijom.2021.09.003 [DOI] [PubMed] [Google Scholar]
- 15. Valente DS, Braga da Silva J, Cora Mottin C, et al. Influence of massive weight loss on the perception of facial age: the facial age perceptions cohort. Plast Reconstr Surg. 2018;142(4):481e–488e. doi: 10.1097/prs.0000000000004738 [DOI] [PubMed] [Google Scholar]
- 16. Santos ME, Laureano Filho JR, Campello RI, Campos JM, Ferraz AA. Improvement in respiration and craniofacial changes associated with weight loss after bariatric surgery. J Oral Maxillofac Surg. 2011;69(6):e177–e185. doi: 10.1016/j.joms.2010.07.079 [DOI] [PubMed] [Google Scholar]
- 17. Sutherland K, Lee RW, Phillips CL, et al. Effect of weight loss on upper airway size and facial fat in men with obstructive sleep apnoea. Thorax. 2011;66(9):797–803. doi: 10.1136/thx.2010.151613 [DOI] [PubMed] [Google Scholar]
- 18. Wong ZY, Ramasamy P, Ingels K, Parmar C, Yang W, Pouwels S. Changes of facial features after bariatric surgery: a systematic review. Obes Surg. 2023;33(1):332–338. doi: 10.1007/s11695-022-06363-8 [DOI] [PubMed] [Google Scholar]
- 19. Freytag L, Alfertshofer MG, Frank K, et al. Understanding facial aging through facial biomechanics: a clinically applicable guide for improved outcomes. Facial Plast Surg Clin North Am. 2022;30(2):125–133. doi: 10.1016/j.fsc.2022.01.001 [DOI] [PubMed] [Google Scholar]
- 20. Swift A, Liew S, Weinkle S, Garcia JK, Silberberg MB. The facial aging process from the “Inside Out”. Aesthet Surg J. 2021;41(10):1107–1119. doi: 10.1093/asj/sjaa339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219–2227. doi: 10.1097/01.prs.0000265403.66886.54 [DOI] [PubMed] [Google Scholar]
- 22. Aldawsari M, Almadani FA, Almuhammadi N, Algabsani S, Alamro Y, Aldhwayan M. The efficacy of GLP-1 analogues on appetite parameters, gastric emptying, food preference and taste among adults with obesity: systematic review of randomized controlled trials. Diabetes Metab Syndr Obes. 2023;16:575–595. doi: 10.2147/dmso.s387116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shah M, Vella A. Effects of GLP-1 on appetite and weight. Rev Endocr Metab Disord. 2014;15(3):181–187. doi: 10.1007/s11154-014-9289-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cabbabe SW. Plastic surgery after massive weight loss. Mo Med. 2016;113(3):202–206. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.