Abstract
Background:
Few longitudinal studies exist comparing medical procedures after football injuries on artificial and natural grass surfaces.
Purpose/Hypothesis:
The purpose of this study was to specifically compare imaging and surgical procedures after surface-related collegiate football injuries on artificial turf versus natural grass. It was hypothesized that there would be no difference in the incidence of imaging and surgical procedures, combined medical procedures, or combined substantial and severe injuries over time between these surfaces.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A total of 39 universities across all Football Bowl Subdivision conferences were evaluated over 15 seasons (2006-2020). Playing surfaces evaluated were either a heavyweight artificial turf infill system (≥9.0 lb infill/ft2) or natural grass. Outcomes of interest included medical procedures across injury category, primary injury type, injury location, and specific procedures. Data involved multivariate analyses of variance (MANOVA) and Wilks λ criteria using general linear model procedures and were expressed as medical procedure incidence rates (IRs) per 10-game season.
Results:
Overall, 2224 games were documented: 1106 (49.7%) on artificial turf and 1118 (50.3%) on natural grass. Of the 9137 total injuries reported, 4010 (44%) were surface-related cases. MANOVA indicated significant main effects between surfaces according to imaging procedure (F2,1738 = 4.718; P = .009), surgical procedure (F1,539 = 5.974; P = .003), and medical diagnosis (F2,456 = 2.643; P = .040). Post hoc analyses indicated significantly lower (P < .05) incidences on artificial turf versus natural grass, respectively, for the following outcomes: imaging procedures ordered after player-to-surface impact trauma (IR [95% CI], 1.5 [1.3-1.8] vs 2.1 [1.9-2.4]), shoe-to-surface trauma during physical contact (4.4 [4.1-4.7] vs 5.2 [4.9-5.5]), foot injuries (0.6 [0.5-0.7] vs 1.1 [0.9-1.2]), ligament sprains/tears (4.6 [4.3-4.9] vs 5.3 [5.0-5.6]), muscle strains/tears (0.2 [0.2-0.3] vs 0.7 [0.6-0.9]), surgeries performed after shoe-to-surface trauma during physical contact (1.1 [0.9-1.3] vs 1.6 [1.4-1.8]), lower body surgeries (1.8 [1.6-2.0] vs 2.3 [2.1-2.6]), and surgeries involving ligament tears (1.0 [0.9-1.2] vs 1.5 [1.3-1.7]), as well as fewer diagnoses of syndesmosis sprains/tears (0.7 [0.5-0.8] vs 1.0 [0.8-1.2]) and Lisfranc trauma (0.3 [0.2-0.4] vs 0.5 [0.4-0.7]). Trends over the 15 seasons indicated a significant rise in combined medical procedures (P = .005) and combined substantial and severe injuries (P = .0007) irrespective of surface.
Conclusion:
Results indicated that collegiate football competition on heavyweight artificial turf resulted in lower incidences of imaging and surgical procedures and medical diagnoses compared with natural grass.
Keywords: synthetic field, MRI, radiograph, trauma
Today’s new generation of artificial turf infill systems are increasingly being installed to duplicate or exceed the playing characteristics of natural grass. Although components vary, in most cases, these synthetic surfaces are composed of a polyethylene slit-film or monofilament/polypropylene fiber blend, stabilized with a 2- or 3-layer infill made of sand and ground ambient styrene-butadiene rubber and laid over a crushed rock base for stability and drainage.
Although heavier weight (≥9.0 lb/ft2) infill systems are widely used at the National Collegiate Athletic Association (NCAA) and National Football League levels of competition and have been proven to provide greater safety than lighter weight artificial infill systems, 37 most studies have focused on injury incidence, with minimal attention to medical interventions after competition. Limited research addressing surgical procedures has been retrospectively conducted at the high school level, 50 with multiple sports across all NCAA divisions 55 and on a single collegiate football team. 34
Except for 1 study involving surface-related trauma and subsequent medical attention in collegiate soccer, 36 none has focused on imaging procedures or the influence of playing surface on medical procedures after football trauma. When juxtaposed against the increasing number and physical attributes of today's football athletes6,13,42 and the rising number of surgeries and rehabilitation reaching into the millions of dollars each season,33,41 efforts to delineate factors possibly contributing to injury have become a priority to enhance player safety.4,32,33,49,58 Recent authors have encouraged future research to move beyond simply quantifying trauma in various sports to addressing the subsequent medical procedures and challenges faced by athletes and their families as well as the potential long-term sequelae as they navigate toward an optimal quality of life and return to play. 3
At this time, limited longitudinal studies exist specifically comparing medical procedures after football injury from competitive play on artificial and natural grass surfaces. Therefore, in this prospective study, we quantified imaging and surgical procedures after surface-related college football game trauma on artificial and natural grass fields. We hypothesized that college football athletes would not experience any difference in the incidence of imaging and surgery after surface-related injury on artificial turf and natural grass. We also hypothesized that there would not be a rise in combined medical procedures or an increase in combined substantial and severe injuries over time.
Methods
Study Population
The study protocol was approved by the institutional review board at the university in which the study was based, and the study was conducted in accordance with the Declaration of Helsinki. A total of 39 universities were evaluated over 15 competitive seasons (2006-2020) across all Football Bowl Subdivision (FBS) conferences for game-related football injuries requiring imaging and surgical procedures after competitive play on artificial turf and natural grass. Criteria for inclusion were based on the availability of both playing surfaces during the same season, the same level of competitive play, and the involvement of a staff of certified athletic trainers (ATC [athletic trainer certified]). This ensured adequate sample size, similarity of sport skill, and a uniform level of professional knowledge among those evaluating and reporting injuries for the study.37,51
After games played on lightweight infill systems were removed (n = 376), selection bias was avoided by reporting on all remaining 2224 games played over the 15-year period on heavyweight artificial turf and natural grass throughout the study. Various stadiums were used by all 39 universities during home and away games. All teams had home facilities with either an indoor or outdoor artificial turf infill system.
Study Procedures
The evaluated playing surfaces were a heavyweight, artificial turf infill system (≥9.0 lb infill/ft2) and natural grass. For this prospective cohort study, an established comprehensive injury surveillance system was used to collect data, as previously described.23,35 Descriptive features and predictors included specific university, ATC, date of injury, personnel determining the injury, athlete weight, type of playing surface, surface quality, period of injury, year and skill level of athlete, and game location where the injury occurred. Outcomes of interest included injury category; anatomic location of trauma; primary type of injury; and specific shoulder, hand, knee, ankle, and foot diagnoses.
After sending an open invitation to all FBS universities that met the criteria for inclusion, interested head ATCs for each university were provided with an overview of the study purpose and procedures, copies of the injury surveillance form, and detailed instructions for completion to avoid the potential for performance and detection biases.49,51 Communication was maintained by the author to discuss potential concerns and ensure accuracy of collection, comprehensiveness of information, and ease of application.
All regular season, conference playoff, and bowl games were included. Injury data and subsequent imaging and surgeries were recorded after games, with adjunct support from ATC notes to avoid lapse of memory leading to inaccuracy or response distortion.39,49 All game injuries were evaluated by the attending ATC and team physicians on-site and, subsequently, in the physician's office when further follow-up and treatment were deemed necessary in accordance with established guidelines. 16 Any game trauma that occurred toward the end of the competitive schedule was monitored beyond the player's specific season to determine the date of recovery and functional return to play, with both team and nonuniversity medical staff procedures documented.36,39,48
If minor injuries occurred, completed injury surveillance forms were emailed to the investigator within 7 working days after a game. Follow-up telephone visits were used to obtain any additional information pertaining to any changes or additions in diagnosis, treatment, or time to return to play. To avoid the potential for on-field detection bias, 51 a single-blind outcome approach was maintained throughout the study period, with data collection of injuries and medical procedures limited to the ATCs and the authors’ role limited to data compilation and analyses.
Definitions
The definition of injury was based on a combination of functional outcome, observation, and treatment.39,44 A reportable surface-related injury was defined as any game-related football trauma involving player-to-surface impacts, shoe-to-surface during physical contact, and shoe-to-surface during non physical contact trauma reported or treated by the ATC or physician that resulted in an athlete's missing all or part of a game.23,37,39Injury severity was based on the number of days absent from game competition (time loss). As previously described, a minor injury was defined as any trauma that required 0 to 6 days of time loss, a substantial injury was any trauma requiring 7 to 21 days of time loss resulting in the athlete's being unable to return to play at the same competitive level, and a severe injury was defined as any trauma that resulted in ≥ 22 days of time loss.35,38
Imaging comprising computed tomography (CT), magnetic resonance imaging (MRI), radiography, and in-season/postseason surgeries was documented. Injury category solely comprised surface-related trauma consisting of player-to-surface impact, injuries attributed to shoe-to-surface interaction during player contact, and injuries attributed to shoe-to-surface interaction without player contact (ie, noncontact). 35
The anatomic location of imaging and surgeries was condensed to 29 anatomic sites. Primary type of injury resulting in imaging and surgical procedures was combined into the following categories: surface or epidermal (abrasion, laceration, puncture wound), contusion, concussion, herniation, inflammation (bursitis, tendinitis, fasciitis, synovitis, capsulitis, apophysitis), ligament sprain or tear, cartilage tear, muscle-tendon strain or tear, hyperextension, neural injury (burner, brachial plexus), subluxation or dislocation, and fracture (standard, epiphyseal, avulsion, stress, osteochondral).9,35
Selective diagnoses after surface-related shoulder and hand injuries and imaging consisted of acromioclavicular separation, rotator cuff tear/strain, various syndromes (dead arm, impingement), subluxation/dislocation, lesions (superior labrum anterior-to-posterior [SLAP], Hill-Sachs, Bankart), and other maladies (gamekeeper thumb, Boutonniere). Knee trauma was grouped by isolated cruciate/collateral ligaments and menisci, ligamentous trauma with associated tissue, fractures (osteochondral, patellar), and syndromes (patellofemoral, plica). Ankle and foot trauma consisted of sprains and tears (syndesmosis, Lisfranc, Chopart, turf toe), and fractures (Jones, Lisfranc, Maisonneuve, dancer fracture).
Statistical Analysis
Data were grouped by surface (artificial turf, natural grass) by outcomes of interest, and tabular-frequency distributions were computed using SPSS Statistics software (Version 28.0; IBM), with 95% CIs determined as described elsewhere. 54 Data were then subjected to multivariate analyses of variance (MANOVAs) and Wilks λ criteria using general linear model procedures and were expressed as imaging and surgical incidence rates (IRs; calculated as [number of procedures/number of team games] × 10) per 10 team games, as previously reported.28,35 Data screening indicated no violations of multivariate normality, linearity, outliers, homogeneity of variance, multicollinearity, or singularity. 54 When significant main effects were observed, univariate post hoc procedures were performed within each dependent variable based on the total percentage of imaging and surgical procedures from injuries reported on artificial turf and natural grass. An experiment-wise type I error rate of .05 was established a priori, and least squared means procedures were required because of the uneven number of observations on which to compare differences among variables. Statistical power analyses (1 –β; n-size calculations) were performed at the P value selected to establish significance in this study. Based on the number of games played on both artificial turf and natural grass surfaces, the number of documented injuries and subsequent imaging and surgical procedures provided adequate statistical power for analyses (1 –β = 0.732-1.000).
Simple linear regression models with natural grass–related combined medical procedures, artificial turf–related combined medical procedures, mean combined medical procedures, and substantial and severe combined injuries as dependent variables were used to establish trends over time. The coefficient of determination (R2) values derived from the trend lines were converted to r values for Pearson product-moment correlation interpretation, which were used to analyze the association between combined medical procedure incidence rates on either surface with time, and substantial and severe injury incidences with time. The magnitude of correlation was interpreted according to the following criteria: ≤0.1, trivial; >0.1 to 0.3, small; >0.3 to 0.5, moderate; >0.5 to 0.7, large; >0.7 to 0.9, very large; and >0.9 to 1.0, extremely large. 17
Results
A total of 2224 games were documented, of which 1106 (49.7%; 632 home, 474 away games) were played on a heavyweight 3-layer artificial turf (≥9.0 lbs/ft2) infill system and 1118 (50.3%; 620 home, 498 away games) were played on natural grass. The participating universities in this study were split between the Power 5 conference (53%; Atlantic Coast [22%], Big Ten [16%], Big 12 [22%], Pac-12 [21%], and Southeastern [19%]) and the Group of 5 conference (47%; American Athletic [18%], Conference USA [22%], Mid-America [19%], Mountain West [20%], and Sun Belt [21%]).
In sum, 9137 total injuries were reported, 4010 (44%) of which were surface-related cases, with 1757 injuries reported on artificial turf and 2253 on natural grass, comprising 1081 player-to-surface impacts, 2429 shoe-to-surface injuries during physical contact, and 500 shoe-to-surface injuries with noncontact. Surface-related trauma on artificial turf resulted in 773 imaging (445 radiographs, 19 CT, 309 MRI) and 231 surgical procedures, with 965 imaging (523 radiographs, 36 CT, 406 MRI) and 308 surgeries performed after injuries on natural grass. Over the 15-year study, a mean of 51.5 imaging requests and 15.4 surgical procedures per season were documented after artificial turf–related injury, in contrast to a mean of 64.3 imaging requests and 20.5 surgical procedures per season reported after natural grass–related trauma. The incidence of surface-related injury attributed to foul play or illegal action was similar across surfaces, comprising only 0.9% of trauma that required advanced medical procedures.
MANOVA indicated a significant main effect by imaging procedure (F2,1738 = 4.718; P = .009) between surfaces. Post hoc analyses (Table 1) indicated significantly lower (P < .05) incidence of radiographs, CTs, MRIs, and imaging procedures combined after trauma on artificial turf versus natural grass. A significantly lower (P < .05) incidence of imaging procedures was ordered on player-to-surface impact trauma, shoe-to-surface trauma during physical contact, foot injuries, contusions, ligament sprains/tears, and muscle strains/tears.
Table 1.
Incidence of Imaging After Surface-Related Trauma on Artificial Turf and Natural Grass by Imaging Procedure, Injury Category, Anatomic Location, and Primary Injury Type a
| Artificial Turf (n = 1097) | Natural Grass (n = 1118) | Total (n = 2215) | ||||
|---|---|---|---|---|---|---|
| Variable | n | IR (95% CI) | n | IR (95% CI) | n | IR |
| Imaging procedure | ||||||
| Radiograph | 445 | 4.1 (3.8-4.4) b | 523 | 4.7 (4.4-5.0) b | 968 | 4.4 |
| CT | 19 | 0.2 (0.1-0.3) | 36 | 0.3 (0.2-0.4) | 55 | 0.3 |
| MRI | 309 | 2.8 (2.6-3.1) b | 406 | 3.6 (3.4-3.9) b | 715 | 3.2 |
| Total | 773 | 7.1 (6.8-7.3) b | 965 | 8.6 (8.4-8.8) b | 1738 | 7.9 |
| Injury category | ||||||
| Player-to-surface impact | 168 | 1.5 (1.3-1.8) b | 238 | 2.1 (1.9-2.4) b | 406 | 1.8 |
| Shoe-to-surface contact | 486 | 4.4 (4.1-4.7) b | 586 | 5.2 (4.9-5.5) b | 1072 | 4.8 |
| Shoe-to-surface noncontact | 119 | 1.2 (0.9-1.3) | 141 | 1.3 (1.1-1.5) | 260 | 1.3 |
| Anatomic location | ||||||
| Upper body | 140 | 1.3 (1.1-1.5) b | 201 | 1.8 (1.6-2.0) b | 341 | 1.6 |
| Head/neck | 6 | 0.1 (0.0-0.1) | 7 | 0.1 (0.0-0.1) | 13 | 0.1 |
| Shoulder girdle | 77 | 0.7 (0.6-0.9) | 101 | 0.9 (0.7-1.1) | 178 | 0.8 |
| Arm/wrist/hand | 46 | 0.4 (0.3-0.6) | 70 | 0.6 (0.5-0.8) | 116 | 0.5 |
| Thoracoabdominal | 11 | 0.1 0.1-0.2) | 23 | 0.2 (0.1-0.3) | 34 | 0.2 |
| Lower body | 633 | 5.8 (5.5-6.1) b | 764 | 6.8 (6.6-7.1) b | 1397 | 6.3 |
| Pelvis/hip | 9 | 0.1 (0.0-0.2) | 15 | 0.1 (0.1-0.2) | 24 | 0.1 |
| Upper leg | 10 | 0.1 (0.1-0.2) | 20 | 0.2 (0.1-0.3) | 30 | 0.2 |
| Knee | 242 | 2.2 (2.0-2.5) | 248 | 2.2 (2.0-2.5) | 490 | 2.2 |
| Lower leg | 78 | 0.7 (0.6-0.9) | 109 | 1.0 (0.8-1.2) | 187 | 0.9 |
| Ankle | 207 | 1.9 (1.7-2.1) | 218 | 2.0 (1.7-2.2) | 425 | 2.0 |
| Foot | 63 | 0.6 (0.5-0.7) b | 118 | 1.1 (0.9-1.2) b | 181 | 0.9 |
| Toe | 24 | 0.2 (0.1-0.3) | 36 | 0.3 (0.2-0.4) | 60 | 0.3 |
| Primary injury type | ||||||
| Concussion | 1 | 0.0 (0.0-0.1) | 3 | 0.0 (0.0-0.1) | 4 | 0.0 |
| Contusion | 48 | 0.4 (0.3-0.6) b | 98 | 0.9 (0.7-1.1) b | 146 | 0.7 |
| Fracture | 92 | 0.8 (0.7-1.0) | 76 | 0.7 (0.5-0.8) | 168 | 0.8 |
| Herniation | 0 | 0.0 (0.0-0.0) | 1 | 0.0 (0.0-0.1) | 1 | 0.0 |
| Hyperextension | 3 | 0.0 (0.0-0.1) | 7 | 0.1 (0.0-0.1) | 10 | 0.1 |
| Inflammation | 8 | 0.1 (0.0-0.1) | 20 | 0.2 (0.1-0.3) | 28 | 0.2 |
| Ligament sprain/tear | 509 | 4.6 (4.3-4.9) b | 588 | 5.3 (5.0-5.6) b | 1097 | 5.0 |
| Muscle strain/tear | 26 | 0.2 (0.2-0.3) b | 78 | 0.7 (0.6-0.9) b | 104 | 0.5 |
| Neural | 2 | 0.0 (0.0-0.1) | 1 | 0.0 (0.0-0.1) | 3 | 0.0 |
| Subluxation/dislocation | 35 | 0.3 (0.2-0.4) | 40 | 0.4 (0.3-0.5) | 75 | 0.4 |
| Tendon strain/tear | 12 | 0.1 (0.1-0.2) | 16 | 0.1 (0.1-0.2) | 28 | 0.1 |
| Torn cartilage | 37 | 0.3 (0.2-0.5) | 37 | 0.3 (0.2-0.5) | 74 | 0.3 |
Wilks λ imaging procedures, F2,1738 = 4.718; P = .009. CT, computed tomography; IR, incidence rate; MRI, magnetic resonance imaging.
Significant difference between surface types (P < .05).
Regarding surgeries, MANOVA indicated a significant main effect by surgical procedure (F1,539 = 5.974; P = .003) between surfaces. Post hoc analyses (Table 2) indicated significantly lower (P < .05) incidences of postseason and total surgeries, surgeries after shoe-to-surface trauma during physical contact, ankle surgeries, and surgeries as a result of ligament tears after competitive play on heavyweight artificial turf when compared with natural grass. Surgical procedures involving artificial turf injuries included single-tissue arthroscopic repair (n = 92; 40%), multiple tissue reconstructive repair (n = 90; 39%), and open reduction and internal fixation (ORIF; n = 49; 21%), whereas (n = 152; 49%) natural grass trauma involved single-tissue arthroscopic repair, followed by multiple tissue reconstructive repair (n = 94; 31%) and ORIF (n = 62; 20%). Anterior cruciate ligament (ACL) and associated tissue comprised 53% (n = 168; IR = 0.8) of surgeries performed on the knee, whereas lesions (Bankart, Hill-Sachs, SLAP) from player-to-surface impact comprised 63% (n = 34; IR = 0.2) of total shoulder surgeries, with no significant surface effect. No information was available addressing surgical revisions.
Table 2.
Incidence of Surgical Procedures After Surface-Related Trauma on Artificial Turf and Natural Grass by Surgery Timing, Injury Category, Anatomic Location, and Primary Injury Type a
| Artificial Turf (n = 1097) | Natural Grass (n = 1118) | Total (n = 2215) | ||||
|---|---|---|---|---|---|---|
| Variable | n | IR (95% CI) | n | IR (95% CI) | n | IR |
| Surgery timing | ||||||
| In-season | 183 | 1.7 (1.5-1.9) | 231 | 2.1 (1.8-2.3) | 414 | 1.9 |
| Postseason | 48 | 0.4 (0.3-0.6) | 77 | 0.7 (0.6-0.9) | 125 | 0.6 |
| Total | 231 | 2.1 (1.9-2.4) b | 308 | 2.8 (2.5-3.0) b | 539 | 2.5 |
| Injury category | ||||||
| Player-to-surface impact | 39 | 0.4 (0.3-0.5) | 55 | 0.5 (0.4-0.6) | 94 | 0.5 |
| Shoe-to-surface contact | 121 | 1.1 (0.9-1.3) b | 178 | 1.6 (1.4-1.8) b | 299 | 1.4 |
| Shoe-to-surface noncontact | 71 | 0.6 (0.5-0.8) | 75 | 0.7 (0.5-0.8) | 146 | 0.7 |
| Anatomic location | ||||||
| Upper body | 36 | 0.3 (0.2-0.5) | 46 | 0.4 (0.3-0.5) | 82 | 0.4 |
| Shoulder girdle | 20 | 0.2 (0.1-0.3) | 34 | 0.3 (0.2-0.4) | 54 | 0.3 |
| Arm/wrist/hand | 15 | 0.1 (0.1-0.2) | 12 | 0.1 (0.1-0.2) | 27 | 0.1 |
| Thoracoabdominal | 1 | 0.0 (0.0-0.1) | 0 | 0.0 (0.0-0.0) | 1 | 0.0 |
| Lower body | 195 | 1.8 (1.6-2.0) b | 262 | 2.3 (2.1-2.6) b | 457 | 2.1 |
| Pelvis/hip | 0 | 0.0 (0.0-0.0) | 1 | 0.0 (0.0-0.1) | 1 | 0.0 |
| Upper leg | 3 | 0.0 (0.0-0.1) | 5 | 0.0 (0.0-0.1) | 8 | 0.0 |
| Knee | 147 | 1.3 (1.2-1.6) | 172 | 1.5 (1.3-1.8) | 319 | 1.4 |
| Lower leg | 22 | 0.2 (0.1-0.3) | 27 | 0.2 (0.2-0.3) | 49 | 0.2 |
| Ankle | 9 | 0.1 (0.0-0.2) | 23 | 0.2 (0.1-0.3) | 32 | 0.2 |
| Foot | 13 | 0.1 (0.1-0.2) | 30 | 0.3 (0.2-0.4) | 43 | 0.2 |
| Toe | 1 | 0.0 (0.0-0.1) | 4 | 0.0 (0.0-0.1) | 5 | 0.0 |
| Primary injury type | ||||||
| Fracture | 49 | 0.4 (0.3-0.6) | 52 | 0.5 (0.4-0.6) | 101 | 0.5 |
| Herniation | 1 | 0.0 (0.0-0.1) | 0 | 0.0 (0.0-0.0) | 1 | 0.0 |
| Ligament tear | 115 | 1.0 (0.9-1.2) b | 168 | 1.5 (1.3-1.7) b | 283 | 1.3 |
| Muscle tear | 3 | 0.0 (0.0-0.1) | 6 | 0.1 (0.0-0.1) | 9 | 0.0 |
| Subluxation/dislocation | 22 | 0.2 (0.1-0.3) | 37 | 0.3 (0.2-0.5) | 59 | 0.3 |
| Tendon tear | 6 | 0.1 (0.0-0.1) | 7 | 0.1 (0.0-0.1) | 13 | 0.1 |
| Torn cartilage | 35 | 0.3 (0.2-0.4) | 38 | 0.3 (0.2-0.5) | 73 | 0.3 |
Wilks λ surgical procedures, F1,539 = 5.974; P = .003. IR, incidence rate.
Significant difference between surface types (P < .05).
MANOVA indicated a significant main effect by medical diagnosis (F2,456 = 2.643; P = .040) between surfaces. Post hoc analyses (Table 3) indicated significantly lower (P < .05) incidence of imaging procedures confirming syndesmosis sprain/tears and Lisfranc diagnoses after injury on heavyweight artificial turf when compared with natural grass surfaces. Overall, syndesmotic sprains/tears resulted in the greatest incidence of imaging procedures and subsequent diagnoses (n = 183; IR = 0.8), followed by ACL and associated tissue (n = 168; IR = 0.8) and medial collateral ligament cases (n = 146; IR = 0.7). No significant differences between surfaces (P > .05), however, were observed across diagnostic procedures involving the knee.
Table 3.
Selective Diagnoses After Surface-Related Trauma and Imaging on Artificial Turf and Natural Grass a
| Artificial Turf (n = 1106) | Natural Grass (n = 1118) | Total (N = 2224) | ||||
|---|---|---|---|---|---|---|
| Variable | n | IR (95% CI) | n | IR (95% CI) | n | IR |
| Shoulder and hand diagnoses | ||||||
| AC separation | 45 | 0.4 (0.3-0.5) | 47 | 0.4 (0.3-0.6) | 92 | 0.4 |
| Rotator cuff tear/strain | 1 | 0.0 (0.0-0.1) | 4 | 0.0 (0.0-0.1) | 5 | 0.0 |
| Dead arm syndrome | 1 | 0.0 (0.0-0.1) | 0 | 0.0 (0.0-0.0) | 1 | 0.0 |
| GH subluxation/dislocation | 2 | 0.0 (0.0-0.1) | 4 | 0.0 (0.0-0.1) | 6 | 0.0 |
| Impingement syndrome | 0 | 0.0 (0.0-0.0) | 2 | 0.0 (0.0-0.1) | 2 | 0.0 |
| SLAP lesion | 4 | 0.0 (0.0-0.1) | 10 | 0.1 (0.0-0.2) | 14 | 0.1 |
| Hill-Sachs lesion | 3 | 0.0 (0.0-0.1) | 5 | 0.0 (0.0-0.1) | 8 | 0.0 |
| Bankart lesion | 6 | 0.1 (0.0-0.1) | 6 | 0.1 (0.0-0.1) | 12 | 0.1 |
| Boutonniere deformity | 5 | 0.0 (0.0-0.1) | 2 | 0.0 (0.0-0.1) | 7 | 0.0 |
| Gamekeeper thumb | 1 | 0.0 (0.0-0.1) | 4 | 0.0 (0.0-0.1) | 5 | 0.0 |
| Knee diagnoses | ||||||
| Medial collateral | 70 | 0.6 (0.5-0.8) | 76 | 0.7 (0.5-0.8) | 146 | 0.7 |
| Lateral collateral | 8 | 0.1 (0.0-0.1) | 8 | 0.1 (0.0-0.1) | 16 | 0.1 |
| Anterior cruciate | 27 | 0.2 (0.2-0.4) | 36 | 0.3 (0.2-0.4) | 63 | 0.3 |
| Posterior cruciate | 13 | 0.1 (0.1-0.2) | 11 | 0.1 (0.1-0.2) | 24 | 0.1 |
| Medial meniscus | 15 | 0.1 (0.1-0.2) | 19 | 0.2 (0.1-0.3) | 34 | 0.2 |
| Lateral meniscus | 22 | 0.2 (0.1-0.3) | 20 | 0.2 (0.1-0.3) | 42 | 0.2 |
| Arcuate-popliteal complex | 5 | 0.0 (0.0-0.1) | 13 | 0.1 (0.1-0.2) | 18 | 0.1 |
| ACL/MCL | 8 | 0.1 (0.0-0.1) | 9 | 0.1 (0.0-0.2) | 17 | 0.1 |
| ACL/LCL | 3 | 0.0 (0.0-0.1) | 7 | 0.1 (0.0-0.1) | 10 | 0.1 |
| ACL/medial meniscus | 11 | 0.1 (0.1-0.2) | 6 | 0.1 (0.0-0.1) | 17 | 0.1 |
| ACL/lateral meniscus | 12 | 0.1 (0.1-0.2) | 12 | 0.1 (0.1-0.2) | 24 | 0.1 |
| ACL/MCL/medial meniscus | 9 | 0.1 (0.0-0.2) | 8 | 0.1 (0.0-0.1) | 17 | 0.1 |
| ACL/MCL/lateral meniscus | 8 | 0.1 (0.0-0.1) | 4 | 0.0 (0.0-0.1) | 12 | 0.1 |
| ACL/LCL/lateral meniscus | 4 | 0.0 (0.0-0.1) | 0 | 0.0 (0.0-0.0) | 4 | 0.0 |
| ACL/PCL/MCL/LCL | 1 | 0.0 (0.0-0.1) | 3 | 0.0 (0.0-0.1) | 4 | 0.0 |
| PCL/MCL | 2 | 0.0 (0.0-0.1) | 6 | 0.1 (0.0-0.1) | 8 | 0.1 |
| PCL/LCL/lateral meniscus | 1 | 0.0 (0.0-0.1) | 2 | 0.0 (0.0-0.1) | 3 | 0.0 |
| Osteochondral fracture | 8 | 0.1 (0.0-0.1) | 3 | 0.0 (0.0-0.1) | 11 | 0.1 |
| Patellofemoral syndrome | 11 | 0.1 (0.1-0.2) | 17 | 0.2 (0.1-0.2) | 28 | 0.2 |
| Plica syndrome | 1 | 0.1 (0.0-0.1) | 1 | 0.0 (0.0-0.1) | 2 | 0.1 |
| Patellar fracture | 4 | 0.0 (0.0-0.1) | 4 | 0.0 (0.0-0.1) | 8 | 0.0 |
| Ankle and foot diagnoses | ||||||
| Syndesmosis sprain/tear | 75 | 0.7 (0.5-0.8) b | 108 | 1.0 (0.8-1.2) b | 183 | 0.9 |
| Lisfranc injury | 35 | 0.3 (0.2-0.4) b | 59 | 0.5 (0.4-0.7) b | 94 | 0.4 |
| Chopart injury | 3 | 0.0 (0.0-0.1) | 5 | 0.0 (0.0-0.1) | 8 | 0.0 |
| Jones fracture | 7 | 0.1 (0.0-0.1) | 8 | 0.1 (0.0-0.1) | 15 | 0.1 |
| Maisonneuve fracture | 1 | 0.0 (0.0-0.1) | 1 | 0.0 (0.0-0.1) | 2 | 0.0 |
| Dancer fracture | 1 | 0.0 (0.0-0.1) | 0 | 0.0 (0.0-0.0) | 1 | 0.0 |
| Turf toe | 26 | 0.2 (0.2-0.3) | 29 | 0.3 (0.2-0.4) | 55 | 0.3 |
Wilks λ medical diagnosis, F2,456 = 2.643; P = .040. AC, acromioclavicular; ACL, anterior cruciate ligament; GH, glenohumeral; LCL, lateral collateral ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament; SLAP, superior labrum anterior-to-posterior; IR, incidence rate.
Significant difference between surface types (P < .05).
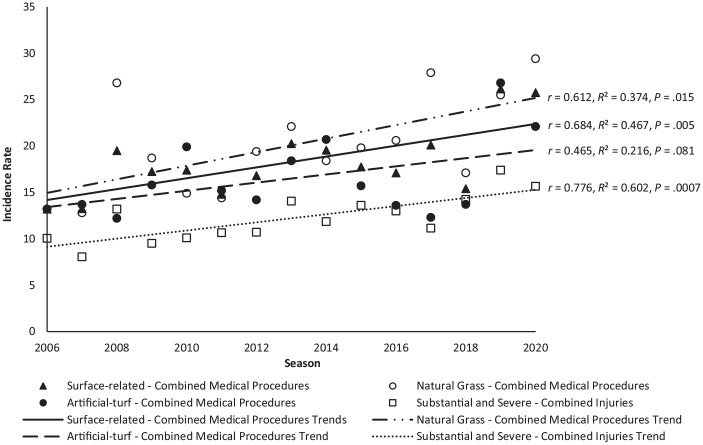
Trends over the 15 seasons evaluated indicated an increase in both combined medical procedures and surface-related injuries (Figure 1). Pearson correlation analysis revealed significant, large, positive correlations for natural grass combined medical procedures (P = .015; r = 0.612), mean combined medical procedures (P = .005; r = 0.684), and substantial and severe combined injuries (P = .0007; r = 0.776) with time as well as a nonsignificant, moderate, and positive correlation for artificial turf combined medical procedures (P = .081; r = 0.465) with time. The coefficient of determination values for natural grass combined medical procedures (R2 = 0.374), artificial turf combined medical procedures (R2 = 0.216), mean combined medical procedures (R2 = 0.467), and substantial and severe combined injuries (R2 = 0.602) indicated that the linear models had minimal predictive capability; however, this was to be expected given the myriad factors that contribute to injury. 26
Figure 1.
Surface-related combined medical procedures compared with substantial and severe injuries over 15 seasons.
Discussion
Although some similarities existed in the rate of medical procedures ordered, games played on natural grass surfaces resulted in significantly greater incidence of imaging, surgical cases, and total medical procedures combined when compared with artificial surfaces. Findings may be related to the greater incidence (P < .001) of substantial and severe injury cases involving physical contact during shoe-to-surface interaction on natural grass as compared with artificial turf (IR [95% CI]: 5.0 [95% CI, 4.7-5.3] vs 3.6 [3.3-3.9], respectively). This is supported by earlier summations noting similar results when comparing the 2 surfaces,1,35,36,39 but it is in contrast to other studies reporting a perceived rise in ACL trauma in a limited review of multigenerational artificial turf studies in high school and college football. 5 Of note, surgical cases per season on both artificial turf (15.4) and natural grass (20.5) in this study were lower than the 25.4 operations per year previously reported after collegiate football trauma. 34 With regard to the potential influence of home and away games played on artificial turf versus natural grass, the 0.8% difference in the number of home games as well as the 2.4% difference in the number of away games played between the 2 surfaces indicated minimal locational effect on injuries and subsequent imaging and surgical procedures.
Results may also be a function of less consistency in natural grass/soil surface quality as compared with heavyweight artificial turf infill systems.27,35 Securing field surface maintenance records, as well as obtaining lower extremity kinematic data during actual play, however, was beyond the scope of this study, which limits further supposition. Further investigation of the effects of various maintenance regimens on biomechanics of the shoe-to-surface interaction beyond the laboratory setting is recommended to more closely replicate the environmental variability, player contact, and anatomic and neuromuscular complexities during actual sports performance.19,26
The incidence of surgeries involving the ACL and associated tissue trauma (53%) in this study was consistent with earlier work indicating 35% to 59% of total knee surgeries involving the ACL.21,34,50 The number of shoulder lesions resulting in surgery from player-to-surface impact, regardless of playing surface, is consistent with prior studies indicating 3% to 71% of total shoulder cases.11,34,45,50,52,56 Foot (8%) and ankle (6%) trauma requiring surgery were lower than the 21% previously reported. 34
The significant rise in the incidence of imaging and surgical procedures over 15 seasons was not only influenced by the increasing number of substantial and severe game-related cases (Figure 1) but may also reflect additional factors. These include today's athletes being larger, more powerful, and faster than observed in prior decades6,13; greater diagnostic training, awareness, and sophistication of practitioners in identifying the growing array of sports-related trauma29,31; and greater access to enhanced imaging procedures24,60 as well as more expeditious surgical techniques leading to optimal return to play.7,46 Although prior findings remain equivocal, the significant increase in lower extremity injuries and subsequent medical procedures observed in this study may also have been influenced by recent rule changes that attempted to reduce cranial/cervical trauma at the expense of greater knee and ankle cases. 57 Of major concern is that the overall results are reflective of and consistent with the continuing increase in severe trauma observed in both high school and collegiate studies across both artificial and natural grass surfaces,22,23,25 eventually resulting in increased health-related issues at a later age.12,18,53
Even though the quality of grass surfaces were deemed adequate throughout the study, the findings suggest the need to further investigate the effect of modifications and maintenance practices of playing surfaces on player safety at this level of competition. Furthermore, with the growing concern in increasing health care costs and equivocal injury findings, the tracking of imaging and surgical procedures has not been largely addressed in prior injury risk studies.34,37,43,55,58 It is strongly encouraged that future injury studies include posttrauma medical care to establish a more accurate measure of severity of injury beyond simply time loss, leading to improvement of playing surfaces, quality of care, and efficacy of outcomes. This may lead to pertinent insight into actual safety improvements and advance the sports medicine discussion beyond supposition and simple documentation of the incidence and severity of trauma across various sport surfaces. 3
Limitations and Strengths
There were potential limitations to the study that may have influenced the type and number of reported injuries leading to imaging and surgical intervention. These included the inability to control the inherently random variation in injury typically observed in high-collision team sports 36 ; the strength, conditioning, and body composition status of the athletes4,20,47,48; the influence of precompetition workloads30,59; previous injury history and associated medical procedures8,10,14; variations in weather conditions and quality of field maintenance4,8,30; differences in postural or joint integrity, musculoskeletal structure, and biomechanics of player movement4,8,15,33; coaching style, experience and play calling5,35,48; foul play and the quality of officiating8,38,48; actual versus mean time to exposure to injury21,26; sports skill level, intensity of play, and fatigue level at time of injury8,21,47; an athlete's reluctance in seeking help after injury40,49; unreported congenital or developmental factors predisposing an athlete to additional injury4,21,48; unforeseen mishap23,48; or simply for an acute injury to go unreported.23,25,38 Additional limitations were the inability to obtain orthotic support information before injury, 6 the time between sport trauma and advanced medical procedures,7,34 the incidence of multiple operations over time,6,52 or long-term quality-of-life differences after trauma between the 2 surface groups.2,52
Key strengths of the study were the opportunity to track a large number of FBS universities during the 15-year period, utilizing prospective, validated methods that reduced fluctuations often observed in single-season injury patterns and individual team effect1,34 and minimized the over- and underestimation of sport trauma observed in publicly obtained databases.20,25,47 In addition, the combined method of assessing functional outcome, direct observation, and treatment records, as well as the daily interactions of ATCs in direct communication with athletes in this study, minimized the potential for transfer bias and unreported injuries throughout the season.26,39 In totality, these efforts enhanced the ability to identify injury differences, subsequent medical procedures, and trends across time between artificial and natural grass fields.
The influence of risk factors other than an artificial turf versus natural grass surface cannot be overlooked. Because of the inherent challenges of collecting data on multiple indices and on numerous teams and players over an extended period of time, the degree of influence from these risk factors remains a limitation that can only be acknowledged at this time.5,26 However, the prospective cohort multivariate design enhanced sample size, resulted in variation of play on all surfaces, controlled for seasonal and team variation, and allowed for greater insight into both significant and subtle differences in imaging and surgical procedures ordered after sport trauma on both heavyweight artificial turf and natural grass surfaces.
Conclusion
In contrast to perception and anecdotal experiences, in many cases, the use of a heavyweight artificial infill system in collegiate football competition was associated with a reduction in the incidence and severity of surface-related sport trauma, resulting in a significantly lower incidence of imaging and surgical procedures when compared with natural grass fields. The hypotheses that (1) collegiate football athletes would not experience any difference in the incidence of imaging and surgery after surface-related injury on artificial turf and natural grass and that (2) there would not be a rise in combined medical procedures, nor an increase in substantial and/or severe combined injuries over time, were not supported. When compared with natural grass, findings reinforce the use of a heavyweight artificial infill system at the collegiate level of play.
Finally, based on the observed trend for football trauma to significantly increase over the 15-year period, what appears to be an increase in aggression in competitive football should be a concern while attempting to balance the traditions of the sport with player safety. The growing intensity of play leading to increased medical care needs to be addressed beyond the playing surface.
This is, to our knowledge, the most extensive, multiteam prospective longitudinal study to address postgame medical procedures as they relate specifically to surface-related injury in collegiate American football. Although the findings of this study may be generalizable to only the collegiate level of football competition, ensuring optimal athletic safety through research-supported guidelines, rather than perception, should be foremost when considering playing field installations at any level of competition.
Footnotes
Final revision submitted January 23, 2024; accepted February 29, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research support was received from FieldTurf USA (to M.C.M.). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Idaho State University (ref No. FY2023-244).
References
- 1. Almutawa M, Scott M, George KP, Drust B. The incidence and nature of injuries sustained on grass and 3rd generation artificial turf: a pilot study in elite Saudi National Team footballers. Phys Ther Sport. 2014;15(1):47-52. [DOI] [PubMed] [Google Scholar]
- 2. Arden CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848-856. [DOI] [PubMed] [Google Scholar]
- 3. Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sports Med. 2018;52(16):1018-1021. [DOI] [PubMed] [Google Scholar]
- 4. Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39(6):324-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Balazs GC, Pavey GJ, Brelin AM, Pickett A, Keblish DJ, Rue JP. Risk of anterior cruciate ligament injury in athletes on synthetic playing surfaces: a systematic review. Am J Sports Med. 2015;43(7):1798-1804. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine-–trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22-27. [DOI] [PubMed] [Google Scholar]
- 7. Buerba RA, Zaffagnini S, Kuroda R, Musahl V. ACL reconstruction in the professional or elite athlete: state of the art. J Am Acad Orthop Surg Glob Res Rev. 2021;6(4):226-236. [DOI] [PubMed] [Google Scholar]
- 8. Chomiak J, Junge A, Peterson L, Dvorak J. Severe injuries in football players. Am J Sports Med. 2000;28(5)(suppl):S58-S68. [DOI] [PubMed] [Google Scholar]
- 9. Clifton DR, Koldenhoven RM, Hertel J, Onate JA, Dompier TP, Kerr ZY. Epidemiological patterns of ankle sprains in youth, high school, and college football. Am J Sports Med. 2017;45(2):417-425. [DOI] [PubMed] [Google Scholar]
- 10. Creighton DW, Shrier I, Shultz R, Meeuwisse WH, Matheson GO. Return to play in sport: a decision-based model. Clin J Sport Med. 2010;20(5):379-385. [DOI] [PubMed] [Google Scholar]
- 11. Cvetanovich GL, Gowd AK, Frantz TL, Erickson BJ, Romeo AA. Superior labral anterior posterior repair and biceps tenodesis surgery: trends of the American Board of Orthopaedic Surgery database. Am J Sports Med. 2020;48(7):1583-1589. [DOI] [PubMed] [Google Scholar]
- 12. Everhart JS, Yalcin S, Spindler KP. Twenty-year outcomes after anterior cruciate ligament reconstruction: a systematic review of prospectively collected data. Am J Sports Med. 2022;50(10):2842-2852. [DOI] [PubMed] [Google Scholar]
- 13. Fitzgerald CF, Jensen RL. A comparison of the National Football League's annual National Football League combine 1999-2000 to 2015-2016. J Strength Cond Res. 2020;34(3):771-781. [DOI] [PubMed] [Google Scholar]
- 14. Fuller CW. Managing the risk of injury in sport. Clin J Sport Med. 2007;17(3):182-187. [DOI] [PubMed] [Google Scholar]
- 15. Hart NH, Nimphius S, Weber J, et al. Musculoskeletal asymmetry in football athletes: a product of limb function over time. Med Sci Sports Exerc. 2016;48(7):1379-1387. [DOI] [PubMed] [Google Scholar]
- 16. Herring SA, Kibler WB, Putukian M. Team physician consensus statement: 2013 update. Med Sci Sports Exerc. 2013;45(8):1618-1622. [DOI] [PubMed] [Google Scholar]
- 17. Hopkins WG, Marshall SW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41(1):3-13. [DOI] [PubMed] [Google Scholar]
- 18. Hubbard-Turner T, Turner MJ. Physical activity levels in college students with chronic ankle instability. J Athl Train. 2015;50(7):742-747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Iacovelli JN, Yang J, Thomas G, et al. The effect of field condition and shoe type on lower extremity injuries in American football. Brit J Sports Med. 2013;47(12):789-793. [DOI] [PubMed] [Google Scholar]
- 20. Inclan PM, Chang PS, Mack CD, et al. Validity of research based on public data in sports medicine: a quantitative assessment of anterior cruciate ligament injuries in the National Football League. Am J Sports Med. 2022;50(6):1717-1726. [DOI] [PubMed] [Google Scholar]
- 21. Joseph DW, Collins CL, Henke NM, et al. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810-817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop (Belle Mead NJ). 2011;40(1):40-44. [PubMed] [Google Scholar]
- 23. Kerr ZY, Dompier TP, Snook EM, et al. National Collegiate Athletic Association Injury Surveillance System: review of methods for 2004-2005 through 2013-2014 data collection. J Athl Train. 2014;49(4):552-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Klontzas ME, Protonotarios A. High-resolution imaging for the analysis and reconstruction of 3D microenvironments for regenerative medicine: an application-focused review. Bioengineering (Basel). 2021;8(11):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kluczynski MA, Kelly WH, Lashomb WM, Bisson LJ. A systematic review of the orthopaedic literature involving National Football League players. Orthop J Sports Med. 2019;7(8):2325967119864356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Krosshaug T, Andersen TE, Olsen O-EO, Myklebust G, Bahr R. Research approaches to describe the mechanisms of injuries in sport: limitations and possibilities. Br J Sports Med. 2005;39(6):330-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kuitunen I, Immonen V, Pakarinen O, Mattila VM, Ponkilainen VT. Incidence of football injuries sustained on artificial turf compared to grass and other playing surfaces: a systematic review and meta-analysis. eClinicalMed. 2023;59:101956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lawrence DW, Hutchinson MG, Comper P. Descriptive epidemiology of musculoskeletal injuries and concussions in the National Football League, 2012-2014. Orthop J Sports Med. 2015;3(5):2325967115583653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lombardi NJ, Tucker B, Freedman KB, et al. Accuracy of athletic trainer and physician diagnoses in sports medicine. Orthopedics. 2016;39(5):e944-e949. [DOI] [PubMed] [Google Scholar]
- 30. Loughran GJ, Vulpis CT, Murphy JP, et al. Incidence of knee injuries on artificial turf versus natural grass in National Collegiate Athletic Association American football: 2004-2005 through 2013-2014 seasons. Am J Sports Med. 2019;47(6):1294-1301. [DOI] [PubMed] [Google Scholar]
- 31. Luginbuhl JC, Sobel AD, Mulcahey MK. Analysis of the sports medicine section of the Orthopaedic In-Training Examination: improvements in levels of evidence and question taxonomy over a 12-year period. Orthopedics. 2020;43(5):e460-e464. [DOI] [PubMed] [Google Scholar]
- 32. Maniar N, Carmichael DS, Hickey JT, et al. Incidence and prevalence of hamstring injuries in field-based team sports: a systematic review and meta-analysis of 5952 injuries from over 7 million exposure hours. Br J Sports Med. 2023;57(2):109-116. [DOI] [PubMed] [Google Scholar]
- 33. McLean SG, Beaulieu ML. Complex integrative morphological and mechanical contributions to ACL injury risk. Exerc Sport Sci Rev. 2010;38(4):192-200. [DOI] [PubMed] [Google Scholar]
- 34. Mehran N, Photopoulos CD, Narvy SJ, et al. Epidemiology of operative procedures in an NCAA Division I football team over 10 seasons. Orthop J Sports Med. 2016;4(7):2325967116657530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Meyers MC. Incidence, mechanisms, and severity of game-related college football injuries on FieldTurf versus natural grass: a 3-year prospective study. Am J Sports Med. 2010;38(4):687-697. [DOI] [PubMed] [Google Scholar]
- 36. Meyers M.C. Incidence, mechanisms, and severity of match-related collegiate men's soccer injuries on FieldTurf and natural grass surfaces: a 6-year prospective study. Am J Sports Med. 2017;45(3):708-718. [DOI] [PubMed] [Google Scholar]
- 37. Meyers MC. Incidence, mechanisms, and severity of game-related high school football injuries on across artificial turf systems of various infill weight: a 7-year prospective study. Orthop J Sports Med. 2019;7(3):2325967119832878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Meyers MC. Surface-related high school football game injuries on pad and no-pad fields. Am J Sports Med. 2021;49(9):2489-2497. [DOI] [PubMed] [Google Scholar]
- 39. Meyers MC, Barnhill BS. Incidence, causes, and severity of high school football injuries on FieldTurf versus natural grass: a 5-year prospective study. Am J Sports Med. 2004;32(7):1626-1638. [DOI] [PubMed] [Google Scholar]
- 40. Meyers MC, Bourgeois AE, LeUnes A. Pain coping response of collegiate athletes involved in high contact, high injury-potential sport. Int J Sport Psychol. 2001;32(1):1-14. [Google Scholar]
- 41. Milne C. Practising sports and exercise medicine in an environment of rising medical costs. Br J Sports Med. 2011;45(12):945-946. [DOI] [PubMed] [Google Scholar]
- 42. National Football Foundation. Football Remains Strong: 774 Colleges and Universities Offering Football. Accessed January 3, 2023. http://footballfoundation.org/news/2022/8/2/football-remains-strong-774-colleges-and-universities-offering-football.aspx
- 43. Nicholas JA, Rosenthal PP, Gleim GW. A historical perspective of injuries in professional football: twenty-six years of game-related events. JAMA. 1988;260(7):939-944. [PubMed] [Google Scholar]
- 44. Noyes FR, Lindenfeld TN, Marshall MT. What determines an athletic injury (definition)? Who determines an injury (occurrence)? Am J Sports Med. 1988;16(suppl 1):S65-S68. [DOI] [PubMed] [Google Scholar]
- 45. Onyekwelu I, Khatib O, Zuckerman JD, Rokito AS, Kwon YW. The rising incidence of arthroscopic superior labrum anterior and posterior (SLAP) repairs. J Shoulder Elbow Surg. 2012;21(6):728-731. [DOI] [PubMed] [Google Scholar]
- 46. Ozeki N, Seil R, Krych AJ, Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS. 2021;6(1):35-45. [DOI] [PubMed] [Google Scholar]
- 47. Palmieri-Smith RM, Mack CD, Brophy RH, et al. Epidemiology of anterior cruciate ligament tears in the National Football League. Am J Sports Med. 2021;49(7):1786-1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Parkkari J, Kujala UM, Kannus P. Is it possible to prevent sports injuries? Review of controlled clinical trials and recommendations for future work. Sports Med. 2001;31(14):985-995. [DOI] [PubMed] [Google Scholar]
- 49. Prager BI, Fitton WL, Cahill BR, et al. High school football injuries: a prospective study and pitfalls of data collection. Am J Sports Med. 1989;17(5):681-685. [DOI] [PubMed] [Google Scholar]
- 50. Rechel JA, Collins CL, Comstock RD. Epidemiology of injuries requiring surgery among high school athletes in the United States, 2005 to 2010. J Trauma. 2011;71(4):982-989. [DOI] [PubMed] [Google Scholar]
- 51. Rudicel S. How to avoid bias. Am J Sports Med. 1988;16(suppl 1):S48-S52. [DOI] [PubMed] [Google Scholar]
- 52. Rutgers C, Verweij LPE, Priester-Vink S, van Deurzen DFP, Maas M, ven den Bekerom MPJ. Recurrence in traumatic anterior shoulder dislocations increases the prevalence of Hill-Sachs and Bankart lesions: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):2130-2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shelbourne KD, Benner RW, Gray T. Results of anterior cruciate ligament reconstruction with patellar tendon autografts: objective factors associated with the development of osteoarthritis at 20 to 33 years after surgery. Am J Sports Med. 2017;45(12):2730-2738. [DOI] [PubMed] [Google Scholar]
- 54. Tabachnick BG, Fidell LS. Using Multivariate Statistics. 2nd ed. Harper & Row; 1989. [Google Scholar]
- 55. Taree A, Charen D, Huang HH, Poeran J, Colvin A. Analysis of surgery rates among 25 National Collegiate Athletic Association sports. Phys Sportsmed. 2022;50(1):30-37. [DOI] [PubMed] [Google Scholar]
- 56. Weber SC, Martin DF, Seiler JG, 3rd, Harrast JJ. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery Part II candidates. Am J Sports Med. 2012;40(7):1538-1543. [DOI] [PubMed] [Google Scholar]
- 57. Westermann RW, Kerr ZY, Wehr P, Amendola A. Increasing lower extremity injury rates across the 2009-2010 to 2014-2015 seasons of National Collegiate Athletic Association football: an unintended consequence of the “targeting” rule used to prevent concussions? Am J Sports Med. 2016;44(12):3230-3236. [DOI] [PubMed] [Google Scholar]
- 58. Williams S, Hume PA, Kara S. A review of football injuries on third and fourth generation artificial turfs compared with natural turf. Sports Med. 2011;41(11):903-923. [DOI] [PubMed] [Google Scholar]
- 59. Windt J, Gabbett TJ. How do training and competition workloads relate to injury? The workload-injury aetiology model. Br J Sports Med. 2017;51(5):428-435. [DOI] [PubMed] [Google Scholar]
- 60. Yousaf T, Dervenoulas G, Politis M. Advances in MRI methodology. Int Rev Neurobiol. 2018;141:31-76. [DOI] [PubMed] [Google Scholar]