Abstract
Background
The management of hemodynamically unstable pelvic ring injuries necessitates surgical intervention, often involving procedures such as external fixation and percutaneous screw placement. Given the infrequent performance of these procedures, regular training is imperative to ensure readiness for emergencies. Our pre- post simulation study aimed to adapt and validate a realistic simulation model for stabilizing unstable pelvic ring injuries, facilitating participants’ knowledge retention and procedural confidence enhancement.
Methods
A standardized simulator of an unstable pelvic ring utilizing synthetic pelvic bones featuring complete disruption of the symphysis and sacroiliac joint was developed. Trauma surgeons of a level one academic hospital were invited to perform external fixation and emergency sacroiliac screw application under C-arm guidance. Prior to and following the simulation session, participants completed a subjective questionnaire assessing their confidence in emergency interventions on a 10-point Likert scale (10-LS). Objective parameters, such as intraoperative imaging quality, reduction accuracy, and the positioning of screws, wires, and external fixators, were also evaluated as secondary outcome measures.
Results
Fifteen trauma surgeons (10 residents, 5 consultants) participated in the simulation over the course of one day. The mean total operation time was 20.34 ± 6.06 min, without significant differences between consultants and residents (p = 0.604). The confidence for emergency SI-Screw placement increased significantly after the simulator (10-LS: Before = 3.8 ± 3.08 vs. After = 5.67 ± 2.35; p = 0.002) as well as after external fixation (10-LS: Before = 3.93 ± 2.79 vs. After = 6.07 ± 2.52; p = 0.002). In addition, confidence in (intraoperative) pelvic imaging increased significantly (10-LS: Before = 4.60 ± 3.0 vs. After = 6.53 ± 2.39; p = 0.011). Overall, the model was rated as a realistic simulation of clinical practice (10-LS = 7.87 ± 1.13).
Conclusions
Our unstable pelvis fracture model is a tool to practice emergency interventions such as external fixation and percutaneous techniques. Participants benefitted from this in terms of technical instrumentation as well as intraoperative imaging. Further studies are required to validate the objective benefits and improvements that participants undergo through frequent training.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13037-024-00412-0.
Keywords: Pelvis surgery, Simulation training, Emergency stabilization
Background
Emergency stabilization of unstable pelvic ring fractures can be challenging and requires repeated surgical practice to improve surgical skills. This is due to the complex anatomy and potentially fatal consequences of inaccurate instrumentation and the need for three-dimensional understanding of the surgeon [1]. These factors can be exacerbated in the setting of an emergency situation [2].
We hypothesize that a pelvic simulator could be used to develop and maintain essential obtained skills for pelvic fracture treatment, such as placement of external fixation and iliosacral screws [3]. Previous publications have underlined the importance of surgical simulators for practical skill development in the field of pelvic trauma [4, 5]. These simulators, have not been adjusted to current standards of minimal invasive pelvic fracture care yet. Pohlemann et al. introduced a pelvic emergency simulator that can be used to practice emergency procedures such as reduction of a closed pelvic fracture with a C-clamp without radiologic support and preperitoneal packing. In addition, Tucker et al. developed a simulator for percutaneous fixation of nondisplaced pelvic fractures [3]. Since C-clamps are rarely used in clinical practice, the interventions of interest for our simulation were external fixation and emergency SI-Screw application (Rescue Screws) since they best represent the emergency stabilization of the unstable pelvic ring in clinical practice in our department [6].
The aim of this study was to develop a simulation program using a standardized fracture model of the pelvis that can be used for adequate simulation of emergency interventions to prepare surgeons for challenging situations.
Methods
The reporting of this pre-post simulation study was performed in according to the STROBE guidelines (STROBE: Strengthening the Reporting of Observational Studies in Epidemiology) [7].
Setting
This pre- post simulation study was conducted at an academic level one trauma center in March 2024. The operative rooms of the surgical research facilities of the hospital were used. The room was equipped with a C-Arm and a radiolucent operation table, which were utilized for the study. Participation in the model was enabled for one entire day. Since this study presented a surgical simulation on synthetic bones and medical personnel took part voluntarily on their own time it is considered pursuant to Art. 2 (outside scope) of the Swiss Federal Act on Research involving Human Beings (Human Research Act, HRA). All participants provided informed consent.
Participants
The invitation to participate in this simulation was distributed to the trauma surgery team of the hospital (residents and consultants). Participation was not mandatory and was only realized on the surgeons’ individual behalf and in consideration of individual obligations in the clinical routine. Participants were stratified to a random number to account for anonymization during further analysis.
Questionnaire
Participants were asked to fill out a questionnaire, half of which were required to answer before and the other half after completing the simulation. Answers were either provided on a 10-point Likert scale (10-LS), a binary option (yes/no) or free to fill to the respective nature of the question to account for suitable analysis. On the 10-point Likert scale [1], indicated the lowest agreement/negative, and [10] indicated the highest agreement/positive.
Questions before the simulation (part A)
Are you still in residency? (yes/no)
How many years of experience do you have? (Free to fill, numeric)
Did you have experience with any other SI simulator in the past (yes/no)?
Do you think that training with an SI simulator can improve your ability to place SI screws? (10-LS)
How prepared do you feel to place SI-screws in an emergency situation? (10-LS)
How confident are you with intraoperative pelvic imaging (inlet/outlet)? (10-LS)
How confident do you feel with the installation of an external fixator for the pelvis? (10-LS)
Questions after the simulation (part B)
The SI-Simulator is a realistic model for placing SI-Screws. (10-LS)
In the future, I would like to use this SI-Simulator to improve my skills further. (10-LS)
Training with this SI simulator can improve my ability to place SI screws. (10-LS)
How prepared do you feel to place SI-screws in an emergency situation now? (10-LS)
How confident do you feel with intraoperative pelvic imaging (inlet/outlet view)? (10-LS)
How confident do you feel with the installation of an external fixator of the pelvis after the simulator? (10-LS)
Further comments (free to fill).
Secondary outcome variables
In addition to the subjective questionnaire, objective outcome parameters were assessed by the organization team of the simulator. These included the amount of radiation in mGray (automatically measured by the C-Arm for each participant), the time of total intervention and the two separate surgical steps (external fixation and SI-Screw). Further parameters assessed were damage of the balloon placed in the pelvic cavity, which simulated damage to the anatomic structures, and overall anatomic reduction, which was rated by the chief pelvic surgeon (range: bad-moderate-good). Sacroiliac screws were assessed for cortical (nonforaminal) and foraminal breaches, and the number of redirections/repositionings of the guidewire or screw was counted. The external fixator was assessed for malpositioning (i.e., contact with the intrapelvic cavity or acetabular joint). These parameters were assessed radiologically as well as by visual inspection of the synthetic pelvis after removal of the soft-tissue-mat.
Conduction of the pelvic fracture model
Our model was adapted from the pelvic simulator described by Tucker N and Mauffrey C et al., as seen and described on “The Ortho academy” website, a free, online platform developed with the purpose to disseminate global education in pelvic and acetabular surgery (https://www.theorthoacademy.com/) [3, 8].
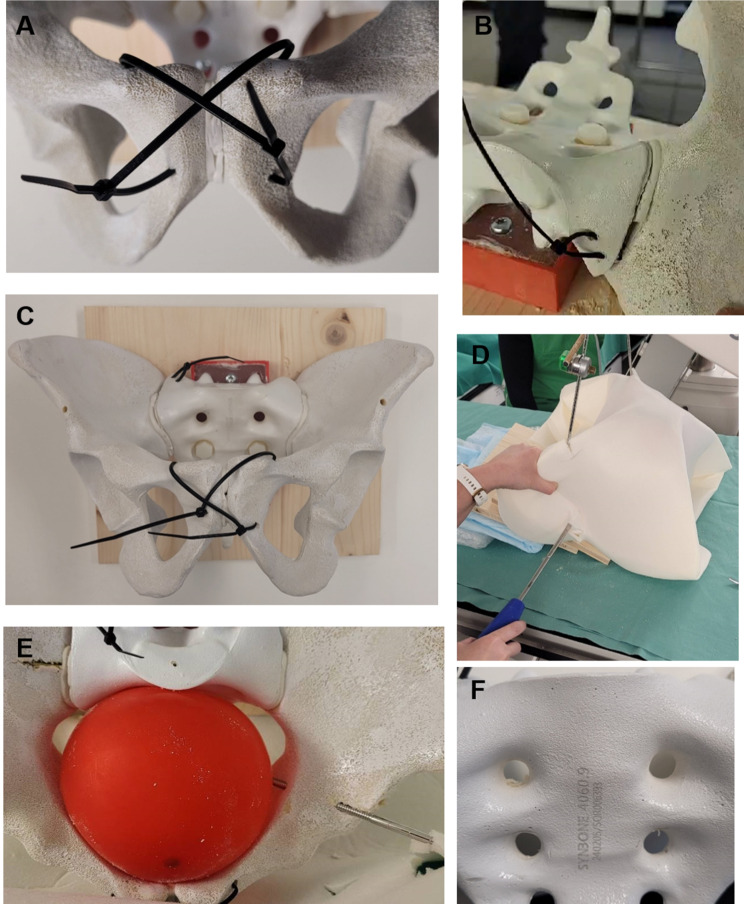
SYNBONE® pelvis models with radiopaque coating were utilized for this study (Model 4060.9, SYNBONE®, Zizers Switzerland). Modifications for fracture simulation were incorporated as described subsequently:
First, we drilled in three places at the top and bottom of both ends of the mounting block and fixed it to the wooden plate with three metal screws. The polyethylene part of the mounting block was shaved manually to fit the back posterior part of the sacral bone and allow plastic-screw application through the S2 foramina into the mounting block.
A surgical wire was applied to the automated driller to then drill through the symphysis in an X-shape from anterior and posterior directions. Afterwards, the symphysis was cut with a scalpel, and two cable ties were applied through the predrilled holes and strapped loosely to ensure instability.
The same procedure was used for the posterior part of the pelvic ring. Two parallel holes were screwed from the back of the right ilium toward the top of the sacrum outside of the direct sacroiliac joint. Next, one cable tie was inserted back and forth through the two holes and closed loosely.
Afterwards, the sacroiliac joint was cut with a scalpel, resulting in complete instability of the right hemipelvis, which was only held loosely by the cable wires.
A balloon with a diameter of 12 cm was placed inside the pelvis to simulate intrapelvic organs. Finally, the pelvic model structure was wrapped with a 0.5 cm thick, white polyester/polyurethan mat to simulate soft tissue coverage (Vlieseline Style-Vil). The edges of the mat and the back of the wooden plate were secured with staples. A collection of images from the simulation is presented in Fig. 1. The entire list of materials utilized is provided as an additional file (see Additional file 1).
Fig. 1.
Pelvic model and postoperative assessment. (A) Symphyseal disruption and fixation, (B) Sacroiliac disruption and fixation, (C) Pelvic model mounted on a wooden plate, (D) Sacroiliac screw application under fluoroscopy, (E) Intrapelvic balloon with penetrating external fixator, (F) Sacral bone with assessment of foraminal penetration on S1 level
Conduction of the simulation
According to the institutions radioprotective guidelines, participants were equipped with X-ray protective clothing and were not allowed to observe other participants during the simulation to control for a passive learning effect. Three conductors of the simulator (FK, KS, RP) attended the simulation and acted as operational personal. One conductor was in charge of positioning the C-Arm and performing the intraoperative imaging according to the participants’ request. The other ones handed over the requested surgical material and documented the a priori defined objective outcome parameters (i.e., time). Standard surgical material for these procedures was provided nonsterile.
Before the simulation started, the participant was required to answer questionnaire part A.
At the beginning of each round, the pelvis was already covered in the soft-tissue-mat and placed on the operation table at a 30° anterior tilt to account for anatomical positioning. Before the start, the participant was instructed on a suspected unstable pelvic ring in the synthetic pelvic model and asked to perform (1) external fixation of the pelvis either using a subcristal or supra-acetabular approach, (2) sacroiliac screw placement on the injured side and (3) reduction of the anterior and posterior pelvic ring. The participants was required to defect the injured side on their own and perform the aforementioned procedures. Intraoperative imaging was performed according to the participants’ instructions by In-, Outlet, Lateral and anterior imaging to simulate clinical practice at best. The participants could choose between cannulated, fully threated and partially threaded sacroiliac screws. The external fixator consisted of two Schanz pins with associated rods and clamps.
When the participant considered both operative steps to be completed, the soft-tissue mat was removed, and the reduction and placement of the screws and external fixator were inspected. Intraoperative images are presented in Fig. 2. Following the exercise, the participant were asked to complete the second part of the survey (part B).
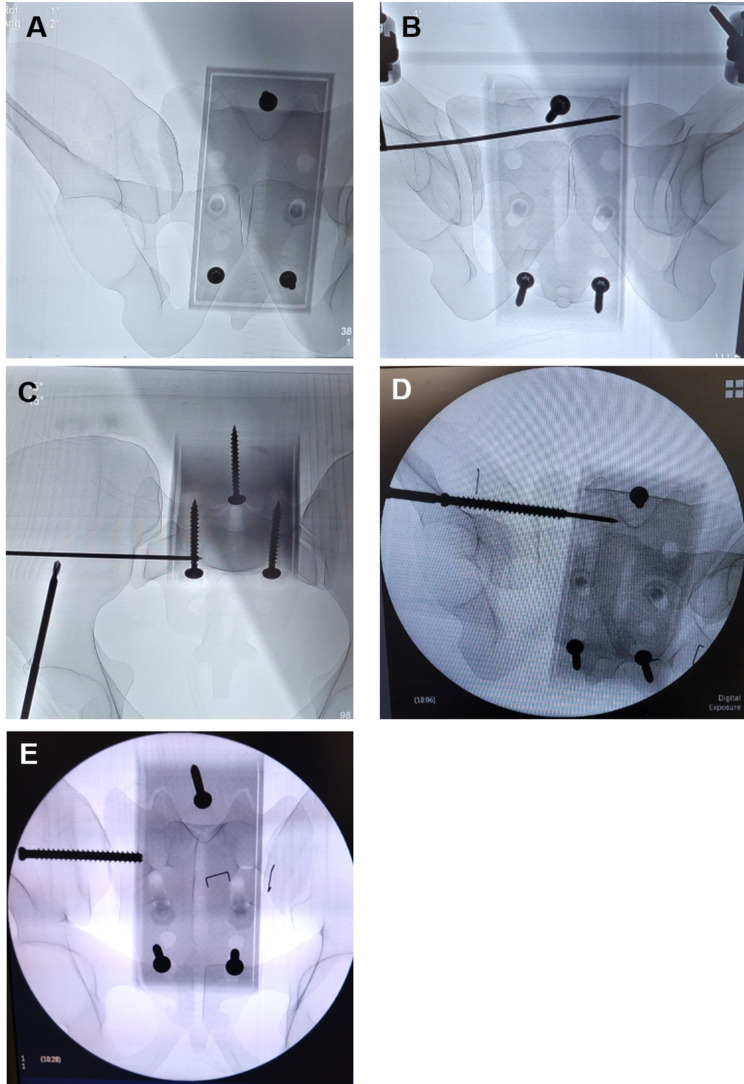
Fig. 2.
Intraoperative Imaging of Rescue Screw application. (A) Fluoroscopic presentation of the simulator with symphyseal and sacroiliac disruption on the right side, (B/C), Guidewire instrumentation on S1 level, (D) SI-screw application, (E) Postoperative imaging assessment with insufficient reduction of the posterior ring
Data analysis
Continuous data are presented as the mean and standard deviation, and categorical variables are presented as numbers and percentages. Missing data was planned to be excluded from the analysis, yet all data points could be collected. Statistical analysis was performed in R using the ‘Stat’ and ‘Tableone’ packages and the “ggplot2” package for the creation of figures [9]. MS-Excel was used for data visualization. The data were visually checked for normality using histograms. Categorical binary outcome data were assessed using a one-tailed Fisher’s exact test, and demographic data were assessed using a two-tailed Fisher’s exact test. Dependent parameters were assessed using a paired Wilcoxon test. Continuous parameters were analyzed using Student’s t test. The significance level was set at 0.05.
Validity assessment
Messick´s framework for construct validity was applied retrospectively to evaluate the effectiveness of our simulation model [10]. All five components of Messick´s framework were assessed: content, substantive, structural, generalizability and consequential validity.
Results
Participants
Fifteen trauma surgeons participated in this simulation over the course of one day on the 20th of March 2024. Ten participants (67%) were residents, five (33%) were consultants (senior physicians). One third of the participants (n = 5) were female physicians. The median professional experience of the participants was two years (IQR = 5.5), whereas the mean was 4.6 (± 5.75) years, representing the partially large experience gap between consultants and residents. Only three participants (20%) had previously participated in some part of the surgical pelvic simulation (Table 1).
Table 1.
Demographics and surgical details
| Parameter | Data |
|---|---|
| N | 15 |
| Residents, n (%) | 10 (67) |
| Male sex, n (%) | 10 (67) |
| Experience (years), (median/IQR) / (mean/SD) | 2 (5.5) / 4.60 (5.75) |
| Experience in pelvic models, n (%) | 3 (20) |
Surgical procedures
The entire operative procedure (external fixation + SI-screw) lasted on average 20.34 (± 6.06) minutes, without significant differences between residents and consultants (p = 0.604). The application of the external fixator took an average of 9.44 (± 2.37) minutes, and the application of the SI-Screw instrumentation took an average of 11.18 (± 4.51) minutes. There were also no significant differences between residents and consultants (p = 0.884/0.364). Significantly, more radiation was administered by consultants (197.4 mGray (± 85.25)) than by residents (78.81 mGray (± 81)) (Table 2).
Table 2.
Operative details
| Parameter | Data | p-value (R vs. C) |
|---|---|---|
| Total operation time (min), mean (± SD) | 20.34 (± 6.06) | 0.604 |
| Residents (R) | 20.48 (± 5.27) | |
| Consultants (C) | 22.57 (± 7.37) | |
| Time External fixation (min), mean (± SD) | 9.44 (± 2.37) | 0.884 |
| Residents (R) | 9.51 (± 2.21) | |
| Consultants (C) | 9.31 (± 3.23) | |
| Time SI-Screw, (min), mean (± SD) | 11.18 (± 4.51) | 0.364 |
| Residents (R) | 10.07 (± 3.03) | |
| Consultants (C) | 13.25 (± 7.00) | |
| Radiation (mGray), mean (± SD) | 121.16 (± 108.65) | 0.042 |
| Residents (R) | 78.81 (± 99.50) | |
| Consultants (C) | 197.4 (± 85.25) |
Subjective feedback
There was no significant difference in the estimated benefit of the pelvis simulator before and after conduction, which was very high (before: 9.20 ± 1.32 vs. after: 9.40 (± 0.91); p = 0.669). The confidence to perform SI-Screw placement in an emergency increased significantly from a mean of 3.8 (± 3.08) to 5.67 (± 2.35) after completing the simulation (p = 0.002) (Fig. 3). The same was true for the application of an external fixator, which increased from an initial 3.93 (± 2.79) points on the 10-point Likert scale to 6.07 (± 2.52) points (p = 0.002) (Fig. 4). Additionally, in terms of intraoperative pelvic imaging, the participants gained significantly more confidence (before: 4.60 ± 3.0 vs. after: 6.53 ± 2.39; p = 0.011) (Fig. 5) (Table 3). In a sub-analysis, residents in particular benefited in terms of improved confidence in the use of rescue screws, intraoperative imaging and external fixation compared to consultants (Table 3).
Fig. 3.
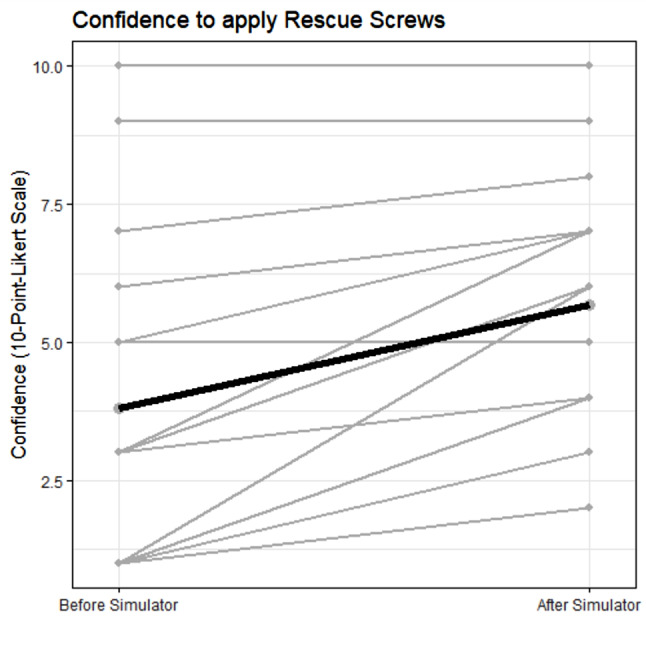
Participants’ self-reported confidence of the application of Rescue screws before training on the simulator (grey = participants, black/bold = mean)
Fig. 4.
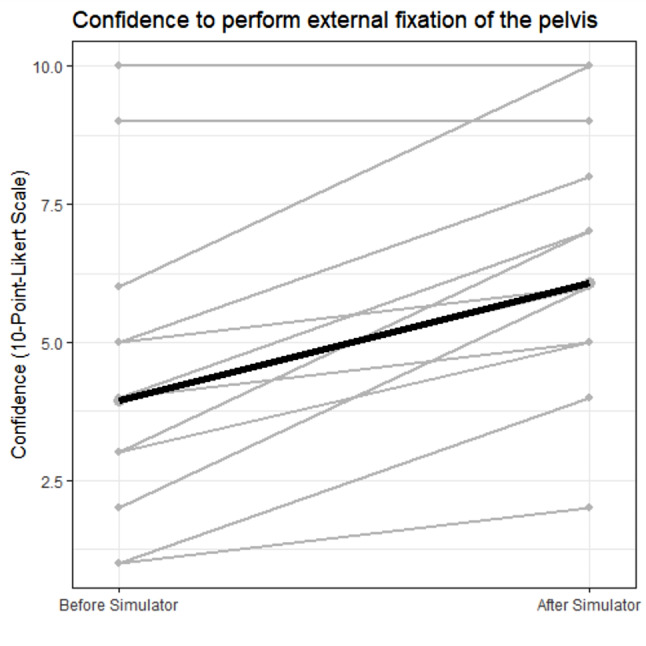
Participants’ self-reported confidence of the application external fixation before training on the simulator (grey = participants, black/bold = mean)
Fig. 5.
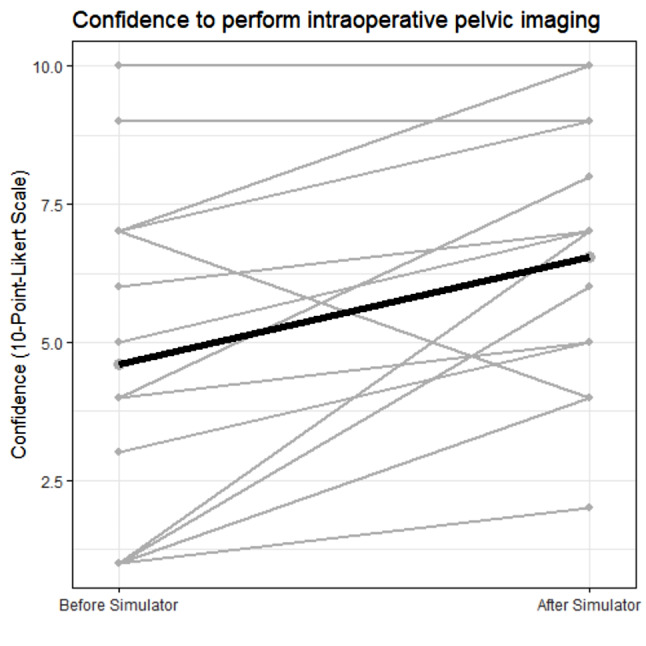
Participants’ self-reported confidence of the intraoperative imaging before training on the simulator (grey = participants, black/bold = mean)
Table 3.
All participants, 10-point-Likert scale (1=Lowest, 10=highest)
| Question | Before | After | p-value |
|---|---|---|---|
| Usefulness Simulator, mean(± SD) | 9.20 (± 1.32) | 9.40 (± 0.91) | 0.669 |
| Confidence Rescue Screw, mean(± SD) | 3.8 (± 3.08) | 5.67 (± 2.35) | 0.002 |
| Residents | 2.00 (± 1.41) | 4.40 (± 1.58) | 0.009 |
| Consultants | 7.40 (± 2.07) | 8.20 (± 1.30) | 1 |
| Confidence Imaging, mean (± SD) | 4.60 (± 3.0) | 6.53 (± 2.39) | 0.011 |
| Residents | 3.00 (± 2.05) | 5.30 (± 1.77) | 0.036 |
| Consultants | 7.80 (± 1.64) | 9.00 (± 1.22) | 0.181 |
| Confidence External Fixation, mean (± SD) | 3.93 (± 2.79) | 6.07 (± 2.52) | 0.002 |
| Residents | 2.60 (± 1.58) | 4.70 (± 1.70) | 0.005 |
| Consultants | 6.60 (± 2.88) | 8.80 (± 1.30) | 0.174 |
Overall, the simulator was rated as a realistic model for clinical practice (7.87 ± 1.13 points on a 10-point Likert scale), and everyone would like to use it again for practice reasons (9.47 ± 0.83 points) (Table 4).
Table 4.
Outcome parameters, 10-point-likert scale (1 = lowest, 10 = highest)
| Feedback | Data |
|---|---|
| Realistic Model, mean (± SD) | 7.87 (1.13) |
| Would like to do it again, mean (± SD) | 9.47 (0.83) |
Objective outcome parameters
Damage to the intrapelvic balloon occurred in only one patient (6.7%). Most reduction results were rated as moderate (n = 9, 60%). Five (33.3%) participants yielded a good reduction, and only one bad reduction (6.7%) occurred. Eight sacroiliac screws (53.3%) breached the cortical area, and three (20%) breached the foramen. On average, the participants performed 3.13 (± 2.17) redirections/repositionings of the screw or wire. Three external fixators (20%) were malpositioned, and whereas an overall of average of 1.20 (± 1.7) redirections was performed (Table 5).
Table 5.
Objective outcome parameter
| Parameter | Outcome |
|---|---|
| Balloon damage, n (%) | 1 (6.7) |
| Reduction quality, n (%) | |
| Good | 5 (33.3) |
| Moderate | 9 (60.0) |
| Bad | 1 (6.7) |
| SI-Screw/Wire | |
| Cortical breach, n (%) | 8 (53.3) |
| Foraminal breach, n (%) | 3 (20.0) |
| Number redirections, mean (± SD) | 3.13 (± 2.17) |
| External fixator | |
| Malpositioning, n (%) | 3 (20.0) |
| Number redirections, mean (± SD) | 1.20 (1.70) |
Validity assessment
The study demonstrates robust content, substantive, and structural validity, indicating that the simulation effectively emulates authentic surgical scenarios and enhances participant confidence and proficiency (Table 6).
Table 6.
Messick´s validity framework
| Aspect of Messick´s Validity | Definition | Evidence from Study |
|---|---|---|
| Content validity | The degree to which the content reflects the construct being measured. | Simulation includes all relevant procedures (e.g., SI-screw placement, external fixation). |
| Substantive validity | The relationship between participants’ responses and the construct. | Increased confidence in performing critical procedures, consistent with the aim of the simulation. |
| Structural validity | How well the structure of the assessment reflects the construct. | Confidence ratings and procedural outcomes align with expected skill improvements. |
| Generalizability | The extent to which results apply to other populations and settings. | Participants included residents and consultants; limited by single institution and small sample size. |
| Consequential validity | The impact of using the assessment on behavior and outcomes. | Increased interest in future practice and improved confidence, but no long-term outcomes (e.g. skills) assessed. |
Areas for further validation: Generalizability could be enhanced with a larger, more diverse sample across multiple settings. Consequential validity would benefit from follow-up studies assessing real-world outcomes post-simulation.
Discussion
In our manuscript, we provide a standardized and easy-to-build unstable pelvic fracture model with a clinical feasibility assessment by surgical experts. In regard to the performed simulation with surgical stabilization techniques, we conclude the following statements:
Practice with a pelvic simulator leads to increased confidence in the use of reposition maneuvers, emergency SI-screws, external fixation and intraoperative imaging in unstable pelvic ring fractures.
In our cohort, the less experienced participants presented the steepest increase in confidence after the simulation, potentially implying that they might especially benefit from this model.
An unstable pelvis fracture model can be built with accessible tools, and the surgical reality can be displayed to a certain extent.
Simulation training in surgery has already been established across several specialties and is reported to be beneficial for surgeons overall [5]. In pelvic surgery, several models already exist. Pohlemann et al. designed a realistic model that requires the application of a c-clamp as well as preperitoneal packing while blood loss is measured [11]. Undoubtedly, this is most likely one of most realistic simulator models available for pelvic emergency situations, yet it requires an extensive setup that might not be affordable for everyone and does not include intraoperative imaging. In addition, the C-clamp is rarely used in modern clinical practice, as percutaneous techniques such as rescue screws are used for the emergency stabilization of posterior pelvic ring fractures and dislocations. Our simulator reflects current standards in the treatment of pelvic injuries.
The Ortho Academy (www.theorthoacademy.com) designed a standardized model for percutaneous fixation of the pelvis that requires affordable material, which is the basis of our fracture simulator [8]. This model has already undergone pilot testing and yielded promising results [3]. The relevant difference here is that our model contains a standardized unstable fracture pattern and might therefore be more suitable for emergency situation training. Additionally, we performed several adjustments, such as the placement of the intrapelvic balloon, which might thereby sharpen the senses of the surgeon for this danger zone and lend the model a slightly drastic touch [4].
Our model is – to the knowledge of the authors – the first model that provides a simulation of an unstable pelvic situation that can be built very easily from everyone who is interested in it.
Frequent repetition of this kind of simulation is reported to provide the best outcome and can thereby quantify the direct impact on surgical performance [12]. The aim of our study was to report the initial subjective benefit reported by the participants and to describe the use of an unstable pelvic fracture simulator. The validation of its objective learning impact is planned for the future.
Simulation-based training is frequently reported in the literature as beneficial for an increase in confidence [13] and seems to be associated with an improved skillset [14]. In the context of surgical simulation, improved operative performance and shorter operation time are aspects that was reported in a recent meta-analysis on this topic [15]. Whether these improvements also occur by using our simulator needs to be assessed by a following study.
Simulation-based training is offered in different variations such as hands-on classes, virtual reality [16] and some hospitals even provide specific simulation centers for their staff [17]. Based on the literature, it may be assumed that especially less experienced participants (i.e. residents) might benefit more from simulation in terms of a steeper learning curve [18] but also more experienced surgeons may profit from a regular “fresh up” to stay in touch with the procedural steps and potential pitfalls. These assumptions are also displayed in our results and are comprehensible.
According to a recent international survey, external fixation is the most common surgical emergency intervention for unstable pelvic ring injuries [6]. With respect to several options for positioning (i.e., supra-acetabular, anterosuperior, etc.), malpositioning and/or inadequate reduction may occur [19]. Emergency sacroiliac screws (“Rescue Screws”) might be somehow more challenging, but – if they are performed properly – they provide sufficient and (at least partial) definitive stabilization of the posterior pelvic ring and close the intrapelvic cavity [20, 21]. Another benefit is that early mobilization is immediately possible in most trauma cases and is limited if external fixation or c-clamps are used. Depending on the overall fracture morphology and the anterior pelvis, an additional external fixator can be placed to manually control the reduction. We propose that these two stabilization techniques should be used by every trauma surgeon.
In an emergency, surgical procedures with the best precision possible are urgently needed. The key to doing so is frequent practice. However, whereas for sacroiliac screw instrumentation, navigated instrumentation has become increasingly established, percutaneous application with the C-Arm view might move into the background [22, 23]. This might occur at the cost of the ability to perform this procedure in an emergency situation, where up-to-date navigation is not feasible due to partially extensive setup times and technical challenges [23]. Frequent training with a simulator might be one step to be on top of practice and retrieve this knowledge when it is needed.
On the other hand, relatively high malpositioning rates of up to 35% have been reported in the literature [24]. Regular training with a simulator might certainly be a way to improve this kind of complication since it allows a deeper understanding of the safe osseous corridors and surgical instrumentation relying on intraoperative fluoroscopy.
According to our results, the simulator resulted in elevated confidence of particularly the residents in performing emergency repositioning, emergency SI-screws (rescue screws), external fixation of the pelvis and intraoperative imaging. The fact that confidence did not increase significantly in the counsellor group may be explained by the fact that their confidence was already high before the simulation and the sample size (n = 5) remained relatively small in the sub-analysis; however, an upward trend was also observed in this group. Interestingly, the consultants administered more intraoperative radiation than did the residents. One likely reason is that they are more aware of the benefits of intraoperative imaging and frequent changes in in- and outlet views, as well as dynamic screening, which enables them to provide an improved three-dimensional conception [25].
Strengths and limitations
The strength of our model is that it is easy to use and inexpensive. The utilized synthetic bones with a simulated soft tissue cover reflect the clinical reality to a certain degree and force the surgeon to rely mostly on intraoperative imaging. This cover can be removed easily after the simulation has finished and provides the participant with a detailed look on the anatomic results and placement of the screws/external fixator, which provides a learning benefit. However, our model naturally cannot simulate physiological impediments to imaging, such as intrapelvic organs. Nevertheless, intra-osseous positioning of hardware does not require additional simulation of intrapelvic organs. Our questionnaire and assessment criteria have not specifically been validated before, yet we are confident that it can display our parameters of interest reliably.
However, this easy feasibility is associated with certain restrictions for clinical translation. For example, the pelvic bone is not attached to a femur, which in clinical practice is often necessary as support for adequate reduction of the fracture. Second, the pelvic model is much lighter than a patient is in real life, and the mat covering the pelvis provides only an approximation of the entire soft tissue, which varies greatly depending on the patient’s physical condition. Our study size might be relatively small with 15 participants overall and might be underpowered in certain aspects, especially in the subgroup analysis (residents vs. consultants) and may contain (unintentional) selection bias. Yet, the focus of our study was on the overall feasibility to conduct this kind of simulator training. Whether an increase of confidence to perform a task is directly associated with improved skills is a separate topic and widely discussed in the literature. In order to further validate the relevance of our model in mimicking relevant emergency pelvic cases, a validation study in a different hospital should be planned.
Conclusions
Our unstable pelvis fracture model is a feasible tool for performing emergency interventions and repositioning techniques. Participants benefitted from this in terms of technical instrumentation as well as intraoperative imaging. Further studies are required to validate the objective benefits and improvements that participants undergo through frequent training.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- SI
Sacroiliac
- mGray
Milligray
- 10-LS
10-Point Likert Scale
Author contributions
F.K.L.K.: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.K.S.: Data curation, Investigation, Writing – original draft, Writing – review & editing.A.M.: Conceptualization, Investigation, Methodology, Writing – review & editing.Y.K.: Conceptualization, Methodology, Writing – review & editing.T.B.: Conceptualization, Methodology, Writing – review & editing.S.H.: Methodology, Writing – review & editing.M.T.: Methodology, Writing – review & editing.V.N.: Methodology, Writing – review & editing.C.M.: Conceptualization, Writing – review & editing.H.-C.P.: Conceptualization, Project administration, Supervision, Writing – review & editing.R.P.: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project .administration, Supervision, Writing – original draft, Writing – review & editing.
Funding
No external funding sources were utilized.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval
Not applicable.
Competing interests
On behalf of all the authors, the corresponding author states that there are no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Symer MM, Keller DS. Human factors in pelvic surgery. Eur J Surg Oncol. 2022;48(11):2346–51. [DOI] [PubMed] [Google Scholar]
- 2.Giannoudis PV, Pape HC. Damage control orthopaedics in unstable pelvic ring injuries. Injury. 2004;35(7):671–7. [DOI] [PubMed] [Google Scholar]
- 3.Tucker NJ, Nardi M, Herrera RF, Scott BL, Heare A, Stacey SC et al. Percutaneous pelvic fixation model: an affordable and realistic simulator for pelvic trauma training. Eur J Orthop Surg Traumatol. 2023. [DOI] [PubMed]
- 4.Riehl J, Widmaier J. A simulator model for sacroiliac screw placement. J Surg Educ. 2012;69(3):282–5. [DOI] [PubMed] [Google Scholar]
- 5.Marchand LS, Sciadini MF. Simulation Training in fracture surgery. J Am Acad Orthop Surg. 2020;28(21):e939–47. [DOI] [PubMed] [Google Scholar]
- 6.Klingebiel FK, Hasegawa M, Parry J, Balogh ZJ, Sen RK, Kalbas Y, et al. Standard practice in the treatment of unstable pelvic ring injuries: an international survey. Int Orthop. 2023;47(9):2301–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. [DOI] [PubMed] [Google Scholar]
- 8.The ortho academy. [cited 2024 29.03.2024]. https://www.theorthoacademy.com/percutaneouspelvicfixationsimulator
- 9.R Core Team. (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org/
- 10.Hamstra SJ, Yamazaki K. A Validity Framework for Effective Analysis and Interpretation of Milestones Data. J Grad Med Educ. 2021;13(2 Suppl):75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pohlemann T, Culemann U, Holstein JH. Initial experience using a pelvic emergency simulator to train reduction in blood loss. Clin Orthop Relat Res. 2012;470(8):2098–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egol KA, Phillips D, Vongbandith T, Szyld D, Strauss EJ. Do orthopaedic fracture skills courses improve resident performance? Injury. 2015;46(4):547–51. [DOI] [PubMed] [Google Scholar]
- 13.Yean LE, Hashim SAB. Role of surgical simulation on self-reported confidence level on cardiothoracic surgical trainees. J Cardiothorac Surg. 2024;19(1):293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aydın A, Ahmed K, Abe T, Raison N, Van Hemelrijck M, Garmo H, et al. Effect of Simulation-based Training on Surgical proficiency and patient outcomes: a Randomised Controlled Clinical and Educational Trial. Eur Urol. 2022;81(4):385–93. [DOI] [PubMed] [Google Scholar]
- 15.Meling TR, Meling TR. The impact of surgical simulation on patient outcomes: a systematic review and meta-analysis. Neurosurg Rev. 2021;44(2):843–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lesch H, Johnson E, Peters J, Cendán JC. VR Simulation leads to enhanced procedural confidence for Surgical trainees. J Surg Educ. 2020;77(1):213–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kolbe M, Goldhahn J, Useini M, Grande B. Asking for help is a strength-how to promote undergraduate medical students’ teamwork through simulation training and interprofessional faculty. Front Psychol. 2023;14:1214091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cardoso SA, Suyambu J, Iqbal J, Cortes Jaimes DC, Amin A, Sikto JT, et al. Exploring the role of Simulation Training in improving Surgical skills among residents: a narrative review. Cureus. 2023;15(9):e44654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McDonald C, Firoozabadi R, Routt ML Jr. Complications Associated with Pelvic External fixation. Orthopedics. 2017;40(6):e959–63. [DOI] [PubMed] [Google Scholar]
- 20.Gardner MJ, Chip Routt ML Jr. The antishock iliosacral screw. J Orthop Trauma. 2010;24(10):e86–9. [DOI] [PubMed] [Google Scholar]
- 21.Schmal H, Larsen MS, Stuby F, Strohm PC, Reising K, Goodwin Burri K. Effectiveness and complications of primary C-clamp stabilization or external fixation for unstable pelvic fractures. Injury. 2019;50(11):1959–65. [DOI] [PubMed] [Google Scholar]
- 22.Kalbas Y, Hoch Y, Klingebiel FK, Klee O, Cester D, Halvachizadeh S, et al. 3D-navigation for SI screw fixation - how does it affect radiation exposure for patients and medical personnel? Injury. 2024;55(2):111214. [DOI] [PubMed] [Google Scholar]
- 23.Takeba J, Umakoshi K, Kikuchi S, Matsumoto H, Annen S, Moriyama N, et al. Accuracy of screw fixation using the O-arm(®) and StealthStation(®) navigation system for unstable pelvic ring fractures. Eur J Orthop Surg Traumatol. 2018;28(3):431–8. [DOI] [PubMed] [Google Scholar]
- 24.Hadeed MM, Woods D, Koerner J, Strage KE, Mauffrey C, Parry JA. Risk factors for screw breach and iatrogenic nerve injury in percutaneous posterior pelvic ring fixation. J Clin Orthop Trauma. 2022;33:101994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hasegawa IG, Gary JL. Intraoperative imaging challenges during Pelvic Ring disruptions and Acetabular fracture surgery. Orthop Clin North Am. 2024;55(1):73–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.