Abstract
Background:
The indications for hip arthroscopy in patients aged ≥40 years remain controversial, as observational studies have suggested that advanced age portends poor functional outcomes, poor durability of improvement, and high rates of conversion to total hip arthroplasty.
Purpose:
To compare hip arthroscopy versus nonoperative management for symptomatic labral tears in patients aged ≥40 years with limited radiographic osteoarthritis.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
This single-surgeon, parallel randomized controlled trial included patients aged ≥40 years with limited osteoarthritis (Tönnis grades 0-2) who were randomized 1:1 to arthroscopic surgery with postoperative physical therapy (SPT) or physical therapy alone (PTA). Patients who received PTA and achieved unsatisfactory improvement were permitted to cross over to SPT after completing ≥14 weeks of physical therapy (CO). The primary outcomes were the International Hip Outcome Tool-33 score and modified Harris Hip Score at 24 months after surgery, and secondary outcomes included other patient-reported outcome measures and the visual analog scale for pain. The primary analysis was performed on an intention-to-treat basis using linear mixed-effects models. Sensitivity analyses included modified as-treated and treatment-failure analyses.
Results:
A total of 97 patients were included, with 52 (53.6%) patients in the SPT group and 45 (46.4%) patients in the PTA group. Of the patients who underwent PTA, 32 (71.1%) patients crossed over to arthroscopy at a mean of 5.10 months (SD, 3.3 months) after physical therapy initiation. In both intention-to-treat and modified as-treated analyses, the SPT group displayed superior mean patient-reported outcome measure and pain scores across the study period for nearly all metrics relative to the PTA group. In the treatment-failure analysis, the SPT and CO groups showed greater improvement across all metrics compared with PTA; however, post hoc analyses revealed no significant differences in improvement between the SPT and CO groups. No significant differences were observed between groups in rates of total hip arthroplasty conversion.
Conclusion:
In patients ≥40 years of age with limited osteoarthritis, hip arthroscopy with postoperative physical therapy led to better outcomes than PTA at a 24-month follow-up. However, additional preoperative physical therapy did not compromise surgical outcomes and allowed some patients to avoid surgery. When surgery is indicated, age ≥40 years should not be considered an independent contraindication to arthroscopic acetabular labral repair.
Registration:
NCT03909178 (ClinicalTrials.gov identifier).
Keywords: randomized controlled trial, acetabular labral tear, hip arthroscopy, physical therapy, patient-reported outcome measures
Acetabular labral tears secondary to femoroacetabular impingement (FAI) are a well-recognized source of hip pain that, when left untreated, pose an elevated risk for the accelerated progression of early-onset osteoarthritis.3,17,20,49 The increased shear stress, redistribution of contact forces, and biomechanical adaptations that occur in the setting of FAI and acetabular labral tears inflict detrimental effects on the articular cartilage and chondrolabral junction.8,49 Thus, the utilization of and clinical indications for hip arthroscopy have expanded over the last 2 decades, resulting in a more diverse range of patients receiving arthroscopic treatment for acetabular labral tears secondary to FAI. Although hip arthroscopy has generally demonstrated positive long-term outcomes, favorable results are predicated on careful patient selection. Although the use of hip arthroscopy is well supported in young, active patients, 4 its utilization in older patients with limited osteoarthritis remains controversial.27,54
Randomized controlled trials (RCTs) comparing hip arthroscopy with physical therapy (PT) for FAI have largely surmised that whereas both treatment modalities can provide significant symptom improvement, hip arthroscopy yields superior clinical benefit and patient-reported outcome measures (PROMs). 39 Three multicenter RCTs have found that surgery leads to significantly greater PROM improvement compared with PT in younger patients (mean age, 33-36 years) at short-term follow-up.19,23,44 Similarly, the 12-month results from the present RCT showed that patients aged ≥40 years who underwent hip arthroscopy reported significantly greater PROMs compared with those who underwent PT alone (PTA), with differences between groups surpassing minimal clinically important difference (MCID) thresholds. 33 Although the single RCT to report 24-month outcomes found no significant difference in improvements between surgery and PT, the study was criticized for its failure to account for high rates of crossover in statistical analyses, limiting the applicability of its findings.15,31 Indeed, surgical RCTs benefit from choosing short primary endpoints to avoid type 2 errors in their intention-to-treat (ITT) analysis; however, sensitivity analyses and appropriate transparency when drawing conclusions can mitigate these downfalls.15,24,45
Extended follow-up is necessary to accurately assess the clinical benefit of surgery in patients ≥40 years of age, as evidenced by several recent studies that have drawn into question the durability of improvements seen in older patients after hip arthroscopy. McCormick et al 38 conducted a case-control study revealing that age >40 years and grade 4 Outerbridge osteoarthritis at the time of arthroscopy were associated with worse PROMs at a minimum 2-year follow-up. A systematic review of hip arthroscopy outcomes in older patients reported rates of conversion to total hip arthroplasty (THA) of 18.1% in patients aged ≥40 years and 23.1% in patients aged ≥50 years at a mean follow-up time of only 25 months. 22 Additionally, an investigation into recovery trajectories by Bodendorfer et al 6 revealed that older age predicted late regression in PROMs at a minimum 2-year follow-up. Although other studies have reported similar findings,16,28 the prognostic implications of age remain contested, as age alone may not be a sole predictor but may represent a surrogate for age-related degeneration and poor outcomes.46,50 Whereas the current literature provides strong evidence that advanced osteoarthritis is a contraindication to hip arthroscopy, older patients with limited osteoarthritis may benefit from hip arthroscopy or nonoperative management before resorting to THA. 16 However, given the low survivorship and poor sustainability in PROM improvements after hip arthroscopy observed in older patients with only limited osteoarthritis, further investigation is warranted to assess the optimal treatment modality for this patient population. Thus, the purpose of the current study was to perform an RCT comparing arthroscopic surgical management versus nonoperative management in patients with symptomatic labral tears who were ≥40 years old and did not have severe osteoarthritis. We hypothesized that hip arthroscopy would not be more clinically effective than PT in these patients at a 24-month follow-up.
Methods
Study Design and Oversight
This study was a single-surgeon (S.D.M.), parallel RCT comparing hip arthroscopy versus PT for the treatment of acetabular labral tears secondary to FAI in patients aged ≥40 years. All study procedures were approved by the senior author’s (S.D.M.) institutional review board (No. 2013P001442) and performed according to the protocol published on ClinicalTrials.gov in April 2019 (NCT03909178). 32
Patient Population
Consecutive patients presenting to the senior author’s clinic between December 2013 and June 2020 were offered enrollment in the study if they met eligibility criteria. Details pertaining to patient selection, inclusion criteria, and exclusion criteria have been reported previously. 33 For the purpose of the present study, patients without a minimum 24-month follow-up were excluded from our analyses unless they converted to THA or underwent a revision hip arthroscopy before the 24-month follow-up, in which case their PROMs before failure were included.
Sample Size Calculation
As previously published, 32 80 participants were needed to detect a 10-point difference in modified Harris Hip Score (mHHS) between cohorts (power = 0.8, alpha = .05). To account for the expected 9% to 13% loss to follow-up rate at the primary endpoint of 12 months, we originally aimed to enroll 90 patients in this study. However, as seen in other prominent surgical RCTs with similar designs,24,45 we expected a substantial crossover rate. Thus, in an effort to maintain power in our ITT analysis and account for an expected loss to follow-up of 12% to 20%, as seen in other surgical RCTs with a 24-month follow-up,1,31 we increased our initial enrollment target to 110 patients.
Interventions and Randomization
For ethical reasons and in accordance with the senior author’s standardized, preoperative evaluation for patients presenting with hip pain, all patients with positive clinical and radiographic findings confirming the presence of a symptomatic acetabular labral tear first underwent nonoperative management for at least 12 weeks before being offered enrollment in the study. Nonoperative management included an intra-articular hip joint injection (eg, combined local anesthetic with a low-dose corticosteroid) and core-based PT (with a home-based component). Patients who did not improve from this nonoperative therapy were offered enrollment in the study. Patients who gave informed consent were randomized in a 1:1 ratio to surgery plus PT (SPT) or PTA. Notably, patients and health care providers were both unblinded due to the infeasibility of blinding.
SPT Group
Patients randomized to the SPT group consented to arthroscopic acetabular labral repair with femoroacetabular osteoplasty. As previously published, the senior surgeon’s hip arthroscopy technique includes sparing use of intermittent traction, 52 pulsed intra-articular lavage to maintain ambient intra-articular temperatures during use of thermal wands, 2 puncture capsulotomy to access the central compartment,11,14 microfracture (2013-2016) or bone marrow aspirate concentrate augmentation (2016-2020) to address significant chondral defects,25,34,35 sparing use of electrocautery, 37 and an emphasis on chondrolabral junction preservation.42,53 Importantly, labral lesions were repaired if adequate, healthy tissue was amenable to suture anchor fixation, but if the labrum was found to be irreparable (eg, tissue insufficiency, advanced degeneration, complex tears), labral reconstruction was used according to a previously published capsular augmentation technique. 41 After surgery, all patients in the SPT group underwent a 5-phase standardized postoperative PT program developed jointly by the senior author (a sports medicine fellowship-trained orthopaedic surgeon) and physical therapists. 40 Details of the postoperative PT protocol are included in Appendix A (available in the online version of this article).
PTA Group
Patients randomized to the PTA group were assigned a standardized, 24-week course of supervised, core-based PT that included active strengthening exercises. 21 This course, designed in concert with physical therapists, was tailored to patients aged ≥40 years with symptomatic acetabular labral tears and mild to moderate osteoarthritis and included the essential elements of the most effective PT protocols, based on the current literature. 21 Specifically, weeks 1 and 2 were focused on gait retraining, and weeks 3 through 24 were focused on optimizing range of motion while slowly integrating active strength training. Unlike the prerandomization PT protocol that all patients completed, the protocol made for the PTA group was predominantly supervised by physical therapists (at least 1 in-person visit per week). Details of the complete 24-week PT protocol assigned to patients who underwent PTA are included in Appendix B (available online).
Crossover
Patients who underwent PTA were permitted to cross over to SPT if (1) they had completed at least 14 weeks of PT and (2) their independent physical therapists determined that they had achieved maximal possible improvement from PTA.
Data Collection
Demographic and descriptive data including age, sex, laterality, body mass index, and radiographic measurements were obtained at the time of randomization. Pre-enrollment standing anteroposterior and Dunn lateral radiographs of the pelvis were assessed to identify the presence of pincer-type and cam-type FAI. 47 Anteroposterior radiographs were also used to obtain Tönnis grade and lateral center-edge angle. Pre-enrollment magnetic resonance imaging scans and associated radiographic reports were assessed for labral condition.
The primary outcome of this original trial was mHHS at 12 months, as has been previously reported. 33 The present study’s primary outcomes, the International Hip Outcome Tool-33 (iHOT-33) score and mHHS at 24 months after surgery (SPT) or the start of PT (PTA), were thus secondary outcomes of the original trial. 33 Secondary outcomes of the present study included the Non-Arthritic Hip Score, Hip Outcome Score–Activities of Daily Living Subscale, Hip Outcome Score–Sports Subscale, and pain symptoms tracked using a standard visual analog scale. Clinically meaningful outcomes were assessed by calculating the number of patients who achieved previously published maximum outcome improvement (MOI) thresholds.30,43 Finally, rates of revision hip arthroscopy and conversion to THA were also tracked.
Statistical Analysis
To account for the repeated-measures data structure of our outcome metrics, we used linear mixed-effects models to assess improvement trajectories across the study period. 7 These models accommodate within-participant correlations over time by linking observations for each participant, account for variability between participants, and incorporate all available data rather than excluding participants missing a single follow-up time point, as would be the case in a repeated-measures analysis of variance. Each regression clustered observations at the patient level; modeled time, treatment, and their interaction as fixed effects; and included random by-participant intercepts. Parameter estimates and descriptive statistics for continuous variables are presented with 95% CIs, with the PTA cohort treated as the reference group (if applicable). Frequency statistics are reported for all noncontinuous variables. A P value of <.05 was considered statistically significant. All statistical analyses were performed using R Version 4.2.1 (R Foundation for Statistical Computing).
ITT Analysis
The primary analysis used a standard ITT approach, in which patients were evaluated in the group to which they were randomly assigned. Weighted mean differences in PROMs and pain scores between SPT and PTA across the study period were calculated with time modeled as a continuous variable. Adjusted mean PROM and pain scores at discrete time points were calculated with time modeled as a categorical variable and compared between groups at each time point. Importantly, given the significant limitations of ITT analyses in providing accurate results in the setting of surgical RCTs with high rates of crossover and extended follow-up,15,29 we performed a series of sensitivity analyses. All sensitivity analyses were designed in conjunction with an independent institutional biostatistician with the goal of retaining statistical power despite high rates of crossover.
Modified As-Treated Analysis
We conducted a modified as-treated analysis using identical methods as those described for the ITT analysis, with the exception that the fixed effect of treatment assignment was replaced with a time-varying fixed effect for the patient’s actual treatment. Thus, for the patients who crossed over, their scores before crossover (ie, before surgery) are attributed to PTA, while their scores after crossover (ie, after surgery) are attributed to SPT. Like the ITT analysis, weighted mean differences in scores across the study period and adjusted mean scores at discrete time points were compared between groups.
Treatment-Failure Analysis
We conducted a treatment-failure analysis to compare PROM and pain score improvements among patients in the SPT group, the PTA group, and a separate crossover (CO) group, using scores at the 24-month follow-up or the time of failure to assess the maximum improvement achieved by each course of treatment within 24 months. Failure was defined as crossing over to SPT, undergoing a revision hip arthroscopy, or converting to THA. PROM and pain scores at the 24-month follow-up were used for all patients except for those who experienced failure before 24 months, in which case the PROM and pain scores at the time of failure were used. Regarding the patients who crossed over, the scores at the time of PT failure (ie, immediately before crossover) were attributed to PTA; however, their 24-month follow-up scores after surgery (ie, 24 months after crossover) were attributed to crossover. The requirements for crossover consisted of an independent physical therapist determining that the patient could receive no additional benefit from PTA and the patient being unwilling to continue PT given the lack of progress. A description of each cohort included in the treatment-failure analysis can be seen in Appendix Table A1 (available online). Thus, this analysis compares the maximum improvement that all patients who underwent PTA received from PT and the maximum improvement that all patients who underwent surgery received from surgery within 24 months. Furthermore, separating SPT and CO postoperative PROM and pain scores allowed us to assess the effect of additional preoperative PT on postoperative outcomes. Improvements between the 3 groups were compared using an analysis of variance with Tukey post hoc analysis. Finally, a binary logistic regression was used to analyze the relationship between course of treatment (ie, PTA, SPT, or CO), age, and Tönnis grade on the probability of achieving the iHOT-33 MOI threshold value. 30 MOI, a psychometric tool that detects clinical success and satisfaction after hip arthroscopy, can be defined as the patient’s change in functional score divided by their total possible improvement (ie, the difference between the maximum score for the specific PRO and the patient’s baseline score). 30 MOI was chosen over other clinically meaningful outcome measures because its threshold values are not unique for a given follow-up time point, as is the case for MCID, Patient Acceptable Symptom State, and substantial clinical benefit. Furthermore, studies have shown that whereas MCID and Patient Acceptable Symptom State achievement are greatly influenced by baseline score, MOI effectively limits potential ceiling effects.5,26
Results
Participants
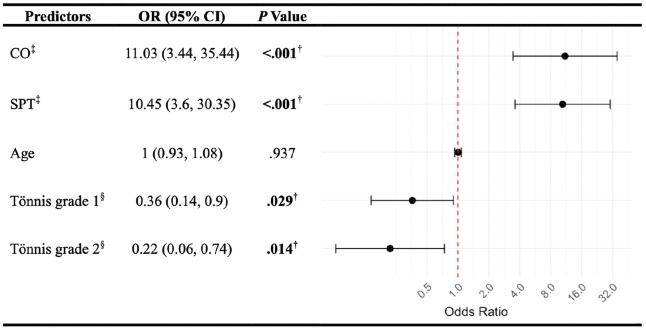
A total of 110 patients were prospectively enrolled in the present study, with 57 (51.8%) patients in the SPT group and 53 (48.2%) patients in the PTA group (Figure 1). Of these patients, 7 (3 SPT, 4 PTA) patients did not undergo their assigned treatment protocol, and 6 (2 SPT, 4 PTA) patients were lost to follow-up before 24 months. Thus, the remaining 97 (52 SPT [53.6%], 45 PTA [46.4%]) patients were included and are the basis of this analysis. The cohort was composed of 40 (41.2%) men and 57 (58.8%) women with a mean age of 48.34 years (SD, 5.7 years), mean body mass index of 26.38 (SD, 4.1), and mean Tönnis grade of 0.82 (SD, 0.7) (Table 1). At the time of analysis, 32 (71.1%) patients who underwent PTA had not achieved adequate progression and crossed over to hip arthroscopy at mean of 5.10 months (SD, 3.3 months; median, 3.88 months) after initiation of the PT protocol.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram. PT, physical therapy; PTA, physical therapy alone; SPT, surgery and physical therapy.
Table 1.
Characteristics of Patients Randomized to SPT and PTA Groups and Patients Who Crossed Over From PTA to SPT a
| SPT Group (n = 52) | PTA Group (n = 45) | CO Group (n = 32) | |
|---|---|---|---|
| Age, y | 47.7 ± 6.0 | 49 ± 5.3 | 49.3 ± 5.1 |
| BMI | 26.5 ± 4.4 | 26.3 ± 3.8 | 26.9 ± 3.8 |
| Sex | |||
| Male | 21 (40.4) | 19 (42.2) | 15 (46.9) |
| Female | 31 (59.6) | 26 (57.8) | 17 (53.1) |
| Race | |||
| White | 48 (92.3) | 41 (91.1) | 31 (96.9) |
| Black | 1 (1.9) | 00 (0) | 00 (0) |
| Asian | 2 (3.8) | 00 (0) | 00 (0) |
| Other | 1 (1.9) | 4 (8.9) | 1 (3.1) |
| Laterality | |||
| Right | 22 (42.3) | 29 (64.4) | 22 (68.8) |
| Left | 30 (57.7) | 16 (35.6) | 10 (31.3) |
| Depression | 4 (7.7) | 5 (11.1) | 3 (9.4) |
| Low back pain | 18 (34.6) | 20 (44.4) | 15 (46.9) |
| Tönnis grade | |||
| 0 | 21 (40.4) | 13 (28.9) | 11 (34.4) |
| 1 | 24 (46.2) | 22 (48.9) | 14 (43.8) |
| 2 | 7 (13.5) | 10 (22.2) | 7 (21.9) |
| Tönnis angle, deg | 5.1 ± 6.2 | 4.3 ± 5.7 | 5.0 ± 6.2 |
| LCEA, deg | 33.0 ± 7.8 | 33.3 ± 6.1 | 33.0 ± 6.7 |
| Alpha angle, deg | 53.3 ± 16.7 | 54.5 ± 17.2 | 54.5 ± 17.5 |
| Radiographic pincer lesion | 20 (38.5) | 23 (51.1) | 15 (46.9) |
| Radiographic cam lesion | 27 (51.9) | 22 (48.9) | 16 (50) |
| MRI labral condition | |||
| Discrete, linear tear | 38 (73.1) | 33 (73.3) | 22 (68.8) |
| Complex tear | 8 (15.4) | 5 (11.1) | 5 (15.6) |
| Degenerative tear | 6 (11.5) | 7 (15.6) | 5 (15.6) |
Data are presented as mean ± SD or n (%). BMI, body mass index; CO, crossover; LCEA, lateral center-edge angle; MRI, magnetic resonance imaging; PTA, physical therapy alone; SPT, surgery and physical therapy.
Primary Analysis
In the ITT analysis, SPT resulted in significantly higher overall iHOT-33 scores compared with PTA across the treatment period (mean difference, 10.5; 95% CI, 3.1-17.9; P = .006) (Table 2). Evaluating adjusted mean iHOT-33 scores at discrete time points also revealed significantly higher scores resulting from SPT at the 3-month (P < .001), 6-month (P = .004), and 12-month (P = .010) follow-ups, but no significant difference was observed at the 24-month follow-up (P = .255) (Table 3). SPT also resulted in significantly higher overall mHHS values compared with PTA across the treatment period (mean difference, 6.4; 95% CI, 1.1-11.7; P = .019) and significantly higher mean mHHS values at the 3-month (P < .001) and 6-month (P = .029) follow-ups. However, no differences were observed in adjusted mean mHHS values at the 12-month (P = .074) and 24-month (P = .157) follow-ups (Tables 2 and 3).
Table 2.
Weighted Differences in Mean PROM and Pain Scores Between SPT and PTA Groups: Intention-to-Treat Analysis a
| PROM | Weighted Difference in Mean Score (95% CI) b | P Value |
|---|---|---|
| iHOT-33 | 10.5 (3.1 to 17.9) | .006 c |
| mHHS | 6.4 (1.1 to 11.7) | .019 c |
| NAHS | 6.8 (1.2 to 12.4) | .017 c |
| HOS-ADL | 6.3 (0.7 to 11.8) | .027 c |
| HOS-SS | 3.4 (–6.1 to 12.9) | .482 |
| VAS | −1.2 (–2.1 to −0.3) | .008 c |
HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sports Subscale; iHOT-33, International Hip Outcome Tool-33; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; PROM, patient-reported outcome measure; PTA, physical therapy alone; SPT, surgery and physical therapy; VAS, visual analog scale.
Reference group: PTA.
Significant difference between groups (P < .05).
Table 3.
Adjusted Mean PROM and Pain Scores: Intention-to-Treat Analysis a
| SPT Group | PTA Group | P Value | |
|---|---|---|---|
| Preoperative | |||
| iHOT-33 | 40.4 (34.4-46.4) | 38.5 (32.1-44.9) | .664 |
| mHHS | 63.9 (59.6-68.3) | 62.8 (58.2-67.5) | .740 |
| NAHS | 64.7 (60.3-69.2) | 63.1 (58.3-67.9) | .626 |
| HOS-ADL | 73.7 (69.3-78.2) | 70.1 (65.4-74.9) | .282 |
| HOS-SS | 42.3 (34.8-49.7) | 42.9 (34.9-50.9) | .911 |
| VAS | 5.0 (4.3-5.8) | 5.4 (4.6-6.2) | .546 |
| 3 mo | |||
| iHOT-33 | 60.1 (54.0-66.2) | 42.3 (35.7-48.9) | <.001 b |
| mHHS | 77.0 (72.6-81.5) | 64.4 (59.6-69.3) | <.001 b |
| NAHS | 76.1 (71.5-80.6) | 65.6 (60.7-70.5) | .002 b |
| HOS-ADL | 80.6 (76.1-85.1) | 71.4 (66.5-76.3) | .007 b |
| HOS-SS | 44.0 (36.4-51.5) | 46.0 (37.8-54.2) | .720 |
| VAS | 2.8 (2.0-3.5) | 5.0 (4.2-5.9) | <.001 b |
| 6 mo | |||
| iHOT-33 | 69.7 (63.7-75.7) | 56.7 (50.2-63.3) | .004 b |
| mHHS | 80.8 (76.4-85.1) | 73.5 (68.7-78.3) | .029 b |
| NAHS | 82.7 (78.2-87.2) | 73.0 (68.1-77.9) | .004 b |
| HOS-ADL | 85.4 (80.9-89.9) | 78.1 (73.2-82.9) | .030 b |
| HOS-SS | 63.2 (55.7-70.7) | 50.4 (42.2-58.5) | .024 b |
| VAS | 2.4 (1.6-3.1) | 3.6 (2.7-4.4) | .038 b |
| 12 mo | |||
| iHOT-33 | 76.5 (70.4-82.5) | 64.7 (58.3-71.2) | .010 b |
| mHHS | 84.5 (80.0-88.9) | 78.5 (73.8-83.3) | .074 |
| NAHS | 84.3 (79.8-88.8) | 78.4 (73.6-83.2) | .081 |
| HOS-ADL | 87.2 (82.7-91.7) | 81.9 (77.1-86.8) | .118 |
| HOS-SS | 71.1 (63.5-78.7) | 59.7 (51.6-67.7) | .045 b |
| VAS | 2.3 (1.5-3.0) | 2.8 (2.0-3.6) | .401 |
| 24 mo | |||
| iHOT-33 | 75.5 (69.4-81.6) | 70.2 (63.6-76.9) | .255 |
| mHHS | 85.8 (81.3-90.2) | 81.0 (76.2-85.8) | .157 |
| NAHS | 85.4 (80.8-89.9) | 81.4 (76.5-86.4) | .253 |
| HOS-ADL | 89.8 (85.3-94.4) | 84.2 (79.3-89.1) | .101 |
| HOS-SS | 75.4 (67.8-83.1) | 70.0 (61.7-78.2) | .339 |
| VAS | 2.4 (1.6-3.2) | 2.6 (1.7-3.4) | .780 |
Data are presented as mean (95% CI). HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sports Subscale; iHOT-33, International Hip Outcome Tool-33; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; PROM, patient-reported outcome measure; PTA, physical therapy alone; SPT, surgery and physical therapy; VAS, visual analog scale.
Significant difference between groups (P < .05).
Modified As-Treated Analysis
In the modified as-treated analysis, SPT resulted in significantly higher overall iHOT-33 scores compared with PTA across the study period (mean difference, 15.0; 95% CI, 9.9-20.1; P < .001) and significantly higher means scores at the 3-month (P < .001), 6-month (P < .001), 12-month (P < .001), and 24-month (P = .001) follow-ups (Tables 4 and 5). SPT also resulted in significantly higher overall mHHS values compared with PTA across the study period (mean difference, 8.6; 95% CI, 5.1-12.1; P < .001) and significantly higher mean scores at the 3-month (P < .001), 6-month (P < .001), 12-month (P < .001), and 24-month (P = .010) follow-ups (Tables 4 and 5).
Table 4.
Weighted Differences in Mean PROM and Pain Scores Between SPT and PTA Groups: Modified As-Treated Analysis a
| PROM | Weighted Difference in Mean Score (95% CI) b | P Value |
|---|---|---|
| iHOT-33 | 15.0 (9.9 to 20.1) | <.001 c |
| mHHS | 8.6 (5.1 to 12.1) | <.001 c |
| NAHS | 8.7 (5.2 to 12.2) | <.001 c |
| HOS-ADL | 6.5 (3.1 to 9.8) | <.001 c |
| HOS-SS | 2.4 (–3.0 to 7.8) | .378 |
| VAS | −1.8 (–2.5 to −1.2) | <.001 c |
HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sports Subscale; iHOT-33, International Hip Outcome Tool-33; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; PROM, patient-reported outcome measure; PTA, physical therapy alone; SPT, surgery and physical therapy; VAS, visual analog scale.
Reference group: PTA.
Significant difference between groups (P < .05).
Table 5.
Adjusted Mean PROM and Pain Scores: Modified As-Treated Analysis a
| SPT Group | PTA Group | P Value | |
|---|---|---|---|
| Preoperative | |||
| iHOT-33 | 39.0 (34.5-43.6) | 37.9 (32.3-43.5) | .706 |
| mHHS | 63.3 (60.0-66.6) | 62.8 (58.7-67.0) | .836 |
| NAHS | 63.6 (60.2-67.0) | 62.9 (58.7-67.0) | .723 |
| HOS-ADL | 71.2 (67.8-74.6) | 70.6 (66.4-74.8) | .799 |
| HOS-SS | 40.7 (35.0-46.4) | 43.1 (36.2-50.0) | .491 |
| VAS | 5.2 (4.6-5.7) | 5.5 (4.8-6.2) | .444 |
| 3 mo | |||
| iHOT-33 | 63.4 (58.9-68.0) | 42.0 (36.0-47.9) | <.001 b |
| mHHS | 77.2 (73.9-80.6) | 64.8 (60.4-69.2) | <.001 b |
| NAHS | 77.1 (73.6-80.5) | 65.6 (61.2-69.9) | <.001 b |
| HOS-ADL | 81.0 (77.5-84.4) | 72.4 (68.0-76.8) | <.001 b |
| HOS-SS | 45.2 (39.4-50.9) | 46.5 (39.2-53.7) | .720 |
| VAS | 2.4 (1.8-2.9) | 5.2 (4.4-5.9) | <.001 b |
| 6 mo | |||
| iHOT-33 | 70.8 (66.2-75.4) | 44.0 (37.1-50.9) | <.001 b |
| mHHS | 81.4 (78.0-84.7) | 65.9 (60.8-71.1) | <.001 b |
| NAHS | 83.2 (79.7-86.6) | 65.6 (60.5-70.8) | <.001 b |
| HOS-ADL | 85.7 (82.3-89.2) | 71.6 (66.5-76.8) | <.001 b |
| HOS-SS | 63.1 (57.3-68.8) | 45.8 (37.5-54.2) | <.001 b |
| VAS | 2.3 (1.7-2.9) | 5.1 (4.2-6.0) | <.001 b |
| 12 mo | |||
| iHOT-33 | 76.8 (72.1-81.4) | 50.2 (41.4-59.1) | <.001 b |
| mHHS | 85.3 (81.8-88.7) | 69.8 (63.3-76.3) | <.001 b |
| NAHS | 85.5 (82.0-89.0) | 69.5 (63.1-75.9) | <.001 b |
| HOS-ADL | 87.9 (84.4-91.4) | 74.7 (68.3-81.2) | <.001 b |
| HOS-SS | 71.4 (65.5-77.2) | 55.0 (44.5-65.6) | .003 b |
| VAS | 2.1 (1.5-2.7) | 4.3 (3.1-5.4) | .001 b |
| 24 mo | |||
| iHOT-33 | 75.1 (70.5-79.8) | 56.5 (46.0-67.1) | .001 b |
| mHHS | 84.8 (81.4-88.2) | 74.5 (67.0-82.0) | .010 b |
| NAHS | 85.1 (81.6-88.6) | 70.9 (63.2-78.6) | <.001 b |
| HOS-ADL | 88.5 (85.0-92.0) | 75.8 (68.1-83.5) | .002 b |
| HOS-SS | 74.8 (69.0-80.6) | 58.0 (45.5-70.5) | .010 b |
| VAS | 2.3 (1.7-2.9) | 3.8 (2.4-5.1) | .039 b |
Data are presented as mean (95% CI). HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sports Subscale; iHOT-33, International Hip Outcome Tool-33; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; PROM, patient-reported outcome measure; PTA, physical therapy alone; SPT, surgery and physical therapy; VAS, visual analog scale.
Significant difference between groups (P < .05).
Treatment-Failure Analysis
A description of each cohort and mean follow-up times can be seen in Table 6. In the treatment-failure analysis, significant differences were seen in mean improvement for all outcome metrics assessed. SPT resulted in significantly greater magnitudes of improvement in iHOT-33 (SPT vs PTA, 33.5 vs 3.3; P < .001) and mHHS (SPT vs PTA, 20.8 vs 2.9; P < .001) compared with PTA. Surgery after crossover also resulted in significantly greater magnitudes of improvement in iHOT-33 (CO vs PTA, 37.6 vs 3.3; P < .001) and mHHS (CO vs PTA, 19.8 vs 2.9; P < .001) compared with PTA. However, on post hoc pairwise analysis, SPT and surgery after crossover did not differentially affect magnitudes of improvement in iHOT-33 (SPT vs CO; 33.5 vs 37.6; P = .741) or mHHS (SPT vs CO; 20.8 vs 19.8; P = .965) (Table 7).
Table 6.
Patients and Follow-up Times Included in Each Cohort for the Treatment-Failure Analysis a
| SPT Group | PTA Group | CO Group | ||||
|---|---|---|---|---|---|---|
| n | Follow-up, Mean (SD), mo | n | Follow-up, Mean (SD), mo | n | Follow-up, Mean (SD), mo | |
| 24-mo follow-up | 49 | 25.8 (5.1) | 13 | 28.2 (4.9) | 30 | 24.9 (5.9) |
| Follow-up at time of failure | ||||||
| THA | 3 | 15.5 (4.8) | 0 b | — | 2 | 14.5 (13.3) |
| Revision arthroscopy | 0 | — | 0 | — | 0 | — |
| Crossover | — | — | 32 | 5.10 (3.3) | — | — |
CO, crossover; PTA, physical therapy alone; SPT, surgery and physical therapy; THA, total hip arthroplasty. Dashes indicate not applicable.
One patient in the PTA group converted to THA 24.1 months after PT initiation, just after the 24-month follow-up.
Table 7.
Cohort Comparison of Improvements in PROM and Pain Scores and Rates of MOI Threshold Achievement at 24 Months or Failure: Treatment-Failure Analysis a
| PROM | SPT Group (n = 52) | PTA Group (n = 45) | CO Group (n = 32) | P Value | Post Hoc P Values | ||
|---|---|---|---|---|---|---|---|
| SPT vs PTA | SPT vs CO | PTA vs CO | |||||
| iHOT-33 | |||||||
| Improvement | 33.5 (26.2 to 40.8) | 3.3 (–2.7 to 9.4) | 37.6 (27.6 to 47.5) | <.001 b | <.001 b | .741 | <.001 b |
| Achieved MOI | 32 (61.5) d | 6 (13.3) e | 19 (59.4) d | <.001 b | |||
| mHHS | |||||||
| Improvement | 20.8 (16.3 to 25.2) | 2.9 (–1.4 to 7.3) | 19.8 (11.8 to 27.8) | <.001 b | <.001 b | .965 | <.001 b |
| Achieved MOI | 31 (59.6) d | 8 (17.8) e | 17 (53.1) | <.001 b | |||
| NAHS | |||||||
| Improvement | 19.4 (14.9 to 23.9) | 1 (–3.5 to 5.5) | 22 (14.2 to 29.8) | <.001 b | <.001 b | .782 | <.001 b |
| Achieved MOI | 32 (61.5) d | 6 (13.3) e | 20 (62.5) d | <.001 b | |||
| HOS-ADL | |||||||
| Improvement | 14.7 (10.2 to 19.2) | −0.6 (–5.2 to 3.9) | 18.4 (9.7 to 27.1) | <.001 b | <.001 b | .635 | <.001 b |
| Achieved MOI c | 0 (0) | — | — | — | |||
| HOS-SS | |||||||
| Improvement | 31.5 (23.7 to 39.2) | 0.6 (–5.6 to 6.9) | 34.3 (24 to 44.5) | <.001 b | <.001 b | .881 | <.001 b |
| Achieved MOI | 32 (61.5) d | 7 (15.6) e | 22 (68.8) d | <.001 b | |||
| VAS | |||||||
| Improvement | −2.5 (–3.4 to −1.6) | −0.3 (–1.3 to 0.7) | −3.3 (–4.6 to −2) | <.001 b | .004 b | .563 | <.001 b |
| Achieved MOI | 27 (51.9) | 9 (20) e | 21 (65.6) d | <.001 b | |||
Improvements in PROM and pain scores are reported as mean (95% CI), and proportions of patients achieving MOI are reported as the number of patients reaching the threshold value (%). Dashes indicate 0 patients achieved MOI.
Significant difference between groups (P < .05). CO, crossover; HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SS, Hip Outcome Score–Sports Subscale; iHOT-33, International Hip Outcome Tool-33; mHHS, modified Harris Hip Score; MOI, maximal outcome improvement; NAHS, Non-Arthritic Hip Score; PROM, patient-reported outcome measure; PTA, physical therapy alone; SPT, surgery and physical therapy; VAS, visual analog scale.
No validated MOI threshold value for HOS-ADL.
Adjusted residual, >1.96.
Adjusted residual, <–1.96.
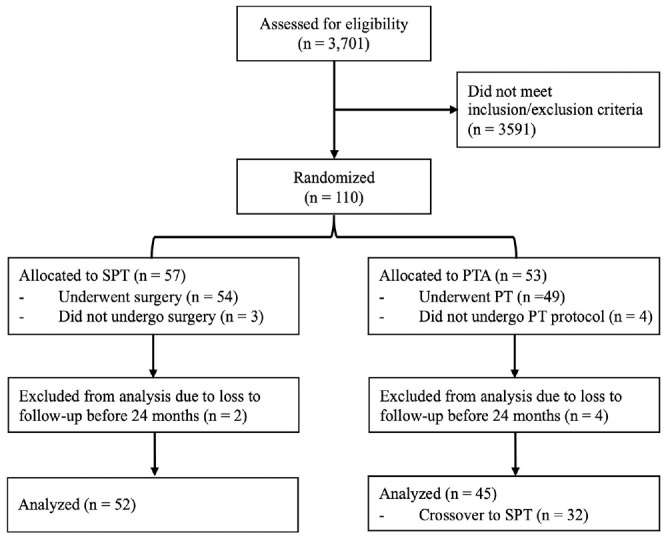
Patients in the SPT group were significantly more likely to achieve MOI than were those in the PTA group for all PROMs, including iHOT-33 (60.4% vs 13.3%; P < .001) and mHHS (58.5% vs 17.8%; P < .001) (Table 7). A logistic regression was performed to assess the effect of course of treatment (ie, SPT, PTA, or delayed surgery after rigorous PT [CO]), age, and Tönnis grade on the likelihood of achieving the MOI threshold value for iHOT-33 (Figure 2). 30 Compared with patients who underwent PTA, those who underwent SPT and surgery after crossover were 10.45 (95% CI, 3.60-30.35; P < .001) and 11.03 (95% CI, 3.44-35.44; P < .001) times more likely to achieve the MOI threshold for iHOT-33, respectively. Conversely, patients with Tönnis grade 1 and 2 changes were 0.36 (95% CI, 0.14-0.90; P = .029) and 0.22 (95% CI, 0.06-0.74; P = .014) times less likely to achieve the MOI threshold for iHOT-33, respectively. However, holding the course of treatment and Tönnis grade constant revealed that age alone was not a significant predictor of iHOT-33 MOI achievement (odds ratio, 1.00; 95% CI, 0.93-1.08; P = .937).
Figure 2.
Predictors of International Hip Outcome Tool-33 maximum outcome improvement achievement at 24 months or treatment failure. Data are presented as OR (95% CI). †Significant difference between groups (P < .05). ‡Reference group: PTA. §Reference group: Tönnis grade 0. CO, crossover; OR, odds ratio; SPT, surgery and physical therapy.
Survivorship
Rates of revision hip arthroscopy and conversion to THA were tracked for all patients through the maximum available follow-up. No significant difference was seen regarding rates of revision hip arthroscopy, as no patient in any cohort underwent a revision arthroscopy (P > .999). Similarly, no significant differences were observed in rates of THA (P > .999), as 3 (5.8%) patients from the SPT group converted at a mean of 15.51 months (SD, 4.8 months) after hip arthroscopy, 1 (2.2%) patient converted to THA directly from the PTA group at 24.1 months after PT initiation, and 2 (6.3%) patients from the CO group converted at a mean of 14.49 months (SD, 13.3 months) after hip arthroscopy (Table 6). Of patients who converted to THA, the mean age at the time of conversion was 55.5 years (SD, 8.1 years) and the mean Tönnis grade was 1.7 (SD, 1.2). Importantly, the rate of conversion to THA after PTA should be considered alongside the 71.1% rate of crossover.
Discussion
Although previous RCTs comparing hip arthroscopy versus nonoperative management for acetabular labral tears in the setting of FAI have reported superior functional outcomes after hip arthroscopy,19,23,31,44 these studies enrolled patients with a mean age of <40 years, leaving uncertainty regarding the efficacy of hip arthroscopy in older patients, a population traditionally associated with inferior outcomes.9,12,13,36,38,48 Furthermore, of previous RCTs, only one reported outcomes beyond a 12-month follow-up, but this study has been criticized for its failure to account for a high crossover rate.15,31 In the present RCT, the first to assess outcomes beyond 12 months in patients ≥40 years of age, we found that SPT led to significantly greater weighted differences in functional improvements in nearly all PROMs over the 24-month follow-up than did PTA in the ITT and modified as-treated analyses. Moreover, in the treatment-failure analysis, the SPT and CO groups both showed significantly greater improvements across all metrics compared with the PTA group. Importantly, post hoc analyses revealed no significant differences in improvement between the SPT and CO groups, suggesting equivalent improvements from surgery regardless of duration of antecedent PT. Overall, these results support the 12-month data from the present trial and suggest that hip arthroscopy is effective in improving functional outcomes in patients aged ≥40 years with limited radiographic osteoarthritis.
Using an ITT analysis, we found that our primary outcomes, iHOT-33 and mHHS, were significantly greater in the SPT group, with weighted differences in mean scores of 10.5 and 6.4 points across the study period, respectively, relative to the PTA group. Significant differences were preserved in the ITT analysis despite their well-documented limitations in RCTs comparing surgical and nonsurgical interventions with high rates of 1-way crossover (71% in the present study). Specifically, the postoperative improvements of patients who crossed over were attributed to the nonsurgical intervention, which likely diluted the contrast between groups.24,31,44 This is particularly pronounced at the 24-month follow-up, as most patients had crossed over (ie, received surgery) and were past the immediate postoperative period by this time point. Nevertheless, our sensitivity analyses, which aimed to account for our high rate of crossover, consistently revealed superior outcomes in favor of the SPT group. For example, the weighted difference in mean iHOT-33 scores between the SPT and PTA cohorts across the study period was 15.0 points in the modified as-treated analysis, relative to a 10.5-point difference in the ITT analysis.
These results contradicted our hypothesis that hip arthroscopy would not be more clinically effective than PT for the treatment of symptomatic labral tears in patients aged ≥40 years. Although older age at the time of hip arthroscopy has been associated with inferior functional outcomes, late regression in PROMs, and greater risk of conversion to THA,9,12,36,38,48 limited studies have explicitly compared the outcomes from surgery versus PT in patients >40 years of age. A subgroup analysis of a previous RCT by Griffin et al 19 found significantly greater improvements in iHOT-33 for those patients randomized to surgery versus PT (+10.9 points). Apart from this subanalysis, the only previous study to report on patients aged ≥40 years was the publication on the primary outcome at 12 months of the present RCT. In that study, the SPT group displayed weighted differences in mean iHOT-33 scores of 15.23 (P < .001) and 12.11 (P = .007) relative to the PTA group in the ITT and modified as-treated analyses, respectively, 33 both of which are comparable to the results demonstrated in the present study. Combined with our previous 12-month data and the previous subgroup analysis by Griffin et al, 19 our results suggest that hip arthroscopy generates superior improvements in functional outcomes compared with PTA in patients ≥40 years of age who have limited radiographic osteoarthritis.
Even though the high rate of crossover observed inhibits our ability to draw strong conclusions regarding treatment superiority based on the present data alone, a key finding of the present study was the equivalent postoperative improvements seen between the SPT and CO cohorts in the treatment-failure analysis. This analysis, which aimed to assess the maximum improvement achieved by each course of treatment within 24 months, revealed no significant differences in PROM improvement between the SPT and CO cohorts. However, both surgical cohorts improved significantly more across all PROMs relative to PTA. This was further corroborated by the logistic regression, which revealed that the SPT and CO cohorts were 11.03 and 10.45 times more likely to achieve iHOT-33 MOI threshold values, respectively, compared with the PTA cohort. Importantly, this finding suggests that delaying surgery for up to an additional 6 months in favor of nonoperative management will not negatively affect potential future improvements in functional outcomes for patients who do ultimately receive hip arthroscopy. Furthermore, this could allow some patients to avoid hip arthroscopy altogether if they feel that they continue to achieve adequate improvements in symptoms, thus potentially representing a more cost-effective treatment.19,31
Given that hip arthroscopy data are particularly limited in patients aged ≥40 years who have Tönnis grade 2 osteoarthritis, we performed a linear regression to assess whether age or Tönnis grade was a greater predictor of inferior outcomes after hip arthroscopy. Interestingly, age was not a significant predictor of iHOT-33 MOI achievement, while Tönnis grade was inversely proportional to one’s odds of iHOT-33 MOI achievement. Thus, our results suggest that age is more likely a surrogate of age-related degeneration and poor outcomes rather than an independent predictor of poor outcomes. This is consistent with previous literature showing that worse chondral damage portends inferior outcomes10,18,51 and may explain the heterogeneity in the current literature regarding the prognostic value of older age in the setting of hip arthroscopy. Specifically, a systematic review by Horner et al 22 found that of 3 studies comparing PROM improvement between patients ≥40 and <40 years of age, 1 found significantly less improvement among patients ≥40 years of age relative to the younger cohort, while the other 2 found no significant differences in improvement between groups. Further research investigating the prognostic value of age in the setting of hip arthroscopy should carefully consider preoperative chondral damage in their analyses.
Limitations
This study was subject to several limitations that should be noted. First, crossover rates in this study were high at 71%. For ethical reasons, all randomized patients had to meet surgical eligibility (failure of at least 3 months of nonoperative management), potentially increasing crossover rates because participants randomized to PTA were aware that they met surgical eligibility criteria. In addition, the high crossover rate of this study confounds the data and limits the reader’s ability to draw significant conclusions. Second, it is possible that some patients had a bias for either the SPT or PTA treatment arm. However, to minimize this bias, we imposed strict inclusion criteria to ensure that patients did not consciously prefer one treatment arm and were committed to completing their assigned treatment before enrollment. Third, despite the inferior hip arthroscopy outcomes that have been associated with a Tönnis grade of 2,10,18 the present study included patients with Tönnis grade 2 changes for pragmatic purposes given the high prevalence of these changes in patients aged ≥40 years with acetabular labral tears secondary to FAI. Fourth, as with previous similar RCTs, our 24-month primary endpoint limited our ability to report long-term outcomes of each study arm, particularly with respect to THA conversion rate. Fifth, our single-surgeon study design limited the sample size and generalizability of our findings. Finally, blinding was not possible in this study, which randomized a surgical versus a nonsurgical intervention.
Conclusion
In patients aged ≥40 years with limited osteoarthritis, arthroscopic acetabular labral repair with postoperative PT led to better outcomes than PTA at a 24-month follow-up. However, an additional course of preoperative PT did not compromise surgical outcomes and may allow some patients to avoid surgery. When surgery is indicated, age ≥40 years should not be considered an independent contraindication to arthroscopic acetabular labral repair.
Supplemental Material
Supplemental material, sj-pdf-1-ajs-10.1177_03635465241263595 for Hip Arthroscopy Versus Physical Therapy for the Treatment of Symptomatic Acetabular Labral Tears in Patients Older Than 40 Years: 24-Month Results From a Randomized Controlled Trial by Scott D. Martin, Michael C. Dean, Stephen M. Gillinov, Nathan J. Cherian, Christopher T. Eberlin, Michael P. Kucharik, Paul F. Abraham, Mark R. Nazal, William K. Conaway, Noah J. Quinlan, Kyle Alpaugh and Kaveh A. Torabian in The American Journal of Sports Medicine
Acknowledgments
The authors thank Shivam Upadhyaya, MD, Jada Gibbs, BA, and Nathan Varady, MD, MBA, for their assistance with data collection and analysis. The authors thank the Conine Family Fund for Joint Preservation for its continued support.
Footnotes
Submitted December 4, 2023; accepted May 15, 2024
Presented at the annual meeting of the AOSSM, Denver, Colorado, July 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: The Conine Family Fund for Joint Preservation provided research support. S.D.M. has received education payments from Kairos Surgical and honoraria from Allergan. N.J.Q. has received fees from Stryker and Medical Device Business Services, grants from Arthrex, and hospitality payments from Encore Medical. K.A. has received hospitality payments from Stryker Corp. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
ORCID iDs: Michael C. Dean  https://orcid.org/0000-0001-5996-6393
https://orcid.org/0000-0001-5996-6393
Stephen M. Gillinov  https://orcid.org/0000-0001-5630-4079
https://orcid.org/0000-0001-5630-4079
Nathan J. Cherian  https://orcid.org/0000-0002-1524-3908
https://orcid.org/0000-0002-1524-3908
Paul F. Abraham  https://orcid.org/0000-0003-0737-362X
https://orcid.org/0000-0003-0737-362X
References
- 1. Abdu WA, Sacks OA, Tosteson ANA, et al. Long-term results of surgery compared with nonoperative treatment for lumbar degenerative spondylolisthesis in the Spine Patient Outcomes Research Trial (SPORT). Spine. 2018;43(23):1619-1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alpaugh K, Shin SR, Martin SD. Intra-articular fluid distension for initial portal placement during hip arthroscopy: the “femoral head drop” technique. Arthrosc Tech. 2015;4(1):e23-e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012-1018. [DOI] [PubMed] [Google Scholar]
- 4. Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24(10):1135-1145. [DOI] [PubMed] [Google Scholar]
- 5. Berglund DD, Damodar D, Vakharia RM, et al. Predicting outstanding results after anatomic total shoulder arthroplasty using percentage of maximal outcome improvement. J Shoulder Elbow Surg. 2019;28(2):349-356. [DOI] [PubMed] [Google Scholar]
- 6. Bodendorfer BM, Clapp IM, DeFroda SF, et al. The natural course of recovery after hip arthroscopy for femoroacetabular impingement according to the International Hip Outcome Tool-12 and Hip Outcome Score Sports Subscale. Am J Sports Med. 2021;49(12):3250-3260. [DOI] [PubMed] [Google Scholar]
- 7. Brown VA. An introduction to linear mixed-effects modeling in R. Adv Methods Pract Psychol Sci. 2021;4(1):2515245920960351. [Google Scholar]
- 8. Bsat S, Frei H, Beaulé PE. The acetabular labrum: a review of its function. Bone Joint J. 2016;98(6):730-735. [DOI] [PubMed] [Google Scholar]
- 9. Büchler L, Grob V, Anwander H, Lerch TD, Haefeli PC. Good outcome scores and low conversion rate to THA 10 years after hip arthroscopy for the treatment of femoroacetabular impingement. Clin Orthop Relat Res. 2021;479(10):2256-2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chandrasekaran S, Darwish N, Gui C, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of hip arthroscopy in patients with Tönnis grade-2 osteoarthritis at a mean 2-year follow-up: evaluation using a matched-pair analysis with Tönnis grade-0 and grade-1 cohorts. J Bone Joint Surg Am. 2016;98(12):973-982. [DOI] [PubMed] [Google Scholar]
- 11. Conaway WK, Martin SD. Puncture capsulotomy during hip arthroscopy for femoroacetabular impingement: preserving anatomy and biomechanics. Arthrosc Tech. 2017;6(6):e2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Domb BG, Martin TJ, Gui C, Chandrasekaran S, Suarez-Ahedo C, Lodhia P. Predictors of clinical outcomes after hip arthroscopy: a prospective analysis of 1038 patients with 2-year follow-up. Am J Sports Med. 2018;46(6):1324-1330. [DOI] [PubMed] [Google Scholar]
- 13. Dwyer MK, Tumpowsky C, Boone A, Lee J, McCarthy JC. What is the association between articular cartilage damage and subsequent THA 20 years after hip arthroscopy for labral tears? Clin Orthop Relat Res. 2019;477(5):1211-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eberlin CT, Kucharik MP, Abraham PF, et al. Puncture capsulotomy technique for hip arthroscopy: midterm functional outcomes. Orthop J Sports Med. 2023;11(1):23259671221144056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Faucett SC, Nepple JJ, Andrade T, et al. Randomized controlled trial of hip arthroscopy surgery vs physical therapy: letter to the editor. Am J Sports Med. 2018;46(8):NP35-NP38. [DOI] [PubMed] [Google Scholar]
- 16. Filan D, Mullins K, Carton P. Hip arthroscopy in the presence of advanced osteoarthritis results in 57% survivorship, with 78% survivor satisfaction, at 10 years: a matched-control study. Arthroscopy. 2023;39(2):256-268. [DOI] [PubMed] [Google Scholar]
- 17. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. [DOI] [PubMed] [Google Scholar]
- 18. Giordano BD, Kuhns BD, Perets I, Yuen L, Domb BG. Acetabular morphologic characteristics predict early conversion to arthroplasty after isolated hip arthroscopy for femoroacetabular impingement. Am J Sports Med. 2020;48(1):188-196. [DOI] [PubMed] [Google Scholar]
- 19. Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet Lond Engl. 2018;391(10136):2225-2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoch A, Schenk P, Jentzsch T, Rahm S, Zingg PO. FAI morphology increases the risk for osteoarthritis in young people with a minimum follow-up of 25 years. Arch Orthop Trauma Surg. 2021;141(7):1175-1181. [DOI] [PubMed] [Google Scholar]
- 21. Hoit G, Whelan DB, Dwyer T, Ajrawat P, Chahal J. Physiotherapy as an initial treatment option for femoroacetabular impingement: a systematic review of the literature and meta-analysis of 5 randomized controlled trials. Am J Sports Med. 2020;48(8):2042-2050. [DOI] [PubMed] [Google Scholar]
- 22. Horner NS, Ekhtiari S, Simunovic N, Safran MR, Philippon MJ, Ayeni OR. Hip arthroscopy in patients age 40 or older: a systematic review. Arthroscopy. 2017;33(2):464-475.e3. [DOI] [PubMed] [Google Scholar]
- 23. Hunter DJ, Eyles J, Murphy NJ, et al. Multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapist-led care for femoroacetabular impingement (FAI) syndrome on hip cartilage metabolism: the Australian FASHIoN trial. BMC Musculoskelet Disord. 2021;22(1):697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kucharik MP, Abraham PF, Nazal MR, et al. Treatment of full-thickness acetabular chondral flaps during hip arthroscopy: bone marrow aspirate concentrate versus microfracture. Orthop J Sports Med. 2021;9(12):23259671211059170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kvien TK, Heiberg T, Hagen KB. Minimal clinically important improvement/difference (MCII/MCID) and patient acceptable symptom state (PASS): what do these concepts mean? Ann Rheum Dis. 2007;66(suppl 3):iii40-iii41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lieberman JR. Hip arthroscopy for femoroacetabular impingement patients older than 50 years—proceed with caution. Arthroscopy. 2019;35(9):2759-2760. [DOI] [PubMed] [Google Scholar]
- 28. Lin LJ, Akpinar B, Bloom DA, Youm T. Age and outcomes in hip arthroscopy for femoroacetabular impingement: a comparison across 3 age groups. Am J Sports Med. 2021;49(1):82-89. [DOI] [PubMed] [Google Scholar]
- 29. Lubowitz JH, D’Agostino RB, Provencher MT, Rossi MJ, Brand JC. Can we trust knee meniscus studies? One-way crossover confounds intent-to-treat statistical methods. Arthroscopy. 2016;32(11):2187-2190. [DOI] [PubMed] [Google Scholar]
- 30. Maldonado DR, Kyin C, Shapira J, et al. Defining the maximum outcome improvement of the modified Harris Hip Score, the Nonarthritic Hip Score, the visual analog scale for pain, and the International Hip Outcome Tool-12 in the arthroscopic management for femoroacetabular impingement syndrome and labral tear. Arthroscopy. 2021;37(5):1477-1485. [DOI] [PubMed] [Google Scholar]
- 31. Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. Am J Sports Med. 2018;46(6):1306-1314. [DOI] [PubMed] [Google Scholar]
- 32. Martin SD. Arthroscopic labral repair versus physical therapy for tears of the acetabular labrum. ClinicalTrials.gov identifier: NCT03909178. 2023.
- 33. Martin SD, Abraham PF, Varady NH, et al. Hip arthroscopy versus physical therapy for the treatment of symptomatic acetabular labral tears in patients older than 40 years: a randomized controlled trial. Am J Sports Med. 2021;49(5):1199-1208. [DOI] [PubMed] [Google Scholar]
- 34. Martin SD, Eberlin CT, Kucharik MP, Cherian NJ. Harvest and application of bone marrow aspirate concentrate to address acetabular chondral damage during hip arthroscopy. JBJS Essent Surg Tech. 2023;13(2):e22.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Martin SD, Kucharik MP, Abraham PF, Nazal MR, Meek WM, Varady NH. Functional outcomes of arthroscopic acetabular labral repair with and without bone marrow aspirate concentrate. J Bone Joint Surg Am. 2022;104(1):4-14. [DOI] [PubMed] [Google Scholar]
- 36. McCarthy JC, Jarrett BT, Ojeifo O, Lee JA, Bragdon CR. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res. 2011;469(2):362-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McCormick F, Alpaugh K, Nwachukwu BU, Xu S, Martin SD. Effect of radiofrequency use on hip arthroscopy irrigation fluid temperature. Arthroscopy. 2013;29(2):336-342. [DOI] [PubMed] [Google Scholar]
- 38. McCormick F, Nwachukwu BU, Alpaugh K, Martin SD. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy. 2012;28(10):1359-1364. [DOI] [PubMed] [Google Scholar]
- 39. Mok TN, He QY, Teng Q, et al. Arthroscopic hip surgery versus conservative therapy on femoroacetabular impingement syndrome: a meta-analysis of RCTs. Orthop Surg. 2021;13(6):1755-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Naessig S, Kucharik M, Meek W, Eberlin C, Martin S. Prehabilitation and rehabilitation program for patients undergoing arthroscopic acetabular labral repair: a comprehensive 5-phase patient-guided program. Orthop J Sports Med. 2022;10(2):232596712110710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nwachukwu BU, Alpaugh K, McCormick F, Martin SD. All-arthroscopic reconstruction of the acetabular labrum by capsular augmentation. Arthrosc Tech. 2015;4(2):e127-e131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nwachukwu BU, McCormick F, Martin SD. Arthroscopic technique for chondrolabral capsular preservation during labral repair and acetabular osteoplasty. Arthrosc Tech. 2013;2(3):e213-e216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Owens JS, Jimenez AE, Lee MS, George T, Maldonado DR, Domb BG. Determining clinically meaningful thresholds for the hip outcome score sport-specific subscale in athletes undergoing hip arthroscopy for femoroacetabular impingement syndrome. Am J Sports Med. 2022;50(11):3009-3018. [DOI] [PubMed] [Google Scholar]
- 44. Palmer AJR, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ. 2019;364:l185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Palmer AJR, Thomas GER, Pollard TCB, et al. The feasibility of performing a randomised controlled trial for femoroacetabular impingement surgery. Bone Jt Res. 2013;2(2):33-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Philippon MJ, Schroder E, Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59-65. [DOI] [PubMed] [Google Scholar]
- 47. Rhee C, Le Francois T, Byrd JWT, Glazebrook M, Wong I. Radiographic diagnosis of pincer-type femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2017;5(5):2325967117708307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Saadat E, Martin SD, Thornhill TS, Brownlee SA, Losina E, Katz JN. Factors associated with the failure of surgical treatment for femoroacetabular impingement: review of the literature. Am J Sports Med. 2014;42(6):1487-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Savage TN, Saxby DJ, Lloyd DG, et al. Hip contact force magnitude and regional loading patterns are altered in those with femoroacetabular impingement syndrome. Med Sci Sports Exerc. 2022;54(11):1831-1841. [DOI] [PubMed] [Google Scholar]
- 50. Shankar DS, Wingo T, Akpinar B, Rynecki ND, Youm T. Patient-reported outcomes and survivorship are not different for primary hip arthroscopy patients of age 50 years and older compared with a 20- to 35-year-old matched cohort at minimum 5-year follow-up. Arthroscopy. 2023;39(7):1651-1659. [DOI] [PubMed] [Google Scholar]
- 51. Sivasundaram L, Rice MW, Horner NS, Alter TD, Ephron CG, Nho SJ. Hip arthroscopy for the treatment of femoroacetabular impingement syndrome in hips with mild osteoarthritis (Tönnis grade 1): a matched comparative cohort analysis at minimum 5-year follow-up. Am J Sports Med. 2022;50(10):2598-2605. [DOI] [PubMed] [Google Scholar]
- 52. Skelley NW, Conaway WK, Martin SD. “In-round” labral repair after acetabular recession using intermittent traction. Arthrosc Tech. 2017;6(5):e1807-e1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Syed HM, Martin SD. Arthroscopic acetabular recession with chondrolabral preservation. Am J Orthop. 2013;42(4):181-184. [PubMed] [Google Scholar]
- 54. Yacovelli S, Sutton R, Vahedi H, Sherman M, Parvizi J. High risk of conversion to THA after femoroacetabular osteoplasty for femoroacetabular impingement in patients older than 40 years. Clin Orthop Relat Res. 2021;479(5):1112-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ajs-10.1177_03635465241263595 for Hip Arthroscopy Versus Physical Therapy for the Treatment of Symptomatic Acetabular Labral Tears in Patients Older Than 40 Years: 24-Month Results From a Randomized Controlled Trial by Scott D. Martin, Michael C. Dean, Stephen M. Gillinov, Nathan J. Cherian, Christopher T. Eberlin, Michael P. Kucharik, Paul F. Abraham, Mark R. Nazal, William K. Conaway, Noah J. Quinlan, Kyle Alpaugh and Kaveh A. Torabian in The American Journal of Sports Medicine