Abstract
Background
The origin of Narrative Medicine dates back to more than 20 years ago at an international level. Narrative Medicine is not an alternative to evidence-based medicine, however these two approaches are integrated. Narrative Medicine is a methodology based on specific communication skills where storytelling is a fundamental tool to acquire, understand and integrate several points of view related to persons involving in the disease and in the healthcare process. Narrative Medicine, henceforth NM, represents a union between disease and illness between the doctor’s clinical knowledge and the patient’s experience. According to Byron Good, “we cannot have direct access to the experience of others’ illness, not even through in-depth investigations: one of the ways in which we can learn more from the experience of others is to listen to the stories of what has happened to other people.” Several studies have been published on NM; however, to the best of our knowledge, no scoping review of the literature has been performed.
Objective
This paper aims to map and synthetize studies on NM according to theory, clinical practice and education/training.
Method
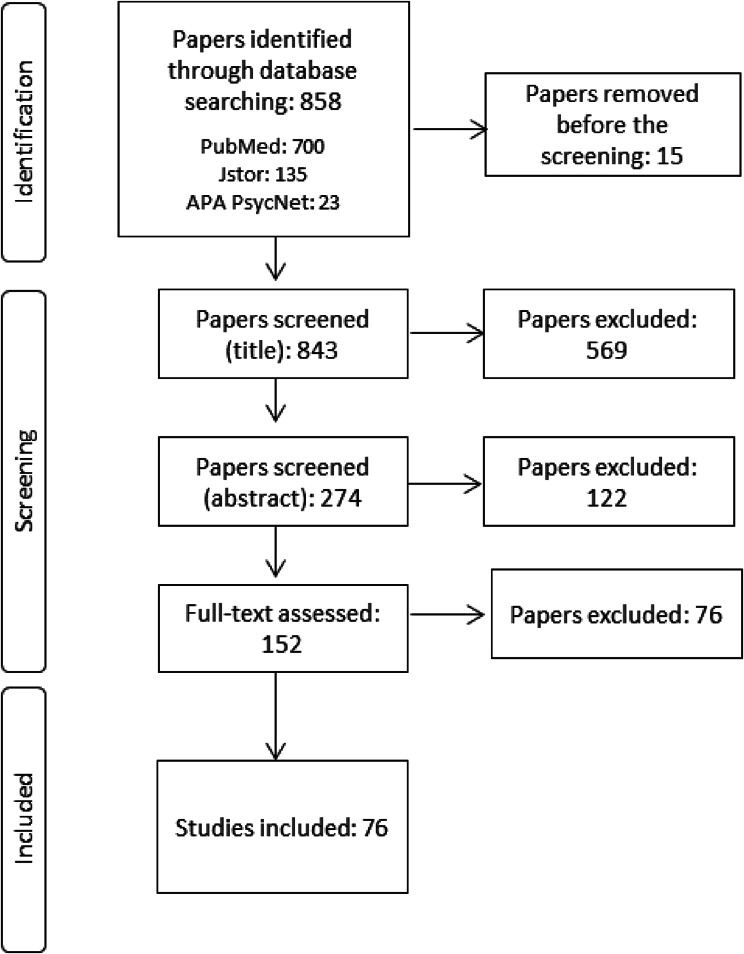
The scoping review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) checklist. A search was conducted in PubMed, APA PsycNet and Jstor. Two authors independently assessed the eligibility and methodological quality of the studies and extracted the data. This review refers to the period from 1998 to 2022.
Results
A total of 843 abstracts were identified of which 274 papers were selected based on the title/abstract. A total of 152 papers in full text were evaluated and 76 were included in the review. Papers were classified according to three issues:
✘ Nineteen studies focused on the definition and concept of NM (Theoretical).
✘ Thirty-eight papers focused on the collection of stories, projects and case reports (Clinical practice).
✘ Nineteen papers focused on the implementation of the Narrative Medicine approach in the education and training of medical doctors (Education and training).
Conclusions
This scoping review presents an overview of the state of the art of the Narrative Medicine. It collect studies performed mainly in Italy and in the United States as these are the countries developing the Narrative Medicine approach in three identified areas, theoretical, clinical practice and education and training. This scoping review will help to promote the power of Narrative Medicine in all three areas supporting the development of methods to evaluate and to measure the Narrative Medicine approach using key performance indicators.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11530-x.
Keywords: Narrative Medicine, Illness, Patient, Healthcare professional, Clinical practice, Education, Training, Scoping review, Personalized medicine
Introduction
Rationale
The role and involvement of patients in healthcare have changed, as has their relationship with healthcare professionals. The patient is no longer a passive subject but part of the healthcare process. Over the years, many approaches to patients’ involvement in healthcare have been developed in the literature, with significant differences in terms of concept and significance.
NM represents a focus on the patient’s needs and the empowerment of their active participation in the healthcare process.
Narrative Medicine enables patients to share their stories with healthcare professionals so that the latter can gain the necessary skills to recognize, interpret and relate to patients [1]. Stories of illness have an important impact on patients and their caregivers, healthcare professionals and organisational systems [2].
Trisha Greenhalgh, an academic in primary healthcare who trained as a General Practitioner, and Brian Hurwitz, an Emeritus Professor of Medicine and The Arts at King’s College (London) [3, 4], affirmed that the core clinical skills in terms of listening, questioning, outlining, collecting, explaining and interpreting can provide a way of navigating among the very different worlds of patients and health professionals. These tasks need to be performed well because they can affect disease outcomes from the patient’s perspective and the scientific aspects of diagnosis and treatment.
In 2013, Rita Charon, a general internist and professor at Columbia University (New York), and Brian Hurwitz promoted “a narrative future for healthcare”, the first global conference on Narrative Based Medicine (NBM). The global conference took place in London in June 2013, where experts in humanities, social sciences and professionals interested in shaping a narrative future for healthcare discussed several topics, such as increasing the visibility of narrative-based concepts and methods; developing strategies that can influence traditional clinical institutions; spreading appreciation for the role of creativity in caring for the sick; articulating the risks of narrative practices in health care; providing a space for Narrative Medicine in the context of other fields, including personalized medicine; and sharing goals for training, research, and clinical care. The conference was the first important opportunity to share different points of view and perspectives at the global level involving several stakeholders with different backgrounds [5].
In the early 2000s, the first Italian experience of Narrative Medicine occurred in Florence with NaMe, a project endorsed by the Local Health Authority aimed at diffusing the culture of patient-centered medicine and integrating strategies to improve doctor‒patient communication in clinical practice [6]. This project was inspired by the articles of Hurwitz and Greenhalgh [3, 4]. In addition, significant input was derived from Arthur Kleinman [7] and Byron Good [8], psychiatrists and anthropologists who studied medicine as a cultural system, as a set of symbolic meanings involving the story of the sick person. Health and illness represent the subjective experience of the person.
Kleinmann [7] defines three dimensions to explain the illness using three different significances:
✘ Disease: “only as an alteration in biological structure or functioning”.
✘ Illness: the subjective experience of suffering and discomfort.
✘ Sickness: the social representation.
Narrative Medicine can be used in several areas such as prevention, diagnosis, treatment, and rehabilitation; adherence to treatment; organization of the care team; awareness of the professional role and the emotional world by health and social workers; prevention of the burnout of professionals and caregivers; promotion and implementation of Patient Care Pathways (PCPs); and prevention of legal disputes and defensive medicine.
The Italian guidelines established by the National Institute of Health in 2015 [9] represent a fundamental step in the process of diffusion and implementation of Narrative Medicine in Italy and currently represents the only document. The guidelines define Narrative Medicine as an intervention methodology based on specific communication skills. Storytelling is a fundamental instrument for acquiring, understanding and integrating the different perspectives of those involved in the disease and in the healthcare process. Storytelling represents a moment of contact between a healthcare professional and the patient’s world. The story told involves people, those who narrate and those who listen. Telling stories is a way of transferring knowledge and experience, connecting, reflecting and feeling emotions.
In the last few years, several studies have been carried out with different objectives and perspectives, but no literature review on Medicine Narrative has been performed. We founded the study of Rui et al. [10] performing a bibliometric analysis of the literature on medical narratives published from 2011 to 2021 showing that the field of narrative medicine is dominated by a few countries. Respect to 736 studies included in the review, 48% (369) are performed in US and 98 papers in Italy.
Objective
The objective of scoping review was to map and synthetize studies on NM according to theory, clinical practice and education/training, three settings where NM was developed.
The research questions formulated: (1) What is Narrative Medicine?; (2) How is Narrative Medicine implemented in clinical practice?; (3) What is the role of Narrative Medicine in education and training for medical doctors?
Methods
The study protocol follows the PRISMA-ScR checklist (PRISMA extension for Scoping Reviews) but it is not registered (Additional file 1).
We included peer-reviewed papers published from 1998 to December 2022 written in Italian or in English. We excluded papers written in other languages. We included articles according to one of these issues: studies on theory of Narrative Medicine, on clinical practice or education/training of Narrative Medicine. We excluded books, case reports, reviews. To identify potentially relevant studies, the following databases were searched from 1998 to December 2022: PubMed, APA PsycNet and Jstor. The search strategy can be founded in Additional file 2. A data charting form was developed by two reviewers to define which variables can be extracted. The reviewers independently charted the data and discussed the results. We grouped the studies by type of application related to the Narrative Medicine and summarized objective, methods and reflections/conclusions. The scoping review maps the evidence on Narrative Medicine according one of the three fields of diffusion and implementation (Fig. 1). Furthermore, the studies classified in “theoretical field “are grouped in subcategories to explain in best way the concepts and permit a clearer and more streamlined reading.
Fig. 1.
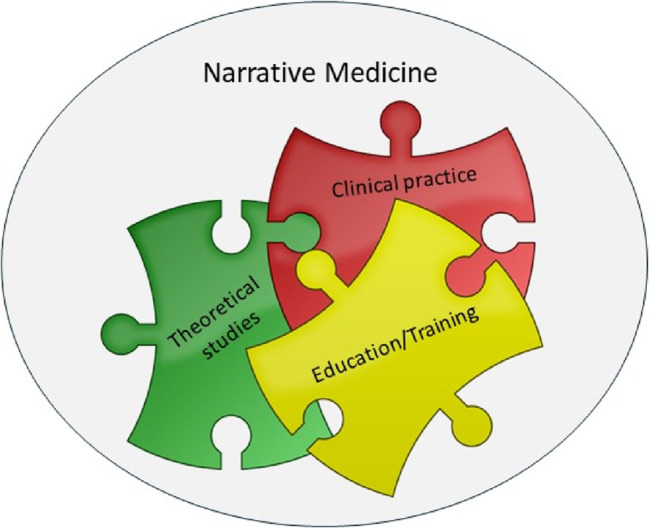
Categories of Narrative Medicine
Results
Review process
After removing duplicates, 843 abstracts from PubMed, Jstor and APA PsycNet were screened. A total of 274 papers were screened based on the abstracts, of which 122 were excluded. A total of 152 full texts were evaluated, and 76 were included in the review (Fig. 2).
Fig. 2.
PRISMA Flow-chart
The studies included were classified into the three fields where the Narrative Medicine is implemented:
✘ Theoretical studies: 19.
✘ Clinical Practice: 38.
✘ Education and training: 19.
The scoping review did not present the results of papers included but the main objectives and the methods used as the aim of the scoping review was to map the studies performed in terms of theory, clinical practice and education/training. We have tried to organize the studies published so far, making it increasingly clear how Narrative Medicine has developed.
Theoretical studies
This section presents the 19 selected theoretical studies grouped into subcategories (Additional file 3).
Narrative Medicine: advantages
In this section, we present seven papers that highlight the benefits of narrative medicine.
Of the seven papers considered, four were performed by Rita Charon emphasizing the value of Narrative Medicine in four different contexts. In the first [11], the study by Goupy et al. evaluated a Narrative Medicine elective course at the Paris-Descartes School of Medicine. In the second [12], Charon rewrote a patient’s family illness to demonstrate how medicine that respects the narrative dimension of illness and care can improve the care of individual patients, their colleagues and effective medical practice. The third paper [13] describes a visit to the Rothko Room at the Tate Modern in London as a pretext to emphasize how for narrative medicine, creativity is at the heart of health care and that the care of the sick is a work of art.
In the fourth [14], Charon provides the elements of narrative theory through a careful reading of the form and content of an excerpt from a medical record. This is part of an audio-recorded interview with a medical student and a reflection on a short section of a modernist novel to show how to determine the significance of patients’ situations.
According to Abettan [15], Narrative Medicine can play a key role in the reform of current medical practice, although to date, there has been little focus on how and why it can deliver results and be cost-effective.
Cenci [16] underlines that the existential objective of the patient is fundamental to know the person’s life project and how they would like to live their future years.
Zaharias [17], whose main sources are Charon and Launer, has published three articles on NM as a valid approach that, if practiced more widely by general practitioners, could significantly benefit both patients and doctors. If the patient’s condition is central, the NM shifts the doctor’s focus from the need to solve the problem to the need to understand. Consequently, the patient‒physician relationship is strengthened, and patients’ needs and concerns are addressed more effectively and with better results.
Narrative Medicine: the role of digital technologies
This section includes 3 papers on the role of digital technologies in Narrative Medicine. Digital narrative medicine is diffusing in care relationship as presents an opportunity for the patient and the clinician. The patient has more time to reflect on his/her needs and communicate in best way with the healthcare professionals. The clinician can access to more information as quantitative and qualitative information and data provided by the patient. These information represent an instrument for the clinician to personalize the care and respond to patient’s unmet needs.
The use of digital technologies, particularly the digital health storymap tool described by Cenci [16], for obtaining a multidisciplinary understanding of the patient’s medical history facilitates communication between the patient and caregiver. According to Charon [18], the relentless specialization and technologization of medicine damages the therapeutic importance of recognizing the context of patients’ lives and witnessing their suffering.
Rosti [19] affirms that e-health technologies will build new bridges and permit professionals to have more time to use narrative techniques with patients.
The increased use of digital technologies could reduce the opportunity for narrative contact but provide a starting point for discussion through the use of electronically transmitted patient pain diaries.
Narrative Medicine: integration with evidence-based medicine
Greenhalgh’s [20] and Rosti’s [19] studies address one of the most significant issues, the integration of Narrative Medicine with Evidence Based Medicine. Narrative Medicine is not an alternative to Evidence Based Medicine, they coexist and can complement each other in clinical practice.
Greenhalgh’s work [20] clearly shows how NM and EBM can be integrated. EBM requires an interpretative paradigm in which the patient experiences the disease in a unique and contextual way and the clinician can draw on all aspects of the evidence and thus arrive at an integrated clinical judgement.
Rosti [19] believes that even “evidence-based” physicians sustain the importance of competence and clinical judgement. Clinicians also need to rely on patients’ narratives to integrate more objective clinical results. Clinical methods are not without their limitations, which Narrative Medicine can help to overcome. Lederman [21] enphatises the importance of social sciences to analyze the stories and to improve the care.
Narrative-based Medicine: insidious
Three papers in this section focus on the possible risks of the Narrative Medicine approach. It is needing a more awareness on role of Narrative Medicine as a robust methodology.
The study by Kalitzus [22] shows how a narrative approach in medicine will be successful only if it has a positive effect on daily clinical practice instead of merely increasing existing problems.
Complex narratives on diseases published in biographies or collected by social scientists are useful only for training and research purposes. NM requires time and effort and cannot be considered the only important issue in medicine. According to Abettan [15], Narrative Medicine can make the treatment more personalised for each patient, but it is not the only way.
Zaharias [17] affirms that Narrative Medicine is often described simplistically as listening to the patient’s story, whereas it is much more common and requires special communication skills. Perhaps for these reasons, and despite its advantages, NM is not as widely practiced as it could be. Narrative skills are an integral part of practice and learning them takes time. As the author also states, “the healing power of storytelling is repeatedly attested to while evidence of effectiveness is scarce”. Lanphier [23] underlines the need to explain the term "narrative medicine" to avoid misunderstandings and to analyze the use of narrative as a tool.
Narrative Medicine: training
Liao et al. [24] presented a study aimed at helping students improve their relationships with patients by listening to them. These results, similar to those described by Charon [25], suggest that Narrative Medicine is worth recommending in academic training. The essay by O’Mahony [26] aims to provoke a debate on how and what the medical humanities should teach. Narratology and narrative medicine are linked to empathy.
Narrative Medicine: clinician-patient communication
Papers included within this category focus on the relationship between the clinician and patient, which is important in the healthcare context.
American healthcare institutions recognize the use of the Narrative Medicine approach to develop quality patient care. As a gastroenterologist at a health centre in Minnesota (US), Rian [27] concluded that the practice of Narrative Medicine should not be kept on the fringes of medicine as a hobby or ancillary treatment for the benefit of the patients but should be considered key to the healthcare process. Improving doctor‒patient communication merits more attention.
According to Rosti [19], NM can be seen as a tool to promote better communication. Although time constraints are often mentioned as an obstacle, the time needed to listen to patients is not excessive, and all healthcare professionals should consider giving patients more freedom from time constraints during consultations by encouraging them to talk about their experiences. The use of NM may also be associated with better diagnosis and treatment of pain.
Zaharias [28] underlines that communication skills are crucial. General practitioners can further develop the strong communication skills they already possess by practicing NM through neutrality, circular questions and hypotheses, and reflective skills.
Narrative Medicine: bioethics in qualitative research
The use of qualitative research in bioethics and narrative approaches to conducting and analysing qualitative interviews are becoming increasingly widespread. As Roest [29] states, this approach enables more “diagnostic thinking”. It is about promoting listening skills and the careful reading of people and healthcare practices, as well as quality criteria for the ethical evaluation of research and training.
Clinical practice
In this classification, we included case studies performed in clinical care. We focused on methods used to guide the patients’ stories or narratives written by healthcare professionals. We analysed how Narrative Medicine has been implemented in clinical healthcare practice.
The studies included (38) were performed in the following countries: Italy (28), USA (4), Australia (1), Canada (1), China (1), Colombia (1), Norway (1), and several European countries (1) (Table 1). The main methods used were semi-structured interviews that guided the patient’s and physician’s narration [30–33], narrative diaries written by patients [34], and paper parallel charts (an instrument to integrate the patients’ stories in clinical practice) written by clinicians [34–36].
Table 1.
Clinical practice: studies included
| Author, Year | Title | Country | Objective | Method | Reflections |
|---|---|---|---|---|---|
| Banfi et al., 2018 [34] | Narrative medicine to improve the management and quality of life of patients with COPD: the first experience applying parallel chart in Italy | Italy | To assess the doctor‒patient relationship and its impact on patient life. | Clinicians: parallel charts were collected through an online survey platform. | Clinicians affirm that the parallel charts were useful for inducing the clinicians to reflect on their relationship with patients. Clinicians believed that listening and understanding the patients’ needs can impact on their adherence and quality of life. |
| Breccia et al., 2016 [30] | Personal history and quality of life in chronic myeloid leukemia patients: a cross-sectional study using narrative medicine and quantitative analysis | Italy | To support clinicians to better understand patients’ needs and to empower communication at different time points of treatment. |
-Quantitative Questionnaire -Narrative diary |
Narrative Medicine in add on to quantitative analysis can help to better management of patients, understanding their needs and improving communication. |
| Cappuccio et al., 2017 [31] | Living with Chronic Spontaneous Urticaria in Italy: a narrative medicine project to improve the pathway of patient care | Italy | To highlight how to improve the care of patients with Chronic Spontaneous Urticaria (CSU). |
Questionnaire: -Patients -Physicians |
Narrative Medicine is useful to underline the critical aspects related to the patient’s pathway in relation to organizational issues. |
| Cappuccio et al., 2018 [35] | Narrative medicine educational project to improve the care of patients with chronic obstructive pulmonary disease | Italy | To teach pulmonologists the basics of narrative medicine in order to listen carefully to patients. |
-Webinar on narrative medicine - At least 5 parallel charts |
The project shows the positive effects of the narrative medicine approach from the clinician’s perspective, highlighting the listening and understanding of patients’ needs. To achieve good health outcomes, it is very important to have a good relationship with doctors. |
| Cappuccio et al., 2019 [36] | Use of narrative medicine to identify key factors for effective doctor-patient relationship in severe asthma | Italy | To analyze the relationship between specialists and patients with severe asthma. |
-Educational course - Parallel charts |
The project showed that the narrative medicine approach can be effective to support clinicians in the relationship with patients and caregivers. |
| Caputo, 2014 [37] | Exploring quality of life of Italian patients with rare diseases: a computer-aided content analysis of illness stories | Italy | To identify the themes related to the illness experience and quality of life of patients affected by rare diseases. | Illness stories written by adults with different rare diseases | Illness stories highlighted the importance of the relationships of patients with rare diseases with healthcare services and the need for a holistic approach. |
| Ceccarelli et al., 2021 [32] | Systemic Lupus Erythematosus before and after COVID-19 Lockdown: how the perception of disease changes through the lenses of Narrative Medicine | Italy | To describe the experience and perspectives of adults living with SLE during COVID. | Collection of Illness stories | Qualitative research helps the patients to understand the experiences and beliefs related to the disease. The narrative approach also enables to highlight the perspectives of patients in relation to the pandemic, by underlining their concerns about the future. |
| Cenci and Mecarelli, 2020 [33] | Digital narrative medicine for the personalization of epilepsy care pathways | Italy | To assess the usefulness and the feasibility of integrating narrative medicine methodologies into routine clinical practice through a digital platform. |
Questionnaires integrated with interviews: -Patients -Physicians |
Most patients affirmed that the methodology should be included in clinical practice. The narrative medicine project required the medical team to be actively involved and that the methodology should be incorporated in clinical training and in the healthcare organization. |
| Cepeda et al., 2008 [38] | Emotional disclosure through patient narrative may improve pain and well-being: results of a randomized controlled trial in patients with cancer pain. | Colombia | To evaluate whether the narrative approach used with patients with cancer decreases pain intensity and increases the global sense of well-being. |
Patients: -Narrative writing -McGill Pain Questionnaire |
The study underlined the need for additional studies to evaluate whether narrative medicine is associated with measurable health benefits. |
| Cercato et al., 2022 [39] | Narrative medicine: feasibility of a digital narrative diary application in oncology | Italy | To evaluate the feasibility, practicability and self-assessed utility of digital narrative medicine form the patients’ and health professionals’ perspectives. |
-Collection of patients’ stories s. -Healthcare professionals reviewed the texts and discussed them with the patients during the visits. -Final questionnaire: evaluation of digital narrative diary by patients and healthcare professionals. |
Digital narrative diary represents a new tool for use in narrative medicine and helps the clinicians to understand the experience of the patients. The results supported the concept that the NM can be introduced in clinical practice and integrated with evidence-based medicine. |
| Cercato et al., 2022 [40] | Narrative medicine: a digital diary in the management of bone and soft tissue sarcoma patients. Preliminary results of a multidisciplinary pilot study | Italy | To evaluate the utility of narrative digital diary integrated in the care pathway of patients with bone and limb soft tissue sarcomas from the patients’ and healthcare professionals’ perspective. |
Patients: digital diary Healthcare professionals: analysis of the text and discussion with the patients during the visits. Questionnaire: Evaluation of feasibility and utility of digital narrative diary using the Likert scale. |
The preliminary results showed that the digital narrative diary was an appreciated tool as this enabled the patients to express their points of view. The paper underlined the importance to strengthen the communication and relationship with the healthcare professionals. |
| De Vincentis et al., 2018 [41] | Narrative Medicine in metastatic prostate cancer reveals ways to improve patient awareness & quality of care | Italy | To map the organizational and procedural care pathway of patients with metastatic prostate cancer with the integration pf clinical and narrative data. |
-Mapping of pathway -Qualitative and narrative patient journey |
The study showed the value of the narrative approach to evaluate the patients’ experience. |
| Di Gangi et al., 2013 [42] | A narrative-based study on communication by family members in intensive care unit | Italy | To analyze stories written by patients’ families in an Intensive Care Unit (ICU) guest book in terms of families’ emotional responses, needs, perceptions and satisfaction with quality of care. | Stories written spontaneously by individuals who visited the patients in the ICU. |
First study using guest book stories from patient’s family members. Stories collected could represent an important instrument to improve the communication among family, patient and professional team. The stories could also be included as input to improve clinical practice. |
| Donzelli et al., 2015 [43] | The role of narrative medicine in pregnancy after liver transplantation | Italy | To study the use of Narrative Medicine with pregnant women after a liver transplant. | Collection of stories | Narrative Medicine could be an important instrument to support pregnant patients after a liver transplant. |
| Fox and Hauser, 2021 [44] | Exploring perception and usage of narrative medicine by specialist physicians: a qualitative analysis | US | To study the perception and usage of narrative medicine across different medical specialties. | Semi structured interviews |
The study underlines the importance of adapting narrative medicine to difference physician’s practices. “… [the patient’s narrative] helps me I guess [be] a little bit more…sensitive to her anxiety about an upcoming operation beyond the usual anxiety that…a patient has” (Surgeon) “I know things about my patients that have nothing to do with their care and that just makes me feel like there’s a real connection, and it’s just humanizing all around. Therefore, I think that this is a really important part of how you really develop that trust because you also value their story right?” (Internist) |
| Gargiulo et al., 2017 [45] | Narrative Based Medicine as a tool for needs assessment of patients undergoing hematopoietic stem cell transplantation | Italy | To investigate the physiological, relational, organizational and clinical care issues related to patients needing hematopoietic stem cell transplantation. |
Patients: unstructured interviews |
The study underlined the importance of integrating qualitative and clinical approaches to improve therapeutic effectiveness and to promote organizational patterns of service and care. The paper highlighted the usefulness of a narrative model in the patient’s care pathway for supporting the healthcare professionals to understand the patient’s needs. |
| Graffigna et al., 2017 [46] | Recovering from chronic myeloid leukemia: the patient’s perspective seen through the lens of narrative medicine | Italy | To analyze the patient’s experience of illness: impact of the latter on patient’s emotions and quality of life; reaction to the ideas of healing from the disease. | Patients: narrative diary | The is the first study adopting a narrative inquiry approach for in-depth exploration of patient perspectives related to the experience of chronic myeloid leukemia. The narrative approach supports the healthcare professionals in understanding and exploring the patient’s unmet needs. |
| Herrington and Parker, 2019 [47] | Narrative methods for assessing “quality of life” in hand transplantation: five case studies with bioethical commentary | US | To help readers imagine key features of the narratives. | Narratives of hand transplantation from an oral history | Qualitative issues concerning patient’s and caregiver’s experience should be used in clinical case studies. |
| Kvale et al., 2020 [48] | Patients’ illness narratives-From being healthy to living with incurable cancer. Encounters with doctors through the disease trajectory | Norway | To gain insight into illness narratives of patients from first symptoms to living with incurable cancer. |
Patients: Writing of stories using an interview guide or questionnaire. |
The study highlights critical issues in terms of communication with the physician and in particular the ability or inability to communicate bad news. |
| Lamprell and Braithwaite, 2019 [49] | Reading between the lines: a five-point narrative approach to online accounts of illness | Australia | To examine the pathographies of people with melanoma published on the internet. |
1. 3 months survey of the internet to understand the environment of patient storytelling. 2. Identification of sources used to tell the stories 3. Selection of narrative texts related to the personal impact of experience. |
The study honors the efforts of people with melanoma who have recounted their stories in a public form. |
| Marini et al., 2017 [50] | Narratives of experience of Italian families facing premature births | Italy | To understand the experience of families experiencing a premature birth. |
-Collection of stories -Quantitative questionnaire integrated within the narrative tool. |
The paper underlines the importance of integrating quantitative information and narratives of families with the organizational aspects of care. Narrative Medicine could be a bridge between healthcare professionals, families and health care managers. |
| Marini et al., 2016 [51] | Stories of experiences of care for growth hormone deficiency: the CRESCERE project | Italy | To understand the children and teenagers with grow hormone deficiency, their parents, siblings and healthcare providers. |
Semi structured draft to guide the narratives: patients and families. -Healthcare professionals: parallel chart |
Narrative tool was the right instrument for different stakeholders involved in grow hormone deficiency. The narratives also represented an important instrument for healthcare professionals as it provided support to improve their actions. |
| Midena et al., 2021 [52] | Real-life patient journey in neovascular age-related macular degeneration: a narrative medicine analysis in the Italian setting | Italy | To analyze the experience of patients affected by neovascular age-related macular degeneration (nAMD) in the disease management. |
-Patient journey mapping: consensus of Italian clinicians with expertise in the treatment and management of nAMD -Narratives of patients and caregivers related to patient journey (survey) |
Narrative Medicine approach highlights critical issues in the healthcare journey and represents a useful background to the patient’s pathway. |
| Palandri et al., 2018 [53] | Life for patients with myelofibrosis: the physical, emotional and financial impact, collected using narrative medicine. Results from the Italian “Back to Life” project | Italy | To investigate the experience of patients affected by myelofibrosis and their families. |
Patients and caregivers -Burden of illness questionnaire -American Medical Association’s Caregivers Self-Assessment Questionnaire -Written narrative survey |
The study underlines that a better understanding of the personal lives of patients and their families could improve the relationship between health professionals and patients. Narrative Medicine integrated with quantitative questionnaire led to a more complete view of patients’ and caregivers experiences. |
| Rushforth et al., 2021 [54] | Long Covid-The illness narratives | Italy |
To understand how and why the stories and storytelling took the forms they did and how they affected their audience. -What stories did people with long COVID tell. |
-Interviews: people with suspected acute Covid-19 thought the NHS. -Focus groups |
The study affirmed that long Covid has gained legitimacy through the stories and actions of online communities. |
| Sansone et al., 2022 [55] | Narrative diaries in the pediatric intensive care unit: a thematic analysis | Italy | To analyze the content of narrative diaries written by healthcare professionals, caregivers and relatives of children in the pediatric intensive care unit (PICU). | Diaries kept by the patient’s bedside. |
The use of diaries in the PICU represents a helpful tool that supports the communication between the healthcare professionals and the family. The use of diaries underlines the involvement of clinical staff in the wellbeing of patients and their family. The nurses affirmed that diary writing for patients is an important step in the building a good relationship with the parents. |
| Scaratti et al., 2020 [56] | Long term perceptions of illness and self after Deep Brain Stimulation in pediatric dystonia: a narrative research | Italy | To explore the experience of adult patients suffering from isolated dystonia who underwent surgery in pediatric age. | Interview guide to collect written narratives. | The study represents a starting point to further exploring and encouraging the research also on the psychological aspects that emerged from the stories. |
| Simonelli et al., 2021 [57] | Care Pathway of RPE65-Related Inherited Retinal Disorders from early symptoms to genetic counseling: a multicenter narrative medicine project in Italy | Italy | To investigate the evolution of the care pathway and expectations about genetic counseling and gene therapy from the perspectives of patients, caregivers and health professionals. |
Patients - illness plot to collect written narratives -audio-track for audio narratives Caregivers -illness plot to collect written narratives Retinologist -parallel chart Multidisciplinary healthcare professionals and Patient Association members -In-depth interviews |
The integration of these different perspectives highlighted several areas of implementation in the management of RPE65-related IRDs. The project analyzed the patient’s care pathway though the Narrative Medicine from several perspectives (patients, caregivers, and attending physicians…). |
| Slocum et al., 2017 [58] | Narrative Medicine perspectives on patient identity and integrative care in neuro-oncology | US | To analyze the role of Narrative Medicine in terms of helping patients and treatment team to build rapport and trust. | Narrative Medicine was included in the care of patients with brain tumors in a university Neuro-Oncology program. | The authors believe that the use of Narrative Medicine in neuro-oncology can provide benefits. Narrative Medicine facilitates a better communication with patients, helping professionals to understand patient needs. Clinicians could introduce Narrative Medicine within their clinical practice. |
| Slocum et al., 2019 [59] | Narrative medicine applications and quality of life in ventricular assist device (VAD) patients | US | To illustrate the role and the applications of Narrative Medicine in patients with advanced heart failure treated with ventricular assist device. | Narrative Medicine was incorporated into the visits when the patients were invited to share their illness story in an open-ended manner. | The case report underlines that the narrative process could encourage patient resilience and improved quality of life. Narrative Medicine could help clinicians to appreciate the impact of disease of illness and treatment. |
| Suter et al., 2021 [60] | The power of writing for informal cancer caregivers: results form a thematic and narrative analysis | Italy | To improve the understanding of the experience of informal caregivers living with patients with cancer. | Collection of written stories by informal caregivers | The study underlines two critical issues: the need to train healthcare professionals about terminal care; the appropriate involvement of caregivers in healthcare organizations. The stories could help other people with similar experiences. The stories written by informal caregivers could also offer significant help to healthcare professionals to manage the patient’s pathway. |
| Talarico et al., 2020 [61] | RarERN Path: a methodology towards the optimization of patients’ care pathways in rare and complex diseases developed within the European Reference Networks | Europe | To create a single reference organisational model for patients’ care pathways. |
Collection of patient views and perspectives: Survey based on the principles of narrative medicine. |
The application of the RarERN Path would help improve a patients’ pathway across Europe. Narrative Medicine is a part of this process integrated within the patients’ pathway. |
| Testa et al., 2020 [62] | The emotional and social burden of heart failure: integrating physicians’, patients’ and caregivers’ perspectives through narrative medicine | Italy | To evaluate the perspectives of patients affected by heart failure, their informal caregivers and specialists on the impact of the disease on their lives. |
Narratives: -patients -caregivers -specialists Before the narration, patients describe heart failure using metaphors or images. |
The study underlines the importance to integrate three different perspectives, patients, caregiver and specialists, in the patients’ pathway. Narrative Medicine could act as a sort of bridge between the perspectives. |
| Tonini et al., 2021 [63] | Narrative Medicine to integrate the migraine experience of patients, caregivers and clinicians: the DRONE multicenter project | Italy | To understand the migraine illness in terms of daily life, real needs and personal resources of migraineurs, their caregivers and clinicians. |
Written narratives collected through the project webpage: sociodemographic survey + illness plot (patients and caregivers) Parallel chart filled from clinicians. |
This project is the first Italian study integrating the daily lives, needs and personal resources of patients, their caregivers and clinicians with the evolution of the care pathway. The comparison between narratives and parallel charts offers significant input for the clinical practice. |
| Vanstone et al., 2016 [64] | Narrative medicine and death in the ICU: world clouds as a visual legacy | Canada | To analyze the contribution of narrative medicine to end life care in ICU. The study aims to describe how World Clouds promote a narrative medicine approach from the perspectives of families, clinicians and project team. |
-Semi structured interviews by telephone: families of patients -Semi structured interviews: clinicians working with the patients |
Word clouds emphasized a narrative orientation to medicine. |
| Volpato et al., 2021 [65] | Narrative Analysis of the impact of COVID-19 on patients with Chronic Obstructive Pulmonary Disease, their caregivers, and healthcare professionals in Italy | Italy | To study how COVID-19 impacted on people with COPD, their caregivers and their health professionals according to the quality of care, quality of life, psychological and social factors. | Semi-structured questionnaire followed by a narrative plot. | This is the first Italian project integrating three different perspectives on COPD during the emergency phase. The Narrative Medicine highlighted the experiences of patients affected by COPD and provided important feedback on the need of services integrating psychological support programs and telemedicine. |
| Zhang et al., 2020 [66] | Influence of Narrative Medicine-based health education combined with an online patient mutual assistance group on the health of patients with inflammatory bowel disease and arthritis | China | To investigate the effects of health education based on Narrative Medicine approach combined with online patient support groups in patients with IBDA. |
4 patient groups: 1. routine health education and treatment guidance 2. health education based on narrative medicine 3. online patient mutual assistance group 4. narrative medicine-based health education combined with online patient mutual assistance group Clinicians: Writing parallel charts |
The study shows that health education based on narrative medicine combined with an online patient mutual assistance group improved patient health. |
| Zocher et al., 2020 [67] | Application of narrative medicine in oncological clinical practice: impact on healthcare professional | Italy | To analyze the experience of healthcare professionals who explored a new methodological approach particularly the use of the digital narrative diary. | Interviews at the start and end of the project. The interviews were characterized by open questions related to the experience of professionals in terms of the significance and role of the patients’ narration. | The digital diary was appreciated by the healthcare professionals. The results highlight the significant role of education and training in narrative medicine. |
The studies underlined the usefulness of narrative medicine not only in qualitative research but also in integration with quantitative analysis. Gargiulo et al. [45] highlighted the importance of integrating narrative medicine and evidence-based approaches to improve therapeutic effectiveness and organizational pathways. Cappuccio et al. [36] affirmed that narrative medicine can be effective in supporting clinicians in their relationships with patients and caregivers.
Narrative Medicine is an important instrument for patients, caregivers and healthcare professionals [63]. Suter et al. [60] affirmed that patients’ stories can help other patients with similar experiences. The studies performed by Cercato [39, 40] and Zocher [67] highlighted the role of digital diaries in the care process from the perspective of healthcare professionals and patients. Sansone et al. [55] highlighted that the use of diaries in the intensive care unit is helpful in facilitating communication between healthcare professionals and the family.
Education and training
This section includes studies on the role of Narrative Medicine in the education and training of medical students and healthcare professionals. The studies discuss the experiences, roles and programmes of the Narrative Medicine programme in education and training. Nineteen studies were carried out, 10 of which were in the USA (Table 2). Only two studies were carried out in Europe, 4 in Taiwan, 1 in Canada, 1 in Iran and 1 in Israel. Seven studies focused on the role of narrative medicine for healthcare professionals [68–74], and 11 were aimed at medical students from different disciplines. All studies underlined the positive role of Narrative Medicine in training. Chou et al. [75] affirmed that the new model of narrative medicine training, “community-based participatory narrative medicine”, which focuses on shared narrative work between healthcare trainees and patients, facilitates the formation of therapeutic patient-clinician relationships but also creates new opportunities to evaluate those relationships. Darayazadeh et al. [70] underlined the effectiveness of Narrative Medicine in improving students’ reflections and empathy with patients. Additionally, Lam et al. [76] highlighted that Narrative Medicine could be a useful tool for improving clinical empathy skills. The studies used different approaches to implement the Narrative Medicine method. Arntfield et al. [77] proposed three tools at different steps of the study (survey, focus group and open-ended questions). Chou et al. [75] asked participants to write a personal narrative. DasGupta and Charon [78] used a reflective writing exercise to analyse personal experiences of illness.
Table 2.
Education and training: studies included
| Author, Year | Title | Country | Objective | Method | Conclusions |
|---|---|---|---|---|---|
| Arntfield et al., 2013 [77] | Narrative medicine as a means of training medical students toward residency competencies | Canada | To explore the influence of narrative medicine training on clinical skill development for medical students. |
Intensive month-long narrative medicine elective for fourth-year students. In-class readings (pomes, fiction, illness narratives…) Anonymous survey with open-ended questions Focus group (final day) Two open-ended questions (after 1.5 years) by email |
Narrative medicine is a promising addition to the current training strategies for future resident physicians and practicing clinicians. From the surveys and focus groups several themes emerged such as narrative medicine is misunderstood; training for narrative medicine was necessary. The study highlights that the students perceive narrative medicine as valuable and effective to empower communication, collaboration and professional development. |
| Chen et al., 2017 [68] | Impact of a narrative medicine programme on healthcare provider’s empathy scores over time | Taiwan | To investigate the role of medicine narrative as an educational programme and its impact on the empathy of clinicians. |
Healthcare professionals attended the narrative medicine programme. Perception of NM programme: 10-item survey using a 5-point Likert scale Measurement of empathy: Jefferson Scale of Empathy |
Narrative Medicine programme as an education tool for empathy is feasible. 91.4% of professionals affirmed that NM was helpful for reflection. 84.5% affirmed it was helpful for patient‒doctor relationships; 81% regarded it as essential for medical care. Empathy scores increased after the NM programme. |
| Chou et al., 2021 [75] | Patient Co-Participation in Narrative Medicine Curricula as a Means of Engaging Patients as Partners in Healthcare: a pilot study involving medical students and patients living with HIV | US | To describe a new model for narrative medicine training, “community-based participatory narrative medicine”. |
Two, five-week long narrative medicine workshops involving medical students and patients. Each participant wrote a personal narrative. Each session included close reading, writing prompt exercises and a workshop on narrative of two participants. -Focus group interviews |
Paper presents a new model of narrative medicine training called community-based participatory narrative medicine (CBPNM). This model facilitates a collaborative narrative work between medical students and patients and between academic medical centers and local communities. |
| Chu et al., 2020 [69] | A qualitative study of clinical narrative competences of medical personnel | Taiwan | To explore the dimensions and the characteristics of clinical narrative competences of medical personnel. | In-depth interview to collect the experiences related to narrative competencies of medical staff. | The results can be used as a framework for behavioral indicators of narrative competences for medical education curriculum. |
| Darayazadeh et al., 2021 [70] | The role of narrative medicine in promoting professional ethics: perceptions of Iranian medical students | Iran | To investigate the perceptions of medical students regarding the first Narrative Medicine program. |
NM program: weekly sessions for 2 months Practicing narrative writing + reflection training: 5 small groups by trained clinical teachers. At the end of the program: 10-item questionnaire with 5-point Likert scale regarding the perceptions of NM. |
The results show the effectiveness of NM in improving student reflections and empathy with patients. 98.5% believe that the NM is effective in improving empathy; 89.4% affirmed that reflection and communication skills can be improved through NM. The authors think that this program could be included in professional ethics education. |
| DasGupta, Charon R., 2014 [78] | Personal illness narratives: using reflective writing to teach empathy | US | To describe a unique exercise that builds empathy through reflective narrative writing. | Reflective writing exercise in a second-year medical student humanities seminar to explore the personal experiences of illness. | The analysis shows that the exercise was well received and recommended for other students. |
| Gowda et al., 2019 [79] |
Implementing an interprofessional narrative medicine program in academic clinics: Feasibility and program evaluation |
US | To improve the interprofessional communication and relationships through a narrative program in academic primary care clinics. |
Narrative medicine program (3 clinics, April 2016 to March 2017) Each 30 min session consisted of 4 stages: -engaging with a creative work -writing to a prompt -sharing writing in pairs -sharing writing in a large group |
Participants were engaged and supported the implementation of the program. |
| Karkabi et al., 2014 [71] |
The use of abstract paintings and narratives to foster reflective capacity in medical educators: a multinational faculty development workshop |
Israel | To enhance reflective capacity in medical educators using abstract paintings and narratives to stimulate students to reflect on their experience with patients and to examine their emotions, feelings and actions. |
Multinational faculty development workshop: 1. 3 abstract paintings presented to the group 2. participants chose one painting to focus on 3. participants described the emotions experienced 4. participants wrote a personal narrative 5. the narrative was shared in pairs |
Participants affirmed that the use of abstract paintings contributed to facilitating the reflective writing. A facilitator without education in the arts or literature can also perform the workshop. In the future, it might be interesting to compare arts-narrative-based workshops with a control group using only reflective narrative or in combination with figurative art. |
| Lam et al., 2022 [76] |
My Life, My Story: Integrating a Life Story Narrative Component Into Medical Student Curricula |
US | To improve patient-centered care competences through the narrative medicine project “My Life, My Story”. | The project was integrated into the Medical School curriculum. First and third year medical students were requested to participate in life story interview with a volunteer or patient in the inpatient hospital setting. | The project could be a useful tool to improve clinical empathy skills and understand the patients. The results showed that 77% believed that the project was a good use of time, fostered the connection with patients (79%) and was effective for appreciating the thoughts and feelings of patient (69%). |
| Lemogne et al., 2020 [80] |
Balint groups and narrative medicine compared to a control condition in promoting students’ empathy |
France | To assess the effect of Balint groups and narrative medicine training on clinical empathy among fourth-year medical students. |
Students were randomly assigned in equal numbers to Balint group, narrative medicine group or control group. Intervention group received either 7 sessions of 1.5 h Balint group or 2 h lecture and 5 sessions of 1.5 h narrative medicine training. Jefferson’s School Empathy Scale (baseline- follow up) |
The study suggests that Balint groups were able promote or maintain clinical empathy among medical students. The change in score was higher in Balint group versus control group. The change in score in the medicine narrative group was not significantly different compared to control group or Balint group. |
| Liao et al., 2020 [81] |
Storytelling in Medical Education: Narrative Medicine as a Resource for Interdisciplinary Collaboration |
Taiwan | To use Narrative Medicine for interdisciplinary collaboration by listening to illness narratives from different perspectives. |
2 groups of students: Experimental (n.33) Control (n.32) Before and after intervention: Reflective Thinking Scale for Healthcare students and providers (RTS-HSP) Empathy Scale in Patient Care (ES-PC) Analytic Narrative Medicine Writing Scoring Rubric (ANMWSR) |
After the 15-week intervention, both groups showed a better performance in all issues. The students receiving narrative medicine showed a higher level of narrative medical writing skills. The study highlights the effective use of narrative medicine for interdisciplinary collaboration. |
| Liao et al., 2021 [82] |
Understanding the lived experiences of medical learners in a narrative medicine course: a phenomenological study |
Taiwan |
The paper had two research questions: 1) What are the experiences of medical learners on a narrative medicine course? 2) How do medical learners learn with narrative medicine? |
A narrative medicine course on a three-month internal medicine for 5th year medical students. Three steps: 1) introductory lecture on narrative medicine 2) narrative writing session in which each participant prepared a personal narrative based on clinical experience 3) an educator facilitated the discussion |
Medical learners can be supported by Narrative Medicine to develop reflective capabilities for professional and personal growth. |
| Lijoi et al., 2020 [72] |
Narrative medicine: Re-engaging and re-energizing ourselves through story |
US | To demonstrate the power of Narrative Medicine to cultivate the skills of listening to patient’s stories. |
Workshop: -brief didactic -full Narrative Medicine experience -presentation of survey data and qualitative responses from resident participants -sharing of curricular materials Resilience survey: Residents’ perceptions of the impact of NM experience on their resilience |
The workshop shows that NM can be introduced in the curriculum for residents. 95% of residents affirmed that the NM provided a broader sense of meaning in their work. Curriculum can be adapted for work in other fields and with other groups of healthcare professionals. |
| Lorenz et al., 2021 [83] |
The Impact of an Unconventional Elective in Narrative Medicine and Pediatric Psycho‑oncology on Humanism in Medical Students |
US | To evaluate the impact of immersive clinical education in pediatric psyco-oncology coupled with narrative medicine on medical students. |
Retrospective review of 120 narrative journals collected from third-fourth year medical students. Students received intensive training on qualitative methods. |
The evaluation contributed to medical education in clinical setting. Experiential teaching methods plus narrative reflection could be an important instrument to empower students with humanism in a critical moment during their training. |
| Miller et al., 2014 [84] |
Sounding Narrative Medicine: Studying Students’ Professional Identity Development at Columbia University College of Physicians and Surgeons |
US | To learn whether the elements of Narrative Medicine are acquired by medical students and explore narrative medicine’s framework. |
In 2010, half-semester narrative medicine seminars. After the seminars, medical students were involved in focus groups to discuss the lessons acquired from seminars. |
Medical students affirmed that the seminars support complex interior, interpersonal and expressive capacities. |
| Shaw et al., 2019 [85] |
Integrating Storytelling into a Communication Skills Teaching Program for Medical Oncology Fellows |
US | To describe the integration between medically themed stories and other narrative methods in communication skills curriculum. |
One or more narrative methods (3–4-hour workshop) 1) reading and discussion about medically themed reflective pieces 2) sharing clinical and nonclinical stories in groups 3) brief writing reflections |
Sharing stories can help to build reflective ability, mindfulness and empathy. Integration of stories into the curriculum to construct empathy. |
| Skelton et al., 2017 [86] | Learning from patients: trainers’ use of narratives for learning and teaching |
UK Ireland Spain |
To evaluate how general practitioner trainers reflect on their experiences with patients. |
Narrative-based evaluative study 24 GP trainers recruited in Ireland, 22 in UK and 16 in Spain. Interviews performed by GP trainers and non-trainers |
The study explores the perception of GP trainers in terms of learning from patients. It empathizes the roles of doctors and patient as people rather than their social or professional roles. |
| Wallace et al., 2021 [73] |
Narrative Medicine for Healthcare Providers: Improving Practices of Advance Care Planning |
US | To analyze the effectiveness of a narrative medicine education workshop for developing the communication skills of health care professionals and facilitating reflection on the connection between personal experience and professional practices in advance care planning. |
3 h education workshop was performed for healthcare professionals. 6–8 participants with one facilitator After the workshop, the participants completed a survey on the usefulness of the training and two open-ended questions about the perceived benefits of the workshop and the connection between personal and professional experiences. |
The pilot study demonstrates that the workshop was beneficial in providing valuable information applicable to clinical practice. |
| Winkel et al., 2016 [74] |
Narrative Medicine Workshops for Obstetrics and Gynecology Residents and Association With Burnout Measures |
US | To analyze if a workshop in Narrative Medicine could improve the burnout among obstetrics and gynecologists. |
Study performed in 3 academic obstetrics and gynecology residency programs. Narrative Medicine curriculum as part of didactic activities. Electronic surveys completed at baseline and after 1 year. Narrative Medicine curriculum: 15 workshops (1 h) implemented at 4 to 8 week intervals. |
The study shows that higher attendance at workshops in Narrative Medicine was associated with reducing emotional exhaustion. |
Discussion
In this scoping review we identified 76 studies addressing dissemination and implementation of Narrative Medicine across three settings between 1998 and 2022. The studies performed by Hurwitz [3] and Greenhalgh [4] provide a path towards the Narrative Medicine affirm that sickness episodes are important milestones in patient life stories. Not only we live through storytelling, but often, with our doctor or nurse as a witness, we get sick, we improve, we get worse, we are stable and finally we also die through the story. affirms that the stories are often evocative and memorable. They are image rich, action packed and laden with emotions. Most people recall them better than they recall lists, graphs or numbers. Stories can convey important elements of nuance, including mood, tone and urgency. We learn through stories because the story form allows our existing schemas to be modified in the light of emerging experiential knowledge. The stories can capture tacit knowledge: in healthcare organizations they can bridge the gap between explicit, codified and formal knowledge (job descriptions, guidelines and protocols) and informal, not codified knowledge (knowing how to get things done in a particular organization or team, sometimes referred to as knowing the ropes). The “story” is the focal point in the studies related to the clinical practice as these discuss about the patient’s experience, illness story thought tools as questionnaires, narrative diary, chart parallels. The patient is an expert patient able to interact with the healthcare professionals, he/she had not a passive role; the patient is part of the process with the other involved stakeholders. Also, the Italian guidelines on Narrative Medicine [9] considers the storytelling as a fundamental instrument to acquire, understand and integrate several points of view related to persons involving in the disease and in the healthcare process. Storytelling represents the interaction between a healthcare professional and the patient’s world. According to this perspective, it is useful to educate in Narrative Medicine the healthcare professionals from the University to provide instruments to communicate and interact with their patients. Charon [11] emphasizes the role of training in narrative skills as an important tool permitting to physicians and medical students to improve their care. Charon [24] underlines that narrative training permits to explore the clinician’s attention to patients and to establish a relationship with patients, colleagues, and the self. The study of Liao [22] underlines that Narrative Medicine is worth recommending for healthcare education as resource for interdisciplinary collaboration among students from different discipline.
John Launer in The Art of Medicine. Narrative medicine, narrative practice, and the creation of meaning (2023) [87] affirm that Narrative Medicine could be complemented by the skills and pedagogy of narrative practice. In addition to the creation and study of words on the page, learners could bring their spoken accounts of their experiences at work and interview each other using narrative practice techniques. He also affirms that narrative practice and narrative medicine could both do more to build alliances with advocacy groups.
We have performed a picture of Narrative Medicine from its origin to today hoping that it will help to promote the power of Narrative Medicine in all three areas becoming increasingly integrated.
Strengths and limitations
The scoping review does not present the results of studies included but objectives, methodology and conclusions/suggestions as it aims to map the evidence related to the Narrative Medicine using a classification defined for the review. This classification had permit to make even clearer the “world” of Narrative Medicine and present a mapping.
English- and Italian-language articles were included because, as seen from the preceding pages, most of the studies were carried out in the United States and Italy.
This could be a limitation, as we may have excluded papers written in other languages. However, the United States and Italy are the countries where Narrative Medicine has developed the most.
Conclusions
The scoping review presents an overview of the literature considering three settings in which Narrative Medicine has emerged from its origins until today highlighting evidence in terms of theory, clinical practice, and education. Currently, a methodology to “measure” Narrative Medicine with indicators, a method assessing the effectiveness and promoting a greater diffusion of Narrative Medicine using objective and measurable indicators, is not available. Furthermore, the literature analysis doesn’t show an integration across three settings. We hope that the review will be a first step towards future projects in which it will be possible to measure Narrative Medicine according to an integrated approach between clinical practice and education/training.
Supplementary Information
Abbreviations
- NM
Narrative Medicine
- NBM
Narrative-Based Medicine
- EBM
Evidence-Based Medicine
Authors’ contributions
I.P. and S.P. carried out the scoping review, conceived the study, data collection process and drafted the manuscript. G.T. participated in the coordination of the study. All authors read, reviewed and approved the final manuscript.
Funding
The work has not been financed.
Availability of data and materials
Availability of data and materials: All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Polvani S. Cura alle stelle. Manuale di salute narrativa. Bulgarini; 2022. [Google Scholar]
- 2.Polvani S, Sarti A. Medicina narrativa in terapia intensiva. Storie di Malattia e di cura. FrancoAngeli; 2013. [Google Scholar]
- 3.Greenhalgh T, Hurwitz B. Narrative based medicine Why study narrative? BMJ. 1999;318:48–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greenhalgh T, Hurwitz B. Narrative-Based Medicine: Dialogue and Discourse in Clinical Practice. London: BMJ Books; 1998. [Google Scholar]
- 5.Hurwitz B, Charon R. A narrative future for health care. Lancet. 2013;381:1886–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ballo P, Milli M, Slater C, Bandini F, Trentanove F, Comper G, Zuppiroli A, Polvani S. Prospective Validation of the Decalogue, a Set of Doctor-Patient Communication Recommendations to Improve Patient Illness Experience and Mood States within a Hospital Cardiologic Ambulatory Setting. Biomed Res Int. 2017. 10.1155/2017/2792131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kleinman A. The Illness Narratives: Suffering, Healing, and the Human Condition. New York: Basic Books; 1988. [Google Scholar]
- 8.Good BJ. Medicine, Rationality, and Experience: An anthropological perspective. Cambridge: Cambridge University Press; 1994. [Google Scholar]
- 9.Istituto Superiore di Sanità, Linee di indirizzo per l’utilizzo della Medicina Narrativa in ambito clinico-assistenziale, per le malattie rare e cronico-degenerative. Sole24Ore Sanità. 2015.
- 10.Rui L. Wang L. Global Trends and Hotspots in Narrative Medicine Studies: A Bibliometric Analysis. 2023. 10.21203/rs.3.rs-2816041/v1. [Google Scholar]
- 11.Charon R. Narrative medicine in the international education of physicians. Presse Med. 2013;42(1):3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charon R. Narrative Medicine. A model for empathy, Reflection, profession and Trust. JAMA. 2001;286(15):1897–902. [DOI] [PubMed] [Google Scholar]
- 13.Charon R. Narrative Medicine: Caring for the sick is a work of art. JAAPA. 2013;26(12):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charon R. The membranes of care: stories in Narrative Medicine. Acad Med. 2012;87(3):342–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abettan C. From method to hermeneutics: which epistemological framework for narrative medicine? Theor Med Bioeth. 2017;38:179–93. [DOI] [PubMed] [Google Scholar]
- 16.Cenci C, Fatati G. Conversazioni online per comprendere la malattia e favorire il rapporto medico-paziente. Recenti Prog Med. 2020;111:682–4. [DOI] [PubMed] [Google Scholar]
- 17.Zaharias G. What is narrative-based medicine? Narrative-based medicine 1. Canadian Family Physician|Le Médecin de famille canadien. 2018;64:176–80. [PMC free article] [PubMed] [Google Scholar]
- 18.Charon R. Form Function, and Ethics. Ann Intern Med. 2001;134:83–7. [DOI] [PubMed] [Google Scholar]
- 19.Rosti G. Role of narrative-based medicine in proper patient assessment. Support Care Cancer. 2017;25(Suppl 1):3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greenhalgh T. Narrative based medicine in an evidence-based word. BMJ. 1999;318:323–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lederman M. Social and gendered readings of illness narratives. J Med Humanit. 2016;37:275–88. [DOI] [PubMed] [Google Scholar]
- 22.Kalitzkus V, Matthiessen PF. Narrative-Based Medicine: Potential, Pitfalls, and Practice. Permanente J. 2009;13(1):80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lanphier E. Narrative and Medicine premises, practices, pragmatism. Perspective in Biology and Medicine. 2021;64(2):211–34. [DOI] [PubMed] [Google Scholar]
- 24.Liao HC, Wang YH. Storytelling in Medical Education: Narrative Medicine as a Resource for Interdisciplinary Collaboration. Int J Environ Res Public Health. 2020. 10.3390/ijerph17041135. [DOI] [PMC free article] [PubMed]
- 25.Charon R. Close Reading and Creative Writing in Clinical Education: teaching attention, representation, and affiliation. Acad Med. 2016;91(3):345–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Mahony S. Against Narrative Medicine. Perspect Biol Med. 2013;56(4):611–9. [DOI] [PubMed] [Google Scholar]
- 27.Rian J, Hammer R. The Practical Application of Narrative Medicine at Mayo Clinic: Imagining the Scaffold of a Worthy House. Cult Med Psychiatry. 2013;37:670–80. [DOI] [PubMed] [Google Scholar]
- 28.Zaharias G. Narrative-based medicine and the general practice consultation. Narrative-based medicine 2. Canadian Family Physician|Le Médecin de famille canadien. 2018;64(4):286–90. [PMC free article] [PubMed] [Google Scholar]
- 29.Roest B, Milota M, Carlo LC. Developing new ways to listen: the value of narrative approaches in empirical (bio)ethics. BMC Med Ethics. 2021. 10.1186/s12910-021-00691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Breccia M, Graffigna G, Galimberti S, Iurlo A, Pungolino E, Pizzuti M, Maggi A, et al. Personal history and quality of life in chronic myeloid leukemia patients: a cross-sectional study using narrative medicine and quantitative analysis. Support Care Cancer. 2016;24(11):4487–93. [DOI] [PubMed] [Google Scholar]
- 31.Cappuccio A, Limonta T, Parodi A, Cristaudo A, Bugliaro F, Cannavò SP, Rossi O. Living with Chronic Spontaneous Urticaria in Italy: A Narrative Medicine Project to Improve the Pathway of Patient Care. Acta Derm Venereol. 2017;97(1):81–5. [DOI] [PubMed] [Google Scholar]
- 32.Ceccarelli F, Covelli V, Olivieri G, Natalucci F, Conti F. Systemic Lupus Erythematosus before and after COVID-19 Lockdown: How the Perception of Disease Changes through the Lenses of Narrative Medicine. Healthcare (Basel). 2021. 10.3390/healthcare9060726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cenci C, Mecarelli O. Digital narrative medicine for the personalization of epilepsy care pathways. Epilepsy Behav. 2020. 10.1016/j.yebeh.2020.107143. [DOI] [PubMed] [Google Scholar]
- 34.Banfi P, Cappuccio A, Latella M, Reale L, Muscianisi E, Marini MG. Narrative medicine to improve the management and quality of life of patients with COPD: the first experience applying parallel chart in Italy. Int J Chron Obstruct Pulmon Dis. 2018;13:287–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cappuccio A, Sanduzzi Zamparelli A, Verga M, Nardini S, Policreti A, Porpiglia PA, Napolitano S, Marini MG. Narrative medicine educational project to improve the care of patients with chronic obstructive pulmonary disease. ERJ Open Res. 2018. 10.1183/23120541.00155-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cappuccio A, Napolitano S, Menzella F, Pellegrini G, Policreti A, Pelaia G, Porpiglia PA, Marini MG. Use of narrative medicine to identify key factors for effective doctor-patient relationships in severe asthma. Multidiscip Respir Med. 2019. 10.1186/s40248-019-0190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caputo A. Exploring quality of life in Italian patients with rare disease: a computer-aided content analysis of illness stories. Psychol Health Med. 2014;19(2):211–21. [DOI] [PubMed] [Google Scholar]
- 38.Cepeda MS, Chapman CR, Miranda N, Sanchez R, Rodriguez CH, Restrepo AE, Ferrer LM, Linares RA, Carr DB. Emotional disclosure through patient narrative may improve pain and well-being: results of a randomized controlled trial in patients with cancer pain. J Pain Symptom Manage. 2008;35(6):623–31. [DOI] [PubMed] [Google Scholar]
- 39.Cercato MC, Colella E, Fabi A, Bertazzi I, Giardina BG, Di Ridolfi P, Mondati M, et al. Narrative medicine: feasibility of a digital narrative diary application in oncology. J Int Med Res. 2022. 10.1177/03000605211045507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cercato MC, Vari S, Maggi G, Faltyn W, Onesti CE, Baldi J, Scotto di Uccio A et al. Narrative Medicine: A Digital Diary in the Management of Bone and Soft Tissue Sarcoma Patients. Preliminary Results of a Multidisciplinary Pilot Study. J Clin Med. 2022. 10.3390/jcm11020406. [DOI] [PMC free article] [PubMed]
- 41.De Vincentis G, Monari F, Baldari S, Salgarello M, Frantellizzi V, Salvi E, Reale L, Napolitano S. Narrative medicine in metastatic prostate cancer reveals ways to improve patient awareness & quality of care. Future Oncol. 2018;14(27):2821–32. [DOI] [PubMed] [Google Scholar]
- 42.Di Gangi S, Naretto G, Cravero N, Livigni S. A narrative-based study on communication by family members in intensive care unit. J Crit Care. 2013;28(4):483–9. [DOI] [PubMed] [Google Scholar]
- 43.Donzelli G, Paddeu EM, D’Alessandro F, Nanni CA. The role of narrative medicine in pregnancy after liver transplantation. J Matern Fetal Neonatal Med. 2015;28(2):158–61. [DOI] [PubMed] [Google Scholar]
- 44.Fox DA, Hauser JM. Exploring perception and usage of narrative medicine by physician specialty: a qualitative analysis. Philos Ethics Humanit Med. 2021. 10.1186/s13010-021-00106-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gargiulo G, Sansone V, Rea T, Artioli G, Botti S, Continisio GI, Ferri P, et al. Narrative Based Medicine as a tool for needs assessment of patients undergoing hematopoietic stem cell transplantation. Acta Biomed. 2017;88:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Graffigna G, Cecchini I, Breccia M, Capochiani E, Della Seta R, Galimberti S, Melosi A, et al. Recovering from chronic myeloid leukemia: the patients’ perspective seen through the lens of narrative medicine. Qual Life Res. 2017;26(10):2739–54. [DOI] [PubMed] [Google Scholar]
- 47.Herrington ER, Parker LS. Narrative methods for assessing “quality of life” in hand transplantation: five case studies with bioethical commentary. Med Health Care Philos. 2019;22(3):407–25. [DOI] [PubMed] [Google Scholar]
- 48.Kvåle K, Haugen DF, Synnes O. Patients’ illness narratives-From being healthy to living with incurable cancer: Encounters with doctors through the disease trajectory. Cancer Rep (Hoboken). 2020. 10.1002/cnr2.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lamprell K, Braithwaite J. Reading Between the Lines: A Five-Point Narrative Approach to Online Accounts of Illness. J Med Humanit. 2019;40(4):569–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marini MG, Chesi P, Bruscagnin M, Ceccatelli M, Ruzzon E. Digits and narratives of the experience of Italian families facing premature births. J Matern Fetal Neonatal Med. 2018;31(17):2258–64. [DOI] [PubMed] [Google Scholar]
- 51.Marini MG, Chesi P, Mazzanti L, Guazzarotti L, Toni TD, Salerno MC, Officioso A, et al. Stories of experiences of care for growth hormone deficiency: the CRESCERE project. Future Sci OA. 2016. 10.4155/fso.15.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Midena E, Varano M, Pilotto E, Staurenghi G, Camparini M, Pece A, Battaglia PM. Real-life patient journey in neovascular age-related macular degeneration: a narrative medicine analysis in the Italian setting. Eye (Lond). 2022;36(1):182–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palandri F, Benevolo G, Iurlo A, Abruzzese E, Carella AM, Paoli C, Palumbo GA, et al. Life for patients with myelofibrosis: the physical, emotional and financial impact, collected using narrative medicine-Results from the Italian “Back to Life” project. Qual Life Res. 2018;27(6):1545–54. [DOI] [PubMed] [Google Scholar]
- 54.Rushforth A, Ladds E, Wieringa S, Taylor S, Husain L, Greenhalgh T. Long Covid-The illness narratives. Soc Sci Med. 2021. 10.1016/j.socscimed.2021.114326. [DOI] [PubMed] [Google Scholar]
- 55.Sansone V, Cancani F, Gagliardi C, Satta T, Cecchetti C, de Ranieri C, Di Nardo M, Rossi A, et al. Narrative diaries in the paediatric intensive care unit: A thematic analysis. Nurs Crit Care. 2022;27(1):45–54. [DOI] [PubMed] [Google Scholar]
- 56.Scaratti C, Zorzi G, Guastafierro E, Leonardi M, Covelli V, Toppo C, Nardocci N. Long term perceptions of illness and self after Deep Brain Stimulation in pediatric dystonia: A narrative research. Eur J Paediatr Neurol. 2020;26:61–7. [DOI] [PubMed] [Google Scholar]
- 57.Simonelli F, Sodi A, Falsini B, Bacci G, Iarossi G, Di Iorio V, Giorgio D, et al. Care Pathway of RPE65-Related Inherited Retinal Disorders from Early Symptoms to Genetic Counseling: A Multicenter Narrative Medicine Project in Italy. Clin Ophthalmol. 2021;2(15):4591–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Slocum RB, Howard TA, Villano JL. Narrative Medicine perspectives on patient identity and integrative care in neuro-oncology. J Neuroncol. 2017;134(2):417–21. [DOI] [PubMed] [Google Scholar]
- 59.Slocum RB, Hart AL, Guglin ME. Narrative medicine applications for patient identity and quality of life in ventricular assist device (VAD) patients. Heart Lung. 2019;48(1):18–21. [DOI] [PubMed] [Google Scholar]
- 60.Suter N, Ardizzone G, Giarelli G, Cadorin L, Gruarin N, Cipolat Mis C, Michilin N, et al. The power of informal cancer caregivers’ writings: results from a thematic and narrative analysis. Support Care Cancer. 2021;29(8):4381–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Talarico R, Cannizzo S, Lorenzoni V, Marinello D, Palla I, Pirri S, Ticciati S, et al. RarERN Path: a methodology towards the optimisation of patients’ care pathways in rare and complex diseases developed within the European Reference Networks. Orphanet J Rare Dis. 2021. 10.1186/s13023-021-01778-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Testa M, Cappuccio A, Latella M, Napolitano S, Milli M, Volpe M, Marini MG. The emotional and social burden of heart failure: integrating physicians’, patients’, and caregivers’ perspectives through narrative medicine. BMC Cardiovasc Disord. 2020. 10.1186/s12872-020-01809-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tonini MC, Fiorencis A, Iannacchero R, Zampolini M, Cappuccio A, Raddino R, Grillo E, et al. Narrative Medicine to integrate patients’, caregivers’ and clinicians ’migraine experiences: the DRONE multicentre project. Neurol Sci. 2021;42:5277–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vanstone M, Toledo F, Clarke F, Boyle A, Giacomini M, Swinton M, Saunders L, et al. Narrative medicine and death in the ICU: word clouds as a visual legacy. BMJ Support Palliat Care. 2016. 10.1136/bmjspcare-2016-001179. [DOI] [PubMed] [Google Scholar]
- 65.Volpato E, Centanni S, Banfi P, D’Antonio S, Peterle E, Bugliaro F, Grattagliano I, et al. Narrative Analysis of the Impact of COVID-19 on Patients with Chronic Obstructive Pulmonary Disease, Their Caregivers, and Healthcare Professionals in Italy. Int J Chron Obstruct Pulmon Dis. 2021;16:2181–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang Y, Pi B, Xu X, Li Y, Chen X, Yang N. Influence of Narrative Medicine-Based Health Education Combined With An Online Patient Mutual Assistance Group On The Health Of Patients With Inflammatory Bowel Disease and Arthritis. Psychol Res Behav Manag. 2020;7(13):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zocher U, Bertazzi I, Colella E, Fabi A, Scarinci V, Franceschini A, Cenci C, et al. Application of narrative medicine in oncological clinical practice: impact on health care professional. Recenti Prog Med. 2020;111(3):154–9. [DOI] [PubMed] [Google Scholar]
- 68.Chen PJ, Huang CD, Yeh SJ. Impact of a narrative medicine programme on healthcare providers’ empathy scores over time. BMC Med Educ. 2017. 10.1186/s12909-017-0952-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chu SY, Wen CC, Lin CW. A qualitative study of clinical narrative competence of medical personnel. BMC Med Educ. 2020. 10.1186/s12909-020-02336-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Daryazadeh S, Adibi P, Yamani N. The role of narrative medicine program in promoting professional ethics: perceptions of Iranian medical students. J Med Ethics Hist Med. 2021. 10.18502/jmehm.v14i21.8181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Karkabi K, Wald HS, Castel OC. The use of abstract paintings and narratives to foster reflective capacity in medical educators: a multinational faculty development workshop. Med Humanit. 2014;40(1):44–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lijoi AF, Tovar AD. Narrative medicine: Re-engaging and re-energizing ourselves through story. Int J Psychiatry Med. 2020;55(5):321–30. [DOI] [PubMed] [Google Scholar]
- 73.Wallace CL, Trees A, Ohs J, Hinyard L. Narrative Medicine for Healthcare Providers: Improving Practices of Advance Care Planning. Omega (Westport). 2023;87(1):87–102. [DOI] [PubMed] [Google Scholar]
- 74.Winkel AF, Feldman N, Moss H, Jakalow H, Simon J, Blank S. Narrative Medicine Workshops for Obstetrics and Gynecology Residents and Association with Burnout Measures. Obstet Gynecol. 2016;128(Suppl 1):27–33. [DOI] [PubMed] [Google Scholar]
- 75.Chou JC, Schepel IRM, Vo AT, Kapetanovic S, Schaff PB. Patient Co-Participation in Narrative Medicine Curricula as a Means of Engaging Patients as Partners in Healthcare: a pilot study involving medical students and patient living with HIV. J Med Humanit. 2021;42(4):641–57. [DOI] [PubMed] [Google Scholar]
- 76.Lam JA, Feingold-Link M, Noguchi J, Quinn A, Chofay D, Cahill K, Rougas S. My Life, My Story: Integrating a Life Story Narrative Component into Medical Student Curricula. MedEdPORTAL. 2022. 10.15766/mep_2374-8265.11211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Arntfield SL, Slesar K, Dickson J, Charon R. Narrative medicine as a means of training medical students toward residency competencies. Patient Educ Couns. 2013;91(3):280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.DasGupta S, Charon R. Personal illness narratives: using reflective writing to teach empathy. Acad Med. 2004;79(4):351–6. [DOI] [PubMed] [Google Scholar]
- 79.Gowda D, Curran T, Khedagi A, Mangold M, Jiwani F, Desai U, Charon R, Balmer D. Implementing an interprofessional narrative medicine program in academic clinics: Feasibility and program evaluation. Perspect Med Educ. 2019;8(1):52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lemogne C, Buffel du Vaure C, Hoertel N, Catu-Pinault A, Limosin F, Ghasarossian C, Le Jeunne C, Jaury P. Balint groups and narrative medicine compared to a control condition in promoting students’ empathy. BMC Med Educ. 2020. 10.1186/s12909-020-02316-w. [DOI] [PMC free article] [PubMed]
- 81.Liao HC, Wang YH. Storytelling in Medical Education: Narrative Medicine as a Resource for Interdisciplinary Collaboration. Int J Environ Res Public Health. 2020. 10.3390/ijerph17041135. [DOI] [PMC free article] [PubMed]
- 82.Liao KC, Peng CH, Snell L, Wang X, Huang CD, Saroyan A. Understanding the lived experiences of medical learners in a narrative medicine course: a phenomenological study. BMC Med Educ. 2021. 10.1186/s12909-021-02741-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lorenz JF, Darok MC, Ho L, Holstrom-Mercader MS, Freiberg AS, Dellasega CA. The Impact of an Unconventional Elective in Narrative Medicine and Pediatric Psycho-oncology on Humanism in Medical Students. J Cancer Educ. 2022;37(6):1798–805. [DOI] [PubMed] [Google Scholar]
- 84.Miller E, Balmer D, Hermann N, Graham G, Charon R. Sounding narrative medicine: studying students’ professional identity development at Columbia University College of Physicians and Surgeons. Acad Med. 2014;89(2):335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shaw AC, McQuade JL, Reilley MJ, Nixon B, Baile WF, Epner DE. Integrating Storytelling into a Communication Skills Teaching Program for Medical Oncology Fellows. J Cancer Educ. 2019;34(6):1198–203. [DOI] [PubMed] [Google Scholar]
- 86.Skelton JR, O’Riordan M, Berenguera Ossȯ A, Beavan J, Weetman K. Learning from patients: trainers’ use of narratives for learning and teaching. BJGP Open. 2017. 10.3399/bjgpopen17X100581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Launer J, Wohlmann A. Narrative medicine, narrative practice, and the creation of meaning. Lancet. 2023;401(10371):98–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Availability of data and materials: All data generated or analysed during this study are included in this published article.