Abstract
Background
New-onset atrial fibrillation (NOAF) is a common adverse outcome in acute ST-segment elevation myocardial infarction (STEMI) patients following percutaneous coronary intervention (PCI) and is associated with a worse prognosis. The platelet-to-albumin ratio (PAR) has been utilized to predict the severity and prognosis of cardiovascular diseases. This study aims to investigate the predictive value of PAR combined with the C2HEST score for NOAF in the elderly population with STEMI undergoing PCI.
Methods
445 elderly STEMI patients without a history of atrial fibrillation (AF) who underwent PCI were consecutively enrolled in this study. Multivariate logistic regression analysis was used to identify independent risk factors for NOAF after PCI.
Results
50 patients (11.2%) developed NOAF after PCI. Multivariate logistic regression analysis revealed that heart rate (HR), systemic immune-inflammation index (SII), uric acid (UA), PAR, and C2HEST score were independent risk factors for NOAF. The area under the curve (AUC) of the combined PAR and C2HEST score was 0.839, and Delong’s test indicated that the combined model had superior predictive value compared to individual markers (AUC of PAR: 0.738; AUC of C2HEST score: 0.752) (P < 0.05). The addition of PAR and C2HEST score to this model (HR, SII, and UA) significantly improved the reclassification and discrimination ability (IDI 0.175; NRI 0.734, both P < 0.001). During regular follow-up, the incidence of MACE was higher in the NOAF group compared to the non-NOAF group.
Conclusion
The combination of PAR and the C2HEST score has a high predictive value for NOAF in elderly STEMI patients following PCI.
Keywords: Acute myocardial infarction, New-onset atrial fibrillation, Elderly, C2HEST score, Platelet to albumin ratio
Background
Atrial fibrillation (AF) is currently the most common persistent arrhythmia in clinical practice, and new-onset atrial fibrillation (NOAF) is one of the common complications of acute ST-segment elevation myocardial infarction (STEMI), with an incidence rate of approximately 5–11% during hospitalization [1, 2]. Studies have shown that NOAF after STEMI is closely related to both short-term and long-term prognosis, especially in the elderly population [3, 4]. The exact mechanisms underlying the occurrence and maintenance of NOAF after percutaneous coronary intervention (PCI) remain unclear. In recent years, various indicators have been proposed to predict NOAF after PCI, including hematological markers, medication effects, imaging parameters, and electrocardiographic indicators, but their predictive value is unsatisfactory [5–7]. Therefore, identifying easily obtainable clinical indicators that can effectively predict NOAF to recognize high-risk patients post-PCI for timely intervention is of great clinical significance for improving patient outcomes. Some studies have shown the C2HEST score as a simple clinical risk stratification model, which is effective not only in identifying the risk of AF in the general population but also in certain high-risk groups [8–10]. However, its predictive value for NOAF in STEMI patients remains unsatisfactory. Moreover, the C2HEST score has limitations in using clinical data rather than biochemical and morphological data. In this context, biomarkers attempt to fill this gap by increasing dominance and expressing disease severity and duration.
Research indicates that inflammation and platelet aggregation play crucial roles in the progression of coronary artery plaques and adverse events following PCI [11–13]. Platelets are not only essential components in thrombosis but also provoke and exacerbate inflammatory responses through interactions with immune cells and the secretion of pro-inflammatory factors [14]. Similarly, albumin possesses antioxidant and anti-inflammatory properties, inhibiting platelet aggregation and activation, thereby influencing plasma viscosity [15]. Studies have shown that high platelet counts and low albumin levels are associated with poor prognosis in patients post-PCI [16, 17]. Recent research suggests that the platelet-to-albumin ratio (PAR) may more effectively reflect systemic inflammatory status than individual markers [18, 19]. However, most studies on PAR have focused on adverse outcomes in diseases like malignancies [18–20], and there is a lack of research exploring the relationship between PAR and NOAF in elderly STEMI patients post-PCI.
This study aims to investigate the association between PAR and the occurrence of NOAF during hospitalization in elderly STEMI patients and to evaluate the combined predictive value of PAR and the C2HEST score for NOAF.
Methods
Study population
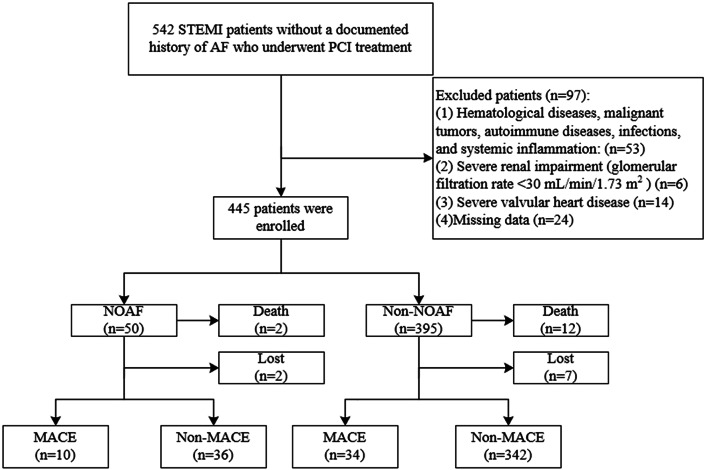
542 elderly (≥ 60 years) STEMI patients without a history of AF who underwent PCI treatment at Xuzhou Medical University Affiliated Hospital from September 2021 to February 2023 were consecutively enrolled in this study. The study was conducted in accordance with the Helsinki Declaration and was approved by the Medical Ethics Committee of the Affiliated Hospital of Xuzhou Medical University (registration number: XYFY2024-KL327-01). Inclusion criteria: (1) Successful completion of PCI treatment within 24 h of symptom onset; (2) Continuous cardiac monitoring during hospitalization. Exclusion criteria: (1) Hematological diseases, malignant tumors, autoimmune diseases, infections, and systemic inflammation; (2) Severe renal impairment (glomerular filtration rate < 30 mL/min/1.73 m2); (3) Severe valvular heart disease; (4) Missing data (Fig. 1).
Fig. 1.
Study flow chart
Data Collection
Data on demographic information, comorbidities, admission clinical characteristics, laboratory, and echocardiographic data were collected through the electronic medical record system. Medications refer to those taken at the time of discharge. Venous blood was drawn to measure biochemical parameters within 24 h of admission, including serum total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), albumin, white blood cells (WBC), neutrophils, and other biomarkers. The PAR was calculated as the platelet count divided by serum albumin concentration. The neutrophil-to-lymphocyte ratio (NLR) was calculated as the neutrophil count divided by the lymphocyte count. The systemic immune-inflammation index (SII) was calculated as (neutrophil count × platelet count) / lymphocyte count. The infarct-related artery was recorded based on coronary angiography results. All patients underwent transthoracic echocardiography within 6 h of admission to measure left ventricular ejection fraction (LVEF) and left atrial (LA) diameter. The C2HEST score was calculated based on the presence of coronary artery disease (CAD) (1 point), chronic obstructive pulmonary disease (COPD) (1 point), hypertension (1 point), elderly age (≥ 75 years, 2 points), systolic heart failure (HF) (2 points), and thyroid disease (1 point) [8–10]. All patients scored 1 point regarding the “CAD “item of the score.
Outcomes and follow-up
All patients received continuous electrocardiographic monitoring postoperatively to identify arrhythmias. NOAF was defined as the occurrence of AF during hospitalization in patients with no prior history of AF and who presented with sinus rhythm upon admission. Based on the occurrence of AF, patients were divided into the NOAF and non-NOAF groups. Patients were followed up regularly for one year through outpatient visits and telephone calls to record their prognosis. Major adverse cardiovascular events (MACE) included cardiac death, new myocardial infarction, hospitalization due to HF, and ischemic stroke.
Statistical analysis
Statistical analyses were performed using SPSS Statistics (IBM, SPSS, version 16) and R Statistical Software (R version 4.0.5, R Foundation for Statistical Computing). Continuous variables were presented as mean ± standard deviation or median (interquartile range), and categorical variables were expressed as numbers (percentages). Independent samples t-tests or non-parametric tests (Mann-Whitney U test) were used for continuous variables, while chi-square tests or Fisher’s exact tests were used for categorical variables. Indicators with statistically significant differences (P < 0.05) in univariate logistic regression analysis were included in multivariate logistic regression analysis using a stepwise regression method to identify independent risk factors for NOAF. Receiver Operating Characteristic (ROC) curves were used to assess the predictive value of relevant risk factors for NOAF, with the optimal cutoff value determined by the maximum Youden index, and the area under the curve (AUC) was calculated. The DeLong test was used to compare differences in AUC between different models. Restricted cubic splines (RCS) were used to explore the dose-response relationship between PAR and NOAF during hospitalization. Net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were further employed to assess improvements in reclassification and discriminatory abilities of the predictive model. The cumulative incidence of postoperative MACE was calculated using Kaplan-Meier survival curves, and the log-rank test comparisons were made. A P-value < 0.05 was considered statistically significant.
Result
Baseline characteristics
A total of 445 patients were included in the study, with 50 patients in the NOAF group (mean age 75.06 ± 6.99 years, 58.0% male) and 395 patients in the non-NOAF group (mean age 70.93 ± 6.56 years, 64.3% male). There was a statistically significant difference in age between the two groups (P < 0.05). The baseline characteristics of the two groups are shown in Table 1. Compared to the non-NOAF group, the NOAF group had a higher proportion of patients with hyperthyroidism, COPD, and HF. The NOAF group had lower systolic blood pressure (SBP) and LVEF but a higher heart rate (HR) than the non-NOAF group. In laboratory blood tests, the NOAF group had higher levels of WBC, neutrophils, peak NT-proBNP, platelets, Uric acid (UA), NLR, SII, and PAR than the non-NOAF group. Conversely, lymphocyte count, albumin, and estimated glomerular filtration rate (eGFR) were lower in the NOAF group. Coronary angiography showed no significant differences in the proportion of vascular lesions between the NOAF and non-NOAF groups. Additionally, the NOAF group had significantly higher C2HEST scores and a greater proportion of patients with Killip class ≥ 2 than the non-NOAF group.
Table 1.
Baseline characteristics of patients
| Non-NOAF group (n = 395) |
NOAF group (n = 50) |
P-value | |
|---|---|---|---|
| Age, years | 70.93 ± 6.56 | 75.06 ± 6.99 | < 0.001 |
| Elderly age (≥ 75 years), n (%) | 105(26.6%) | 30(60.0%) | < 0.001 |
| Male, n (%) | 254(64.3%) | 29(58.0%) | 0.383 |
| BMI, kg/m2 | 24.32 ± 3.63 | 24.48 ± 3.57 | 0.761 |
| SBP, mmHg | 124.66 ± 21.02 | 115.54 ± 22.11 | 0.004 |
| DBP, mmHg | 76.53 ± 12.93 | 73.76 ± 13.45 | 0.155 |
| HR, beats/min | 78.10 ± 12.80 | 85.82 ± 12.63 | < 0.001 |
| Smoking, n (%) | 102(25.8%) | 12(24.0%) | 0.781 |
| Hypertension, n (%) | 174(44.1%) | 28(56.0%) | 0.110 |
| Diabetes, n (%) | 88(22.3%) | 11(22.0%) | 0.964 |
| Stroke/TIA, n (%) | 51(12.9%) | 9(18.0%) | 0.321 |
| Hyperthyroidism, n (%) | 3(0.8%) | 4(8.0%) | < 0.001 |
| COPD, n (%) | 21(5.3%) | 12(24.0%) | < 0.001 |
| HF, n (%) | 53(13.4%) | 13(26.0%) | 0.018 |
| WBC, 10^9/L | 8.71 ± 2.32 | 9.88 ± 3.33 | 0.002 |
| Neutrophil, 10^9/L | 6.92 ± 2.21 | 7.83 ± 3.06 | 0.010 |
| Lymphocyte, 10^9/L | 1.21 ± 0.51 | 0.99 ± 0.41 | 0.003 |
| Peak hs-TnT, ng/L | 3872.0(1701.0,6618.0) | 4662.0(2385.5,6922.3) | 0.326 |
| Peak NT-proBNP, pg/mL | 1815.0(925.1,3484.5) | 3176.9(1553.6,6288.3) | 0.001 |
| Peak hs-CRP, mg/L | 13.3(4.7,37.0) | 17.8(8.9,47.6) | 0.141 |
| Platelet, 10^9/L | 187.37 ± 47.80 | 246.72 ± 86.49 | < 0.001 |
| FBG, mmol/L | 6.94 ± 2.85 | 6.86 ± 1.83 | 0.845 |
| Albumin, g/L | 37.98 ± 3.53 | 36.01 ± 4.84 | < 0.001 |
| NLR | 7.03 ± 4.74 | 9.96 ± 7.24 | < 0.001 |
| PAR | 4.97 ± 1.32 | 7.08 ± 3.17 | < 0.001 |
| SII | 1041.68(687.35,1642.22) | 1848.03 (943.64,3211.81) | < 0.001 |
| TG, mmol/L | 1.37 ± 0.81 | 1.32 ± 1.03 | 0.708 |
| TC, mmol/L | 4.26 ± 1.04 | 4.17 ± 1.38 | 0.570 |
| LDL-C, mmol/L | 2.67 ± 0.86 | 2.64 ± 1.15 | 0.823 |
| HDL-C, mmol/L | 1.06 ± 0.28 | 1.11 ± 0.32 | 0.244 |
| UA, µmol/L) | 294.72 ± 84.29 | 324.94 ± 107.42 | 0.021 |
| eGFR, mL/min/1.73m2 | 101.27 ± 21.02 | 89.89 ± 29.96 | 0.001 |
| LVEF, % | 51.87 ± 7.09 | 47.14 ± 7.21 | < 0.001 |
| LA diameter, mm | 38.09 ± 5.78 | 39.42 ± 5.15 | 0.121 |
| Killip class ≥ 2, n (%) | 66(16.7%) | 15(30.0%) | 0.022 |
| C2HEST score | 2.30 ± 1.25 | 3.60 ± 1.49 | < 0.001 |
| LAD, n (%) | 178(45.1%) | 22(44.0%) | 0.887 |
| LCX, n (%) | 43(10.9%) | 8(16%) | 0.285 |
| RCA, n (%) | 173(43.8%) | 20(40.0%) | 0.610 |
| Other, n (%) | 1(0.3%) | 0(0%) | 0.722 |
| Onset to balloon time, min | 278.00(255.00,303.00) | 247.00(178.75,394.75) | 0.754 |
| Statin, n (%) | 381(96.5%) | 47(94.0%) | 0.393 |
| ACEI/ARB, n (%) | 173(43.8%) | 21(42.0%) | 0.809 |
| β-blockers, n (%) | 288(72.9%) | 40(80.0%) | 0.283 |
| Spironolactone, n (%) | 55(13.9%) | 8(16.0%) | 0.692 |
| Calcium channel blockers, n (%) | 132(33.4%) | 17(34.0%) | 0.934 |
| Death, n (%) | 12(3.0%) | 2(4.0%) | 0.714 |
Abbreviations BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: Heart rate; TIA: transient ischemic attack; COPD: chronic obstructive pulmonary disease; HF: heart failure; WBC: white blood cells; hs-TnT: high-sensitivity Troponin T; NT-proBNP: N-terminal pro-brain natriuretic peptide; hs-CRP: high-sensitivity C-reactive protein; FBG: Fasting Blood Glucose; NLR: neutrophil to lymphocyte ratio; PAR: neutrophil percentage to albumin ratio; SII: systematic immune-inflammation index; TG: triglyceride; TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; eGFR: estimated glomerular filtration rate; LVEF: left ventricle ejection fraction; LA: left atrial; LAD: left anterior descending artery; LCX: left circumflex artery; RCA: right coronary artery; ACE-I: indicates angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker
Independent risk factors of NOAF
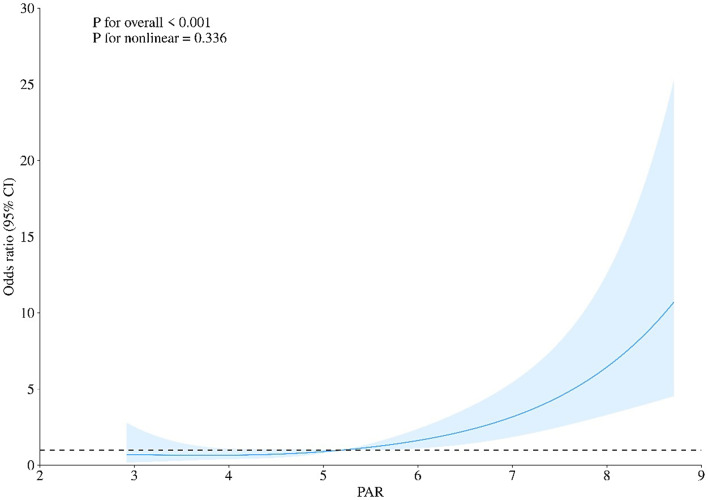
In the univariate logistic regression analysis, Age, SBP, HR, WBC, Ln(Peak NT-proBNP), NLR, PAR, SII, UA, eGFR, LVEF, Killip class ≥ 2, and C2HEST score were found to be significantly associated with NOAF (P < 0.05). These variables were included in the multivariate logistic regression analysis. After using a stepwise forward method to eliminate confounding factors, the results revealed that HR, PAR, SII, UA, and C2HEST score remained significantly associated with NOAF after PCI (Table 2). Additionally, RCS analysis demonstrated a linear association between baseline PAR levels and NOAF (Fig. 2; nonlinear P = 0.336).
Table 2.
Independent clinical predictors for AF after STEMI
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P-value | OR | 95%CI | P-value | |
| Male | 1.304 | 0.717–2.372 | 0.384 | |||
| Age | 1.092 | 1.046–1.141 | < 0.001 | |||
| BMI | 1.013 | 0.935–1.097 | 0.760 | |||
| SBP | 0.979 | 0.964–0.993 | 0.005 | |||
| DBP | 0.983 | 0.961–1.006 | 0.156 | |||
| HR | 1.048 | 1.024–1.074 | < 0.001 | 1.037 | 1.008–1.066 | 0.012 |
| WBC | 1.189 | 1.066–1.327 | 0.002 | |||
| Ln (Peak hs-TnT) | 1.192 | 0.860–1.652 | 0.291 | |||
| Ln (Peak NT-proBNP) | 1.597 | 1.213–2.103 | 0.001 | |||
| Peak hs-CRP | 1.003 | 0.997–1.009 | 0.379 | |||
| NLR | 1.083 | 1.035–1.132 | < 0.001 | |||
| PAR | 1.789 | 1.480–2.162 | < 0.001 | 1.657 | 1.319–2.081 | < 0.001 |
| SII | 1.001 | 1.000-1.001 | < 0.001 | 1.000 | 1.000-1.001 | 0.031 |
| TG | 0.931 | 0.640–1.354 | 0.707 | |||
| TC | 0.922 | 0.696–1.220 | 0.569 | |||
| LDL | 0.963 | 0.689–1.344 | 0.823 | |||
| HDL | 1.756 | 0.680–4.533 | 0.244 | |||
| UA | 1.004 | 1.001–1.007 | 0.022 | 1.004 | 1.000-1.008 | 0.042 |
| eGFR | 0.981 | 0.971–0.993 | 0.001 | |||
| LVEF | 0.919 | 0.883–0.956 | < 0.001 | |||
| LA diameter | 1.042 | 0.989–1.097 | 0.122 | |||
| Killip class ≥ 2 | 2.136 | 1.104–4.134 | 0.024 | |||
| Onset to balloon time | 1.003 | 0.998–1.009 | 0.236 | |||
| C2HEST score | 1.897 | 1.531–2.349 | < 0.001 | 1.780 | 1.396–2.270 | < 0.001 |
Abbreviations BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; WBC: white blood cells; hs-TnT: high-sensitivity Troponin T; NT-proBNP: N-terminal pro- brain natriuretic peptide; hs-CRP: high-sensitivity C-reactive protein; NLR: neutrophil to lymphocyte ratio; PAR: neutrophil percentage to albumin ratio; SII: systematic immune-inflammation index; TG: triglyceride; TC: total cholesterol; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; UA: uric acid; eGFR: estimated glomerular filtration rate; LVEF: left ventricle ejection fraction; LA: left atrial
Fig. 2.
RCS for the odds ratio of the risk of NOAF
The discriminatory ability of PAR and C2HEST score
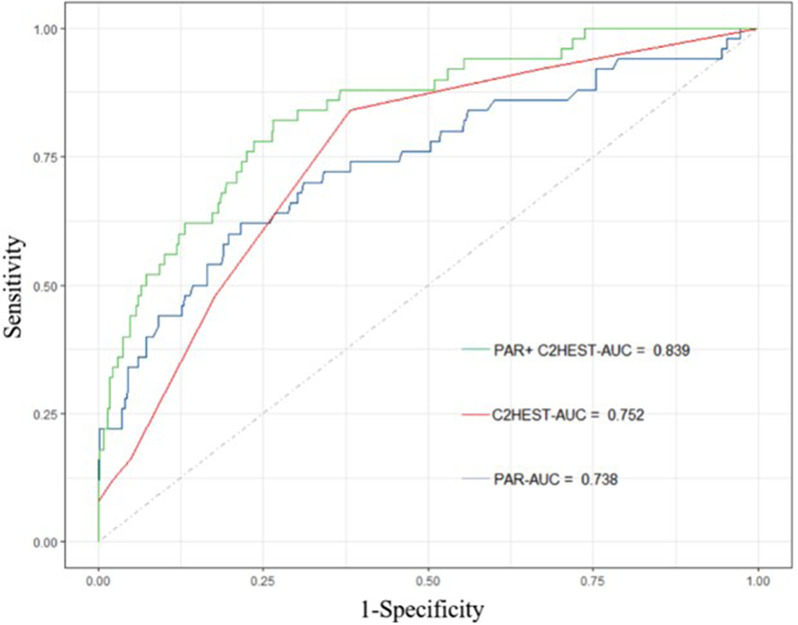
In the cohort study, ROC curve analysis revealed that PAR and C2HEST score had relatively larger AUC areas than other clinical risk factors (HR, UA, and SII) (Table 3). Further evaluation of the predictive value of NOAF by combining PAR and C2HEST score showed an AUC of 0.839 (Fig. 3). The DeLong test indicated that the predictive value of the combined PAR and C2HEST score was significantly superior to that of individual indicators (P < 0.05) (Table 4). A clinical model was constructed using independent risk factors identified from multivariate analysis, including HR, UA, and SII. When PAR and C2HEST scores were added to this clinical risk model, significant improvements in reclassification and discriminatory abilities were observed (IDI 0.175; NRI 0.734, both P < 0.001) (Table 5).
Table 3.
ROC curve for the prediction of AF after STEMI
| AUC | 95%CI | Sensitivity | Specificity | |
|---|---|---|---|---|
| HR | 0.672 | 0.594–0.751 | 0.680 | 0.612 |
| SII | 0.694 | 0.604–0.783 | 0.460 | 0.886 |
| UA | 0.562 | 0.468–0.656 | 0.280 | 0.919 |
| PAR | 0.738 | 0.655–0.820 | 0.620 | 0.885 |
| C2HEST score | 0.752 | 0.684–0.821 | 0.840 | 0.618 |
| PAR + C2HEST score | 0.839 | 0.780–0.897 | 0.820 | 0.734 |
Abbreviations HR: Heart rate; SII: systematic immune-inflammation index; UA: uric acid; PAR: neutrophil percentage to albumin ratio
Fig. 3.
ROC curve for the prediction of NOAF after STEMI
Table 4.
Comparison of different ROC curves
| Different ROC curves | Z | P-value |
|---|---|---|
| PAR vs. C2HEST score | 0.256 | 0.798 |
| PAR + C2HEST score vs. PAR | 3.504 | < 0.001 |
| PAR + C2HEST score vs. C2HEST score | 2.504 | 0.012 |
Abbreviations SII: systematic immune-inflammation index; PAR: neutrophil percentage to albumin ratio
Table 5.
Discrimination accuracy and reclassification of risk markers of NOAF after STEMI
| NRI | IDI | |||
|---|---|---|---|---|
| Estimate (95% CI) | P-value | Estimate (95% CI) | P-value | |
| Conventional model | Reference | - | Reference | - |
| + PAR | 0.573 (0.284–0.862) | < 0.001 | 0.107 (0.042–0.172) | 0.001 |
| + C2HEST score | 0.616 (0.337–0.895) | < 0.001 | 0.078 (0.037–0.119) | < 0.001 |
| + C2HEST score + PAR | 0.734 (0.450–1.018) | < 0.001 | 0.175 (0.100–0.250) | < 0.001 |
Conventional model included HR, SII, and UA
Abbreviations CI, confidence interval; IDI, integrated discrimination index; NRI, net reclassification improvement. HR: Heart rate; SII: systematic immune-inflammation index; UA: uric acid; PAR: neutrophil percentage to albumin ratio
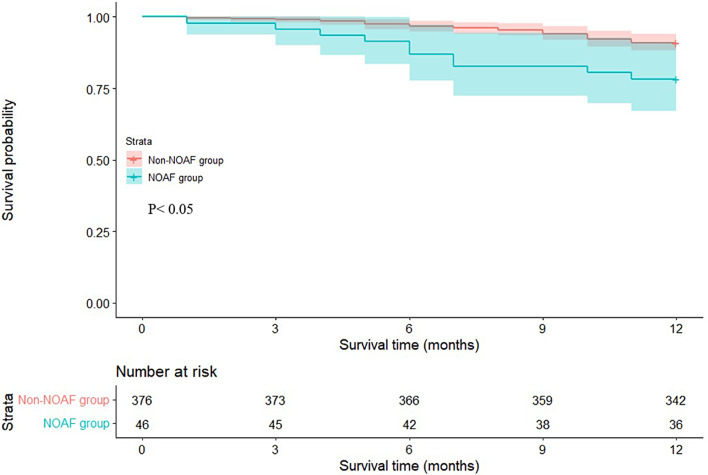
Long-term survival analysis
During the hospital stay, 14 patients died. A further 1-year follow-up was conducted on the remaining 431 patients, with 9 patients lost to follow-up. During the follow-up period, the incidence of MACE was 21.7% in the NOAF group and 9.0% in the non-NOAF group. Kaplan-Meier survival analysis showed that the incidence of MACE was significantly higher in the NOAF group compared to the non-NOAF group (log-rank, P < 0.05) (Fig. 4).
Fig. 4.
The Kaplan–Meier curves of long-term MACE between the NOAF and non-NOAF groups
Discussion
In this study, 445 elderly STEMI patients were included to analyze the independent risk factors for NOAF after PCI. The results indicated that: (1). PAR and C2HEST score are independent risk factors for NOAF after PCI, and their combination has a higher predictive value; (2). Adding PAR and C2HEST score to the clinical risk factors model significantly improves the discrimination and reclassification ability for predicting NOAF; (3). A regular 1-year follow-up of the included patients showed that the NOAF group had a higher incidence of MACE outside the hospital, as demonstrated by Kaplan-Meier survival analysis.
NOAF is a common complication after PCI in STEMI patients, with an incidence rate of approximately 5–11%, which can prolong hospital stays, increase in-hospital mortality risk, and is associated with a worse long-term prognosis [1–4]. Mrdovic et al. demonstrated that patients in the NOAF group had a higher risk of MACE within 30 days [21]. Another study by Reinstadler et al. further confirmed that NOAF is an independent predictor of composite outcomes, including all-cause mortality, non-fatal reinfarction, and congestive HF within one year after acute myocardial infarction (AMI) [22]. In this study, the incidence of NOAF in elderly STEMI patients after PCI was 11.2%, and the NOAF group had a higher incidence of MACE during the follow-up period (21.7% vs. 9.0%). Research indicates that the adverse hemodynamic effects of NOAF, such as loss of atrial contraction and atrioventricular synchrony, acceleration of ventricular rate, valvular regurgitation, and irregularity of the beat-to-beat interval, can lead to reduced cardiac output [23]. Therefore, early identification of high-risk patients for NOAF after PCI is of significant clinical value in ensuring preventive treatment and care during hospitalization.
Atrial electrical and structural remodeling forms the basis for the occurrence of AF [24]. Research indicates that inflammatory cytokines in cardiac tissue can cause oxidative damage to the atrial myocardium, subsequently promoting the occurrence of AF [25]. Although many indicators reflecting the inflammatory response have been confirmed to be closely related to the prognosis of AMI patients, their predictive value is often limited [26, 27]. The SII, which is based on a combination of neutrophil, platelet, and lymphocyte counts, has shown a strong correlation with adverse outcomes in stroke, AMI, and various malignancies [26, 28–30]. Although this study also confirmed that SII is an independent risk factor for NOAF after PCI, its predictive value and sensitivity are relatively low, which is a notable limitation. Therefore, searching for new hematologic markers that effectively predicting NOAF is of significant clinical importance.
Basic research indicates that activated platelets can promote interactions between leukocytes and damaged vascular endothelial cells, leading to excessive production of pro-inflammatory factors. This results in releasing many inflammatory mediators, which participate in myocardial injury [14]. A nationwide study by Song et al. involving 13,085 patients confirmed that baseline platelet count is associated with the prognosis of AMI patients, independent of potential confounding factors [17]. Serum albumin is primarily used clinically to assess malnutrition and possesses various physiological properties, including anti-inflammatory, antioxidant, anticoagulant, antiplatelet aggregation, and maintenance of capillary membrane stability [15]. Hypoalbuminemia has been shown to be associated with poor prognosis in various cardiovascular diseases, including AF, venous thromboembolism, stroke, and ischemic heart disease [31]. In recent years, the PAR has gained attention as a reliable new indicator that comprehensively reflects systemic inflammation, platelet aggregation, immune, and nutritional status [18, 19, 32]. PAR provides a more accurate and objective overall assessment than evaluating platelets or albumin alone. Tan et al. confirmed that PAR is a risk factor for the prognosis of patients with IgA nephropathy, independent of other platelet parameters [18]. Saito et al. also demonstrated that PAR is associated with the prognosis of cholangiocarcinoma [20]. However, studies on the relationship between PAR and cardiovascular disease prognosis are still limited. A study by Hao et al. found that PAR is an independent risk factor for MACE in patients after AMI, but there have been no reports on its association with in-hospital NOAF [19]. Our study found that PAR is an independent risk factor for in-hospital NOAF in elderly STEMI patients and has superior predictive value compared to other risk factors. Additionally, as a simple and easily assessed serum biomarker, PAR helps stratify the risk of STEMI in patients undergoing PCI and facilitates early identification of their risk for NOAF.
The C2HEST score, a simple scoring tool, was initially designed to identify the risk of incident AF in the general population [10]. Recent studies have found that the C2HEST score can effectively predict the risk of NOAF in patients after a stroke, suggesting that it may have a similar predictive value for NOAF in certain high-risk populations [9]. Although the C2HEST score is composed of cardiovascular disease risk factors, there is currently limited research on evaluating prognosis in STEMI populations after PCI for prognosis. A study involving 555 Italian patients found that the C2HEST score could effectively predict the risk of NOAF after PCI [8], which is lacking relevant research in the Asian population. Our study confirms that the C2HEST score is a good predictor of the risk of NOAF after PCI in elderly Asian STEMI patients. Furthermore, when the C2HEST score is combined with the PAR, its predictive value is significantly enhanced. Components included in the C2HEST score, such as hypertension [33], CAD [34], and HF [35], are associated with activated inflammatory states. PAR levels reflect the inflammatory state of the body, increasing the risk of patients with related diseases, which may be more clinically relevant for patients with NOAF as a complementary stratification marker for the C2HEST score.
This study also found that HR, SII, and UA are independent risk factors for NOAF in STEMI patients, but the predictive value of these individual factors is relatively low. By sequentially adding PAR and the C2HEST score to predictive models based on these independent risk factors, we observed a significant improvement in the model’s reclassification and discrimination ability. This indicates that combining PAR and the C2HEST score can further optimize the risk stratification for NOAF in elderly STEMI patients. Additionally, Regarding the comparison of " onset to balloon time”, our study showed no significant differences between the two groups, suggesting that the occurrence of NOAF may be more related to the patient’s underlying disease state (such as previous HF or other comorbidities).
Limitations
Firstly, the number of patients included in this study is limited and is a single-center study. Future research should expand the sample size and conduct multi-center studies to validate these conclusions. Secondly, although patients with a previous history of AF were excluded, we cannot completely rule out the possibility of misclassifying NOAF, as undiagnosed AF patients may be included. Lastly, unidentified confounding factors may still exist despite using multivariable modeling to determine independent risk factors that could affect the study results.
Conclusions
PAR and C2HEST score are independent risk factors for NOAF in hospitalized elderly STEMI patients, and their combination improves prediction accuracy. Patients who experience NOAF during their hospital stay have a higher proportion of MACE in the follow-up period.
Acknowledgements
Not applicable.
Author contributions
FY. W and RL. Y designed the study. FY. W, YD. S collected the data. FY. W, N. A, T.L and RR. L analyzed the data. Y. L, DF. P and SL. L were responsible for drafting or revising the article critically for important intellectual content. All authors wrote the manuscript and approved the final manuscript.
Funding
None.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval and consent to participate
All methods were carried out by the Declaration of Helsinki. This study protocol was reviewed and approved by the Medical Ethics Committee, the Affiliated Hospital of Xuzhou Medical University, registration number [XYFY2024-KL327-01]. Written informed consent was obtained from all patients, allowing for the retrospective utilization of their de-identified data for health-related research purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mazzone A, Scalese M, Paradossi U, Del Turco S, Botto N, De Caterina A, Trianni G, Ravani M, Rizza A, Molinaro S, et al. Development and validation of a risk stratification score for new-onset atrial fibrillation in STEMI patients undergoing primary percutaneous coronary intervention. Int J Clin Pract. 2018;72(4):e13087. [DOI] [PubMed] [Google Scholar]
- 2.Rene AG, Généreux P, Ezekowitz M, Kirtane AJ, Xu K, Mehran R, Brener SJ, Stone GW. Impact of atrial fibrillation in patients with ST-elevation myocardial infarction treated with percutaneous coronary intervention (from the HORIZONS-AMI [Harmonizing outcomes with revascularization and stents in Acute Myocardial Infarction] trial). Am J Cardiol. 2014;113(2):236–42. [DOI] [PubMed] [Google Scholar]
- 3.Morishima I, Tomomatsu T, Okumura K, Sone T, Tsuboi H, Morita Y, Inoue Y, Yoshida R, Yura Y, Murohara T. New-onset atrial fibrillation may be a more important predictor of cardiac mortality in acute myocardial infarction patients than preexisting atrial fibrillation. Int J Cardiol. 2015;187:475–7. [DOI] [PubMed] [Google Scholar]
- 4.Petersen JK, Butt JH, Yafasova A, Torp-Pedersen C, Sørensen R, Kruuse C, Vinding NE, Gundlund A, Køber L, Fosbøl EL, Østergaard L. Incidence of ischaemic stroke and mortality in patients with acute coronary syndrome and first-time detected atrial fibrillation: a nationwide study. Eur Heart J. 2021;42(44):4553–61. [DOI] [PubMed] [Google Scholar]
- 5.Raczkowska-Golanko M, Raczak G, Gruchała M, Daniłowicz-Szymanowicz L. Comprehensive Use of Routine Clinical parameters to identify patients at risk of New-Onset Atrial Fibrillation in Acute myocardial infarction. J Clin Med. 2021;10(16). [DOI] [PMC free article] [PubMed]
- 6.Zeng RX, Chen MS, Lian BT, Liao PD, Zhang MZ. Left ventricular ejection fraction and left atrium diameter related to new-onset atrial fibrillation following acute myocardial infarction: a systematic review and meta-analysis. Oncotarget. 2017;8(46):81137–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rencuzogullari I, Çağdaş M, Karakoyun S, Yesin M, Gürsoy MO, Artaç İ, İliş D, Efe SC, Tanboga IH. Propensity score matching analysis of the impact of Syntax score and syntax score II on new onset atrial fibrillation development in patients with ST segment elevation myocardial infarction. Ann Noninvasive Electrocardiol. 2018;23(2):e12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biccirè FG, Tanzilli G, Prati F, Sammartini E, Gelfusa M, Celeski M, Budassi S, Barillà F, Lip GYH, Pastori D. Prediction of new onset atrial fibrillation in patients with acute coronary syndrome undergoing percutaneous coronary intervention using the C2HEST and mC2HEST scores: a report from the multicenter REALE-ACS registry. Int J Cardiol. 2023;386:45–9. [DOI] [PubMed] [Google Scholar]
- 9.Li YG, Bisson A, Bodin A, Herbert J, Grammatico-Guillon L, Joung B, Wang YT, Lip GYH, Fauchier L. C2HEST score and prediction of Incident Atrial Fibrillation in Poststroke patients: a French Nationwide Study. J Am Heart Assoc. 2019;8(13):e012546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li YG, Pastori D, Miyazawa K, Shahid F, Lip GYH. Identifying At-Risk patients for sustained Atrial High-Rate episodes using the C2HEST score: the West Birmingham Atrial Fibrillation Project. J Am Heart Assoc. 2021;10(6):e017519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crea F, Libby P. Acute Coronary syndromes: the Way Forward from mechanisms to Precision Treatment. Circulation. 2017;136(12):1155–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–95. [DOI] [PubMed] [Google Scholar]
- 13.Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32(9):2045–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holinstat M. Normal platelet function. Cancer Metastasis Rev. 2017;36(2):195–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17(6):432–7. [DOI] [PubMed] [Google Scholar]
- 16.Arques S. Human serum albumin in cardiovascular diseases. Eur J Intern Med. 2018;52:8–12. [DOI] [PubMed] [Google Scholar]
- 17.Song PS, Ahn KT, Jeong JO, Jeon KH, Song YB, Gwon HC, Rha SW, Jeong MH, Seong IW. Association of baseline platelet count with all-cause mortality after acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2021;10(2):176–83. [DOI] [PubMed] [Google Scholar]
- 18.Tan J, Song G, Wang S, Dong L, Liu X, Jiang Z, Qin A, Tang Y, Qin W. Platelet-to-albumin ratio: a novel IgA. Nephrop Prognosis Predictor. 2022;13:842362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hao P, Feng S, Suo M, Wang S, Wu X. Platelet to albumin ratio: a risk factor related to prognosis in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention. Int J Cardiol. 2024;395:131588. [DOI] [PubMed] [Google Scholar]
- 20.Saito N, Shirai Y, Horiuchi T, Sugano H, Shiba H, Sakamoto T, Uwagawa T, Yanaga K. Preoperative platelet to albumin ratio predicts outcome of patients with Cholangiocarcinoma. Anticancer Res. 2018;38(2):987–92. [DOI] [PubMed] [Google Scholar]
- 21.Mrdovic I, Savic L, Krljanac G, Perunicic J, Asanin M, Lasica R, Antonijevic N, Kocev N, Marinkovic J, Vasiljevic Z, Ostojic M. Incidence, predictors, and 30-day outcomes of new-onset atrial fibrillation after primary percutaneous coronary intervention: insight into the RISK-PCI trial. Coron Artery Dis. 2012;23(1):1–8. [DOI] [PubMed] [Google Scholar]
- 22.Reinstadler SJ, Stiermaier T, Eitel C, Fuernau G, Saad M, Pöss J, de Waha S, Mende M, Desch S, Metzler B, et al. Impact of Atrial Fibrillation during ST-Segment-Elevation myocardial infarction on infarct characteristics and prognosis. Circ Cardiovasc Imaging. 2018;11(2):e006955. [DOI] [PubMed] [Google Scholar]
- 23.Clark DM, Plumb VJ, Epstein AE, Kay GN. Hemodynamic effects of an irregular sequence of ventricular cycle lengths during atrial fibrillation. J Am Coll Cardiol. 1997;30(4):1039–45. [DOI] [PubMed] [Google Scholar]
- 24.Sagris M, Vardas EP, Theofilis P, Antonopoulos AS, Oikonomou E, Tousoulis D. Atrial fibrillation: Pathogenesis, predisposing factors, and Genetics. Int J Mol Sci. 2021;23(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015;12(4):230–43. [DOI] [PubMed] [Google Scholar]
- 26.Li H, Meng S, Chen W, Lei X, Kong X, Zhu H. Comparison of different systemic inflammatory markers in Predicting Clinical outcomes with Syntax score in patients with Non-ST segment elevation myocardial infarction: a retrospective study. Int J Gen Med. 2023;16:2595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li W, Song Y. Red cell distribution width to albumin ratio is a risk factor for atrial fibrillation in subjects hospitalized with coronary angiography. BMC Cardiovasc Disord. 2024;24(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang YW, Yin XS, Li ZP. Association of the systemic immune-inflammation index (SII) and clinical outcomes in patients with stroke: a systematic review and meta-analysis. Front Immunol. 2022;13:1090305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Cao D, Huang Y, Xiong Q, Tan D, Liu L, Lin T, Wei Q. The prognostic and clinicopathological significance of systemic Immune-inflammation index in bladder Cancer. Front Immunol. 2022;13:865643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karakayali M, Altunova M, Yakisan T, Aslan S, Omar T, Artac I, Ilis D, Arslan A, Cagin Z, Karabag Y, Rencuzogullari I. The relationship between the systemic Immune-inflammation index and ischemia with non-obstructive coronary arteries in patients undergoing coronary angiography. Arq Bras Cardiol. 2024;121(2):e20230540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arques S. Serum albumin and cardiovascular disease: state-of-the-art review. Ann Cardiol Angeiol (Paris). 2020;69(4):192–200. [DOI] [PubMed] [Google Scholar]
- 32.Huang Y, Deng W, Pan X, Liu M, Zhong Z, Huang Q, Li T. The relationship between platelet to albumin ratio and disease activity in axial spondyloarthritis patients. Mod Rheumatol. 2022;32(5):974–9. [DOI] [PubMed] [Google Scholar]
- 33.Crowley SD. The cooperative roles of inflammation and oxidative stress in the pathogenesis of hypertension. Antioxid Redox Signal. 2014;20(1):102–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Medina-Leyte DJ, Zepeda-García O, Domínguez-Pérez M, González-Garrido A, Villarreal-Molina T, Jacobo-Albavera L. Endothelial dysfunction, inflammation and coronary artery disease: potential biomarkers and promising therapeutical approaches. Int J Mol Sci. 2021;22(8):3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wrigley BJ, Lip GY, Shantsila E. The role of monocytes and inflammation in the pathophysiology of heart failure. Eur J Heart Fail. 2011;13(11):1161–71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.