Abstract
Background
There is currently no practice-based, multicenter database of poisoned patients admitted to intensive care units (ICUs). The INTOXICATE study, endorsed by the ESICM and EAPCCT, aimed to determine the rate of eventful admissions among acutely intoxicated adult ICU patients.
Methods
Ethical approval was obtained for this multicenter, prospective observational study, and data-sharing agreements were signed with each participating center. An electronic case report form was used to collect data on patient demographics, exposure, clinical characteristics, investigations, treatment, and in-hospital mortality data. The primary outcome, ‘eventful admission’, was a composite outcome defined as the rate of patients who received any of the following treatments in the first 24 h after the ICU admission: oxygen supplementation with a FiO2 > 40%, mechanical ventilation, vasopressors, renal replacement therapy (RRT), cardiopulmonary resuscitation, antidotes, active cooling, fluid resuscitation (> 1.5 L of intravenous fluid of any kind), sedation, or who died in the hospital.
Results
Seventy-eight ICUs, mainly from Europe, but also from Australia and the Eastern Mediterranean, participated. A total of 2,273 patients were enrolled between November 2020 and June 2023. The median age of the patients was 41 years, 72% were exposed to intoxicating drugs. The observed rate of patients with an eventful ICU admission was 68% (n = 1546/2273 patients). The hospital mortality was 4.5% (n = 103/2273).
Conclusions
The vast majority of patients survive, and approximately one third of patients do not receive any ICU-specific interventions after admission in an intensive care unit for acute intoxication. High-quality detailed clinical data have been collected from a large cohort of acutely intoxicated ICU patients, providing information on the pattern of severe acute poisoning requiring intensive care admission and the outcomes of these patients.
Trial registration: OSF registration ID: osf.io/7e5uy.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-024-05096-7.
Keywords: Toxicology, Poisoning, Intensive care units, Critical care outcomes, Database management systems
Background
The severity of poisoning depends on many factors, such as the type and dose of xenobiotics, patient characteristics (age, sex, comorbidities), clinical features at hospital presentation (level of consciousness, blood pressure, pulse rate, respiratory rate, temperature), time to treatment, poisoning circumstances (intentional or accidental; coingestions) and/or laboratory findings (electrolyte imbalances, coagulation abnormalities, renal function etc.) [1–5]. In addition to these predictors, the ICU mortality rate after poisoning also depends upon the class of medications/chemicals to which a patient is being exposed (e.g. opioids, sedatives, street drugs, etc.…), which differs between low- and middle-income countries and countries such as the USA, Australia or European countries. ICU mortality in the USA and European ICUs is ranging from 0 to 6% depending on the study [4, 6–9].
Previously published studies have reported conflicting data on ICU admission and mortality rates. Comparisons between these studies is difficult because they often lacked common methodology and definitions, were relatively small single-center retrospective studies, or missed information on exposure and on treatment. Additional file 1: Table S1 in the Supplement contains information on the source, number of centers, population, age range, number of patients, most prevalent intoxications, important findings and limitation per study.
The limitations of these previous studies and the lack of multinational database of ICU patients with severe poisonings in Europe were the basis for our prospective study. The INTOXICATE study aims to collect data on admissions to ICUs after acute poisoning in Europe and other continents to determine the rate of eventful admissions among acutely intoxicated adult ICU patients and to provide information on the prognosis of these patients.
Methods
Study design, registration and approval
This prospective multicenter observational cohort study was prospectively registered in an Open Science Framework (OSF) (OSF registration ID: osf.io/7e5uy). The accredited Medical Research Ethics Committee of the University Medical Centre Utrecht (UMCU) did not consider the Dutch Medical Research Involving Human Subjects Act to be applicable to this study (ethics reference number: 20-495/C). The original name was the "TOXIC-Europe study", but the name was changed to the INTOXICATE-study in October 2021 at the request of researchers involved in the Toxicology Investigators Consortium (ToxIC) run by the American College of Medical Toxicology, to avoid confusion.
Setting
ICU physicians in Europe and other continents were invited to participate in the INTOXICATE study through the European Association of Poison Centres and Clinical Toxicologists (EAPCCT) [10] and the European Society of Intensive Care Medicine (ESICM) [11]. The eligibility criteria for ICUs were that they were university affiliated-, community teaching-, and community non-teaching hospitals in Europe or other continents. The ICU could be medical, surgical, specialized in toxicology or any other specialty, or mixed. An ICU was defined as a unit where a patient can be endotracheally intubated and mechanically ventilated. Therefore, high-dependency units (HDUs) or high-care units (HCUs) that can mechanically ventilate patients, were considered an ICU in this study. Ethics approval and signing a data sharing contract were mandatory.
Data were collected between 1st November 2020 and 30th June 2023. A list of collaborators is provided in the Acknowledgments section. The study was managed by a central coordinating team supervising the national coordinators. All participating units provided either local research ethics committee approval or a waiver of consent. A data-sharing contract had to be signed between the participating unit and the coordinating center.
Patients
The patient inclusion criteria were adult patients (aged 18 years or older); patients admitted to the ICU from an emergency department, ambulance, or ward; intoxication (due to poisoning) as the main reason for ICU admission; and patients who stayed in the ICU for four hours or more. Patients were excluded if they were younger than 18 years; admitted to the ICU because of another serious comorbidity (e.g., trauma from a car accident while intoxicated as the management, outcome and duration of admission were likely to be dictated by the comorbidity rather than the intoxication); and an ICU stay of less than four hours. Toxicity was defined as the occurrence of any toxic effect to humans following a single or repeated exposure to a mixture of natural or synthetic substances available on the market or present in the environment. Pure ethanol intoxication was covered by the exposure definition. Informed consent of the participating patients was either required or not, depending on the country and/or the unit.
Variables
The primary outcome, ‘eventful ICU admission’, was a composite outcome defined as the rate of patients who received any of the following treatments in the first 24 h after the ICU admission: oxygen supplementation with a FiO2 > 40%, mechanical ventilation, vasopressors, renal replacement therapy (RRT), cardiopulmonary resuscitation, antidotes, active cooling, fluid resuscitation (> 1.5 L of intravenous fluid of any kind), sedation, or who died in the hospital.
Exposure variables were the exposure exact name, category, dose, and route. Human medications were categorized according to the underlying pharmacological group based on [4]: alcohol (ethanol, other alcohols); analgesics; antidepressants (cyclic antidepressants, lithium); street drugs (opiates, cocaine, amphetamine); sedatives (hypnotics, antipsychotic, benzodiazepines); ‘other poisons’ (carbon monoxide, arsenic, cyanides); other toxins; and mixed intoxications (combination of two or more sub-types of intoxication).
Data were collected on potential predictors (type of units, unit size, country, patient’s age, sex, comorbidities, possible second reason for ICU admission, vital signs, investigations (including ECG).
Data sources
The data entered by local investigators included only information that would have been collected as part of routine clinical care. Local investigators reported only pseudoanonymized data. The data were entered into two study-specific databases (one for units and one for patients) developed in Castor EDC (Electronic Data Capture) [12]. Local investigators could access Castor through an account that required two-factor authentication (2FA). Local investigators entered their data into the database for patients identified as eligible, usually after hospital discharge. Data from Denmark were imported into Castor EDC in a single block (all patients from all Danish units at the same time) because Danish investigators collected patient data using the Redcap system; this made it easier for the Danish investigators to obtain the necessary institutional approval.
Bias
Standard definitions of the variables were provided on the study website. To ensure complete case ascertainment, any missing or inconsistent data were identified at the end of the overall study data collection period and the local investigator was contacted to update/provide the data. We predicted that there would be enough eligible patients in one year. However, the COVID-19 pandemic hit almost immediately after the start of the study, forcing us to extend the study by a further year and eight months.
Study size
Before the study began, we calculated the sample size, based on the hypothesized proportion of outcome in the population of interest, using the following formula:
Taking the values p = 6.5% (based on [4]); z = 1.96 for a 95% level of confidence; d = 0.065/2 (the allowable error); a correction factor DE = 7.65 for 20 clusters (the 20 countries where the study would be conducted, we get n = 1691. We applied a non-response rate of 10%, which resulted in n = 1691/0.9 = 1879 patients.
Quantitative variables
Quantitative variables concerning the ICUs were the number of ICU beds, the total number of ICU admissions in the last year, and the number of ICU admissions related to poisoning in the last year. All were grouped in categories.
Patient’s age, Body Mass Index (BMI), time elapsed between exposure and hospital admission, number of exposures, systolic blood pressure, heart rate, body temperature, SaO2, arterial pH, potassium, lactate, leucocytes, serum creatinine were considered as quantitative variables. None of them were categorized. The Glasgow Coma Score was categorized in four categories (GCS ≥ 14; GCS > 9 and < 14; GCS > 6 and ≤ 9; GCS < 6).
Statistical methods
Quantitative variables related to ICUs are expressed as numbers and percentages by category. Continuous patient data are expressed as median ± interquartile range. Patient categorical data are expressed as numbers (percentages). Rates were calculated as the number of outcomes divided by the total number of included patients, with the corresponding 95% confidence interval (CI). Rates were calculated before and after exclusion of patients who received mechanical ventilation, vasopressors or cardiopulmonary resuscitation before ICU admission.
Patients with missing data were identified. Percentages were calculated for those with available data, and the denominator with missing data removed is reported throughout. When patients were transferred to another ICU, this second ICU was contacted by the local investigator to obtain the patient data.
In a post-hoc analysis, we used two alternative definitions of ‘eventful ICU admission’ in order to compare our findings with previous studies [4, 13]. The alternative definitions of “eventful ICU admission” included fewer ICU treatments. In alternative definition 1, according to [13], an eventful ICU admission was defined as having received mechanical ventilation and/or vasopressors and/or renal replacement therapy (RRT) and/or cardiopulmonary resuscitation in the first 24 h in ICU or who died in-hospital. In alternative definition 2, according to [4], eventful ICU admission was defined as having received mechanical ventilation and/or vasopressors and/or cardiopulmonary resuscitation in the first 24 h in the ICU, or having died in hospital (similar to alternative definition 1 except that RRT was not considered).
We hypothesized that the rate of eventful admission (with alternative definition 1 and definition 2) was greater than previously reported in the two studies [4, 13]. A one-sample z test was used to test the difference in outcome in this study compared with the rate reported in each study (15.4% in [13] and 6.5% in [4]).
We also performed two sensitivity analyses. First, to mitigate the potential influence of the heterogeneity in enrollment rates between ICUS, we repeated the main analysis after including only units that included at least 80% of the patients admitted to their unit in the study. Second, to minimize the potential influence of a mandatory informed consent, we repeated the main analysis to units where an informed consent was not mandatory.
Statistical analyses were carried out in SPSS Statistics 29.0 and/or R studio version 2023.06.2 for Windows (R version 4.2.2.). The STROBE checklist was used in the preparation of this manuscript following the EQUATOR guidelines.
Results
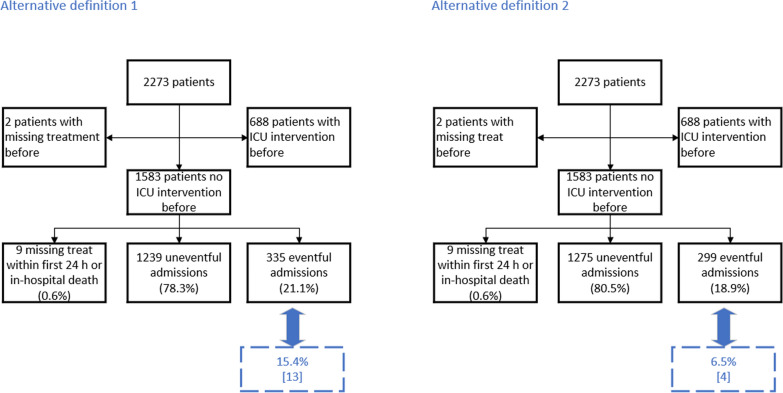
During the study period, 237 units contacted us (Fig. 1), yet only 78 ICUs that met the inclusion criteria contributed data to the INTOXICATE study (Table 1). Data collection was complicated by various technical challenges, including the COVID-19 pandemic, the data sharing agreement, and the different application of the General Data Protection Regulation (GDPR) in European countries, which may or may not require patient informed consent (Additional file 1: Table S2).
Fig. 1.
Study Flow Diagram for units. Data entered by local investigators (black outlines), reasons for exclusion (purple), and study phase (blue) are represented
Table 1.
Location of the INTOXICATE intensive care units (ICUs) (N = 78)
| City | Institution | Unit |
|---|---|---|
| Australia | ||
| Brisbane | Redcliffe Hospital | Intensive care unit |
| Austria | ||
| Salzburg | Paracelsus Medical University Salzburg | Medical intensive care unit |
| Belgium | ||
| Ghent | Ghent University Hospital | Intensive care unit |
| Brussels | Cliniques Universitaires St Luc | SIM/SIT |
| Ottignies | Clinique Saint Pierre Ottignies | Intensive care unit |
| Brugge | AZ Sint-Jan Brugge-Oostende AV | Intensieve zorgen |
| Charleroi | CHU Charleroi | Medico surgical ICU |
| Brunei Darussalam | ||
| Bandar Seri Begawan | Hospital RIPAS | Critical care medicine |
| Croatia | ||
| Split | University Hospital of Split | Internal medicine department, division of emergency and intensive medicine |
| Denmark | ||
| Copenhagen | Bispebjerg Hospital | Department of anaesthesia and intensive care |
| Herlev | Herlev Hospital | Afdeling for bedøvelse, operation og intensiv behandling |
| Roskilde | Zealand University Hospital | Intensive care unit I 12, Roskilde. dept. of anesthesiology |
| Køge | University Hospital Zealand—Køge | Intensive care unit, SUH Køge |
| Odense | OUH—Odense University Hospital | Department of intensive care |
| Viborg | Viborg Regional Hospital | Intensive care unit |
| Aalborg | Aalborg University Hospital | Anesthesia and intensive care department |
| Slagelse | Slagelse Hospital | Department of anaesthesia and intensive care |
| Egypt | ||
| Tanta | TANTA University Emergency Hospital | Emergency medicine and traumatology intensive care unit |
| Ismailia | Suez Canal University Hospitals (SCUH) | Department of anaesthesia and intensive care |
| Germany | ||
| Munich | Rechts der Isar Hospital | Toxikologische intensivstation |
| Essen | University Hospital Essen | Anästhesiologische intensivstation IT 2 |
| Greece | ||
| Thessaloniki | Saint Paul (“Agios Pavlos”) General Hospital | Intensive care unit |
| Iraq | ||
| Najaf | Al-Sader Medical city Teaching Hospital | Intensive care unit |
| Italy | ||
| Milan | Humanitas Research Hospital | Department of anesthesiology and intensive care |
| Jordan | ||
| Amman | Jordan University Hospital, Amman | Medical intensive care unit |
| Amman | Islamic hospital | Surgical ICU |
| Amman | Amman Field Hospital | Intensive care unit |
| Lithuania | ||
| Vilnius | Republic Vilnius University hospital | Toxicology Centre |
| Netherlands | ||
| Utrecht | University Medical Center Utrecht | Department of intensive care medicine |
| Utrecht | Diakonessenhuis Utrecht | Intensive care unit |
| Enschede | Medisch Spectrum Twente | Intensive care center |
| Den Haag | Haaglanden Medisch centrum | Intensive care unit |
| Leeuwarden | Medisch Centrum Leeuwarden | Afdeling intensive care |
| Amsterdam | Onze Lieve Vrouwe Gasthuis (OLVG) hospital | Intensive care |
| Arnhem | Rijnstate Hospital | Intensive care unit |
| Maastricht | Maastricht University Medical Center + | Intensive care |
| Rotterdam | Franciscus Gasthuis & Vlietland | Afdeling intensive care |
| Amsterdam | Antoni van Leeuwenhoek ziekenhuis | Intensive care |
| Groningen | University Medical Center Groningen | Department of critical care |
| Rotterdam | Maasstad Hospital | Intensive care unit |
| Rotterdam | Ikazia Ziekenhuis | Intensive care unit |
| Deventer | Deventer Ziekenhuis | Intensive care unit |
| Portugal | ||
| Lisbon | Hospital de São Francisco Xavier, Unidade Local de Saúde de Lisboa Ocidental, EPE. Lisboa, Portugal | Unidade de cuidados intensivos polivalente |
| Vila Nova de Gaia | Centro Hospitalar de Vila Nova de Gaia, ULS Gaia e Espinho, Vila Nova de Gaia, Portugal | Serviço de medicina intensiva polivalente |
| Santiago do Cacém | Hospital do Litoral Alentejano, Unidade Local De Saúde de Lisboa Ocidental, EPE, Santiago do Cacém, Portugal | Serviço de medicina intensiva |
| Romania | ||
| Bucharest | Clinical Emergency Hospital Bucharest | Anesthesiology and intensive care—toxicology |
| Cluj | Clinical Emergency County Hospital Cluj-Napoca | Anaesthesia and intensive care I department |
| Spain | ||
| Valencia | Consorcio Hospital General Universitario | UCI anestesia |
| Santiago de Compostela | University Clinic Hospital of Santiago de Compostela | Intensive care unit, intensive care medicine department |
| Tortosa | Hospital Verge de la Cinta | Servicio de medicina intensiva |
| Zaragoza | Hospital Universitario Lozano-Blesa | Unidad de cuidado intensivos |
| Girona | Hospital Santa Caterina de Salt | Unidad de cuidados intensivos |
| Girona | Hospital Universitario Dr Josep Trueta | Unidad de cuidados intensivos |
| Octubre Madrid | Hospital Universitario 12 de Octubre | Trauma and emergency ICU. Intensive care medicine service |
| Valencia | IMED Hospital Valencia | UCI |
| Huesca | University San Jorge Hospital | Intensive care medicine |
| Granollers | Hospital General Granollers | Intensive care unit |
| Valladolid | Hospital Universitario Río Hortega | Servicio de medicina intensiva, unidad 1 |
| Valladolid | Hospital Universitario Río Hortega | Servicio de medicina intensiva, unidad 2 |
| Sudan | ||
| Khartoum-EastNile | East Nile (Sharg Alneel) Hospital | Intensive care unit |
| Sweden | ||
| Stockholm | South hospital | Intensive care unit |
| Stockholm | Capio St Görans hospital | Intensivvårdsavdelningen (IVA) |
| Lund | Skånes University Hospital Lund | Intensivvårdsavdelning lund |
| Hudiksvalls | Hudiksvalls sjukhus | ICU Hudiksvall |
| Norrtälje | Norrtälje Hospital | Intensive care unit |
| Malmö | Skånes University Hospital, Malmö | Intensive care unit |
| Turkey | ||
| Istanbul | Dr. Lutfi Kirdar Training and Research Hospital General | General ICU |
| Ankara | Hacettepe University Faculty of Medicine, Ankara | Medical intensive care unit |
| Istanbul | Kanuni Sultan Suleyman Education and Training Hospital | Anesthesiology intensive care unit (Reanimation) |
| Giresun | Giresun Training and Research Hospital | Reanimation |
| Sakarya | Sakarya University Faculty of Medicine | Department of internal medicine-intensive care unit |
| Trabzon | Karadeniz Technical University, Farabi Hospital | Anesthesia ICU-2 |
| Kahramanmaraş | Kahramanmaraş Sütçü İmam University, Faculty of Medicine, Training and Research Hospital | Anesthesiology intensive care unit (Reanimation) |
| Adana | Seyhan Public Hospital | Mixed-intensive care unit |
| Ankara | Ataturk Sanatorium Training and Research Hospital | General intensive care unit |
| United Kingdom | ||
| Nottingham | Nottingham University Hospitals NHS Trust | Intensive care unit |
| London | Guy’s and St Thomas’ NHS Foundation Trust | Intensive care unit |
| Cramlington | Northumbria Healthcare NHS foundation trust | Northumbria specialist emergency care hospital |
Characteristics of intensive care units
Table 2 shows the characteristics of the units. The majority (N = 49, 62%) were university-affiliated ICUs. The size of ICUs was also usually less than 30 beds, and the number of admissions was usually less than 2000 per year per unit. Most units had fewer than 60 poisoning-related admissions in the year before the study. In the majority of ICUs, the doctors who wrote the orders (laboratory tests and medication prescriptions) were specialists in intensive care medicine (62%), and 42% of the units had physicians certified in medical toxicology.
Table 2.
Characteristics of intensive care units (ICUs) (N = 78 units)
| Parameter | N (%) |
|---|---|
| Institution/hospital type | |
| University affiliated | 49 (62) |
| Community teaching | 22 (28) |
| Community nonteaching | 6 (8) |
| Private sector–teaching hospital | 1 (1) |
| Number of ICU beds | |
| < 10 | 17 (22) |
| 10–15 | 20 (25) |
| 15–30 | 24 (30) |
| 30–45 | 10 (13) |
| > 45 | 7 (9) |
| Total number of ICU admissions in the last year | |
| < 500 | 18 (23) |
| 500–1000 | 25 (32) |
| 1000–2000 | 25 (32) |
| 2000–3000 | 6 (8) |
| > 3000 | 4 (5) |
| ICU admissions related to poisoning last year | |
| < 30 | 38 (48) |
| 30–60 | 21 (27) |
| 60–120 | 12 (15) |
| 120–180 | 1 (1) |
| > 180 | 6 (8) |
| What kind of doctors write orders in the ICU? | |
| Non-IC doctors can write orders | 22 (28) |
| Only IC doctors write orders | 49 (62) |
| Other doctors | 5 (6) |
| Unknown | 2 (3) |
| Specialtiesa | |
| Medical | 71 (90) |
| Toxicological | 33 (42) |
| Respiratory or pulmonary | 61 (77) |
| Surgical | 56 (71) |
| Trauma | 44 (56) |
| Cardiothoracic surgery | 15 (19) |
| Cardiac or coronary | 25 (32) |
| Transplantation | 13 (16) |
| Burns | 6 (8) |
| Neurological and/or neurosurgical | 40 (51) |
| Otherb | 11 (14) |
| Informed consent needed | |
| No | 33 (42) |
| Yes | 45 (57) |
No missing values in the parameters related to the ICUs
aTotal greater than 78 because most ICUs have multiple specialties
b‘Addiction care’ (n = 1); ‘ECMO’ (Extra Corporeal Membrane Oxygenation) or ‘renal disease’ (n = 2); ‘General’ or ‘mixed’ or ‘multidisciplinary’ or ‘no specialty’ (n = 5); ‘Obstetrics and gynecology’ (n = 1); ‘Oncology’ or ‘Palliative’ (n = 2)
Patient characteristics
A total of 2,273 patients were enrolled during this extended data collection period. The Netherlands was the largest contributor, followed by Denmark and Spain. Table 3 shows the characteristics of the patients. The median patient age was 41 years (IQR 28–56) and slightly more women were affected (53.2% women). Most patients presented a comorbidity, either psychiatric and/or somatic; fifty-nine percent of patients had a coexisting psychiatric illness (other than addiction)diabetes was the most common somatic comorbidity. Most patients were admitted from the emergency department (92.5%), a second reason for ICU admission was recorded in 16.2% of the patients (Table 3).
Table 3.
Collected patient data with missing values per variable (n = 2,273 patients)
| Parameter | N = 2,273 (100%) | Missing value N (%) |
|---|---|---|
| Age, median (IQR) | 41 (28;56) | 0 (0) |
| Sex | 4 (0.2) | |
| Female, n (%) | 1209 (53.2) | |
| Male, n (%) | 1054 (46.4) | |
| Non-binary, n (%) | 6 (0.3) | |
| BMI, median (IQR) | 24.98 (21.95;29.30) | 212 (9.3) |
| Comorbidities, n (%) | ||
| Psychiatric comorbidity, n (%) | ||
| Other than addictiona, n (%) | 1338 (58.9) | |
| Addictionb, n (%) | 511 (22.5) | |
| Somatic comorbidity, n (%) | ||
| Diabetes, n (%) | 227 (10) | |
| Chronic obstructive pulmonary disease, n (%) | 126 (5.5) | |
| Heart Failurec, n (%) | 67 (2.9) | |
| Metabolic or endocrine disease, n (%) | 56 (2.5) | |
| Chronic kidney disease, n (%) | 46 (2) | |
| Source of ICU admission | 0 (0) | |
| Emergency department, n (%) | 2103 (92.5) | |
| Ward, n (%) | 117 (5.1) | |
| Other ICU, n (%) | 53 (2.3) | |
| No second reason for admission, n (%) | 1899 (83.5) | 5 (0.2) |
| Second reason for admission, n (%) | 369 (16.2) | |
| Time from exposure to presentation (h), n (%) | 8 (0.4) | |
| Known, n (%) | 667 (29.3) | |
| Estimated, n (%) | 481 (21.2) | |
| Unknown, n (%) | 1117 (49.1) | |
| Time from exposure to presentation (among known or estimated times, in h), median (IQR) | 4 (2.8; 8) | 30 (2.6) |
| Poisoning-related factors | ||
| Intent of poisoning | 8 (0.4) | |
| Unintentional, n (%) | 272 (12.0) | |
| Intentional, n (%) | 1993 (87.7) | |
| Number of exposures, median (IQR) | 2 (1; 3) | 24 (1.1) |
| Category of substances | 56 (2.5) | |
| Combination of two or more intoxications types | 1131 (49.8) | |
| Sedatives, n (%) | 241 (10.6) | |
| Street drugs, n (%) | 203 (8.9) | |
| Alcohols, n (%) | 123 (5.4) | |
| Analgesics, n (%) | 105 (4.6) | |
| Antidepresseurs, n (%) | 89 (3.9) | |
| Other poisons (e.g., CO, arsenic, cyanide), n (%) | 18 (0.8) | |
| Toxins not otherwise specified, n (%) | 307 (13.5) | |
| Initial vital signs | ||
| Systolic Blood pressure (mmHg), median (range) | 115 (95; 139) | 18 (0.8) |
| Heart rate (beat/mn), median (range) | 95 (74; 115) | 6 (0.3) |
| Respiratory rate, median (IQR) | 17 (12; 22) | 62 (2.7%) |
| Temperature (Celsius degree), median (IQR) | 36.3 (35.7; 37) | 35 (1.5) |
| Glasgow Coma Score (GCS) | 101 (4.4) | |
| GCS available, n (%) | 2089 (91.9) | |
| GCS not available because the patient was intubated or sedated, n (%) | 83 (3.7) | |
| GCS ≥ 14 | 696 (30.6) | |
| GCS > 9 and < 14 | 411 (18.1) | |
| GCS > 6 and ≤ 9 | 360 (15.8) | |
| GCS < 6 | 622 (27.4) | |
| Most common signs or symptoms | 0 (0) | |
| Neurological signs | ||
| Altered consciousness | 979 (43.1) | |
| Coma | 747 (32.9) | |
| Agitation | 294 (12.9) | |
| Confusion | 250 (11.0) | |
| Miosis | 155 (6.8) | |
| Seizures | 133 (5.9) | |
| Cardiologic signs or symptoms | 0 (0) | |
| Palpitations | 108 (4.8) | |
| Hypotension | 107 (4.7) | |
| Tachycardia | 86 (3.8) | |
| Bradycardia | 63 (2.8) | |
| Cardiac arrest or asystole | 35 (1.5) | |
| Chest pain | 32 (1.4) | |
| Gastro-intestinal signs or symptoms | 0 (0) | |
| Vomiting, n (%) | 359 (15.8) | |
| Nausea, n (%) | 227 (10.0) | |
| Abdominal pain, n (%) | 141 (6.2) | |
| Diarrhea, n (%) | 64 (2.8) | |
| Respiratory signs | 1 (0.04) | |
| Respiratory depression, n (%) | 339 (14.9) | |
| Bradypnea, n (%) | 274 (12.1) | |
| Tachypnea, n (%) | 157 (6.9) | |
| Apnea, n (%) | 134 (5.9) | |
| Initial blood performed, n (%) | ||
| Arterial gas | 1598 (70.3) | |
| SaO2 in %, median (IQR) | 95 (91; 98) | 7 (0.4) |
| Arterial pH, median (IQR) | 7.34 (7.27; 7.40) | 10 (0.6) |
| Electrolytes measured, n (%) | 2169 (95.4) | |
| Potassium (mmol/L), median (IQR) | 3.87 (3.50; 4.21) | 36 (1.7) |
| Lactate measured, n (%) | 1645 (72.4) | |
| Lactate (mmol/L), median (IQR) | 1.89 (1.0; 3.1) | 2 (0.1) |
| Leucocytes measured, n (%) | 1940 (85.3) | |
| Leucocytes (109/L), median (IQR) | 9.5 (7.0; 12.9) | 11 (0.6) |
| Creatinine measured, n (%) | 2101 (92.4) | |
| Creatinine (micromole/L), median (IQR) | 72.5 (59.8; 93.2) | 11 (0.5) |
| Blood toxicology screening performed, n (%) | 949 (41.8) | |
| Blood toxicology screening performed and positive, n (% among performed) | 549 (57.9) | 2 (0.2) |
| Urine toxicology screening performed, n (%) | 688 (30.3) | |
| Urine toxicology screening performed and positive, n (% among performed) | 520 (75.6) | 2 (0.3) |
| ECG performed, n (%) | 1982 (87%) | 5 (0.2) |
| ECG with abnormalities, n (%) | 498 (25.1) | 43 (2.2) |
| Care measures before admission | 2 (< 0.1) | |
| Mechanical ventilation before, n (%) | 647 (28.5) | |
| Antidote before, n (%) | 670 (29.5) | |
| Gastro-intestinal decontamination before, n (%) | 550 (24.2) | |
| Oxygen with FiO2 > 0.4 before, n (%) | 364 (16) | |
| Vasopressors before, n (%) | 66 (2.9) | |
| Cardiopulmonary resuscitation before, n (%) | 61 (2.7) | |
| Intensive care measures first 24H, n (%) | 7 (0.3) | |
| Mechanical ventilation first 24H, n (%) | 809 (35.6) | |
| Vasopressors first 24H, n (%) | 447 (19.6) | |
| Calming medication first 24H, n (%) | 379 (16.7) | |
| Renal Replacement Therapy first 24H, n (%) | 132 (5.8) | |
| Serum alkalinization first 24H, n (%) | 121 (5.3) | |
| Active cooling first 24H, n (%) | 22 (1.0) | |
| Cardiopulmonary resuscitation first 24H, n (%) | 13 (0.6) | |
| ICU mortality, n (%) | 85 (3.7) | 11 (0.5) |
| In-hospital mortality, n (%) | 103 (4.5) | 11 (0.5) |
| Mortality 30 days after ICU admission, n (%) | 117 (5.1) | 243 (10.7) |
aIncluding depression, borderline personality disorder, schizophrenia, bipolar disorders, eating disorders, posttraumatic stress disorder, anxiety and neurodevelopmental disorders including deficits in intellectual functioning
ICU intensive care unit, IQR interquartile range, SaO2 oxygen saturation, FiO2 fraction of inspired oxygen
bAddiction as defined in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5: American Psychiatric Association, 2013), including gambling or sex addiction
cHeart failure including cardiomyopathy, severe heart valve or coronary diseases with angina or symptoms at rest or minimal physical effort such as changing clothing and day-to-day care (New York Heart Association or NYHA Class VI)
Exposure
The vast majority of the patients (72%) were exposed to intoxicating drugs, and almost a quarter were exposed to alcohol, most often mixed with another drug. The group of mixed intoxications accounted for 1131 cases (49.8%) in all patients (Table 3). When considering isolated intoxications, sedatives (10.6%) and street drugs (8.9%) were most frequently used.
Clinical features
Neurological signs and symptoms were the most common on admission, with the top three most common neurological symptoms being altered consciousness (N = 979 patients, 43% of admissions), coma (N = 747 patients, 32.9% of admissions), and agitation (N = 294 patients, 12.9% of admissions). Respiratory and gastro-intestinal signs were also frequently observed (at least one sign observed in 41.1% and 23.5% of admission, respectively). The most frequently observed cardiologic signs or symptoms were palpitations (4.8%) and hypotension (4.7%).
Primary outcome and in-hospital mortality
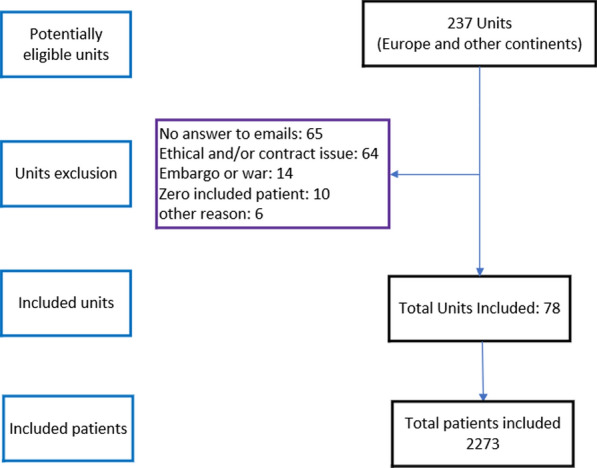
The observed rate of patients with an eventful ICU admission was 68% (95% CI: 64.6%; 71.4%) (n = 1546/2273 patients) in all patients. Six hundred and eighty-eight patients (n = 688/2273, 30.3%) received an ICU intervention (CPR or mechanical ventilation or vasopressors for at least one hour) prior to their ICU admission, and for 2 patients, it was unknown whether they had had a treatment before their ICU admission (n = 2/2273, 0.1%). The observed rate of patients with an eventful admission) was 56.5% (95% CI: 53%; 60%) (n = 895/1583 patients) after exclusion of patients who received an IC intervention before their ICU admission (Fig. 2). For 9 patients, the treatment received in ICU was missing (n = 9/1583, 0.6%).
Fig. 2.
Study Flow Diagram for patients in the main analysis. An “eventful ICU admission” was defined as receiving an ICU intervention within the first 24 h after ICU admission or in-hospital death. An ICU intervention was defined as receiving any of the following treatments: oxygen supplementation with a FiO2. 40%, mechanical ventilation, vasopressors, renal replacement therapy (RRT), cardiopulmonary resuscitation, antidote, active cooling, fluid resuscitation (> 1.5 L of intravenous fluid of any kind), and sedation. ICU intervention before ICU admission was defined as receiving mechanical ventilation or cardiopulmonary resuscitation or vasopressors (over at least 1 h) before ICU admission
The majority of patients survived to hospital discharge, with 3.7% (n = 85/2273 patients) dying in the ICU and 0.8% (n = 18/2273 patients) dying in the ward following discharge from the ICU, resulting in an in-hospital mortality of 4.5% (n = 103/2273) (95% CI: 3.7%; 5.4%).
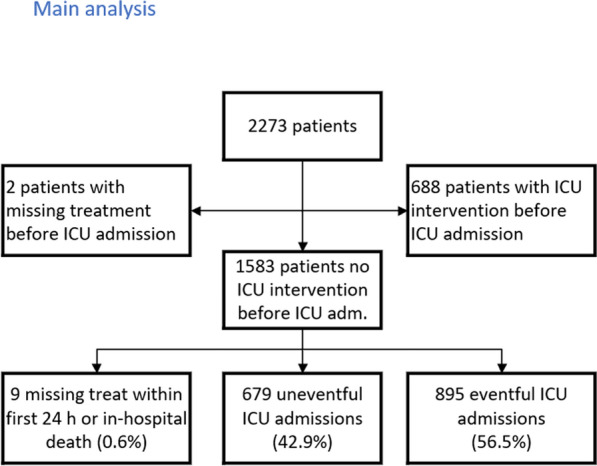
With the post-hoc analysis, the rate of ICU eventful admission after exclusion of the patients who received an ICU intervention before their ICU admission was 21.1% (n = 335/1583) when alternative definition 1 was used (Fig. 3, left panel). This rate was significantly greater than 15.4%, the rate reported previously in [13] (z-statistic = 6.47, p < 0.001). When alternative definition 2 was used, the rate of ICU eventful admission after exclusion of the patients who received an ICU intervention before their ICU admission was 18.9% (n = 299/1583) (Fig. 3, right panel). This rate was significantly greater than 6.5%, the rate of ICU eventful admission reported in [4] (z-statistic = 20.1; p < 0.001).
Fig. 3.
Study Flow Diagram for patients in the post-hoc analysis (using alternative definitions 1 and 2 for “eventful ICU admission”). In alternative definition 1, an “eventful admission” was defined as receiving mechanical ventilation and/or vasopressors and/or renal replacement therapy and/or cardiopulmonary resuscitation in the first 24 h after ICU admission, or in-hospital death (as in [13]. In alternative definition 2, only receiving mechanical ventilation and/or vasopressors, or in-hospital death were included in the definition of an “eventful ICU admission” (as in [4]. ICU intervention before ICU admission was defined as receiving mechanical ventilation or cardiopulmonary resuscitation or vasopressors (over at least 1 h) before ICU admission
When including only the units that included at least 80% of the patients admitted due to intoxication to their unit in the study, the rate of eventful ICU admission was 68.7% (n = 574/835) before exclusion of the patients who received an ICU treatment before their ICU admission (versus 68% [95% CI: 64.6%; 71.4%] in the 2273 patients. The in-hospital mortality rate was 4.2% (n = 35/835) versus 4.5% [95% CI: 3.7%; 5.4%] in the 2273 patients.
When including only the units where an informed consent was not mandatory, the rate of eventful ICU admission was 71.6% (n = 756/1056 patients) before exclusion of the patients who received an ICU treatment before their ICU admission (versus 68% [95% CI: 64.6%; 71.4%] in the 2273 patients). The in-hospital mortality rate was 4.5% (n = 48/1056) versus 4.5% [95% CI: 3.7%; 5.4%] in the 2273 patients.
Discussion
The primary findings of our study show that almost all patients presenting with acute intoxication had comorbidities, with psychiatric comorbidities being the most common. The majority of intoxications in our study involved human medications. The overall mortality rate was low (4.5%). About two thirds of the patients admitted to the ICU received ICU-specific treatments, but this percentage drops to about 56.5% when excluding patients who had already received an ICU intervention before admission.
Our study confirms several findings from previous research. Consistent with previous studies, we observed a slightly higher number of females than males among the intoxicated patients [8]. The predominance of mixed intoxication [7, 13–17] and intoxicating drugs as the cause of intoxication [7, 9, 16, 18–20] is also in line with the existing literature. The low mortality rates both in the ICU (3.7%) and in the hospital (4.5%) are in accordance with the mortality rates reported in the literature. The ICU mortality rate ranged from 0.4 to 5.9% when considering studies with more than 100 intoxicated patients (Table S1) [4, 7–9, 19–22], while the in-hospital mortality rate reported in the literature ranged from 0.7 to 6.7% [1, 4, 9, 13, 14, 18, 20, 22].
However, our study differs significantly in the proportion of intoxicated patients admitted to the ICU who required mechanical ventilation, vasopressors or died in hospital. We found this proportion to be significantly higher than that reported in a French study that also included renal replacement therapy (RRT) as part of ICU-specific treatment (15.4%)[13] and a Dutch study that did not include RRT (6.5%) [4]. This suggests that our cohort had a higher severity of intoxication, as our criteria for ICU treatment were similar to prior studies [4, 13].
The strengths of our study are many. We achieved a high level of data completeness and quality, with very few missing values. Our prospective study design, in contrast to the retrospective nature of most previous studies, increases the reliability of our findings. The international scope of our study, covering approximately 20 countries, increases the generalizability of our findings. With 2,273 admissions, the sample size of our study is robust and exceeds many previous single-center or single-country studies. In addition, our inclusive criteria, covering all types of poisoning rather than focusing solely on suicides or intoxicating drugs, provide a comprehensive overview of the problem.
However, our study has limitations. There was an imbalance in enrolment between countries, with six countries (the Netherlands, Denmark, Spain, Sweden, Turkey and Belgium) contributing more than 75% of the patients. This bias does not reflect the population size of these countries in Europe. However, we believe that the management of ICU patients after acute poisoning does not differ significantly between European countries or between Europe and Australia. Therefore, the 3.7% ICU mortality observed in the study seems to be a plausible estimate for European countries, although variations may be more pronounced in regions with different resources, inpatient care or patients’ exposure. The sensitivity analysis showed that the effect of the heterogeneity of enrollment between units represented a limited bias since the rates of eventful ICU admission and in-hospital mortality rate were comparable (68% eventful ICU admissions and 4.5% in-hospital mortality rate in the total study sample versus 68.7% eventful ICU admissions and 4.2% in-hospital mortality rate in the units that included at least 80% of the patients admitted to their unit).
In addition, the over-representation of university hospitals in our study may indicate a bias towards more complex cases due to the research focus and capabilities of the centers. Future analyses will need to investigate whether patients at university centers had more severe exposures or comorbidities. Finally, written informed consent was mandatory in many intensive care units, which meant that we could not know how many patients were excluded from the study. We have therefore missed a certain number of patients. This may cause a selection bias, because the prognosis of the patients may vary according to whether an informed consent was considered necessary or not. However, the sensitivity analysis showed that this effect was limited.
Conclusions
Our results show a higher rate of intoxicated patients being treated in the ICU than has been reported in previous studies. Comprehensive data has been successfully collected on a large cohort of patients admitted to the ICU after acute intoxication, predominantly from European ICUs, with some representation from other continents. Future research needs to look more closely at outcomes by type of intoxication, externally validate existing prediction models predicting the need for ICU admission, identify risk factors for complicated intoxications, perform competing risk analysis for likelihood of discharge, and assess the prognosis of patients after specific exposures, such as street drugs. However, this requires large and detailed databases. INTOXICATE is a first step towards such a granular database. The findings from this study will inform future research efforts, particularly in understanding prognosis and refining data collection methods for similar studies.
Supplementary Information
Additional file 1: Table S1. Summary of the prior observational studies conducted with patients admitted to an intensive care unit (ICU) after acute intoxication. Search criteria: (1) setting: intensive care unit (ICU) in Europe or North-America or Australia or Hong Kong; (2) adult patients admitted to an ICU after an acute intoxication; (3) Design: observational study; (4) Studies reporting at least one of the outcomes of interest i.e. ICU mortality, in-hospital mortality and/or mortality 30 days after ICU admission. The studies are ordered from the most recent to the oldest year of publication and within each year by study size. A study population with fewer than 100 included patients was considered as being a “small size population study”, and with fewer than 300 included patients as a “relatively small size population study”. Table S2. Technical challenges related to multicenter data collection in the INTOXICATE study.
Acknowledgements
INTOXICATE Study Investigators Group (collaborators): Christian Aage Wamberg, Hazim Ababneh, Eman Abdulwahed, Sefanja Achterberg, Entisar Ahmed Ali Alshareea, Aiman Al-Touny, Mahmoud Alali, Ali Najeh Al-Awwady, Amar Al-Jarrah, Maytham A. Al-Juaifari, Hazem Zuhair Hussain Alnatour, Khayry Al-Shami, Ahmed Altobal, Shimaa Ahmed Hamed Abdelrahman Al-Touny, Mahmut Arslan, Theodoros Aslanidis, Avinash Aujayeb, Munire Babayigit, Robertas Badaras, Stuart Baker, Patricia Barral Segade, Najat Ben Hasan, Dennis C.J.J. Bergmans, Yeliz Bilir, Muhannud Binnawara, Patrick Biston, Dirk P. Boer, Hans Christian Boesen, Hella F. Borggreve, Helene Brix, Thirsa Brommer, Nestor Bueno-Vidales, Isabel Canas-Pérez, Maxim P. Carlier, Alba Castellanos Esparraguera, Deniz Cekic, Mario Chico-Fernández, Lisbeth Christiansen, Cristian Cobilinschi, Luis Coelho, Catalin Constantinescu, Alexander D. Cornet, Elena Crescioli, Cristina Cuenca-Rubio, Paul I Dargan, Raluca Darie, Dylan W. de Lange, Francisco de Paula Delgado-Moya, Nicolas De Schryver, Bram Dewulf, Willem Dieperink, Patrick Druwé, Simon Dubler, Maree Duroux, Mohamed Elbahnasawy, Muhammed Elhadi, Ahmet Eroglu, Selin Eyüpoğlu, Raquel Feria Gil, Ana Silva Fernandes, Carolina Ferrer, Ana Ferrer Dufol, Sune Forsberg, Diego Franch-Llasat, Rik T. Gerritsen, Reem Ghmagh, Juliana Gonzalez Londoño, Christoffer Grant Sølling, Kjeld Gravgaard, Massimiliano Greco, Goncalo Guerreiro, Nicole Gustavsson, Seda Güzeldag, Burcin Halacli, Hytham K. S. Hamid, Philippe Hantson, Thijs T. W. van Herpt, Jantine van Holten, F. van der Horst, Aletta P.I. Houwink, Claudine C. Hunault, Malene Hvass Renner Block, Christian Jung, Stavri Karasiali, Mohamed Karghul, Ebru Kaya, Almu’atasim Khamees, Khalid Mahmood Khan Nafees, Justin Koh, Matty Koopmans, Vedran Kovacic, Gabija Laubner Sakalauskienė, Lenneke E. M. van Lelyveld-Haas, Elin Lindqvist, Meritxell Lladó Vilar, Mette Lolk, Beatriz Martín-Pérez, Eva Maria Mateo Rodríguez, Hélène P. Mattijsen, Ayman Meelad, Iris Miltenburg, Ahmed Mohamed Ibrahim Mohamed, Rui Moreno, Marwa Morgom, Mercedes Mucia-Anayaa, Mohamed Nassredin, Binti Haji Abd Rashid Nurhikmahtul Aqilah, Huub L. A. van den Oever, Evelien A. N. Oostdijk, Ozlem Ozkan Kuscu, Catarina Pacheco, Dorte Palmqvist, Despoina Papachristou, David Pérez-Torres, Cristina Petrişor, Michael Piagnerelli, Wouter Pijper, Christian Rabe, Radu Țincu, Megan Ratcliffe, Nanna Reiter, Richard Rezar, Ferran Roche-Campo, Emilio Rodriguez-Ruiz, Harm Roetert, J. Ruiz-Izquierdo, Ana Maria Ruiz Mena, Vusala Rzayeva, Nick van Sabben, Elfayadh Saidahmed, Gustaf Sandström, Kemal Tolga Saracoglu, Clemens Seelmaier, Nicolas Serck, Carlos Serón-Arbeloa, Susanne Stads, Louise Stenbryggen Herløv, Ayca Sultan Sahin, Josefine Thomsen, Arzu Topeli, Yen Tran, Bas van den Bogaard, Irma S. van den Hengel-Koot, Klaas Vanderbiest, Liam van Dielen, Abram L. van Duijn, Jolien Van Hecke, Klaus Vennick Marcussen, Marie Vergotten, Wytze Vermeijden, Ester Viktorsdottir, Peter H.J. van der Voort, Evert-Jan Wils, Xavier Wittebole, Esther Wolthuis, David M. Wood, Max Wretman, Hana B. Yahya, Cengizhan Yavuz, Selcuk Yaylaci, Begoña Zalba Etayo, Samanta M. Zwaag. We would like to thank the European Society of Intensive Care Medicine (ESICM) and the European Association of Poison Centres and Clinical Toxicologists (EAPCCT) for supporting the study, and all the patients who participated in the study.
Abbreviations
- APC
America's Poison Centers
- DPIC
Dutch Poisons Information Centre
- EAPCCT
European Association of Poison Centres and Clinical Toxicologists
- ECMO
Extra Corporeal Membrane Oxygenation
- eCRF
Electronic Case Report Form
- ED
Emergency Department
- EDC
Electronic Data Capture
- ESICM
European Society of Intensive Care Medicine
- FiO2
Fraction of inspired oxygen
- GDPR
General Data Protection Regulation
- HDU
High Dependency Unit
- ICU
Intensive Care Unit
- IQR
Interquartile range
- OSF
Open Science Framework
- SaO2
Oxygen saturation
Author contributions
SMZ and CCH performed the analysis, prepared the figures and wrote the manuscript. All the authors contributed to the data collection. All authors have thoroughly reviewed and approved the manuscript. DWdeL and CCH supervised the study.
Funding
None.
Availability of data and materials
The participants of the study did not give written consent for their personal data to be shared publicly, so supporting data are not available.
Declarations
Ethics approval and consent to participate
Data collection was approved by the accredited Medical Research Ethics Committee of the University Medical Centre Utrecht, The Netherlands (ethics reference number: 20-495/C). All participating units provided either local research ethics committee approval or a waiver of consent. The study was registered prospectively with an Open Science Framework (OSF) (OSF registration ID: osf.io/7e5uy).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Claudine C. Hunault, Email: C.Hunault@umcutrecht.nl
the INTOXICATE Study Investigators Group:
Christian Aage Wamberg, Hazim Ababneh, Eman Abdulwahed, Sefanja Achterberg, Entisar Ahmed Ali Alshareea, Aiman Ahmed Hamed, Mahmoud Alali, Ali Najeh Al-Awwady, Amar Al-Jarrah, Maytham A. Al-Juaifari, Hazem Zuhair Hussain Alnatour, Khayry Al-Shami, Ahmed Altobal, Shimaa Ahmed Hamed Al-Touny, Mahmut Arslan, Theodoros Aslanidis, Avinash Aujayeb, Munire Babayigit, Robertas Badaras, Stuart Baker, Patricia Barral Segade, Najat Ben Hasan, Dennis C. J. J. Bergmans, Yeliz Bilir, Muhannud Binnawara, Patrick Biston, Dirk P. Boer, Hans Christian Boesen, Hella F. Borggreve, Helene Brix, Thirsa Brommer, Nestor Bueno-Vidales, Isabel Canas-Pérez, Maxim P. Carlier, Alba Castellanos Esparraguera, Deniz Cekic, Mario Chico-Fernández, Lisbeth Christiansen, Cristian Cobilinschi, Luis Coelho, Catalin Constantinescu, Alexander D. Cornet, Elena Crescioli, Cristina Cuenca-Rubio, Paul I. Dargan, Raluca Darie, Dylan W. de Lange, Francisco de Paula Delgado-Moya, Nicolas De Schryver, Bram Dewulf, Willem Dieperink, Patrick Druwé, Simon Dubler, Maree Duroux, Mohamed Elbahnasawy, Muhammed Elhadi, Ahmet Eroglu, Selin Eyüpoğlu, Raquel Feria Gil, Ana Silva Fernandes, Carolina Ferrer, Ana Ferrer Dufol, Sune Forsberg, Diego Franch-Llasat, Rik T. Gerritsen, Reem Ghmagh, Juliana Gonzalez Londoño, Christoffer Grant Sølling, Kjeld Gravgaard, Massimiliano Greco, Goncalo Guerreiro, Nicole Gustavsson, Seda Güzeldag, Burcin Halacli, Hytham K. S. Hamid, Philippe Hantson, Thijs T. W. van Herpt, Jantine van Holten, Femke van der Horst, Aletta P. I. Houwink, Claudine C. Hunault, Malene Hvass Renner Block, Christian Jung, Stavri Karasiali, Mohamed Karghul, Ebru Kaya, Almu’atasim Khamees, Justin Koh, Matty Koopmans, Vedran Kovacic, Gabija Laubner Sakalauskienė, Lenneke E. M. van Lelyveld-Haas, Elin Lindqvist, Meritxell Lladó Vilar, Mette Lolk, Beatriz Martín-Pérez, Eva Maria Mateo Rodríguez, Hélène P. Mattijsen, Ayman Meelad, Iris Miltenburg, Ahmed Ibrahim Mohamed Mohamed, Rui Moreno, Marwa Morgom, Mercedes Mucia-Anayaa, Khalid Mahmood Khan Nafees, Mohamed Nassredin, Binti Haji Abd Rashid Nurhikmahtul Aqilah, Huub L. A. van den Oever, Evelien A. N. Oostdijk, Ozlem Ozkan Kuscu, Catarina Pacheco, Dorte Palmqvist, Despoina Papachristou, David Pérez-Torres, Cristina Petrişor, Michael Piagnerelli, Wouter Pijper, Christian Rabe, Radu Țincu, Megan Ratcliffe, Nanna Reiter, Richard Rezar, Ferran Roche-Campo, Emilio Rodriguez-Ruiz, Harm Roetert, Jessica Ruiz-Izquierdo, Ana Maria Ruiz Mena, Vusala Rzayeva, Nick van Sabben, Elfayadh Saidahmed, Gustaf Sandström, Kemal Tolga Saracoglu, Clemens Seelmaier, Nicolas Serck, Carlos Serón-Arbeloa, Susanne Stads, Louise Stenbryggen Herløv, Ayca Sultan Sahin, Josefine Thomsen, Arzu Topeli, Yen Tran, Bas van den Bogaard, Irma S. van den Hengel-Koot, Klaas Vanderbiest, Liam van Dielen, Abram L. van Duijn, Jolien Van Hecke, Klaus Vennick Marcussen, Marie Vergotten, Wytze Vermeijden, Ester Viktorsdottir, Peter H. J. van der Voort, Evert-Jan Wils, Xavier Wittebole, Esther Wolthuis, David M. Wood, Max Wretman, Hana B. Yahya, Cengizhan Yavuz, Selcuk Yaylaci, Begoña Zalba Etayo, and Samanta M. Zwaag
References
- 1.Liisanantti J, Ohtonen P, Kiviniemi O, Laurila JJ, Ala-Kokko TI. Risk factors for prolonged intensive care unit stay and hospital mortality in acute drug-poisoned patients: an evaluation of the physiologic and laboratory parameters on admission. J Crit Care. 2011;26:160–5. [DOI] [PubMed] [Google Scholar]
- 2.Maignan M, Pommier P, Clot S, Saviuc P, Debaty G, Briot R, et al. Deliberate drug poisoning with slight symptoms on admission: are there predictive factors for intensive care unit referral? A three-year retrospective study. Basic Clin Pharmacol Toxicol. 2014;114:281–7. [DOI] [PubMed] [Google Scholar]
- 3.Vallersnes OM, Jacobsen D, Ekeberg Ø, Brekke M. Outpatient treatment of acute poisoning by substances of abuse: a prospective observational cohort study. Scand J Trauma Resusc Emerg Med. 2016;24:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brandenburg R, Brinkman S, De Keizer NF, Kesecioglu J, Meulenbelt J, De Lange DW. The need for ICU admission in intoxicated patients: a prediction model. Clin Toxicol (Phila). 2017;55:4–11. [DOI] [PubMed] [Google Scholar]
- 5.Han KS, Kim SJ, Lee EJ, Shin JH, Lee JS, Lee SW. Development and validation of new poisoning mortality score system for patients with acute poisoning at the emergency department. Crit Care. 2021;25:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gummin DD, Mowry JB, Beuhler MC, Spyker DA, Rivers LJ, Feldman R, et al. 2022 Annual report of the national poison data system® (NPDS) from America’s poison centers®: 40th annual report. Clin Toxicol (Phila). 2023;61:717–939. [DOI] [PubMed] [Google Scholar]
- 7.Reisinger A, Rabensteiner J, Hackl G. Diagnosis of acute intoxications in critically ill patients: focus on biomarkers-part 1: epidemiology, methodology and general overview. Biomarkers. 2020;25:9–19. [DOI] [PubMed] [Google Scholar]
- 8.Rezar R, Jung C, Mamandipoor B, Seelmaier C, Felder TK, Lichtenauer M, et al. Management of intoxicated patients-a descriptive outcome analysis of 4,267 ICU patients. BMC Emerg Med. 2022;22:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banderas-Bravo ME, Arias-Verdú MD, Macías-Guarasa I, Aguilar-Alonso E, Castillo-Lorente E, Pérez-Costillas L, et al. Patients admitted to three Spanish intensive care units for poisoning: type of poisoning, mortality, and functioning of prognostic scores commonly used. Biomed Res Int. 2017;2017:5261264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.European Association of Poison Centres and Clinical Toxicologists (EAPCCT). https://www.eapcct.org. Accessed 21 June 2024. [DOI] [PubMed]
- 11.European Society of Intensive Care Medicine (ESICM). https://www.esicm.org/. Accessed 21 June 2024.
- 12.Castor EDC. Electronic data capture solution. https://www.castoredc.com/electronic-data-capture-system/. Accessed 21 June 2024.
- 13.El Gharbi F, El Bèze N, Jaffal K, Sutterlin L, Mora P, Malissin I, et al. Does the ICU requirement score allow the poisoned patient to be safely managed without admission to the intensive care unit? A validation cohort study. Clin Toxicol (Phila). 2022;60:298–303. [DOI] [PubMed] [Google Scholar]
- 14.Lindqvist E, Edman G, Hollenberg J, Nordberg P, Ösby U, Forsberg S. Intensive care admissions due to poisoning. Acta Anaesthesiol Scand. 2017;61:1296–304. [DOI] [PubMed] [Google Scholar]
- 15.Böll R, Romanek K, Schmoll S, Stich R, Ott A, Stenzel J, et al. Independent validation of the ICU requirement score in a cohort of acutely poisoned adults. Clin Toxicol (Phila). 2018;56:664–6. [DOI] [PubMed] [Google Scholar]
- 16.Kovacic V, Kvartuc L, Mikacic M, Jerkovic I, Begovic TI, Maras M, et al. Clinical and demographic features with outcome predictors of adult patients with acute intoxication admitted to a medical intensive care unit in the Mediterranean part of Croatia. Toxicol Res (Camb). 2023;12:626–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yaylaci S, Genc AB, Demir MV, Cinemre H, Tamer A. Retrospective evaluation of patients at follow-up with acute poisoning in Intensive Care Unit. Niger J Clin Pract. 2016;19:223–6. [DOI] [PubMed] [Google Scholar]
- 18.Lam SM, Lau AC, Yan WW. Over 8 years experience on severe acute poisoning requiring intensive care in Hong Kong, China. Hum Exp Toxicol. 2010;29:757–65. [DOI] [PubMed] [Google Scholar]
- 19.Vujaklija Brajković A, Grgat M, Bielen L, Brajković J, Zlopaša O, Vrdoljak NG, et al. Self-poisoning as a cause of admission in a medical intensive care unit and a question of misuse of prescription medications. Heart Lung. 2022;51:17–21. [DOI] [PubMed] [Google Scholar]
- 20.Athavale V, Green C, Lim KZ, Wong C, Tiruvoipati R. Characteristics and outcomes of patients with drug overdose requiring admission to intensive care unit. Australas Psychiatry. 2017;25:489–93. [DOI] [PubMed] [Google Scholar]
- 21.Henderson A, Wright M, Pond SM. Experience with 732 acute overdose patients admitted to an intensive care unit over six years. Med J Aust. 1993;158:28–30. [DOI] [PubMed] [Google Scholar]
- 22.Clark D, Murray DB, Ray D. Epidemiology and outcomes of patients admitted to critical care after self-poisoning. J Intensive Care Soc. 2011;12:268–73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Summary of the prior observational studies conducted with patients admitted to an intensive care unit (ICU) after acute intoxication. Search criteria: (1) setting: intensive care unit (ICU) in Europe or North-America or Australia or Hong Kong; (2) adult patients admitted to an ICU after an acute intoxication; (3) Design: observational study; (4) Studies reporting at least one of the outcomes of interest i.e. ICU mortality, in-hospital mortality and/or mortality 30 days after ICU admission. The studies are ordered from the most recent to the oldest year of publication and within each year by study size. A study population with fewer than 100 included patients was considered as being a “small size population study”, and with fewer than 300 included patients as a “relatively small size population study”. Table S2. Technical challenges related to multicenter data collection in the INTOXICATE study.
Data Availability Statement
The participants of the study did not give written consent for their personal data to be shared publicly, so supporting data are not available.