Abstract
Background:
Although the Chronic Disease Self-Management Program (CDSMP) improves chronic disease outcomes, little is known about CDSMP participation in populations less than 65 years of age. We explore study and CDSMP participation rates by demographic characteristics with younger (40–64 years old), lower-to-middle wage workers with chronic disease in a randomized clinical trial (RCT) conducted in North Carolina.
Methods:
Descriptive statistics and regression models were used to examine associations between demographic, chronic disease burden, and employment variables, and time-dependent study enrollment and intervention participation outcomes that ranged from initiating consent (n = 1,067) to CDSMP completion (n = 41).
Results:
Overall, participation among non-Whites was disproportionately higher (43%–59%) than that of Whites (42%–57%) relative to the age-matched racial composition of North Carolina (31% non-White and 69% White). Among participants randomized to the CDSMP, racial and ethnic minorities had the highest rates of participation. There were no significant demographic, chronic disease burden, or employment predictors among the participation outcomes examined, although this may have been due to the limited number of CDSMP workshop participation observations.
Conclusions:
Extending the CDSMP to lower-to-middle wage workers may be particularly effective in reaching racial and ethnic minority populations, who complete the program to a greater extent than their White, non-Hispanic counterparts.
Keywords: chronic disease, health equity, self-management
1 |. BACKGROUND
An estimated 60% of U.S. adults have at least one chronic disease, while 42% have multiple chronic diseases (Buttorff, Ruder, & Bauman, 2017). Broadly defined, chronic disease includes “conditions that last a year or more and require ongoing medical attention and/or limit activities of daily living” (U. S. Department of Health & Human Services, 2010b). The risk of developing chronic disease is not confined to older adults over age 65; rather, risk increases with age, such that among adults aged 45–64 years, 50% have one or more chronic disease conditions (Buttorff et al., 2017). Moreover, chronic disease disproportionately, and more adversely, affects socioeconomically disadvantaged and racial/ethnic minority populations, who have two-three times the prevalence of chronic disease than others in their age group, as well as higher symptom burden, functional limitations, and disability (Institute of Medicine, 2012; U.S. Department of Health & Human Services, 2010a).
Given this overall distribution, it is not surprising that chronic disease exacts a heavy toll on the U.S. workforce, with workers approaching retirement and those that are lower wage earners bearing the brunt of chronic disease burden (Harris, Huang, Hannon, & Williams, 2011). Compared to employed adults aged 25–74 years in the general population who report an average of 1.1 “impaired” work days per month (i.e., they had either missed work or had reduced productivity), workers with chronic health conditions average 6.7 impaired workdays per month (Kessler, Greenberg, Mickelson, Meneades, & Wang, 2001). On a national scale, this is equivalent to over 2.5 billion days per month that employees with chronic disease are either absent or less productive in their employment role (Kessler et al., 2001). This increase in absenteeism creates a challenging cycle of income and health-related limitations for lower wage earning employees with chronic disease to escape, whereby income limits access to health resources, and poor health limits employment-related productivity and opportunity (Muennig, 2008).
Community-based programs focused on enhancing self-management of chronic conditions may offer employed adults of lower socioeconomic status (SES) a means to escape this web of health and work-related limitations. The Chronic Disease Self-Management Program (CDSMP), for example, is a 6-week, peerled workshop that has been associated with significant health and functional improvements among working-aged adults as demonstrated in the national dissemination studies and a meta-analysis of CDSMP study findings (Brady et al., 2013; Ory et al., 2014). Such improvements include fewer days of poor mental and physical health, improved quality of life, and fewer days of limited activity (Ory et al., 2014). While these outcomes have been observed among CDSMP participants across a range of socioeconomic backgrounds, this national dissemination study demonstrated that the CDSMP has primarily attracted non-Hispanic white, aging females (Ory et al., 2014; Smith, Cho, Salazar, & Ory, 2013). Current research provides mixed results regarding whether sociodemographic factors are associated with CDSMP completion (defined as attendance of at least four of the six sessions; Jiang et al., 2015; Korda et al., 2013; O’Connell & Kaw, 2015; Ory et al., 2013; Ory et al., 2014; Smith et al., 2013). It is therefore unclear whether current CDSMP courses are targeting and engaging populations who are most at-risk for worsened chronic disease morbidity, including those from socioeconomically disadvantaged and racial/ethnic minority backgrounds.
2 |. AIMS
Given the limited number of studies examining lower-to-middle wage, middle-aged adults’ participation in the CDSMP, this research has the following aims:
To describe the sociodemographic characteristics of the sample at study initiation (beginning the consent process), multiple stages in the enrollment process (completing consent, completing eligibility screening, completing enrollment), and two key stages of intervention participation (attending the first CDSMP session and CDSMP completion, which was defined as attending 4+ sessions).
To describe participant retention from one study enrollment and CDSMP participation stage to the next, within sociodemographic characteristic categories.
To explore which sociodemographic characteristics (a) are associated with retention across each enrollment and CDSMP participation stage, and (b) are independent predictors of retention at each enrollment and CDSMP participation stage.
3 |. METHODS
3.1 |. Design and sample
We applied a descriptive, correlational design to meet the study aims using longitudinal data that were collected between 29 June 2015 and 30 September 2018 as part of a recently completed randomized controlled trial (RCT). The aims of the SMART Life RCT were to (a) test the effect of the CDSMP on employment, health, and health care utilization outcomes, (b) conduct an economic evaluation of the CDSMP for employers, the health care system, and state governments, and (c) assess factors associated with the reach, effectiveness, adoption, and implementation of the CDSMP using marketing strategies designed to improve program engagement.
We recruited participants from the following five counties in North Carolina: Wake, Durham, Cumberland, Orange, and Guilford. To recruit participants, we circulated study advertisements through fliers, email, and digital media through professional news outlets, small and large public and private employers, state health insurance agencies, and other community agency channels. There was no specific reference to the CDSMP on study recruitment materials; rather, materials indicated participation in either a “health self-management program” or a “financial self-management program” as part of the study.
Recruitment materials directed individuals to a website where they could begin completing a series of online survey processes required for participation (see Figure 1). This process began with a “registration step,” where individuals with initial interest in study participation provided basic contact and demographic information to receive more information and gain access to informed consent materials. Once “registered,” potential participants began the online consent process, indicated their consent for participation, and if they gave consent, they were taken to a section of screening questions to determine whether they met study eligibility criteria and inform them of their eligibility to continue in the enrollment process. Eligible participants who wanted to continue to enrollment completed baseline data collection, and, in a final step, they were then randomly assigned to either the “health self-management program” group (i.e., the CDSMP as the intervention) or the “financial self-management program” group (i.e., the attention control condition) and notified of their group assignment. The baseline survey questions took approximately 30–45 min to complete. Those who enrolled were scheduled in their respective counties to attend the CDSMP or the attention control program in their respective counties and complete follow-up data collection at 3, 6, 9, and 12 months. An incentive of $25.00 was given to study participants 1-month post-enrollment. An additional $40.00 incentive was given when they completed 12-month data collection. The study was approved by The University of North Carolina at Chapel Hill institutional review board. Twelve-month data collection will be completed in September 2018.
FIGURE 1.
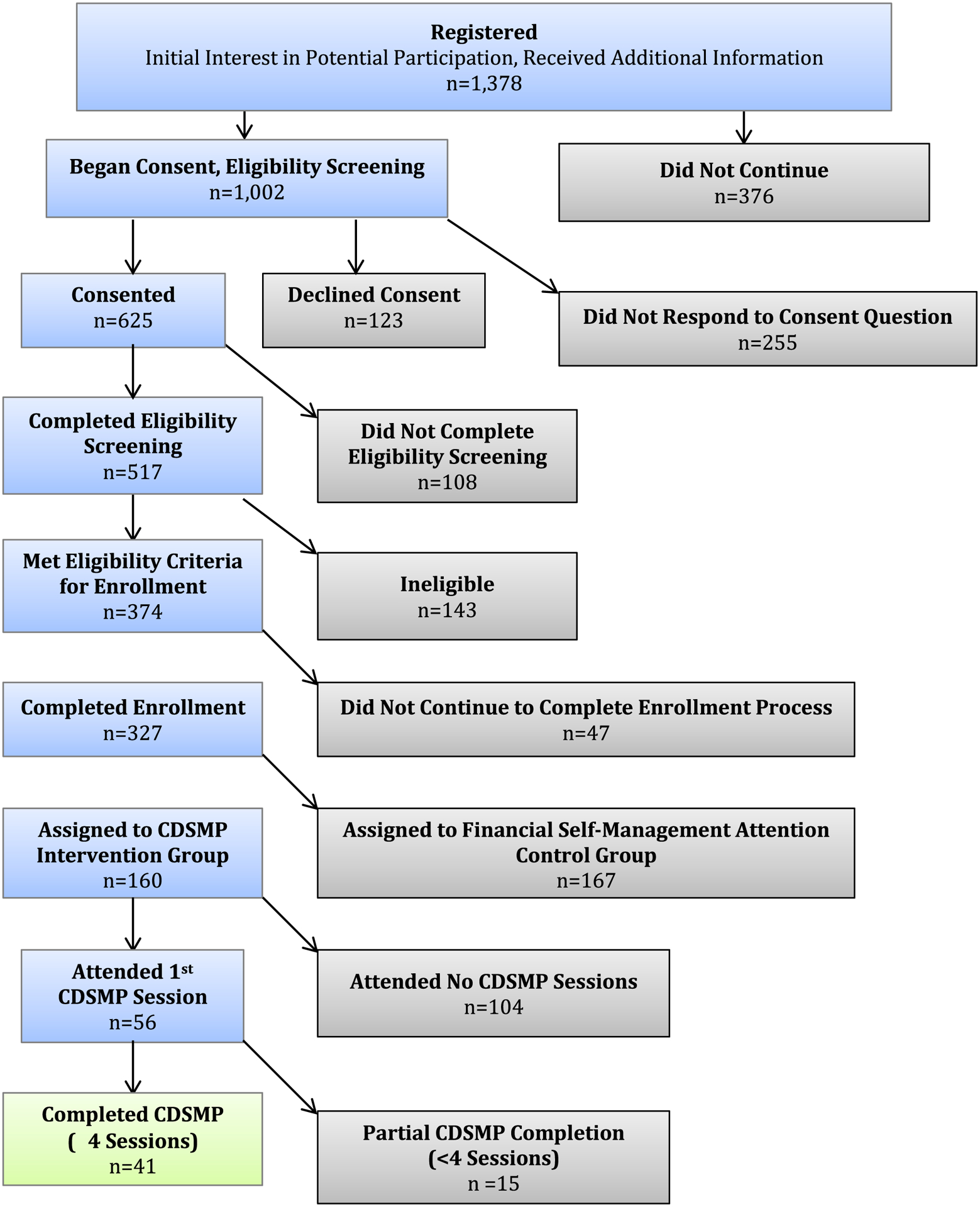
CONSORT algorithm for the SMART Life randomized controlled trial (RCT)
Eligibility criteria for enrollment included: (a) being between the age of 40–64 years, (b) working at least 32 hr per week, (c) earning less than $60,000 per year, (d) having at least one chronic health condition (broadly defined), (e) being fluent in spoken and written English, and (f) living or working in one of the five North Carolina counties (Wake, Durham, Cumberland, Orange, and Guilford) where the CDSMP was being delivered by community-based organizations we partnered with for the study. Given our community partners who would be responsible for delivering the CDSMP had concerns about safety and managing the group interaction that occurs during the CDSMP sessions, potential participants were excluded if they had mental health symptoms that have previously interfered with their participation in group activities, or reported engaging in any violent behavior in the past four months. We had a total of 1,002 individuals begin the online study consent process. From this initial group, we ultimately enrolled 327 employed adults in the RCT.
3.2 |. Measures
For the purpose of this study, data are reported in a series of study related time points. Enrollment consisted of five sequential steps (beginning consent, completion of consent, completion of eligibility screening, eligibility determination based on study protocol, and completion of enrollment and baseline data collection). Intervention participation consisted of three primary steps (randomization per study protocol, attended first CDSMP session, and attended ≥4 CDSMP sessions.
Data collection intensified as participants completed different sections of the online enrollment process. Because of this, early in the process (i.e., registration) data are limited (i.e., only basic demographic information was collected), with more data collected to determine eligibility in the interim online survey process steps, and the full battery of baseline measures being completed only after individuals consented to enrollment.
3.2.1 |. Demographic characteristics
We collected demographic data on participants at different points in the study registration and enrollment process. Prior to individuals beginning the informed consent process, we collected self-reported data on gender, age, race, and annual household income. Once participants completed the study consent, additional data related to chronic health condition and employment history were collected to determine if they met eligibility criteria. Given this, not all data on demographic variables of interest are available at earlier study participation occasions.
We used the Department of Health and Human Services (DHHS) minimum response options of American Indian or Alaskan Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, and White for self-reported race, and Hispanic or non-Hispanic for self-reported ethnicity (U. S. Department of Health & Human Services, 2011). For analytic purposes, American Indian/Alaskan Native, Asian, and respondents self-reporting they belonged to either two or more racial groups or self-identified as “other” were combined. The number of chronic health conditions was collected during eligibility determination, where participants identified which, if any, chronic health conditions they had from a broad list of 26. The list was generated to include conditions from the CDSMP national evaluation and a standardized list used to define chronic conditions for the US Department of Health and Human Services’ strategic framework for addressing multiple chronic conditions (Goodman, Posner, Huang, Parekh, & Koh, 2013). Example conditions on this list include arthritis, cancer, diabetes, seizures, and chronic pain.
3.3 |. Analytic strategy
Descriptive statistics that included means, standard deviations, and percentages were calculated to examine the distribution of select demographic, health, and employment characteristics at each enrollment and CDSMP participation time point, as well as the proportions of the sample retained by specific characteristics from one time point to the next. Given that data collection on variables of interest was initiated at specified time points in the study enrollment process, there were no data available for the number of chronic health conditions or working at more than one job for participants who did not complete study eligibility screening questions.
Tests of differences in proportions were applied to assess differences in key demographic, health, and employment characteristics of participants who were retained from one study time point (t) to the next (t + 1) using the prtesti command in Stata®/SE Version 15.1 (StataCorp LLC, 2017b). Although there are no specific sample size requirements for conducting equality of proportions testing using prtesti, in cases where there were fewer than 50 observations, an exact hypothesis test for random binomial variables was applied (bit-esti), as recommended with smaller samples (StataCorp LLC, 2017a).
In addition, we used logistic regression to assess the extent to which select demographic, health, and employment characteristics predicted participation at each time point, for a total of eight regression models. Given that all independent variables could theoretically be expected to at least partially explain ongoing participation, all variables were entered into each regression model simultaneously.
4 |. RESULTS
The Consolidated Standards of Reporting Trials (CONSORT) algorithm of study participation provides detailed information on sample size and attrition as the trial progressed (see Figure 1; Schulz, Altman, & Moher, 2010). Tables 1 and 2 present demographic composition of participants, and the percent of participants continuing from one study time point to the next, respectively. Shaded columns indicate time points in the study in which participant continued participation or representation was constrained by the necessity of meeting eligibility criteria and being randomized into group per study protocol; thus, at these select time points participant representation does not reflect free choice to either continue with enrollment or a preference for CDSMP participation.
TABLE 1.
Demographic characteristics of participants at select study time points
| Began consent process (n = 1,002) | Consented (n = 625) | Completed eligibility screening (n = 517) | Met eligibility criteria (n = 374) | Completed baseline and enrolled (n = 327) | Randomized to CDSMP (n = 160) | Attended 1st CDSMP session (n = 56) | Attended 4+ CDSMP sessions (n = 41) | |
|---|---|---|---|---|---|---|---|---|
| Variable | ||||||||
| Gender | ||||||||
| Female | 86.5% | 86.9% | 87.8% | 89.3% | 89.0% | 90% | 89.3% | 87.8% |
| Male | 13.5% | 13.1% | 12.2% | 10.7% | 11.0% | 10% | 10.7% | 12.2% |
| Agea | 48.6 [9.1] | 49.5 [8.1] | 49.1 [8.4] | 50.7 [6.7] | 50.5 [6.6] | 50.6 [6.6] | 52.9 [6.4] | 53.0 [6.8] |
| Race | ||||||||
| White | 56.8% | 54.5% | 54.9% | 53.6% | 53.5% | 50% | 42.9% | 41.5% |
| Black | 35.4% | 36.6% | 36.5% | 38.3% | 38.8% | 43.1% | 48.2% | 51.2% |
| Other | 7.8% | 8.9% | 8.6% | 8.1% | 7.7% | 6.9% | 8.9% | 7.3% |
| Ethnicity | ||||||||
| Hispanic | 4.2% | 5% | 4.3% | 4% | 4.3% | 4.4% | 7% | 7% |
| Non-Hispanic | 95.8% | 95% | 95.7% | 96% | 95.7% | 95.6% | 93% | 93% |
| Income (household) | ||||||||
| ≤$39,000 | 18.7% | 21.7% | 23.7% | 25.3% | 24.8% | 23.8% | 26.8% | 31.7% |
| $40,000–$79,000 | 49% | 52.0% | 50.4% | 52.3% | 53.2% | 51.9% | 55.4% | 53.7% |
| ≥$80,000 | 32.3% | 26.3% | 25.9% | 22.4% | 22.0% | 24.4% | 17.9% | 14.6% |
| Number of chronic health conditions | ||||||||
| 1 | ND | ND | 28% | 23.5% | 24.5% | 25.3% | 26.9% | 25.6% |
| 2–3 | 42% | 47.0% | 46.5% | 48.7% | 48.1% | 46.2% | ||
| 4 or more | 30% | 29.6% | 28.9% | 26% | 25% | 28.2% | ||
| Working at >1 job | ||||||||
| Yes | ND | ND | 19% | 18.2% | 17.4% | 16.9% | 16.1% | 14.6% |
| No | 81% | 81.8% | 82.6% | 83.1% | 83.9% | 85.4% | ||
Mean age; [sd]. ND = no data collected on variable at specified time point. Demographic composition of sample at “Met Eligibility Criteria” and “Randomized to CDSMP” conditional on study processes, and do not reflect voluntary continued participation.
TABLE 2.
Retention at study participation time points, within demographic characteristic categoriesa
| Began consent process (n = 1,002) | Consented (n = 625) | Completed eligibility screening (n = 517) | Met eligibility criteria (n = 374) | Completed baseline and enrolled (n = 327) | Randomized to CDSMP (n = 160) | Attended 1st CDSMP session (n = 56) | Attended 4+ CDSMP sessions (n = 41) | |
|---|---|---|---|---|---|---|---|---|
| Variable n, (% retained from prior time point) | ||||||||
| Gender | ||||||||
| Female | 867 | 543 (63%) | 454 (84%) | 334 (74%) | 291 (87%) | 144 (49%) | 50 (35%) | 36 (72%) |
| Male | 135 | 82 (61%) | 63 (77%) | 40 (63%) | 36 (90%) | 16 (44%) | 6 (38%) | |
| Age (in years) | ||||||||
| <301 | 22 | 14 (64%) | 0 (0%)*3−5 | – | – | – | – | – |
| 30–392 | 88 | 39 (44%)*3–5 | 0 (0%)*3–5 | – | – | – | – | – |
| 40–493 | 424 | 276 (65%) | 214 (78%)*5 | 178 (83%) | 160 (90%)*5 | 78 (49%) | 18 (24%)*4,5 | 12 (67%) |
| 50–594 | 361 | 225 (62%) | 188 (84%) | 145 (77%) | 126 (87%)*5 | 62 (49%) | 26 (43%)*5 | 19 (73%) |
| 60+5 | 103 | 68 (66%) | 61 (90%) | 48 (79%) | 38 (79%) | 18 (47%) | 11 (61%) | 9 (82%) |
| Race | ||||||||
| White1 | 565 | 336 (59%)*3 | 280 (83%) | 199 (71%) | 175 (88%) | 80 (46%) | 24 (30%)*3 | 17 (71%) |
| Black2 | 352 | 226 (64%) | 186 (82%) | 142 (76%) * 3 | 127 (89%)*3 | 69 (54%) * 3 | 27 (39%) | 21 (78%) |
| Other3 | 77 | 55 (71%) | 44 (80%) | 30 (68%) | 25 (83%) | 11 (44%) | 5 (45%) | 3 (60%) |
| Ethnicity | ||||||||
| Hispanic | 42 | 31 (74%)* | 22 (71%)* | 15 (68%) * | 14 (93%)* | 7 (50%) | 4 (57%)* | 3 (75%) |
| Non-Hispanic | 960 | 594 (62%) | 495 (83%) | 359 (73%) | 313 (87%) | 153 (49%) | 52 (34%) | 38 (73%) |
| Income (household) | ||||||||
| ≤$39,0001 | 186 | 134 (72%)*3 | 121 (90%)*2,3 | 94 (78%) * 3 | 81 (86%)*3 | 38 (47%) | 15 (39%) | 13 (87%)*2,3 |
| $40,000–$79,0002 | 487 | 321 (66%)*3 | 257 (80%) | 194 (75%) * 3 | 174 (90%)*3 | 83 (48%) | 31 (37%)*3 | 22 (63%) |
| ≥$80,0003 | 321 | 162 (51%) | 132 (81%) | 83 (63%) | 72 (87%) | 39 (54%) | 10 (26%) | 6 (60%) |
| Number of chronic health conditions | ||||||||
| 11 | ND | ND | 133 | 85 (70%) * 2 | 78 (92%) | 39 (50%) | 14 (36%) | 10 (71%) |
| 2–32 | 201 | 170 (85%) * 3 | 148 (87%) | 75 (51%) | 25 (33%) | 18 (72%) | ||
| 4 or more3 | 145 | 107 (74%) | 92 (86%) | 40 (43%) | 13 (33%) | 11 (85%) | ||
| Working at >1 job | ||||||||
| Yes | ND | ND | ND | 68 | 57 (84%) | 27 (47%) | 9 (33%) | 6 (67%) |
| No | 306 | 270 (88%) | 133 (49%) | 47 (35%) | 35 (74%) | |||
Note: Values for columns with italicized text indicates study time points that do not entirely reflect participant decisions determine continuing to subsequent part of the study.
Proportions reflect percent retained within demographic characteristic categories, from participants at previous study time point. “Began Consent Process” = index time point. ND = no data collected on variable at specified time point. Retention at “Met Eligibility Criteria” and “Randomized to CDSMP” conditional on study processes, and does not reflect voluntary continued participation. “Randomized to CDSMP” proportions expected to be approximately 50%, given equal randomization probability. No observations of participants <age 40 expected at the “Met Eligibility Criteria” time point and thereafter, as only those ≥40 years old met study inclusion criteria.
Test of equal proportions retained at each time period across individual response categories significant at p < 0.05. Designated number in superscript indicates which response category is compared (e.g., in the “Consented” column, the proportion of those age 30–39 who consented (44%) was significantly different from the 40- to 49-year old, 50- to 59-year old, and 60+ year old age groups, designed by superscript “3–5”).
Demographic characteristics of participants at select recruitment, enrollment, and CDSMP participation time points are detailed in Table 1. As noted, there were no data available for the number of chronic health conditions or whether potential participants were working at more than one job until they had completed the study eligibility screening questions. Overall, sample participants were overwhelmingly female (>86%) at each point of the study. The mean age at the initial registration step was 50 years, and increased incrementally in participants remaining in the study through CDSMP completion. Trends in sample composition related to household income included those in the lowest household income group gradually increasing in representation through CDSMP completion (from 18.7% to 31.7%), those in the middle household income group showing little fluctuation (ranging between 49%−55.4%), and those in the highest household income group markedly decreasing (from 32.3% to 14.6%) across study time points. Because household income reflects participant individual earned income, trends in household income reflect to some degree participation restrictions where earning <$60,000 annually was required for study eligibility. Sample composition with respect to the number chronic health conditions and working at >1 job remained relatively constant over study time points.
Racial and ethnic composition was more varied as participants moved through the enrollment process to CDSMP workshop completion; however, across all study engagement outcomes, participation among non-Whites was disproportionately higher (43%–59%) than that of Whites (42%–57%) relative to the age-matched racial composition of North Carolina (31% non-White and 69% White). Specifically, the proportion of the sample that was White trended downward (from 56.8% that began the consent process to 41.5% through completion), while the proportion of Black participants steadily increased from 35.4% to 51.2%. Notably, although Whites comprised the majority of the sample through being randomized to the CDSMP group, the racial majority converted to Black participants at the point of CDSMP program participation (see Figure 2). The combined racial category of “other” accounted for 7.7% of the total sample that began the consent process, whereby n = 9 were American Indian/Alaskan Native, n = 18 were Asian, n = 41 self-reported two or more racial groups, and n = 9 self-reported as “other” (detailed racial data not shown at each study time point in tables or figures). Representation of participants in the “other” racial group category, and those of Hispanic descent remained relatively constant at each time point, between 7.3%–8.9% and 4%–7%, respectively.
FIGURE 2.
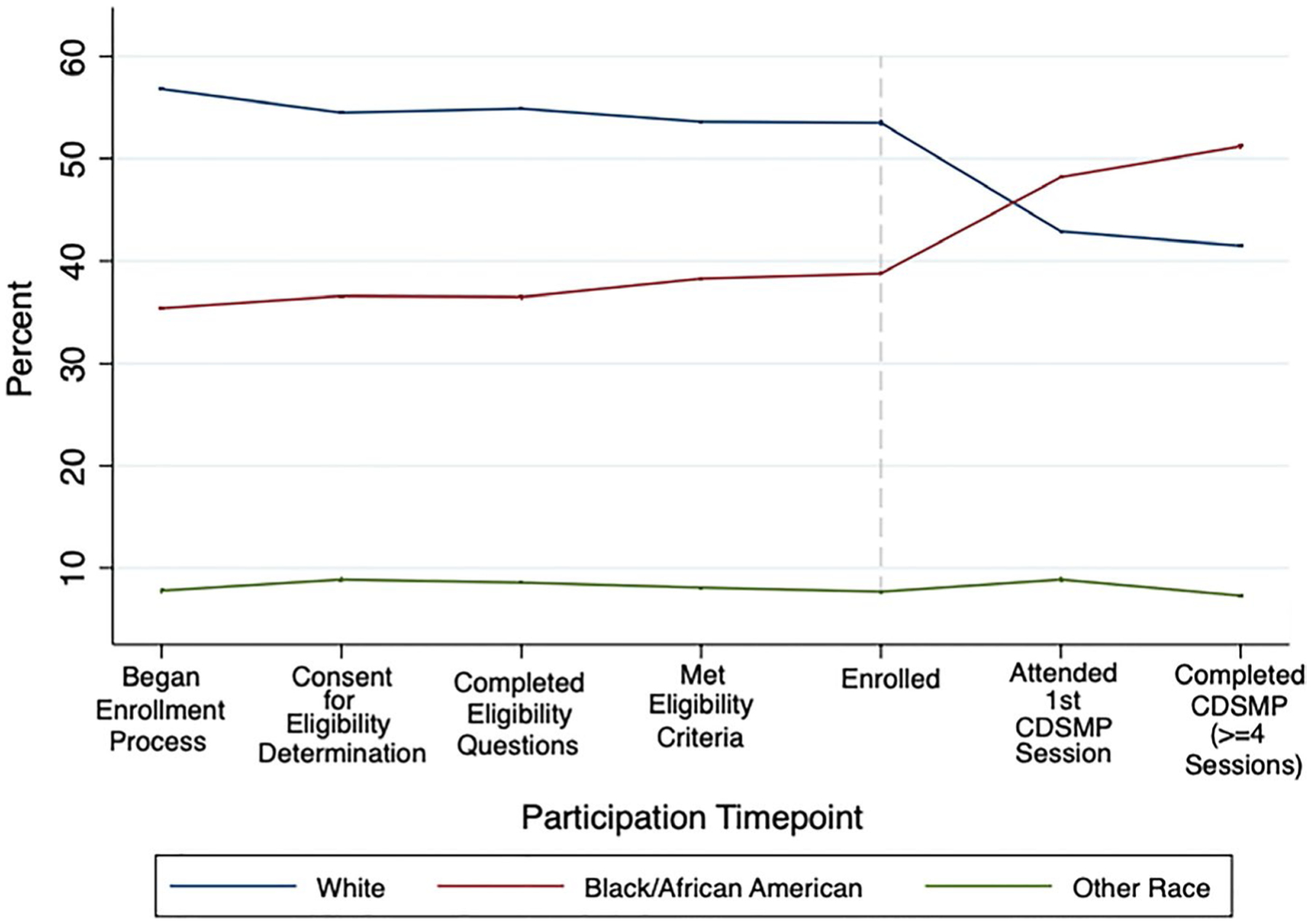
Study and CDSMP participant racial composition, at select timepoints
Results in Table 2 present the percent of participants in select demographic categories retained at each subsequent study time point. For gender, for example, 63% of females who began the consent process consented; while 84% of females who consented went on to complete the eligibility screening, and so on. Most striking is the difference in the average continuation rate through completing the baseline data collection and study enrollment () compared to the much lower percent that continued to attend the first CDSMP session () after being randomized (data not shown, Figure 3). With the exception of meeting eligibility criteria, continuation percentages by gender were not significantly different.
FIGURE 3.
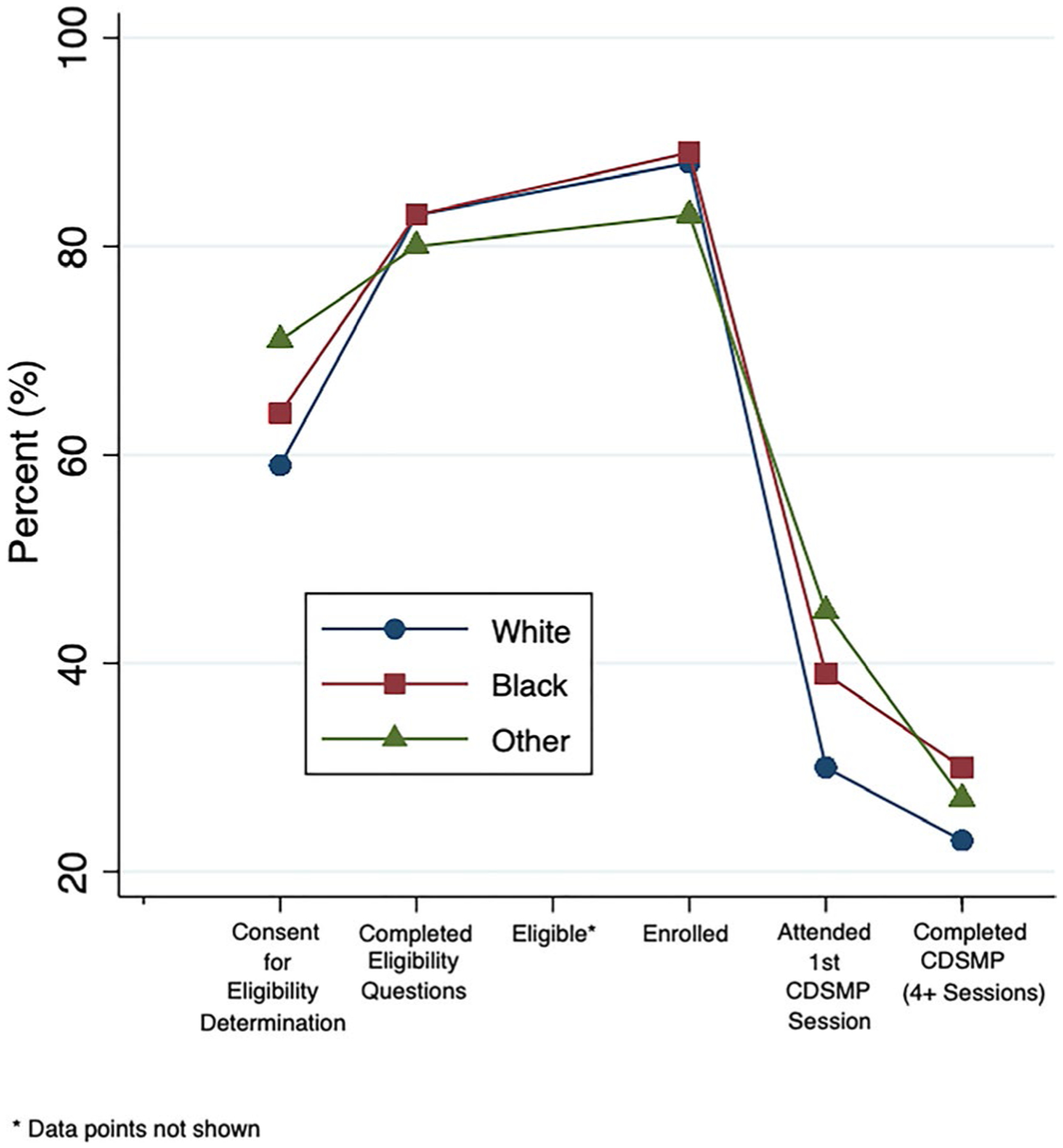
Percent retained at select study time points, within race
Although eligible 40–49 and 50–59 y/o s enroll at a higher rate than the 60+ (90%, 87% vs. 79%), there was a general stepwise trend of those in higher age groups continuing participation at each time point, while the younger age groups attend the first session at a lower rate (24%, 43% respectively vs. 61%). Across the majority of study time points, a higher proportion of participants who were non-White continued to the next time point than their White and/or non-Hispanic counterparts. Among these differences that were statistically significant, the proportion of Whites continuing to participate was between 5% and 15% less than those in one of the non-White categories. Eligible Hispanics both complete enrollment at a higher rate than non Hispanics (93% vs. 87%), and follow through to attend the first session at a higher rate (57% vs. 34%). Although a statistically significant lower proportion of Hispanic participants (71%) who consented went on to complete eligibility screening than non-Hispanic participants (83%), retention was significantly higher among Hispanic participants across the vast majority of other time points.
Across levels of household annual income, which is an income measure that is different from (albeit related) the individual earned income criterion used for study eligibility, retention at each time point varied. In general, compared to participants in households with an annual income of >$80,000, retention at each time point also tended to be higher among the lower two household income categories, with many statistically significant differences in the proportion retained between the lowest and highest household income groups. Middle income participants both complete enrollment and attend the first session at a significantly higher rate than do the highest income group (complete enrollment 90% vs. 87%; attend first session 37% vs. 26%).
The proportion of participants retained was also relatively similar by the number of chronic health conditions, with the exception of a higher proportion of those with 2–3 chronic health conditions meeting eligibility criteria (p < 0.05) compared to those with one chronic condition or four or more chronic conditions. There were no differences across study time points in whether participants were working at >1 job.
Results of the logistic regression models are shown in Table 3. Few demographic characteristics were found to be significant predictors of ongoing participation at each time point. Although age was a statistically significant variable, it only marginally increased the odds of ongoing participation when meeting eligibility criteria (as expected given age was a criterion for study enrollment), and in CDSMP attendance (first session, and completed attendance). Similarly, higher household income significantly reduced the odds of study continuation at the point of consenting for eligibility screening (OR = 0.41, p < 0.05 of highest household income group), completing eligibility screening (OR = 0.41 and 0.34, p < 0.05 of highest and middle household income groups, respectively), and meeting eligibility criteria (OR = 0.52, p < 0.05 in the highest household income group). As noted previously, these reduced odds of continued participation at these time points likely reflect the fact that, as potential participants moved through the enrollment process and reviewed eligibility criteria, those with individual earned income of >$60,000 per year realized they did not meet criteria and opted not to continue. Although the demographic shifts in sample composition and the proportion retained at each time point by racial/ethnic and household income characteristics suggested they could be significant predictors with regard to CDSMP attendance, the few observations of CDSMP attendance limited the power available for inferential statistical testing.
TABLE 3.
Predictors of participant engagement at select recruitment, enrollment, and Chronic Disease Self-Management Program (CDSMP) participation processes
| Outcome | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 |
|---|---|---|---|---|---|---|---|---|
| Study enrollment process: Began (n = 1,002) Did not begin (n = 376) |
Consented to eligibility screening: Yes (n = 625) No (n = 123) |
Eligibility screening: Completed (n = 517) Did not complete (n = 108) |
Eligibility criteria: Met (n = 374) Not Met (n = 143) |
Completed enrollment: Yes (n = 327) No (n = 47) |
Randomized, allocated to: CDSMP (n = 160) Control (n = 167) |
CDSMP attendance: 1st session (n = 54) Did not attend (n = 104) |
CDSMP completion (≥4 sessions) (n = 41) Did not complete ≥ 4 sessions (n = 119) |
|
| Model n | 1,067 | 989 | 607 | 506 | 367 | 324 | 158 | 158 |
| Variable | Odds ratios | |||||||
| Gender | ||||||||
| Female | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Male | 0.91 | 1.0 | 0.59 | 0.73 | 1.3 | 0.87 | 1.1 | 1.5 |
| Age | 1.02 | 1.0 | 1.0 | 1.1 | 0.98 | 1.0 | 1.1 | 1.08 |
| Race | ||||||||
| White | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Black | 1.04 | 1.0 | 0.87 | 1.2 | 1.2 | 1.6 | 1.8 | 1.7 |
| Other | 0.77 | 1.5 | 0.91 | 0.84 | 0.61 | 1.1 | 1.6 | 1.0 |
| Ethnicity | ||||||||
| Hispanic | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Non-Hispanic | 0.92 | 1.5 | 0.44 | 0.77 | 2.1 | 1.1 | 2.5 | 2.5 |
| Income (Household) | ||||||||
| ≤$39,000 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| $40,000-$79,000 | 1.47 | 0.79 | 0.34 | 0.91 | 1.4 | 1.1 | 1.4 | 1.0 |
| ≥$80,000 | 0.87 | 0.41 | 0.41 | 0.52 | 1.0 | 1.6 | 1.0 | 0.64 |
| Number of chronic health conditions | ||||||||
| 1 | ND | ND | ND | ND | Ref. | Ref. | Ref. | Ref. |
| 2–3 | 0.88 | 0.91 | 0.77 | 0.88 | ||||
| 4 or more | 0.89 | 0.71 | 0.62 | 0.98 | ||||
| Working at >1 job | ||||||||
| Yes | ND | ND | ND | ND | Ref. | Ref. | Ref. | Ref. |
| No | 0.73 | 0.94 | 0.80 | 0.72 | ||||
Note: Bolded text indicates statistically significant finding at p < .05.
ND: No data collected at select time point.
5 |. DISCUSSION
One of the primary findings from this study is that among middle-aged, lower-to-middle wage workers, racial/ethnic minorities, those with lower household income, and those who are older are more likely to participate in CDSMP workshops that are delivered in the community. The precipitous drop in participation from study enrollment to attending a first CDSMP session was also a major finding, suggesting that many in this population may have barriers to participating in the CDSMP, even when the timing and locations of workshops are tailored to meet the needs of variable working hours. Given that the CDSMP has been consistently funded through the Administration on Aging (AOA), dissemination has occurred predominantly through local Agency’s Services Network community sites that are readily accessible to older adult populations (Smith et al., 2012). This dissemination plan generally continues to follow the majority of the CDSMP’s early efficacy findings, which were conducted largely in samples 65 years old or greater (Lorig, Ritter, Laurent, & Plant, 2006; Lorig, Ritter, et al., 2001; Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001; Lorig et al., 1999), although dissemination efforts through broader public health systems are growing as the literature shows positive outcomes in populations <65 years old (Brady et al., 2013).
Our findings also demonstrated, however, that greater participation and retention rates of our sample at key study time points were higher among racial/ethnic minorities and those with lower household incomes. Despite reduced participation at the point of attending CDSMP workshops in our sample overall, all of these data indicate that, younger, less wealthy, and racial/ethnic minority populations are all interested in programs like the CDSMP if recruited through mechanisms designed to reach them, and possibly more likely to attend if workshops are offered at times and locations easily accessible to them. From a chronic disease morbidity stand-point, racial/ethnic minorities and adults with lower socioeconomic status bear the brunt of the burden. Nationally, prevalence rates of chronic disease conditions such as hypertension and diabetes among Blacks are 40% and 77% higher than non-Hispanic White populations, respectively (Centers for Disease Control & Prevention, 2016). Although mental illness is more prevalent in select racial minority groups (i.e., American Indian/Alaskan Natives) and can be less prevalent in other racial and ethnic minority groups (i.e., Black or African American, and Hispanic) than among Whites, racial/ethnic minorities have disproportionately higher rates of disability due to mental illness (American Psychiatric Association, 2017). Further, racial and ethnic minorities have more barriers to accessing what is needed to optimally control disease progression and receive self-management education within the US health care system (Boutaugh et al., 2014). In addition, studies of the CDSMP with Hispanic populations have shown positive effects on health (Lorig, Ritter, & Gonzalez, 2003; Lorig, Ritter, & Jacquez, 2005). For these reasons, making the CDSMP more accessible to middle-aged working adults who are racial/ethnic minorities or lower wage earning could provide a community-wide support for individuals to expand upon the chronic disease self-management skills they currently have.
A small but growing number of studies suggest that middle-aged adults, racial/ethnic minorities, and adults with lower SES participate in the CDSMP when given the opportunity. As Lorig and colleagues have developed a six-session internet version of the CDSMP to test its efficacy through online delivery (ICDSMP) in South Australia, they enrolled 254 adults, with 56% <55 years of age. In the ICDSMP trial, 65% participated through the sixth session—indicating that at least a younger, less educated population engages in the CDSMP when made more accessible via the internet (Lorig et al., 2013). In another study with a predominantly younger adult sample (80% were <65 years of age) by Forjuoh and colleagues, 36.4% were either non-White or Hispanic and nearly 68% had less than a 4-year college degree, where 75.6% randomized to the CDSMP completed four of six sessions (Forjuoh, Bolin, et al., 2014; Forjuoh, Ory, Jiang, Vuong, & Bolin, 2014). Finally, our participation-oriented findings are consistent with two studies that have used the Putting Prevention to Work: Chronic Disease Self-Management Program national evaluation data. In the first, Horrell and colleagues assessed CDSMP participation completion among 19,365 adults aged 50–64 years of age, where 23.7% of the sample was African American, 62.5% White, and 11.7% Hispanic. They found CDSMP participants living in the most socioeconomically impoverished geographical areas had a completion rate of 87%—higher than those living in higher SES areas, where completion rates were between 74.9% and 78.9% (Horrell et al., 2017). In the second, Mingo and colleagues assessed CDSMP completion among the 11,895 African Americans who participated in the CDSMP across delivery site types, where 79.4% completed the program.
6 |. IMPLICATIONS FOR RESEARCH AND PRACTICE
While the findings from these studies suggest high rates of CDSMP participation and completion among predominantly younger, racially/ethnically diverse, less college-educated populations are possible, further research in this area is needed. Overwhelmingly, for example, studies have not assessed the extent to which both SES and race/ethnicity might jointly moderate program participation, program completion, and/or study outcomes. One approach to advancing the science of self-management interventions is to consider the role that intersectionality plays in influencing disease, symptom, and quality of life intervention outcomes for groups at the highest risk of morbidity and mortality from chronic disease (Bauer, 2014). Nurse scientists are applying such a perspective in other public health domains, such as to better understand HIV risk factors and self-management strategies (Caiola, Barroso, & Docherty, 2017). As a theoretical approach, intersectionality illuminates the fact that one’s social location is never unidimensional (i.e., age group, race, ethnicity, and/or other indicators of social/economic status). Therefore, how individuals respond to interventions such as the CDSMP will depend on the influences these factors have at their intersection. Such an approach can inform a wide range of intervention-related research questions posed by public health-oriented nurse scientists to improve population health outcomes.
From a practice perspective, our findings and those of others suggest extending the CDSMP’s reach to make participation more accessible to groups that are most likely to be living with, limited by, and die from chronic disease is not only possible, but when made accessible, results in higher rates of program completion. For public health nurses and other public health practitioners at the local level, this means ensuring that programs currently available in communities for older adults are held in locations that make attending as accessible as possible for racial/ethnic minorities and those of lower SES. This could mean planning CDSMP sessions in public housing developments, in conjunction with faith-based communities to be held immediately after weekly services, or in conjunction with neighborhood watch groups. Extending the reach to slightly younger aged, working individuals may require nurses working in local health departments or other non-profit agencies seek non-aging-affiliated sources of funding to offer the CDSMP.
Whatever the strategies may be used to extend the program’s reach, narratives of racial/ethnic minority and lower SES populations as being disengaged or unreliable from an attendance point of view are cultural myths that have no empirical basis in these CDSMP participation findings. To work toward the goal of health equity, public health nurses should be active participants in disrupting such narratives and providing opportunities for CDSMP participation at the local level.
ACKNOWLEDGEMENTS
This manuscript is a product of a Health Promotion & Disease Prevention Research Center supported by Cooperative Agreement Number 1U48DP005017-01 from the Centers for Disease Control and Prevention. The findings and conclusions in this presentation are the author(s) and do not necessarily represent the position of the Centers for Disease Control and Prevention (CDC).
REFERENCES
- American Psychiatric Association. (2017). Mental health disparities: Diverse populations. In Washington, DC. [Google Scholar]
- Bauer GR (2014). Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science and Medicine, 110, 10–17. 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- Boutaugh ML, Jenkins SM, Kulinski KP, Lorig K, Ory MG, & Smith ML (2014). Closing the disparity gap: The work of the administration on aging. Generations, 38(4), 107–118. [Google Scholar]
- Brady TJ, Murphy L, O’Colmain BJ, Beauchesne D, Daniels B, Greenberg M, … Chervin D (2013). A meta-analysis of health status, health behaviors, and health care utilization outcomes of the Chronic Disease Self-Management Program. Prev Chronic Dis, 10, 120112. 10.5888/pcd10.120112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttorff C, Ruder T, & Bauman M (2017). Multiple chronic conditions in the United States. Santa Monica, CA: Rand Corporation. [Google Scholar]
- Caiola C, Barroso J, & Docherty SL (2017). Capturing the social location of African American mothers living with HIV: An inquiry into how social determinants of health are framed. Nursing Research, 66(3), 209–221. 10.1097/NNR.0000000000000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Racial and Ethnic Approaches to Community Health (REACH). In N. C. f. C. D. P. a. H. P. (NCCDPHP) (Ed.). Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Forjuoh SN, Bolin JN, Huber JC Jr, Vuong AM, Adepoju OE, Helduser JW, … Ory MG (2014). Behavioral and technological interventions targeting glycemic control in a racially/ethnically diverse population: A randomized controlled trial. BMC Public Health, 14, 71. 10.1186/1471-2458-14-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forjuoh SN, Ory MG, Jiang L, Vuong AM, & Bolin JN (2014). Impact of chronic disease self-management programs on type 2 diabetes management in primary care. World J Diabetes, 5(3), 407–414. 10.4239/wjd.v5.i3.407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman RA, Posner SF, Huang ES, Parekh AK, & Koh HK (2013). Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice. Preventing Chronic Disease, 10, E66. 10.5888/pcd10.120239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JR, Huang Y, Hannon PA, & Williams B (2011). Low-socioeconomic status workers: Their health risks and how to reach them. Journal of Occupational and Environmental Medicine, 53(2), 132–138. 10.1097/JOM.0b013e3182045f2c [DOI] [PubMed] [Google Scholar]
- Horrell LN, Kneipp SM, Ahn S, Towne SD Jr, Mingo CA, Ory MG, & Smith ML (2017). Chronic disease self-management education courses: Utilization by low-income, middle-aged participants. International Journal for Equity in Health, 16(1), 114. 10.1186/s12939-017-0604-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2012). How far have we come in reducing health disparities? Progress since 2000. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Jiang L, Smith ML, Chen S, Ahn S, Kulinski KP, Lorig K, & Ory MG (2015). The role of session zero in successful completion of chronic disease self-management program workshops. Frontiers in Public Health, 3, 205. 10.3389/fpubh.2014.00205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Greenberg PE, Mickelson KD, Meneades LM, & Wang PS (2001). The effects of chronic medical conditions on work loss and work cutback. Journal of Occupational and Environmental Medicine, 43(3), 218–225. 10.1097/00043764-200103000-00009 [DOI] [PubMed] [Google Scholar]
- Korda H, Erdem E, Woodcock C, Kloc M, Pedersen S, & Jenkins S (2013). Racial and ethnic minority participants in chronic disease self-management programs: Findings from the communities putting prevention to work initiative. Ethnicity and Disease, 23(4), 508–517. [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, & Gonzalez VM (2003). Hispanic chronic disease self-management: A randomized community-based outcome trial. Nursing Research, 52(6), 361–369. 10.1097/00006199-200311000-00003 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, & Jacquez A (2005). Outcomes of border health Spanish/English chronic disease self-management programs. Diabetes Educator, 31(3), 401–409. 10.1177/0145721705276574 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter PL, Laurent DD, & Plant K (2006). Internet-based chronic disease self-management: A randomized trial. Medical Care, 44(11), 964–971. 10.1097/01.mlr.0000233678.80203.c1 [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Plant K, Laurent DD, Kelly P, & Rowe S (2013). The South Australia health chronic disease self-management Internet trial. Health Education and Behavior, 40(1), 67–77. 10.1177/1090198112436969 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, William Brown B, Bandura A, … Holman HR (2001). Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care, 39(11), 1217–1223. 10.1097/00005650-200111000-00008 [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, & Hobbs M (2001). Effect of a self-management program on patients with chronic disease. Effective Clinical Practice, 4, 256–262. [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, … Holman HR (1999). Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care, 37(1), 5–14. 10.1097/00005650-199901000-00003 [DOI] [PubMed] [Google Scholar]
- Muennig P (2008). Health selection vs. causation in the income gradient: What can we learn from graphical trends? Journal of Health Care for the Poor and Underserved, 19(2), 574–579. 10.1353/hpu.0.0018 [DOI] [PubMed] [Google Scholar]
- O’Connell S, & Kaw D (2015). Predictors of non-completion of community-based chronic disease self-management programs: The Rhode Island experience during an economic recession. Rhode Island Medical Journal, 98(6), 47. [PubMed] [Google Scholar]
- Ory MG, Ahn SN, Jiang L, Lorig K, Ritter P, Laurent DD, … Smith ML (2013). National study of chronic disease self-management: Six-month outcome findings. Journal of Aging and Health, 25(7), 1258–1274. 10.1177/0898264313502531 [DOI] [PubMed] [Google Scholar]
- Ory MG, Smith ML, Ahn S, Jiang L, Lorig K, & Whitelaw N (2014). National study of chronic disease self-management: Age comparison of outcome findings. Health Education & Behavior, 41(Suppl. 1), 34S–42S. 10.1177/1090198114543008 [DOI] [PubMed] [Google Scholar]
- Schulz KF, Altman DG, & Moher D (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Trials, 11(32), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Belza B, Altpeter M, Ahn S, Dickerson JB, & Ory MG (2012). Disseminating an evidence-based disease self-management program for older Americans: Implications for diversifying participant reach through delivery site adoption. In Maddock J(Ed.), Public health: Social and behavioral health (pp. 385–404). IntechOpen. Available from: https://www.intechopen.com/books/public-health-social-and-behavioral-health/assessing-evidence-basedprograms-for-older-americans-implications-for-diversifying-participant-reac[Last accessed 4 June 2014]. 10.5772/36728 [DOI] [Google Scholar]
- Smith ML, Cho J, Salazar CJ, & Ory MG (2013). Changes in quality of life indicators among chronic disease self-management program participants: An examination by race and ethnicity. Ethnicity and Disease, 23(2), 182–188. [PubMed] [Google Scholar]
- StataCorp LLC. (2017a). Stata 15 base reference manual. College Station, TX: Stata Press. [Google Scholar]
- StataCorp LLC. (2017b). Stata/SE (version 13.0). College Station, TX: Stata Press. [Google Scholar]
- U. S. Department of Health and Human Services. (2010a). Healthy people 2020. In Washington, DC. [Google Scholar]
- U. S. Department of Health and Human Services. (2010b). Multiple chronic conditions – A strategic framework: Optimum health and quality of life for individuals with multiple chronic conditions. Retrieved from Washington, DC. [Google Scholar]
- U. S. Department of Health and Human Services. (2011). HHS implementation guidance on data collection standards for race, ethnicity, sex, primary language, and disability status. Office of the Assistant Secretary for Planning and Evaluation; Retrieved from https://aspe.hhs.gov/basic-report/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-and-disability-status [Google Scholar]


