Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic impacted cancer services worldwide. We examined the effect of the first three pandemic waves on the number of electronic (e)-referrals to rapid access clinics (RACs) for breast, lung and prostate cancer in Ireland.
Methods
This study used a retrospective, repeated cross-sectional design. The predicted weekly number of e-referrals by suspected cancer types from March 2020 to May 2021 was calculated using the Holt-Winters seasonal smoothing method, based on the observed numbers from a representative pre-pandemic period (01 January 2019 to 01 March 2020) and compared this with the observed number across the first three pandemic waves (02 March 2020 to 09 May 2021). Percentage differences were calculated between observed and predicted numbers of e-referrals for the three RACs and patterns were examined in each wave.
Results
Observed e-referrals were lower than predicted for all three RACs in the first wave of the pandemic (15.7% lower for breast, 39.5% lower for lung and 28.1% lower for prostate) with varying levels of recovery in the second and third waves for the three e-referral types.
Conclusions
The COVID-19 pandemic impacted patterns of e-referrals to RACs in the first three pandemic waves in Ireland. Early identification of changes in engagement with health services, such as a decrease in primary care presentations with a resultant decrease in e-referrals to RACs can allow for a rapid response from cancer control programmes. Continued surveillance of the impact of service disruption on cancer services allows policy makers and strategic leaders in cancer control programmes to respond rapidly to mitigate the impact on cancer outcomes.
Introduction
In March 2020, the World Health Organization declared the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), to be a global pandemic.1 The first coronavirus disease 2019 (COVID-19) case was confirmed in Ireland on 29th February 2020.2 From 12th March, the level of public health mitigation measures was upgraded due to the increasing high rate of COVID-19 infection, which impacted on healthcare services.3 In response to an increase in COVID-19 cases in the acute hospital system, health services were curtailed. The reconfiguration of health care services disrupted standards of care and internationally was associated in the literature with worse outcomes for those with non-COVID-19 illnesses, though the true impact is still to be determined.4,5
With the reconfiguration of health services and care pathways there was disruption to many aspects of cancer care, including to diagnostic services.6 A delay in diagnosis may result in a later stage at presentation. This would impact on the complexity of care needed and may lead to increased cancer mortality. A major concern was the potential for delayed presentation of those with cancer symptoms for investigation.6 Despite an increase in telephone consultations, visits to general practitioners (GPs) decreased.7 A UK study demonstrated a decrease in GP consultations for the clinical features of cancer of 24.2% between 2019 and 2020, particularly in the first wave of the pandemic.8 Modelling studies have shown that delays in cancer diagnoses due to the COVID-19 pandemic are expected to result in an increase in deaths due to cancer.9,10 Ultimately, the potential for delayed cancer diagnoses will have an impact on planning for cancer management in the coming years with cancer diagnosed at a later stage, being more difficult to treat, more likely to reduce survival and result in increased costs to health services.9
In Ireland, there are eight designated adult cancer centres that provide rapid access clinics (RACs) to investigate patients with suspected breast, lung and prostate cancers. Patients can be referred to RACs by GPs or from the emergency department of acute hospitals. Referral to RACs by GPs nationally are electronic referrals (e-referrals) through a secure messaging system called Healthlink.11 Prior to the COVID-19 pandemic, GP e-referrals accounted for 80% of referrals to symptomatic breast, lung and prostate clinics.6 Cancers detected in RACs represent 21% of cancers (excluding non-melanoma skin cancer; NMSC) diagnosed annually in Ireland.12
In response to the COVID-19 pandemic in Ireland, the NCCP in conjunction with the Department of Health instigated a number of key actions to mitigate the impact on cancer patients.13 To inform these actions, and due to the concern regarding delayed presentation of patients with cancer symptoms, Healthlink provided weekly data to the Health Service Executive (HSE) National Cancer Control Programme (NCCP). Healthlink data provided near real time data and was used as a proxy to measure engagement with health services during the pandemic and the impact of the pandemic on cancer referral patterns.14
This study builds on previous reports which showed that referrals to RACs were adversely impacted during the COVID-19 pandemic with overall clinic attendance activity for the three RACs in Ireland at 88.1% of 2019 levels.6,12 The aim of this study was to examine the impact of the COVID-19 pandemic on e-referrals to RACs for breast, lung and prostate cancer during the first three pandemic waves in Ireland.
Methods
Study design and data source
The reporting of this study conforms to the STROBE statement (Supplementary table S1).15 This study used a retrospective, repeated cross-sectional design using Healthlink data.11 Healthlink is a web-based service for the secure transfer of patient information between hospitals, healthcare agencies and GPs, and captures e-referrals for suspected breast, lung and prostate cancer nationally. Anonymized aggregate data on weekly numbers of e-referrals were provided by the HSE NCCP in Ireland, which captured all referrals from GPs to each of RACs via Healthlink. The timeline of the pandemic waves was modified from the Health Protection Surveillance Centre (HSPC) definitions.16 E-referral data are reported from a Monday to Sunday as opposed to the pandemic waves which are defined by the HPSC from Sunday to Saturday (see table 1 for the period relating to the first three waves). E-referral data were assessed up to 9th May 2021 due to the occurrence of a cyber-attack on national health computer systems on Friday 14th May which severely impacted the functioning of health services in Ireland.17
Table 1.
COVID-19 pandemic waves covered in the data analysis.
| Wave | COVID-19 pandemic wave period | Week number |
|---|---|---|
| 1 | 02 March 2020 to 02 August 2020 | Week 10–31 (2020) |
| 2 | 03 August 2020 to 22 November 2020 | Week 32–47 (2020) |
| 3 | 23 November 2020 to 09 May 2021 | Week 48 (2020)–week 19 (2021) |
Statistical analysis
The predicted weekly number of e-referrals by suspected cancer types was calculated for the scenario of an absence of the pandemic, based on observed weekly e-referral numbers from the pre-pandemic period (01 January 2019 to 01 March 2020). The predicted weekly number of e-referrals by suspected cancer types was calculated using the Holt-Winters (HW) seasonal smoothing method, which controlled for the exponential weighted moving average and seasonal trends in time series data forecast.18 Percentage difference for observed 2019 and observed 2020 e-referral numbers by cancer type was calculated as follows: difference in percentage between 2020 and 2019 numbers: (observed 2020 − observed 2019)/observed 2019. A positive difference indicated a higher number of observed e-referrals than predicted e-referrals, while a negative difference indicated a lower number of observed than predicted e-referrals.
Descriptive analyses of weekly observed and predicted numbers of e-referrals were used to analyse trends in e-referrals to the three RACS through the first three waves of the pandemic. All analyses were performed using Stata SE 17.0. The graphs were generated using Tableau Desktop 2022.
Sensitivity analysis
To further examine the accuracy of predicted number of e-referrals, the weekly e-referral numbers for breast and lung RACs in 2018 were included with 2019 numbers in the pre-pandemic baseline period and used to calculate the predicted number of e-referrals for the pandemic period (02 March 2020 and 09 May 2021). Due to the continuing roll out and uptake of the e-referral system for suspected prostate cancer in 2018, we did not include this data in the sensitivity analysis.
Ethical approval
This study used fully anonymized aggregated electronic referral data, provided by the NCCP for the purpose of this analysis, and therefore ethical approval was not required.
Results
E-referrals for breast, lung and prostate cancer between 2019 and 2020 and predicted and observed for 2020
Comparison of the observed numbers of e-referrals for all three RACs for January to December 2019 and 2020 demonstrated that in 2020 observed e-referrals were at 112% (45 585) of those observed in 2019 (40 210). The observed and predicted number of e-referrals for 2020 and for the first three pandemic waves is shown in table 2.
Table 2.
Annual total number of e-referrals by suspected cancer type for 2019 and 2020 and observed and predicted number of e-referrals by suspected cancer type for each pandemic wave.
| Breast e-referrals | Lung e-referrals | Prostate e-referrals | ||
|---|---|---|---|---|
| Annual total | Observed 2019 | 35 026 | 1713 | 3471 |
| Observed 2020 | 40 592 | 1586 | 3407 | |
| Difference between 2019 and 2020 | 5566 | −127 | −64 | |
| % Difference between 2019 and 2020 | 15.9% | −7.4% | −1.8% | |
| Wave 1 | Observed | 14 287 | 545 | 1126 |
| (02 March 2020 to 02 August 2020) | Predicted | 16 954 | 901 | 1566 |
| Difference | −2667 | −356 | −440 | |
| % Difference | −15.7% | −39.5% | −28.1% | |
| Wave 2 | Observed | 14 803 | 469 | 1204 |
| (03 August 2020 to 22 November 2020) | Predicted | 13 254 | 648 | 1202 |
| Difference | 1549 | −179 | 2 | |
| % Difference | 11.7% | −27.6% | −0.2% | |
| Wave 3 | Observed | 22 807 | 733 | 1654 |
| (23 November 2020 to 09 May 2021) | Predicted | 19 159 | 866 | 1917 |
| Difference | 3648 | −133 | −263 | |
| % Difference | 19.0% | −15.4% | −13.7% |
Comparison of trends in observed and predicted e-referrals for suspected breast, lung and prostate cancer
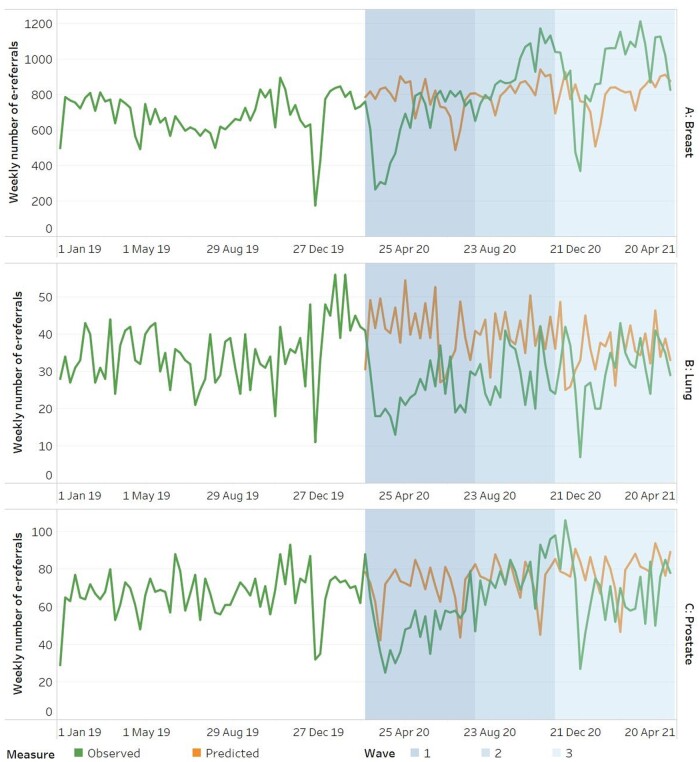
E-referrals were consistently low in weeks 51 and 52 in 2019 and 2020 due to the seasonal reduction in GP and acute hospital services during holiday periods. For breast e-referrals in the first pandemic wave (shaded area 1, figure 1A), there were 15.7% lower e-referrals than predicted (table 2). In the second and third wave (shaded areas 2 and 3, figure 1A), there was a recovery in numbers of e-referrals to suspected breast cancer RACs with a positive difference between observed and predicted e-referrals of 11.7% and 19.0%, respectively (table 2).
Figure 1.
(A–C) Number of observed and predicted new e-referrals RACs between 1 January 2019 and 9 May 2021 (shaded areas 1, 2 and 3 represent the three distinct pandemic waves). (A) Breast cancer e-referrals. (B) Lung cancer e-referrals. (C) Prostate cancer e-referrals.
For suspected lung cancer RACs (figure 1B), there were 39.5% fewer e-referrals than predicted in the first pandemic wave (shaded area 1) (table 2). The observed number of weekly e-referrals for suspected lung cancer remained lower than predicted for the second and third pandemic waves (27.6% lower and 15.4% lower, respectively, table 2) with some recovery seen towards the end of the third wave (figure 1B).
For suspected prostate cancer RACs (figure 1C), there were 28.1% fewer e-referrals than predicted in the first pandemic wave (table 2). A recovery was seen in the second pandemic wave with numbers of observed e-referrals just above predicted numbers (table 2). However, in the third pandemic wave (shaded area 3, figure 1C) numbers of observed e-referrals were below what was predicted (13.7% fewer than predicted, table 2) with no recovery seen (figure 1C).
Sensitivity analysis
In the sensitivity analysis, calculation of predicted e-referrals for each RAC using both 2018 and 2019 data in the pre-pandemic baseline data versus using 2019 data alone demonstrated similar predictions (Supplementary table S2 and Supplementary figure S1).
Discussion
In this study, we identified three key findings. Firstly, observed numbers of e-referrals in 2020 (45 585) were 112% of those observed in 2019 (40 210). This increase was accounted for mainly by the increase in breast e-referrals. The reasons for this increase are most likely multifactorial but may be partially accounted for by the increase in GP e-referrals during the pandemic to over 95% from 80% pre-pandemic.6 Secondly, observed e-referrals for suspected breast, lung and prostate cancer RACs in the first wave of the pandemic (02 March 2020 to 02 August 2020) were lower than predicted. Thirdly, there was varying levels of recovery of e-referrals for each suspected cancer type throughout the first three pandemic waves.
The lower than predicted number of e-referrals for suspected breast, lung and prostate cancer to RACs in the first wave of the pandemic is consistent with international findings.19 Early cancer registry data from across Europe has shown a significant decrease in the numbers of incident cancers diagnosed in the early stages of the pandemic in April 2020, consistent with a decrease in patients presenting with concerning symptoms and subsequent referrals.20,21 In Ireland, national cancer registry data has shown a 10% reduction in cancer incidence in 2020 compared to what was projected for 2020.22 A systematic review on breast cancer screening and diagnosis during the pandemic demonstrated a ≥25% reduction in breast cancer diagnoses in the majority of studies performed on a similar period to our study, from January 2020 to March 2021.23 Reasons for a decrease in incident cancers diagnosed include changes to delivery of normal cancer services during the pandemic, including decreased capacity of diagnostic services, pausing of screening services and changes in engagement with health services.4 A recent study in England of over eight million electronic health records of primary care patients demonstrated that consultations for symptoms that were suspicious for cancer decreased by 24% between 2019 and 2020, particularly in the 6–12 weeks after the beginning of the first wave.8 Urgent referrals decreased by 10.5% for the same period. These findings suggest that the decrease in referrals was due to fewer patients presenting with symptoms. This potential alteration in engagement with health services may have been due to the restrictions imposed during pandemic wave ‘lockdowns’ or systemic factors creating barriers to access. During ‘lockdowns’ people were urged to cocoon and at times not to travel more than 5 km from their homes.24 Systemic factors included closure of primary care facilities due to lack of staff due to isolation or lack of availability of in person appointments for patients with respiratory symptoms.7
Our findings showed different patterns of recovery across the three suspected cancer types examined. In England, differences in recovery times by cancer type were also found, with recovery for breast cancer referrals quicker than referrals for suspected prostate and lung cancer.25 It is likely the differing recovery rates were impacted by the establishment of COVID-19 pathways for those with lung symptoms,6 age profile of patients with symptoms and patient attendance at GP.
Breast cancer is the second most common cancer in Ireland (excluding NMSC) comprising almost one-third of all cancer cases in women.22 Between 2018 and 2020, there were on average 3363 new cases of invasive breast cancer diagnosed annually in females in Ireland. Patterns of e-referrals to suspected breast cancer RACs demonstrated a reduction at the onset of the first wave, with a recovery in the latter half of the first wave. This is consistent with international literature.26 A UK paper demonstrated a fall in urgent breast referrals between January and July 2020 (77% of same period 2019), an increase from July to December 2020 (106% of same period 2019) and an increase in January to July 2021 (110% of same period 2019).26 This increase is consistent with our findings; however, the increase in Ireland was greater with e-referrals to suspected breast cancer RACs in January to July 2021 at 137% of the same period in 2019. This increase may reflect the fact that the population-based breast screening services in Ireland were paused between March 2020 and October 2020 and again in January to March 2021. It is possible that women who were asymptomatic and would have been picked up by screening presented instead to the GP with symptoms and were referred to the RAC. In England, delays of up to 7 months in breast cancer screening due to the COVID-19 pandemic is estimated, in a modelling study, to have resulted in a shift from screening detected to symptomatic breast cancer in the region of 2500–4100 cases, which would lead to between 148 and 452 additional breast cancer deaths.27
Lung cancer is the leading cause of death due to cancer worldwide.28 In Ireland, lung cancer is the third most common cancer in males and females combined, excluding NMSC with an average of 2668 lung cancer cases diagnosed each year between 2018 and 2020.22 Management of patients with lung cancer presents challenges because a large proportion present with late-stage disease, with a resulting reduced five-year survival.29 The Surveillance, Epidemiology and End Results Program (SEER) reports that up to 55% of lung cancer cases present with distant metastases and that these cases have only a 7% relative five-year survival.30 Our study findings highlight that suspected lung cancer e-referrals in Ireland were impacted during the first three pandemic waves, with a sustained lower number of observed referrals compared to predicted numbers. While recovery occurred towards the end of the third wave, where predicted numbers of e-referrals were similar to observed numbers, it is not clear if this was a sustained recovery. Similar results have been noted in lung referrals in the urgent cancer referral pathway in England, where there was a sustained reduction in referrals to the suspected lung cancer two-week wait pathway between March 2020 and August 2021 and a 26% reduction of suspected lung cancer referrals overall for that period.31
During the pandemic, there was evidence of a significant shift to remote consultations for those with respiratory symptoms.32 An Irish study highlighted that healthcare providers expressed concern regarding missed lung cancer diagnosis due the lack of ability to appraise symptoms, such as weight loss, over the phone.33 It is likely that suspected lung cancer e-referrals to the RACs will have been affected by the introduction of COVID-19 pathways in primary care and acute hospital settings, where patients presenting with a cough or other respiratory symptoms underwent adapted triage and treatment protocols to minimize potential spread of COVID-19 in these settings.34 Reasons for this have been postulated to be due to more patients being referred to secondary care via different pathways to the RACs including from COVID-19 community hubs due to the overlapping symptoms of COVID-19 and lung cancer.31 It has also been suggested that patients with overlapping symptoms between COVID-19 and lung cancer may have assumed they had COVID-19 due to the increased prevalence of COVID-19 during certain periods.35
Prostate cancer is the most common cancer in Ireland (excluding NMSC) and comprises over one-third of all cancers diagnosed each year in men with an annual average of 3941 new cases per year between 2018 and 2020.22 Suspected prostate cancer e-referrals followed a similar pattern to suspected breast cancer with a rapid decrease in e-referrals at the beginning of the first wave, and a recovery in the second wave. However, in the third wave the number of e-referrals remained below what was predicted throughout. Prostate cancer occurs in older men, with an average median age in Ireland of 68 years for 2018–2020.22 E-referrals for suspected prostate cancer are often the result of a combination of urinary symptoms and an elevated prostate specific antigen (PSA) or opportunistic screening with PSA alone. During the first three pandemic waves in Ireland, people over the age of 70 years were repeatedly advised to cocoon.24 A reduction in opportunistic screening in primary care settings may have occurred due to lower GP visits. Similar to the present study, data from Catalonia in Spain found a significant decrease in diagnoses of prostate cancer in the first wave of the pandemic and demonstrated recovery to pre-pandemic levels in July 2021.36 Data from the US demonstrated a sustained reduction in prostate referrals in three oncology practices in July 2020 at the end of the first wave.37 In the UK, data from April 2020 to March 2021 showed 55 000 fewer referrals for suspected prostate cancer compared to April 2019–March 2020.38
During the COVID-19 pandemic, there was disruption to many aspects of cancer care, including to diagnostic services.6 The impact of a delay in diagnoses can potentially extend to a later stage at diagnosis leading to more complex clinical management/treatment and ultimately increased cancer mortality. In response to the COVID-19 pandemic in Ireland, the NCCP in conjunction with the Department of Health instigated a number of key actions to mitigate the impact on cancer patients.13 To inform these actions, and due to the concern regarding delayed presentation of patients with cancer symptoms, Healthlink provided weekly data to the NCCP. Healthlink data provided near real time data and were used as a proxy to measure levels of engagement with health services and the impact of the pandemic on cancer referral patterns.14
Strengths/limitations
The study has a number of strengths in that e-referrals to RACs by GPs is the preferred route of referral to RACs as per NCCP national policy and, therefore, data on the majority of referrals were available.39 Therefore, data in this study are nationally representative. For suspected breast and prostate cancer, the majority of referrals originate from primary care and therefore e-referrals represent the majority of referrals to the relevant RACs. The period covered within the study included the first three waves of the pandemic, providing a longer timeframe than previous reports.6,12 Limitations of this study include that a small proportion of GP referrals to RACs may have been via fax and, therefore, e-referrals in this study do not report on all referrals to RACs. It is also worth noting that referrals from other hospitals or within hospitals are not made by the e-referral route and are referred by phone, fax or email and therefore not captured in these data. For example, due to late presentation in a large proportion of those diagnosed with lung cancer, it is estimated that 50% of referrals are from primary care and 50% are through other routes including the acute hospital setting.33 E-referrals capture all new referrals and duplicate first time referrals cannot be excluded from the data. However, it is likely that this number is small as the nature of the referrals is mostly urgent and managed accordingly.39 It is also worth noting that due to the aggregate nature of the Healthlink data analysed, we were also unable to explore the potential inequitable impact on specific populations or geographical regions. The lack of linked outcome data also impacts on our ability to calculate whether outcomes such as stage at presentation were affected by the disruption to routine care pathways during the pandemic. Future qualitative research would assist in further determining the challenges posed by the pandemic in relation to referring of symptomatic patients. Also, there is a need for future research to focus on identifying ‘missed’ referral opportunities, despite the change in referring practice, during the pandemic in order to learn how to mitigate the impact of future pandemics on the symptomatic assessments of primary care patients.
Conclusion
The COVID-19 pandemic impacted on e-referrals with lower than predicted numbers of e-referrals in the first three waves. Early identification of changes in levels of engagement with health services and a reduction in referrals for suspected cases allows for a rapid response from cancer control programmes. The findings in this study support the use of e-referrals as a proxy for near real time data on engagement with health services at a time of disruption of cancer services. Near real time monitoring of the impact of the COVID-19 pandemic on cancer diagnosis services will allow policy makers sufficient time to mitigate against the potential negative downstream effects on cancer outcomes. However, the differing impact on and the variable rate of recovery of e-referrals across the three suspected cancer is noteworthy and action is needed to explore the impact of these findings on clinical outcomes.
Supplementary Material
Acknowledgements
We would like to thank the project advisory group, composed of clinical and non-clinical including patient and public representatives, for providing valuable support and feedback on this project. We also acknowledge the assistance of Ms. Eileen Nolan, National Cancer Control Programme.
Contributor Information
Niamh Bambury, National Cancer Registry in Ireland, Cork, Ireland; National Cancer Control Programme, Dublin 1, Ireland; School of Public Health, University College Cork, Cork, Ireland.
Mengyang Zhang, School of Population Health, RCSI University of Medicine and Health Sciences, Dublin 2, Ireland.
Triona McCarthy, National Cancer Control Programme, Dublin 1, Ireland.
Ian Dawkins, National Cancer Control Programme, Dublin 1, Ireland.
Louise Burke, Department of Pathology, Cork University Hospital/School of Medicine, University College Cork, Cork, Ireland.
Paula Tierney, National Cancer Registry in Ireland, Cork, Ireland.
Paul M Walsh, National Cancer Registry in Ireland, Cork, Ireland.
Patrick Redmond, Department of General Practice, RCSI University of Medicine and Health Sciences, Dublin 2, Ireland.
Maeve Mullooly, School of Population Health, RCSI University of Medicine and Health Sciences, Dublin 2, Ireland.
Deirdre Murray, National Cancer Registry in Ireland, Cork, Ireland; School of Public Health, University College Cork, Cork, Ireland.
Kathleen Bennett, School of Population Health, RCSI University of Medicine and Health Sciences, Dublin 2, Ireland.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
This project is funded by the Irish Cancer Society, grant reference number CMP21BEMU. MM is supported by funding from the Health Research Board. The opinions, findings and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the view of the Irish Cancer Society or the Health Research Board.
Conflicts of interest: None declared.
Author contributions
N.B. and M.Z. drafted and reviewed the manuscript. M.Z. conducted data analysis. T.M.C. and I.D. collected data, supported data interpretation and reviewed the manuscript. L.B., P.T., P.M.W., P.R. and D.M. reviewed the manuscript. K.B. and M.M. obtained the funding, designed the study, and drafted and reviewed the manuscript. All authors approved the final manuscript draft that was submitted.
Data availability
The data underlying this article were provided by Healthlink by permission. For queries regarding this data, please contact the National Cancer Control Programme at info@cancercontrol.ie.
Key points.
Electronic (e)-referrals from general practitioners to suspected cancer rapid access clinics (RACs) were negatively impacted by the COVID-19 pandemic in the first three waves.
Recovery of e-referrals during the second and third waves varied according to suspected cancer type and remained below predicted levels for suspected lung and prostate cancer.
E-referral data provide near real-time data and may act as a proxy measure of ‘engagement with health services’ during health service disruption.
Continued monitoring of the impact of service disruption on cancer services allows policymakers and cancer control programmes to respond rapidly to mitigate the impact on cancer outcomes.
References
- 1. World Health Organisation. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19—11 March 2020 2020 January 23, 2023. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
- 2. Irish Centre for Human Rights NUoIG. Coronavirus COVID-19 Outbreak in the EU Fundamental Rights Implications—Ireland. European Union Agency for Fundamental Rights. 2020.
- 3. Department of Health, Department of the Taoiseach. New Public Health Measures Effective Now to Prevent Further Spread of COVID-19. Dublin, 2020.
- 4. Carvalho AS, Brito Fernandes Ó, de Lange M, et al. Changes in the quality of cancer care as assessed through performance indicators during the first wave of the COVID-19 pandemic in 2020: a scoping review. BMC Health Serv Res 2022;22:786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lau VI, Dhanoa S, Cheema H, et al. Non-C OVID outcomes associated with the coronavirus disease-2019 (COVID-19) pandemic effects study (COPES): a systematic review and meta-analysis. PLoS One 2022;17:e0269871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Faculty of Pathology Royal College of Physicians of Ireland, National Cancer Control Programme, et al. Cancer Care in Ireland in 2020—The Impact of the COVID-19 Pandemic. 2021.
- 7. Homeniuk R, Collins C. How COVID-19 has affected general practice consultations and income: general practitioner cross-sectional population survey evidence from Ireland. BMJ Open 2021;11:e044685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nicholson BD, Ordóñez-Mena JM, Lay-Flurrie S, et al. Consultations for clinical features of possible cancer and associated urgent referrals before and during the COVID-19 pandemic: an observational cohort study from English primary care. Br J Cancer 2022;126:948–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol 2020;21:1035–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lai AG, Pasea L, Banerjee A, et al. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open 2020;10:e043828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Healthlink. 2022. [Internet]. Available at: https://www.healthlink.ie/healthlinkhome/.
- 12. National Histopathology Quality Improvement Programme, National Cancer Control Programme, et al. Deploying Data-Driven Intelligence to Measure the Impact of COVID-19 on Cancer Care and Cancer Patients; December 2020. Available at: https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2021/01/Cancer-Care-and-COVID19-Report.pdf.
- 13. Department of Health, Health Service Executive, National Cancer Control Programme. Cancer Services in Ireland in the context of Covid-19. Dublin, Ireland: Department of Health, Health Service Executive; December 2020.
- 14. McCarthy T, Dawkins I, Burns H, Nolan E. Use of cancer e-referral data to monitor health-seeking behaviours during the COVID-19 pandemic. Eur J Public Health 2021;31:ckab165.650. [Google Scholar]
- 15. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg (London, England) 2014;12:1495–9. [DOI] [PubMed] [Google Scholar]
- 16. Health Protection Surveillance Centre. Weekly Report on the Epidemiology of COVID-19 in Ireland—Week 48, 2022. Health Protection Surveillance Centre; 2022, 08 December 2022.
- 17. Health Service Executive. Conti Cyber Attack on the HSE: Independent Post-Incident Review. Dublin; 2021.
- 18. Holt CC. Forecasting seasonals and trends by exponentially weighted moving averages. Int J Forecast 2004;20:5–10. [Google Scholar]
- 19. Watt T, Sullivan R, Aggarwal A. Primary care and cancer: an analysis of the impact and inequalities of the COVID-19 pandemic on patient pathways. BMJ Open 2022;12:e059374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Peacock HM, Tambuyzer T, Verdoodt F, et al. Decline and incomplete recovery in cancer diagnoses during the COVID-19 pandemic in Belgium: a year-long, population-level analysis. ESMO Open 2021;6:100197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Skovlund CW, Friis S, Dehlendorff C, et al. Hidden morbidities: drop in cancer diagnoses during the COVID-19 pandemic in Denmark. Acta Oncol 2021;60:20–3. [DOI] [PubMed] [Google Scholar]
- 22. National Cancer Registry Ireland. Cancer in Ireland 1994–2020: Annual Statistical Report of the National Cancer Registry. Cork: NCRI, 2022.
- 23. Li T, Nickel B, Ngo P, et al. A systematic review of the impact of the COVID-19 pandemic on breast cancer screening and diagnosis. Breast 2023;67:78–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Health Protection Surveillance Centre. Guidance on Cocooning to Protect People Over 70 years and Those Extremely Medically Vulnerable from COVID-19 – Updated Guidance from 29 June. Dublin, Ireland: Health Service Executive, 2020.
- 25. Mahase E. Cancer treatments fall as referrals are slow to recover, show figures. BMJ 2020;371:m3958. [DOI] [PubMed] [Google Scholar]
- 26. Gathani T, Reeves G, Dodwell D, et al. Impact of the COVID-19 pandemic on breast cancer referrals and diagnoses in 2020 and 2021: population-based study in England. Br J Surg 2022;109:e29–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Duffy SW, Seedat F, Kearins O, et al. The projected impact of the COVID-19 lockdown on breast cancer deaths in England due to the cessation of population screening: a national estimation. Br J Cancer 2022;126:1355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: an overview. Int J Cancer 2021;149:778–89. [DOI] [PubMed] [Google Scholar]
- 29. National Cancer Registry Ireland. Cancer Factsheet: Lung. Cork, 2018.
- 30. SEER Cancer Stat Facts: Lung and Bronchus Cancer [Internet]. National Cancer Institute. Available at: https://seer.cancer.gov/statfacts/html/lungb.html (22 February 2023, date last accessed).
- 31. Maxwell SS, Weller D. Lung cancer and covid-19: lessons learnt from the pandemic and where do we go from here? NPJ Prim Care Respir Med 2022;32:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dambha-Miller H, Hounkpatin HO, Morgan-Harrisskitt J, et al. Primary care consultations for respiratory tract symptoms during the COVID-19 pandemic: a cohort study including 70,000 people in South West England. Fam Pract 2021;39:440–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saab MM, O'Driscoll M, FitzGerald S, et al. Referring patients with suspected lung cancer: a qualitative study with primary healthcare professionals in Ireland. Health Promot Int 2022;37:daac088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Crowley P, Hughes A. The impact of the COVID-19 pandemic and the societal restrictions on the health and wellbeing of the population, on our staff and on health service capacity and delivery: a plan for healthcare and population health recovery. Version 2 (May 2021) [Internet]. May 2021. 22 Oct 2021.
- 35. Gourd E. Lung cancer control in the UK hit badly by COVID-19 pandemic. Lancet Oncol 2020;21:1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ribes J, Pareja L, Sanz X, et al. Cancer diagnosis in Catalonia (Spain) after two years of COVID-19 pandemic: an incomplete recovery. ESMO Open 2022;7:100486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Maganty A, Yu M, Anyaeche VI, et al. Referral pattern for urologic malignancies before and during the COVID-19 pandemic. Urol Oncol: Semin Orig Investig 2021;39:268–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cancer Waiting Times [Internet]. National Health Service of England. Available at: https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times/ (7 March 2023, date last accessed).
- 39. National Cancer Control Programme, Health Service Executive. NCCP Policy on Electronic Referrals from Primary Care for Patients with Suspected Cancer. 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were provided by Healthlink by permission. For queries regarding this data, please contact the National Cancer Control Programme at info@cancercontrol.ie.
Key points.
Electronic (e)-referrals from general practitioners to suspected cancer rapid access clinics (RACs) were negatively impacted by the COVID-19 pandemic in the first three waves.
Recovery of e-referrals during the second and third waves varied according to suspected cancer type and remained below predicted levels for suspected lung and prostate cancer.
E-referral data provide near real-time data and may act as a proxy measure of ‘engagement with health services’ during health service disruption.
Continued monitoring of the impact of service disruption on cancer services allows policymakers and cancer control programmes to respond rapidly to mitigate the impact on cancer outcomes.