Abstract
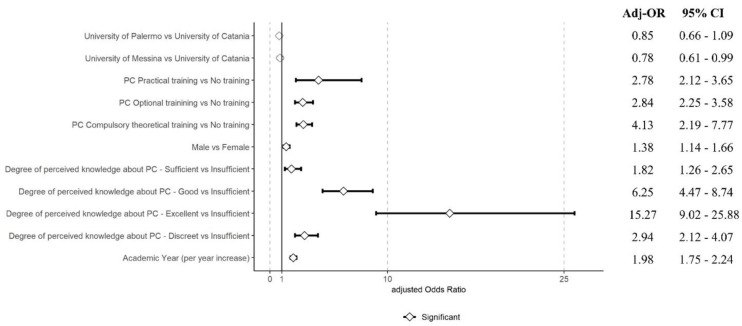
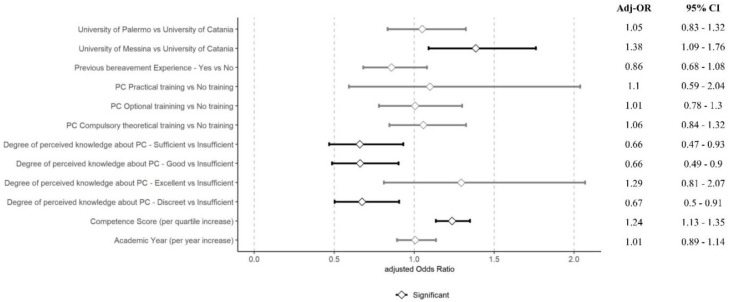
Introduction: Caring for the dying can generate anxiety and emotional distress, particularly in nursing students, and perceived competence could play a crucial role in enabling nurses to perform their duties with greater confidence. Unfortunately, few studies describe the relationship between students’ nursing attitudes and perceived self-efficacy in palliative care (PC). To overcome this gap, this survey aimed to assess the attitudes towards dying patients and the perceived competence of nursing students in palliative care at different universities in the south of Italy. Methods: A cross-sectional study was conducted from September 2022 to March 2023 involving nursing students from the three major Sicilian universities (Italy). The study included a survey investigating socio-demographic characteristics, palliative care training, knowledge about pain management, and previous experience with dying. Moreover, the Professional Competence of the Core Curriculum in Palliative Care Nursing (CCPCN) questionnaire and the Frommelt Attitudes Toward Care of the Dying—B Italian version (FATCOD-B-I) assessed competencies and emotional attitudes. Results: A total of 1913 nursing students were recruited, of which 71.3% were females, and 53.9% were in the age range of 18 to 21 years. In the multivariable analysis, practical PC training was a substantial factor in enhancing competencies (Adj-OR 2.78 [95% CI = 2.12–3.65]). Male students had higher competence odds (Adj-OR 1.38 [95% CI = 1.14–1.66]), and perceived knowledge strongly correlated with self-assessed competence. Advancement in academic years also positively influenced competence self-assessment (Adj-OR 1.98 [95% CI = 1.75–2.24]). Regarding emotional attitudes, a per-quartile increase in competence score was found to improve the attitude score (Adj-OR 1.24 [95% CI = 1.13–1.35]). Conclusions: Nursing students gain valuable experience during clinical experience. PC training and perceived knowledge of PC significantly increase nurses’ competencies, and the latter seem to be strongly associated with attitudes. Thus, introducing palliative care education into nurses’ core curricula could be a way to reduce anxiety and emotional distress in young students.
Keywords: self-assessment, competencies, attitudes, palliative care, dying, undergraduate, nursing
1. Introduction
Globally, it is estimated that 40 million individuals require palliative care (PC) annually, a demand projected to rise significantly in the forthcoming years, particularly in the realm of end-of-life care and dying [1,2]. The primary objective of PC is to enhance the quality of life for patients and their families by preventing and treating pain, along with addressing physical, psychosocial, and spiritual issues until death and beyond. PC neither hastens nor postpones death but views it as a natural process, employing an interdisciplinary approach that emphasizes personalized care delivered by various healthcare practitioners [2,3].
Among healthcare practitioners, nurses spend the most time with dying patients and their families, often witnessing the process of death [4,5]. They are a crucial support system for the patient, family, and caregivers [6,7].
Generally, PC can be an emotionally challenging and sometimes threatening experience for nurses because it needs advanced skills, appropriate attitudes, and a natural acceptance of dying and death [8,9]. Death can trigger intense emotional reactions, influenced by several factors, including individual perceptions of death, values, beliefs, past experiences, and cultural characteristics [10,11]. Dealing with death and caring for patients in palliative care can induce stress in nurses, eliciting feelings of helplessness, nervousness, guilt, regret, sadness, anxiety, frustration, anger, and repulsion, possibly because the propensity to care for dying individuals is not innate [12,13].
Caring for the dying can generate anxiety, terror, and emotional distress, particularly in nursing students due to fear of their reactions to death, loss of control, and perceived inability to provide adequate and sensitive support to patients and family members [14]. Such feelings can foster negative attitudes towards the care of dying patients [15].
Positive attitudes, specific knowledge, and perceived competence (self-efficacy) in PC and end-of-life care are pivotal to adequately supporting these patients and influencing the quality of palliative care [9,16]. According to the Shared Theory of Palliative Care, the ability of nurses to provide competent palliative care is linked to their perceived competence [17]. Perceived competence is crucial in enabling nurses to confidently perform their duties [9].
The literature suggests that undergraduate nursing students lack the competence to provide palliative care and feel unprepared for palliative care and encountering death [18,19,20]. People tend to avoid situations requiring a skill when perceived competence is low. Conversely, individuals demonstrate more persistent determination toward completing an action when perceived competence is high. Therefore, educators should evaluate students’ perceived competence as it can impact the provision of palliative care [21].
Studies worldwide on nursing students’ attitudes towards care of the dying have identified several factors that can positively or negatively influence these attitudes, showing often contradictory results. Researchers have widely investigated death attitude as a possible factor impacting attitudes toward care of the dying [22]. The literature suggests that nurses and nursing students who have a more positive attitude towards death are more likely to have a positive attitude towards end-of-life care [4,11,23,24,25,26,27,28].
The training received in palliative and end-of-life care is the factor that can most influence attitudes towards care of the dying [29,30]. Studies conducted in different parts of the world have shown that nursing students’ attitudes improve with specific education in palliative care [30,31,32,33], although in a study conducted in Indonesia, training had no relation to students’ attitudes to care of the dying [34]. Being a woman [11], year of study, and older age are significant predictors of positive attitudes [9,26], while religiosity and cultural and social circumstances could also be influential [23,35]. Religiosity, in fact, in a study carried out on a Swedish–Iranian sample, increased negative attitudes towards caring for people who were dying [24].
A multicenter European study involving Spain, England, and Italy assessed nursing students’ attitudes towards caring for dying patients using the FATCOD-B scale. The study found that students across all three countries showed moderate attitudes, with scores falling in the middle range of the scale. Italian students demonstrated slightly more positive attitudes compared to their Spanish and English counterparts, although this difference was not statistically significant. Interestingly, the study reported that various factors such as age, sex, year of study, religious beliefs, palliative care nursing education, previous experience with dying patient care, and personal bereavement did not significantly influence these attitudes. This suggests a relatively consistent baseline attitude among nursing students across these countries, regardless of personal or educational factors [36]. An Italian study showed that higher scores were significantly associated with training in palliative care and experience with terminally ill patients. Moreover, students described more negative attitudes when they perceived patients losing hope of recovering and patients’ family members interfering with health professionals’ work. They believe caring for a terminally ill patient is a helpful learning experience but feel they need to be adequately prepared in practice [37]. Specific training should improve nursing students’ knowledge and self-perceived competence about palliative care and end-of-life care, thus enhancing a positive death attitude to better deal with dying patients, increasing self-awareness on death, and allowing to provide quality care [35,38]. However, to orientate nursing education appropriately, more knowledge about nursing students’ self-perceived competence in palliative care and attitudes towards care of the dying is needed [37,39].
Only a few studies have described the relationship between nursing students’ attitudes and perceived self-efficacy in palliative care [9,40], particularly on undergraduate nursing students.
In order to obtain a clearer picture of the attitudes towards dying patients and the perceived competence of nursing students in palliative care, the objective of this survey is to assess these two essential aspects in different universities in the south of Italy.
2. Methods
2.1. Design, Instruments, and Data Collection
This cross-sectional study involved 1913 nursing students from three Italian universities: the University of Messina, the University of Palermo, and the University of Catania. The study utilized a two-section questionnaire. These participants represented 89% of the total enrolled nursing students across the three universities (N = 2150). Students were contacted using the official university email databases for nursing degree programs, ensuring a comprehensive reach to the target population. Non-responders were proportionally distributed among the three universities: 97 from Messina (10% of the total students), 85 from Palermo (11%), and 30 from Catania (7%). The first questionnaire section collected data on socio-demographic characteristics such as sex, age, year of study, PC education, perceived degree of knowledge about pain management, previous experience with dying individuals, previous bereavement experience, current bereavement experience, religion, and university affiliation. In the second section, two specific instruments were used:
Professional Competence of the Core Curriculum in Palliative Care Nursing (Professional Competence-CCPCN) [41]: This instrument, composed of 24 items, was used to measure students’ perceived competence in palliative care. Each item is scored on a scale from 0 to 10, with higher scores indicating higher perceived competence. The total score was divided into quartiles (q1, q2, q3, q4).
Frommelt Attitudes Toward Care of the Dying—B Italian version (FATCOD-B-I) [42]: This questionnaire, consisting of 30 items, gauges attitudes towards care of the dying. The scoring is based on a five-point Likert scale ranging from “strongly agree” to “strongly disagree”. Fifteen items (1, 2, 4, 10, 12, 16, 18, 20, 21, 22, 23, 24, 25, 27, and 30) are formulated positively, and the remaining fifteen negatively. The response scale is a 5-point Likert-type scale. For positive items, the score ranges from 1 (“Strongly disagree”) to 5 (“Strongly agree”). For negative items, the score is reversed. The total score ranges between a minimum of 30 and a maximum of 150, with higher scores indicating more positive attitudes. Scores > 65% of the total possible score (>97.5) were considered as positive attitudes, those between 50% and 65% (>75–<97.5) as neutral, and those below 50% (<75) as negative. The total score was categorized into equal quartiles (eq1, eq2, eq3, eq4) to assess emotional attitudes. Data were collected over the period from September 2022 to March 2023. The questionnaire was delivered to participants online through a survey platform, ensuring convenience and anonymity.
2.2. Inclusion and Exclusion Criteria
All students, regardless of sex and with no age limit, were included in the 1st, 2nd, and 3rd years, as well as out-of-course students of the Degree Courses in Nursing at each of the three universities. This includes both native speakers and international students with an excellent command of the Italian language. International students unfamiliar with the Italian language, or those who did not consent to participate, were excluded.
2.3. Bachelor’s Degree in Nursing Science and Palliative Care Curricula
In Italy, a bachelor’s degree in nursing science spans three years, amounting to 180 European Credit Transfer System (ECTS) credits (1 ECTS = 30 h), with at least 70 ECTS credits dedicated to internships to develop specific skills in various clinical areas. Training in palliative care in the three universities under study is organized as reported below:
-
(a)
The Palermo program, in the third year, provides 3 ECTS credits of a compulsory theoretical module;
-
(b)
The Messina program offers 2 ECTS credits in the second year;
-
(c)
The Catania program does not have a compulsory dedicated training but allows students to participate in an optional didactic activity.
Clinical placements for palliative care apprenticeships are provided in all three universities, but they are limited and not compulsory.
2.4. Statistical Analysis
Quantitative variables are summarized using the mean and standard deviation (or median and inter-quartile range where appropriate). Qualitative variables are expressed as absolute frequencies and percentages.
In the univariate analysis, Chi-square tests were performed to examine the association between competence or emotional attitude quartiles (based on Professional Competence-CCPCN and FATCOD-B-I scores, respectively) and categorical variables from the first part of the questionnaire. Age was stratified into categories reflecting presumed variations in education level. Quartiles for each scale were derived from the score distributions, arranging the dataset in ascending order. Thresholds for quartiles for each scale were established according to the distribution, segmenting the dataset into four groups of equal size. Each participant was subsequently allocated into a specific quartile based on their total score. For instance, a participant with a score falling within the range of the first quartile for the Professional Competence-CCPCN scale was assigned to the first competence quartile (q1), and the process was analogous for the FATCOD-B-I scale. Quartile analysis is a robust method for examining the distribution of scores and allows for comparing group characteristics across the spectrum of the dataset. Subsequently, we performed multinomial ordinal regression to define variables able to predict competence and emotional attitudes quartiles (based on Professional Competence-CCPCN and FATCOD-B-I scores, respectively). The adjusted odds ratios (Adj-OR) and their 95% confidence intervals (CI) were then calculated.
A p-value of less than 0.05 was considered statistically significant. R Studio software version 2023.12.1 was used for the statistical analyses, including the following packages: dplyr, ggplot2, car, and nnet for ordinal multinomial regression.
2.5. Ethical Issues
The study was conducted following the principles of the Helsinki Declaration and was approved by the Local Ethics Committee (Ethics Committee Palermo 1 N. 05/2022, 11 May 2022). Students received detailed oral and written information about the study. Those who agreed to participate provided informed consent. The anonymity of the participants was guaranteed throughout the entire data analysis and reporting process.
3. Results
A total of 1913 students were included in the analyses (Table 1), a robust proxy of the total population of nursing students in Sicily (89%). Distribution by university was as follows: University of Messina (42.6%), University of Palermo (35.5%), and University of Catania (21.8%). The cohort predominantly consisted of females (71.3%) aged 18 to 21 years (53.9%). The competence score quartiles, based on even distribution among the participants, are detailed in Table 2. Univariate analyses showed a significant association between emotional attitudes and competence, particularly notable in the upper quartiles. For instance, a higher proportion of students in the top emotional attitude quartile (eq4) were also in the highest competence quartile (q4, 37%), with the converse true for the lowest quartile (q1, 22%) (p < 0.001). A significant variation in distribution among the universities was observed across competence quartiles (p < 0.001), with the University of Messina contributing more to the highest quartile and the University of Catania contributing more to the lowest. Sex showed no significant difference across quartiles, whereas age was statistically significantly associated with different competency quartiles (p < 0.001). The academic year of study was a differentiator, with first-year students primarily in the lowest quartile (50%) and those in their third year or higher in the top quartiles (q3 and q4) (p < 0.001). Palliative care (PC) training also correlated significantly with higher competence quartiles, where students who completed compulsory theoretical training were predominantly in the upper half (q3 and q4).
Table 1.
Demographic and experiential characteristics of the nursing students.
| Students’ Characteristics | University of Catania N = 417 |
University of Messina N = 816 |
University of Palermo N = 680 |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sex | |||
| Female | 299 (71.7) | 609 (74.6) | 457 (67.2) |
| Male | 118 (28.3) | 207 (25.4) | 223 (32.8) |
| Age (years) | |||
| 18–21 | 202 (48.4) | 431 (52.8) | 398 (58.5) |
| 22–25 | 145 (34.8) | 248 (30.4) | 173 (25.4) |
| 26–30 | 49 (11.8) | 89 (10.9) | 57 (8.4) |
| >30 | 21 (5.0) | 48 (5.9) | 52 (7.6) |
| Year of Study | |||
| First | 153 (36.7) | 365 (44.7) | 258 (37.9) |
| Second | 134 (32.1) | 248 (30.4) | 254 (37.4) |
| Third or + | 130 (31.2) | 203 (24.9) | 168 (24.7) |
| PC Education | |||
| Compulsory theoretical training | 81 (19.42) | 429 (52.6) | 250 (36.8) |
| Optional training | 16 (3.8) | 160 (19.6) | 116 (17.1) |
| Practical training | 10 (2.4) | 14 (1.7) | 11 (1.6) |
| No | 310 (74.3) | 213 (26.1) | 303 (44.6) |
| Perceived degree of knowledge about pain management | |||
| Insufficient | 27 (6.5) | 73 (9) | 102 (15) |
| Good | 156 (37.4) | 309 (37.9) | 195 (28.7) |
| Moderate | 170 (6.5) | 282 (34.6) | 265 (39) |
| Sufficient | 49 (11.8) | 96 (11.8) | 93 (13.7) |
| Excellent | 15 (3.6) | 56 (6.9) | 25 (3.7) |
| Previous experience with dying individuals | |||
| Internship in PC | 15 (3.6) | 38 (4.7) | 16 (2.4) |
| Internship in other settings | 143 (34.3) | 90 (11.0) | 170 (25) |
| Personal experience | 76 (18.32) | 235 (28.8) | 158 (23.2) |
| Working experience | 10 (2.4) | 20 (2.5) | 17 (2.5) |
| No | 173 (41.5) | 433 (53.1) | 319 (46.9) |
| Previous bereavement experience | |||
| Yes | 348 (83.9) | 701 (85.9) | 568 (83.5) |
| No | 69 (16.5) | 115 (14.1) | 112 (16.5) |
| Current bereavement experience | |||
| No | 350 (83.9) | 685 (83.9) | 576 (84.7) |
| I am preparing for the death of a loved one | 14 (3.4) | 37 (4.5) | 24 (3.5) |
| I am grieving for a loved one who recently passed away | 53 (12.7) | 94 (11.5) | 80 (11.8) |
| Religion | |||
| Agnostic or atheist | 114 (27.3) | 143 (17.5) | 199 (29.3) |
| Catholic Christians | 286 (68.6) | 646 (79.2) | 458 (67.4) |
| Other (Muslim, Jewish, Protestant) | 17 (4.1) | 27 (3.3) | 23 (3.4) |
Table 2.
Competence quartiles from the Professional Competence-CCPCN questionnaire scores.
| Competence Score Quartile | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | q1 | % | q2 | % | q3 | % | q4 | % | p-Value |
| N | 480 | 477 | 480 | 476 | |||||
| Emotional attitudes (%) | <0.001 | ||||||||
| eq1 | 149 | 29% | 146 | 28% | 134 | 26% | 85 | 17% | |
| eq2 | 110 | 24% | 123 | 27% | 127 | 27% | 103 | 22% | |
| eq3 | 127 | 25% | 122 | 24% | 128 | 25% | 126 | 25% | |
| eq4 | 94 | 22% | 86 | 20% | 91 | 21% | 162 | 37% | |
| University (%) | <0.001 | ||||||||
| Catania | 84 | 20% | 145 | 35% | 113 | 27% | 75 | 18% | |
| Messina | 203 | 25% | 167 | 20% | 192 | 24% | 254 | 31% | |
| Palermo | 193 | 28% | 165 | 24% | 175 | 26% | 147 | 22% | |
| Sex (%) | 0.13 | ||||||||
| Female | 360 | 26% | 344 | 25% | 331 | 24% | 330 | 24% | |
| Male | 120 | 22% | 133 | 24% | 149 | 27% | 146 | 27% | |
| Age (years) (%) | <0.001 | ||||||||
| 18–21 | 308 | 30% | 253 | 25% | 225 | 22% | 245 | 24% | |
| 22–25 | 87 | 15% | 156 | 28% | 180 | 32% | 143 | 25% | |
| 26–30 | 43 | 22% | 47 | 24% | 46 | 24% | 59 | 30% | |
| 30+ | 42 | 35% | 21 | 17% | 29 | 24% | 29 | 24% | |
| Academic year (%) | <0.001 | ||||||||
| First | 388 | 50% | 148 | 19% | 99 | 13% | 141 | 18% | |
| Second | 71 | 11% | 215 | 34% | 184 | 29% | 166 | 26% | |
| Third or + | 21 | 4% | 114 | 23% | 197 | 39% | 169 | 34% | |
| PC education (%) | <0.001 | ||||||||
| Compulsory theoretical training | 65 | 9% | 176 | 23% | 255 | 34% | 264 | 35% | |
| No | 355 | 43% | 218 | 26% | 139 | 17% | 114 | 14% | |
| Optional training | 58 | 20% | 78 | 27% | 73 | 25% | 83 | 28% | |
| Practical training | 2 | 6% | 5 | 14% | 13 | 37% | 15 | 43% | |
| Perceived degree of knowledge about pain management (%) | <0.001 | ||||||||
| Insufficient | 125 | 62% | 47 | 23% | 17 | 8% | 13 | 6% | |
| Sufficient | 84 | 35% | 78 | 33% | 49 | 21% | 27 | 11% | |
| Moderate | 158 | 22% | 211 | 29% | 215 | 30% | 133 | 19% | |
| Good | 95 | 14% | 133 | 20% | 185 | 28% | 247 | 37% | |
| Excellent | 18 | 19% | 8 | 8% | 14 | 15% | 56 | 58% | |
| Previous experience with dying individuals (%) | <0.001 | ||||||||
| Internship in another setting | 22 | 5% | 108 | 27% | 156 | 39% | 117 | 29% | |
| Internship in PC | 1 | 1% | 16 | 23% | 24 | 35% | 28 | 41% | |
| No | 318 | 34% | 227 | 25% | 182 | 20% | 198 | 21% | |
| Personal experience | 136 | 29% | 116 | 25% | 103 | 22% | 114 | 24% | |
| Working experience | 3 | 6% | 10 | 21% | 15 | 32% | 19 | 40% | |
| Previous bereavement experience (%) | 0.96 | ||||||||
| No | 71 | 24% | 75 | 25% | 77 | 26% | 73 | 25% | |
| Yes | 409 | 25% | 402 | 25% | 403 | 25% | 403 | 25% | |
| Current bereavement experience (%) | 0.78 | ||||||||
| I am grieving for a loved one who recently passed away | 64 | 28% | 50 | 22% | 54 | 24% | 59 | 26% | |
| I am preparing for the death of a loved one | 16 | 21% | 22 | 29% | 20 | 27% | 17 | 23% | |
| No | 400 | 25% | 405 | 25% | 406 | 25% | 400 | 25% | |
| Religion (%) | 0.08 | ||||||||
| Agnostic or atheist | 117 | 25% | 118 | 26% | 135 | 29% | 92 | 20% | |
| Catholic Christian | 349 | 25% | 340 | 25% | 330 | 24% | 367 | 26% | |
| Other (Muslim, Jewish, Protestant) | 14 | 22% | 19 | 29% | 15 | 23% | 17 | 26% | |
Knowledge about pain management was significantly associated with competence level, with students self-rating as “excellent” being mostly in the top quartile (p < 0.001). Experience with dying individuals was associated with higher competence, but bereavement experience and religious beliefs were not.
Students were also categorized into quartiles for emotional attitude based on FATCOD-B-I scores, with significant differences in distribution among universities (p = 0.0035) (Table 3), and the study year was also significantly related to higher emotional attitude quartiles (p = 0.002). The University of Messina contributed more to the highest quartile, while the University of Catania contributed more to the lowest. For emotional attitudes, there were also significant differences in distribution among universities (p = 0.0035).
Table 3.
Emotional attitudes quartiles from the FATCOD-B-I questionnaire scores.
| Emotional Attitudes Quartiles | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | eq1 | % | eq2 | % | eq3 | % | eq4 | % | p-Value |
| N | 514 | 463 | 503 | 433 | |||||
| Competence score quartile (%) | <0.001 | ||||||||
| q1 | 149 | 31% | 110 | 23% | 127 | 26% | 94 | 20% | |
| q2 | 146 | 31% | 123 | 26% | 122 | 26% | 86 | 18% | |
| q3 | 134 | 28% | 127 | 26% | 128 | 27% | 91 | 19% | |
| q4 | 85 | 18% | 103 | 22% | 126 | 26% | 162 | 34% | |
| University (%) | 0.0035 | ||||||||
| Catania | 129 | 31% | 104 | 25% | 105 | 25% | 79 | 19% | |
| Messina | 193 | 24% | 184 | 23% | 220 | 27% | 219 | 27% | |
| Palermo | 192 | 28% | 175 | 26% | 178 | 26% | 135 | 20% | |
| Sex (%) | 0.20 | ||||||||
| Female | 358 | 26% | 343 | 25% | 367 | 27% | 297 | 22% | |
| Male | 156 | 28% | 120 | 22% | 136 | 25% | 136 | 25% | |
| Age (years) (%) | 0.57 | ||||||||
| 18–21 | 290 | 28% | 243 | 24% | 268 | 26% | 230 | 22% | |
| 22–25 | 152 | 27% | 147 | 26% | 148 | 26% | 119 | 21% | |
| 26–30 | 42 | 22% | 47 | 24% | 52 | 27% | 54 | 28% | |
| 30+ | 30 | 25% | 26 | 21% | 35 | 29% | 30 | 25% | |
| Academic year (%) | 0.002 | ||||||||
| First | 234 | 30% | 167 | 22% | 183 | 24% | 192 | 25% | |
| Second | 169 | 27% | 171 | 27% | 174 | 27% | 122 | 19% | |
| Third or + | 111 | 22% | 125 | 25% | 146 | 29% | 119 | 24% | |
| PC education (%) | 0.013 | ||||||||
| Compulsory theoretical training | 173 | 23% | 187 | 25% | 218 | 29% | 182 | 24% | |
| No | 261 | 32% | 195 | 24% | 189 | 23% | 181 | 22% | |
| Optional training | 72 | 25% | 74 | 25% | 84 | 29% | 62 | 21% | |
| Practical training | 8 | 23% | 7 | 20% | 12 | 34% | 8 | 23% | |
| Perceived degree of knowledge about pain management (%) | 0.0025 | ||||||||
| Insufficient | 55 | 27% | 41 | 20% | 53 | 26% | 53 | 26% | |
| Sufficient | 75 | 32% | 56 | 24% | 61 | 26% | 46 | 19% | |
| Moderate | 192 | 27% | 193 | 27% | 187 | 26% | 145 | 20% | |
| Good | 174 | 26% | 157 | 24% | 180 | 27% | 149 | 23% | |
| Excellent | 18 | 19% | 16 | 17% | 22 | 23% | 40 | 42% | |
| Previous experience with dying individuals (%) | 0.505 | ||||||||
| Internship in another setting | 109 | 27% | 106 | 26% | 106 | 26% | 82 | 20% | |
| Internship in PC | 13 | 19% | 17 | 25% | 24 | 35% | 15 | 22% | |
| No | 252 | 27% | 217 | 23% | 242 | 26% | 214 | 23% | |
| Personal experience | 129 | 28% | 112 | 24% | 123 | 26% | 105 | 22% | |
| Working experience | 11 | 23% | 11 | 23% | 8 | 17% | 17 | 36% | |
| Previous bereavement experience (%) | 0.016 | ||||||||
| No | 85 | 29% | 54 | 18% | 74 | 25% | 83 | 28% | |
| Yes | 429 | 27% | 409 | 25% | 429 | 27% | 350 | 22% | |
| Current bereavement experience (%) | 0.805 | ||||||||
| I am grieving for a loved one who recently passed away | 61 | 27% | 59 | 26% | 51 | 22% | 56 | 25% | |
| I am preparing for the death of a loved one | 22 | 29% | 18 | 24% | 17 | 23% | 18 | 24% | |
| No | 431 | 27% | 386 | 24% | 435 | 27% | 359 | 22% | |
| Religion (%) | 0.428 | ||||||||
| Agnostic or atheist | 115 | 25% | 127 | 27% | 114 | 25% | 106 | 23% | |
| Catholic Christian | 385 | 28% | 321 | 23% | 371 | 27% | 309 | 22% | |
| Other | 14 | 22% | 15 | 23% | 18 | 28% | 18 | 28% | |
The level of PC education showed a trend where those with compulsory theoretical training were more likely to be in the upper quartile, whereas those without it were in the lower quartile (p = 0.013); thus, the differences in curricula between universities with compulsory training (Messina and Palermo) and those without (Catania) could explain such differences.
As shown in Figure 1, multinomial ordinal regression revealed that practical PC training substantially enhanced competencies (Adj-OR 2.78 [95% CI = 2.12–3.65]). Male students had higher competence odds (Adj-OR 1.38 [95% CI = 1.14–1.66]), and perceived knowledge strongly correlated with self-assessed competence. Advancement in academic years also positively influenced competence self-assessment (Adj-OR 1.98 [95% CI = 1.75–2.24]).
Figure 1.
Adjusted odds ratios for Professional Competence-CCPCN scores.
Regarding emotional attitudes, knowledge of PC showed mixed effects on attitude, with excellent knowledge not significantly affecting attitude scores. However, a per-quartile increase in competence score improved the attitude (Adj-OR 1.24 [95% CI = 1.13–1.35]), although the academic year did not significantly impact it. Figure 2 illustrates the adjusted odds ratios for the FATCOD-B-I score, visually representing the relationships between various factors and emotional attitudes towards care of the dying. The figure highlights the significant positive association between competence scores and emotional attitudes, while also showing the relatively minimal impact of other factors such as academic year and PC education on these attitudes.
Figure 2.
Adjusted odds ratios for FATCOD-B-I scores.
4. Discussion
This study explored the perceived competence in palliative care and attitudes towards dying patient care in Italian nursing students using the Professional Competence-CCPCN and the FATCOD-B-I, respectively. Overall, our findings revealed a spectrum of perceived competence ranging from low to intermediate, aligning with Zhou et al. [22] and Max and Mackenzie [40], who reported similar levels of self-efficacy in palliative care among nursing students in China and the United States, respectively. Progression in the academic curriculum proved to be a pivotal factor; in fact, perceived self-competence in palliative care was observed to improve from the first to the third year in our study. Regarding attitudes towards caring for dying patients, our results showed that nursing students scored positively, although slightly less so than in another Italian study [36,37]. However, Italian results are only sometimes in line with those from other countries. In China [22], Sweden [30], Switzerland [9], and the United States [43], the results are better than the Italian ones. However, the same cannot be said of those in Mongolia [44], England [31], Iran [32], and India [45]. The wide variability in results between countries could be due to cultural, social, and religious differences, which may influence students’ attitudes towards death and dying patients [35].
Moreover, our results show that more than 70% of the sample stated that they optimally perceive pain management in terms of knowledge and attitudes. This result is probably overestimated, as some studies observed that Italian education pays little attention to palliative care training and presents limited knowledge and attitudes toward pain management [36,46], particularly about the combination of interventions [47]. Moreover, even nurses report limited attitudes and knowledge about acute and chronic pain assessment and treatment, and not only in Italy [48,49].
The link between the level of PC education and higher competence quartiles indicates the essential role of mandatory theoretical training. This requirement needs to be uniformly implemented across Italian universities. Although the Italian Ministries of Research and Universities strongly encourage palliative care training of healthcare workers, to date, theoretical and clinical curricula on PC are compulsory only in two out of the three surveyed universities, and this problem is present at a national and European level [47,50]. In 14 European countries (56%), PC was not identified as mandatory in undergraduate nursing education. The broad awareness and use of the EAPC 2004 Guide show how policy measures can influence the development of palliative care education. Recommendations have been built and focus on fostering the use of this guide and implementing policy measures to ensure that palliative care nursing is recognized and certified as a specialty in all European countries [51]. Moreover, a recent scoping review showed that using multiple learning methods increases undergraduate student nurses’ knowledge and positive attitudes towards providing palliative care and clinical exposure to meaningful learning opportunities with patients experiencing severe life-threatening illnesses, which facilitates learning and enables a change of attitudes. Furthermore, from an educational perspective, there needs to be more integration of palliative care philosophy and conceptual frameworks. Issues such as crowded curricula, a lack of nurse educators, and a lack of expertise in teaching palliative care within nursing faculties, as well as issues related to the timing and delivery of palliative care education, must also be addressed.
Although our results demonstrated the importance of enhancing competencies through practical training in palliative care, clinical placements for nursing students pose significant barriers to increased learning opportunities in palliative and end-of-life care. Although progress has been made towards integrating PC curricula into undergraduate nurse education in Italy, this research shows that further curriculum development is needed to build the workforce capacity to meet the increasing demand for primary palliative care. Adding content to an overcrowded nursing curriculum is challenging, as is also the case for other health professionals such as doctors. However, it is not impossible. Several researchers and educators recommend an integrated, spiral approach with multidisciplinary teaching that introduces foundational concepts early to prepare students for clinical encounters with people who require palliative care [52]. Further, from a clinical practice perspective in palliative care, there are difficulties in providing clinical placement [53,54]. Moreover, health policy, clinical, and academic nursing leaders should prioritize the integration of palliative care content into the curricula across nursing schools in the face of increasing palliative and end-of-life care needs in patients. Nursing schools should ensure that students are adequately prepared by designing culturally and socioeconomically relevant curricula, integrating theoretical and experiential learning and offering students a thorough understanding of palliative and end-of-life care. Clinical staff and nursing instructors should support students emotionally and guide them in patient care [55,56].
Notably, students with PC education displayed better attitudes toward the care of the dying. However, prior experience with dying individuals and bereavement experiences did not exhibit relations to any significant difference across quartiles. A recent meta-analysis of qualitative studies describing nursing students’ experiences when caring for dying patients and their families found that nursing students advocated for more caring for patients’ families [55].
Our results show that males had better attitudes compared to female students about care of the dying. These results, however, contrast with other studies in the literature, where females showed better attitudes than males in the management of dying patients [56].
Lastly, while the simultaneous per-year increase in academic experience and perceived self-efficacy suggests that experience and progression in studies positively influence self-perceived competencies in PC, on the contrary, the academic year was not significant for attitudes. In the literature, those with the most clinical experience had more positive attitudes toward caring for the dying, and senior students were found to have positive attitudes toward caring for the dying. These results are supported by Petrolongo and Tooteaker [43], who found a significant positive relationship between years of experience and caring for dying patients. The more academic experience and exposure to death one has, the higher their awareness and ability to manage and adapt are.
Limitations
Despite the large sample of surveyed students (89% of the total nursing students in the whole region) and the significance of the results, our study could have some limitations that should be considered. In particular, using a convenience sample, although representative of one region’s nursing student population, limits the generalizability of our findings. Another notable limitation of this study is its reliance on self-reported measures of competence and attitudes. While the consistency observed across our detailed, multi-item questionnaire suggests coherent self-perception among participants, we acknowledge that self-perceived competencies may not always accurately reflect actual knowledge or skills. Future research could address these limitations by incorporating objective measures of palliative care knowledge and skills alongside self-reported data and extending the analysis beyond regional boundaries to better understand nursing students’ competencies and attitudes on palliative care on a broader scale.
5. Conclusions
This study revealed low to intermediate levels of perceived palliative care competence among Italian nursing students, which improved with academic progression. Practical training was significantly linked to enhanced competencies and attitudes towards end-of-life care. These findings underscore the need to integrate comprehensive palliative care education, including practical experiences, earlier in nursing curricula. Such integration could address competency gaps and improve attitudes towards end-of-life care. Future research should examine the long-term impacts of enhanced palliative care education on nursing practice and patient outcomes. Developing competencies and positive attitudes in palliative care is crucial for preparing nursing students to provide high-quality end-of-life care, emphasizing the importance of targeted educational interventions and clinical experiences in nursing education.
Acknowledgments
We would like to express our gratitude to the nursing students from the Universities of Messina, Palermo, and Catania for their participation in this study. We also extend our appreciation to the faculty members and administrators who facilitated the data collection process. This research would not have been possible without their support and cooperation.
Author Contributions
Conceptualization, C.L.I., E.A., G.D., A.G., M.S., G.I., and R.L.; methodology, E.A., G.V., and R.L.; software, G.V.; validation, E.A., G.V., and R.L.; formal analysis, G.V.; investigation, C.L.I., M.C., G.D., A.G., M.S., G.I., and R.L.; resources, C.L.I., M.C., G.D., A.G., M.S., G.I., and R.L.; data curation, E.A., G.V., M.C., G.D., A.G., M.S., and G.I.; writing—original draft, C.L.I., E.A., G.V., and R.L.; writing—review and editing, C.L.I., E.A., G.V., and R.L.; visualization, G.V.; supervision, E.A., G.V., and R.L.; project administration, E.A. and R.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University Hospital Paolo Giaccone in Palermo (Session n.5/2022 11 May 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article. Clinical Resources: Palliative Care in Acute & Critical Care Settings—American Association of Critical-Care Nurses: https://www.aacn.org/clinical-resources/palliative-end-of-life (accessed on 1 April 2024); Palliative Care and the Nurse’s Role—University of UTAH: https://sigma.nursingrepository.org/server/api/core/bitstreams/2ef4fee9-2c6c-4fad-ae38-6b33aa6df5eb/content (accessed on 1 April 2024); CARES: Competencies And Recommendations for Educating Undergraduate Nursing Students Preparing Nurses to Care for the Seriously Ill and their Families—American Association of Colleges of Nursing: https://www.aacnnursing.org/Portals/0/PDFs/Teaching-Resources/New-Palliative-Care-Competencies.pdf (accessed on 1 April 2024)
Public Involvement Statement
There was no public involvement in any aspect of this research.
Guidelines and Standards Statement
This manuscript was drafted against the STROBE guidelines for cross-sectional studies. This study underscores the importance of integrating practical palliative care training early in nursing education to enhance clinical competence and foster positive attitudes towards caring for dying patients, ultimately improving the quality of end-of-life care.
Use of Artificial Intelligence
AI or AI-assisted tools were not used in drafting any aspect of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Connor S. Global Atlas of Palliative Care, October 72nd Ed 2020. The Worldwide Hospice Palliative Care Alliance. [(accessed on 15 September 2024)]. Available online: http://www.thewhpca.org/resources/global-atlas-on-end-of-life-care.
- 2.World Health Organization Palliative Care. (s.d.) [(accessed on 15 September 2024)]. Available online: https://www.who.int/news-room/fact-sheets/detail/palliative-care.
- 3.Bausewein C., Daveson B.A., Currow D.C., Downing J., Deliens L., Radbruch L., Defilippi K., Lopes Ferreira P., Costantini M., Harding R., et al. EAPC White Paper on outcome measurement in palliative care: Improving practice, attaining outcomes and delivering quality services—Recommendations from the European Association for Palliative Care (EAPC) Task Force on Outcome Measurement. Palliat. Med. 2016;30:6–22. doi: 10.1177/0269216315589898. [DOI] [PubMed] [Google Scholar]
- 4.Razban F., Iranmanesh S., Rafiei H. Nurses’ attitudes toward palliative care in south-east Iran. Int. J. Palliat. Nurs. 2013;19:403–410. doi: 10.12968/ijpn.2013.19.8.403. [DOI] [PubMed] [Google Scholar]
- 5.Sanli D., Iltus F. Experiences of a group of senior nursing students with end of life care and death in Turkey. Omega. 2022;85:936–957. doi: 10.1177/0030222820961232. [DOI] [PubMed] [Google Scholar]
- 6.Ramjan J.M., Costa C.M., Hickman L.D., Kearns M., Phillips J.L. Integrating palliative care content into a new undergraduate nursing curriculum: The University of Notre Dame, Australia–Sydney experience. Collegian. 2010;17:85–91. doi: 10.1016/j.colegn.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 7.Prandi C., Mastroianni C., D’Angelo D., Marson R., Malinverni E., Guarda M. Il Core Competence Italiano Dell’Infermiere in Cure Palliative (Italian Palliative Nursing Core Competence). [Report]. SICP. [(accessed on 19 June 2024)]. Available online: http://www.sicp.it/web/procedure/contenuto.cfm?List=WsPageNameCaller,WsIdEvento,WsIdRisposta,WsRelease&c1=%2Fweb%2Feventi%2FSICP%2Fcorecurriculum%2Ecfm%3FList%3DWsStartRow%26c1%3D11&c2=CORECUSICP&c3=11&c4=1.
- 8.Shi H., Shan B., Zheng J., Peng W., Zhang Y., Zhou X., Miao X., Hu X. Knowledge and attitudes toward end-of-life care among community health care providers and its influencing factors in China: A cross-sectional study. Medicine. 2019;98:e17683. doi: 10.1097/MD.0000000000017683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laporte P., Juvet T., Desbiens J.F., Tapp D., Pasquier J., Bornet M.A. Factors affecting attitudes towards caring for terminally ill patients among nursing students in Switzerland: A cross-sectional study. BMJ Open. 2020;10:e037553. doi: 10.1136/bmjopen-2020-037553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gül Ş., Demir Karabulut S., Eren H., Durmuş İskender M., Göçmen Baykara Z., Keles Ş., Yıldız A., Yalim N.Y. Nursing students’ experiences with death and terminal patients during clinical education. Omega. 2022;85:628–649. doi: 10.1177/0030222820950510. [DOI] [PubMed] [Google Scholar]
- 11.Zahran Z., Hamdan K.M., Hamdan-Mansour A.M., Allari R.S., Alzayyat A.A., Shaheen A.M. Nursing students’ attitudes towards death and caring for dying patients. Nurs. Open. 2022;9:614–623. doi: 10.1002/nop2.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallory J.L. The impact of a palliative care educational component on attitudes toward care of the dying in undergraduate nursing students. J. Prof. Nurs. 2003;19:305–312. doi: 10.1016/S8755-7223(03)00094-2. [DOI] [PubMed] [Google Scholar]
- 13.Zheng R., Lee S.F., Bloomer M.J. How new graduate nurses experience patient death: A systematic review and qualitative meta-synthesis. Int. J. Nurs. Stud. 2016;53:320–330. doi: 10.1016/j.ijnurstu.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Lewis C., Reid J., McLernon Z., Ingham R., Traynor M. The impact of a simulated intervention on attitudes of undergraduate nursing and medical students towards end of life care provision. BMC Palliat. Care. 2016;15:67. doi: 10.1186/s12904-016-0143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson N.E., Kent B., Owens R.G. Experiencing patient death in clinical practice: Nurses’ recollections of their earliest memorable patient death. Int. J. Nurs. Stud. 2015;52:695–704. doi: 10.1016/j.ijnurstu.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Juvet T.M., Bornet M.A., Desbiens J.F., Tapp D., Roos P. “Do Not Protect Us, Train Us.”-Swiss Healthcare Students’ Attitudes Toward Caring for Terminally Ill Patients. Omega. 2023;86:1190–1211. doi: 10.1177/00302228211007003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Desbiens J.F., Gagnon J., Fillion L. Development of a shared theory in palliative care to enhance nursing competence. J. Adv. Nurs. 2012;68:2113–2124. doi: 10.1111/j.1365-2648.2011.05917.x. [DOI] [PubMed] [Google Scholar]
- 18.Chover-Sierra E., Martínez-Sabater A. Analysis of Spanish nursing students’ knowledge in palliative care. An online survey in five colleges. Nurse Educ. Pract. 2020;49:102903. doi: 10.1016/j.nepr.2020.102903. [DOI] [PubMed] [Google Scholar]
- 19.Deravin Malone L., Anderson J., Croxon L. Are newly graduated nurses ready to deal with death and dying?—A literature review. Nurs. Palliat. Care. 2016;1:89–93. doi: 10.15761/NPC.1000123. [DOI] [Google Scholar]
- 20.Mastroianni C., Marchetti A., D’Angelo D., Artico M., Giannarelli D., Magna E., Motta P.C., Piredda M., Casale G., De Marinis M.G. Italian nursing students’ attitudes towards care of the dying patient: A multi-center descriptive study. Nurse. Educ. Today. 2021;104:104991. doi: 10.1016/j.nedt.2021.104991. [DOI] [PubMed] [Google Scholar]
- 21.Lippe M., Davis A., Threadgill H., Ricamato A. Development of a new measure to assess Primary Palliative Care Perceived Competence. Nurse. Educ. 2020;45:106–110. doi: 10.1097/NNE.0000000000000682. [DOI] [PubMed] [Google Scholar]
- 22.Zhou Y., Li Q., Zhang W. Undergraduate nursing students’ knowledge, attitudes and self-efficacy regarding palliative care in China: A descriptive correlational study. Nurs. Open. 2020;8:343–353. doi: 10.1002/nop2.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iranmanesh S., Dargahi H., Abbaszadeh A. Attitudes of Iranian nurses toward caring for dying patients. Palliat. Support. Care. 2008;6:363–369. doi: 10.1017/S1478951508000588. [DOI] [PubMed] [Google Scholar]
- 24.Iranmanesh S., Axelsson K., Häggström T., Sävenstedt S. Caring for dying people: Attitudes among Iranian and Swedish nursing students. Indian. J. Palliat. Care. 2010;16:147–153. doi: 10.4103/0973-1075.73643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peters L., Cant R., Payne S., O’Connor M., McDermott F., Hood K., Morphet J., Shimoinaba K. How death anxiety impacts nurses’ caring for patients at the end of life: A review of literature. Open. Nurs. J. 2013;7:14–21. doi: 10.2174/1874434601307010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dimoula M., Kotronoulas G., Katsaragakis S., Christou M., Sgourou S., Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurse. Educ. Today. 2019;74:7–14. doi: 10.1016/j.nedt.2018.11.025. [DOI] [PubMed] [Google Scholar]
- 27.Xu F., Huang K., Wang Y., Xu Y., Ma L., Cao Y. A Questionnaire Study on the Attitude towards Death of the Nursing Interns in Eight Teaching Hospitals in Jiangsu, China. Biomed. Res. Int. 2019;2019:3107692. doi: 10.1155/2019/3107692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu H., Sun C., Xie L., Wang L., Song J., Zhu Y., Xiao R., Lowe S., Bentley R., Zhou D. Using a mediating model of death attitude and meaning in life to understand nursing students attitude about hospice care. Nurse. Educ. Today. 2022;116:105448. doi: 10.1016/j.nedt.2022.105448. [DOI] [PubMed] [Google Scholar]
- 29.Barrere C.C., Durkin A., LaCoursiere S. The influence of end-of-life education on attitudes of nursing students. Int. J. Nurs. Educ. Scholarsh. 2008;5:11. doi: 10.2202/1548-923X.1494. [DOI] [PubMed] [Google Scholar]
- 30.Berndtsson I.E.K., Karlsson M.G., Rejnö Å.C.U. Nursing students’ attitudes toward care of dying patients: A pre- and post-palliative course study. Heliyon. 2019;5:e02578. doi: 10.1016/j.heliyon.2019.e02578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grubb C., Arthur A. Student nurses’ experience of and attitudes towards care of the dying: A cross-sectional study. Palliat. Med. 2016;30:83–88. doi: 10.1177/0269216315616762. [DOI] [PubMed] [Google Scholar]
- 32.Jafari M., Rafiei H., Nassehi A., Soleimani F., Arab M., Noormohammadi M.R. Caring for dying patients: Attitude of nursing students and effects of education. Indian. J. Palliat. Care. 2015;21:192–197. doi: 10.4103/0973-1075.156497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muliira J.K., Lazarus E.R., Mirafuentes E.C. A Multi-country Comparative Study on Palliative Care Knowledge and Attitudes Toward End-of-Life Care Among Undergraduate Nursing Students. J. Cancer. Educ. 2023;38:837–844. doi: 10.1007/s13187-022-02193-5. [DOI] [PubMed] [Google Scholar]
- 34.A’la M.Z., Setioputro B., Kurniawan D. Nursing students’ attitudes towards caring for dying patients. Nurse Media J. Nurs. 2018;8:25. doi: 10.14710/nmjn.v8i1.17270. [DOI] [Google Scholar]
- 35.Jiang Q., Lu Y., Ying Y., Zhao H. Attitudes and knowledge of undergraduate nursing students about palliative care: An analysis of influencing factors. Nurse. Educ. Today. 2019;80:15–21. doi: 10.1016/j.nedt.2019.05.040. [DOI] [PubMed] [Google Scholar]
- 36.Ferri P., Di Lorenzo R., Stifani S., Morotti E., Vagnini M., Jiménez Herrera M.F., Bonacaro A., Artioli G., Rubbi I., Palese A. Nursing student attitudes toward dying patient care: A European multicenter cross-sectional study. Acta Biomed. 2021;92:e2021018. doi: 10.23750/abm.v92iS2.11403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mastroianni C., Ramon Codina M., D’Angelo D., Petitti T., Latina R., Casale G., Turrziani A., Piredda M., De Marinis M.G. Palliative care education in undergraduate nursing curriculum in Italy. J. Hosp. Palliat. Nurs. 2019;21:96–103. doi: 10.1097/NJH.0000000000000515. [DOI] [PubMed] [Google Scholar]
- 38.Hökkä M., Lehto J.T., Kyngäs H., Pölkki T. Finnish nursing students’ perceptions of the development needs in palliative care education and factors influencing learning in undergraduate nursing studies—A qualitative study. BMC Palliat. Care. 2022;21:40. doi: 10.1186/s12904-022-00915-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leombruni P., Miniotti M., Bovero A., Zizzi F., Castelli L., Torta R. Attitudes toward caring for dying patients: An overview among Italian nursing students and preliminary psychometrics of the FATCOD-B scale. J. Nurs. Educ. Pract. 2014;4:188–196. doi: 10.5430/jnep.v4n3p188. [DOI] [Google Scholar]
- 40.Max E., Mackenzie M. Just in KASE: Evaluating nursing students’ knowledge, attitudes and self-efficacy to care for the dying patient (S721) J. Pain. Sympt. Manag. 2017;53:421. doi: 10.1016/j.jpainsymman.2016.12.231. [DOI] [Google Scholar]
- 41.Prandi C., Biagioli V., Fida R. L’autovalutazione delle Competenze degli infermieri di Cure Palliative: Uno studio preliminare sulla validità del questionario Professional-Competence del Core Curriculum Infermieristico in Cure Palliative (CCICP) [Palliative Care Nurses’ Self-Assessment of Competence: A Preliminary study on the validity of the Professional-Competence Questionnaire of the Palliative Care Nursing Core Curriculum] Riv. Ital. Di Cure Palliat. 2015;17:150–160. [Google Scholar]
- 42.Mastroianni C., Piredda M., Taboga C., Mirabella F., Marfoli E., Casale G., Matarese M., Frommelt K.H., De Marinis M.G. Frommelt Attitudes Toward Care of the Dying Scale Form B: Psychometric testing of the Italian version for students. Omega. 2015;70:227–250. doi: 10.1177/0030222815568944. [DOI] [PubMed] [Google Scholar]
- 43.Petrongolo M., Toothaker R. Nursing students perceptions of death and dying: A descriptive quantitative study. Nurse. Educ. Today. 2021;104:104993. doi: 10.1016/j.nedt.2021.104993. [DOI] [PubMed] [Google Scholar]
- 44.Gelegjamts D., Yong Yoo J., Kim J., Sun Kim J. Undergraduate nursing students’ palliative care knowledge and attitudes towards end-of-life care: A cross-sectional descriptive study. Contemp. Nurse. 2020;56:477–490. doi: 10.1080/10376178.2021.1890165. [DOI] [PubMed] [Google Scholar]
- 45.Paul S.S., Renu G., Thampi P.T. Creating a positive attitude toward dying patients among Nursing students: Is the current curriculum adequate? Indian. J. Palliat. Care. 2019;25:142–146. doi: 10.4103/IJPC.IJPC_148_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Latina R., Forte P., Mastroianni C., Paterniani A., Mauro L., Fabriani L., D’Angelo D., De Marinis M.G. Pain education in schools of Nursing: A survey of the Italian academic situation. Prof. Inferm. 2018;70:115–122. doi: 10.7429/pi.2018.712115. [DOI] [PubMed] [Google Scholar]
- 47.D’Angelo D., Coclite D., Napoletano A., Fauci A.J., Latina R., Gianola S., Castellini G., Salomone K., Gambalunga F., Sperati F., et al. The efficacy of balneotherapy, mud therapy and spa therapy in patients with osteoarthritis: An overview of reviews. Int. J. Biometeorol. 2021;65:1255–1271. doi: 10.1007/s00484-021-02102-3. [DOI] [PubMed] [Google Scholar]
- 48.Mitello L., Marucci A.R., Salvatore S., Sii Onesto A., Baglio G., Latina R. Predictors of nurses’ attitudes and knowledge towards pain management in Italy. A cross-sectional study in the hospital settings. Appl. Nurs. Res. 2021;62:151512. doi: 10.1016/j.apnr.2021.151512. [DOI] [PubMed] [Google Scholar]
- 49.McCabe C., Feeney A., Basa M., Eustace-Cook J., McCann M. Nurses knowledge, attitudes and education needs towards acute pain management in hospital settings: A meta-analysis. J. Clin. Nurs. 2023;32:4325–4336. doi: 10.1111/jocn.16612. [DOI] [PubMed] [Google Scholar]
- 50.Italian Minister of University & Research Programma per L’Insegnamento/Apprendimento Delle Cure Palliative E Dellaterapia Del Dolore Neicorsi DI Laurea in Medicina E Chirurgia, Scienzeinfermieristiche, Psicologia E Serviziosociale [Programme for the Teaching/Learning of Palliative Care and Pain Management in Degree Courses in Medicine, Nursing, Psychology and Social Work] [(accessed on 8 February 2024)];2020 Available online: https://www.miur.gov.it/documents/20182/482871/Documento+n.+512+del+10.01.2020.pdf/851973a1-cd16-7b23-8d5b-6c3784819602?t=1578919032878.
- 51.Martins Pereira S., Hernández-Marrero P., Pasman H.R., Capelas M.L., Larkin P., Francke A.L. Nursing education on palliative care across Europe: Results and recommendations from the EAPC Taskforce on preparation for practice in palliative care nursing across the EU based on an online-survey and country reports. Palliat. Med. 2021;35:130–141. doi: 10.1177/0269216320956817. [DOI] [PubMed] [Google Scholar]
- 52.Erlich D., Lee A., Duggan A., Walec K. Preparing for the end of life: Medical students completing their own advance directives described increased empathy for patients. Fam. Med. 2023;55:195–198. doi: 10.22454/FamMed.2023.183324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Durojaiye A., Ryan R., Doody O. Student nurse education and preparation for palliative care: A scoping review. PLoS ONE. 2023;18:e0286678. doi: 10.1371/journal.pone.0286678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Heath L., Egan R., Ross J., Iosua E., Walker R., MacLeod R. Preparing nurses for palliative and end of life care: A survey of New Zealand nursing schools. Nurse. Educ. Today. 2021;100:104822. doi: 10.1016/j.nedt.2021.104822. [DOI] [PubMed] [Google Scholar]
- 55.Yoong S.Q., Wang W., Seah A.C.W., Kumar N., Gan J.O.N., Schmidt L.T., Lin Y., Zhang H. Nursing students’ experiences with patient death and palliative and end-of-life care: A systematic review and meta-synthesis. Nurse. Educ. Pract. 2023;69:103625. doi: 10.1016/j.nepr.2023.103625. [DOI] [PubMed] [Google Scholar]
- 56.Davis A., Lippe M., Glover T.L., McLeskey N., Shillam C., Mazanec P. Integrating the ELNEC undergraduate curriculum into Nursing Education: Lessons learned. J. Prof. Nurs. 2021;37:286–290. doi: 10.1016/j.profnurs.2020.12.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are contained within the article. Clinical Resources: Palliative Care in Acute & Critical Care Settings—American Association of Critical-Care Nurses: https://www.aacn.org/clinical-resources/palliative-end-of-life (accessed on 1 April 2024); Palliative Care and the Nurse’s Role—University of UTAH: https://sigma.nursingrepository.org/server/api/core/bitstreams/2ef4fee9-2c6c-4fad-ae38-6b33aa6df5eb/content (accessed on 1 April 2024); CARES: Competencies And Recommendations for Educating Undergraduate Nursing Students Preparing Nurses to Care for the Seriously Ill and their Families—American Association of Colleges of Nursing: https://www.aacnnursing.org/Portals/0/PDFs/Teaching-Resources/New-Palliative-Care-Competencies.pdf (accessed on 1 April 2024)