Abstract
Cyclic weight loss and subsequent regain after dieting and non-dieting periods, a phenomenon termed yoyo dieting, places individuals at greater risk of metabolic complications and alters gut microbiome composition. Resistant starch (RS) improves gut health and systemic metabolism. This study aimed to investigate the effect of yoyo dieting and RS on the metabolism and gut microbiome. C57BL/6 mice were assigned to 6 diets for 20 weeks, including control, high fat (HF), yoyo (alternating HF and control diets every 5 weeks), control with RS, HF with RS, and yoyo with RS. Metabolic outcomes and microbiota profiling using 16S rRNA sequencing were examined. Yoyo dieting resulted in short–term weight loss, which led to improved liver health and insulin tolerance but also a greater rate of weight gain compared to continuous HF feeding, as well as a different microbiota profile that was in an intermediate configuration between the control and HF states. Mice fed HF and yoyo diets supplemented with RS gained less weight than those fed without RS. RS supplementation in yoyo mice appeared to shift the gut microbiota composition closer to the control state. In conclusion, yoyo dieting leads to obesity relapse, and increased RS intake reduces weight gain and might help prevent rapid weight regain via gut microbiome restoration.
Keywords: weight cycling, yoyo dieting, obesity, resistant starch, gut microbiome, metabolism, short-chain fatty acid, fatty liver
1. Introduction
Overweight and obesity have tripled worldwide since 1975, affecting more than 1.9 billion adults across all ages and socioeconomic groups. This places many people at a high risk of developing an array of comorbidities, including psychological health burdens [1] and numerous related metabolic disorders [2,3,4,5,6], such as cardiovascular diseases [7,8], type 2 diabetes [9], and fatty liver diseases [10,11]. Moreover, obesity has been associated with lowered life expectancy [12] and quality of life [13] and has become a major health and economic crisis in both developed and developing countries [14,15,16,17].
For many individuals, weight loss is difficult and often unsustainable. Current evidence suggests that 80–95% of individuals who had previously lost weight typically regained most of their lost weight within 5 years [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35]. Repeated phases of dieting and non-dieting periods resulting in cyclic weight loss and regain are commonly called yoyo dieting [36]. Currently, weight loss remains the gold standard strategy for many metabolic complications, such as diabetes and fatty liver disease [37,38]. Yoyo dieting results in relapsing metabolic complications that can surpass the pre-weight loss metabolic derangement [39,40].
There has been substantial progress in studying the pathogenesis of obesity, especially with increasing evidence that gut microbiome alterations play an important role in its development. However, the role of the gut microbiome in yoyo dieting remains unknown [41,42]. Gut dysbiosis refers to an imbalance in gut microbiota homeostasis that leads to the loss of beneficial microbial organisms and changes in gut microbiota composition and function [43]. This is known to influence metabolic homeostasis and is associated with an increased risk of metabolic disturbances [44,45], including obesity, as shown in both animal [46,47,48] and human studies [49,50,51,52,53]. Moreover, it is well established that diet is one of the main drivers of the composition and function of the gut microbiome. Changes in diet profoundly impact the gut microbiome within days [54,55,56]. There is some evidence suggesting that yoyo dieting results in long–term modification of the gut microbiome profile [47]. This alteration in gut microbiota composition is believed to contribute to susceptibility to weight gain relapse, hence the challenge of maintaining weight loss [47].
Prior studies suggest that increasing the intake of resistant starch (RS), a type of dietary fibre, improves gut health [57,58,59,60,61,62,63,64] and weight management [65,66,67,68,69]. RS is a type of dietary fibre that resists digestion in the small intestine and is passed to the large intestine for fermentation by the colonic microbiome, producing short-chain fatty acids (SCFAs) [70]. These SCFAs are known to provide an energy supply for the colonic mucosa [71,72,73] and act as signalling molecules that regulate metabolic pathways [74,75,76,77,78,79,80,81,82,83,84,85]. The most abundant SCFAs are butyrate, acetate, and propionate, which are associated with reduced adiposity [86] and a decreased risk of developing cardiometabolic disease and bowel disorders [87,88,89,90]. RS can be classified into five categories based on composition and source [60,91,92,93,94,95]. This study investigated the role of RS4, which represents chemically modified starch that is commercially available as a food ingredient [95]. Our study aimed to determine the effects of yoyo dieting on gut and metabolic health and investigate whether supplementation with RS might be a promising and effective weight management strategy.
2. Materials and Methods
2.1. Animals and Diets
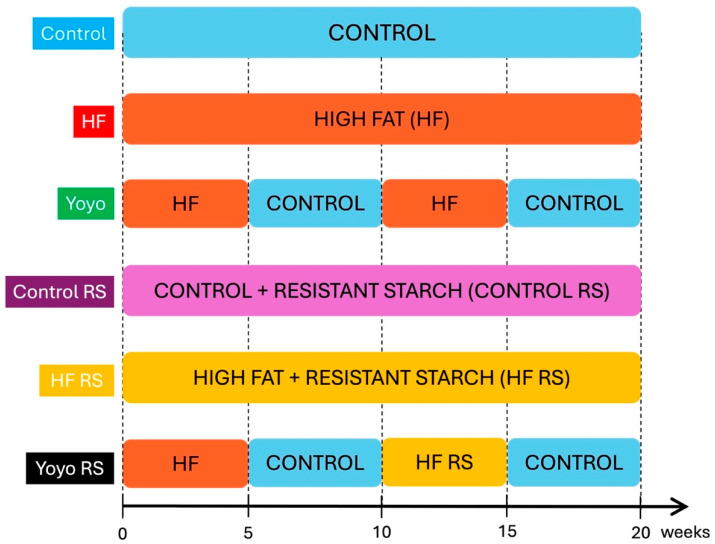
Five-week-old male and female C57BL/6 mice were purchased from the Animal Resource Centre (Perth, WA, Australia). Following arrival at our facility, the mice were acclimatised for 1 week, during which they were fed a normal chow diet. Following this acclimation period, mice were exposed to six diet treatments (n = 7–8/diet group/sex) for 20 weeks. The sample size was calculated using power calculations based on previous experiments that examined changes in gastrointestinal function in obesity using a 2-tailed hypothesis with an alpha of 0.05 and a power of 0.8. Dietary groups included: (1) control (SF17-091; 12.3% kcal from fat); (2) high fat (HF, SF16-048; 60% kcal from fat); (3) yoyo, in which mice alternated between an HF and control every 5 weeks (yoyo); (4) control supplemented with RS (control RS, SF21-019, 13.9% kcal from fat); (5) HF supplemented with RS (HF RS) (SF21-018, 60% kcal from fat); and (6) yoyo supplemented with RS in the second weight gain cycle, in which mice were fed an HF (SF16-048) diet for 5 weeks, control (SF17-091) diet for 5 weeks, HF RS (SF21-018) diet for 5 weeks, and a control (SF17-091) diet for 5 weeks (yoyo RS) (Figure 1).
Figure 1.
Diet treatments. Male and female mice were exposed to 6 diets for 20 weeks, including combinations of control and high-fat (HF) diets with and without resistant starch (RS).
Six weeks of age was chosen as the starting age given the increased appearance of obesity in humans at a corresponding age (mice aged 6–26 weeks correspond to humans aged approximately 18–32 years old [96,97]). Mice were housed in groups of 4 per cage and 2 cages per diet treatment, and they were maintained on a strict 12-hour light/dark cycle, controlled temperature at 21 °C, humidity between 40–70% and given ad libitum access to irradicated pallet food and autoclaved water.
All diets were customised by Specialty Feeds Australia (Glen Forrest, Western Australia). The RS was supplemented with GemStar® RS, Hamburg, IA, USA (RS type 4, 117–140 g/kg).
There was no significant difference in the body weight of all animals at the beginning of the diet intervention. At baseline, mice weighed 20.5 ± 0.5 g (males) or 17 ± 0.5 g (females). There was no difference in food intake (in grams) between all dietary groups when measured during weeks 15–17.
All procedures were conducted according to the guidelines of the National Health and Medical Research Council and approved by the Deakin University Animal Ethics Committee. Animals were humanely culled from the study if they showed clinical illness or experienced 20% body weight loss over 7 days.
Body Weight and Sample Collection: Body weight measurements and faecal collection were performed weekly throughout the 20-week experimental period. Mice were humanely killed by cervical dislocation after 20 weeks. Terminal cardiac blood was collected for SCFA analysis, and liver and adipose tissues (gonadal and perirenal) were collected and weighed.
2.2. Oral Glucose Tolerance Test
To assess glucose homeostasis under physiologically relevant conditions, an oral glucose tolerance test (OGTT) was conducted in week 19 of the study after a 5-hour fast. Glucose (2 g/kg body weight) was administrated by oral gavage in saline (200–300 µL), and tail blood was collected at 0, 15, 30, 45, 60, and 90 min post gavage for glucose level examination (AccuChek, Roche Diagnostics, Indianapolis, IN, USA) and insulin response. Insulin was determined using a mouse ultrasensitive insulin ELISA kit (ALPCO Diagnostics, Salem, NH, USA) measurement according to the manufacturer’s protocol.
2.3. Insulin Tolerance Test
An insulin tolerance test (ITT) was conducted in week 20 of the study. Animals were fasted for 5 h and then administrated 1.0 U/kg body weight Humulin Insulin 30/70 (Eli Lilly) via intraperitoneal injection. Blood glucose measurements were performed 0, 30, 60, 90, and 120 min following the Humulin injection (AccuChek, Roche Diagnostics, Indianapolis, IN, USA).
2.4. Liver Histology
Liver was fixed in 10% neutral buffered formalin, processed, paraffin-embedded, and sectioned (5 μm) before haematoxylin and eosin staining to assess steatohepatitis. Slides were examined and photographed using an EVOSTM M7000 Imaging System (AMF7000, Thermal Fisher Scientific, Waltham, MA USA). Hepatocyte ballooning was defined as regions of liver cells that had enlarged 1.5–2 times the normal hepatocyte diameter [98,99]. Hepatocyte ballooning was quantified using 20 randomised light microscopic fields per animal at ×20 magnification in a blinded fashion.
2.5. Liver Triglyceride Determination
Triglyceride was extracted from 20 mg of frozen mouse liver using Jouihan’s liver triglyceride assay protocol [100]. Prior to the triglyceride assay, the sample was diluted in sterile Milli-Q water with a ratio of 1/4 sample/water. The free glycerol concentration was determined in the assay using Triglycerides GPO-PAP (Cobas C pack green, Roche Diagnostics, Indianapolis, IN, USA). The hepatic triglyceride content was determined using the following equation:
| Triglyceride content (mg/g of liver) = [glycerol] (mg/dL) × 0.0083 (dL)/liver mass (g) |
2.6. Short-Chain Fatty Acids (SCFAs)
Plasma propionate and butyrate measurements were made using negative chemical ionization (NCI) gas chromatography–mass spectrometry (GC–MS, Agilent Technologies, Santa Clara, CA, USA), based on the method of Tomcik et al. [101], with some modifications described below.
Terminal blood plasma was used for the determination of relative propionate and butyrate levels. Briefly, 40 µL of either plasma or extraction blanks (Milli-Q Water) was added to a 1 mL glass VEREXTM vial (Phenomenex, Torrance, CA, USA), followed by the addition of 60 µL of Dullbecco modified PBS (no calcium, no magnesium, pH 7.0–7.3 cell culture grade; Thermo Fisher Scientific) containing internal standards (4 µM 13C3 propionate and 4 µM 13C4 butyrate; Cambridge Isotope Laboratories, Inc., Tewksbury, MA, USA). The samples were then chemically derivatised via the addition of 200 µL of GC grade acetone containing 100 mM 2,3,4,5,6-pentafluorobenzyl bromide (PFBBr; Sigma, St. Louis, MO, USA), and after capping the samples were vortexed for 1 min and incubated at 60 °C for 1 h. Subsequently, vials were left to cool down to room temperature, and the PFB propionate and butyrate esters were extracted via the addition of 125 µL of analytical-grade isooctane, followed by 1 min of vortexing and centrifugation at 5000× g for 5 min. Finally, 50 µL of the top isooctane (organic) phase was removed and transferred to glass inserts held in 2 mL GC vials, ready for GC–MS analysis. The samples were analysed using an Agilent 7890B GC system and an Agilent 5977B MSD (Agilent Technologies, Santa Clara, CA, USA) in NCI mode, with helium as the carrier and methane as the reagent gas. Each sample was injected (1 μL) with a 10:1 split ratio. A VF-5 capillary column with a 10 m inert EZ-guard (J&W Scientific, Folsom, CA, USA, 30 m, 0.25 mm, 0.25 µM) was used, and the front inlet and transfer line temperatures were set to 250 °C and 270 °C, respectively, while the quadrupole and source temperatures were both set to 150 °C. The oven temperature gradient was set to 70 °C (1 min), 70 °C–160 °C at 5 °C/min, and 160–320 °C at 50 °C/min, followed by a 1-minute hold time at 320 °C. The propionate was analysed by selected monitoring of the 73 m/z (M0; unlabelled) and 76 m/z (M+3; internal standard) ions, while butyrate was analysed by selected monitoring of the 87 m/z (M0; unlabelled) and 91 m/z (M+4; internal standard) ions. All chromatographic peaks were integrated using the Quantitative Mass Hunter Workstation (Agilent Technologies, Santa Clara, CA, USA), and individual sample unlabelled-to-labelled peak area ratios were normalised to the control group, with data presented as a fold change compared to the control.
2.7. Metabolic Statistical Analysis
Metabolic statistical analysis has been conducted using GraphPad Prism (version Prism 10.0.2), R (version 2023-03-15), and RStudio (version 2023.06.1+524). Descriptive and analytical statistics were performed using GraphPad Prism for multiple endpoints, such as body weight, OGTT, ITT, insulin, and SCFAs, which were analysed using two-way ANOVA (diet and RS status) with Tukey’s honestly significant difference (HSD) test for post hoc comparisons unless otherwise stated. If a two-way ANOVA for diet by RS status indicated a significant interaction between the basic diet type and RS supplementation, subsequent comparisons of individual diets were evaluated using Tukey’s HSD test. The rate of weight gain data was analysed in R and RStudio using a linear mixed effect model with the function lmer from the lme4 package (version 1.1.-35.3) and the lmerTest package (version 3.1-3) to provide the p-value. Models were fitted using the REML criterium, and p-values came from t-tests using Satterthwaite’s method. This analysis was conducted to compare the average rate of body weight regain. The analysis included random and fixed effects; the random effect was the per-mouse intercept, while the fixed effects were the slope in different phases (phases 1 and 2), time points within the phase (5 weeks per phase), and diet/sex groups (4 diets, 2 sexes). Data are presented as mean ± SEM unless otherwise stated, with a p-value threshold of 0.05 for statistical significance.
2.8. Taxonomic Microbiota Analysis
Faecal samples collected in weeks 15 and 20 were processed for microbiota analysis. DNA was isolated using QIAamp Fast DNA Stool Mini kits (Qiagen Pty Ltd., Dandenong, VIC, Australia), according to the manufacturer’s instructions. Faecal DNA was used for PCR amplification sequencing (16S rRNA producing amplicon sequence variants (ASVs), variable region V3–V4), conducted by the Australian Genome Research Facility (Melbourne, VIC, Australia). Raw data of the metagenome sequencing have been submitted to NCBI Sequence Read Archive database under submission ID SUB14694204.
Calculations of alpha diversity (Shannon and Fisher) were conducted to assess the microbiome diversity within each sample using the estimate_richness function in the phyloseq package and visualised using the ggplot2 package. Beta diversity was measured using Bray–Curtis dissimilarities and visualised using principal coordinate analysis (PCoA) plots with phyloseq. To identify differences in the bacterial microbiota between groups, permutational multivariate analysis of variance (PERMANOVA) was conducted on the Bray–Curtis dissimilarity matrix with the adonis2 function within the vegan package. Additionally, DESeq2 was used to determine genera that were differentially expressed (with a false discovery rate [FDR] of 0.01 to determine significance) between samples in the phyloseq package.
3. Results
3.1. Body Weight Change, Rate of Weight Regain, and Tissue Mass
3.1.1. Body Weight Change
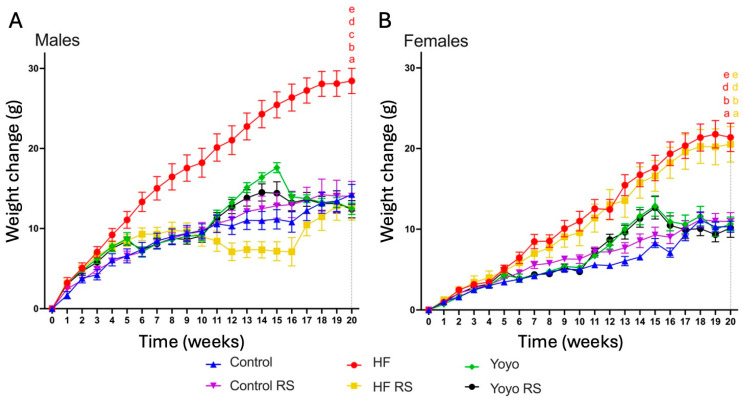
At the end of the diet intervention, regardless of sex, yoyo mice (green) had a similar body weight change to control mice (blue) (two-way ANOVA diet × RS status in both sexes p < 0.0001; Tukey’s HSD: male p = 0.8110 (Figure 2A); female p = 0.9995 (Figure 2B)) and were significantly lighter than HF mice (red) (Tukey’s HSD: male p < 0.0001, female p = 0.0026 (Figure 2)).
Figure 2.
Body weight change in male (A) and female mice (B). Weight change of mice fed control (blue), HF (red), yoyo (green), control RS (purple), HF RS (yellow), and yoyo RS (black) diets. RS supplemented in an HF diet (HF RS) significantly lowered body weight change in male mice compared to an HF diet alone, but no significant difference was observed in female mice. n = 7–8/group/sex; statistic at week 20 p ≤ 0.05 versus a control, b control RS, c HF RS, d yoyo, and e yoyo RS mice. HF—high fat; RS—resistant starch.
Supplementation with RS in a control diet (control RS, purple) did not alter weight gain in male or female mice in comparison with a control diet only (Tukey’s HSD: male p > 0.9999 (Figure 2A), female p = 0.9994 (Figure 2B)). In contrast, RS supplementation in an HF diet (HF RS) (yellow) resulted in significantly less weight gain than an HF diet alone in male (Tukey’s HSD: p = 0.0002 (Figure 2A)) but not in female mice (Tukey’s HSD: p = 0.9995 (Figure 2B)).
With RS supplementation in the second phase of the yoyo diet (yoyo RS) (black), there was no significant difference in the final body weight change compared to the yoyo group (Tukey’s HSD: both sexes p > 0.9999 (Figure 2A,B)). Moreover, while the body weight change between yoyo RS- and HF RS-fed male mice did not differ (Tukey’s HSD: p > 0.9999 (Figure 2A)), the body weight change of the yoyo RS group was significantly lower than HF RS-fed female mice (Tukey’s HSD: p = 0.0110) (Figure 2B).
3.1.2. Rates of Body Weight Gain during High-Fat Feeding Periods
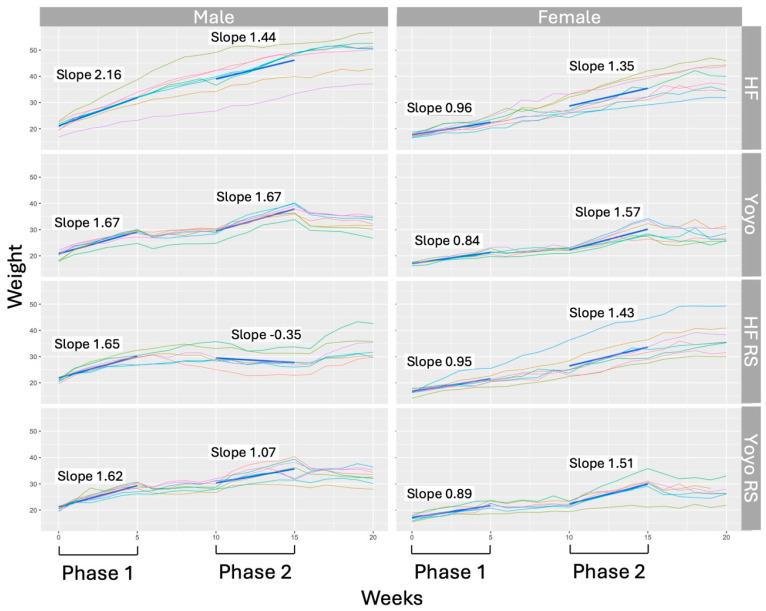
Further analysis of body weight gain was performed on the HF and yoyo groups supplemented with and without RS to explore the rate of weight regain of yoyo mice during the two HF feeding periods: Phase 1 (weeks 0–5) and Phase 2 (weeks 10–15) (Figure 3).
Figure 3.
Rate of weight regain of male and female mice in high-fat and yoyo groups, supplemented with and without resistant starch, during two non-restricted (high-fat) feeding periods: Phase 1 (weeks 0–5) and Phase 2 (10–15). The weight of each animal is represented by an individual coloured line. The difference in the rate of weight gain between the 2 phases was identified as the difference in the average slopes of the same-coloured lines in Phase 1 and Phase 2. Bold blue solid lines indicate the average rate of weight gain/loss in Phase 1 and Phase 2 per diet group, respectively. In male mice, across the two HF feeding phases, yoyo mice had a significantly greater rate of weight gain compared to HF mice. RS supplementation in HF and yoyo diets (HF RS and yoyo RS) resulted in significantly lower rates of weight gain compared to diets supplemented with no RS. In female mice, across the two HF feeding phases, HF and yoyo mice had similar rates of weight gain. RS supplementation did not affect the rate of weight gain in female mice. HF—high-fat diet; RS—resistant starch.
Across the two HF feeding phases, male yoyo mice had a significantly higher rate of weight gain compared to HF mice (+0.7171 g/week, p = 0.0087). However, in female mice, HF and yoyo mice had similar rates of weight gain (p = 0.2158) (Figure 3).
Supplementation with RS in an HF diet (HF RS) resulted in a significantly reduced rate of weight gain in male mice compared to those fed no RS (−1.28 g/week, p < 0.001). In contrast, there were no significant differences in the rates of weight gain in female mice (p = 0.79) (Figure 3).
With RS supplementation in the second phase of the yoyo diet (yoyo RS), male yoyo RS mice gained significantly less weight compared to yoyo mice (−1.28 g/week, p < 0.0001). However, the rate of weight gain of yoyo RS mice was still significantly higher than HF RS mice (+1.44 g/week, p < 0.001) (Figure 3). Conversely, in female mice, there was no significant difference in the rates of weight gain between the yoyo and yoyo RS groups (p = 0.631) and between the yoyo RS and HF RS groups (p = 0.6405) (Figure 3).
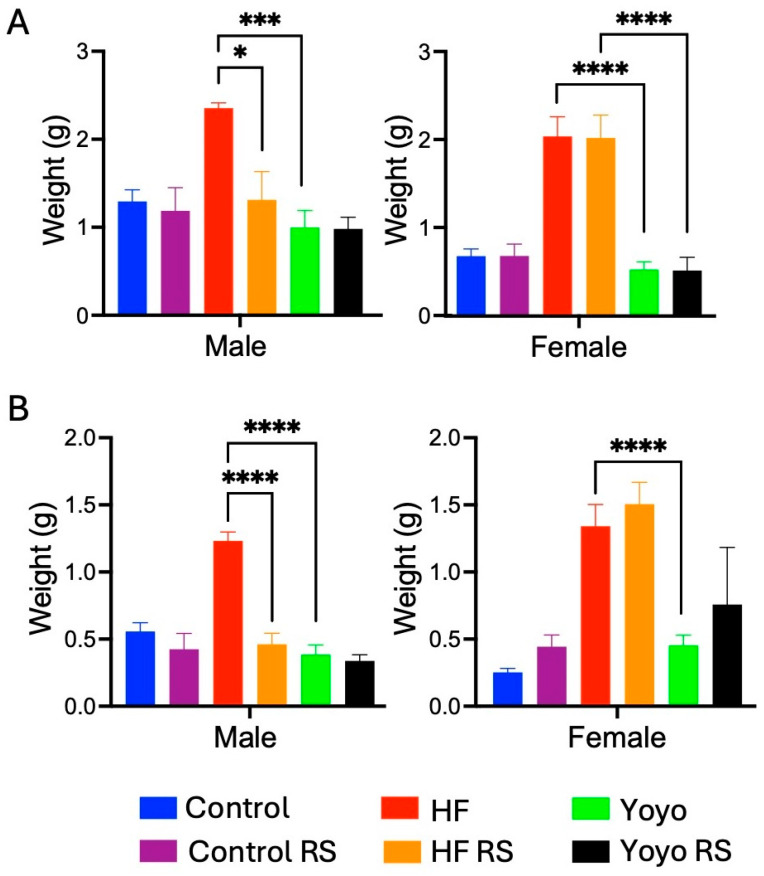
3.1.3. Fat Mass
After 20 weeks, regardless of sex and RS status, yoyo mice (green) had similar gonadal and perirenal fat mass compared to control mice (blue) (two-way ANOVA diet × RS status: male p = 0.0232 and female p < 0.0001; Tukey’s HSD: male p = 0.8784 (Figure 4A) and p = 0.9858 (Figure 4B); female p = 0.9816 (Figure 4A) and p = 0.8352 (Figure 4B), respectively) and were significantly lower than HF mice (red) (Tukey’s HSD: male p = 0.0002 (Figure 4A) and p < 0.0001 (Figure 4B), female p < 0.0001 (Figure 4A) and p = 0.0173 (Figure 4B), respectively).
Figure 4.
Fat mass. Gonadal fat (A). Perirenal fat (B). RS supplemented in an HF diet (HF RS) resulted in a significant reduction in fat mass in male mice compared to an HF diet alone, but no significant difference was observed in female mice. * p ≤ 0.05, *** p ≤ 0.001, **** p ≤ 0.0001, with n = 7–8/group/sex.
Supplementation with RS in mice fed a control diet (control RS) (purple) did not alter gonadal and perirenal fat mass compared to those fed a control diet only (Tukey’s HSD: male p = 0.9991 (Figure 4A) and p = 0.8336 (Figure 4B), female p > 0.9999 (Figure 4A) and p = 0.9716 (Figure 4B), respectively). In contrast, the supplementation of an HF diet with RS (HF RS) (yellow) resulted in significantly less gonadal and perirenal fat mass than an HF diet alone in male (Tukey’s HSD: p = 0.0085 (Figure 4A) and p < 0.0001 (Figure 4B), respectively) but not in female mice (Tukey’s HSD: p > 0.9999 (Figure 4A) and p = 0.9849 (Figure 4B), respectively).
With RS supplementation in the second phase of the yoyo diet (yoyo RS) (black), there was no significant difference in gonadal and perirenal fat mass compared to the yoyo group (Tukey’s HSD: male p > 0.9999 (Figure 4A) and p = 0.9978 (Figure 4B), female p > 0.9999 (Figure 4A) and p = 0.8847 (Figure 4B), respectively). Gonadal and perirenal fat mass between male yoyo RS mice and male HF RS mice did not differ (Tukey’s HSD: p = 0.8332 (Figure 4A) and p = 0.9469 (Figure 4B), respectively). However, gonadal fat mass in female yoyo RS mice was significantly lower than in HF RS mice (Tukey’s HSD: p < 0.0001 (Figure 4A).
3.2. Liver Health
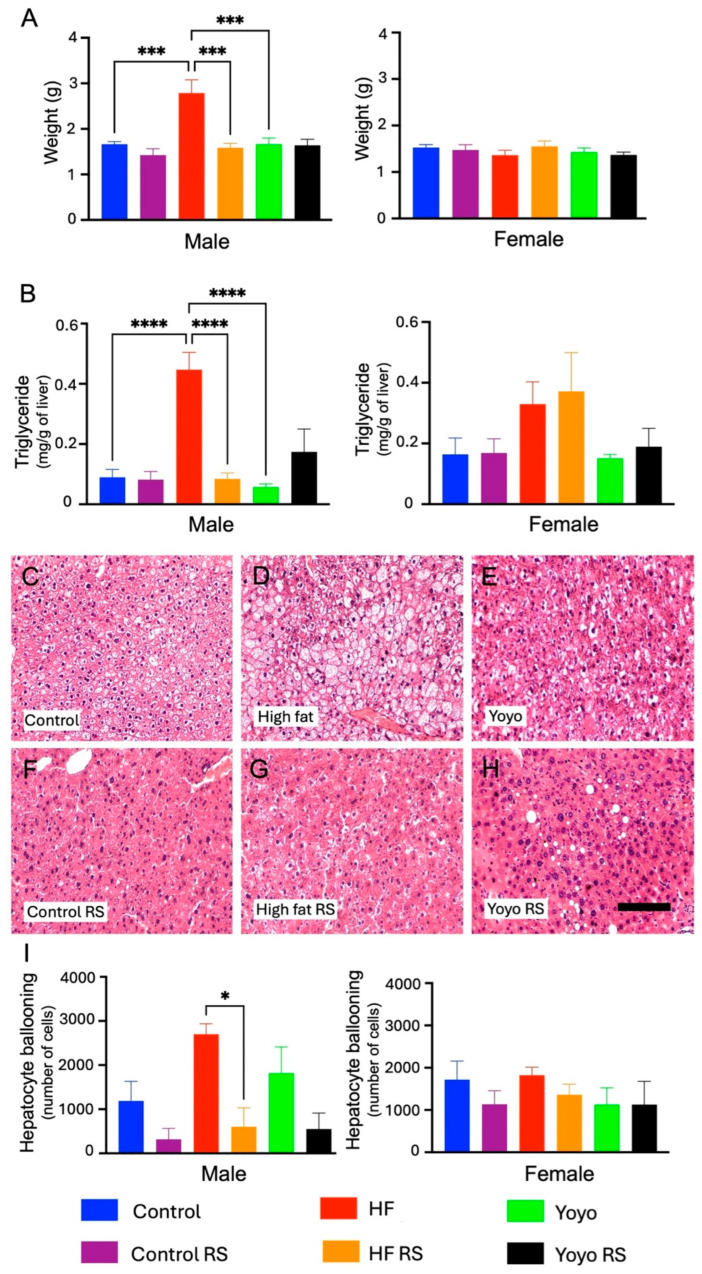
At the end of the dietary intervention, yoyo dieting improved indices of liver health in male mice compared to HF feeding alone. In particular, male yoyo mice (green) had similar a liver mass, liver triglycerides (two-way ANOVA diet × RS status, both p< 0.0001; Tukey’s HSD: both p > 0.9999 (Figure 5A,B)), and hepatocyte ballooning (two-way ANOVA diet × RS status, p = 0.0009; Tukey’s HSD: p = 0.8740 (Figure 5C,E,I)) compared to control mice (blue). Additionally, male yoyo mice had a significantly lower liver mass and triglycerides, but not hepatocyte ballooning, compared to HF mice (red) (Tukey’s HSD: p = 0.0003 (Figure 5A), p = 0.5401 (Figure 5B), and p = 0.6313 (Figure 5I), respectively). Conversely, regardless of diet and RS status, there were no differences in liver mass (two-way ANOVA diet × RS status, p = 0.3927 (Figure 5A)), liver triglycerides (two-way ANOVA diet × RS status, p = 0.9606 (Figure 5B)), or hepatocyte ballooning (two-way ANOVA diet × RS status, p = 0.7146 (Figure 5I)) in female mice.
Figure 5.
Indices of liver health. Liver mass (A). Liver triglycerides (B). Hepatocyte ballooning images of male mice using haematoxylin and eosin staining (C–H). Hepatocyte ballooning (I). RS supplementation in an HF diet (HF RS) significantly improved the liver health of male mice compared to an HF diet only, but no significant difference was observed in female mice. * p ≤ 0.05, *** p ≤ 0.001, **** p ≤ 0.0001, n = 7–8/group/sex. Scale bar = 150 µm. RS: resistant starch.
Supplementation with RS in male mice fed a control diet (control RS) (purple) did not alter the liver mass (Tukey’s HSD: p = 0.9001 (Figure 5A)), liver triglycerides (Tukey’s HSD: p > 0.9999 (Figure 5B)), or hepatocyte ballooning (Tukey’s HSD: p = 0.6431 (Figure 5C,F,I)) compared to a control diet alone. However, supplementation with RS in an HF diet (HF RS) (yellow) resulted in a significantly lower liver mass (Tukey’s HSD: p = 0.0001 (Figure 5A)), liver triglycerides (Tukey’s HSD: p < 0.0001 (Figure 5B)), and hepatocyte ballooning (Tukey’s HSD: p = 0.0109 (Figure 5C,D,I)) compared to an HF diet alone.
With RS supplementation in the second phase of the yoyo diet (yoyo RS) (black), there were no significant differences in liver mass, liver triglycerides, and hepatocyte ballooning compared to the yoyo group (Tukey’s HSD: p > 0.9999 (Figure 5A), p = 0.9994 (Figure 5B), and p = 0.2437 (Figure 5E,H,I), respectively) and between the yoyo RS and HF RS groups (Tukey’s HSD: p = 0.9999 (Figure 5A), p > 0.9999 (Figure 5B), and p = 0.5663 (Figure 5G–I), respectively).
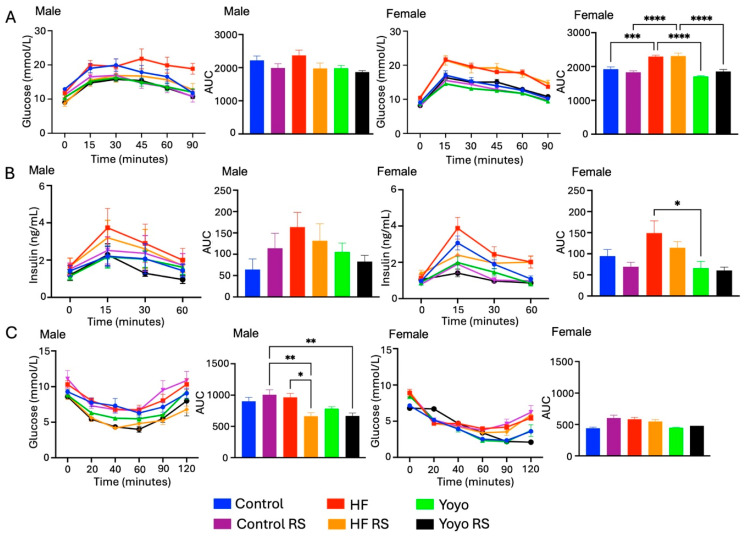
3.3. Blood Glucose Metabolism
In male mice, there was no significant difference in glucose and insulin levels during an OGTT, and glucose levels during an ITT between the HF (red) and control (blue) groups (two-way ANOVA diet × RS status, p = 0.0664 (Figure 6A), p = 0.1893 (Figure 6B), p = 0.0004 (Figure 6C); Tukey’s HSD: p = 0.9545, p = 0.1468, p = 0.9702, respectively) and between the yoyo and control groups (Tukey’s HSD: p = 0.7229, p = 0.8876, p = 0.7367, respectively). Yoyo dieting (green) appeared to improve blood glucose homeostasis compared to continuous HF feeding; however, this was not significantly different (Tukey’s HSD: p = 0.2536 (Figure 6A), p = 0.6849 (Figure 6B), p = 0.3299 (Figure 6C), respectively). In female mice, HF mice had significantly higher glucose tolerance (two-way ANOVA diet × RS status, p < 0.0001; Tukey’s HSD: p = 0.0006 (Figure 6A)) but similar insulin levels during an OGTT (two-way ANOVA diet × RS status, p = 0.004; Tukey’s HSD: p = 0.1906 (Figure 6B)) and glucose levels during an ITT (two-way ANOVA diet × RS status, p = 0.0234; Tukey’s HSD: p = 0.0502 (Figure 6C)) compared to control mice. There was no significant difference in glucose homeostasis and plasma insulin between the yoyo and control groups (Tukey’s HSD: p = 0.1312 (Figure 6A), p > 0.9999 (Figure 6B), p = 0.8399 (Figure 6C), respectively). Yoyo dieting significantly lowered glucose and insulin levels during an OGTT, but not ITT, compared to HF mice (Tukey’s HSD: p < 0.0001 (Figure 6A), p = 0.0286 (Figure 6B), p = 0.2294 (Figure 6C), respectively).
Figure 6.
Metabolic measurements. Blood glucose during an oral glucose tolerance test (A). Plasma insulin during an oral glucose tolerance test (B). Blood glucose during an insulin tolerance test (C). RS supplementation in an HF diet (HF RS) resulted in a significantly improved insulin tolerance in male mice compared to an HF diet alone, but no significant difference was observed in female mice. * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001, and **** p ≤ 0.0001 used to determine significance, with n = 7–8/group/sex. AUC: area under the curve.
Supplementation with RS in mice fed a control diet (control RS) (purple) did not significantly alter glucose and insulin measured during an OGTT or insulin tolerance compared to mice fed a control diet only (male Tukey’s HSD: p = 0.7583 (Figure 6A), p = 0.8321 (Figure 6B), p = 0.7941 (Figure 6C), respectively; female Tukey’s HSD: p = 0.8731 (Figure 6A), p = 0.8374 (Figure 6B), p = 0.0528 (Figure 6C), respectively). Similarly, RS supplementation in mice fed an HF diet (HF RS) (yellow) did not significantly alter glucose and insulin levels during an OGTT compared to HF mice (male Tukey’s HSD: p = 0.2760 (Figure 6A), p = 0.9685 (Figure 6B), respectively; female Tukey’s HSD: p > 0.9999 (Figure 6A), p = 0.6550 (Figure 6B), respectively). However, male mice consuming an HF RS diet had significantly improved insulin tolerance compared to mice fed an HF diet alone (Tukey’s HSD: p = 0.0123 (Figure 6C)).
With RS supplementation in the second phase of the yoyo diet (yoyo RS) (black), there were no significant differences in glucose and insulin levels during an OGTT or in glucose during an ITT between yoyo RS and yoyo mice (male Tukey’s HSD: p = 0.9852 (Figure 6A), p = 0.9909 (Figure 6B), p = 0.7946 (Figure 6C), respectively; female Tukey’s HSD: p = 0.5349 (Figure 6A), p > 0.9999 (Figure 6B), p = 0.9992 (Figure 6C), respectively). Similarly, there was no difference in glucose and insulin levels in male yoyo RS and HF RS mice (Tukey’s HSD: p = 0.9892 (Figure 6A), p > 0.9999 (Figure 6B), p = 0.8179 (Figure 6C), respectively). On the other hand, female yoyo RS mice had significantly improved glucose tolerance compared to HF RS mice (Tukey’s HSD: p < 0.0001 (Figure 6A)).
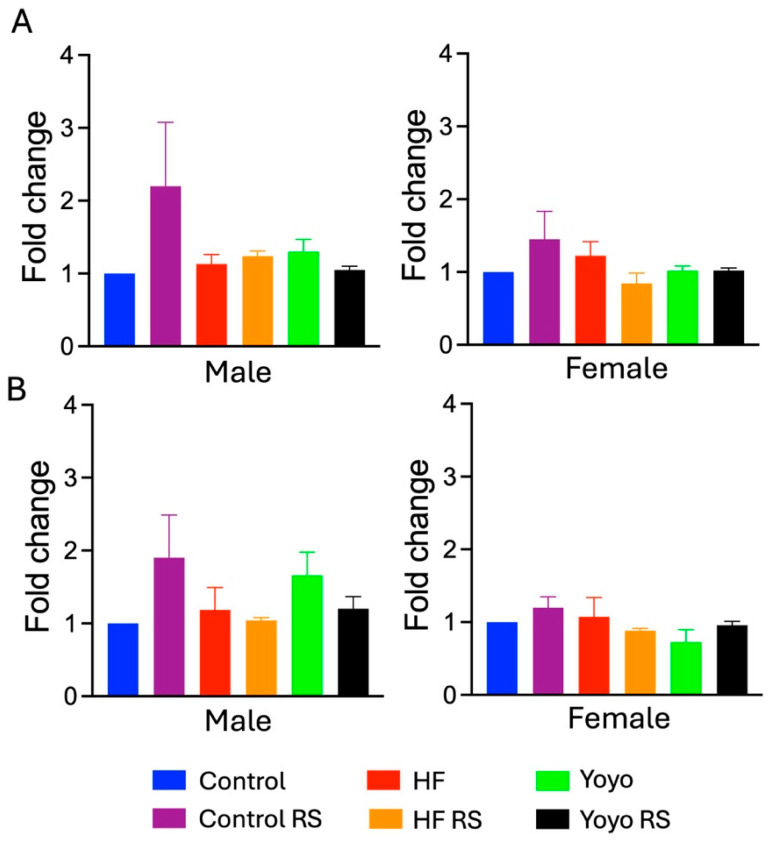
3.4. Short-Chain Fatty Acid Concentration
There were no significant differences in SCFA levels across all diets (propionate: two-way ANOVA diet × RS status male p = 0.3066, female p = 0.0705; n–Butyrate: two-way ANOVA diet × RS status male p = 0.1932, female p = 0.4170) (Figure 7).
Figure 7.
Short-chain fatty acid levels. n-Butyrate (A). Propionate (B). No change in SCFA levels across diet groups. n = 7–8/group/sex.
3.5. Resistant Starch and Yoyo Dieting Reshaped Gut Microbiota
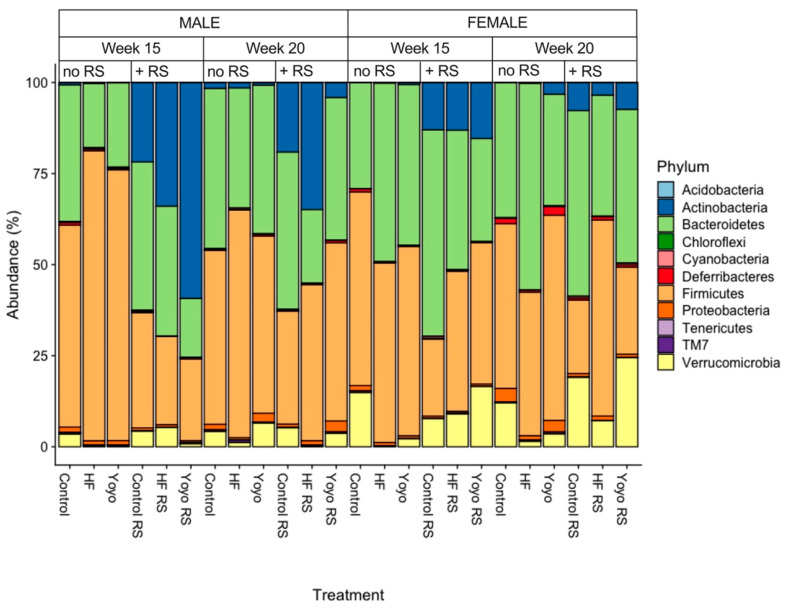
3.5.1. Relative Abundance by Phylum
From a simple visual inspection, in male mice, during the second phase of HF feeding, yoyo mice had enriched Bacteroidetes (23.2%) compared to HF (17.7%), but it was reduced compared to control mice (37.6%). However, the relative abundance of Firmicutes in yoyo mice (74.3%) was reduced compared to HF mice (79.7%) but enriched compared to controls (55.4%). By the end of the diet intervention, yoyo mice had lower Bacteroidetes (40.8%) and similar Firmicutes (48.6%) compared to controls (44.0% and 47.8%, respectively), but they had enriched Bacteroidetes and lower Firmicutes compared to HF mice (32.9% and 62.5%, respectively) (Figure 8, male, week 15). In female mice, during the second phase of HF feeding, yoyo mice had a lower relative abundance of Bacteroidetes (44.2%) than HF mice (49%), but it was higher than in control mice (29.1%). However, the relative abundance of Firmicutes between yoyo (52.0%), HF (49.3%), and control mice (53.2%) did not differ. By the end of the diet intervention, yoyo mice had lower Bacteroidetes (30.7%) and enriched Firmicutes (56.3%) compared to HF (56.8% and 39.4%, respectively) and control mice (37.0% and 45.2%, respectively) (Figure 8, female, week 15).
Figure 8.
Relative abundance. Stacked column charts representing the relative abundance of amplicon sequence variants (ASVs) at the taxonomic level of the phylum. The visualisation of ASV data displays the gut microbiota of male and female mice consuming 6 different diets in weeks 15 and 20. Diets supplemented with RS were associated with a higher relative abundance of Actinobacteria. HF: high fat. RS: resistant starch.
Supplementation with RS in a control diet (control RS) was associated with a greater relative abundance of Actinobacteria compared to a control diet only (Figure 8, male, week 15: 21.8% versus 0.63%, week 20: 19.09% versus 1.6%; Figure 8, female, week 15: 12.9% versus 0.05%, week 20: 7.73% versus 0.09%). Likewise, RS supplementation in an HF diet (HF RS) was also associated with enriched Actinobacteria compared to an HF diet only (Figure 8, male, week 15: 33.9% versus 0.26%, week 20: 34.9% versus 1.5%; Figure 8, female, week 15: 13.08% versus 0.15%, week 20: 3.46% versus 0.21%).
During the second phase of HF feeding, RS supplementation in the yoyo diet (yoyo RS) resulted in a greater relative abundance of Actinobacteria compared to the yoyo diet supplemented without RS (Figure 8, male, week 15: 59.3% versus 0.1%; Figure 8, female, week 15: 15.4% versus 7.36%, respectively). Similarly, yoyo RS mice had increased Actinobacteria compared to HF RS mice (Figure 8, male, week 15: 59.3% versus 33.9%, Figure 8, female, week 15: 15.4% versus 13.08%) (Figure 8).
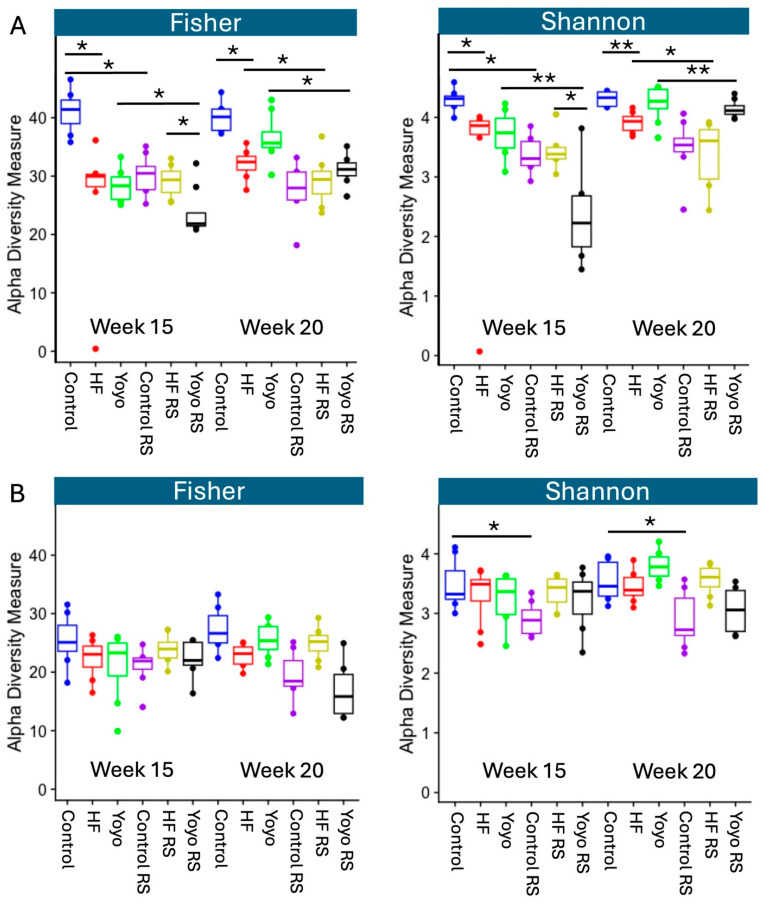
3.5.2. Alpha Diversity
Alpha diversity indices are used to describe the microbial diversity within an ecological community with respect to its richness and/or evenness [102]. The Fisher index considers ASV richness, and the Shannon index considers both richness and evenness.
At the end of the diet intervention, male mice fed an HF diet (red) had significantly lower alpha diversity than control mice (blue) (Fisher p = 0.015, Shannon p = 0.001). Male yoyo mice (green) appeared to have an alpha diversity that was in an intermediate state between control and HF mice; however, this was not significantly different (yoyo versus control: Fisher p = 0.70 and Shannon p = 0.97; yoyo versus HF: Fisher p = 0.16 and Shannon p = 0.07 (Figure 9A, week 20)). In female mice, there were no significant differences in alpha diversity at the end of the diet intervention between the HF, yoyo, and control groups (Fisher and Shannon—yoyo versus HF: p = 0.36 and p = 0.07; yoyo versus control: p = 0.23 and p = 0.31; HF versus control: p = 0.91 and p = 0.73, respectively (Figure 9B, week 20)).
Figure 9.
Alpha diversity. Fisher’s and Shannon’s diversity indices of faecal samples of male (A) and female mice (B) in week 15 and week 20. The median is illustrated by the horizontal line inside the box. The lowest and highest values within 1.5 times the interquartile range from the 1st and 3rd quartiles, respectively, are illustrated by whiskers. * p ≤ 0.05, ** p ≤ 0.01, with n = 6–8/group/sex. Boxes represent the interquartile range between the first and third quartiles. The horizontal line inside the box illustrates the median. Solid dots (●) outside the whiskers indicate greater than 1.5 times and less than 3 times the interquartile range. Graphs were generated from raw and untrimmed data. HF—high-fat diet; RS—resistant starch.
Additionally, supplementation with RS in a control diet (control RS) (purple) significantly reduced alpha diversity in comparison with a control diet only (male: Fisher p = 0.005, Shannon p = 0.001 (Figure 9A, week 20); female: Fisher p = 0.11, Shannon p = 0.04 (Figure 9B, week 20)). Similarly, RS supplementation in an HF diet (HF RS) (yellow) reduced alpha diversity compared to an HF diet alone in male (Fisher p = 0.05, Shannon p = 0.04 (Figure 9A, week 20)) but not in female mice (Fisher p = 0.76, Shannon p = 0.97 (Figure 9B, week 20)).
Likewise, RS supplementation in the second phase of the yoyo diet (yoyo RS) (black) resulted in significantly reduced alpha diversity compared to the yoyo group in male (Fisher p = 0.015, Shannon p = 0.007 (Figure 9A, week 15)) but not in female mice (Fisher p = 0.91, Shannon p = 0.97 (Figure 9B, week 15)).
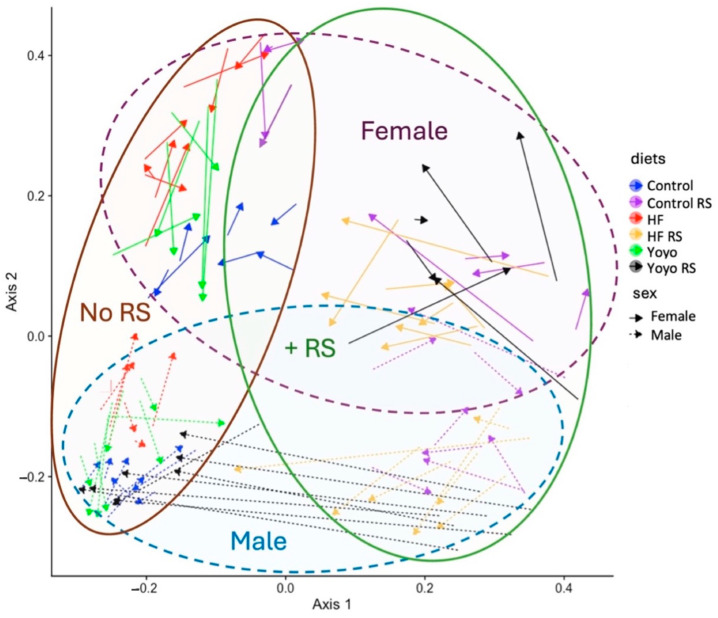
3.5.3. Beta Diversity
The Bray–Curtis measure was used to describe similarities and dissimilarities between diet treatment groups based on their gut microbial community members and abundances, and a principal coordinate analysis (PCoA) plot was constructed (Figure 10).
Figure 10.
Principal coordinate analysis (PCoA)—beta diversity. Bray–Curtis ordination plot showing the dissimilarity of the gut microbiota from mice fed six different diets at two time points (weeks 15 and 20). The microbiota profiles of different dietary treatments are represented by different colours: blue (control), purple (control RS), red (HF), yellow (HF RS), green (yoyo), and black (yoyo RS). Solid arrows represent female mice, and arrows with dashed lines represent male mice. The tail of an arrow indicates microbiota composition in week 15, while the tip of an arrow indicates microbiota composition in week 20. RS—resistant starch; HF—high fat.
HF mice (red) had a significantly different microbiota composition compared to control mice (blue) (adjusted for sex, R2 = 0.13, p = 0.001). Supplementation with RS regardless of diet (purple, yellow, black) also resulted in significantly different microbiota compositions compared to those supplemented without RS (blue, red, green) (adjusted for sex, R2 = 0.0650, p = 0.001). Moreover, we observed significantly different gut microbiota compositions in male and female mice (R2 = 0.0575, p = 0.001) (Figure 10).
At the end of the second HF feeding phase, the microbiota signatures of yoyo mice were significantly different from the control (week 15, adjusted for sex, R2 = 0.22, p = 0.001) and HF states (week 15: adjusted for sex, R2 = 0.05, p = 0.045). Moreover, by the end of the dietary intervention, this significantly altered microbiota composition of yoyo mice persisted even after a 5-week control feeding period and achieving weight loss (week 20: yoyo versus control: adjusted for sex, R2 = 0.09, p = 0.002; yoyo versus HF: adjusted for sex, R2 = 0.17, p = 0.001). Interestingly, RS supplementation in the second phase of the yoyo diet in male mice (yoyo RS) (black) appeared to exhibit a shift in the gut microbiota composition that was closer to the control group by the end of the dietary intervention. However, the microbiota profile of male yoyo RS mice remained significantly different from control mice (week 20, black versus blue, R2 = 0.26, p = 0.001). No such shift was observed in female yoyo RS mice (Figure 10).
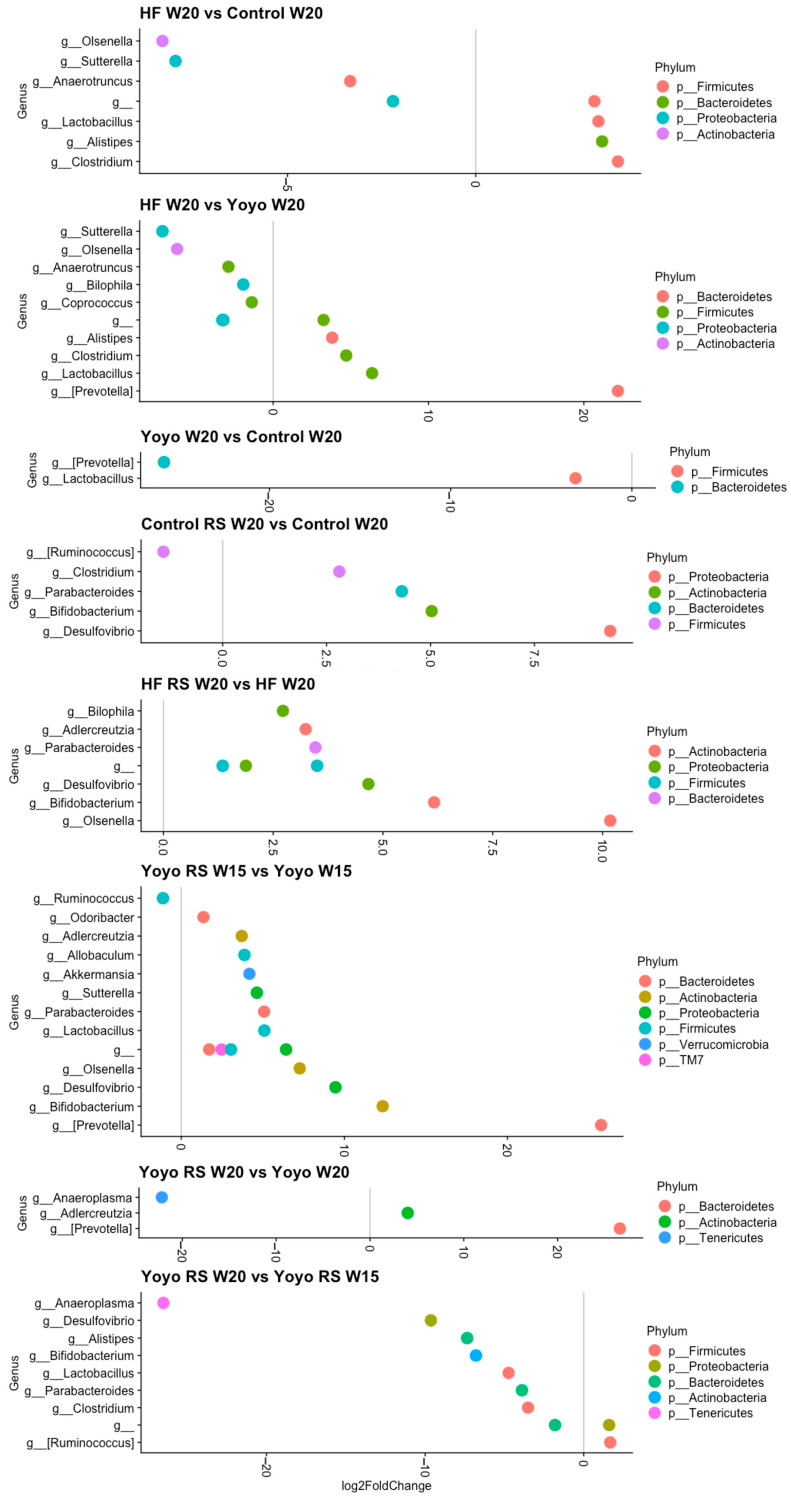
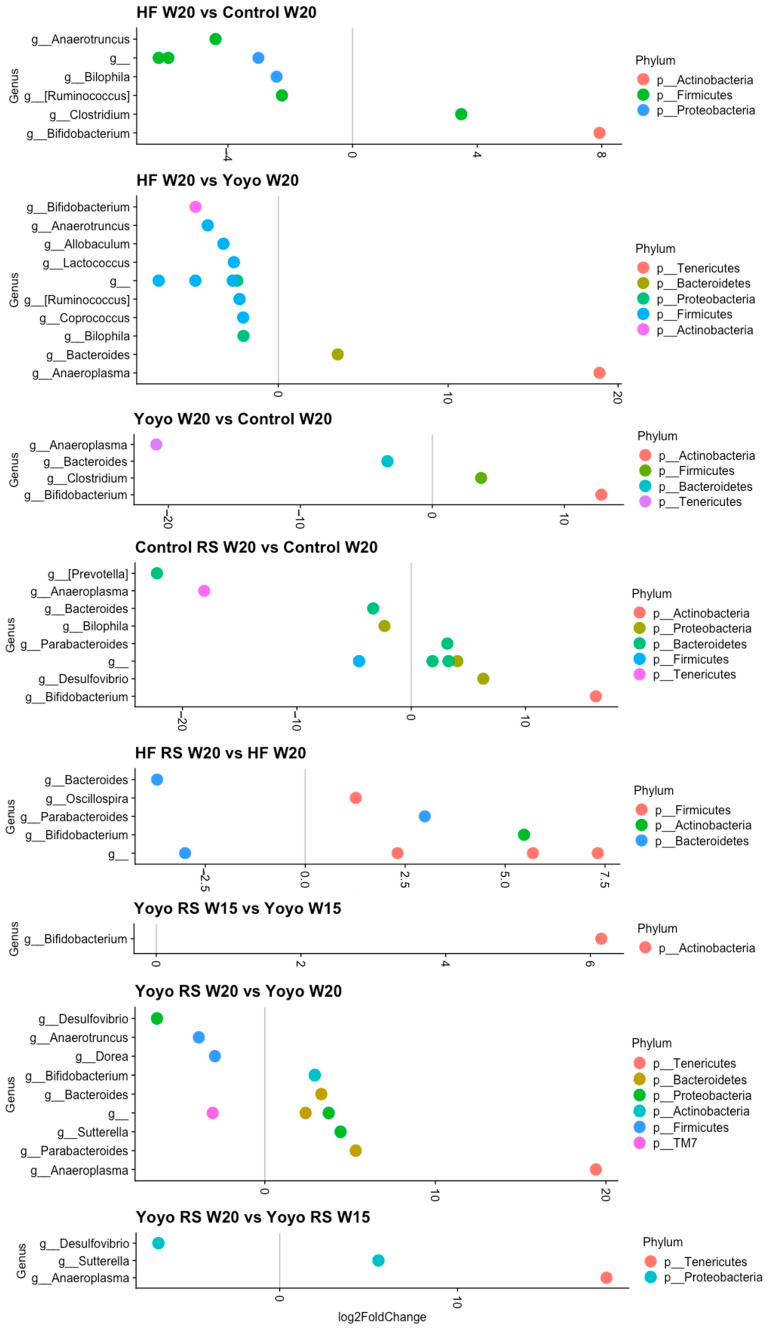
3.5.4. Differential Abundance Analysis
At the end of the diet intervention, we observed 16 (8 male; 8 female) differentially abundant genera between HF and control mice (Figure 11 and Figure 12). HF-fed mice had significantly enriched Clostridium (male: log2FC = 3.78; female: log2FC = 3.49) and reduced Anaerotruncus (male: log2FC = 3.33; female: log2FC = 4.40) compared to control mice. On the other hand, we observed 25 (12 male; 13 female) differentially abundant genera between HF and yoyo mice. HF-fed mice had significantly reduced Anaerotruncus (male: log2FC = −2.89; female: log2FC = −4.15), Bilophila (male: log2FC = −1.92; female: log2FC = −2.05), and Coprococcus (male: log2FC = −1.38; female: log2FC = −2.07) compared to yoyo mice. Additionally, there were six (two male; four female) differentially abundant genera between yoyo and control mice. Male yoyo mice had significantly reduced Prevotella (see Supplementary Materials for details on this classification) (log2FC = −25.8) and Lactobacillus (log2FC = −3.1) (Figure 11), while female yoyo mice had significantly reduced Anaeroplasma (log2FC = −20.9) and Bacteroides (log2FC = −3.4), but enriched Clostridium (log2FC = 3.7) and Bifidobacterium (log2FC = 12.8), compared to control mice (Figure 12).
Figure 11.
Differentially abundant genera in male mice. Only genera that were significantly different in relative abundance (FDR ≤ 0.01) are shown in the plot, with log2FoldChange estimated by DESeq2. RS—resistant starch; HF—high fat; W—week.
Figure 12.
Differentially abundant genera in female mice. Only genera that were significantly different in relative abundance (FDR ≤ 0.01) are shown in the plot, with log2FoldChange estimated by DESeq2. RS—resistant starch; HF—high fat; W—week.
Supplementation with RS in a control diet (control RS) resulted in 16 (5 male; 11 female) differentially abundant genera in comparison with a control diet only, particularly markedly increased Parabacteroides (male: log2FC = 4.31; female: log2FC = 3.16), Bifidobacterium (male: log2FC = 5.03 [female: log2FC = 16.16), and Desulfovibrio (male: log2FC = 9.32; female: log2FC = 6.31). Similarly, RS supplementation in an HF diet (HF RS) resulted in 30 (19 male; 11 female) differentially abundant genera compared to an HF diet alone, particularly enriched Parabacteroides (male: log2FC = 3.46; female: log2FC = 2.99) and Bifidobacterium (male: log2FC = 6.16; female: log2FC = 5.47) (Figure 11 and Figure 12).
In males, RS supplementation in the second phase of the yoyo diet (yoyo RS) resulted in 15 differentially abundant genera (Figure 11 and Figure 12). In particular, yoyo RS mice had enriched Parabacteroides (log2FC = 5.08), Bifidobacterium (log2FC = 12.35), Desulfovibrio (log2FC = 9.46), Lactobacillus (log2FC = 5.09), and Adlercreutzia (log2FC = 3.71) but reduced Ruminococcus (log2FC = −1.12) compared to yoyo mice. Interestingly, at the end of the dietary intervention, we only observed three differentially abundant genera in yoyo RS mice compared to yoyo mice, including Prevotella (log2FC = 26.63), Anaeroplasma (log2FC = −22.18), and Adlercreutzia log2FC = 4.02) (Figure 11). On the other hand, in female mice, we observed 11 differentially abundant genera between yoyo RS and yoyo mice. Particularly, yoyo RS mice had significantly enriched Bifidobacterium (log2FC = 6.15), Parabacteroides (log2FC = 5.33), and Bacteroides (log2FC = 3.31) but reduced Desulfovibrio (log2FC = −6.32) and Dorea (log2FC = −2.93) compared to yoyo mice (Figure 12).
In order to explore which genera may have accounted for the shift in beta diversity closer to the control state of male yoyo RS mice, we observed nine differentially abundant genera. At the end of the dietary intervention, compared to the second phase of HF feeding with RS supplementation, yoyo RS mice exhibited significantly enriched Ruminococcus (also known as Mediterraneibacter, refer to Supplementary Materials for more details) (log2FC = 1.67) and significantly reduced Parabacteroides (log2FC = −3.90), Bifidobacterium (log2FC = −6.79), Desulfovibrio (log2FC = −9.64), and Lactobacillus (log2FC = −4.74) (Figure 11).
4. Discussion
Relatively few studies have evaluated the effect of yoyo dieting and RS supplementation on metabolic and gut health. The present study revealed that yoyo dieting is both beneficial and detrimental to metabolic health, with the gut microbiome composition remaining in an intermediate state of dysbiosis. We also showed the beneficial effects of RS supplementation in improving metabolic outcomes, in addition to reshaping the gut microbiome.
4.1. Yoyo Dieting Appears to Be a Double-Edged Sword: Beneficial and Deleterious Effects of Yoyo Dieting on Metabolic and Gut Health
While there have been controversial findings around the effects of yoyo dieting on the metabolism, our study revealed similar metabolic outcomes following yoyo and control dieting. This aligns with previous studies [47,103] highlighting the overall importance of weight loss in improving metabolic health despite yoyo dieting. However, despite the benefits of weight loss, we also observed that yoyo dieting led to a greater rate of weight regain in male but not female mice, compared to continuous HF feeding, potentially due to gut microbial differences between sexes. This is consistent with previous studies suggesting that yoyo dieting may be a risk factor in future weight regain and obesity development [47,104,105]. Given the sex differences that we observed in metabolic health and gut microbiome changes, our study further emphasises the need to investigate both sexes in metabolic studies given the paucity of studies in this area.
It is well established that HF diet feeding alters the gut microbiota composition [55,106,107]. There is also increasing evidence to suggest that yoyo dieting results in significantly different gut bacterial diversity and long–term alterations in gut microbiota composition [47,48]. A study by Thaiss et al. [47] investigated the long–term effects of yoyo dieting on mice exposed to two cycles of yoyo dieting. They found that despite achieving successful weight loss, the microbiota profile of yoyo mice remained in an intermediate configuration between the obese and control states. Furthermore, this post-dieting microbiome signature persisted and required a period more than five times longer than the last dieting period to reverse back to the control state. Our results are consistent with this study as we found different bacterial signatures and bacterial diversity from the control and HF states, despite successful weight loss. Collectively, these results imply that although the weight loss following yoyo dieting has short–term benefits on metabolic health [108], it is possible that the intermediate gut microbiome signature present in yoyo dieting may play a role in increasing the susceptibility to weight regain shortly after weight loss.
4.2. Beneficial Effects of Resistant Starch on Metabolic Health
Our findings highlight the beneficial effects of RS in improving metabolic outcomes, which are in line with numerous animal [69,109,110,111,112,113,114,115,116] and human studies [53,117,118,119,120,121]. Additionally, our study shows a striking protective effect of RS in improving metabolic outcomes, particularly in reducing body weight in male HF RS mice only. It is also important to note that there were no clinical signs of illness or changes in food intake in any of our dietary groups. The observed weight loss with RS supplementation in the HF diet (HF RS) during the second half of our study (particularly during weeks 11–16) may be due to impaired nutrient absorption and/or increased energy expenditure, which we were not able to measure in this study. Therefore, future studies are warranted to verify this hypothesis. There are also inconsistencies in the literature around RS and weight loss that could be attributed to several factors, such as variations in experimental models, treatment durations, types of RS, and different treatment dosages. Moreover, most of what we know about the effects of RS is based on animal and human studies that have mainly used RS2 (raw potato, green banana, high-amylose maize starch) [52,53,69,111,113,116,122,123,124,125,126,127,128], with limited studies on RS4 (chemically modified starch) [129,130,131,132]. Although RS2 is more commonly found in foods, it is less resistant and easily degraded by heat (such as in cooking). In contrast, RS4 offers significantly greater chemical resistance to digestive enzymes in the gut compared to RS2 [80,133].
RS represents a small portion in most foods (<2.5%, dry matter basis), even in starchy foods (<15%, dry matter basis) [91]. On average, Australian adults consume only 3–9 g of RS per day [115], which is significantly below the recommended daily intake of 15–20 g/day of RS [115] considered essential for promoting bowel health benefits [91,115]. Currently, there is no consensus on the effective dosage for different types of RS. In our study, we incorporated RS4 at fractions ranging from 11% to 14% (by weight), which is similar to previous rodent studies [134,135,136]. However, it is important to note that these doses, while effective in rodents, are not directly comparable to the RS levels required in humans. Several human studies have been conducted to explore the effective dosage of RS4 in increasing SCFA production to exert beneficial effects. A 26-week clinical study by Upadhyaya et al. [131] showed that dietary supplementation with 30% RS4 (v/v in flour) significantly increased several faecal SCFA levels in individuals with metabolic syndrome, including propionate, butyrate, valerate, and hexanoate. In another study, a dose–response trial was conducted to investigate the effectiveness of different doses of RS4 (ranging from 10 to 50 g/day of RS4) in healthy participants [132]. Their findings indicated that the majority of tested RS4 doses did not change the overall concentration of faecal SCFAs. However, a significant increase in the concentration of propionate was observed at a minimum of a very high RS4 dose of 35 g/day. SCFA concentrations in past studies were usually assessed in faecal samples as a measure of colonic absorption and metabolism. However, it is important to analyse plasma SCFA levels in order to assess their systemic effects. Therefore, in our study, we analysed plasma propionate and butyrate concentrations and observed no differences in any of our dietary groups. Of note, the concentrations of SCFAs in plasma and faecal samples are known to be different [137,138,139]. It is important to consider that SCFA concentrations can be influenced by diet, the gut microbiome, the and host metabolism [140], which can lead to considerable variations in SCFA profiles in various conditions and methods of analysis. Thus, further research is required to gain a better understanding of the role that SCFAs play in yoyo dieting and RS supplementation, as well as their potential use as biomarkers or therapeutic targets.
4.3. Beneficial Effects of Resistant Starch on Gut Microbiome
We observed that RS supplementation resulted in enriched Bifidobacterium and Parabacteroides, along with reduced bacterial diversity and distinct microbiota composition. The increase in the relative abundance of Bifidobacterium aligns with findings from various studies [79,141,142,143], showing the effect of RS in significantly altering the gut microbiome. This is likely to be advantageous as this genus is representative of microbial probiotics [144,145], which are associated with stomach acid tolerance and carbohydrate metabolism [146,147,148], anti-inflammatory properties [149], and the regulation of bowel movement [131,150,151,152]. Likewise, the enrichment of Parabacteroides is likely beneficial, as it has been linked to improvements in conditions such as heparinase-exacerbated acute pancreatitis [153], neuroprotection [154], and the attenuation of inflammation [155]. Notably, Bifidobacterium and Parabacteroides are both SCFA producers [153,156,157,158] that exert beneficial effects on human health [159,160]. Moreover, we observed reduced bacterial diversity following resistant starch supplementation in male mice. This was an unexpected finding as reduced diversity is often associated with dysbiosis, particularly in obesity [161,162,163]. However, the notion of diversity as an indicator of health status is being challenged, with a suggested focus towards using health-associated taxa as a better metric for health status. There is also emerging evidence showing that reduced diversity after dietary fibre intervention has been associated with improved clinical outcomes [164,165,166]. Moreover, it is important to consider that dietary fibre structure plays a key role in influencing the ability of gut bacteria to utilise these substrates [167,168]. For example, low/intermediate-specificity dietary fibres, such as RS2 [168], can be utilised and shared by many bacteria [167,168], which may promote the growth of multiple microbes, resulting in increased bacterial diversity [169]. On the other hand, RS4, a type of dietary fibre with greater specificity than RS2 [132,168], can only be utilised by a small group of bacteria [167,168], which will promote the increased growth of fewer microbes, resulting in reduced diversity [169]. This is an important consideration as reduced diversity is not always detrimental and can still be associated with improved health status.
Furthermore, we found that supplementation with RS in male yoyo mice shifted their gut microbiota profile closer to the control state following weight loss. However, the microbiota profiles of yoyo RS and control mice were still significantly different by the end of the dietary intervention, which is consistent with the findings by Thaiss et al. [47]. This suggests a promising effect of RS supplementation in shifting the gut microbiota composition in the short–term but not in the long–term restoration of the gut microbiome. Of note, microbiota restoration requires not only consuming a healthy (control) diet and achieving successful weight loss but also long–term weight management to ensure sustainable weight loss [47]. Moreover, we also observed significantly different genera associated with shifting the gut microbiome composition of yoyo RS after weight loss. These include enriched Mediterraneibacter and reduced Bifidobacterium, Parabacteroides, and Desulfovibrio, which may have contradictory implications for human health. On one hand, enriched Mediterraneibacter is likely not to be advantageous as this has been positively associated with increased risks of developing obesity [170], liver cancer [171], and gut dysbiosis [172]. Likewise, a reduction in Bifidobacterium and Parabacteroides might not be beneficial as they have been associated with increased risks of irritable bowel syndrome [173,174,175,176,177] and obesity [178,179,180]. However, reduced Desulfovibrio is likely to be beneficial as these have been associated with reduced risks of obesity [161,181,182], inflammatory bowel disease [183,184], fatty liver disease [182], and diabetes [185].
In this study, while the effect of yoyo dieting and resistant starch on the gut microbiome was investigated, one explicit limitation was the potential confounding effect of cohousing animals (four mice per cage and two cages per diet treatment). However, single housing was not feasible due to ethical concerns around compromising the biological and behavioural well-being of animals, which could result in heightened emotional stress and a lack of thermoregulation [186,187,188,189,190]. Furthermore, exploring gut microbiota changes using full-length 16S long-read sequencing or shotgun sequencing will provide valuable insights as these techniques provide higher taxonomy resolution and functional profiling.
5. Conclusions
In summary, our study reveals significant sex-dependent differences in metabolic outcomes and microbiome signatures. While yoyo dieting leads to metabolic health improvement through short–term weight loss, it also results in a greater risk of obesity relapse. Interestingly, increased resistant starch intake reduces body weight and may reduce the risk of rapid weight regain, potentially via gut microbiome restoration in male but not in female mice. However, the functional implications of resistant starch-induced microbiota changes for metabolic health, weight regain susceptibility, and sex differences remain to be further explored. This study emphasises the importance of improving the gut microbiome as an attractive target for sustainable weight management and the development of interventions for obesity and related conditions. Additional research is required to determine the effective dosage of resistant starch in humans to support the development of evidence-based lifestyle management initiatives to improve gut and metabolic health. Moreover, further long–term human studies are warranted to elucidate the underlying mechanisms of how resistant starch and yoyo dieting affect the gut microbiota and contribute to varying weight loss and weight regain susceptibility outcomes between sexes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu16183138/s1. Refs. [170,191,192] are cited in the supplementary materials.
Author Contributions
Conceptualization, L.R.R., S.L.M. and K.P.-N.; methodology, L.R.R., K.P.-N., S.L.M. and G.M.K.; animal experiments, K.P.-N. and L.R.R.; SCFA experiment, G.M.K., K.P.-N. and L.R.R.; group allocation, K.P.-N. and L.R.R.; OGTT and ITT experiments, K.P.-N., L.R.R., S.L.M., T.C. and K.A.-M.; histological experiment and examination, K.P.-N.; histological analysis, K.P.-N. and M.Q.M.; formal analysis, K.P.-N. and M.O.; writing—original draft preparation, K.P.-N.; writing—review and editing, K.P.-N., L.R.R., M.O., K.A.-M., S.L.M., G.M.K., M.Q.M. and T.C.; visualization, K.P.-N.; supervision, L.R.R.; project administration, K.P.-N. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The animal study was conducted in accordance with the guidelines of the National Health and Medical Research Council and approved by the Deakin University Animal Ethics Committee (G01-2021; date of approval: 7 May 2021).
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article or upon reasonable request.
Conflicts of Interest
M.O’H. has a financial interest in Prevatex Pty Ltd., a company developing probiotic-based biotherapeutics. Other authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Sarwer D.B., Polonsky H.M. The Psychosocial Burden of Obesity. Endocrinol. Metab. Clin. N. Am. 2016;45:677–688. doi: 10.1016/j.ecl.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Obesity: Preventing and Managing the Global Epidemic. World Health Organization; Geneva, Switzerland: 2000. [PubMed] [Google Scholar]
- 3.O’Brien P.D., Hinder L.M., Callaghan B.C., Feldman E.L. Neurological consequences of obesity. Lancet Neurol. 2017;16:465–477. doi: 10.1016/S1474-4422(17)30084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blüher M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019;15:288–298. doi: 10.1038/s41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 5.Godoy-Matos A.F., Silva Júnior W.S., Valerio C.M. NAFLD as a continuum: From obesity to metabolic syndrome and diabetes. Diabetol. Metab. Syndr. 2020;12:60. doi: 10.1186/s13098-020-00570-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang M., Liu S., Zhang C. The Related Metabolic Diseases and Treatments of Obesity. Healthcare. 2022;10:1616. doi: 10.3390/healthcare10091616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guh D.P., Zhang W., Bansback N., Amarsi Z., Birmingham C.L., Anis A.H. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petrie J.R., Guzik T.J., Touyz R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018;34:575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Goblan A.S., Al-Alfi M.A., Khan M.Z. Mechanism linking diabetes mellitus and obesity. Diabetes Metab. Syndr. Obes. 2014;7:587–591. doi: 10.2147/dmso.S67400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fabbrini E., Sullivan S., Klein S. Obesity and nonalcoholic fatty liver disease: Biochemical, metabolic, and clinical implications. Hepatology. 2010;51:679–689. doi: 10.1002/hep.23280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarwar R., Pierce N., Koppe S. Obesity and nonalcoholic fatty liver disease: Current perspectives. Diabetes Metab. Syndr. Obes. 2018;11:533–542. doi: 10.2147/dmso.S146339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhaskaran K., dos-Santos-Silva I., Leon D.A., Douglas I.J., Smeeth L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–953. doi: 10.1016/S2213-8587(18)30288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stephenson J., Smith C.M., Kearns B., Haywood A., Bissell P. The association between obesity and quality of life: A retrospective analysis of a large-scale population-based cohort study. BMC Public Health. 2021;21:1990. doi: 10.1186/s12889-021-12009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Finkelstein E.A., Trogdon J.G., Cohen J.W., Dietz W. Annual medical spending attributable to obesity: Payer-and service-specific estimates. Health Aff. Millwood. 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 15.Griffith R. Obesity, Poverty and Public Policy. Econ. J. 2022;132:1235–1258. doi: 10.1093/ej/ueac013. [DOI] [Google Scholar]
- 16.Australian Institute of Health Welfare (AIHW) Overweight and Obesity among Australian Children and Adolescents. AIHW; Canberra, Australia: 2020. [Google Scholar]
- 17.Bhurosy T., Jeewon R. Overweight and obesity epidemic in developing countries: A problem with diet, physical activity, or socioeconomic status? Sci. World J. 2014;2014:964236. doi: 10.1155/2014/964236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Velapati S.R., Shah M., Kuchkuntla A.R., Abu-dayyeh B., Grothe K., Hurt R.T., Mundi M.S. Weight Regain after Bariatric Surgery: Prevalence, Etiology, and Treatment. Curr. Nutr. Rep. 2018;7:329–334. doi: 10.1007/s13668-018-0243-0. [DOI] [PubMed] [Google Scholar]
- 19.Kraschnewski J.L., Boan J., Esposito J., Sherwood N.E., Lehman E.B., Kephart D.K., Sciamanna C.N. Long-term weight loss maintenance in the United States. Int. J. Obes. 2010;34:1644–1654. doi: 10.1038/ijo.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neumark-Sztainer D., Rock C.L., Thornquist M.D., Cheskin L.J., Neuhouser M.L., Barnett M.J. Weight-control behaviors among adults and adolescents: Associations with dietary intake. Prev. Med. 2000;30:381–391. doi: 10.1006/pmed.2000.0653. [DOI] [PubMed] [Google Scholar]
- 21.Jeffery R.W., Adlis S.A., Forster J.L. Prevalence of dieting among working men and women: The healthy worker project. Health Psychol. 1991;10:274. doi: 10.1037//0278-6133.10.4.274. [DOI] [PubMed] [Google Scholar]
- 22.Anderson J.W., Konz E.C., Frederich R.C., Wood C.L. Long-term weight-loss maintenance: A meta-analysis of US studies. Am. J. Clin. Nutr. 2001;74:579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 23.Weiss E.C., Galuska D.A., Khan L.K., Gillespie C., Serdula M.K. Weight regain in US adults who experienced substantial weight loss, 1999–2002. Am. J. Prev. Med. 2007;33:34–40. doi: 10.1016/j.amepre.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 24.Bacon L., Aphramor L. Weight Science: Evaluating the Evidence for a Paradigm Shift. Nutr. J. 2011;10:9. doi: 10.1186/1475-2891-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mann T., Tomiyama A.J., Westling E., Lew A.-M., Samuels B., Chatman J. Medicare’s search for effective obesity treatments: Diets are not the answer. Am. Psychol. 2007;62:220. doi: 10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]
- 26.Anastasiou C.A., Karfopoulou E., Yannakoulia M. Weight regaining: From statistics and behaviors to physiology and metabolism. Metabolism. 2015;64:1395–1407. doi: 10.1016/j.metabol.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 27.Franz M.J., VanWormer J.J., Crain A.L., Boucher J.L., Histon T., Caplan W., Bowman J.D., Pronk N.P. Weight-loss outcomes: A systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J. Am. Diet. Assoc. 2007;107:1755–1767. doi: 10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 28.Jimenez L.S., Mendonça Chaim F.H., Mendonça Chaim F.D., Utrini M.P., Gestic M.A., Chaim E.A., Cazzo E. Impact of Weight Regain on the Evolution of Non-alcoholic Fatty Liver Disease after Roux-en-Y Gastric Bypass: A 3-Year Follow-up. Obes. Surg. 2018;28:3131–3135. doi: 10.1007/s11695-018-3286-9. [DOI] [PubMed] [Google Scholar]
- 29.Crujeiras A.B., Zulet M.A., Lopez-Legarrea P., de la Iglesia R., Pardo M., Carreira M.C., Martínez J.A., Casanueva F.F. Association between circulating irisin levels and the promotion of insulin resistance during the weight maintenance period after a dietary weight-lowering program in obese patients. Metabolism. 2014;63:520–531. doi: 10.1016/j.metabol.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 30.Lien L.F., Haqq A.M., Arlotto M., Slentz C.A., Muehlbauer M.J., McMahon R.L., Rochon J., Gallup D., Bain J.R., Ilkayeva O. The STEDMAN project: Biophysical, biochemical and metabolic effects of a behavioral weight loss intervention during weight loss, maintenance, and regain. OMICS J. Integr. Biol. 2009;13:21–35. doi: 10.1089/omi.2008.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang P., Holst C., Wodzig W., Andersen M., Astrup A., Van Baak M., Larsen T., Jebb S., Kafatos A., Pfeiffer A. Circulating ACE is a predictor of weight loss maintenance not only in overweight and obese women, but also in men. Int. J. Obes. 2012;36:1545–1551. doi: 10.1038/ijo.2011.278. [DOI] [PubMed] [Google Scholar]
- 32.Linna M., Borg P., Kukkonen-Harjula K., Fogelholm M., Nenonen A., Ahotupa M., Vasankari T. Successful weight maintenance preserves lower levels of oxidized LDL achieved by weight reduction in obese men. Int. J. Obes. 2007;31:245–253. doi: 10.1038/sj.ijo.0803413. [DOI] [PubMed] [Google Scholar]
- 33.Thomas T.R., Warner S.O., Dellsperger K.C., Hinton P.S., Whaley-Connell A.T., Rector R.S., Liu Y., Linden M.A., Chockalingam A., Thyfault J.P. Exercise and the metabolic syndrome with weight regain. J. Appl. Physiol. 2010;109:3–10. doi: 10.1152/japplphysiol.01361.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Delbridge E.A., Prendergast L.A., Pritchard J.E., Proietto J. One-year weight maintenance after significant weight loss in healthy overweight and obese subjects: Does diet composition matter? Am. J. Clin. Nutr. 2009;90:1203–1214. doi: 10.3945/ajcn.2008.27209. [DOI] [PubMed] [Google Scholar]
- 35.Matsuo T., Kato Y., Murotake Y., Kim M., Unno H., Tanaka K. An increase in high-density lipoprotein cholesterol after weight loss intervention is associated with long-term maintenance of reduced visceral abdominal fat. Int. J. Obes. 2010;34:1742–1751. doi: 10.1038/ijo.2010.95. [DOI] [PubMed] [Google Scholar]
- 36.Brownell K.D., Rodin J. Medical, Metabolic, and Psychological Effects of Weight Cycling. Arch. Intern. Med. 1994;154:1325–1330. doi: 10.1001/archinte.1994.00420120035004. [DOI] [PubMed] [Google Scholar]
- 37.Brunner K.T., Henneberg C.J., Wilechansky R.M., Long M.T. Nonalcoholic Fatty Liver Disease and Obesity Treatment. Curr. Obes. Rep. 2019;8:220–228. doi: 10.1007/s13679-019-00345-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hallberg S.J., Gershuni V.M., Hazbun T.L., Athinarayanan S.J. Reversing Type 2 Diabetes: A Narrative Review of the Evidence. Nutrients. 2019;11:766. doi: 10.3390/nu11071644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kakinami L., Knäuper B., Brunet J. Weight cycling is associated with adverse cardiometabolic markers in a cross-sectional representative US sample. J. Epidemiol. Community Health. 2020;74:662–667. doi: 10.1136/jech-2019-213419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mackie G.M., Samocha-Bonet D., Tam C.S. Does weight cycling promote obesity and metabolic risk factors? Obes. Res. Clin. Pract. 2017;11:131–139. doi: 10.1016/j.orcp.2016.10.284. [DOI] [PubMed] [Google Scholar]
- 41.Korkeila M., Rissanen A., Kaprio J., Sørensen T.I., Koskenvuo M. Weight-loss attempts and risk of major weight gain: A prospective study in Finnish adults. Am. J. Clin. Nutr. 1999;70:965–975. doi: 10.1093/ajcn/70.6.965. [DOI] [PubMed] [Google Scholar]
- 42.Pietiläinen K., Saarni S., Kaprio J., Rissanen A. Does dieting make you fat? A twin study. Int. J. Obes. 2012;36:456–464. doi: 10.1038/ijo.2011.160. [DOI] [PubMed] [Google Scholar]
- 43.Martin A.M., Sun E.W., Rogers G.B., Keating D.J. The Influence of the Gut Microbiome on Host Metabolism through the Regulation of Gut Hormone Release. Front. Physiol. 2019;10:428. doi: 10.3389/fphys.2019.00428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sultan S., El-Mowafy M., Elgaml A., Ahmed T.A.E., Hassan H., Mottawea W. Metabolic Influences of Gut Microbiota Dysbiosis on Inflammatory Bowel Disease. Front. Physiol. 2021;12:715506. doi: 10.3389/fphys.2021.715506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boulangé C.L., Neves A.L., Chilloux J., Nicholson J.K., Dumas M.-E. Impact of the gut microbiota on inflammation, obesity, and metabolic disease. Genome Med. 2016;8:42. doi: 10.1186/s13073-016-0303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ley R.E., Bäckhed F., Turnbaugh P., Lozupone C.A., Knight R.D., Gordon J.I. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thaiss C.A., Itav S., Rothschild D., Meijer M.T., Levy M., Moresi C., Dohnalová L., Braverman S., Rozin S., Malitsky S., et al. Persistent microbiome alterations modulate the rate of post-dieting weight regain. Nature. 2016;540:544–551. doi: 10.1038/nature20796. [DOI] [PubMed] [Google Scholar]
- 48.Humblot C., Seyoum Y., Turpin W., Mrabt R., List E.O., Berryman D.E., Jensen E.A., Sustarsic E.G., Kopchick J.J., Ricort J.-M. Long Term Weight Cycling Affects Fecal Microbiota of Mice. Mol. Nutr. Food Res. 2022;66:2200439. doi: 10.1002/mnfr.202200439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 50.Ridaura V.K., Faith J.J., Rey F.E., Cheng J., Duncan A.E., Kau A.L., Griffin N.W., Lombard V., Henrissat B., Bain J.R., et al. Gut Microbiota from Twins Discordant for Obesity Modulate Metabolism in Mice. Science. 2013;341:1241214. doi: 10.1126/science.1241214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim M.H., Yun K.E., Kim J., Park E., Chang Y., Ryu S., Kim H.L., Kim H.N. Gut microbiota and metabolic health among overweight and obese individuals. Sci. Rep. 2020;10:19417. doi: 10.1038/s41598-020-76474-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alfa M.J., Strang D., Tappia P.S., Olson N., DeGagne P., Bray D., Murray B.L., Hiebert B. A Randomized Placebo Controlled Clinical Trial to Determine the Impact of Digestion Resistant Starch MSPrebiotic(®) on Glucose, Insulin, and Insulin Resistance in Elderly and Mid-Age Adults. Front. Med. 2017;4:260. doi: 10.3389/fmed.2017.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li H., Zhang L., Li J., Wu Q., Qian L., He J., Ni Y., Kovatcheva-Datchary P., Yuan R., Liu S., et al. Resistant starch intake facilitates weight loss in humans by reshaping the gut microbiota. Nat. Metab. 2024;6:578–597. doi: 10.1038/s42255-024-00988-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qin J., Li R., Raes J., Arumugam M., Burgdorf K.S., Manichanh C., Nielsen T., Pons N., Levenez F., Yamada T., et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leeming E.R., Louca P., Gibson R., Menni C., Spector T.D., Le Roy C.I. The complexities of the diet-microbiome relationship: Advances and perspectives. Genome Med. 2021;13:10. doi: 10.1186/s13073-020-00813-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Filippis F., Pellegrini N., Vannini L., Jeffery I.B., La Storia A., Laghi L., Serrazanetti D.I., Di Cagno R., Ferrocino I., Lazzi C. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65:1812–1821. doi: 10.1136/gutjnl-2015-309957. [DOI] [PubMed] [Google Scholar]
- 57.Qian Y., Zhao X., Kan J. Preventive effect of resistant starch on activated carbon-induced constipation in mice. Exp. Ther. Med. 2013;6:228–232. doi: 10.3892/etm.2013.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang J., Huang J.H., Cheng Y.F., Yang G.M. Banana resistant starch and its effects on constipation model mice. J. Med. Food. 2014;17:902–907. doi: 10.1089/jmf.2013.3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Clarke J.M., Topping D.L., Bird A.R., Young G.P., Cobiac L. Effects of high-amylose maize starch and butyrylated high-amylose maize starch on azoxymethane-induced intestinal cancer in rats. Carcinogenesis. 2008;29:2190–2194. doi: 10.1093/carcin/bgn192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bojarczuk A., Skąpska S., Mousavi Khaneghah A., Marszałek K. Health benefits of resistant starch: A review of the literature. J. Funct. Foods. 2022;93:105094. doi: 10.1016/j.jff.2022.105094. [DOI] [Google Scholar]
- 61.Nofrarías M., Martínez-Puig D., Pujols J., Majó N., Pérez J.F. Long-term intake of resistant starch improves colonic mucosal integrity and reduces gut apoptosis and blood immune cells. Nutrition. 2007;23:861–870. doi: 10.1016/j.nut.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 62.Qin S., Zhang K., Ding X., Bai S., Wang J., Tian G., Xuan Y., Su Z., Zeng Q. Microbiome-metabolomics analysis insight into the effects of dietary resistant starch on intestinal integrity. Food Chem. 2023;401:134148. doi: 10.1016/j.foodchem.2022.134148. [DOI] [PubMed] [Google Scholar]
- 63.Zhao Y., Hasjim J., Li L., Jane J.-L., Hendrich S., Birt D.F. Inhibition of azoxymethane-induced preneoplastic lesions in the rat colon by a cooked stearic acid complexed high-amylose cornstarch. J. Agric. Food Chem. 2011;59:9700–9708. doi: 10.1021/jf202002c. [DOI] [PubMed] [Google Scholar]
- 64.Cray N., Zhao Y., Fang Y., Liu P., Pollak L., Duvick S., Birt D.F., Whitley E.M. Effects of dietary resistant starch on the wnt signaling pathway and preneoplastic cells in the colons of azoxymethane-treated rats. Nutr. Cancer. 2017;69:632–642. doi: 10.1080/01635581.2017.1299875. [DOI] [PubMed] [Google Scholar]
- 65.Hu J., Lin S., Zheng B., Cheung P.C. Short-chain fatty acids in control of energy metabolism. Crit. Rev. Food Sci. Nutr. 2018;58:1243–1249. doi: 10.1080/10408398.2016.1245650. [DOI] [PubMed] [Google Scholar]
- 66.Liu H., Zhang M., Ma Q., Tian B., Nie C., Chen Z., Li J. Health beneficial effects of resistant starch on diabetes and obesity via regulation of gut microbiota: A review. Food Funct. 2020;11:5749–5767. doi: 10.1039/d0fo00855a. [DOI] [PubMed] [Google Scholar]
- 67.Keenan M.J., Zhou J., McCutcheon K.L., Raggio A.M., Bateman H.G., Todd E., Jones C.K., Tulley R.T., Melton S., Martin R.J. Effects of resistant starch, a non-digestible fermentable fiber, on reducing body fat. Obesity. 2006;14:1523–1534. doi: 10.1038/oby.2006.176. [DOI] [PubMed] [Google Scholar]
- 68.Zhou J., Martin R.J., Tulley R.T., Raggio A.M., McCutcheon K.L., Shen L., Danna S.C., Tripathy S., Hegsted M., Keenan M.J. Dietary resistant starch upregulates total GLP-1 and PYY in a sustained day-long manner through fermentation in rodents. Am. J. Physiol.-Endocrinol. Metab. 2008;295:E1160–E1166. doi: 10.1152/ajpendo.90637.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Higgins J.A., Jackman M.R., Brown I.L., Johnson G.C., Steig A., Wyatt H.R., Hill J.O., MacLean P.S. Resistant starch and exercise independently attenuate weight regain on a high fat diet in a rat model of obesity. Nutr. Metab. 2011;8:49. doi: 10.1186/1743-7075-8-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.DeMartino P., Cockburn D.W. Resistant starch: Impact on the gut microbiome and health. Curr. Opin. Biotechnol. 2020;61:66–71. doi: 10.1016/j.copbio.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 71.Rivière A., Selak M., Lantin D., Leroy F., De Vuyst L. Bifidobacteria and butyrate-producing colon bacteria: Importance and strategies for their stimulation in the human gut. Front. Microbiol. 2016;7:979. doi: 10.3389/fmicb.2016.00979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roediger W. Role of anaerobic bacteria in the metabolic welfare of the colonic mucosa in man. Gut. 1980;21:793–798. doi: 10.1136/gut.21.9.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Donohoe D.R., Garge N., Zhang X., Sun W., O’Connell T.M., Bunger M.K., Bultman S.J. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 2011;13:517–526. doi: 10.1016/j.cmet.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gao Z., Yin J., Zhang J., Ward R.E., Martin R.J., Lefevre M., Cefalu W.T., Ye J. Butyrate improves insulin sensitivity and increases energy expenditure in mice. Diabetes. 2009;58:1509–1517. doi: 10.2337/db08-1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Koh A., De Vadder F., Kovatcheva-Datchary P., Bäckhed F. From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell. 2016;165:1332–1345. doi: 10.1016/j.cell.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 76.Chen Z., Liang N., Zhang H., Li H., Guo J., Zhang Y., Chen Y., Wang Y., Shi N. Resistant starch and the gut microbiome: Exploring beneficial interactions and dietary impacts. Food Chem. X. 2024;21:101118. doi: 10.1016/j.fochx.2024.101118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Canani R.B., Di Costanzo M., Leone L., Pedata M., Meli R., Calignano A. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J. Gastroenterol. WJG. 2011;17:1519. doi: 10.3748/wjg.v17.i12.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Haub M.D., Hubach K.L., Al-Tamimi E.K., Ornelas S., Seib P.A. Different types of resistant starch elicit different glucose reponses in humans. J. Nutr. Metab. 2010;2010:230501. doi: 10.1155/2010/230501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Martínez I., Kim J., Duffy P.R., Schlegel V.L., Walter J. Resistant starches types 2 and 4 have differential effects on the composition of the fecal microbiota in human subjects. PLoS ONE. 2010;5:e15046. doi: 10.1371/journal.pone.0015046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Si X., Zhou Z., Strappe P., Blanchard C. A comparison of RS4-type resistant starch to RS2-type resistant starch in suppressing oxidative stress in high-fat-diet-induced obese rats. Food Funct. 2017;8:232–240. doi: 10.1039/C6FO01225F. [DOI] [PubMed] [Google Scholar]
- 81.Le Leu R.K., Brown I.L., Hu Y., Bird A.R., Jackson M., Esterman A., Young G.P. A synbiotic combination of resistant starch and Bifidobacterium lactis facilitates apoptotic deletion of carcinogen-damaged cells in rat colon. J. Nutr. 2005;135:996–1001. doi: 10.1093/jn/135.5.996. [DOI] [PubMed] [Google Scholar]
- 82.Tazoe H., Otomo Y., Kaji I., Tanaka R., Karaki S., Kuwahara A. Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J. Physiol. Pharmacol. 2008;59:251–262. [PubMed] [Google Scholar]
- 83.Fushimi T., Suruga K., Oshima Y., Fukiharu M., Tsukamoto Y., Goda T. Dietary acetic acid reduces serum cholesterol and triacylglycerols in rats fed a cholesterol-rich diet. Br. J. Nutr. 2006;95:916–924. doi: 10.1079/bjn20061740. [DOI] [PubMed] [Google Scholar]
- 84.Todesco T., Rao A.V., Bosello O., Jenkins D. Propionate lowers blood glucose and alters lipid metabolism in healthy subjects. Am. J. Clin. Nutr. 1991;54:860–865. doi: 10.1093/ajcn/54.5.860. [DOI] [PubMed] [Google Scholar]
- 85.Yamashita H., Fujisawa K., Ito E., Idei S., Kawaguchi N., Kimoto M., Hiemori M., Tsuji H. Improvement of obesity and glucose tolerance by acetate in Type 2 diabetic Otsuka Long-Evans Tokushima Fatty (OLETF) rats. Biosci. Biotechnol. Biochem. 2007;71:1236–1243. doi: 10.1271/bbb.60668. [DOI] [PubMed] [Google Scholar]
- 86.Birkeland E., Gharagozlian S., Valeur J., Aas A.-M. Short-chain fatty acids as a link between diet and cardiometabolic risk: A narrative review. Lipids Health Dis. 2023;22:40. doi: 10.1186/s12944-023-01803-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tan J., McKenzie C., Potamitis M., Thorburn A.N., Mackay C.R., Macia L. The role of short-chain fatty acids in health and disease. Adv. Immunol. 2014;121:91–119. doi: 10.1016/B978-0-12-800100-4.00003-9. [DOI] [PubMed] [Google Scholar]
- 88.Geirnaert A., Calatayud M., Grootaert C., Laukens D., Devriese S., Smagghe G., De Vos M., Boon N., Van de Wiele T. Butyrate-producing bacteria supplemented in vitro to Crohn’s disease patient microbiota increased butyrate production and enhanced intestinal epithelial barrier integrity. Sci. Rep. 2017;7:11450. doi: 10.1038/s41598-017-11734-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Li Q., Cao L., Tian Y., Zhang P., Ding C., Lu W., Jia C., Shao C., Liu W., Wang D. Butyrate suppresses the proliferation of colorectal cancer cells via targeting pyruvate kinase M2 and metabolic reprogramming. Mol. Cell. Proteom. 2018;17:1531–1545. doi: 10.1074/mcp.RA118.000752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zheng L., Kelly C.J., Battista K.D., Schaefer R., Lanis J.M., Alexeev E.E., Wang R.X., Onyiah J.C., Kominsky D.J., Colgan S.P. Microbial-derived butyrate promotes epithelial barrier function through IL-10 receptor–dependent repression of claudin-2. J. Immunol. 2017;199:2976–2984. doi: 10.4049/jimmunol.1700105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Birt D.F., Boylston T., Hendrich S., Jane J.-L., Hollis J., Li L., McClelland J., Moore S., Phillips G.J., Rowling M., et al. Resistant starch: Promise for improving human health. Adv. Nutr. 2013;4:587–601. doi: 10.3945/an.113.004325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Liu S., Reimer M., Ai Y. In vitro digestibility of different types of resistant starches under high-temperature cooking conditions. Food Hydrocoll. 2020;107:105927. [Google Scholar]
- 93.Gutiérrez T.J., Tovar J. Update of the concept of type 5 resistant starch (RS5): Self-assembled starch V-type complexes. Trends Food Sci. Technol. 2021;109:711–724. [Google Scholar]
- 94.Wang Z., Wang S., Xu Q., Kong Q., Li F., Lu L., Xu Y., Wei Y. Synthesis and functions of resistant starch. Adv. Nutr. 2023;14:1131–1144. doi: 10.1016/j.advnut.2023.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Englyst H.N., Kingman S., Cummings J. Classification and measurement of nutritionally important starch fractions. Eur. J. Clin. Nutr. 1992;46:S33–S50. [PubMed] [Google Scholar]
- 96.Flurkey K., Currer J.M., Harrison D.E. Chapter 20—Mouse Models in Aging Research. In: Fox J.G., Davisson M.T., Quimby F.W., Barthold S.W., Newcomer C.E., Smith A.L., editors. The Mouse in Biomedical Research. 2nd ed. Academic Press; Burlington, VT, USA: 2007. pp. 637–672. [Google Scholar]
- 97.Fox J., Barthold S.W., Davisson M.T., Newcomer C.E., Quimby F., Smith A.L. The Mouse in Biomedical Research. Elsevier; Amsterdam, The Netherlands: 2007. [Google Scholar]
- 98.Lackner C., Gogg-Kamerer M., Zatloukal K., Stumptner C., Brunt E.M., Denk H. Ballooned hepatocytes in steatohepatitis: The value of keratin immunohistochemistry for diagnosis. J. Hepatol. 2008;48:821–828. doi: 10.1016/j.jhep.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 99.Caldwell S., Ikura Y., Dias D., Isomoto K., Yabu A., Moskaluk C., Pramoonjago P., Simmons W., Scruggs H., Rosenbaum N., et al. Hepatocellular ballooning in NASH. J. Hepatol. 2010;53:719–723. doi: 10.1016/j.jhep.2010.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jouihan H. Measurement of liver triglyceride content. Bio-Protocol. 2012;2:e223 [Google Scholar]
- 101.Tomcik K., Ibarra R.A., Sadhukhan S., Han Y., Tochtrop G.P., Zhang G.F. Isotopomer enrichment assay for very short chain fatty acids and its metabolic applications. Anal. Biochem. 2011;410:110–117. doi: 10.1016/j.ab.2010.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Willis A.D. Rarefaction, Alpha Diversity, and Statistics. Front. Microbiol. 2019;10:2407. doi: 10.3389/fmicb.2019.02407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Smith D.L., Jr., Yang Y., Nagy T.R., Patki A., Vasselli J.R., Zhang Y., Dickinson S.L., Allison D.B. Weight Cycling Increases Longevity Compared with Sustained Obesity in Mice. Obesity. 2018;26:1733–1739. doi: 10.1002/oby.22290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rossi A.P., Rubele S., Calugi S., Caliari C., Pedelini F., Soave F., Chignola E., Vittoria Bazzani P., Mazzali G., Dalle Grave R. Weight cycling as a risk factor for low muscle mass and strength in a population of males and females with obesity. Obesity. 2019;27:1068–1075. doi: 10.1002/oby.22493. [DOI] [PubMed] [Google Scholar]
- 105.Zamarron B.F., Porsche C.E., Luan D., Lucas H.R., Mergian T.A., Martinez-Santibanez G., Cho K.W., DelProposto J.L., Geletka L.M., Muir L.A. Weight regain in formerly obese mice hastens development of hepatic steatosis due to impaired adipose tissue function. Obesity. 2020;28:1086–1097. doi: 10.1002/oby.22788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhang P. Influence of Foods and Nutrition on the Gut Microbiome and Implications for Intestinal Health. Int. J. Mol. Sci. 2022;23:9588. doi: 10.3390/ijms23179588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Leeming E.R., Johnson A.J., Spector T.D., Le Roy C.I. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients. 2019;11:862. doi: 10.3390/nu11122862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jensen M.D., Ryan D.H., Apovian C.M., Ard J.D., Comuzzie A.G., Donato K.A., Hu F.B., Hubbard V.S., Jakicic J.M., Kushner R.F. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102–S138. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Seo K., Cho H.-W., Chun J.L., So K.M., Kim K.H. Body Weight Development in Adult Dogs Fed a High Level Resistant Starch Diet. Animals. 2022;12:3440. doi: 10.3390/ani12233440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liang D., Zhang L., Chen H., Zhang H., Hu H., Dai X. Potato resistant starch inhibits diet-induced obesity by modifying the composition of intestinal microbiota and their metabolites in obese mice. Int. J. Biol. Macromol. 2021;180:458–469. doi: 10.1016/j.ijbiomac.2021.02.209. [DOI] [PubMed] [Google Scholar]
- 111.Fu J., Wang Y., Tan S., Wang J. Effects of Banana Resistant Starch on the Biochemical Indexes and Intestinal Flora of Obese Rats Induced by a High-Fat Diet and Their Correlation Analysis. Front. Bioeng. Biotechnol. 2021;9:575724. doi: 10.3389/fbioe.2021.575724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhou Y., Zhao S., Jiang Y., Wei Y., Zhou X. Regulatory function of buckwheat-resistant starch supplementation on lipid profile and gut microbiota in mice fed with a high-fat diet. J. Food Sci. 2019;84:2674–2681. doi: 10.1111/1750-3841.14747. [DOI] [PubMed] [Google Scholar]
- 113.Rosado C.P., Rosa V.H.C., Martins B.C., Soares A.C., Santos I.B., Monteiro E.B., Moura-Nunes N., da Costa C.A., Mulder A.d.R.P., Daleprane J.B. Resistant starch from green banana (Musa sp.) attenuates non-alcoholic fat liver accumulation and increases short-chain fatty acids production in high-fat diet-induced obesity in mice. Int. J. Biol. Macromol. 2020;145:1066–1072. doi: 10.1016/j.ijbiomac.2019.09.199. [DOI] [PubMed] [Google Scholar]
- 114.Wang B., Yu H., He Y., Wen L., Gu J., Wang X., Miao X., Qiu G., Wang H. Effect of soybean insoluble dietary fiber on prevention of obesity in high-fat diet fed mice via regulation of the gut microbiota. Food Funct. 2021;12:7923–7937. doi: 10.1039/D1FO00078K. [DOI] [PubMed] [Google Scholar]
- 115.CSIRO Understanding Resistant Starch and Its Role in Gut Health. [(accessed on 17 June 2024)]; Available online: https://www.csiro.au/en/research/health-medical/nutrition/resistant-starch.
- 116.Xu J., Ma Z., Li X., Liu L., Hu X. A more pronounced effect of type III resistant starch vs. type II resistant starch on ameliorating hyperlipidemia in high fat diet-fed mice is associated with its supramolecular structural characteristics. Food Funct. 2020;11:1982–1995. doi: 10.1039/C9FO02025J. [DOI] [PubMed] [Google Scholar]
- 117.Zhang L., Ouyang Y., Li H., Shen L., Ni Y., Fang Q., Wu G., Qian L., Xiao Y., Zhang J., et al. Metabolic phenotypes and the gut microbiota in response to dietary resistant starch type 2 in normal-weight subjects: A randomized crossover trial. Sci. Rep. 2019;9:4736. doi: 10.1038/s41598-018-38216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Peterson C.M., Beyl R.A., Marlatt K.L., Martin C.K., Aryana K.J., Marco M.L., Martin R.J., Keenan M.J., Ravussin E. Effect of 12 wk of resistant starch supplementation on cardiometabolic risk factors in adults with prediabetes: A randomized controlled trial. Am. J. Clin. Nutr. 2018;108:492–501. doi: 10.1093/ajcn/nqy121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wutzke K.D., Schmidek K.V. The effect of resistant starches on fat oxidation in healthy adults as measured by a 13CO2-breath test. Isot. Environ. Health Stud. 2017;53:553–562. doi: 10.1080/10256016.2017.1328418. [DOI] [PubMed] [Google Scholar]
- 120.Jiménez-Domínguez G., Ble-Castillo J.L., Aparicio-Trápala M.A., Juárez-Rojop I.E., Tovilla-Zárate C.A., Ble-Castillo D.J., García-Vázquez C., Olvera-Hernández V., Pérez-Pimienta B., Diaz-Zagoya J.C. Effects of acute ingestion of native banana starch on glycemic response evaluated by continuous glucose monitoring in obese and lean subjects. Int. J. Environ. Res. Public Health. 2015;12:7491–7505. doi: 10.3390/ijerph120707491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gargari B.P., Namazi N., Khalili M., Sarmadi B., Jafarabadi M.A., Dehghan P. Is there any place for resistant starch, as alimentary prebiotic, for patients with type 2 diabetes? Complement. Ther. Med. 2015;23:810–815. doi: 10.1016/j.ctim.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 122.Goldsmith F., Guice J., Page R., Welsh D.A., Taylor C.M., Blanchard E.E., Luo M., Raggio A.M., Stout R.W., Carvajal-Aldaz D., et al. Obese ZDF rats fermented resistant starch with effects on gut microbiota but no reduction in abdominal fat. Mol. Nutr. Food Res. 2017;61:1501025. doi: 10.1002/mnfr.201501025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bergeron N., Williams P.T., Lamendella R., Faghihnia N., Grube A., Li X., Wang Z., Knight R., Jansson J.K., Hazen S.L. Diets high in resistant starch increase plasma levels of trimethylamine-N-oxide, a gut microbiome metabolite associated with CVD risk. Br. J. Nutr. 2016;116:2020–2029. doi: 10.1017/S0007114516004165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ble-Castillo J.L., Aparicio-Trápala M.A., Francisco-Luria M.U., Córdova-Uscanga R., Rodríguez-Hernández A., Méndez J.D., Díaz-Zagoya J.C. Effects of native banana starch supplementation on body weight and insulin sensitivity in obese type 2 diabetics. Int. J. Environ. Res. Public Health. 2010;7:1953–1962. doi: 10.3390/ijerph7051953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bodinham C.L., Smith L., Wright J., Frost G.S., Robertson M.D. Dietary fibre improves first-phase insulin secretion in overweight individuals. PLoS ONE. 2012;7:e40834. doi: 10.1371/journal.pone.0040834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Robertson M.D., Bickerton A.S., Dennis A.L., Vidal H., Frayn K.N. Insulin-sensitizing effects of dietary resistant starch and effects on skeletal muscle and adipose tissue metabolism. Am. J. Clin. Nutr. 2005;82:559–567. doi: 10.1093/ajcn.82.3.559. [DOI] [PubMed] [Google Scholar]
- 127.Robertson M.D., Wright J.W., Loizon E., Debard C., Vidal H., Shojaee-Moradie F., Russell-Jones D., Umpleby A.M. Insulin-sensitizing effects on muscle and adipose tissue after dietary fiber intake in men and women with metabolic syndrome. J. Clin. Endocrinol. Metab. 2012;97:3326–3332. doi: 10.1210/jc.2012-1513. [DOI] [PubMed] [Google Scholar]
- 128.Karimi P., Farhangi M.A., Sarmadi B., Gargari B., Zare Javid A., Pouraghaei M., Dehghan P. The therapeutic potential of resistant starch in modulation of insulin resistance, endotoxemia, oxidative stress and antioxidant biomarkers in women with type 2 diabetes: A randomized controlled clinical trial. Ann. Nutr. Metab. 2016;68:85–93. doi: 10.1159/000441683. [DOI] [PubMed] [Google Scholar]
- 129.Bindels L.B., Segura Munoz R.R., Gomes-Neto J.C., Mutemberezi V., Martínez I., Salazar N., Cody E.A., Quintero-Villegas M.I., Kittana H., de Los Reyes-Gavilán C.G. Resistant starch can improve insulin sensitivity independently of the gut microbiota. Microbiome. 2017;5:1–16. doi: 10.1186/s40168-017-0230-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nichenametla S.N., Weidauer L.A., Wey H.E., Beare T.M., Specker B.L., Dey M. Resistant starch type 4-enriched diet lowered blood cholesterols and improved body composition in a double blind controlled cross-over intervention. Mol. Nutr. Food Res. 2014;58:1365–1369. doi: 10.1002/mnfr.201300829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Upadhyaya B., McCormack L., Fardin-Kia A.R., Juenemann R., Nichenametla S., Clapper J., Specker B., Dey M. Impact of dietary resistant starch type 4 on human gut microbiota and immunometabolic functions. Sci. Rep. 2016;6:28797. doi: 10.1038/srep28797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Deehan E.C., Yang C., Perez-Muñoz M.E., Nguyen N.K., Cheng C.C., Triador L., Zhang Z., Bakal J.A., Walter J. Precision Microbiome Modulation with Discrete Dietary Fiber Structures Directs Short-Chain Fatty Acid Production. Cell Host Microbe. 2020;27:389–404. doi: 10.1016/j.chom.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 133.Ding Y., Xiao Y., Ouyang Q., Luo F., Lin Q. Modulating the in vitro digestibility of chemically modified starch ingredient by a non-thermal processing technology of ultrasonic treatment. Ultrason. Sonochem. 2021;70:105350. doi: 10.1016/j.ultsonch.2020.105350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Toden S., Bird A.R., Topping D.L., Conlon M.A. Dose-dependent reduction of dietary protein-induced colonocyte DNA damage by resistant starch in rats correlates more highly with caecal butyrate than with other short chain fatty acids. Cancer Biol. Ther. 2007;6:253–258. doi: 10.4161/cbt.6.2.3627. [DOI] [PubMed] [Google Scholar]
- 135.Tachon S., Zhou J., Keenan M., Martin R., Marco M.L. The intestinal microbiota in aged mice is modulated by dietary resistant starch and correlated with improvements in host responses. FEMS Microbiol. Ecol. 2013;83:299–309. doi: 10.1111/j.1574-6941.2012.01475.x. [DOI] [PubMed] [Google Scholar]
- 136.Wang A., Liu M., Shang W., Liu J., Dai Z., Strappe P., Zhou Z. Attenuation of metabolic syndrome in the ob/ob mouse model by resistant starch intervention is dose dependent. Food Funct. 2019;10:7940–7951. doi: 10.1039/C9FO01771B. [DOI] [PubMed] [Google Scholar]
- 137.Mayo-Martínez L., Paz Lorenzo M., Martos-Moreno G.Á., Graell M., Barbas C., Rupérez F.J., Argente J., García A. Short-chain fatty acids in plasma and feces: An optimized and validated LC-QqQ-MS method applied to study anorexia nervosa. Microchem. J. 2024;200:110255. doi: 10.1016/j.microc.2024.110255. [DOI] [Google Scholar]
- 138.Higueras C., Rey A.I., Escudero R., Díaz-Regañón D., Rodríguez-Franco F., García-Sancho M., Agulla B., Sainz A. Short-Chain and Total Fatty Acid Profile of Faeces or Plasma as Predictors of Food-Responsive Enteropathy in Dogs: A Preliminary Study. Animals. 2022;12:89. doi: 10.3390/ani12010089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chen S.J., Chen C.C., Liao H.Y., Lin Y.T., Wu Y.W., Liou J.M., Wu M.S., Kuo C.H., Lin C.H. Association of Fecal and Plasma Levels of Short-Chain Fatty Acids With Gut Microbiota and Clinical Severity in Patients With Parkinson Disease. Neurology. 2022;98:e848–e858. doi: 10.1212/wnl.0000000000013225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ilyés T., Silaghi C.N., Crăciun A.M. Diet-Related Changes of Short-Chain Fatty Acids in Blood and Feces in Obesity and Metabolic Syndrome. Biology. 2022;11:1556. doi: 10.3390/biology11111556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Reuter M.A., Tucker M., Marfori Z., Shishani R., Bustamante J.M., Moreno R., Goodson M.L., Ehrlich A., Taha A.Y., Lein P.J., et al. Dietary resistant starch supplementation increases gut luminal deoxycholic acid abundance in mice. Gut Microbes. 2024;16:2315632. doi: 10.1080/19490976.2024.2315632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hald S., Schioldan A.G., Moore M.E., Dige A., Lærke H.N., Agnholt J., Bach Knudsen K.E., Hermansen K., Marco M.L., Gregersen S., et al. Effects of Arabinoxylan and Resistant Starch on Intestinal Microbiota and Short-Chain Fatty Acids in Subjects with Metabolic Syndrome: A Randomised Crossover Study. PLoS ONE. 2016;11:e0159223. doi: 10.1371/journal.pone.0159223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Metzler-Zebeli B.U., Canibe N., Montagne L., Freire J., Bosi P., Prates J.A.M., Tanghe S., Trevisi P. Resistant starch reduces large intestinal pH and promotes fecal lactobacilli and bifidobacteria in pigs. Animal. 2019;13:64–73. doi: 10.1017/s1751731118001003. [DOI] [PubMed] [Google Scholar]
- 144.Chen J., Chen X., Ho C.L. Recent Development of Probiotic Bifidobacteria for Treating Human Diseases. Front. Bioeng. Biotechnol. 2021;9:770248. doi: 10.3389/fbioe.2021.770248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Nakamura Y., Suzuki S., Murakami S., Nishimoto Y., Higashi K., Watarai N., Umetsu J., Ishii C., Ito Y., Mori Y., et al. Integrated gut microbiome and metabolome analyses identified fecal biomarkers for bowel movement regulation by Bifidobacterium longum BB536 supplementation: A RCT. Comput. Struct. Biotechnol. J. 2022;20:5847–5858. doi: 10.1016/j.csbj.2022.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sela D.A., Price N., Mills D.A. Metabolism of bifidobacteria. Bifidobact. Genom. Mol. Asp. 2010:45–70. [Google Scholar]
- 147.Bello-Medina P.C., Hernández-Quiroz F., Pérez-Morales M., González-Franco D.A., Cruz-Pauseno G., García-Mena J., Díaz-Cintra S., Pacheco-López G. Spatial Memory and Gut Microbiota Alterations Are Already Present in Early Adulthood in a Pre-clinical Transgenic Model of Alzheimer’s Disease. Front. Neurosci. 2021;15:595583. doi: 10.3389/fnins.2021.595583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sánchez B., Champomier-Vergès M.C., Collado Mdel C., Anglade P., Baraige F., Sanz Y., de los Reyes-Gavilán C.G., Margolles A., Zagorec M. Low-pH adaptation and the acid tolerance response of Bifidobacterium longum biotype longum. Appl. Environ. Microbiol. 2007;73:6450–6459. doi: 10.1128/aem.00886-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Krishnan S., Ding Y., Saedi N., Choi M., Sridharan G.V., Sherr D.H., Yarmush M.L., Alaniz R.C., Jayaraman A., Lee K. Gut microbiota-derived tryptophan metabolites modulate inflammatory response in hepatocytes and macrophages. Cell Rep. 2018;23:1099–1111. doi: 10.1016/j.celrep.2018.03.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Simrén M., Barbara G., Flint H.J., Spiegel B.M., Spiller R.C., Vanner S., Verdu E.F., Whorwell P.J., Zoetendal E.G. Intestinal microbiota in functional bowel disorders: A Rome foundation report. Gut. 2013;62:159–176. doi: 10.1136/gutjnl-2012-302167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cheng J., Laitila A., Ouwehand A.C. Bifidobacterium animalis subsp. lactis HN019 Effects on Gut Health: A Review. Front. Nutr. 2021;8:790561. doi: 10.3389/fnut.2021.790561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Metzler-Zebeli B.U., Schmitz-Esser S., Mann E., Grüll D., Molnar T., Zebeli Q. Adaptation of the cecal bacterial microbiome of growing pigs in response to resistant starch type 4. Appl. Environ. Microbiol. 2015;81:8489–8499. doi: 10.1128/AEM.02756-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lei Y., Tang L., Liu S., Hu S., Wu L., Liu Y., Yang M., Huang S., Tang X., Tang T., et al. Parabacteroides produces acetate to alleviate heparanase-exacerbated acute pancreatitis through reducing neutrophil infiltration. Microbiome. 2021;9:115. doi: 10.1186/s40168-021-01065-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ahmed S., Busetti A., Fotiadou P., Vincy Jose N., Reid S., Georgieva M., Brown S., Dunbar H., Beurket-Ascencio G., Delday M.I., et al. In vitro Characterization of Gut Microbiota-Derived Bacterial Strains with Neuroprotective Properties. Front. Cell. Neurosci. 2019;13:402. doi: 10.3389/fncel.2019.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kverka M., Zakostelska Z., Klimesova K., Sokol D., Hudcovic T., Hrncir T., Rossmann P., Mrazek J., Kopecny J., Verdu E. Oral administration of Parabacteroides distasonis antigens attenuates experimental murine colitis through modulation of immunity and microbiota composition. Clin. Exp. Immunol. 2011;163:250–259. doi: 10.1111/j.1365-2249.2010.04286.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Usta-Gorgun B., Yilmaz-Ersan L. Short-chain fatty acids production by Bifidobacterium species in the presence of salep. Electron. J. Biotechnol. 2020;47:29–35. doi: 10.1016/j.ejbt.2020.06.004. [DOI] [Google Scholar]
- 157.Pessione E. Lactic acid bacteria contribution to gut microbiota complexity: Lights and shadows. Front. Cell. Infect. Microbiol. 2012;2:86. doi: 10.3389/fcimb.2012.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Du X., Xiang Y., Lou F., Tu P., Zhang X., Hu X., Lyu W., Xiao Y. Microbial Community and Short-Chain Fatty Acid Mapping in the Intestinal Tract of Quail. Animal. 2020;10:1006. doi: 10.3390/ani10061006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cui Y., Zhang L., Wang X., Yi Y., Shan Y., Liu B., Zhou Y., Lü X. Roles of intestinal Parabacteroides in human health and diseases. FEMS Microbiol. Lett. 2022;369:fnac072. doi: 10.1093/femsle/fnac072. [DOI] [PubMed] [Google Scholar]
- 160.O’Callaghan A., van Sinderen D. Bifidobacteria and Their Role as Members of the Human Gut Microbiota. Front. Microbiol. 2016;7:925. doi: 10.3389/fmicb.2016.00925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Andoh A., Nishida A., Takahashi K., Inatomi O., Imaeda H., Bamba S., Kito K., Sugimoto M., Kobayashi T. Comparison of the gut microbial community between obese and lean peoples using 16S gene sequencing in a Japanese population. J. Clin. Biochem. Nutr. 2016;59:65–70. doi: 10.3164/jcbn.15-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ozato N., Saito S., Yamaguchi T., Katashima M., Tokuda I., Sawada K., Katsuragi Y., Kakuta M., Imoto S., Ihara K. Blautia genus associated with visceral fat accumulation in adults 20–76 years of age. NPJ Biofilms Microbiomes. 2019;5:28. doi: 10.1038/s41522-019-0101-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Osborne G., Wu F., Yang L., Kelly D., Hu J., Li H., Jasmine F., Kibriya M.G., Parvez F., Shaheen I. The association between gut microbiome and anthropometric measurements in Bangladesh. Gut Microbes. 2020;11:63–76. doi: 10.1080/19490976.2019.1614394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhao L., Zhang F., Ding X., Wu G., Lam Y.Y., Wang X., Fu H., Xue X., Lu C., Ma J., et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359:1151–1156. doi: 10.1126/science.aao5774. [DOI] [PubMed] [Google Scholar]
- 165.Luo S., He L., Zhang H., Li Z., Liu C., Chen T. Arabinoxylan from rice bran protects mice against high-fat diet-induced obesity and metabolic inflammation by modulating gut microbiota and short-chain fatty acids. Food Funct. 2022;13:7707–7719. doi: 10.1039/D2FO00569G. [DOI] [PubMed] [Google Scholar]
- 166.Zhang C., Yin A., Li H., Wang R., Wu G., Shen J., Zhang M., Wang L., Hou Y., Ouyang H., et al. Dietary Modulation of Gut Microbiota Contributes to Alleviation of Both Genetic and Simple Obesity in Children. EBioMedicine. 2015;2:968–984. doi: 10.1016/j.ebiom.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Cantu-Jungles T.M., Hamaker B.R. New View on Dietary Fiber Selection for Predictable Shifts in Gut Microbiota. mBio. 2020;11:e02179-19. doi: 10.1128/mbio.02179-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Cantu-Jungles T.M., Bulut N., Chambry E., Ruthes A., Iacomini M., Keshavarzian A., Johnson T.A., Hamaker B.R. Dietary Fiber Hierarchical Specificity: The Missing Link for Predictable and Strong Shifts in Gut Bacterial Communities. mBio. 2021;12:e0102821. doi: 10.1128/mBio.01028-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Cantu-Jungles T.M., Hamaker B.R. Tuning Expectations to Reality: Don’t Expect Increased Gut Microbiota Diversity with Dietary Fiber. J. Nutr. 2023;153:3156–3163. doi: 10.1016/j.tjnut.2023.09.001. [DOI] [PubMed] [Google Scholar]
- 170.Togo A.H., Diop A., Bittar F., Maraninchi M., Valero R., Armstrong N., Dubourg G., Labas N., Richez M., Delerce J., et al. Description of Mediterraneibacter massiliensis, gen. nov., sp. nov., a new genus isolated from the gut microbiota of an obese patient and reclassification of Ruminococcus faecis, Ruminococcus lactaris, Ruminococcus torques, Ruminococcus gnavus and Clostridium glycyrrhizinilyticum as Mediterraneibacter faecis comb. nov., Mediterraneibacter lactaris comb. nov., Mediterraneibacter torques comb. nov., Mediterraneibacter gnavus comb. nov. and Mediterraneibacter glycyrrhizinilyticus comb. nov. Antonie Van Leeuwenhoek. 2018;111:2107–2128. doi: 10.1007/s10482-018-1104-y. [DOI] [PubMed] [Google Scholar]
- 171.Behary J., Amorim N., Jiang X.-T., Raposo A., Gong L., McGovern E., Ibrahim R., Chu F., Stephens C., Jebeili H. Gut microbiota impact on the peripheral immune response in non-alcoholic fatty liver disease related hepatocellular carcinoma. Nat. Commun. 2021;12:187. doi: 10.1038/s41467-020-20422-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Crost E.H., Coletto E., Bell A., Juge N. Ruminococcus gnavus: Friend or foe for human health. FEMS Microbiol. Rev. 2023;47:fuad014. doi: 10.1093/femsre/fuad014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Torres-Maravilla E., Holowacz S., Delannoy J., Lenoir L., Jacouton E., Gervason S., Meynier M., Boucard A.-S., Carvalho F.A., Barbut F., et al. Serpin-positive Bifidobacterium breve CNCM I-5644 improves intestinal permeability in two models of irritable bowel syndrome. Sci. Rep. 2022;12:19776. doi: 10.1038/s41598-022-21746-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Pratt C., Campbell M.D. The Effect of Bifidobacterium on Reducing Symptomatic Abdominal Pain in Patients with Irritable Bowel Syndrome: A Systematic Review. Probiot. Antimicrob. Proteins. 2020;12:834–839. doi: 10.1007/s12602-019-09609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Guglielmetti S., Mora D., Gschwender M., Popp K. Randomised clinical trial: Bifidobacterium bifidum MIMBb75 significantly alleviates irritable bowel syndrome and improves quality of life—A double-blind, placebo-controlled study. Aliment. Pharmacol. Ther. 2011;33:1123–1132. doi: 10.1111/j.1365-2036.2011.04633.x. [DOI] [PubMed] [Google Scholar]
- 176.Ringel-Kulka T., Palsson O.S., Maier D., Carroll I., Galanko J.A., Leyer G., Ringel Y. Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: A double-blind study. J. Clin. Gastroenterol. 2011;45:518–525. doi: 10.1097/MCG.0b013e31820ca4d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Rajilić–Stojanović M., Biagi E., Heilig H.G., Kajander K., Kekkonen R.A., Tims S., de Vos W.M. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. 2011;141:1792–1801. doi: 10.1053/j.gastro.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 178.Gong H., Gao H., Ren Q., He J. The abundance of bifidobacterium in relation to visceral obesity and serum uric acid. Sci. Rep. 2022;12:13073. doi: 10.1038/s41598-022-17417-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Minami J., Iwabuchi N., Tanaka M., Yamauchi K., Xiao J.Z., Abe F., Sakane N. Effects of Bifidobacterium breve B-3 on body fat reductions in pre-obese adults: A randomized, double-blind, placebo-controlled trial. Biosci. Microbiota Food Health. 2018;37:67–75. doi: 10.12938/bmfh.18-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wu T.R., Lin C.S., Chang C.J., Lin T.L., Martel J., Ko Y.F., Ojcius D.M., Lu C.C., Young J.D., Lai H.C. Gut commensal Parabacteroides goldsteinii plays a predominant role in the anti-obesity effects of polysaccharides isolated from Hirsutella sinensis. Gut. 2019;68:248–262. doi: 10.1136/gutjnl-2017-315458. [DOI] [PubMed] [Google Scholar]
- 181.Chen J., Liu X., Zou Y., Gong J., Ge Z., Lin X., Zhang W., Huang H., Zhao J., Saw P.E., et al. A high-fat diet promotes cancer progression by inducing gut microbiota–mediated leucine production and PMN-MDSC differentiation. Proc. Natl. Acad. Sci. USA. 2024;121:e2306776121. doi: 10.1073/pnas.2306776121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Lin Y.-C., Lin H.-F., Wu C.-C., Chen C.-L., Ni Y.-H. Pathogenic effects of Desulfovibrio in the gut on fatty liver in diet-induced obese mice and children with obesity. J. Gastroenterol. 2022;57:913–925. doi: 10.1007/s00535-022-01909-0. [DOI] [PubMed] [Google Scholar]
- 183.Xie R., Gu Y., Li M., Li L., Yang Y., Sun Y., Zhou B., Liu T., Wang S., Liu W., et al. Desulfovibrio vulgaris interacts with novel gut epithelial immune receptor LRRC19 and exacerbates colitis. Microbiome. 2024;12:4. doi: 10.1186/s40168-023-01722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kushkevych I., Castro Sangrador J., Dordević D., Rozehnalová M., Černý M., Fafula R., Vítězová M., Rittmann S.K.R. Evaluation of Physiological Parameters of Intestinal Sulfate-Reducing Bacteria Isolated from Patients Suffering from IBD and Healthy People. J. Clin. Med. 2020;9:1920. doi: 10.3390/jcm9061920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Su L., Hong Z., Zhou T., Jian Y., Xu M., Zhang X., Zhu X., Wang J. Health improvements of type 2 diabetic patients through diet and diet plus fecal microbiota transplantation. Sci. Rep. 2022;12:1152. doi: 10.1038/s41598-022-05127-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Schipper L., Harvey L., van der Beek E.M., van Dijk G. Home alone: A systematic review and meta-analysis on the effects of individual housing on body weight, food intake and visceral fat mass in rodents. Obes. Rev. 2018;19:614–637. doi: 10.1111/obr.12663. [DOI] [PubMed] [Google Scholar]
- 187.Schipper L., van Heijningen S., Karapetsas G., van der Beek E.M., van Dijk G. Individual housing of male C57BL/6J mice after weaning impairs growth and predisposes for obesity. PLoS ONE. 2020;15:e0225488. doi: 10.1371/journal.pone.0225488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chourbaji S., Zacher C., Sanchis-Segura C., Spanagel R., Gass P. Social and structural housing conditions influence the development of a depressive-like phenotype in the learned helplessness paradigm in male mice. Behav. Brain Res. 2005;164:100–106. doi: 10.1016/j.bbr.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 189.Kalliokoski O., Teilmann A.C., Jacobsen K.R., Abelson K.S., Hau J. The lonely mouse—Single housing affects serotonergic signaling integrity measured by 8-OH-DPAT-induced hypothermia in male mice. PLoS ONE. 2014;9:e111065. doi: 10.1371/journal.pone.0111065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Macedo G.C., Morita G.M., Domingues L.P., Favoretto C.A., Suchecki D., Quadros I.M.H. Consequences of continuous social defeat stress on anxiety- and depressive-like behaviors and ethanol reward in mice. Horm. Behav. 2018;97:154–161. doi: 10.1016/j.yhbeh.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 191.Downes J., Dewhirst F.E., Tanner A.C., Wade W.G. Description of Alloprevotella rava gen. nov., sp. nov., isolated from the human oral cavity, and reclassification of Prevotella tannerae Moore et al. 1994 as Alloprevotella tannerae gen. nov., comb. nov. Int. J. Syst. Evol. Microbiol. 2013;63:1214–1218. doi: 10.1099/ijs.0.041376-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ndongo S., Lagier J.C., Fournier P.E., Raoult D., Khelaifia S. “Prevotellamassilia timonensis,” a new bacterial species isolated from the human gut. New Microbes New Infect. 2016;13:102–103. doi: 10.1016/j.nmni.2016.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article or upon reasonable request.