Abstract
The use of classical smallpox vaccines based on vaccinia virus (VV) is associated with severe complications in both naïve and immune individuals. Modified vaccinia virus Ankara (MVA), a highly attenuated replication-deficient strain of VV, has been proven to be safe in humans and immunocompromised animals, and its efficacy against smallpox is currently being addressed. Here we directly compare the efficacies of MVA alone and in combination with classical VV-based vaccines in a cynomolgus macaque monkeypox model. The MVA-based smallpox vaccine protected macaques against a lethal respiratory challenge with monkeypox virus and is therefore an important candidate for the protection of humans against smallpox.
Following a worldwide vaccination program, the World Health Organization declared smallpox to be eradicated in May 1980. Soon thereafter, general vaccination against smallpox was discontinued (3). Variola virus, the etiological agent of smallpox, is now ranked high on the list of biological agents that may be used as a bioweapon (9) because infection with this virus results in approximately 30% mortality and, to date, the vast majority of the population lacks protective immunity. In addition, there are growing concerns regarding the observation that other mammalian poxviruses, such as cowpox virus and monkeypox virus (MPXV), may now cross the species barrier to humans more easily (13). While traditional (first-generation) smallpox vaccines based on replicating vaccinia viruses (VV) are efficacious and were the basis for the eradication of smallpox, they are associated with rare but severe side effects, particularly in immunocompromised individuals (1, 2, 14). Indeed, the recent vaccination of U.S. soldiers against smallpox infection was not only a timely reminder of the adverse reactions associated with traditional smallpox vaccines but also showed another complication—myopericarditis—in healthy young males following vaccination (8). Moreover, the fact that it has been estimated that at least 25% of the U.S. population should not receive traditional smallpox vaccines in the absence of a direct threat highlights the growing need for a safe, new generation of smallpox vaccine that is suitable even for immunocompromised individuals (10). One such candidate vaccine is based on modified vaccinia virus Ankara (MVA), which has been attenuated from a VV by being passaged >500 times in chicken embryo fibroblast cells. This resulted in a virus which is replication deficient in most mammalian cell lines (4, 15). MVA has been used as a prevaccine in a two-step vaccination program against smallpox and was shown to be safe for >120,000 primary vaccinees (15, 19). Various MVA strains have also been shown to be safe for a variety of immunodeficient animals (7, 20), and more recently, MVA was shown to be immunogenic and efficacious in both mice and nonhuman primates (5, 23). Efficacy testing of candidate vaccines such as MVA in experimental animals, in comparison with traditional smallpox vaccines, will form an essential part of the data required to register new candidate smallpox vaccines. To this end, animal models that mimic the natural infection of variola virus in humans are particularly important. While a previous study indicated the efficacy of an MVA-based vaccine in a cynomolgus macaque (Macaca fascicularis) model (5), this relied on an intravenous (i.v.) lethal challenge with MPXV, and as such, did not examine the ability of the vaccine to afford protection against a respiratory challenge, which is the most prevalent natural route of infection. Therefore, we have performed vaccination experiments with cynomolgus macaques with different combinations of candidate and traditional vaccines, followed by MPXV challenge via the tracheal route. A sublethal and a lethal challenge dose of MPXV were chosen to meet the regulatory requirements for registration (18). The MVA strain included in this study (MVA-BN, or IMVAMUNE) is currently being tested in >300 human subjects in on-going phase I and II clinical studies, including individuals for whom vaccination with traditional smallpox vaccines is traditionally contraindicated. For the present study, the immune response and efficacy of MVA-BN vaccination were compared to those of a primary vaccination with MVA-BN followed by vaccination with a first-generation smallpox vaccine produced on calf skins (Elstree-RIVM). For this purpose, a low dose of MVA was chosen to prime the immune system, thus reducing the side effects of vaccination with a traditional vaccine shortly thereafter without changing the take rate of the traditional vaccine (15). In addition, vaccination protocols with Elstree-RIVM alone and vaccination with a second-generation vaccine (Elstree-BN) (15, 19) were evaluated. Elstree-BN is based on the same vaccinia virus strain as Elstree-RIVM, but the former was passaged and produced on chicken embryo fibroblasts to further attenuate the virus and to make a better defined vaccine preparation that does not depend on the use of calves. The MVA-BN doses for priming and vaccination as well as the subcutaneous (s.c.) administration of MVA-BN were chosen on the basis of historical data, previous animal studies, and preliminary data from 300 human volunteers (15, 19).
MATERIALS AND METHODS
Vaccines, animals, vaccinations, and samplings.
The classical smallpox vaccine (lot no. SP003; produced in July 2002), referred to as Elstree-RIVM, was produced by The National Institute for Public Health and the Environment (Bilthoven, The Netherlands). Elstree-RIVM was reconstituted as recommended by the manufacturer to give a final concentration of 108 50% tissue culture infective doses (TCID50)/ml. A bifurcated needle was used to deliver the human equivalent dose of 2.5 × 105 TCID50.
MVA-BN and Elstree-BN were produced at Impstoffwerk Dessau-Tornau GmbH (Germany) and provided as freeze-dried cGMP material. MVA-BN was reconstituted in water to a final concentration of 2 × 108 PFU/ml. Elstree-BN was reconstituted as recommended for the Dryvax smallpox vaccine (Wyeth Laboratories, Inc.) to give a final concentration of 108 TCID50/ml. A bifurcated needle was used to deliver the human equivalent dose of 2.5 × 105 TCID50. Viruses were grown on specific-pathogen-free chicken embryo fibroblast cells (Charles River Laboratories, Sulzfeld, Germany). Following incubation for 1 to 2 days, the virus-cell suspension was harvested by one round of freeze-thawing and then concentrated by centrifugation. The pellet was resuspended and subjected to several rounds of ultrasonic homogenization. Elstree-BN was purified by ultrafiltration and MVA-BN was purified by sedimentation through a sucrose gradient as previously described (22).
The studies were performed with 35 captive-bred subadult healthy cynomolgus macaques (Macaca fascicularis) in accordance with the institutional guidelines for care and use of laboratory animals. We vaccinated four groups of six monkeys each (Fig. 1): the first group was vaccinated twice subcutaneously (s.c.) with a high dose of 108 TCID50 MVA-BN at an interval of 4 weeks, the second group was vaccinated s.c. with a low dose of 2 × 106 TCID50 MVA-BN followed 10 days later by an intracutaneous (i.c.) vaccination with Elstree-RIVM, the third group was vaccinated with one i.c. standard dose of Elstree-RIVM, and the fourth group was vaccinated i.c. with one standard dose of Elstree-BN. Group V was sham vaccinated. EDTA-blood samples for plasma and the isolation of peripheral blood mononuclear cells (PBMC) were processed as described previously (21).
FIG. 1.
Experimental design. Each group consisted of six adult cynomolgus macaques (Macaca fascicularis). For group I animals, MVA-BN (108 PFU) was administered by s.c. injection on days −28 and 0; for group II animals, an MVA-BN primer dose (2 × 106 PFU) was administered by s.c. injection on day −10 and Elstree-RIVM was administered i.c. with a bifurcated needle on day 0; for group III animals, Elstree-RIVM was administered i.c. with a bifurcated needle on day 0; for group IV, Elstree-BN was administered i.c. with a bifurcated needle on day 0; and group V consisted of nonvaccinated animals. Fifteen weeks after the (last) vaccination, all animals were challenged i.t. with MPXV strain MSF#6 in the trachea by intubation.
VV-specific ELISA.
Total immunoglobulin G (IgG) plasma antibody responses to VV were measured by using an enzyme-linked immunosorbent assay (ELISA). MaxiSorp 96-well plates (Nunc, Wiesbaden, Germany) were coated overnight at 4°C with a polyclonal rabbit anti-VV antibody (Quartett Immunodiagnostika, Berlin, Germany), blocked with phosphate-buffered saline-5% fetal calf serum (PAA Laboratories, Linz, Austria) for 30 min at room temperature, and incubated with crude MVA antigen (3 μg/well) for 1 h at room temperature. Subsequently, twofold serially diluted, heat-inactivated plasma samples (starting at 1:100) were added for 1 h at room temperature, followed by a horseradish peroxidase-labeled rabbit anti-monkey antibody (Sigma-Aldrich GmbH, Seelze, Germany). After each incubation, the plates were washed and developed according to established procedures (21). The optical density was read at 492 nm, with a reference of 405 nm. The antibody titers were calculated by linear regression and defined as the plasma dilutions that resulted in an optical density of 0.3.
Plaque reduction assay.
Neutralizing anti-vaccinia virus antibody titers were measured with a plaque reduction assay. Heat-inactivated plasmas were serially diluted and incubated with 100 PFU of wild type IHD-J VV for 2 h at 37°C in 5% CO2. Subsequently, the plasma dilutions were transferred to 24-well plates preseeded with 1.5 × 105 Vero cells per well, and the plates were incubated for 24 to 30 h at 37°C with 5% CO2. Plaques were stained with a crystal violet solution, and the neutralizing titers were determined as the plasma dilutions resulting in a 50% reduction of the total amount of plaques.
ELISPOT assays.
The frequency of specific gamma interferon (IFN-γ)-secreting PBMC was determined by the use of an enzyme-linked immunospot (ELISPOT) kit (U-Cytech, Utrecht, The Netherlands) according to the manufacturer's recommendations. In brief, 3 × 105 viable PBMC were transferred to wells of ELISPOT plates coated with an IFN-γ-specific monoclonal antibody. Subsequently, purified MVA was added to the cells at a multiplicity of infection of 5 or medium was added as a control. After 16 h of incubation at 37°C, ELISPOT plates were developed and spots were enumerated with an automatic spot reader (Bioreader 3000; Bio-Sys GmbH, Germany).
Lymphoproliferation assay.
Specific lymphoproliferation was determined with a bromodeoxyuridine (BrdU) flow kit (BD Biosciences, San Diego, Calif.) according to the manufacturer's recommendations. In brief, 2 × 105 viable PBMC were cultured for 5 days at 37°C in the absence or presence of purified MVA at a multiplicity of infection of 5. During the last 16 h of this incubation period, BrdU was added. Subsequently, the cells were harvested and stained with peridinin-chlorophyll-protein-labeled CD3-specific monoclonal (clone SP34-2; BD Biosciences) and fluorescein isothiocyanate-labeled anti-BrdU antibodies. The percentages of CD3+ BrdU+ cells were then measured by flow cytometry. The results are expressed as a stimulation index (SI), which was calculated as the ratio of the percentage of CD3+ BrdU+ cells obtained in the presence of MVA to the percentage of CD3+ BrdU+ cells obtained in the absence of MVA, with an SI of >2 considered a positive response.
Monkeypox virus, challenge infection, and samplings.
Monkeypox virus strain MSF#6, which was obtained from a fatally infected human in Congo, was kindly provided by Herman Meyer (16). The virus was passaged two times in MA104 cells and two times in Vero cells. The challenge virus stock had a titer of 2 × 108 PFU per ml in Vero cell monolayers.
Fifteen weeks after the last vaccination, the monkeys were inoculated intratracheally with either 106 or 107 PFU of monkeypox virus in 5 ml of phosphate-buffered saline. Throat swabs and EDTA-blood samples were collected on days 0, 4, 6, 8, 11, 14, 21, and 28 after the challenge.
Gross pathology, histology, and ultrastructural examination.
Gross pathology was performed on all control animals and on one MVA-BN-vaccinated animal that showed skin lesions. Samples of the lungs, liver, kidneys, trachea, tongue, skin, spleen, and mandibular and tracheobronchial lymph nodes were collected in 10% neutral-buffered formalin for histologic examination, in transport medium for virus isolation, and in lysis buffer (6 M guanidine-HCl, 20% Triton X-100 [vol/vol], pH 4.4, at 25°C) for virus detection by PCR. After fixation in formalin and embedment in paraffin, 5-μm-thick, hematoxylin-and-eosin-stained sections were prepared by routine methods and examined by light microscopy. Selected lung and skin samples were also examined by transmission electron microscopy as described previously (11).
Monkeypox virus isolation.
Following the MPXV challenge, the viral loads were monitored in throat swabs. Samples were freeze-thawed three times and sonicated in a cup sonicator. Two dilutions (1:10 and 1:100) in transport medium supplemented with 1% fetal bovine serum were used to inoculate Vero cell monolayers in six-well plates (Greiner). After 1 h of incubation at 37°C, the inocula were removed and replaced with culture medium supplemented with 1% fetal bovine serum. The monolayers were cultured for 5 days at 37°C and stained with a crystal violet solution.
Virus detection by quantitative PCR.
DNAs were isolated by use of a MagnaPure LC isolation station (Roche Applied Science, Penzberg, Germany). A fixed amount of internal PhHV-1 virus was added to each sample to monitor for a loss of sample or inhibition, as described before (17). During the isolation procedure, a 10-fold dilution series of monkeypox virus strain MSF#6 in lysis buffer, starting from 2 × 108 PFU/ml and going down to 20 PFU/ml, was included. Monkeypox virus DNA was detected with a LightCycler instrument (Roche Applied Science) as described previously (6). For improved sensitivity, detection was performed with SYBR green.
Statistical analysis.
Antibody titers were compared by using the Student t test. Viral loads were compared by multiple linear regression analysis with the area under the concentration-time curve (AUC) as a dependent variable and the challenge doses, vaccination regimens, and their interaction terms as independent variables. Differences were considered significant at P values of <0.05.
RESULTS
Local effects at the site of vaccination.
As expected, s.c. vaccination with MVA-BN (group I) did not result in a “vaccine take” (pustule, scab, and scar) (Fig. 2a). The vaccine takes following i.c. vaccination with Elstree-RIVM (group III) were more pronounced in size than those following i.c. vaccination with Elstree-BN (group IV) (P = 0.08). Prevaccination with a low dose of MVA-BN (group II) resulted in reduced vaccine takes upon subsequent intracutaneous vaccination with Elstree-RIVM (P = 0.05), suggesting that it had indeed induced an immune response that interfered with the replication of VV. This phenomenon has been observed in other animal experiments, albeit with the use of higher doses of MVA (108 PFU) and a longer interval between the vaccinations (5). One animal from group III died 10 weeks after vaccination from a cause that was not related to the experiment.
FIG. 2.
Reactivities and immunogenicities of different smallpox vaccines. (a) Sizes (areas) of vaccine-induced pocks measured on day 7 at the site of s.c. inoculation of MVA (groups I and II) or i.c. inoculation of Estree-RIVM (groups II and III) or Elstree-BN (group IV). (b, left side) Induction of MVA-specific IFN-γ-secreting cells, as measured by an ELISPOT assay. PBMC were isolated before vaccination, 4 and 9 weeks after the (last) vaccination, and at the moment of challenge (week 15). The data are expressed as the average numbers of specific IFN-γ-secreting cells in 300,000 PBMC per group ± SD. (b, right side) Induction of MVA-specific lymphoproliferation, as determined by fluorescence-activated cell sorting after a BrdU incorporation assay. PBMC were isolated before vaccination and 3 weeks after the (last) vaccination. The data are expressed as the average SI per group ± SD. (c) Development of specific plasma IgG responses in samples collected on different days after vaccination, as measured by ELISA. The data are expressed as average titers per group ± SD. (d) Vaccinia virus-specific neutralizing plasma antibody titers in samples collected on different days after vaccination, as measured by a plaque reduction assay. The moments of vaccination are indicated with the respective symbols. The data are expressed as average 50% plaque reduction titers (PRNT) per group ± SD.
Vaccine-induced cell-mediated immune responses.
Specific T-cell responses in PBMC were measured with an ELISPOT assay detecting IFN-γ-secreting cells and a BrdU incorporation assay measuring lymphoproliferation. For all four groups, specific IFN-γ-secreting T cells were detected 4 weeks after the last vaccination, with considerable variation within each group (Fig. 2b, left side). Five weeks later, the frequencies of these cells were considerably lower, and at 15 weeks, they were virtually undetectable. Similarly, at week 3 after the last vaccination, specific lymphoproliferation responses were induced in all four groups, with considerable variation within each group (Fig. 2b, right side). For both assays, differences between the groups were not significant.
Vaccine-induced humoral immune responses.
Sera from the animals were tested with an MVA-specific ELISA measuring VV-specific IgG (Fig. 2c) and with a plaque reduction neutralization assay (Fig. 2d). The kinetics of the antibody responses measured by ELISA and the plaque reduction neutralization assay were largely similar within the respective groups. The monkeys vaccinated with two high MVA-BN doses (group I) showed a rapid increase in IgG antibodies until week 2 after the first vaccination. A clear boost was seen after the second vaccination. For four of the six animals, low neutralizing antibody titers were also detected after the first vaccination. One week after the second vaccination, all of the animals had developed high neutralizing antibody titers. The monkeys in group II all developed IgG antibodies within 2 weeks of the low-dose MVA-BN vaccination, which increased until the vaccination with Elstree-RIVM. The latter resulted in a clear boost of IgG antibodies. No neutralizing antibodies were detected in these animals after the first vaccination, but high titers were found in all animals within 1 week after the second vaccination, highlighting the immunological priming of the low-dose vaccination. The monkeys vaccinated once with either Elstree-RIVM or Elstree-BN (groups III and IV, respectively) all developed high IgG titers within 2 weeks, reaching peak levels at 3 weeks. Neutralizing antibodies also developed within 2 weeks in all of these animals, reaching peak levels at 4 weeks. For all of the groups, IgG antibody levels gradually declined, with no statistically significant differences between the groups on the day of challenge. for groups II, III, and IV, the neutralizing antibodies reached a plateau between 4 and 9 weeks after the last vaccination. For group I, which had developed the strongest peak responses, neutralizing antibodies gradually declined until the day of challenge. At that time, the highest neutralizing antibody titers were found among the animals of group III and the lowest titers were found with group I, with statistically significant differences between groups I and III (P < 0.001) and between groups I and IV (P = 0.004).
Protection from intratracheal MPXV challenge infection.
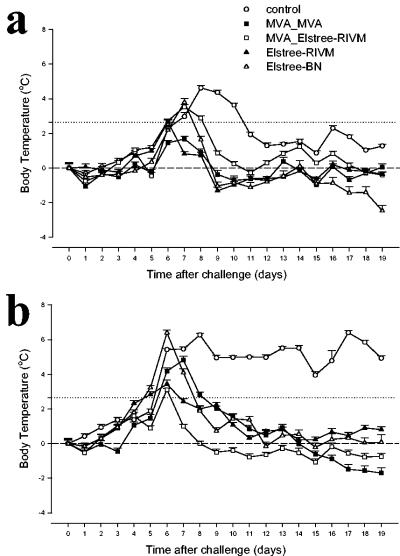
Fifteen weeks after the last vaccination, all of the animals were challenged intratracheally (i.t.) with either 106 PFU (three animals per group) or 107 PFU (three animals per group) of MPXV, which were chosen as sublethal and lethal challenges, respectively. Control animals challenged with 106 PFU of MPXV showed elevated body temperatures (>2%) from days 6 to 11, with a second peak around day 16 (Fig. 3a). On day 11, 20 to 40 characteristic pocks appeared on all three animals. On day 14, the number of pocks increased to >100, and from days 19 to 21, the animals were clearly lethargic. The pocks were virtually resolved on day 28. One of these animals was euthanized on day 19 to serve as a control for histopathological comparisons. The lungs of this animal and those of the two other animals in the same group, which were euthanized at the end of the follow-up period, showed mild pulmonary lesions consistent with a MPXV infection. These comprised a few small foci of necrosis surrounded by inflammatory cells mixed with fibroblasts and a few collagen fibers. Pathological changes in other tissues from these animals included tracheitis, glossitis, and reactive lymph nodes.
FIG. 3.
Body temperature profiles after respiratory inoculation with 106 (a) or 107 (b) PFU of MPXV strain MSF#6. The macaques were not vaccinated or had been vaccinated with two doses of MVA-BN, one low dose of MVA-BN followed by Elstree-RIVM, Elstree-RIVM alone, or Elstree-BN. Each macaque had an active temperature transponder in its peritoneal cavity. The animals exhibited differences in their baseline temperatures (37.7 ± 0.9°C) and slight shifts in their day-night temperature cycles. Therefore, the data are expressed as percentages of the average temperature change per day per group with (upper limit) 95% confidence intervals. The dotted line denotes a 1°C temperature increase above the average baseline.
Control animals challenged with 107 PFU of MPXV showed an episode of elevated body temperature (>1°C; ∼2.65%) from day 5 onwards until death (days 15 to 19) (Fig. 3b). On days 8 to 10, pocks, which were more pronounced than those on control animals challenged with 106 PFU of MPXV, appeared on all three animals. At this stage, all three animals showed anorexia and dyspnea. Three days later, two of the animals had >100 pocks, and one of these two had conjunctivitis and nasal discharge. The other animal had approximately 50 pocks at this time point. On day 14, the pocks could be classified as typical pustules, the clinical signs became more severe, and the animals were lethargic. One animal died on day 15, while the other two animals deteriorated and were euthanized on day 19 for ethical reasons. Upon histopathological examination, the lungs of these three animals showed severe macroscopic lesions which were histologically characterized by fibrinonecrotic bronchopneumonia (Fig. 4b), as has been described previously for animals dying from MPXV infection (24). Transmission electron microscopy performed on the lungs of the animal that died on day 15 revealed the abundant presence of poxvirus particles in the alveolar wall (Fig. 4d). This animal and the two other animals from the same group, which were euthanized on day 19, showed typical cutaneous lesions (24) characterized by acanthosis, necrosis, and intracytoplasmic amphophilic inclusion bodies (Fig. 4a); these were seen to contain poxvirus particles upon electron microscopy (Fig. 4c). Changes in other tissues in these animals included tracheitis, necrotizing glossitis, lymphadenitis, and splenitis with lymphoid depletion.
FIG. 4.
Histological lesions and ultrastructural detection of MPXV in lung and skin of a nonvaccinated macaque. (a) Edge of typical cutaneous lesion characterized by epidermal hyperplasia, orthokeratotic hyperkeratosis, ballooning degeneration of keratinocytes (arrowhead) with necrosis, and infiltration by inflammatory cells towards the center (arrow). (b) Necrosis of pulmonary alveolar wall, indicated with arrowheads, and flooding of alveolar lumen with fibrin, edema fluid, foamy macrophages, degenerative neutrophils, and necrotic cellular debris. (c) Mature (arrowhead) and immature poxvirus particles in keratinocyte. Bar, 5,000 nm. (d) Poxvirus particles in necrotic alveolar wall. Bar, 5,000 nm. (Inset) Higher magnification of mature poxvirus particle with characteristic dumbbell structure of the core (left) and immature poxvirus particle (right). Sections were stained with hematoxylin and eosin (a and b) or with uranyl acetate and lead citrate (c and d). Original magnification, ×10 (a) or ×40 (b).
All vaccinated animals that were challenged with 106 or 107 PFU of MPXV showed an episode of elevated body temperature (>1°C; ∼2.65%) that occurred between days 5 and 8 postchallenge which returned to normal by day 12 (Fig. 3a and b).
Viral loads in the plasma were measured by MPXV-specific real-time PCR, and viral loads in throat swabs were measured by MPXV-specific real-time PCR and quantitative virus isolation. The latter was done to estimate the risk for virus spread. Although sampling by throat swabbing may be subject to sampling error, the data provided in Fig. 5 show that the standard deviations (SD) between animals were low and that the kinetics closely followed those of the data obtained by analyzing viral loads in plasma. The throat swab viral load kinetics measured with the two assays were largely similar for the same animals (Fig. 5a to c). For the control animals challenged with 106 PFU of MPXV, the viral loads in plasma increased rapidly, reaching peak levels on days 11 to 14. All of the animals were virtually aviremic between days 14 and 28. For the control animals challenged with 107 PFU of MPXV, the viral loads in plasma reached higher peak levels on days 11 to 15 and remained elevated until death. The viral load kinetics of the vaccinated animals peaked between days 6 and 8 and decreased gradually thereafter, becoming aviremic between days 14 and 28 (Fig. 5a to c). While there was no significant difference in the mean peak viral loads among all vaccinated groups, the total viral burden, as measured by an analysis of the area under the curve (AUC), revealed a trend suggesting differences between the different groups (Fig. 5d). Vaccination reduced viral loads significantly compared to the loads in the respective controls. The strongest reductions in viral loads were observed for animals vaccinated with a low dose of MVA followed by Elstree-RIVM (group II) or for those vaccinated with Elstree-RIVM alone (group III).
FIG. 5.
Monkeypox viral loads in plasmas and throat swabs from vaccinated and control animals at different time points after respiratory inoculation with 106 PFU (left graphs) or 107 PFU of MPXV (right graphs). The data are expressed as average log10 values per group plus SD. (a) Viral loads in throat swabs, as measured by real-time quantitative PCR; (b) plasma viremia, as measured by real-time quantitative PCR; (c) viral loads in throat swabs, as measured by quantitative virus isolation in Vero cell monolayers. †, natural death; X, euthanasia. (d) AUCs of the viral loads in plasmas and throat swabs from vaccinated and control animals over a 28-day follow-up after respiratory inoculation with 106 PFU (left graph) or 107 PFU of MPXV (right graph). The data are expressed as average log10 values per group plus SD.
Only one vaccinated animal developed pocks upon MPXV challenge, while all others showed no clinical signs of the disease apart from an elevated body temperature. This animal, which was vaccinated with MVA-BN (group I), initially developed pocks (>70) on day 11 after the challenge with 107 PFU of MPXV, but these were reduced in number and less progressive than those in the naïve control animals and had completely resolved by day 28. This animal was euthanized on day 28, and its tissues were collected for histopathological examination. Multifocally, in the lungs of this animal, the alveolar septa, alveolar lumina, and peribronchiolar and perivascular interstitium contained moderate numbers of macrophages and fewer lymphocytes and fibroblasts mixed with collagen fibers. The lung parenchyma contained one small focus of necrosis surrounded by abundant macrophages, fibroblasts, and lymphocytes. Although this animal had a significantly higher viral load in the plasma than those of the other vaccinated animals, there were no other parameters (humoral immune response or body temperature) that could correlate with the observation of pocks following challenge. While no T cells specific to VV could be detected in this animal, this observation is unlikely to correlate with a higher level of viremia given that the other animals vaccinated with MVA-BN or traditional smallpox vaccines also had very low or absent detectable T-cell responses.
DISCUSSION
Collectively, our data show that all of the vaccination regimens used in this study induced specific T-cell and antibody responses as well as protection against lethal and sublethal MPXV challenges via the respiratory route. Differences in protective efficacies, as measured by the absence of pocks in all but one vaccinated animal, the kinetics of body temperatures, and viral loads, were observed between the groups, although none of them reached statistical significance. However, the efficacy of each of the vaccination regimens was impressive given the massive challenge doses used. It may be expected that human challenge doses with variola virus under natural conditions and even during a bioterrorist attack would be significantly lower.
A comparison of the outcome of the lethal i.t. MPXV challenge with that of a lethal i.v. challenge in the same monkey species in an earlier study (5) shows some striking differences: the peak of the viremia was seen about 5 days later and after vaccination was reduced rather than shortened in the i.v. challenge model compared to the i.t. challenge model. Although the MPXV strains used in both studies were not the same, it may still be argued that MPXV, like variola virus, has evolved primarily as a respiratory pathogen which replicates massively in the lungs, resulting in higher viral loads than those seen after direct i.v. infection. These expectations should be substantiated in further studies.
There are numerous severe side effects associated with traditional smallpox vaccines that are mainly associated with the fact that all traditional vaccines are based on a replicating VV. In addition, a frequent serious side effect of traditional smallpox vaccines is the accidental infection of others by the resultant infectious pustule, or vaccine take following vaccination, which was the leading cause of eczema vaccinatum during the eradication campaign (12). While there are encouraging data from both immunocompromised people and animals showing that a nonreplicating vaccine based on MVA, such as MVA-BN, could overcome these safety concerns of traditional smallpox vaccines, there have been doubts about whether such a nonreplicating vaccine would be efficacious. The results of this study are therefore a substantial development in demonstrating the efficacy of MVA-BN, a smallpox vaccine candidate that may have significant safety advantages compared to traditional vaccines, particularly for the 25% of the population for whom traditional smallpox vaccines are currently contraindicated (10). Although the efficacy and safety of a MVA vaccine have recently been studied with different immunodeficient strains of knockout mice (23), further efficacy and safety studies, particularly with immunocompromised nonhuman primates, could shed further light on this issue.
ADDENDUM
In a follow-up experiment in which 12 other macaques were vaccinated with MVA twice and then challenged with MPXV, exactly in the same way as in the experiment presented here, essentially the same results were observed. However, for five animals that had cleared the MPXV by day 14 after challenge, the virus could be demonstrated in their throats, but not in their plasma, on day 21, and for four of these animals, also on day 28. This phenomenon is the subject of further studies.
Acknowledgments
This work was supported by the National Institutes of Health under a contract awarded to Bavarian Nordic for the development and testing of an MVA vaccine.
We thank Robert Dias d'Ullois, Ron Briegoos, Ed Lansbergen, Liesbeth Vroegop, Guido van der Net, and Nicole Houba for technical assistance, Frank van der Panne for figure preparation, Jeanette Rimmelzwaan-Offutt for logistical assistance, and Jan de Jong for helpful discussions.
REFERENCES
- 1.Amorosa, V. K., and S. N. Isaacs. 2003. Separate worlds set to collide: smallpox, vaccinia virus vaccination, and human immunodeficiency virus and acquired immunodeficiency syndrome. Clin. Infect. Dis. 37:426-432. [DOI] [PubMed] [Google Scholar]
- 2.Bray, M., and M. E. Wright. 2003. Progressive vaccinia. Clin. Infect. Dis. 36:766-774. [DOI] [PubMed] [Google Scholar]
- 3.Breman, J. G., and I. Arita. 1980. The confirmation and maintenance of smallpox eradication. N. Engl. J. Med. 303:1263-1273. [DOI] [PubMed] [Google Scholar]
- 4.Drexler, I., K. Heller, B. Wahren, V. Erfle, and G. Sutter. 1998. Highly attenuated modified vaccinia virus Ankara replicates in baby hamster kidney cells, a potential host for virus propagation, but not in various human transformed and primary cells. J. Gen. Virol. 79:347-352. [DOI] [PubMed] [Google Scholar]
- 5.Earl, P. L., J. L. Americo, L. S. Wyatt, L. A. Eller, J. C. Whitbeck, G. H. Cohen, R. J. Eisenberg, C. J. Hartmann, D. L. Jackson, D. A. Kulesh, M. J. Martinez, D. M. Miller, E. M. Mucker, J. D. Shamblin, S. H. Zwiers, J. W. Huggins, P. B. Jahrling, and B. Moss. 2004. Immunogenicity of a highly attenuated MVA smallpox vaccine and protection against monkeypox. Nature 428:182-185. [DOI] [PubMed] [Google Scholar]
- 6.Espy, M. J., F. R. Cockerill III, R. F. Meyer, M. D. Bowen, G. A. Poland, T. L. Hadfield, and T. F. Smith. 2002. Detection of smallpox virus DNA by LightCycler PCR. J. Clin. Microbiol. 40:1985-1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franchini, M., H. Hefti, S. Vollstedt, B. Glanzmann, M. Riesen, M. Ackermann, P. Chaplin, K. Shortman, and M. Suter. 2004. Dendritic cells from mice neonatally vaccinated with modified vaccinia virus Ankara transfer resistance against herpes simplex virus type I to naive one-week-old mice. J. Immunol. 172:6304-6312. [DOI] [PubMed] [Google Scholar]
- 8.Grabenstein, J. D., and W. Winkenwerder, Jr. 2003. US military smallpox vaccination program experience. JAMA 289:3278-3282. [DOI] [PubMed] [Google Scholar]
- 9.Henderson, D. A., T. V. Inglesby, J. G. Bartlett, M. S. Ascher, E. Eitzen, P. B. Jahrling, J. Hauer, M. Layton, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. Perl, P. K. Russell, and K. Tonat. 1999. Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA 281:2127-2137. [DOI] [PubMed] [Google Scholar]
- 10.Kemper, A. R., M. M. Davis, and G. L. Freed. 2002. Expected adverse events in a mass smallpox vaccination campaign. Eff. Clin. Pract. 5:84-90. [PubMed] [Google Scholar]
- 11.Kuiken, T., R. A. Fouchier, M. Schutten, G. F. Rimmelzwaan, G. van Amerongen, D. van Riel, J. D. Laman, T. de Jong, G. van Doornum, W. Lim, A. E. Ling, P. K. Chan, J. S. Tam, M. C. Zambon, R. Gopal, C. Drosten, S. van der Werf, N. Escriou, J. C. Manuguerra, K. Stohr, J. S. Peiris, and A. D. Osterhaus. 2003. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet 362:263-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lane, J. M., F. L. Ruben, E. Abrutyn, and J. D. Millar. 1970. Deaths attributable to smallpox vaccination, 1959 to 1966, and 1968. JAMA 212:441-444. [PubMed] [Google Scholar]
- 13.Lewis-Jones, S. 2004. Zoonotic poxvirus infections in humans. Curr. Opin. Infect. Dis. 17:81-89. [DOI] [PubMed] [Google Scholar]
- 14.Mayr, A. 2003. Smallpox vaccination and bioterrorism with pox viruses. Comp. Immunol. Microbiol. Infect. Dis. 26:423-430. [DOI] [PubMed] [Google Scholar]
- 15.Mayr, A., H. Stickl, H. K. Muller, K. Danner, and H. Singer. 1978. The smallpox vaccination strain MVA: marker, genetic structure, experience gained with the parenteral vaccination and behavior in organisms with a debilitated defence mechanism. Zentbl. Bakteriol. B 167:375-390. [PubMed] [Google Scholar]
- 16.Meyer, H., M. Perrichot, M. Stemmler, P. Emmerich, H. Schmitz, F. Varaine, R. Shungu, F. Tshioko, and P. Formenty. 2002. Outbreaks of disease suspected of being due to human monkeypox virus infection in the Democratic Republic of Congo in 2001. J. Clin. Microbiol. 40:2919-2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niesters, H. G. 2002. Clinical virology in real time. J. Clin. Virol. 25(Suppl.):3-12. [DOI] [PubMed] [Google Scholar]
- 18.Rosenthal, S. R., and J. C. Clifford. 2002. Development of vaccines for bio-warfare agents. Dev. Biol. (Basel) 110:99-105. [PubMed] [Google Scholar]
- 19.Stickl, H., V. Hochstein-Mintzel, A. Mayr, H. C. Huber, H. Schafer, and A. Holzner. 1974. MVA vaccination against smallpox: clinical tests with an attenuated live vaccinia virus strain (MVA). Dtsch. Med. Wochenschr. 99:2386-2392. [DOI] [PubMed] [Google Scholar]
- 20.Stittelaar, K. J., T. Kuiken, R. L. de Swart, G. van Amerongen, H. W. Vos, H. G. Niesters, P. van Schalkwijk, K. T. van der, L. S. Wyatt, B. Moss, and A. D. Osterhaus. 2001. Safety of modified vaccinia virus Ankara (MVA) in immune-suppressed macaques. Vaccine 19:3700-3709. [DOI] [PubMed] [Google Scholar]
- 21.Stittelaar, K. J., L. S. Wyatt, R. L. de Swart, H. W. Vos, J. Groen, G. van Amerongen, R. S. van Binnendijk, S. Rozenblatt, B. Moss, and A. D. Osterhaus. 2000. Protective immunity in macaques vaccinated with a modified vaccinia virus Ankara-based measles virus vaccine in the presence of passively acquired antibodies. J. Virol. 74:4236-4243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sutter, G., and B. Moss. 1992. Nonreplicating vaccinia vector efficiently expresses recombinant genes. Proc. Natl. Acad. Sci. USA 89:10847-10851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wyatt, L. S., P. L. Earl, L. A. Eller, and B. Moss. 2004. Highly attenuated smallpox vaccine protects mice with and without immune deficiencies against pathogenic vaccinia virus challenge. Proc. Natl. Acad. Sci. USA 101:4590-4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zaucha, G. M., P. B. Jahrling, T. W. Geisbert, J. R. Swearengen, and L. Hensley. 2001. The pathology of experimental aerosolized monkeypox virus infection in cynomolgus monkeys (Macaca fascicularis). Lab. Investig. 81:1581-1600. [DOI] [PMC free article] [PubMed] [Google Scholar]