Abstract
There are no studies exploring the correlation between sleep duration and abdominal aortic calcification (AAC). This study aims to investigate this relationship and its significance. Additionally, given the higher prevalence of sleep disorders and AAC in patients with chronic kidney disease (CKD), we conducted further studies in this population. We analyzed data from the National Health and Nutrition Examination Survey (NHANES) 2013–2014. Sleep duration was assessed by a sleep questionnaire and categorized into 2–5, 6–8, and ≥ 9 h. The AAC-24 score is determined using the Kauppila scoring system and used for AAC assessment. Multivariable linear and logistic regression analysis were used to explore the relationship between sleep duration and AAC. Among the 2,996 participants, 14.29% reported nightly short sleep (2–5 h), 77.64% reported intermediate sleep (6–8 h), and 8.08% reported long sleep (≥ 9 h). After adjusting for potential confounding factors, among male participants with CKD, long sleep (≥ 9 h) significantly increased AAC-24 scores compared with intermediate sleep (6–8 h) (β: 2.12; 95% CI: 0.75, 3.50), and the risk of severe AAC (SAAC) was increased by 1.55 times (OR: 2.55; 95% CI: 1.02, 6.36). And among female CKD and non-CKD participants, sleep duration was not associated with AAC. Long sleep duration increases the risk of AAC among male adults with CKD. Prospective studies are needed to confirm this finding.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-72879-x.
Keywords: Sleep duration, Abdominal aortic calcification, Chronic kidney disease, Male, Risk factor, NHANES
Subject terms: Kidney diseases, Outcomes research
Introduction
Approximately one-third of a person’s life is spent sleeping. As a biological behavior that spans throughout life, sleep has a profound impact on our well-being1. The World Health Organization reports that sleep disorders impact an estimated 27% of individuals worldwide, constituting a significant challenge to public health. Both inadequate and excessive sleep duration are associated with an increased risk of cardiovascular diseases and an increase in mortality rates2,3.
Abdominal aortic calcification (AAC) is a common type of vascular calcification that frequently occurs as a clinical manifestation of atherosclerosis4–6. Emerging evidence suggests that AAC is not only measure of subclinical cardiovascular disease but may also serve as an independent predictor of cardiovascular events7,8.
The incidence of sleep disorders is significantly increased in patients with chronic kidney disease (CKD)9. Short or long sleep is closely related to the progression of CKD and significantly increases the risk of cardiovascular disease, which may lead to adverse health outcomes10–12. Specifically, sleep disorders may affect renal and cardiovascular function through a variety of mechanisms, including promoting chronic inflammation, activating the sympathetic nervous system and the renin-angiotensin-aldosterone system, and inducing endothelial dysfunction13–16. Especially in CKD patients, sleep disorders not only aggravate the decline of renal function, but may also lead to cardiovascular complications, thus forming a vicious cycle.
In addition, CKD is also thought to play a role in promoting vascular inflammation and calcification, which may accelerate the progression of atherosclerosis17. The 2017 update of the KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) guidelines advocates for the employment of abdominal lateral X-rays for AAC assessment in patients with CKD G3a–G5D18. Severe AAC (SAAC) correlates with a higher mortality risk in patients receiving maintenance hemodialysis and is strongly associated with cardiovascular event incidence in pre-dialysis CKD patients19,20. This suggests that AAC is an important predictor of cardiovascular events and mortality in the CKD patients.
Abnormal sleep patterns may contribute to an increased risk of arterial calcification via several mechanisms21–25. Although many studies have investigated the association between sleep duration and coronary, aortic, and carotid artery calcification, the relationship between sleep duration and AAC remains unexplored26–31. Therefore, this study aims to further investigate this relationship using data from the National Health and Nutrition Examination Survey (NHANES) 2013–2014, particularly focusing on the CKD population.
Methods
Data source
The research population stemmed from the NHANES 2013–2014 database, a nationally representative survey by the National Center for Health Statistics (NCHS). NHANES is designed to assess the health and nutritional status of Americans outside of health care settings by interviewing participants about their health status, socioeconomic status, and other relevant factors. Each cycle consists of a questionnaire and a standardized health examination, with physical examinations and laboratory tests using mobile testing equipment. Detailed NHANES study designs and data are available to the public at https://www.cdc.gov/nchs/nhanes/. Our cross-sectional study adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) Statement.
Study population
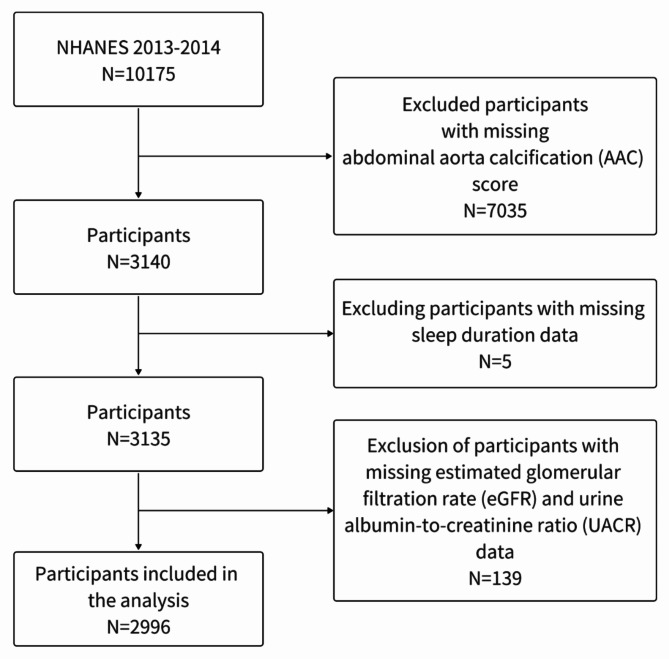
Our study population stemmed from the NHANES 2013–2014 database. NHANES 2013–2014 only performed dual-energy X-ray absorptiometry (DXA) scans on eligible participants aged 40 years and older. The initial cohort included 10,175 participants. Participants with missing AAC score (n = 7035), missing sleep duration questionnaire responses (n = 5), and missing estimated glomerular filtration rate (eGFR) and urine albumin-to-creatinine ratio (UACR) date (n = 139) were excluded, leaving 2996 participants for the final analysis. The process of participant inclusion and exclusion is shown in Fig. 1.
Fig. 1.
Flowchart of participant inclusion and exclusion from NHANES 2013–2014.
Sleep duration
Sleep duration was assessed by the sleep questionnaire, with answer choices spanning from 2 to 11 h, 12 h or more, rejection or unknown. Adhering to the consensus statement from the American Academy of Sleep Medicine, we categorized sleep duration into three groups: short sleep (2–5 h), intermediate sleep (6–8 h), and long sleep (≥ 9 h)32. The detailed description of the sleep disorders questionnaire is shown in Supplementary Table 1.
Abdominal aortic calcification
AAC was quantitatively assessed using DXA in participants aged 40 and above. The NHANES Mobile Examination Center’s certified radiologic technologists performed the scans. Exclusion criteria for these scans included pregnancy, recent use of radiographic contrast materials (barium), or a bodyweight exceeding 450 pounds. The AAC-24 score is determined using the Kauppila scoring system and used for AAC assessment, which ranges from 0 to 24. A score of 1 or higher indicates the presence of AAC, while scores > 6 indicate severe calcification and are classified as SAAC.
Chronic kidney disease
CKD was defined as eGFR below 60 ml/min/1.73 m2 and/or UACR ≥ 30 mg/g33. The eGFR was computed using the CKD-EPI formula, with the UACR calculated by dividing the urinary albumin concentration (in milligrams) by the urinary creatinine concentration (in grams)34.
Study covariates
Based on previous studies, we considered some potential confounding variables that may affect the association between sleep duration and AAC in our analyses. These variables include age, gender, race, body mass index, poverty-income ratio, education level, smoking history, alcohol drinking, hypertension, diabetes, cardiovascular diseases, chronic kidney disease, sedentary time, eGFR, total cholesterol, high-density lipoprotein cholesterol, serum total calcium, serum phosphorus, serum total 25-hydroxyvitamin D and neutrophil-to-lymphocyte ratio. Smoking history was defined as having smoked at least 100 cigarettes in a lifetime, and alcohol drinking was defined as having consumed at least 12 drinks of alcohol in any one year. Hypertension and diabetes were determined based on self-report. Although self-reported hypertension and diabetes do not equate to a formal diagnosis, they have been validated as screening measures for hypertension and diabetes in epidemiological studies35–37. Sedentary time was defined based on the physical activity questionnaire. The diagnosis of cardiovascular disease was determined based on self-reported physician diagnoses obtained through standardized medical status questionnaires administered in individual interviews. In addition, we also included potentially relevant laboratory data. The detailed instructions on specimen collection and processing are recorded in the NHANES laboratory procedure manual, and the quality control conforms to the standard procedure. The detailed description of the questionnaire is shown in Supplementary Table 1.
Statistical analyses
Baseline characteristics were categorized according to sleep duration and the AAC-24 score. Missing values in continuous variables are handled using mean substitution, while missing values in categorical variables are treated as a separate category. Categorical variables were represented by number (percentage, %) while continuous variables were described by the mean (standard deviation, SD) or median (interquartile range, IQR), as appropriate. To compare the differences across groups, one-way analyses of variance (normal distribution), Kruskal–Wallis tests (skewed distribution), and chi-square tests (categorical variables) were undertaken. Multivariable linear regression analysis was used to investigate the relationship between sleep duration and the AAC-24 score. Multivariable logistic regression analysis was used to explore the correlation between sleep duration and SAAC. In addition, subgroup analyses were performed according to CKD (CKD vs. non-CKD), with stratified analysis by gender (male vs. female). To assess heterogeneity among subgroups, the interaction between subgroup and sleep duration was also examined by likelihood ratio testing. In Supplementary Tables 3 and 4, we also show the results of the interaction tests between sleep duration and different eGFR groups in the CKD participants. All statistical analyses were performed using Free Statistics software (version 1.9.2) and the R software packages (http://www.R-project.org, The R Foundation). By a two-tailed testing, a p-value of < 0.05 was declared significant.
Ethics approval and consent to participate
All participants gave written informed consent, and the NCHS Ethics Review Board (ERB) approved the NHANES study methods. The NCHS IRB/ERB protocol number for 2013–2014 was #2011-17. Details of the institutional review boards at CDC and NCHS are available at https://www.cdc.gov/nchs/nhanes/irba98.htm. All methods of this study were performed in accordance with the principles outlined in the Declaration of Helsinki. No further institutional review board approval was required for this secondary analysis38. Users can download the data free of charge for research and publication.
Results
Characteristics of the study population
Among the 2,996 participants (Table 1), the average age was 58.55 ± 12.00 years, with 48.23% males and 51.77% females. The ethnic distribution is as follows: Mexican Americans accounted for 13.21%, non-Hispanic whites accounted for 44.19%, and non-Hispanic blacks accounted for 19.13%. Educational level shows that 22.83% did not complete high school education or above. The combined diseases included hypertension (47.13%), diabetes (16.26%), cardiovascular disease (12.68%) and CKD (21.03%). The average AAC-24 score of the participants was 1.61 ± 3.48. In addition, 14.29% reported nightly short sleep (2–5 h), 77.64% reported intermediate sleep (6–8 h), and 8.08% reported long sleep (≥ 9 h).
Table 1.
Characteristics of participants ≥ 40 years of age from the NHANES 2013–2014.
| Characteristics | Total | Sleep duration, h | AAC-24 score | |||||
|---|---|---|---|---|---|---|---|---|
| 2–5 h | 6–8 h | ≥ 9 h | P-value | Non-SAAC | SAAC | P-value | ||
| n (%) | 2996 | 428 (14.29) | 2326 (77.64) | 242 (8.08) | 2732 (91.19) | 264 (8.81) | ||
| Age (year), Mean ± SD | 58.55 ± 12.00 | 56.27 ± 11.16 | 58.37 ± 11.94 | 64.31 ± 12.25 | < 0.001 | 57.31 ± 11.49 | 71.37 ± 9.27 | < 0.001 |
| Gender, n (%) | 0.971 | 0.864 | ||||||
| Male | 1445 (48.23) | 206 (48.13) | 1124 (48.32) | 115 (47.52) | 1319 (48.28) | 126 (47.73) | ||
| Female | 1551 (51.77) | 222 (51.87) | 1202 (51.68) | 127 (52.48) | 1413 (51.72) | 138 (52.27) | ||
| Race, n (%) | < 0.001 | < 0.001 | ||||||
| Mexican American | 399 (13.32) | 55 (12.85) | 318 (13.67) | 26 (10.74) | 376 (13.76) | 23 (8.71) | ||
| Other Hispanic | 285 ( 9.51) | 52 (12.15) | 212 (9.11) | 21 (8.68) | 274 (10.03) | 11 (4.17) | ||
| Non-Hispanic White | 1324 (44.19) | 141 (32.94) | 1049 (45.1) | 134 (55.37) | 1153 (42.2) | 171 (64.77) | ||
| Non-Hispanic Black | 573 (19.13) | 125 (29.21) | 408 (17.54) | 40 (16.53) | 541 (19.8) | 32 (12.12) | ||
| Other | 415 (13.85) | 55 (12.85) | 339 (14.57) | 21 (8.68) | 388 (14.2) | 27 (10.23) | ||
| Education < high school, n (%) | 684 (22.83) | 104 (24.3) | 509 (21.88) | 71 (29.34) | 0.085 | 614 (22.47) | 70 (26.52) | 0.278 |
| Smoking history, n (%) | 1379 (46.03) | 218 (50.93) | 1042 (44.8) | 119 (49.17) | 0.126 | 1221 (44.69) | 158 (59.85) | < 0.001 |
| Alcohol drinking, n (%) | 2018 (67.36) | 277 (64.72) | 1573 (67.63) | 168 (69.42) | 0.412 | 1835 (67.17) | 183 (69.32) | 0.324 |
| Hypertension, n (%) | 1412 (47.13) | 221 (51.64) | 1054 (45.31) | 137 (56.61) | 0.001 | 1216 (44.51) | 196 (74.24) | < 0.001 |
| Diabetes, n (%) | 487 (16.26) | 79 (18.46) | 352 (15.13) | 56 (23.14) | 0.009 | 410 (15.01) | 77 (29.17) | < 0.001 |
| Cardiovascular diseases, n (%) | 380 (12.68) | 66 (15.42) | 271 (11.65) | 43 (17.77) | 0.003 | 291 (10.65) | 89 (33.71) | < 0.001 |
| Chronic kidney disease, n (%) | 630 (21.03) | 99 (23.13) | 450 (19.35) | 81 (33.47) | < 0.001 | 501 (18.34) | 129 (48.86) | < 0.001 |
| Body mass index (kg/m2), Mean ± SD | 28.48 ± 5.56 | 29.28 ± 5.88 | 28.31 ± 5.47 | 28.61 ± 5.72 | 0.004 | 28.60 ± 5.64 | 27.20 ± 4.38 | < 0.001 |
| Poverty-income ratio, Mean ± SD | 2.69 ± 1.58 | 2.32 ± 1.49 | 2.78 ± 1.58 | 2.49 ± 1.63 | < 0.001 | 2.70 ± 1.58 | 2.57 ± 1.50 | 0.196 |
| AAC-24 score, Mean ± SD | 1.61 ± 3.48 | 1.38 ± 3.19 | 1.56 ± 3.43 | 2.47 ± 4.24 | < 0.001 | 0.69 ± 1.46 | 11.18 ± 3.87 | < 0.001 |
| Sedentary time (min), Mean ± SD | 410.82 ± 190.59 | 389.29 ± 213.15 | 413.11 ± 186.30 | 426.98 ± 186.85 | 0.023 | 408.57 ± 192.04 | 434.20 ± 173.43 | 0.037 |
| Sleep duration (h), Mean ± SD | 6.88 ± 1.41 | 4.53 ± 0.70 | 7.04 ± 0.80 | 9.50 ± 0.80 | < 0.001 | 6.84 ± 1.41 | 7.27 ± 1.39 | < 0.001 |
| Laboratory measurements | ||||||||
| eGFR (ml/min/1.73m2), Mean ± SD | 84.62 ± 20.25 | 85.98 ± 21.22 | 85.28 ± 19.53 | 75.84 ± 23.16 | < 0.001 | 86.18 ± 19.39 | 68.51 ± 21.90 | < 0.001 |
| UACR (mg/g), median ± IQR | 7.93 (5.17, 15.85) | 8.11 (5.33, 18.16) | 7.73 (5.00, 15.03) | 9.25 (6.02, 17.42) | 0.002 | 7.56 (5.00, 14.40) | 13.17 (7.07, 29.38) | < 0.001 |
| Total cholesterol (mg/dL), Mean ± SD | 195.03 ± 43.65 | 196.95 ± 44.03 | 195.07 ± 43.83 | 191.27 ± 41.10 | 0.269 | 196.16 ± 43.85 | 183.37 ± 39.75 | < 0.001 |
| High-density lipoprotein cholesterol (mg/dL), Mean ± SD | 54.05 ± 16.72 | 51.82 ± 15.64 | 54.48 ± 16.91 | 53.90 ± 16.46 | 0.010 | 54.12 ± 16.73 | 53.34 ± 16.65 | 0.470 |
| Serum total calcium (mg/dL), Mean ± SD | 9.45 ± 0.37 | 9.44 ± 0.37 | 9.45 ± 0.36 | 9.47 ± 0.40 | 0.639 | 9.45 ± 0.37 | 9.49 ± 0.35 | 0.137 |
| Serum phosphorus (mg/dL), Mean ± SD | 3.79 ± 0.57 | 3.86 ± 0.60 | 3.78 ± 0.56 | 3.83 ± 0.58 | 0.018 | 3.79 ± 0.57 | 3.87 ± 0.58 | 0.024 |
| Serum total 25-hydroxyvitamin D (nmol/L), Mean ± SD | 70.48 ± 29.46 | 64.59 ± 28.48 | 71.32 ± 29.41 | 72.80 ± 30.58 | < 0.001 | 69.53 ± 28.85 | 80.37 ± 33.67 | < 0.001 |
| Neutrophil-to-lymphocyte ratio, Mean ± SD | 2.22 ± 1.30 | 2.15 ± 1.33 | 2.22 ± 1.30 | 2.33 ± 1.26 | 0.219 | 2.18 ± 1.26 | 2.61 ± 1.60 | < 0.001 |
Significant results are in bold.
AAC abdominal aortic calcification, SAAC severe abdominal aortic calcification, eGFR estimated glomerular filtration rate, UACR urine albumin-to-creatinine ratio.
Significant variations were observed in the AAC-24 score among the three participant groups with different sleep durations (p < 0.001). In particular, the AAC-24 score was highest in the long sleep (≥ 9 h) group. In addition, the participants with long sleep (≥ 9 h) were older and had a higher prevalence of hypertension, diabetes, cardiovascular disease and CKD. Participants in the long sleep (≥ 9 h) group had higher UACR and serum total 25-hydroxyvitamin D levels, longer sedentary time, and lowest eGFR levels.
In the SAAC group, participants were older on average, had longer sedentary and sleep duration, had more comorbidities, and were more likely to smoke. Also, there were significant differences between the SAAC group and the non-SAAC group in lab test results for eGFR, UACR, total cholesterol, serum phosphorus, serum total 25-hydroxyvitamin D and neutrophil-to-lymphocyte ratio (all p < 0.05).
Sleep duration and AAC
As shown in Table 2, in unadjusted model 1, long sleep (≥ 9 h) was associated with a higher AAC-24 score (β: 0.91; 95% CI: 0.45, 1.37) and an increased SAAC risk (OR: 1.84; 95% CI: 1.25, 2.69). However, in adjusted models 2 and 3, there was no significant difference between sleep duration and the AAC-24 score or SAAC risk (p > 0.05).
Table 2.
Association between sleep duration and AAC (AAC-24 score and SAAC).
| Sleep duration, h | Model 1 | P-value | Model 2 | P-value | Model 3 | P-value |
|---|---|---|---|---|---|---|
| AAC-24 Score/β (95% CI) | ||||||
| 2–5 h | -0.18 (-0.54, 0.17) | 0.315 | 0.15 (-0.18, 0.48) | 0.374 | 0 (-0.33, 0.32) | 0.99 |
| 6–8 h | Reference | Reference | Reference | |||
| ≥ 9 h | 0.91 (0.45, 1.37) | < 0.001 | 0.20 (-0.22, 0.63) | 0.351 | 0.04 (-0.38, 0.45) | 0.864 |
| SAAC/OR (95% CI) | ||||||
| 2–5 h | 0.68 (0.45, 1.04) | 0.073 | 0.98 (0.62, 1.55) | 0.925 | 0.87 (0.54, 1.39) | 0.552 |
| 6–8 h | Reference | Reference | Reference | |||
| ≥ 9 h | 1.84 (1.25, 2.69) | 0.002 | 1.03 (0.68, 1.56) | 0.899 | 0.93 (0.6, 1.44) | 0.739 |
Significant results are in bold.
AAC abdominal aortic calcification, SAAC severe abdominal aortic calcification, CKD chronic kidney disease, eGFR estimated glomerular filtration rate, β effect size, OR odds ratio, 95% Cl 95% confidence interval.
Model 1: no covariates were adjusted. Model 2: adjusted for age, gender and race. Model 3: adjusted for age, gender, race, body mass index, poverty-income ratio, education level, smoking history, alcohol drinking, hypertension, diabetes, CKD, cardiovascular diseases, sedentary time, eGFR, total cholesterol, high-density lipoprotein cholesterol, serum total calcium, serum phosphorus, serum total 25-hydroxyvitamin D and neutrophil-to-lymphocyte ratio.
Sleep duration, CKD and AAC
Tables 3 and 4 show the adjusted multivariable regression model for subgroup analysis according to the CKD, with stratified analysis by gender. Among male CKD participants, long sleep (≥ 9 h) was associated with a high AAC-24 score (β: 2.12; 95% CI: 0.75, 3.50) compared with intermediate sleep (6–8 h), and the risk of SAAC increased by 1.55 times (OR: 2.55; 95% CI: 1.02, 6.36). In contrast, among female CKD and non-CKD participants, no significant association was observed between different sleep durations and AAC (all p > 0.05). In addition, there were significant interactions between sleep duration and CKD in the overall population, especially in male participants but not in female participants (p for interaction < 0.05).
Table 3.
Association between sleep duration and AAC-24 score in CKD and non-CKD subgroups.
| Subgroups | Total β (95%CI) |
P-value | P for interaction | Male β (95%CI) |
P-value | P for interaction | Female β (95%CI) |
P-value | P for interaction |
|---|---|---|---|---|---|---|---|---|---|
| 0.011 | 0.001 | 0.784 | |||||||
| CKD | |||||||||
| 2–5 h | 0.33 (-0.66, 1.31) | 0.515 | -0.50 (-1.87, 0.88) | 0.478 | 0.83 (-0.61, 2.27) | 0.26 | |||
| 6–8 h | Reference | Reference | Reference | ||||||
| ≥ 9 h | 0.63 (-0.42, 1.69) | 0.241 | 2.12 (0.75, 3.50) | 0.003 | -1.20 (-2.83, 0.42) | 0.148 | |||
| Non-CKD | |||||||||
| 2–5 h | -0.07 (-0.38, 0.24) | 0.649 | -0.18 (-0.65, 0.28) | 0.446 | 0.01 (-0.41, 0.44) | 0.951 | |||
| 6–8 h | Reference | Reference | Reference | ||||||
| ≥ 9 h | -0.29 (-0.71, 0.14) | 0.183 | -0.11 (-0.77, 0.55) | 0.74 | -0.41 (-0.97, 0.15) | 0.15 | |||
Significant results are in bold.
AAC abdominal aortic calcification, CKD chronic kidney disease, eGFR estimated glomerular filtration rate, β effect size, 95% Cl 95% confidence interval.
All subgroups were adjusted for age, gender, race, body mass index, poverty-income ratio, education level, smoking history, alcohol drinking, hypertension, diabetes, CKD, cardiovascular diseases, sedentary time, eGFR, total cholesterol, high-density lipoprotein cholesterol, serum total calcium, serum phosphorus, serum total 25-hydroxyvitamin D, and neutrophil-to-lymphocyte ratio, except the stratification factor itself.
Table 4.
Association between sleep duration and SAAC in CKD and non-CKD subgroups.
| Subgroups | Total OR (95% CI) |
P-value | P for interaction | Male OR (95% CI) |
P-value | P for interaction | Female OR (95% CI) |
P-value | P for interaction |
|---|---|---|---|---|---|---|---|---|---|
| 0.034 | 0.023 | 0.515 | |||||||
| CKD | |||||||||
| 2–5 h | 1.42 (0.71, 2.86) | 0.324 | 1.25 (0.34, 4.58) | 0.741 | 1.42 (0.56, 3.61) | 0.46 | |||
| 6–8 h | Reference | Reference | Reference | ||||||
| ≥ 9 h | 1.39 (0.76, 2.54) | 0.279 | 2.55 (1.02, 6.36) | 0.044 | 0.72 (0.27, 1.89) | 0.506 | |||
| Non-CKD | |||||||||
| 2–5 h | 0.55 (0.27, 1.12) | 0.099 | 0.45 (0.15, 1.35) | 0.153 | 0.66 (0.25, 1.73) | 0.401 | |||
| 6–8 h | Reference | Reference | Reference | ||||||
| ≥ 9 h | 0.59 (0.28, 1.22) | 0.153 | 0.71 (0.25, 2.04) | 0.527 | 0.38 (0.12, 1.21) | 0.102 | |||
Significant results are in bold.
SAAC severe abdominal aortic calcification, CKD chronic kidney disease, eGFR estimated glomerular filtration rate, OR odds ratio, 95% Cl 95% confidence interval.
All subgroups were adjusted for age, gender, race, body mass index, poverty-income ratio, education level, smoking history, alcohol drinking, hypertension, diabetes, CKD, cardiovascular diseases, sedentary time, eGFR, total cholesterol, high-density lipoprotein cholesterol, serum total calcium, serum phosphorus, serum total 25-hydroxyvitamin D, and neutrophil-to-lymphocyte ratio, except the stratification factor itself.
Supplementary Tables 2, 3, and 4 showed further subgroup analyses based on eGFR in CKD participants, with stratified analysis by gender. The results showed that in the adjusted model, there were no significant interactions between sleep duration and different eGFR subgroups (p for interaction > 0.05).
Discussion
To our knowledge, this study is the first to investigate the association between sleep duration and AAC. We finally included 2,996 participants and found that long sleep (≥ 9 h) compared with intermediate sleep (6–8 h) was clinically significantly associated with AAC in male CKD participants. Among female CKD and non-CKD participants, sleep duration was not associated with AAC.
The relevant research conclusions are not consistent. The Pittsburgh SleepSCORE study indicated no association between sleep duration or efficiency and coronary artery calcification27. Similarly, a prospective cohort study with a median follow-up of 5 years found no link between nighttime or total sleep duration and the progression of coronary artery calcification30. In contrast, a cohort study from Chicago (the CARDIA study) observed that longer sleep duration was associated with a reduced incidence of calcification over a 5-year period26. In addition, another cross-sectional study highlighted that both insufficient and excessive sleep duration contribute to a higher prevalence of coronary artery calcification29.
It is worth noting that previous studies have not explored high-risk groups for sleep disorders and arterial calcification. Given the high prevalence of sleep disorders and AAC in CKD patients, we further investigated this population. Our study found that among male participants with CKD, long sleep (≥ 9 h) was associated with an increased AAC-24 score, significantly increasing the likelihood of developing AAC. Additionally, the interaction results also indicated that sleep duration had different effects on AAC between CKD and non-CKD subgroups among male participants. This observation is particularly significant given the consensus statement from the American Academy of Sleep Medicine regarding the uncertain health risk of sleeping more than 9 h per night in certain populations32.
The prevalence of vascular calcification increases with age and varies by gender and racial demographics6. AAC is one of the common types. Previously deemed benign, recent evidence positions AAC as a significant predictor of cardiovascular event incidence and mortality6,8. Despite the increasing number of pharmacological interventions aimed at slowing the progression of vascular calcification, effective clinical treatment strategies remain uncertain39,40. Moreover, vascular calcification is more common and progresses more rapidly in patients with CKD, especially those undergoing dialysis41–43. Studies across Europe and Japan have underscored the predictive value of AAC for cardiovascular morbidity and mortality in dialysis and pre-dialysis CKD populations20,44. AAC has been shown to be superior to other forms of arterial calcification in predicting mortality in peritoneal dialysis patients45,46. Notably, sleep disorders are also very common in patients with CKD, and a large proportion of patients in the advanced stage or receiving hemodialysis will experience excessive sleepiness and fatigue47–49.
Our study highlights the clinical significance of investigating the impact of sleep duration on AAC risk, particularly in CKD patients. As an intervenable behavioral factor, exploring the relationship between sleep duration and the risk of AAC can guide us in sleep screening and management in specific populations. Given the increased frequency and severity of cardiovascular disease in CKD patients, early detection of AAC and interventions for risk factors are critical50.
However, the mechanisms underlying the association between long sleep duration and AAC remain largely unexplored. Long-sleep-associated behavioral risk factors and metabolic syndrome may be involved, including smoking and drinking, hypertriglyceridemia, low-level HDL, hyperglycemia, and so on21,51–56. Additionally, sleep duration was associated with markers of inflammation56,57. Excessive sleep duration or daytime sleepiness and fatigue lead to increased levels of inflammatory markers and cytokines, as evidenced by significantly higher levels of CRP and IL-6 in individuals who slept longer58–60. The increase in inflammation and cytokine levels could potentially play a role in the formation of AAC24. Notably, the pathophysiological mechanisms of CKD also involve chronic inflammation, oxidative stress, and endothelial dysfunction61. CKD patients also have higher blood phosphorus levels compared to the general population62–64. These factors may increase the risk of AAC in CKD patients with comorbid long sleep.
Our analysis also revealed a gender-specific relationship between sleep duration and AAC. Specifically, unlike male CKD participants, there was no significant association between sleep duration and AAC risk in female CKD participants. This gender-specificity suggests that sex hormones might play a moderating role in this relationship. Prior studies have associated male sex hormones with an increased risk of cardiovascular calcification, whereas female sex hormones have been acknowledged for their cardioprotective properties65. Additionally, a cross-sectional study found that longer sleep duration may lead to lower testosterone levels in middle-aged men66. And lower testosterone levels may increase the risk of arterial calcification in adult men67. Nonetheless, additional future studies are needed to further explore the clinical implications of these findings.
Strengths and limitations
The study has several strengths. First, this is the first study to explore the relationship between sleep duration and AAC. Second, by stratifying CKD participants, our study provides precise guidance for clinical practices targeting high-risk groups. Third, the inclusion of a racially and ethnically diverse sample of the United States population enhances the generalizability of our findings. Finally, based on previously published literature, we adjusted for covariates that might influence our findings wherever possible, thereby improving the reliability of our results. Overall, our study provides new insights into the effects of long sleep on specific populations and enriches the current field of research.
Our study also has several limitations. The cross-sectional design limits our capacity to affirm causal relationships between sleep duration and AAC. The reliance on self-reported sleep duration data introduces the potential for reporting bias and may not accurately reflect the full spectrum of sleep disorders among participants, given that the questionnaire focused solely on nighttime sleep and omitted total sleep duration. Meanwhile, responses to sleep duration in the questionnaire were recorded as integers, which may not accurately represent the actual sleep duration experienced by the patients. These potential limitations may have introduced bias in classifying the sleep duration groups. More importantly, the absence of data on self-reported wake and sleep initiation times also constrains our analysis of the circadian rhythm’s impact on AAC risk. In addition, the criteria for DXA inclusion being restricted to individuals aged 40 and above narrows the scope of our findings. Despite adjusting for numerous confounding variables, we cannot discount the possibility of residual confounding factors influencing our results. It is worth noting that the data used in this study covers the period from 2013 to 2014, and this time limitation may affect the applicability of our findings to the current situation. Lastly, prospective studies are still needed to verify whether our conclusions drawn from the NHANES database can be generalized to other populations and regions.
Conclusions
Our research indicates that long sleep (≥ 9 h) is associated with the risk of AAC in male CKD adults. These insights underscore the importance of sleep screening and management within CKD care strategies to prevent potential cardiovascular complications in this population. In addition, these findings highlight the complex relationship between sleep duration and AAC, especially in male CKD patients, which emphasizes the need for further prospective studies to validate this conclusion and further elucidate the underlying biological mechanisms of the association between sleep duration and AAC.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We gratefully acknowledge the NHANES for providing data support for this study.
Abbreviations
- NHANES
National Health and Nutrition Examination Survey
- NCHS
National Center for Health Statistics
- AAC
Abdominal aortic calcification
- SAAC
Severe abdominal aortic calcification
- DXA
Dual-energy X-ray absorptiometry
- CKD
Chronic kidney disease
- eGFR
Estimated glomerular filtration rate
- UACR
Urine albumin-to-creatinine ratio
Author contributions
Y.W. and X.L. wrote the main manuscript text and performed the statistical analysis. J.Z. performed the statistical analysis. B.Z. and W.Y. reviewed and edited the manuscript. K.H. designed and supervised the study, revised and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by grant from the National Natural Science Foundation of China (No. 82270101).
Data availability
Detailed NHANES study designs and data are available to the public at https://www.cdc.gov/nchs/nhanes/.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All participants gave written informed consent, and the NCHS Ethics Review Board approved the NHANES study methods. The NCHS IRB/ERB protocol number for 2013–2014 was #2011-17.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yuhan Wang and Xu Liu.
References
- 1.Grandner, M. A. & Sleep health, and society. Sleep Med. Clin.12, 1–22 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krittanawong, C. et al. Association between short and long sleep durations and cardiovascular outcomes: A systematic review and meta-analysis. Eur. Heart J. Acute Cardiovasc. Care8, 762–770 (2019). [DOI] [PubMed] [Google Scholar]
- 3.Kuehn, B. M. Sleep duration linked to cardiovascular disease. Circulation139, 2483–2484 (2019). [DOI] [PubMed] [Google Scholar]
- 4.Danielsen, R., Sigvaldason, H., Thorgeirsson, G. & Sigfússon, N. Predominance of aortic calcification as an atherosclerotic manifestation in women: The Reykjavik study. J. Clin. Epidemiol.49, 383–387 (1996). [DOI] [PubMed] [Google Scholar]
- 5.Jayalath, R. W., Mangan, S. H. & Golledge, J. Aortic calcification. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg.30, 476–488 (2005). [DOI] [PubMed] [Google Scholar]
- 6.Bartstra, J. W., Mali, W. P. T. M., Spiering, W. & de Jong, P. A. Abdominal aortic calcification: From ancient friend to modern foe. Eur. J. Prev. Cardiol.28, 1386–1391 (2021). [DOI] [PubMed] [Google Scholar]
- 7.Wong, N. D. et al. Abdominal aortic calcium and multi-site atherosclerosis: The multiethnic study of atherosclerosis. Atherosclerosis214, 436–441 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bastos Gonçalves, F. et al. Calcification of the abdominal aorta as an independent predictor of cardiovascular events: A meta-analysis. Heart Br. Card. Soc.98, 988–994 (2012). [DOI] [PubMed] [Google Scholar]
- 9.De Santo, R. M., Cesare, C. M., Bartiromo, M. & Cirillo, M. High prevalence of sleep disorders at the time of CKD diagnosis. J. Ren. Nutr. Off. J. Counc. Ren. Nutr. Natl. Kidney Found.18, 104–106 (2008). [DOI] [PubMed] [Google Scholar]
- 10.Jiang, L. & Xu, H. U-Shaped relationship between Sleep Duration and CKD in US adults: Data from National Health and Nutrition Examination Survey (NHANES) 2005–2014. Am. J. Nephrol.54, 275–280 (2023). [DOI] [PubMed] [Google Scholar]
- 11.Turek, N. F., Ricardo, A. C. & Lash, J. P. Sleep disturbances as nontraditional risk factors for development and progression of CKD: Review of the evidence. Am. J. Kidney Dis. Off. J. Natl. Kidney Found.60, 823–833 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cappuccio, F. P., Cooper, D., D’Elia, L., Strazzullo, P. & Miller, M. A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J.32, 1484–1492 (2011). [DOI] [PubMed] [Google Scholar]
- 13.Cirillo, P. et al. Systemic inflammation, metabolic syndrome and progressive renal disease. Nephrol. Dial. Transpl. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc.24, 1384–1387 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vink, E. E., de Jager, R. L. & Blankestijn, P. J. Sympathetic hyperactivity in chronic kidney disease: Pathophysiology and (new) treatment options. Curr. Hypertens. Rep.15, 95–101 (2013). [DOI] [PubMed] [Google Scholar]
- 15.Miller, M. A. & Howarth, N. E. Sleep and cardiovascular disease. Emerg. Top. Life Sci.7, 457–466 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Javaheri, S. et al. Sleep apnea: Types, mechanisms, and clinical cardiovascular consequences. J. Am. Coll. Cardiol.69, 841–858 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogers, M., Goettsch, C. & Aikawa, E. Medial and intimal calcification in chronic kidney disease: Stressing the contributions. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis.2, e000481 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ketteler, M. et al. Executive summary of the 2017 KDIGO chronic kidney disease-mineral and bone disorder (CKD-MBD) guideline update: What’s changed and why it matters. Kidney Int.92, 26–36 (2017). [DOI] [PubMed] [Google Scholar]
- 19.Okuno, S. et al. Presence of abdominal aortic calcification is significantly associated with all-cause and cardiovascular mortality in maintenance hemodialysis patients. Am. J. Kidney Dis. Off. J. Natl. Kidney Found.49, 417–425 (2007). [DOI] [PubMed] [Google Scholar]
- 20.Hanada, S. et al. Assessment and significance of abdominal aortic calcification in chronic kidney disease. Nephrol. Dial. Transpl. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc.25, 1888–1895 (2010). [DOI] [PubMed] [Google Scholar]
- 21.Williams, C. J., Hu, F. B., Patel, S. R. & Mantzoros, C. S. Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes. Diabetes Care30, 1233–1240 (2007). [DOI] [PubMed] [Google Scholar]
- 22.Hall, M. H. et al. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep31, 635–643 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Golledge, J. Abdominal aortic calcification: Clinical significance, mechanisms and therapies. Curr. Pharm. Des.20, 5834–5838 (2014). [DOI] [PubMed] [Google Scholar]
- 24.Szulc, P. Abdominal aortic calcification: A reappraisal of epidemiological and pathophysiological data. Bone84, 25–37 (2016). [DOI] [PubMed] [Google Scholar]
- 25.Irwin, M. R., Olmstead, R. & Carroll, J. E. Sleep disturbance, sleep duration, and inflammation: A systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol. Psychiatry80, 40–52 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.King, C. R. et al. Short sleep duration and incident coronary artery calcification. JAMA300, 2859–2866 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matthews, K. A. et al. Associations of Framingham risk score profile and coronary artery calcification with sleep characteristics in middle-aged men and women: Pittsburgh SleepSCORE study. Sleep34, 711–716 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matthews, K. A. et al. Do reports of sleep disturbance relate to coronary and aortic calcification in healthy middle-aged women? Study of women’s health across the nation. Sleep Med.14, 282–287 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim, C. W. et al. Sleep duration, sleep quality, and markers of subclinical arterial disease in healthy men and women. Arterioscler. Thromb. Vasc. Biol.35, 2238–2245 (2015). [DOI] [PubMed] [Google Scholar]
- 30.Kowall, B. et al. Sleep characteristics and progression of coronary artery calcification: Results from the Heinz Nixdorf Recall cohort study. Atherosclerosis271, 45–52 (2018). [DOI] [PubMed] [Google Scholar]
- 31.Suzuki, S. et al. Self-reported sleep duration and subclinical atherosclerosis in a general population of Japanese men. J. Atheroscler. Thromb.25, 186–198 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Watson, N. F. et al. Recommended amount of Sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep38, 843–844 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kidney Disease Improving global outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 Clinical Practice Guideline for the management of glomerular diseases. Kidney Int.100, S1–S276 (2021). [DOI] [PubMed] [Google Scholar]
- 34.Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med.150, 604–612 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giles, W. H., Croft, J. B., Keenan, N. L., Lane, M. J. & Wheeler, F. C. The validity of self-reported hypertension and correlates of hypertension awareness among blacks and whites within the stroke belt. Am. J. Prev. Med.11, 163–169 (1995). [PubMed] [Google Scholar]
- 36.Casagrande, S. S., Cowie, C. C. & Genuth, S. M. Self-reported prevalence of diabetes screening in the U.S., 2005–2010. Am. J. Prev. Med.47, 780–787 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martin, L. M., Leff, M., Calonge, N., Garrett, C. & Nelson, D. E. Validation of self-reported chronic conditions and health services in a managed care population. Am. J. Prev. Med.18, 215–218 (2000). [DOI] [PubMed] [Google Scholar]
- 38.Bradway, D. Guidance on Secondary Analysis of Existing Data Sets | Office of the Vice President for Research. https://ovpr.uconn.edu/services/rics/irb/researcher-guide/secondary-analysis-of-data-sets/ (2015).
- 39.Singh, A., Tandon, S. & Tandon, C. An update on vascular calcification and potential therapeutics. Mol. Biol. Rep.48, 887–896 (2021). [DOI] [PubMed] [Google Scholar]
- 40.Cozzolino, M. et al. Future treatment of vascular calcification in chronic kidney disease. Expert Opin. Pharmacother.24, 2041–2057 (2023). [DOI] [PubMed] [Google Scholar]
- 41.Toussaint, N. D., Lau, K. K., Strauss, B. J., Polkinghorne, K. R. & Kerr, P. G. Associations between vascular calcification, arterial stiffness and bone mineral density in chronic kidney disease. Nephrol. Dial. Transpl. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc.23, 586–593 (2008). [DOI] [PubMed] [Google Scholar]
- 42.Górriz, J. L. et al. Vascular calcification in patients with nondialysis CKD over 3 years. Clin. J. Am. Soc. Nephrol. CJASN10, 654–666 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang, H. et al. Progression of vascular calcification and clinical outcomes in patients receiving maintenance dialysis. JAMA Netw. Open6, e2310909 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Verbeke, F. et al. Prognostic value of aortic stiffness and calcification for cardiovascular events and mortality in dialysis patients: Outcome of the calcification outcome in renal disease (CORD) study. Clin. J. Am. Soc. Nephrol. CJASN6, 153–159 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martino, F. et al. Abdominal aortic calcification is an independent predictor of cardiovascular events in peritoneal dialysis patients. Ther. Apher. Dial. Off. Peer-Rev. J. Int. Soc. Apher. Jpn. Soc. Apher. Jpn. Soc. Dial. Ther.17, 448–453 (2013). [DOI] [PubMed] [Google Scholar]
- 46.Niu, Q. et al. Abdominal aortic calcification is superior to other arteries calcification in predicting the mortality in peritoneal dialysis patients—A 8 years cohort study. BMC Nephrol.20, 439 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hanly, P. Sleep apnea and daytime sleepiness in end-stage renal disease. Semin. Dial. 17, 109–114 (2004). [DOI] [PubMed] [Google Scholar]
- 48.Roumelioti, M. E. et al. Sleep-disordered breathing and excessive daytime sleepiness in chronic kidney disease and hemodialysis. Clin. J. Am. Soc. Nephrol. CJASN6, 986–994 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adejumo, O. A. et al. Sleep quality and associated factors among patients with chronic kidney disease in Nigeria: A cross-sectional study. BMJ Open.13, e074025 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gansevoort, R. T. et al. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet Lond. Engl.382, 339–352 (2013). [DOI] [PubMed] [Google Scholar]
- 51.Roehrs, T. & Roth, T. Sleep, sleepiness, and alcohol use. Alcohol Res. Health J. Natl. Inst. Alcohol Abuse Alcohol25, 101–109 (2001). [PMC free article] [PubMed] [Google Scholar]
- 52.Htoo, A., Talwar, A., Feinsilver, S. H. & Greenberg, H. Smoking and sleep disorders. Med. Clin. North Am.88, 1575–1591 (2004). xii. [DOI] [PubMed] [Google Scholar]
- 53.Mahajan, H. et al. Association of alcohol consumption and aortic calcification in healthy men aged 40–49 years for the ERA JUMP Study. Atherosclerosis268, 84–91 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smiley, A., King, D. & Bidulescu, A. The association between sleep duration and metabolic syndrome: The NHANES 2013/2014. Nutrients11, 2582 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang, S. W., Yang, H. F., Chen, Y. Y. & Chen, W. L. Unraveling the link between metabolic syndrome and abdominal aortic calcification. Nutr. Metab. Cardiovasc. Dis. NMCD31, 464–471 (2021). [DOI] [PubMed] [Google Scholar]
- 56.Agudelo, C. et al. Sleep duration is associated with subclinical carotid plaque burden. Stroke54, 2347–2355 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Patel, S. R. et al. Sleep duration and biomarkers of inflammation. Sleep32, 200–204 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vgontzas, A. N. et al. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: Role of sleep disturbance and obesity. J. Clin. Endocrinol. Metab.82, 1313–1316 (1997). [DOI] [PubMed] [Google Scholar]
- 59.Dowd, J. B., Goldman, N. & Weinstein, M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann. Epidemiol.21, 799–806 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grandner, M. A. et al. Extreme sleep durations and increased C-reactive protein: Effects of sex and ethnoracial group. Sleep36, 769–779E (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Düsing, P. et al. Vascular pathologies in chronic kidney disease: Pathophysiological mechanisms and novel therapeutic approaches. J. Mol. Med. Berl. Ger.99, 335–348 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seifert, M. E. et al. Effects of phosphate binder therapy on vascular stiffness in early stage chronic kidney disease. Am. J. Nephrol.38, 158–167 (2013). [DOI] [PMC free article] [PubMed]
- 63.Lioufas, N. et al. Can we IMPROVE cardiovascular outcomes through phosphate lowering in CKD? Rationale and protocol for the IMpact of phosphate reduction on vascular end-points in chronic kidney disease (IMPROVE-CKD) study. BMJ Open9, e024382 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang, Y. X., Tang, R. N., Wang, L. T. & Liu, B. C. Role of crosstalk between endothelial cells and smooth muscle cells in vascular calcification in chronic kidney disease. Cell Prolif.54, e12980 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Woodward, H. J., Zhu, D., Hadoke, P. W. F. & MacRae, V. E. Regulatory role of sex hormones in cardiovascular calcification. Int. J. Mol. Sci.22, 4620 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hernández-Pérez, J. G. et al. Association of sleep duration and quality with serum testosterone concentrations among men and women: NHANES 2011–2016. Andrology12, 518–526 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sharma, A. et al. Associations of endogenous sex hormone levels with the prevalence and progression of valvular and thoracic aortic calcification in the multi-ethnic study of atherosclerosis (MESA). Atherosclerosis341, 71–79 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Detailed NHANES study designs and data are available to the public at https://www.cdc.gov/nchs/nhanes/.