Abstract
In May-Thurner syndrome (MTS), the left iliac vein is compressed by the right iliac artery, leading to restricted blood flow from the leg to the heart. MTS commonly manifests in young females; however, its occurrence in older adults necessitates verifying the possibility of malignancy. A 77-year-old female experienced leg swelling and discomfort for 1 week. Computed tomography angiography suggested extensive thrombosis in the left iliac vein. Despite heparin treatment, the thrombus persisted and required mechanical thrombectomy, balloon venoplasty, and stent placement for tight iliac vein stenosis. The procedure was successful; however a biopsy of thrombus revealed malignant cells. An underlying malignancy and a hypercoagulable state were identified as the contributing factors after further evaluations. This case underscores the importance for vigilant diagnosis of hypercoagulable conditions and malignancies in MTS, emphasizing the role of malignancy in the development of DVT and MTS.
Keywords: May-Thurner syndrome, Deep vein thrombosis, Malignancy-associated deep vein thrombosis
INTRODUCTION
May-Thurner syndrome (MTS) is a vascular condition commonly affecting young or middle-aged females. It results from a compressed left common iliac vein between the lumbar spine and the right common iliac artery [1]. Its primary symptoms include pain, swelling, fatigue, varicose veins, skin discoloration, and left leg ulcers, which can lead to serious complications, such as deep vein thrombosis (DVT), chronic venous insufficiency, and pulmonary embolism in severe cases [2-4]. The incidence of DVT in MTS has been known to be approximately 2% to 5% [2]. In cases of DVT associated with MTS, although most cases developed without other risk factors except of MTS, clinicians should investigate additional causes, such as oral contraceptive use, prolonged hospitalization, and hidden malignancy [1].
Here, we describe a female patient with extensive DVT and tight stenosis of the left common iliac vein caused by an unrecognized malignancy. She underwent endovascular treatment, including thrombectomy and percutaneous balloon angioplasty with stent placement, to resolve thrombosis and stenosis and to ensure vascular patency. Malignant cells were identified in the thrombus upon histological examination. She underwent further imaging, including positron emission tomography-computed tomography (PET-CT). This DVT was associated with an underlying malignancy and MTS, necessitating further research into the various clinical manifestations of MTS.
The study was approved by the Institutional Review Board (IRB) of the Eulji University Uijeongbu Hospital (IRB No. UEMC 2024-04-002-003).
CASE
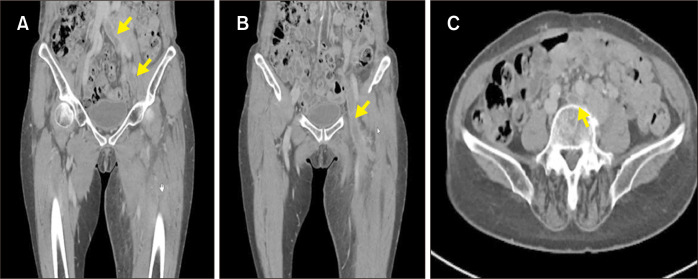
A 77-year-old female was admitted to the emergency department with complaints of swelling, pain, and erythema in her left leg that had commenced 1 week prior. CT venography revealed DVT extending from the left common iliac vein to the femoral and popliteal veins (Fig. 1). As the patient exhibited no symptoms suggestive of pulmonary embolism, a chest CT was not perfomed. Additionally, an electrocardiogram did not indicate atrial fibrillation, so no further tests were conducted. The patient had no history of prolonged hospitalization, smoking, or hyperlipidemia; however, tenderness was accompanied by swelling from her ankle to the proximal thigh. The patient received low-molecular-weight heparin, and based on the acute presentation of her symptoms within 2 weeks, intravascular thrombectomy and percutaneous transluminal angioplasty were planned.
Fig. 1.
Computed tomography scan for DVT with MTS indicated the extent of thrombus. (A) Arrows denotes thrombus in the left common and external iliac veins. (B) Arrow denotes thrombus in the left common femoral and femoral veins. (C) Arrow denotes thrombus in the left common iliac vein in axial image. DVT, deep vein thrombosis; MTS, May-Thurner syndrome.
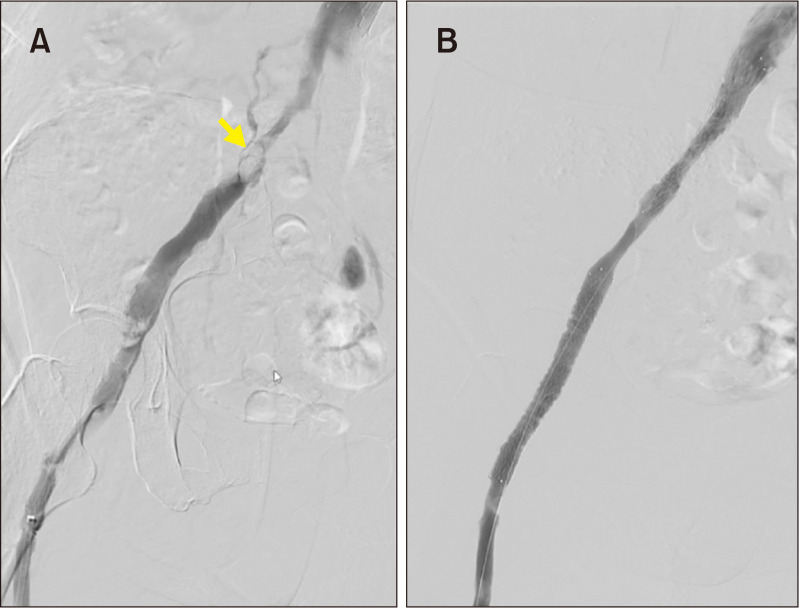
She was transferred to the operating room and positioned supine. After standard preparation, an inferior vena cava (IVC) filter (DenaliTM Vena Cava filter, BARD) was inserted through the right great saphenous vein into the infrarenal IVC under local anesthesia. The prone position ensured venous access through the left popliteal vein for thrombectomy. Venography confirmed complete occlusion of the left femoral, common femoral, and iliac veins, with thrombosis extending to the left common iliac vein. Prior to aspiration thrombectomy, 5 mg of actilyse mixed with 50 cc of normal saline was injected. Aspiration thrombectomy was conducted using a 7Fr Shuttle Sheath (Cook Medical) through 10Fr sheath (Terumo) via popliteal vein. Postprocedural venography confirmed thrombus removal and suggested external compression-induced constriction at the distal left common iliac vein (Fig. 2A). Transluminal balloon angioplasty (Mustang 10×80 mm, Boston Scientific) followed by stent placement (VenovoTM Stent 16×10 mm and 12×120 mm, BARD) from the left common iliac vein to the femoral vein was performed. Postprocedural venography confirmed restored venous flow (Fig. 2B). The access site was sealed with compression, and the procedure was considered successful.
Fig. 2.
Ascending venography was performed with contrast. (A) Arrow denotes severe compression of left common iliac vein in venogram performed before aspiration thrombectomy. (B) After thrombectomy and iliac vein stenting, venogram indicated complete resolution of iliac vein occlusion.
The patient received subcutaneous enoxaparin (1 mg/kg) twice daily for 3 days before discharge. The patient’s swelling and pain improved rapidly. Upon discharge, she was prescribed rivaroxaban 15 mg twice daily for 21 days with compression stocking, followed by 20 mg once daily, along with aspirin 100 mg daily. However, the pathologic examination of intraoperative thrombus suggested malignant tissues. Considering the patient’s age and result of pathologic examination, we investigated other causes for DVT in this patient. Additional imaging, including PET-CT and abdominal CT, revealed a hypermetabolic mass in the psoas muscle and hypermetabolic lymph nodes in the axilla (Fig. 3). Biopsies of these lesions were performed.
Fig. 3.
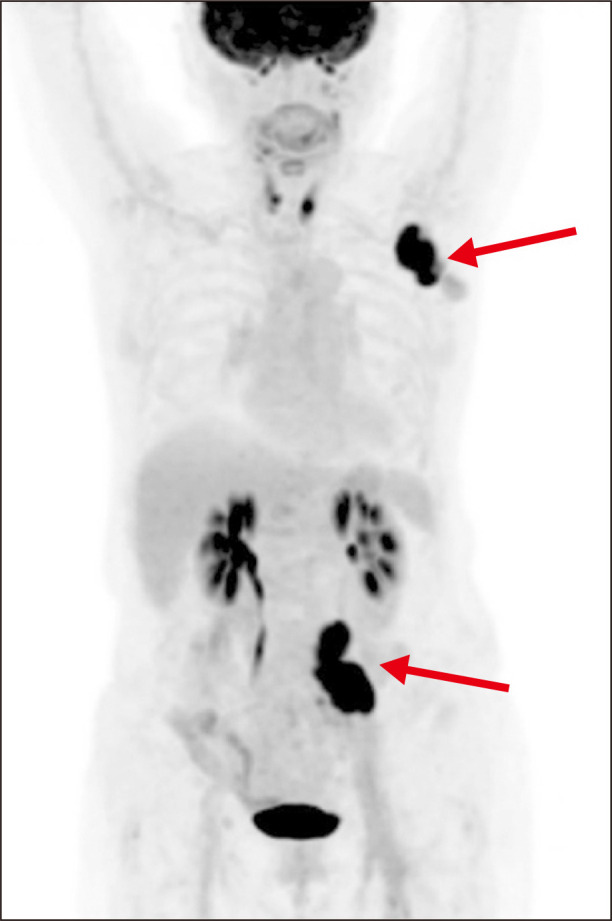
Positron emission tomography-computed tomography was performed after thrombectomy and iliac vein stenting. Red arrows showed uptake lesion of axilla and psoas muscle.
Four weeks later, a follow-up CT confirmed the patency of the iliac vein, and the IVC filter was removed. Two months later, duplex ultrasound indicated no DVT recurrence, and the left iliac vein stent remained patent. Biopsy results of the axillary and psoas muscle lesions confirmed metastatic adenocarcinoma, and the patient was referred to an oncologist for further management. Endoscopy was performed to identify the primary site of the cancer, but the source could not be determined. The patient subsequently started chemotherapy (5-FU) and radiation therapy.
DISCUSSION
This report describes the case of a 77-year-old female who developed MTS-induced DVT, accompanied by malignancy. Unlike typical MTS cases, which often occur in younger adults, this patient was an older and had unique risk factors such as vascular constriction and malignancy [5]. MTS-induced DVT has a high probability of recurrence because of structural constriction of the vascular lesion, despite anticoagulant use [6]. Approximately 70% of recurrences occur with angioplasty alone because of vein compression by the iliac artery. In our patient, given the external compression due to MTS and acute onset of thrombosis within 1 week, the patient underwent thrombectomy and stenting. MTS studies have demonstrated a 90% to 96% patency rate after 1 year of treatment [6-8]. In this case used a self-expanding stent, the VenovoTM Stent, specifically designed for veins, with an 88.3% stent patency rate at 1 year [1]. No consensus exists on the post-procedure use of anticoagulants or antiplatelet agents; however, the Korean insurance review standards prescribe rivaroxaban, warranting further research.
May-Thurner lesion was first identified in 1908 and is found in approximately 33% of the asymptomatic general population [9,10], with a prevalence of up to 66% in certain studies [11]. Despite their widespread prevalence, the rate of symptom manifestation is low, accounting for only 1% to 5% of the cases [12]. In the present case, unlike young females commonly affected by MTS, the patient was an older adult without any predisposing factors, such as a history of surgery, oral contraceptive use, atrial fibrillation, or prolonged immobility, which may induce a hypercoagulable state. This feature suggested a possibility of hidden malignancy as the underlying cause of MTS, which was confirmed by tissue examination of the thrombus. The present case underscores the importance of careful examination to identify potential causes, particularly malignancy, in elderly patients presenting with DVT and MTS. In addition, clinicians should consider that underlying malignancy with tumor invasion to the iliac vein can be a cause of DVT [13]. After aspiration thrombectomy, the specimen, including the thrombus, should be presented for pathological examination. The AngioJetTM device (Boston Scientific) is increasingly being used for DVT management. Unlike aspiration thrombectomy, the aspirated thrombus, after fragmentation by the AngioJetTM device, is collected in a bag during the procedure. While it seems reasonable to send the thrombus in the bag for pathological examination, there needs to be further discussion on how the specimen should be handled after using the AngioJetTM.
The present case is important because both iliac vein constriction and malignancy contributed to MTS. The patient did not exhibit any symptoms or signs of malignancy, such as weight loss or abdominal pain; however, she presented with sudden lower limb swelling and pain. The imaging performed before the surgery was CT angiography rather than abdominal pelvic CT, which made it difficult to directly identify the mass’s invasion into left iliac vein before the surgery, leading to treatment focused on MTS. However, the result was a case of MTS accompanied by tumor invasion, suggesting the importance of careful imaging and examination in older adult patients without predisposing factors.
In summary, this case illustrates the successful treatment of extensive thrombosis concomitant with serious underlying anatomical compression as well as a malignancy identified after endovascular treatment. MTS commonly manifests in young females; however, its occurrence in older adults necessitates verifying the possibility of thrombosis caused by malignancy, requiring further treatment. Therefore, to establish an appropriate treatment for MTS, clinicians should not only assess the acute or chronic symptoms but also examine the causes of thrombosis. Additionally, future investigations into the association among the causes of MTS, endovascular treatment types, and long-term patency rates could significantly improve the treatment. However, the patency and follow-up results after iliac vein stenting in cases with tumor invasion were not well-defined; therefore, further research is necessary.
ACKNOWLEDGEMENTS
The authors thank Dr. Sungil Park (Department of Radiology, Uijeongbu Eulji Medical Center, Eulji University, Uijeongbu, Korea) for his technical assistance with this study.
Funding Statement
FUNDING None.
Footnotes
CONFLICTS OF INTEREST
The authors have nothing to disclose.
AUTHOR CONTRIBUTIONS
Concept and design: CSS. Analysis and interpretation: CSS. Data collection: CSS. Writing the article: CSS. Critical revision of the article: JK, KCY. Final approval of the article: KCY. Statistical analysis: none. Obtained funding: none. Overall responsibility: KCY.
REFERENCES
- 1.Radaideh Q, Patel NM, Shammas NW. Iliac vein compression: epidemiology, diagnosis and treatment. Vasc Health Risk Manag. 2019;15:115–122. doi: 10.2147/VHRM.S203349. https://doi.org/10.2147/vhrm.s203349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu D, Peterson E, Dooner J, Baerlocher M, Zypchen L, Gagnon J, et al. Interdisciplinary Expert Panel on Iliofemoral Deep Vein Thrombosis (InterEPID), author Diagnosis and management of iliofemoral deep vein thrombosis: clinical practice guideline. CMAJ. 2015;187:1288–1296. doi: 10.1503/cmaj.141614. https://doi.org/10.1503/cmaj.141614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh A, Zahra F. In: StatPearls. Aboubakr S, Abu-Ghosh A, Adibi Sedeh P, Aeby TC, Aeddula NR, Agadi S, et al., editors. StatPearls Publishing; 2024. Chronic venous insufficiency. [Google Scholar]
- 4.Mangla A, Hamad H. In: StatPearls. Aboubakr S, Abu-Ghosh A, Adibi Sedeh P, Aeby TC, Aeddula NR, Agadi S, et al., editors. StatPearls Publishing; 2024. May-Thurner syndrome. [Google Scholar]
- 5.MacDowell CJ, Idzikowski E, Saifuddin A, Kang F. Endovascular resolution of complete common iliac vein stenosis in a case of May-Thurner syndrome with underlying malignancy. Int J Surg Case Rep. 2023;112:108987. doi: 10.1016/j.ijscr.2023.108987. https://doi.org/10.1016/j.ijscr.2023.108987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mickley V, Schwagierek R, Rilinger N, Görich J, Sunder-Plassmann L. Left iliac venous thrombosis caused by venous spur: treatment with thrombectomy and stent implantation. J Vasc Surg. 1998;28:492–497. doi: 10.1016/S0741-5214(98)70135-1. https://doi.org/10.1016/s0741-5214(98)70135-1. [DOI] [PubMed] [Google Scholar]
- 7.Rossi FH, Kambara AM, Izukawa NM, Rodrigues TO, Rossi CB, Sousa AG, et al. Randomized double-blinded study comparing medical treatment versus iliac vein stenting in chronic venous disease. J Vasc Surg Venous Lymphat Disord. 2018;6:183–191. doi: 10.1016/j.jvsv.2017.11.003. https://doi.org/10.1016/j.jvsv.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 8.O'Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000;11:823–836. doi: 10.1016/S1051-0443(07)61796-5. https://doi.org/10.1016/s1051-0443(07)61796-5. [DOI] [PubMed] [Google Scholar]
- 9.May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8:419–427. doi: 10.1177/000331975700800505. https://doi.org/10.1177/000331975700800505. [DOI] [PubMed] [Google Scholar]
- 10.Negus D, Fletcher EW, Cockett FB, Thomas ML. Compression and band formation at the mouth of the left common iliac vein. Br J Surg. 1968;55:369–374. doi: 10.1002/bjs.1800550510. https://doi.org/10.1002/bjs.1800550510. [DOI] [PubMed] [Google Scholar]
- 11.Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39:937–943. doi: 10.1016/j.jvs.2003.12.032. https://doi.org/10.1016/j.jvs.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 12.Taheri SA, Williams J, Powell S, Cullen J, Peer R, Nowakowski P, et al. Iliocaval compression syndrome. Am J Surg. 1987;154:169–172. doi: 10.1016/0002-9610(87)90172-3. https://doi.org/10.1016/0002-9610(87)90172-3. [DOI] [PubMed] [Google Scholar]
- 13.Thangjui S, Trongtorsak A, Zoltick JM, Doyle A. May-Thurner syndrome in an elderly man. Cureus. 2022;14:e21611. doi: 10.7759/cureus.21611. https://doi.org/10.7759/cureus.21611. [DOI] [PMC free article] [PubMed] [Google Scholar]