Abstract
Objective
Insufficient or prolonged sleep each day may contribute to the onset of cardiovascular disease and diabetes, and there may be some variability between genders; however, current research evidence is limited. We aimed to investigate the effects of gender on self-reported sleep duration and the prevalence of cardiovascular disease and diabetes.
Research design and methods
This study is a population-based, cross-sectional analysis. Data from a nationally representative sample of US adults obtained from the National Health and Nutrition Examination Survey (NHANES) (2005–2020), and 13,002 participants, including 6,774men and 6,228women, were obtained by excluding the missing values for each variable self-reported sleep duration data obtained by using a habitual baseline questionnaire. Logistic regression models investigated the associations between gender-specific self-reported sleep duration, CVDs, and diabetes events.
Result
In all participants, respectively, compared with sleep 7–8 h/day, the multivariable-adjusted odds ratios significantly associated with < 7 h /day and > 8 h /day were (1.43[1.15, 1.78]) and (1.34[1.01, 1.76]) for CHF, (1.62[1.28, 2.06]) for Angina, (1.42[1.17, 1.71]) for heart attack, (1.38[1.13, 1.70]) and (1.54[1.20, 1.97]) for Stroke, (1.21[1.09, 1.35]) and (1.28[1.11, 1.48]) for diabetes. In men, CHF (1.67[1.21, 2.14]), Angina (1.66[1.18, 2.15]), Stroke (1.55[1.13,1.97]), and diabetes (1.15[1.00, 1.32]) were significantly associated with < 7 h /day, and stroke (1.73[1.16, 2.32]) and diabetes (1.32[1.06, 1.52]) were significantly associated with > 8 h /day. In women, angina(1.83[1.16, 2.50]), heart attack(1.63[1.11, 2.15]), and diabetes (1.32[1.11, 1.54]) were significantly associated with < 7 h /day, while diabetes (1.31[1.03, 1.59]) was significantly associated with > 8 h /day.
Conclusion
Self-reported long and short sleep duration was independently associated with partial CVDs and diabetes risk. However, sleep duration and gender did not have multiplicative or additive interactions with the onset of diabetes and CVDs.
Keywords: Diabetes, Cardiovascular disease, Gender, Sleep, Regression
Introduction
It has been widely recognized that sleep is closely related to health, that sleep is necessary for the performance of emotional and physical functions, and that good quality sleep can help the body maintain a high level of energy in daily activities [1, 2]. The American Academy of Sleep Medicine (AASM) and the Society for Sleep Research (SRS) recommend that adults should aim for an optimal self-reported sleep duration of 7–8 h per night [3, 4]. However, recent epidemiological analysis indicates that nearly two-fifths of American adults sleep less than seven hours per night, with only 45% achieving the recommended amount [5].
Gender encompasses biological and sociocultural aspects that differentiate individuals in terms of their constitution, identity, roles, behaviors, and expressions. Recent studies have indicated that inadequate sleep is associated with an increased risk of cardiovascular disease and diabetes [6, 7]. Moreover, studies have shown disparities in the risk of cardiovascular disease and diabetes between men and women. Therefore, further investigation is warranted to determine whether divergent sleep patterns between genders affact susceptibility to cardiovascular disease and diabetes [8, 9]. However, limited research has explored the specific association between self-reported sleep duration and these conditions, particularly in relation to gender-specific differences.
Consequently, we conducted this study using data from the US National Health and Nutrition Examination Survey (NHANES) conducted between 2005 and 2020. This study aimed to examine the relationship between self-reported sleep duration and the risk of cardiovascular disease and diabetes, while also considering the potential gender differences in this association.
Materials and methos
Study design and sample
The National Center for Health Statistics (NCHS) is an ongoing national survey of the health and nutritional status of the general American population. The NCHS Institutional Review Committee approved the NHANES research plan, and all participants provided written informed consent. This study is a population-based, cross-sectional analysis. Data from a nationally representative sample of US adults was obtained from the National Health and Nutrition Examination Survey (NHANES)(2005–2020).
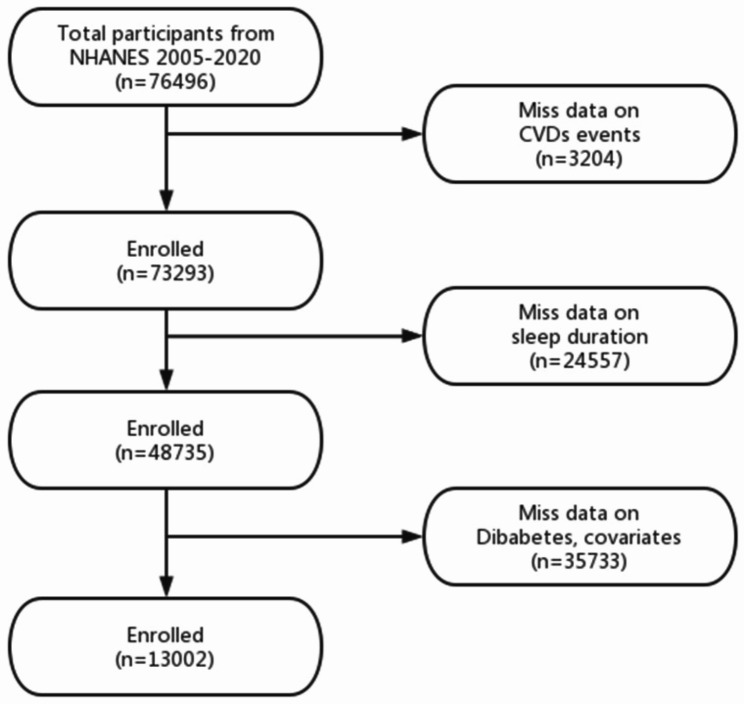
In this study, we excluded participants who did not participate in the recording of cardiovascular disease content (n = 3204), those who did not record self-reported sleep duration (n = 24557), and those who did not record diabetes, covariates, and content data loss (n = 35733). Finally, 13,002 participants were included in this study (Fig. 1).
Fig. 1.
Flow chart of sample selection
Cardiovascular disease: outcome
During the personal interviews, a standardized health questionnaire was used to assess various health problems, including heart failure, coronary heart disease, angina pectoris, heart attack, and stroke. “Have doctors or other health professionals ever informed you that you suffer from heart failure/coronary heart disease/angina pectoris/heart disease/stroke?” It was a question for the participants (this was a group of five questions with exact wording). If participants answer “Yes” to any previous questions, these questions will be classified as CVD cases.
Measurement of diabetes
Diabetes status groups were defined as follows: diabetes self-report of a physician or health care professional diagnosis, fasting blood glucose > 7 mmol/L, or HbA1c ≥ 6.5%, confirmed as diabetes.
Self-reported sleep duration
The definition was based on the “sleep disorders” data in the “NHANES Questionnaire.” Question SLQ012 asked, “Number of hours usually sleep on weekdays or workdays.” The participants answered regarding their self-reported sleep duration and hours rounded to the nearest half-hour. Self-reported sleep duration analysis is both a continuous and a categorical variable. Self-reported sleep duration was classified into three groups: self-reported sleep duration < 7 h/day, 7 h/day ≤ self-reported sleep duration ≤ 8 h/day, and 8 h/day < self-reported sleep duration. The reference average self-reported sleep duration was 7–8 h/day (“short” self-reported sleep duration: <7 h/day; “long” self-reported sleep duration: >8 h/day.
Covariates
According to the statement on the NHANES website, all research centers collected data from trained personnel using standardized procedures. Demographic characteristics included age(years), gender (male, female), race(American Mexican American,
Other Hispanic, non-Hispanic white, non-Hispanic black, and other races), chronic diseases included (hypertension and high cholesterol), lifestyle behavior(drinking and smoking), and examination data (BMI). Gender is defined as gender identity.
Chronic diseases were assessed using self-reported medical history, and participants were asked if a doctor or other health professional told them to have a specific health condition, including hypertension (yes or no) and high cholesterol (yes or no). Participants were asked, ‘Do you smoke every day now?’ If the participants answer “Yes,” they are classified as smokers. Similarly, participants were asked,’ Have you ever drunk 4/5 or more alcohol every day?’ If participants answer “Yes,” they are classified as drinkers. Body mass index calculated in kilograms per square meter (kg/m2).
The study employed logistic regression models to adjust for confounding variables such as age, race, gender, BMI, alcohol consumption, diabetes, smoking, and hypertension to examine the overall associations between self-reported sleep duration and CVDs risk.
Statistical analysis
The extraction and merging of NHANES data from 2005 to 2020 used R Studio (version 4.2.2). All analyses used SPSS version 26.0 (IBM Corporation, Armonk, New York, USA) [10].
Non-normally distributed continuous variables are expressed as medians and quartiles and compared using nonparametric tests. For categorical variables, frequencies and percentages were reported, and the chi-square test was used for comparison. The association between Baseline self-reported sleep duration (< 7 h/day and > 8 h/day) and the risk of CHF, CHD, Angina, Heart attack, Stroke, and Diabetes was examined using a logistic regression risk model, with 7–8 h/day serving as the reference odds ratios(ORs) with 95% confidence intervals (CIs) were estimated from the model after adjusting for confounders. Adjusted confounders included age, race, BMI, drinker, smoker, and hypertension.
Multiplicative interaction analysis using a logistic regression model, additive interaction analysis using R Studio, the relative excess risk of interaction (RERI), the attributable proportion of interaction (AP), and the Synergy Index (SI) were calculated. The 95% CI of RERI and AP did not contain 0, the 95% CI of Si did not contain 1, and the two-sided P < 0.05 was statistically significant.
Patient and public involvement statement
Collecting, collating, and analyzing sample data from the NHANES database completed this study. While the NHANES database has been collecting patient information, the findings from this survey will be used to determine the prevalence of major diseases and their risk factors. This information can be used to assess nutritional status and its association with health promotion and disease prevention. NHANES findings are also the basis for national measurement standards, such as height, weight, and blood pressure. Epidemiological studies and health sciences research will use data from this survey to help develop sound public health policies, direct and design health programs and services, and expand national health knowledge.
Result
Baseline characteristics
Of the 13,002 participants (6774 men and 6228 women) shown in Tables 1 and 33.76%, 53.42%, and 12.81% reported sleeping < 7, 7–8 and > 8 h/day, respectively. The mean age of eligible participants was 51 ± 13.13 years; women comprised 47.9% of the study population. BMI was available for all participants, and the mean BMI was 29.49 ± 7.16. Self-reported sleep duration identified significant gender differences: women seemed to sleep more than men. Additionally, men had a higher prevalence of diabetes and cardiovascular disease, higher rates of alcohol consumption and smoking, higher cholesterol levels, and lower obesity (Tables 1 and 2).
Table 1.
Baseline characteristics of participants by different sexes
| Total (13002) | Male (6774) | Female (6228) | P-value | |
|---|---|---|---|---|
|
Age, Median(q1-q3) |
51.00(37.00–65.00) | 52.00(38.00–65.00) | 50.00(36.00–63.00) | < 0.001 |
|
BMI, Median(q1-q3) |
28.30(24.60-32.96) | 28.10(24.90–31.90) | 28.67(24.23–34.20) | < 0.001 |
| Race(%) | < 0.01 | |||
| Mecican American | 1685(13.0) | 903(13.3) | 782(12.6) | |
| Other Hispanic | 1276(9.8) | 660(9.7) | 616(9.9) | |
| Non-Hispanic white | 5902(45.4) | 3079(45.5) | 2823(45.3) | |
| Non-Hispanic black | 2785(21.4) | 1376(20.3) | 1409(22.6) | |
| Other race | 1354(10.4) | 756(11.2) | 598(9.6) | |
| Drinking(%) | < 0.001 | |||
| Yes | 2115(16.3) | 1575(23.3) | 540(8.7) | |
| No | 10,887(83.7) | 5199(76.7) | 5688(91.3) | |
| Smoking(%) | ||||
| Yes | 6477(49.8) | 3847(56.8) | 2630(42.2) | < 0.001 |
| No | 6525(50.2) | 2927(43.2) | 3598(57.8) | |
| Hypertension(%) | = 0.15 | |||
| Yes | 5108(39.3) | 2701(39.9) | 2407(38.6) | |
| No | 7894(60.7) | 4073(60.1) | 3821(61.4) | |
| High cholesterol(%) | < 0.01 | |||
| Yes | 5004(38.5) | 2692(39.7) | 2312(37.1) | |
| No | 7998(61.5) | 4082(60.3) | 3916(61.9) | |
| Sleep duration(%) | < 0.001 | |||
| < 7 h/day | 4390(33.8) | 2389(35.3) | 2001(32.1) | |
| 7–8 h/day | 6946(53.5) | 3596(50.1) | 3350(52.8) | |
| > 8 h/day | 1666(12.8) | 789(11.6) | 877(14.1) |
Abbreviations: NHANES: National Health and Nutrition Examination Survey; BMI: Body mass index; CHF: Congestive heart failure; CHD: Coronary heart disease
P- value for difference between males and females, compared by Non-parametric test for Non-normally distributed continuous variable and chi- squared test for categorical variables, p < 0.05 identifies statistical significance
Table 2.
Outcome characteristics of participants by different sexes
| Total(13002) | Male(6774) | Female(6228) | P-value | |
|---|---|---|---|---|
| CHF(%) | < 0.01 | |||
| Yes | 451(3.5) | 267(3.9) | 184(3.0) | |
| No | 12,551(96.5) | 6507(96.1) | 6044(97.0) | |
| CHD(%) | < 0.001 | |||
| Yes | 598(4.6) | 446(6.6) | 152(2.4) | |
| No | 12,404(95.4) | 6328(93.4) | 6076(97.6) | |
| Angina(%) | < 0.001 | |||
| Yes | 370(2.8) | 231(3.4) | 139(2.2) | |
| No | 12,632(97.2) | 6543(96.6) | 6089(97.8) | |
| Heart attact(%) | < 0.001 | |||
| Yes | 617(4.7) | 424(6.3) | 193(3.1) | |
| No | 12,385(95.3) | 6350(93.7) | 6035(96.9) | |
| Stroke(%) | = 0.3 | |||
| Yes | 535(4.1) | 289(4.3) | 246(3.9) | |
| No | 12,467(95.9) | 6485(95.7) | 5982(96.1) | |
| Diabetes(%) | < 0.001 | |||
| Yes | 2502(19.2) | 1458(21.5) | 1044(16.8) | |
| No | 10,500(80.8) | 5316(78.5) | 5184(83.2) |
Abbreviations: CHF: Congestive heart failure; CHD: Coronary heart disease
P-value for difference between males and females, compared by Non-parametric test for Non-normally distributed continuous variable and chi- squared test for categorical variables, p < 0.05 identifies statistical significance
Overall and gender-specific associations between self-reported sleep duration and CVDs risk
Findings revealed that self-reported sleep durations of less than 7 h/day were associated with statistically significant increased risks for all CVDs, except CHD, compared to the reference group of 7–8 h of sleep. The adjusted odds ratios (ORs) for incident CVDs were as follows: (1.43 [1.15, 1.78]) for CHF, (1.62 ([1.28, 2.06]) for angina, (1.42 [1.17, 1.71]) for heart attack, and (1.38 [1.13, 1.70]) for stroke. Self-reported sleep durations exceeding 8 h/day were associated with a 34% higher risk of CHF (1.34 [1.01, 1.76]) and a 54% higher risk of stroke (1.54 [1.20, 1.97]). According to the self-reported sleep duration, there was a U-shaped relationship between CVDs and long sleep duration and short sleep duration (Table 3).
Table 3.
Overall association of sleep duration and CVDs and diabetes
| Disease events | Sleep duration(h/day) | ||
|---|---|---|---|
| < 7 h/day | 7–8 h/day | > 8 h/day | |
| CHF | |||
| OR(95%CI) | 1.43(1.15–1.78) | 1.00(1.00–1.00) | 1.34(1.01–1.76) |
| P-value | < 0.001 | < 0.05 | |
| CHD | |||
| OR(95%CI) | 1.17(0.96–1.42) | 1.00(1.00–1.00) | 1.07(0.84–1.38) |
| P-value | = 0.12 | = 0.5 | |
| Angina | |||
| OR(95%CI) | 1.62(1.28–2.06) | 1.00(1.00–1.00) | 1.24(0.91–1.70) |
| P-Value | < 0.001 | = 0.17 | |
| Heart attact | |||
| OR(95%CI) | 1.42(1.17–1.71) | 1.00(1.00–1.00) | 1.17(0.91–1.50) |
| P-value | < 0.001 | = 0.2 | |
| Stroke | |||
| OR(95%CI) | 1.38(1.13–1.70) | 1.00(1.00–1.00) | 1.54(1.20–1.97) |
| P-value | < 0.01 | < 0.001 | |
| Diabetes | |||
| OR(95%CI) | 1.21(1.09–1.35) | 1.00(1.00–1.00) | 1.28(1.11–1.48) |
| P-value | < 0.001 | < 0.001 | |
Abbreviations: CHF: Congestive heart failure; CHD: Coronary heart disease; OR: Odds radio; CI: confidence interval
CVDs models adjusted for age, race, gender BMI, drinker, smoker, diabetes and hypertension
Diabetes model adjusted for age, race, gender BMI, drinker, smoker, and hypertension
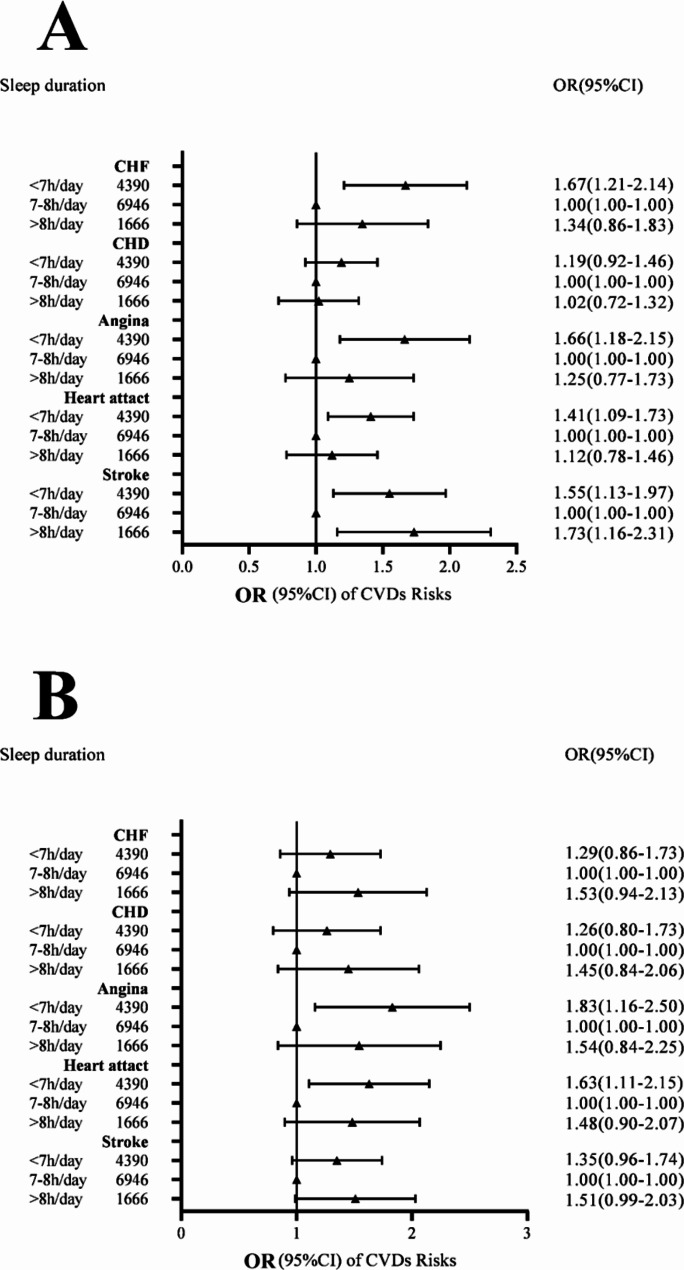
Figure 2 presents the gender-specific associations between self-reported sleep duration and CVDs. Among women, self-reported sleep durations of less than 7 h/day were associated with an 84% higher risk of angina (1.83 [1.16, 2.50]) and a 63% higher risk of heart attack (1.63 [1.11, 2.15]) than the reference group of 7–8 h/day. Conversely, among men, self-reported sleep durations of less than 7 h/day were associated with an increased risk of CHF (1.67 [1.21, 2.14]), angina (1.66 [1.18, 2.15]), heart attack (1.41 [1.09, 1.73]), and stroke (1.55 [1.13, 1.90]). Additionally, self-reported sleep durations exceeding 8 h/day were associated with an increased risk of stroke (1.73 [1.16, 2.31]) (Fig. 2).
Fig. 2.
Sex-specific association between sleep duration and CVDs risk. (A) Male; (B) Female. Models adjusted for age, race, BMI, drinker, smoker, and hypertension. The points represent the adjusted OR, and the lines represent its 95% confidence interval (95% CI)
Overall and gender-specific associations between self-reported sleep duration and diabetes risk
The adjusted odds ratios (ORs) for incident diabetes, compared to sleeping for 7 h/day, were 1.21 (95% CI 1.09, 1.35) for self-reported sleep durations less than 7 h/day and 1.28 (95% CI 1.11, 1.48) for self-reported sleep durations exceeding 8 h/day. According to the self-reported sleep duration, there was a U-shaped relationship between diabetes and long and short sleep duration (Table 3).
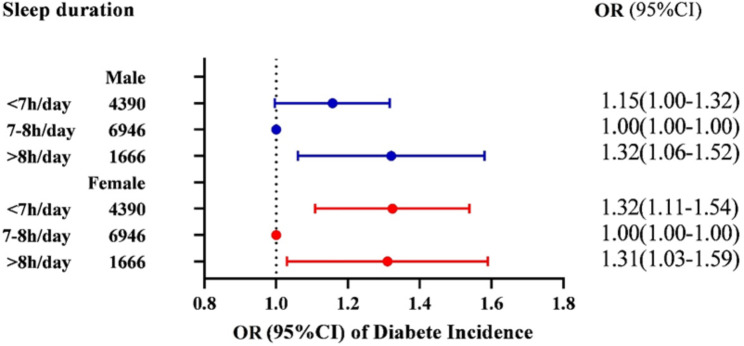
Figure 3 illustrates the sex-specific associations between self-reported sleep duration and diabetes. Both men and women demonstrated increased risks of diabetes for self-reported sleep durations less than 7 h/day and greater than 8 h/day, compared to the reference group of 7–8 h/day. When self-reported sleep duration was less than 7 h/day, the risk of diabetes increased by 15% in men and 32% in women. Moreover, self-reported sleep durations exceeding 8 h/day were associated with a 32% higher risk of diabetes in men (1.32 [1.11, 1.54]) and a 31% higher risk in women (1.31 [1.03, 1.59])(Fig. 3).
Fig. 3.
Sex-specific association between sleep duration and Diabetes. Blue and red boxes represent males and females respectively. Models adjusted for age, race, BMI, drinker, smoker, and hypertension. The points represent the adjusted OR, and the lines represent its 95% confidence interval (95% CI)
Analysis of interaction of gender and sleep duration on CVDs and diabetes
The logistic regression model and Rstudio included the product of gender and sleep duration for multiplicative interaction analysis and additive interaction analysis. After adjusting for other relevant factors such as age, race, gender, BMI, drinker, smoker, and hypertension, no multiplicative interaction and additive interaction were found between gender and sleep duration (Tables 4 and 5).
Table 4.
Multiplicative interaction of gender and sleep duration on CVDs and diabetes
| Disease events | Gender | Sleep duration | Gender*Sleep duration |
|---|---|---|---|
| CHF | |||
| Wald X² | 2.83 | 6.42 | 0.19 |
| P-value | = 0.09 | < 0.01 | = 0.66 |
| OR(95%CI) | 1.28(0.96–1.71) | 1.46(1.09–1.97) | 1.09(0.74–1.60) |
| CHD | |||
| Wald X² | 63.75 | 0.90 | 0.18 |
| P-value | < 0.01 | = 0.34 | = 0.67 |
| OR(95%CI) | 2.93(2.25–3.81) | 1.17(0.85–1.61) | 0.92(0.63–1.34) |
| Angina | |||
| Wald X² | 9.23 | 8.16 | 0.33 |
| P-value | < 0.01 | < 0.01 | = 0.57 |
| OR(95%CI) | 1.66(1.19–2.29) | 1.64(1.17–2.31) | 0.88(0.57–1.36) |
| Heart attact | |||
| Wald X² | 38.65 | 8.33 | 0.83 |
| P-value | < 0.001 | < 0.01 | = 0.36 |
| OR(95%CI) | 2.28(1.76–2.95) | 1.53(1.15–2.04) | 0.85(0.60–1.21) |
| Stroke | |||
| Wald X² | 0.02 | 6.97 | 0.92 |
| P-value | = 0.88 | < 0.01 | = 0.34 |
| OR(95%CI) | 0.98(0.75–1.27) | 1.41(1.09–1.82) | 1.19(0.83–1.68) |
| Diabete | |||
| Wald X² | 31.467 | 29.11 | 1.44 |
| P-value | < 0.001 | < 0.001 | = 0.23 |
| OR(95%CI) | 1.44(1.27–1.63) | 1.44(1.26–1.65) | 0.90(0.75–1.07) |
Abbreviations: CHF: Congestive heart failure; CHD: Coronary heart disease; OR: Odds radio; CI: confidence interval
Table 5.
Additive interaction of gender and sleep duration on CVDs and diabetes
| Disease events | OR | 95%CI | RERI | 95%CI | AP | 95%CI | SI | 95%CI |
|---|---|---|---|---|---|---|---|---|
| CHF | 2.04 | 1.56–2.67 | 0.30 | -0.21-0.80 | 0.14 | -0.10-0.39 | 1.40 | 0.70–2.80 |
| CHD | 3.16 | 2.43–4.11 | 0.06 | -0.79-0.91 | 0.02 | -0.25-0.29 | 1.03 | 0.69–1.54 |
| Angina | 2.40 | 1.75–3.29 | 0.10 | -0.58-0.78 | 0.04 | -0.24-0.33 | 1.08 | 0.64–1.82 |
| Heart attact | 2.96 | 2.29–3.82 | 0.15 | -0.52-0.83 | 0.05 | -0.17-0.28 | 1.09 | 0.75–1.57 |
| Stroke | 1.64 | 1.29–2.09 | 0.25 | -0.17-0.68 | 0.15 | -0.10-0.41 | 1.64 | 0.54–4.95 |
| Diabete | 1.86 | 1.64–2.11 | -0.02 | -0.29-0.25 | -0.01 | -0.16-0.14 | 0.98 | 0.72–1.34 |
Abbreviations: CHF: Congestive heart failure; CHD: Coronary heart disease; OR: Odds radio; CI: confidence interval; RERI: Relative excess risk of interaction; AP: Attributable proportion of interaction; SI: Synergy Index
Discussion
Overall, after adjusting for potential confounders, our study revealed a U-shaped relationship between self-reported sleep duration and CVDs and diabetes such that minimum risk was associated with a sleep duration of 7–8 h in a large US population. Participants with shorter self-reported sleep durations had a higher risk of cardiovascular disease and diabetes than those with optimal self-reported sleep duration. After grouping the participants by gender, we observed a stronger association between self-reported sleep duration and cardiovascular events in male participants, with significant increases in the risk of CHF, Angina, Heart attack, and stroke. Among the female participants, shorter self-reported sleep duration was significantly associated with an increased risk of Angina and Heart attack. However, no significant association was found between longer self-reported sleep duration and cardiovascular disease in women, except for stroke in men.
Previous studies have reported associations between self-reported sleep duration and cardiovascular disease and diabetes, supporting our findings [11–13]. For instance, a recent study found that shorter self-reported sleep duration increased the prevalence of various cardiovascular diseases [14, 15]. Another study conducted in China reported an increased risk of cardiovascular mortality with both very short (< 4 h/day) and very long (> 10 h/day) self-reported sleep durations [16]. These findings are consistent with our study, which identified similar associations between different self-reported sleep durations and the risk of cardiovascular disease and diabetes [17, 18]. Various mechanisms have been proposed to explain the relationship between self-reported sleep duration and the development of diabetes and cardiovascular disease. Prolonged sleep has been linked to insulin resistance and decreased insulin sensitivity, leading to endocrine and metabolic disorders and elevated blood sugar levels, which ultimately contribute to the development of diabetes. Moreover, long-term hyperglycemia resulting from diabetes can lead to organ damage and vascular complications, becoming a significant risk factor for cardiovascular disease [19–22]. Other potential mechanisms include hyperactivation of the sympathetic nervous system during inadequate sleep, increased oxidative stress, and direct damage to the cardiovascular system [23, 24]. Further research is needed to explore and establish the underlying mechanisms connecting self-reported sleep duration with diabetes and cardiovascular disease.
Previous studies have identified gender-related differences in the risk of cardiovascular disease and diabetes, although the impact of self-reported sleep duration on these differences remains largely unexplored. Our study did not observe a significant association between longer self-reported sleep durations and cardiovascular disease in women. However, we found that longer self-reported sleep duration was significantly associated with stroke in men. We hypothesized that the differential association between the effects of shorter or longer sleep duration in men and women might be due to the lack of statistical significance due to the lack of an adequate sample size. We also found that self-reported sleep duration (< 7 h/day and > 8 h/day) was associated with an increased risk of diabetes in both men and women. Other studies have shown that women are more likely than men to have diabetes, and more women with diabetes are more likely to develop cardiovascular diseases, such as atrial fibrillation and coronary heart disease [8, 14, 25]. Potential contributing factors include the influence of female gender hormones, metabolic conditions, and a higher prevalence of dyslipidemia among women, which may affect the association between self-reported sleep duration, gender, cardiovascular disease, and diabetes [26, 27]. Further analysis of the interaction between gender and self-reported sleep duration revealed that there was neither additive interaction nor multiplicative interaction between the two for diabetes and CVDs; this suggests that the two factors do not have a synergistic effect on the development of CVDs and diabetes, and a literature search revealed that there are few reports of such studies.
Conclusions
In conclusion, our study highlights the gender-specific association between self-reported sleep duration, diabetes, and cardiovascular disease. For men, the shorter the self-reported sleep duration, the higher the risk of heart failure, angina, heart disease, and stroke, and the longer the self-reported sleep duration, the higher the risk of stroke. In women, the shorter the self-reported sleep duration, the higher the risk of angina and heart disease. In addition, self-reported sleep duration (< 7 h/day and > 8 h/day) was significantly associated with diabetes in both men and women. However, self-reported sleep duration and gender had neither additive nor multiplicative interaction on diabetes and CVDs. Further studies are needed to validate these findings and elucidate the mechanisms underlying these associations.
Strengths and limitations of this study
Strengths
First, it utilized the NHANES database, a nationally representative, large-sample survey, to ensure robust data collection criteria. Second, this is the first study to examine the association between self-reported sleep duration and cardiovascular disease and diabetes in a gender-diverse population in the United States using a large sample size. Finally, the study accounted for relevant confounders in the analysis, thus enhancing the validity of the results.
Limitations
First, there was a possibility of residual confounding due to unmeasured or unknown factors such as the use of psychotropic medications, which may lead to increased sleep duration, but as this was not the primary objective of this study, it was not taken into account. Second, the study’s cross-sectional nature limits our ability to establish causality, necessitating further longitudinal investigations. Third, respiratory diseases such as obstructive sleep apnea can affect sleep quality, which is also a risk factor for cardiovascular disease. Finally, this study did not consider the effect of sleep quality. The outcomes are self-reported, which can potentially lead to either misclassification or misclassification bias, where this misclassification of the outcomes depends on the sleep status, and this study limits the sample to a person with no missing variables and therefore creates a possible biased effect.
Acknowledgements
I would like to take this opportunity to thank many people who have offered invaluable assistance in the study. My deepest gratitude goes first and foremost to Professor Xue Rui, who has guided me through all the stages of the writing of this thesis. Her critical comments, constant encouragement and guidance have greatly enlightened me not only on the academic pursuit but also on the morals of being a doctor. Secondly, I would like to thank all my colleagues who participated in this study, which was completed with the joint efforts of everyone. Finally, I would like to thank my girlfriend and my family, in the study of the road they have been without hesitation to support me.
Author contributions
Material preparation and data collection were performed by CYF, YGQ, HT and CYM. Data analysis was performed byCYF. The first draft of the manuscript was written by CYF, article review provided by XR, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.All authors contributed to the study’s conception and design.
Funding
Hubei Province Science and technology Department key research and development plan(Grant No.2022BCE007);National Natural Science Foundation of China, (81701891)
Data availability
Research data supporting this publication are available from the NN repository located at www.cdc.gov/nchs/nhanes/index.htm.
Declarations
Ethics approval and consent to participate
The NHANES research plan was approved by the NCHS Institutional Review Committee and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mallah MA, Changxing L, Mallah MA, Naveed M, Liu Y, Noreen S, et al. Association of urinary polycyclic aromatic hydrocarbon metabolites and cardiovascular disease among US population: a cross-sectional study. Environ Res. 2022;209:112775. [DOI] [PubMed] [Google Scholar]
- 2.Thosar SS, Butler MP, Shea SA. Role of the circadian system in cardiovascular disease. J Clin Invest. 2018;128(6):2157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li J, Guo L. Association between sleep duration and albumin in US adults: a cross-sectional study of NHANES 2015–2018. BMC Public Health. 2022;22(1):1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang C, Bangdiwala SI, Rangarajan S, Lear SA, AlHabib KF, Mohan V, et al. Association of estimated sleep duration and naps with mortality and cardiovascular events: a study of 116 632 people from 21 countries. Eur Heart J. 2019;40(20):1620–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Svensson T, Saito E, Svensson AK, Melander O, Orho-Melander M, Mimura M, et al. Association of Sleep Duration with All- and major-cause mortality among adults in Japan, China, Singapore, and Korea. JAMA Netw Open. 2021;4(9):e2122837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peters SAE, Woodward M. Sex and gender matter in cardiovascular disease and beyond. Heart. 2022;108(13):994–5. [DOI] [PubMed] [Google Scholar]
- 7.Liu L, Miura K, Kadota A, Fujiyoshi A, Gracely EJ, Xue F, et al. The impact of sex on risk of cardiovascular disease and all-cause mortality in adults with or without diabetes mellitus: a comparison between the U.S. and Japan. J Diabetes Complications. 2019;33(6):417–23. [DOI] [PubMed] [Google Scholar]
- 8.Bisson A, Bodin A, Fauchier G, Herbert J, Angoulvant D, Ducluzeau PH, et al. Sex, age, type of diabetes and incidence of atrial fibrillation in patients with diabetes mellitus: a nationwide analysis. Cardiovasc Diabetol. 2021;20(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connelly PJ, Azizi Z, Alipour P, Delles C, Pilote L, Raparelli V. The importance of gender to Understand Sex differences in Cardiovascular Disease. Can J Cardiol. 2021;37(5):699–710. [DOI] [PubMed] [Google Scholar]
- 10.Deng MG, Liu F, Liang Y, Chen Y, Nie JQ, Chai C, et al. Associations of serum zinc, copper, and selenium with sleep disorders in the American adults: data from NHANES 2011–2016. J Affect Disord. 2023;323:378–85. [DOI] [PubMed] [Google Scholar]
- 11.Montano N, Fiorelli E, Tobaldini E. Sleep duration and the heart: I sleep, therefore I beat. J Am Coll Cardiol. 2019;74(10):1315–6. [DOI] [PubMed] [Google Scholar]
- 12.Li J, Cao D, Huang Y, Chen Z, Wang R, Dong Q, et al. Sleep duration and health outcomes: an umbrella review. Sleep Breath. 2022;26(3):1479–501. [DOI] [PubMed] [Google Scholar]
- 13.Yan B, Wu Y, Fan X, Lu Q, Ma X, Bai L. Sleep fragmentation and incidence of congestive heart failure: the Sleep Heart Health Study. J Clin Sleep Med. 2021;17(8):1619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cappuccio FP, Miller MA. Sleep and Cardio-Metabolic Disease. Curr Cardiol Rep. 2017;19(11):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavallino V, Rankin E, Popescu A, Gopang M, Hale L, Meliker JR. Antimony and sleep health outcomes: NHANES 2009–2016. Sleep Health. 2022;8(4):373–9. [DOI] [PubMed] [Google Scholar]
- 16.Li CI, Lin CC, Liu CS, Lin CH, Yang SY, Li TC. Sleep duration predicts subsequent long-term mortality in patients with type 2 diabetes: a large single-center cohort study. Cardiovasc Diabetol. 2022;21(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu H, Chen A. Roles of sleep deprivation in cardiovascular dysfunctions. Life Sci. 2019;219:231–7. [DOI] [PubMed] [Google Scholar]
- 18.Mireku MO, Rodriguez A. Sleep Duration and Waking Activities in Relation to the National Sleep Foundation’s Recommendations: An Analysis of US Population Sleep Patterns from 2015 to 2017. Int J Environ Res Public Health 2021;18(11). [DOI] [PMC free article] [PubMed]
- 19.Wang Y, Jiang G, Hou N, Chen M, Yang K, Wen K, et al. Effects and differences of sleep duration on the risk of new-onset chronic disease conditions in middle-aged and elderly populations. Eur J Intern Med. 2023;107:73–80. [DOI] [PubMed] [Google Scholar]
- 20.Zhang HR, Yang Y, Tian W, Sun YJ. Dietary Fiber and all-cause and Cardiovascular Mortality in older adults with hypertension: a cohort study of NHANES. J Nutr Health Aging. 2022;26(4):407–14. [DOI] [PubMed] [Google Scholar]
- 21.Wang X, Ma H, Gupta S, Heianza Y, Fonseca V, Qi L. The joint secular trends of Sleep Quality and Diabetes among US adults, 2005–2018. J Clin Endocrinol Metab. 2022;107(11):3152–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu CD, Chang RB. Goodnight from the heart: a cardiovascular circuit that promotes sleep. Neuron. 2022;110(23):3857–9. [DOI] [PubMed] [Google Scholar]
- 23.Tobaldini E, Fiorelli EM, Solbiati M, Costantino G, Nobili L, Montano N. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat Rev Cardiol. 2019;16(4):213–24. [DOI] [PubMed] [Google Scholar]
- 24.Yu Y, Chen Y, Zhang H, Ai S, Zhang J, Benedict C, et al. Sleep duration and visceral adipose tissue: Linear and nonlinear mendelian randomization analyses. J Clin Endocrinol Metab. 2022;107(11):2992–9. [DOI] [PubMed] [Google Scholar]
- 25.Kautzky-Willer A, Harreiter J. Sex and gender differences in therapy of type 2 diabetes. Diabetes Res Clin Pract. 2017;131:230–41. [DOI] [PubMed] [Google Scholar]
- 26.Ogilvie RP, Patel SR. The epidemiology of Sleep and Diabetes. Curr Diab Rep. 2018;18(10):82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Depner CM, Stothard ER, Wright KP. Jr. Metabolic consequences of sleep and circadian disorders. Curr Diab Rep. 2014;14(7):507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data supporting this publication are available from the NN repository located at www.cdc.gov/nchs/nhanes/index.htm.