Abstract
Background
Aerophagia is caused by the swallowing of excessive air and associated with various gastrointestinal symptoms. Aerophagia is diagnosed based on the observation of the occurrence of excessive air swallowing or ingestion; however, it tends to be difficult and often delayed. Early recognition and diagnosis of aerophagia are required to avoid unnecessary diagnostic investigations or serious clinical complications. Given that multichannel intraluminal impedance–pH measurement can discriminate gas, liquid, and mixed swallows, it can be useful for the diagnosis of aerophagia.
Case presentation
A 7-year-old girl presented to us with vomiting, and abdominal radiography showed dilatation of the stomach and intestine with no signs of mechanical obstruction. After successful conservative treatment, her symptoms recurred. Along with frequent visible and audible air swallowing, computed tomography (CT) revealed a severely dilated stomach with organoaxial volvulus. Multichannel intraluminal impedance–pH measurement was performed for further exploration. Patients showed numerous air swallows, particularly in the daytime during the 24-h recording period. She was diagnosed with aerophagia complicated by gastric volvulus. Given that she had a mental disorder and psychological counseling was difficult, laparoscopic anterior gastropexy and gastrostomy were performed to correct the gastric volvulus and decompression of gastric dilation by gastrostomy.
Conclusions
In addition to clinical symptoms, multichannel intraluminal impedance–pH measurement may help more accurately and objectively diagnose aerophagia. Further studies of air swallowing patterns may be useful for understanding the pathophysiological mechanism of aerophagia.
Keywords: Case report, Aerophagia, Multichannel intraluminal impedance, Gastric volvulus
Background
Aerophagia in children is defined by the Rome IV criteria as all of the following signs and symptoms: excessive air swallowing, abdominal distension caused by intraluminal air that increases during the day, repetitive belching and/or increased flatus, and repetitive belching or increased flatus occurring for a minimum of 2 months after appropriate evaluation [1]. Aerophagia has been observed in 8.8% of the institutionalized mentally handicapped population [2]. Until recently, studying air swallowing objectively for a prolonged period was difficult. With esophageal multichannel intraluminal impedance (MII) monitoring, evaluating swallowing frequencies and discriminating normal swallows from air swallows has become possible [3]. This study aimed to assess the advantage of MII–pH measurement for the diagnosis of aerophagia.
Case presentation
A 7-year-old girl with mental disability caused by chromosome 4 q34-pter partial monosomy and chromosome 7 p21-pter partial trisomy was referred to our emergency department after vomiting six or seven times. Her blood examination revealed a blood urea nitrogen level of 24.6 mg/dL, indicating dehydration. Plain abdominal radiography showed stomach dilation following vomiting (Fig. 1a), and the intestines had no signs of mechanical obstruction (Fig. 1b). After successful conservative treatment, such as intravenous fluid infusion and withdrawal of food and water, her symptoms recurred twice more. Along with frequent visible and audible air swallowing, CT revealed a severely dilated stomach with organoaxial volvulus. MII–pH measurement was conducted for further exploration.
Fig. 1.
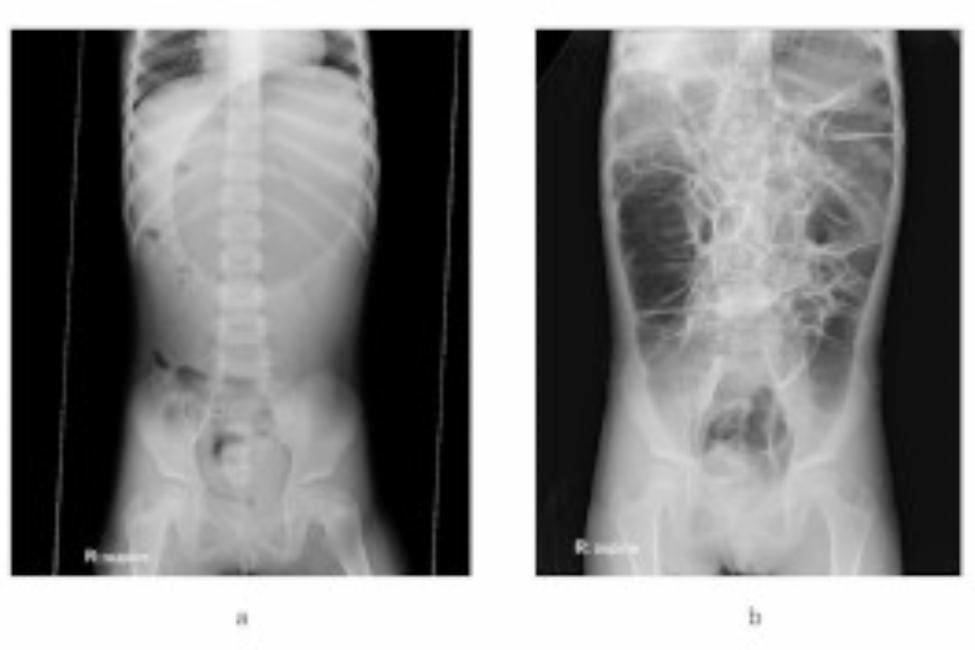
Plain abdominal X-ray image. (a) Plain abdominal X-ray image showing markedly distended stomach when vomiting. (b) Plain abdominal X-ray image showing massively dilated intestines when not vomiting with no signs of mechanical obstruction
The study protocol was approved by the Kagawa University Ethics Review Board (No. H26-137). The patient was examined after informed consent was obtained from her parents.
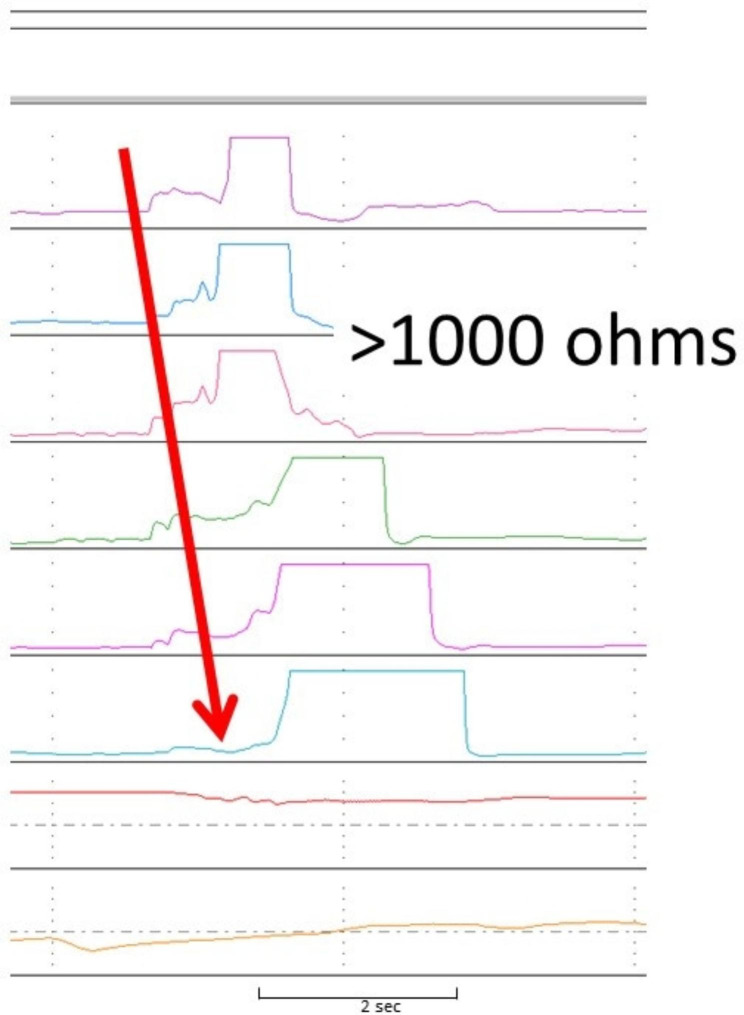
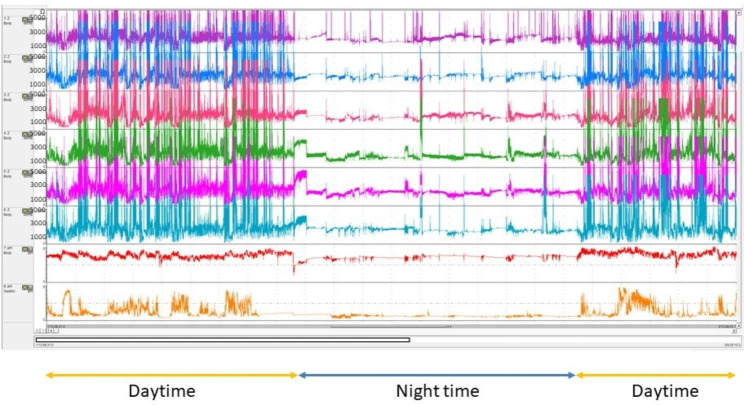
In this case, 24-h MII–pH measurement was performed using Sleuth recording devices (Sandhill Scientific System, Denver, CO, USA). The position of the MII–pH catheter was confirmed by X-ray imaging. Impedance data were automatically evaluated using the BioVIEW analysis software program, and each tracing was manually reviewed. An air swallow was defined as a peak superior to 1000 ohms above the baseline moving in the antegrade direction and measured in the most distal impedance segment (Fig. 2) [4]. During the 24-h recording period, the patient exhibited aerophagia 374 during the day and 13 times during the night. (Fig. 3). A gastric air reflux or a gastric belch was defined as a rapid rise of > 3000 ohms in the retrograde direction over at least two consecutive impedance sites that moved toward the mouth [5]. She also belched repetitively. Abnormal gastroesophageal reflux (GER) was not observed, and her pH reflux index, bolus exposure index, and number of total reflux episodes were 0%, 1.2%, and 20, respectively. She was diagnosed with aerophagia complicated with gastric volvulus. Because she had mental retardation, psychological counseling was difficult. Despite of conservative treatment, she had repeated gastric volvulus. Therefore, laparoscopic anterior gastropexy and gastrostomy were performed to correct the gastric volvulus and decompression of gastric dilation. Thereafter, she was free of symptoms, and plain abdominal X-ray imaging did not show dilatation of the stomach after surgery.
Fig. 2.
Aerophagia. A peak of impedance superior to 1000 ohms above the baseline moving in the antegrade direction and measured in the most distal impedance segment
Fig. 3.
MII waveform during the 24-h recording period
Discussion and conclusions
Pathologic aerophagia is observed in 8.8% of institutionalized mentally handicapped individuals [2]. Moreover, aerophagia has been observed in mentally handicapped patients and in those with neurologic disorders as a habitual means of self-harm, or as a way of dealing with boredom [6]. In healthy children with high sensitivity and introverted personalities that present aerophagia as part of a functional disease, the symptoms are precipitated by psychological stress [7].
In most of the reported cases, the correct diagnosis of pediatric aerophagia was initially missed [6–8]. Early recognition and correct diagnosis help alleviate parents’ or patient’s anxiety and prevent unnecessary testing, treatments, and hospital admissions [2, 6, 8]. In some cases, severe aerophagia causes massive bowel distention and can result in ileus, volvulus, and intestinal necrosis or perforation [6]. Confirming the excessive volume of air objectively has been difficult. Recently, combined MII–pH measurement has become increasingly important for evaluating GER or esophageal function [5, 9]. MII detects GER episodes based on changes in electrical resistance to the flow of an electrical current between a pair of electrodes placed on the MII probe when a liquid, semisolid, or gas bolus moves between them [10, 11]. By detecting reflux regardless of the pH value and distinguishing swallowing (antegrade flow) from authentic GER (retrograde flow), the combination of esophageal pH monitoring and impedance measurement offers several advantages over standard pH monitoring. In addition, it can accurately detect the height of the refluxate by multi channels. Esophageal MII monitoring can evaluate swallowing frequencies and discriminate normal swallows from air swallows [3]. In this case, MII monitoring helped us diagnose aerophagia. Although no description about MII monitoring when diagnose aerophagia is present in Rome IV criteria, MII monitoring may be potentially helpful for the diagnosis of aerophagia. For obvious ethical reasons, no controlled study is conducted in pediatric populations. Given that only small reports evaluate aerophagia using MII monitoring [3, 8, 12], more studies are needed to evaluate the diagnostic value of MII in children with aerophagia.
In the present case, overdistended transverse colon and distended stomach caused by aerophagia have also been considered important predisposing factors to the development of gastric volvulus. Such distended intestines, particularly the distended transverse colon, further promoted the volvulation of the stomach. Thus, the vicious circle caused by gastric volvulus and pathologic aerophagia contributed to the progression of abdominal distension, resulting in persistent gastrointestinal tract distention. The treatment of chronic gastric volvulus depends on symptomatology [13].
Effective reassurance and explanation of symptoms to the parents and child are essential in the treatment of aerophagia. Often, during the visit, the clinician can help the child become aware of air swallowing. For conservative therapy, eating slowly, avoiding chewing gum and drinking carbonated beverages, and using psychotherapeutic strategies for the alleviation of anxiety may be helpful [2]. Moreover, simethicone and dimethicone can reduce gas formation in the bowel [7]. Benzodiazepines are also used sometimes for expectation of antianxiety [1]. Those with persistent and severe symptoms should undergo gastropexy [13, 14]. Some recent studies have reported the usefulness of laparoscopic gastropexy, which is a minimally invasive technique, in patients with chronic gastric volvulus [15]. Although gastropexy could not treat aerophagia, laparoscopic gastropexy combined with gastrostomy is a good indication for chronic gastric volvulus complicated by pathologic aerophagia. As our patient had mental retardation and recurrent symptoms, psychological counseling seemed to be difficult and surgical treatment was selected.
MII–pH measurement can provide objective evidence of excessive air swallowing and repetitive belch; therefore, this case report could be an example of the well-known role of MII–pH measurement in supporting diagnosis of aedophagia.
Acknowledgements
The authors thank Dr D. Sifrim for his experienced advice in the analysis of MII–pH waveform.This work was supported by JSPS KAKENHI Grant Number JP22K11778.
Abbreviations
- GER
Gastroesophageal reflux
- MII
Multichannel intraluminal impedance
- CT
Computed tomography
- IV
Four
Author contributions
Study conception and design: AT and RS. Acquisition of data: AT, TF, and HK. Analysis and interpretation of data: AT and RS. Drafting of manuscript: AT and RS. Critical revision: AT and RS.
Funding
The authors declare that they have no funding.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Kagawa University Ethics Review Board (No. H26-137). The patient was examined after informed consent was obtained from her parents.
Consent for publication
The study protocol was approved by the Kagawa University Ethics Review Board (No. H26-137). Written informed consent for publication of identifying images or other personal or clinical details was obtained. The patient was examined after informed consent was obtained from her parents.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2016;150:1456–68. [Google Scholar]
- 2.Loening-Baucke V. Aerophagia as cause of gaseous abdominal distention in a toddler. J Pediatr Gastroenterol Nutr. 2000;31:204–7. [DOI] [PubMed] [Google Scholar]
- 3.Hemmink GJM, Weusten BLAM, Bredenoord AJ, Timmer R, Smout AJPM. Areophagia: excessive air swallowing demonstrated by esophageal impedance monitoring. Clin Gastroenterol Hepatol. 2009;7:1127–9. [DOI] [PubMed] [Google Scholar]
- 4.Kessing BF, Bredenoord AJ, Smout AJP. Mechanisms of gastric and supragastric belching: a study using concurrent high-resolution manometry and impedance monitoring. Neurogastroenterol Motil. 2012;24:e573–9. [DOI] [PubMed] [Google Scholar]
- 5.Hwang JB, Choi WJ, Kim JS, Lee SY, Jung CH, Lee YH, et al. Clinical features of pathologic childhood aerophagia: early recognition and essential diagnostic criteria. J Pediatr Gastroenterol Nutr. 2005;41:612–6. [DOI] [PubMed] [Google Scholar]
- 6.Morabito G, Romeo C, Romano C. Functional aerophagia in children: a frequent, atipical disorder. Case Rep Gastroenterol. 2014;8:123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halb C, Pomerleau M, Faure C. Multichannel intraesophageal impedance pattern of children with aerophagia. Neurogastroenterol Motil. 2014;26:1010–4. [DOI] [PubMed] [Google Scholar]
- 8.Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definition of acid, non-acid, and gas reflux. Gut. 2004;53:1024–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agrawal A, Castell DO. Clinical importance of impedance measurements. J Clin Gastroenterol. 2008;42:579–83. [DOI] [PubMed] [Google Scholar]
- 10.van Wijk MP, Benninga MA, Omari TI. Role of the multichannel intraluminal impedance technique in infants and children. J Pediatr Gastroenterol Nutr. 2009;48:2–12. [DOI] [PubMed] [Google Scholar]
- 11.Mousa HM, Rosen R, Woodley FW, Orsi M, Armas D, Faure C, et al. Esophageal impedance monitoring for gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2011;52:129–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bredenoord AJ, Weusten BLAM, Sifrim D, Timmer R, Smout AJPM. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut. 2004;53:1561–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Salem AH. Acute and chronic gastric volvulus in infants and children: who should be treated surgically? Pediatr Surg Int. 2007;23:1095–9. [DOI] [PubMed] [Google Scholar]
- 14.Porcaro F, Mattioli G, Romano C. Pediatric gastric volvulus: diagnostic and clinical approach. Case Rep Gastroenterol. 2013;7:63–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Komoro H, Matoba K, Kaneko M. Laparoscopic gastropexy for chronic gastric volvulus complicated by pathologic aerophagia in a boy. Pediatr Int. 2005;47:701–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.