Abstract
Scleroderma, an autoimmune connective tissue disorder, leads to skin and tissue thickening. In this autoimmune disease condition, the defense mechanism works against the body itself and mistakenly attacks normal cells. Ayurveda links it to vatarakta, initially affecting tvak, rakta, and mamsa. Vata is primarily involved, but as the disease progresses, all doshas and dhatu get involved.
A 45-year-old woman presented with skin hardening, skin depigmentation all over her body, limb stiffness, weakness, arthralgia, anorexia, constipation and burning in the chest region for the last three years.
She was diagnosed with diffuse systemic sclerosis (SSc) but as per Ayurveda we can correlate with aamvata and vatarakta based on her lakshanas(symptoms).
Ayurvedic treatment commenced with vardhamana pippali(Piper longum)rasayan, svedana karma, and virechan karma, followed by basti(enema) chikitsa (pathyadi kvath niruh basti) and oral ayurvedic medication viz., Manjisthadi kvatha, kaishora guggulu, Jatamansi(Nardostachys Jatamansi) churna, mishreya(Foeniculum vulgare) arka, dashang churna with water for local application and daily shamanarth panchtikta ghrit.
After 8 weeks, depigmentation was reduced, new hair growth emerged, mild skin softening occured, chest burning, anorexia, sleeplessness was decreased and enhanced mental well-being.
The treatment aimed to balance vitiated doshas and dhatu while alleviating symptoms, and enhancing overall well-being, demonstrating the efficacy of the holistic approach in managing scleroderma through Ayurveda.
Auto-immune disorder, scleroderma, chronic complications, skin tightness, salt pepper depigmentation, sclerodactyly.
Keywords: Systemic sclerosis, Scleroderma, Auto-immune disease, Ayurveda, Herbal medicine, Salt-pepper depigmentation
Highlights of case report
-
•
In alternative medicines, scleroderma like disorder are corrected only with steroids and analgesics.
1. Introduction
Scleroderma is a chronic, autoimmune connective tissue disorder that is primarily characterized by thickening and hardening of the skin and other tissue [1]. The combining form “sclero” means “hard” in Greek, and the word “dermis” means skin. There are two primary types of sclerodermas: localized and systemic (also called systemic sclerosis). SSc is a generalized connective tissue disease characterized by microvasculopathy, specific immunological abnormalities and fibrosis of skin and internal organs [2,3].
The causes of scleroderma are not fully known. There is some evidence that genetic and environmental factors play a role in the genesis of scleroderma. Silica and certain organic solvents are recognized as risk factors for the occurrence of systemic scleroderma. The result is an activation of the immune system, causing blood vessel damage and injury to tissues that result in scar tissue formation and the accumulation of excess collagen [1].
Systemic scleroderma is an acquired sporadic disease with a worldwide distribution and affecting all races. In the United States, the incidence is 9–46 cases per million per year. There are an estimated 100,000 U S. cases, although this number may be significantly higher if patients who do not meet classification criteria are also included. Prevalence rates in England, Europe, and Japan appear to be lower than in North America and Australia. Age, sex, and ethnicity influence disease susceptibility, and blacks have higher age-specific incidence rates. In common with other connective tissue diseases, systemic scleroderma shows a strong female predominance (4.6:1), which is most pronounced in the childbearing years and declines after menopause. An additional risk factor is having an affected first-degree family member, which increases disease risk 13-fold. Although systemic scleroderma can present at any age, the peak age of onset in women with both limited cutaneous systemic scleroderma (lcSSc) and diffuse cutaneous systemic scleroderma (dcSSc) is 65–74 years, although in blacks, disease onset occurs at an earlier age. Furthermore, blacks with SSc are more likely to have dcSSc, Interstitial Lung Disease (ILD) [4], and a worse prognosis [5].
According to Ayurveda, in scleroderma tvak(∼skin), rakta (∼blood) and mamsa(∼muscle mass) are vitiated initially. Vata is the main dosha but as disease advances all the dosha as well as all the dusyas get involved. In Ayurveda, it can be correlated with the vatarakta. In this autoimmune disease condition defense mechanism works against the body itself and mistakenly attacks normal cells. Abnormal interactions between endothelial cells, fibroblasts, and lymphocytes (B and T) lead to microcirculatory vascular involvement [6,7]. In this condition joints, tendons, and muscles are also affected, suggesting mamsa-meda(∼fatty tissue) and asthi(∼bone) dhatu involvement.
2. Patient information
On September 11, 2023, a 45 years old female patient came to our hospital with complaints of weakness, skin hardening-tightness, whitish discoloration (depigmentation) all over the body, restricted movement of the limbs since last three years, and other associated complaints like sleeplessness, anorexia, constipation, fatigue, itching all over the body and weight loss and due to skin tightening she was facing difficulty while opening her mouth. According to the history given, before three years, she began to experience weakness, tightening of skin (first starts from bilateral upper limb, thoracic area and then lower limbs get affected), sometimes interphalangeal joint pain, and diagnosed with hypothyroidism and rheumatoid arthritis. Over the period, she felt a worsening in the symptoms and was diagnosed with scleroderma in 2019. She received oral allopathic medications like Nonsteroidal Anti-Inflammatory Drugs (NSAIDs), Hydroxychloroquine (HCQS), steroids and ointments for local application during that period. Her history revealed that the patient was suffering from hypothyroidism for the last 3 years and her thyroid profile levels are under control with medication. After visiting numerous hospitals consecutively and trying both allopathic and ayurvedic treatments without experiencing any relief from her symptoms, she stopped taking any medicine for next 6–8 months.
According to the patient's relative, three years ago, her weight was 58kg. Within one year, it significantly reduced, and currently, she weighs only 29kg.
3. Clinical presentation of SSc patient
Patient was having thick indurated skin (scleroderma). Vitiligo like hypopigmentation (salt-pepper depigmentation) of the skin. Sclerodactyly – extensive skin induration starting in the fingers are present in both hands with fixed flexion contractures of fingers. Microstomia: Reduction in size of oral aperture was observed. Face appearance: “Mauskopf” appearance with pinched nose, pursed lips, lip thinning and retractions noticed. Muscle weakness, fatigue was present. Decreased joint mobility-wrist, elbows, shoulders, hip, knees and ankles become stiff due to fibrosis or skin tightness. Limited movement of the upper and lower limb and need support in day-to-day activities. Skin induration present with hair loss. Severe weight loss from 58kg to 29kg was encountered.
3.1. Findings of physical examination on rest (September 13, 2023)
Patient's Blood pressure (BP):110/70 mmHg, Pulse −64/min (feeble), Saturation of peripheral oxygen (SpO2)– 98%. General examination: Hyposthenic. Locomotor system examination: Restricted movement of the limbs present while folding hands and legs and during holding things, difficulty in walking, sitting, standing, forward bending and she walks slowly with short steps. Respiratory examination: Expiration time is much shorter than the inspiration time and no other abnormal/added sound is heard (suspect due to ILD changes) [4].
4. Timeline
Table 1 represents the timeline of the occurrence of events in the present case study. It represents all the symptoms along with the previous treatment taken by the patient and the results obtained.
Table 1.
Timeline of the disease.
| TIME | Disease condition | Treatment |
|---|---|---|
| 23/04/2019 | Weakness, skin tightness, joint pain for 2–3 weeks; Diagnosed: Hypothyroidism, Rheumatoid arthritis. | Conservative treatment for 2 months: Tab. Omnacortil 20mg 1 BD, Tab. Shelcal HB 1 OD, Tab. Thyronorm 50mg 1 OD. |
| June 2019 to November 2020 | Arthritis, dry skin hardening, muscle pain, whitish skin discoloration, sour belching, and chest burning persisting for two months. | Took medication viz., Methotrexate 25mg once a week, HCQS 300mg 1 HS, Sulphasalazine 500mg 1 BD, Tab. Nexpro 40 twice a day (BD) and Tab.Thyroxin Once daily (OD) for 16–17 months but did not fill relief in symptoms. |
| 18/10/2021 | A patient experiencing vomiting, diarrhoea, and burning chest pain for the last 10–12 days | Hospitalized and Inj. Cefaxone, Inj. Pantodac, Inj. Emeset, Tab. Thyroxin and Syp. Mucaine gel is started. At the time of discharge prescribed Tab. Domstal 1 TDS, Tab. Ganaton 150mg 1 TDS, Tab. Pantop 40 1 OD, Tab. Thyronorm 50 1 OD, Mucaine gel 2tsf every 4th hourly, Syp. Betonin 2tsf 3rd hourly for 1 month. |
| 15/11/2021 | Weight loss, weakness, white skin discoloration, joint pain (morning/winter), skin tightness- hardening. | Ayurvedic panchakarma treatments—Abhyanga, Svedana, Pottali seka, Basti Chikitsa, and Pattabandhan for 15 days. |
| 8/08/2022 | Patient with c/o weakness, weight loss, anorexia, fatigue, skin tightness-hardening, whitish discoloration all over the body diagnosed with diffuse cutaneous systemic sclerosis. | Patient took allopathic medication Tab. Omnacortil 5mg 1 OD, Tab. Calcium 1 OD, Tab. Crocin Advance 500 SOS (If Necessary) and many others for 1 month but after ingestion of medication nausea-vomiting occured, hence the patient stopped all the medication for 6–8 months. |
| 11/09/2023 | The patient came to P. D. Patel Ayurvedic hospital. | |
| The patient experiences weakness, difficulty in day-to-day activities, whitish skin discoloration, hardening, difficulty in mobility, sleeplessness, anorexia, constipation, fatigue, body itching, chest burning, and ulceration on interphalangeal joints (2–3) and left elbow over 2–3 months. Weight: 29kg Diagnosed with diffuse SSc and according Ayurveda correlate with aamvata and vatarakta. | In ayurvedic treatment Vardhaman pippali rasayan started (for 13days) 1 gm twice a day with luke warm water, before meal. Daily increases 1 gm up to 5 gm and then continue 5 gm for 5days and then taper the dose. Daily Sarvanga nadi svedana was done. | |
| 24/09/2023 | Same as above complaints. | Virechan karma with eranda sneha 40ml+ draksha kvatha - Q.S. followed by Samsarjana krama. |
| 26/09/2023 | Itching all over body, sleeplessness and burning in chest region decreases. | Starts daily oral Ayurvedic medication, 1)Pippali churna 3 gm + shankh bhasma 250mg twice a day with luke warm water before meal. 2)Manjisthadi kvatha 40ml twice. 3)Kaishor guggulu 3 tablet – 3 times a day with luke warm water, after meal 4) Jatamansi churna 3 gms – 1time before sleep with water. 5)Dasanga churna 3 gms- 2times for Local Application (L/A) (At the site of ulceration). 6) Mishreya arka 10–15 drops thrice a day before meal. |
| 27/09/’23 | Same as above. | 1)Started pathyadi basti (200ml) on alternate day in morning time after pancakarma procedure, sarvang abhyanga with jatyadi tail followed by sarvang nadi svedana. 2)Daily shamanarth panchtikta ghrit 20ml twice a day with decoction on empty stomach. |
| 01/10/’23 to 11/11/’23 | She got some relieve in symptoms, stiffness/tightness over both thighs and forearm decreases. Anorexia not present. No burning in chest region, skin depigmentation decreases. | Continue oral Ayurvedic medication and pancakarma procedure. Continue Tab.Thyronorm 50 1 OD. |
| 12/11/2023 | Burning in abdomen present. | Panchtikta matrabasti 40ml given for 4 days. |
| 16/11/2023 | Significant improvement noted: reduced skin tightness, and depigmentation; improved appetite, earlier bedtime; itching relieved, resolved constipation; weight: 28kg. | Patient discharged and advised to take oral medication at home and come for follow up on every two weeks |
5. Diagnostic assessments
The patient was diagnosed with diffuse systemic sclerosis (SSc) due to presence of skin thickening, sclerodactyly, ILD and SSc related antibodies in her body based on American college of Rhematology / European league against rheumatism (ACR/EULAR) SSc classification criteria [8] but as per Ayurveda we can correlate with aamvata and vatarakta based on her lakshanas(∼symptoms) similarity with SSc i.e., vaivarnya (∼salt-pepper depigmentation), stambha(∼stiffness), arochak(∼anorexia), karshya(∼weightloss), dhamanianguli sandhinamsankoch, angulivakrata (∼sclerodactyly), nidraviparyayam (sleeplessness) and vidvibadhhatam (constipation) kandu (itching) [9,10]. After dipana-pachan treatment in clinical findings there are no aam features present in patient's body.
5.1. Investigations
The investigations like parameters from haemogram, biochemical investigations related to thyroid problems, arthritis, ANA profile etc were done and outcomes are mentioned in Table 2. Her chest X-ray was done on October 18, 2021, and no significant abnormality is detected. On October 19, 2021, 2D Echo was done and it showed LVEF ∼60%, normal LV systolic function, mild Pulmonary Arterial Hypertension (PAH), and mild pericardial effusion. Multidetector Computed Tomography (MDCT) scan of the thorax was done showed both lung fields show posterior subpleural subtle ground glass, reticular, and microcystic changes. Subtle subpleural microcystic changes in the anterior segment of the right upper lobe – the possibility of early changes of ILD but in patient any type of symptomatology not present. Mild dilated thoracic esophagus consistent with esophageal involvement in scleroderma ± Gastroesophageal Reflux Disease (GERD) correlates with endoscopic view to rule out esophagitis. Multislice Spiral Computed Tomography (MSCT) scan of the abdomen with pelvis showed dilated overdistended stomach and 1st and 2nd part of the duodenum was noted, suggesting the possibility of gastric and duodenal dysmotility with delayed emptying. Mild dilated thoracic esophagus-consistent with esophageal involvement in scleroderma ± GERD.
Table 2.
Investigations
| 2019 | 2020 | 2021 | 2022 | 18/12/2023 | |
|---|---|---|---|---|---|
| Hemoglobin | 11.5 | 11.3 | 11.1 | 10.2 | 11.6 |
| RBC (mill/cumm) | 4.06 | 4.16 | 4.21 | 3.90 | 4.18 |
| Platelet count | 375000 | 327000 | 584000 | 378000 | 438000 |
| TSH(μIU/ml) | 7.744 | 2.89(on medication) | 2.53(on medication) | – | 3.51(on medication) |
| T3(ng/dL) | 95.81 | 116.14 | 192 | – | 136 |
| T4(μg/dL) | 9.01 | 10.22 | 13 | – | 11.08 |
| CRP (mg/L) | – | – | 14.9 | – | – |
| ESR (mm/hr) | 4 (April 2019) 6 (2hrly) 42(13/12/19) |
58 | 44 | 55 | 26 |
| RA Factor (IU/ml) | – | – | 10 | – | – |
| ANA Profile | +2 Intensity, Mildly Positive (23/4/2019) |
– | +4 Intensity, Strong Positive, highly suggestive of collagen vascular disease |
– | – |
| CPK (IU/L) | 32 | – | 77 | – | 86 |
6. Therapeutic intervention
The patient was treated through shodhan and shaman treatment as follows:
Stage 1. At the beginning of the Inpatient Department (IPD) period, finely powdered dried fruit of pippali (Piper longum) was administered orally (Vardhaman kramen for 13 days-modified) 1 gm twice a day with lukewarm water, before meal. Daily increases 1 gm up to 5 gm and then continue 5 gm for 5 days and then taper the dose. Daily Sarvanga mrudu nadi svedana(∼mild sudation therapy) was done. Vatarakta is contraindicated for svedana karma but in condition of stiffness, arthralgia it's indicated [11].
Vardhaman pippali is mentioned as rasayana(∼rejuvenation) and rasayana will helpful to increase the oja and it's responsible for the bala (immunity) and ultimately auto-immune process occurs less, so on this basis we have used Vardhaman pippali. In classics as anupana(∼consumed along with food or medicine) milk was mentioned but aam is present in body, so we selected luke warm water as anupana. In initial period aam was present in the body, that's why we modify it from the classics and not given abhyang in aam condition.
Stage 2. On the morning of the 14th day, mild purgation was performed once, orally administering eranda sneha with draksha kvatha on an empty stomach in a 40ml dose and according to the patient's sensitivity to purgatives (kostha) dose of the purgatives may varying from 40 to 60ml. Patient having alpabala(less stamina), the medicine was given in mild dose, but virechan karma(procedure) was completed with 14 vega. Before virechan(purgation), vardhaman pippali krama completed, snehapan was not given because of aam and in virechan we have given eranda (Ricinus communis) sneha(∼oil) because of its importance in aamvata as “erandasnehakesari” [12] and as “agrah erandam tu virechane” [13].
Stage 3. After one rest day, basti chikitsa (pathyadi kvath niruh basti) started with oral ayurvedic medications.
1) Pathyadi kvath niruh basti: It contains madhu(honey), saindhav(Rock salt), tila(Sesamum indicum) tail, putoyavani kalka [14] and pathyadi kvath [15] and prepare as per classics which is helpful to reduce the disease progress that's why we selected it. We give in 200ml dose on alternate days because of patient's bala(strength) and niruh basti is shodhana(purificatory therapy)kind of basti(enema) not continuously given in alpabala rugna(patient), so we modified it. 2) Pippali(Piper longum)churna 3 gm + shankh(Turbinella pyrum) bhasma 250mg twice a day with lukewarm water before meal. 3) Manjisthadi kwath 40ml twice a day. 3) Kaishor guggulu 900mg–3 times a day with lukewarm water, after meal 4) Jatamansi(Nardostachys Jatamansi)churna [16] 3 gms – 1 time before sleep with water. 5) Dasanga churna 3 gms- 2 times with water for L/A (At the site of ulceration). 6) Mishreya(Foeniculum vulgare)arka [17]10–15 drops thrice a day before meal given for anorexia and chest burning and after the stiffness subsides sarvanga abhyanga starts with the jatyadi taila followed by sarvanga nadi svedana. Shamanarth snehapana starts with panchtikta ghrit 20ml twice daily with the decoction. After dipana-pachan treatment, there is no aam(∼toxic or indigested material) features are observed in the patient's body.
We treated the patient according to the clinical condition, and classical references or classical treatment was kept in mind. Still, some modifications were required according to the patient's clinical condition. In this condition aam was present, so that's why we could not give sneha basti which is mentioned first in the classics, so some modification was required and according to the requirement we have modified the treatment schedule. Physician are free to choose the interventions depending on the patient's disease condition and strength [18].
Dietary intake: The patient was advised to take mung (green gram), mung bean soup, boiled vegetables like ridge gourd, sponge gourd, bottle gourd, pointed gourd, ash gourd, fenugreek seed leaves, drumstick, and bitter gourd. Brown rice, shali rice in food and lukewarm water for drinking. Advised to take cow ghee and milk.
The patient was advised t-o avoid oily, spicy and fermented food, dairy products, refined wheat products, biscuit, salty items, pickles, curd, buttermilk, tomato, lemon etc.
7. Outcome
After treatment weakness decreased, skin hardening on both upper and lower limbs, thoracic region and face decreases. Salt-pepper depigmentation on the face, hands, legs and neck region decreased. At the time of admission, she felt mild itching all over her body and it subsides. Gastroesophageal Tract (GI) problems are subsided. The dryness of the skin moderately decreased. In microstomia mild improvement or smoothness was observed. After treatment, new hair growth was visible on the affected parts but long studies are needed to assess the sustained results.
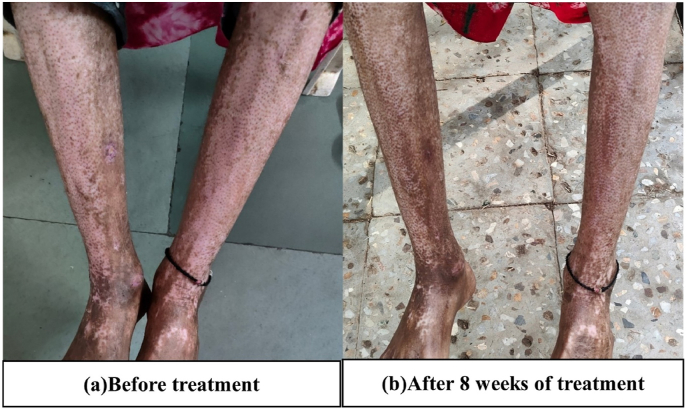
The outcome of this case study reveals that the patient feels relieved in her symptoms Table 3. The changes in signs were as follows: as per Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7.
Table 3.
Assessment of the disease symptoms before and after treatment.
| Sign and symptoms | Before treatment | After 8 weeks of treatment | |
|---|---|---|---|
| 1. | Weakness | Severe | Moderate |
| 2. | Skin hardening on both upper & lower limbs, thoracic region, face | Severe | Decreased on the upper arm, thigh, face, and flank |
| 3. | Depigmentation on the face, hands, legs, neck region | Severe [See Fig. 2, Fig. 3, Fig. 5, Fig. 6, Fig. 7] | Moderate to Severe [See Fig. 2, Fig. 3 and 5(b), 6(b), 7(b)] |
| 4. | Difficulty in day-to-day activities | Need the support of others. | Need the support of others. |
| 5. | Ulceration on interphalangeal joints (2–3) and left elbow | Moderate | Mild |
| 6. | Itching all over the body | Moderate | Absent |
| 7. | Anorexia | Moderate | Absent |
| 8. | Sometime constipation | Once in 1–2 days | 1-2 times/day |
| 9. | Burning in chest and sour belching | In evening time | Absent |
| 10. | Dryness of the skin | Severe | Moderate |
| 10. | Mouth opening | One to one and half finger. | Two fingers |
| 11. | Hair growth on the affected part | Less or no [see Fig. 7(a)] | New hair eruptions were observed [see Fig. 7(b)] |
| 12. | Mood | Depressed, unhappy | Happy |
Fig. 1.
Facial expression changes, before 3 years her weight was 58kg, and at present 29kg. A) Healthy condition B) At the time of admission.
Fig. 2.
Before treatment and after 8 weeks of treatment changes are observed in Fig. 5. A. and Fig. 5. B. salt pepper pigmentation on the thoracic region is decreased.
Fig. 3.
Before treatment and after 8 weeks of treatment changes are observed in salt-pepper pigmentation on bilateral lower limbs.
Fig. 4.
Before and after 8 weeks of treatment changes were observed in microstomia.
Fig. 5.
In image (a) minimum or no hair growth is observed. In the image (b) new hair eruptions are visible. In comparison to image (a), after 8 weeks of treatment salt-pepper depigmentation is reduced on hand.
Fig. 6.
In the images (a) and (b) yellow arrow shows changes in salt-pepper pigmentation before and after 8 weeks of treatment. The red round shows sclerodactyly.
Fig. 7.
Before and after 8 weeks of treatment remarkable changes are observed on the face.
8. Discussion
In the patient, we cannot directly correlate with systemic sclerosis, but as per symptomatology found in the patient's body the diagnosis was confirmed as systemic sclerosis and according to Ayurveda some findings suggest aamvata and some findings suggest vatarakta. Ayurvedic scholars specifically in South India, also consider rheumatoid arthritis as vatarakta and some scholars take the aamvata as rheumatoid arthritis. There is also some contradiction in Ayurvedic diagnosis, so the treatment we selected here is a combination or those which are common in aamvata and vatarakta.
In this disease condition tvak, rakta and mamsa dhatu are involved, which share certain symptoms with vatarakta and aamvata. The disease is caused by vata pradhan tridosha prakopa. In shamana chikitsa initially, vardhamana pippali rasayan (modified) is given, it possesses the rasayan and dipana-pachan properties, as well as helps in aam, auto-immune condition [19]. Charak aacharya mentioned that ‘churnikrita harsvabale’ means in alpabala patient, pippali rasayan used in powder form [20]. Sushruta aacharya also mentioned ‘pippalivardhamanakam’ in vatashonit and arochak treatment [21]. Pippali increases digestive power, having antipyretic, antioxidant, tridoshashamak properties and also works on mental well-being as medhagnivardhini [22]. Ama is responsible for the development of autoimmune disorders in the body, so pippali helps in the correction of immune system activities. Sarvanga nadi svedana is helpful in the condition of stiffness and skin hardening, additionally, it will work on body tissue. Skin is the site of the vata dosha, so vata dosha gets subsided by the sudation therapy.
Virechan karma helps to subside the aggravated pitta dosha and in this disease condition, it will be carried out with eranda sneha and draksha kvatha. Eranda works on vata and draksha kvatha acts with its purgative properties and it will also subside the pitta dosha. Basti chikitsa works on vata dosha and pathyadi dravyas has properties of pitta shamana and raktashodhak. It will help increase the GI motility and increases the gastric emptying time.
In shaman chikitsa manjisthadi kvatha [23] works on the raktavaha srotas, which help to heal ulcers, balance the doshas, and enhance cellular growth and tissue generation with antioxidant and anti-inflammatory properties. Manjistha act as jvarahar, pittashamak, kusthghna, varnakrit [24], so helpful in depigmentation. Aacharya yogaratnakar mentioned as manjisthadi kvath used in vatarakta and kustha roga [25]. Kaishora guggulu [26] works in vatarakta, kustha roga as main ingredient has rasayan, tridoshamak, purgative, anti-inflammatory, antipyretic, wound healing, analgesic, anti-inflammatory properties [27]. Jatyadi taila helps to heal ulcers and reduces itching [28]. Mishreya arka helpful in the condition of anorexia, chest burning, it will work on piita dosha. Jatamansi churna helps in relieving stress, works as an anti-depressant, and might be beneficial in the condition of sleep disturbances. Charaka described ghrit as having the best vata pitta shamaka properties. Panchatikta ghrit used in all skin diseases and in vatadi rogas [29,30]. Stimulates the agni and is used in skin disorders with anti-inflammatory and detoxification properties. Ultimately whole treatment is irradicate the disease progress and patient get the relief.
After 8 weeks of treatment skin depigmentation decreases, new hair growth is observed, and skin hardening mildly decreases. Burning in the chest, anorexia, sleeplessness, and lethargy are decreased. Significant improvements in psychological and social behavior are observed.
9. Conclusion
The present study concludes that Ayurvedic interventions are helpful in patients with systemic sclerosis and they will improve the patient's quality of life. Depending on the dosha and dusya involvement Ayurvedic treatment should be selected but in this type of disease condition long stay and long-term follow-up are required for sustained results. Patient may be advised to follow the lifestyle changes, diet, and regimens strictly.
10. Patient's perspective
It was reported by the patient on 16th November 2023. The patient's view “When I came to this hospital, I was very weak, my skin was very tight, my whole body was stiff which made it difficult for me to get out of bed and do daily activities and also didn't feel hungry, suffered from acidity, whole body itching present, sleeplessness, lethargy throughout the day, and sometimes constipation. After treatment in this hospital, I have considerable changes in stiffness, skin loosening a bit, appetite improvement, go to bed early, relief in itching, and no constipation.”
11. Informed consent
Written permission for the publication of this case study was obtained from the patient.
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Sources of funding
None.
Author Contributions
The contributions were made by each author to the research and preparation of this manuscript (conceptualization, study design, conduct, writing, review etc) and all authors have read and approved the final version of the manuscript and approved its content, and agreed with the order of authorship.
Declaration of Generative AI in scientific writing
During the preparation of this work, the author (corresponding author) declared that we have not used any tool/service or AI. We have only used basic tools such as the Grammarly app for checking grammar and we have nothing to disclose.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors are thankful to J. S. Ayurveda Mahavidhyalaya for the support.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Odonwodo A, Badri T, Hariz A. Statpearls Publishing; Treasure Island (FL): 2024. Scleroderma. StatPearls,https://www.ncbi.nlm.nih.gov/books/NBK537335/ [PubMed] [Google Scholar]
- 2.Vanhaecke A, De Schepper S, Paolino S, Heeman L, Callens H, Gutermuth J, et al. Coexistence of systemic and localized scleroderma: a systematic literature review and observational cohort study. Rheumatology. 2020;59:2725–2733. doi: 10.1093/rheumatology/keaa297. [DOI] [PubMed] [Google Scholar]
- 3.Denton CP, Khanna D. Systemic sclerosis. The Lancet. 2017;390:1685–1699. doi: 10.1016/S0140-6736(17)30933-9. [DOI] [PubMed] [Google Scholar]
- 4.Schoenfeld SR, Castelino FV. Interstitial lung disease in scleroderma. Rheum Dis Clin N Am. 2015;41:237–248. doi: 10.1016/j.lpm.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, editors Harrison’s Principles of Internal Medicine. Part II, Chapter 353: Immune-mediated, Inflammatory and Rheumatologic Disorders. 20th ed. p. 2546.
- 6.Dumoitier N, Lofek S, Mouthon L. Pathophysiology of systemic sclerosis: state of the art in 2014. Presse Méd. 2014;43:e267–e278. doi: 10.1016/j.lpm.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Gilbane AJ, Denton CP, Holmes AM. Scleroderma pathogenesis: a pivotal role for fibroblasts as effector cells. Arthritis Res Ther. 2013;15:215. doi: 10.1186/ar4230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pope JE, Johnson SR. New classification criteria for systemic sclerosis (scleroderma) Rheum Dis Clin N Am. 2015;41:383–398. doi: 10.1016/j.rdc.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Shashirekha HK, Bargale SS Charak Samhita, Vol. IV. Varanasi: Chaukhamba Prakashan. p. 646–653.
- 10.Sastri S, Upadhyaya Y, editors Madhava Nidana of Sri Madhavakara with the Madhukosha Sanskrit commentary. Part 1. p. 511.
- 11.Krushavaha HS. Charak Samhita. Vol. 2. Chowkhamba publication; Varanasi: 2016. p. 224. Part 1. [Google Scholar]
- 12.Shrikrishnadas K, Bhaishjya Ratnavali, Bhashatika Samhita, 2009, pg.729.
- 13.Krushavaha HS. Charak Samhita. Part 2. Chowkhamba Publication; Varanasi: 2016. p. 199. Part 1. [Google Scholar]
- 14.Shashirekha HK, Bargale SS. Vol. V. Chawkhamba Publications; Varanasi: 2018. p. 162. (Charak Samhita). [Google Scholar]
- 15.Tripathi B. Sharangadhara Samhita, Madhyamkhanda. Chowkhamba Surbharati Prakashana; Varanasi: 2023. p. 100. [Google Scholar]
- 16.Bapalal V. Nighantu Aadarsh Purvardh. Chaukhamba Bharati Academy; Varanasi: 2011. p. 597. [Google Scholar]
- 17.Vaidyanath S. Ayurveda Sarasangraha. Vaidyanath Ayurveda Bhavan; Ilahabad: 2015. pp. 647–648. [Google Scholar]
- 18.Krushavaha HS. Charak Samhita. Part 2. Varanasi: Chowkhamba Publication; 2016. Part 1. p.781.
- 19.Patel K, Soni A, Gupta S. Clinical evaluation of Vardhamana Pippali Rasayana in the management of Amavata (Rheumatoid Arthritis) Ayu. 2011;32:177. doi: 10.4103/0974-8520.92555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acharya SNM., Editor. Part 2. Chowkhamba Publication; Varanasi: 2012. p. 31. (Charaka Samhita with Ayurveda-Dipika Ayushi Hindi commentary of Chakrapanidatta.). [Google Scholar]
- 21.Shastri AD. Sushruta Samhita. Chaukhambha Sanskrit samsthan; Varanasi: 2018. p. 40. [Google Scholar]
- 22.Bapalal V. Nighantu Aadarsh Purvardh. Chaukhamba Bharati Academy; Varanasi: 2011. p. 870. [Google Scholar]
- 23.Tripathi BT. Sharangadhara Samhita, Madhyamakhanda. Chowkhamba Surbharati Prakashana; Varanasi: 2017. p. 102. [Google Scholar]
- 24.Bapalal V. Nighantu Aadarsh Purvardh. Chaukhamba Bharati Academy; Varanasi: 2011. p. 589. [Google Scholar]
- 25.Shastri SLP Yogaratnakar Vidhyotini Hindi Tika. Varanasi: Chowkhamba Prakashana. p. 554. Purvardha.
- 26.Tripathi B. Sharangadhara Samhita, Madhyamakhanda. Chowkhamba Surbharati Prakashana; Varanasi: 2017. p. 136. [Google Scholar]
- 27.Sharma PC, Yelne MB, Denis TJ. Vol. 3. Central Council for Research in Ayurveda & Siddha; Delhi: 2005. (Database on Medicinal Plants used in Ayurveda). [Google Scholar]
- 28.Sharma H. Sharangadhara Samhita, Madhyamakhanda. 7th ed Varanasi: Chowkhamba Surbharati Prakashana; 229.
- 29.Thakur N. Rasatantrasara va Siddhaprayogasangrah, Prathamkhanda. Krishna Gopal Ayurveda Bhavan Prakashak; Ajmer: 2012. p. 441. [Google Scholar]
- 30.Tripathi B. Sharangadhara Samhita, Madhyamakhanda. Chowkhamba Surbharati Prakashana; Varanasi: 2017. p. 152. [Google Scholar]