Abstract
Background
Adults living with human immunodeficiency virus (ALWHIV) receiving antiretroviral therapy (ART) exhibit higher pneumococcal carriage prevalence than adults without HIV (HIV-). To assess factors influencing high pneumococcal carriage in ALWHIV, we estimated pneumococcal carriage acquisition and clearance rates in a high transmission and disease-burdened setting at least 10 years after introducing infant PCV13 in routine immunisation.
Methods
We collected longitudinal nasopharyngeal swabs from individuals aged 18–45 in Blantyre, Malawi. The study group included both HIV- individuals and those living with HIV, categorised based on ART duration as either exceeding 1 year (ART > 1y) or less than 3 months (ART < 3 m). Samples were collected at baseline and then weekly for 16 visits. To detect pneumococcal carriage, we used classical culture microbiology, and to determine pneumococcal serotypes, we used latex agglutination. We modelled trajectories of serotype colonisation using multi-state Markov models to capture pneumococcal carriage dynamics, adjusting for age, sex, number of under 5 year old (< 5y) children, social economic status (SES), and seasonality.
Results
We enrolled 195 adults, 65 adults in each of the study groups. 51.8% were females, 25.6% lived with more than one child under 5 years old, and 41.6% lived in low socioeconomic areas. The median age was 33 years (IQR 25–37 years). The baseline pneumococcal carriage prevalence of all serotypes was 31.3%, with non-PCV13 serotypes (NVT) at 26.2% and PCV13 serotypes (VT) at 5.1%. In a multivariate longitudinal analysis, pneumococcal carriage acquisition was higher in females than males (hazard ratio [HR], NVT [1.53]; VT [1.96]). It was also higher in low than high SES (NVT [1.38]; VT [2.06]), in adults living with 2 + than 1 child < 5y (VT [1.78]), and in ALWHIV on ART > 1y than HIV- adults (NVT [1.43]). Moreover, ALWHIV on ART > 1y cleared pneumococci slower than HIV- adults ([0.65]). Residual VT 19F and 3 were highly acquired, although NVT remained dominant.
Conclusions
The disproportionately high point prevalence of pneumococcal carriage in ALWHIV on ART > 1y is likely due to impaired nasopharyngeal clearance, which results in prolonged carriage. Our findings provide baseline estimates for comparing pneumococcal carriage dynamics after implementing new PCV strategies in ALWHIV.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-024-03631-5.
Keywords: Pneumococcal acquisition, Pneumococcal duration, Serotype, Human immunodeficiency virus, Modelling, Malawi
Background
Streptococcus pneumoniae (pneumococcus) commonly colonises the nasopharynx (NP) of children and adults [1]. Pneumococcal colonisation precedes disease, such as pneumonia, meningitis, and bacteraemia [1–3], and is also prerequisite for transmission [1]. The pneumococcus causes excessively high pneumococcal carriage and disease burden in adults living with human immunodeficiency virus (ALWHIV) on antiretroviral therapy (ART) compared to adults without HIV (HIV-) [4, 5], despite the substantial coverage of ART and suppression of viral load [6, 7]. Paradoxically, the higher pneumococcal carriage prevalence among ALWHIV with longer than shorter ART experience remains unexplained in this setting [8].
Pneumococcal conjugate vaccines (PCVs) protect against carriage due to specific vaccine-targeted (VT) serotypes, thereby interrupting VT transmission and reducing VT disease risk [9, 10]. In November 2011, Malawi introduced the 13-valency infant PCV (PCV13) into the national extended programme on immunisation (EPI) using a three-primary dose schedule without a booster (3 + 0; one dose at 6, 10, and 14 weeks of age) [11]. Despite at least 12 years of more than 90% infant PCV13 coverage among age-eligible children [12], in the absence of a direct PCV vaccination programme for ALWHIV [13], there is evidence of residual VT-carriage prevalence and VT-invasive pneumococcal disease (VT-IPD) incidence in children and ALWHIV in Malawi [14–17].
A change of infant PCV schedule from 3 + 0 to 2 + 1 (one primary dose at 6, 10, and booster dose at 36 weeks of age) or 2 + 1 + 1 (2 + 1 and one additional booster dose at 60 weeks of age) to enhance herd immunity, or direct routine PCV vaccination of ALWHIV has been suggested as potential vaccine strategies to eliminate persistent VT pneumococcal carriage risk and VT disease in ALWHIV [18]. Thus, to better assess the impact of a new vaccination strategy against VT carriage and disease among ALWHIV on ART, longitudinal studies are needed to generate the evidence base of pneumococcal serotype dynamics before the introduction of a new vaccine strategy [2, 19]. This may improve our understanding of serotypes that are frequently acquired or prolongedly carried, determinants of VT and NVT carriage acquisition and clearance, post-PCV serotype replacement, and the choice of vaccine product with the greatest potential to further reduce pneumococcal carriage and subsequent disease.
Here, we leveraged data from a longitudinal study of natural pneumococcal colonisation (Nasomune) among ALWHIV on ART and HIV- adults in Blantyre, Malawi, to estimate pneumococcal carriage parameters to inform transmission dynamic models of alternative vaccine strategies in ALWHIV. In particular, we estimated pneumococcal serotype-specific and vaccine-serotype group acquisition and clearance rates, as well as associated factors among ALWHIV using multi-state Markov transition models.
Methods
Ethics approval
Nasomune study nasopharyngeal (NP) samples were obtained from each Malawian adult through written consent. Study ethics approval was granted by the Malawi National Health Sciences Research Ethics Committee (NHSRC) (21/24/2680) and the Liverpool School of Tropical Medicine Research Ethics (21–035) in accordance with the Declaration of Helsinki. Written informed consent to participate was obtained from all of the participants in the study.
Data description
Nasomune study data were collected between 17 September 2021 and 11 December 2023 in Blantyre, Malawi. Using a random sampling approach, individuals were enrolled from different communities across Blantyre of whom 65 were HIV-, 65 ALWHIV with at most 3 months ART experience (ART < 3 m), and 65 ALWHIV with at least 1 year ART experience (ART > 1y). HIV infection status was determined according to the double rapid test algorithm in Malawi with an overall sensitivity of 99.6% and specificity of 100% [20, 21]. Inclusion criteria included asymptomatic adults aged 18 to 45 years living with at least one child under 5 years old. Adults with 4 weeks prior use of antibiotics (except cotrimoxazole), history of smoking, pregnancy, current respiratory tract illness, cancer, and taking immunosuppressive medications (except ART) were excluded from the study.
NP swabs were taken during 17 total visits: at baseline (visit 1) and then weekly during the next 16 visits of the study period per protocol, resulting in 3152 total NP samples from 195 individuals adjusted for missed visits. The swabs were tested for the presence of pneumococci using the World Health Organisation (WHO) NP sampling procedure and standard microbiological culture [22]. Serotyping of every positive pneumococcal sample was done using latex agglutination, based on picking a single colony, to identify serotypes or serogroups [23]. Pneumococcal carriage density was measured using microbiological culture serial dilutions on gentamicin-sheep blood sugar agar plate (5 µl gentamicin/ml) and results reported as colony forming units per millilitre (CFU/ml) [24]. On enrolment and during follow-up, clinical and demographic characteristics of the study participants were recorded which included antibiotic use during follow-up, pneumococcal carriage density, age, sex, number of children under 5 years old (< 5y) living in the house, socioeconomic status (SES) based on owning different functioning items [3], and third-level administrative unit location where the study participant resided.
Continuous-time time-homogeneous multi-state Markov models
We adapted a previously published Markov modelling framework to fit three variants of continuous-time time-homogeneous multi-state Markov models to individual-level trajectories of pneumococcal colonisation during the study period, assuming a susceptible-infected-susceptible (SIS) model structure [25]. The first model estimated total carriage dynamics regardless of specific serotypes and vaccine serotype category, the second model was expanded to capture VT and NVT carriage dynamics separately, and the last model was further expanded to also assess individual serotype carriage dynamics. Since multiple serotype carriage was not tested in this study due to use of latex agglutination serotyping method, we assumed that at any time-point , an individual can only carry a single dominant serotype and be in a colonised state carrying pneumococcus (model 1) or separately VT and NVT (model 2) or any individual serotype (model 3) abbreviated as , or be in a uncolonised state () where is the subscript for a carriage state. Thus, the transition intensities between { and } can be described by transition matrices for model 1 (, for model 2 (, or for model 3 with 16 individual serotypes () (Additional file 1: Fig. S1). To ensure model convergence due to limited data points, model 3 was limited to capture 16 carriage states, each corresponding to serotype 15A/B/C/F, 7A/B/C, 3, 11A/B/C/D/F, 23A/B, 17A/F, 19F, 10A/B/C/F, 20, 6C, 19A, 9A/L/N, 6A, combined identified VT (1, 4, 9 V, 14, 18C, 23F), combined identified NVT (22A/F, 33A/B/C/D/F, 18A/B/C/F, 12A/B/F, 19B/C, 8, and 6D), and unidentified NVT.
Our models describe acquisition and clearance rates of overall carriage, VT and NVT carriage or serotype-specific carriage from to and from to , captured by transition matrix entries and , respectively. The effects () of a vector of clinical and demographic characteristics () of th individual on acquisition and clearance rates are only estimated in model 1 and model 2 and not in model 3 due to limited data points. Thus, is modelled using hazard rates [26], e.g. over all transitions () where refer to being in state at time given that the previous state was . Since acquisition of pneumococci is not observed for individuals already carrying pneumococci at baseline, we assume that their baseline rates of acquisition are similar to steady state rates over the study period. Our model also assumes that the future colonisation state is independent of its history beyond the current state [26]. We assume that the time spent in each state is exponentially distributed [25], thus pneumococcal carriage duration is estimated as the inverse of clearance, allowing precise estimation of pneumococcal carriage episode. To obtain acquisition probabilities, the matrix is computed through matrix exponential, , over a constant through the study period. To adjust for potential changes in pneumococcal carriage intensities over time due to seasonality, we include in model 1 and model 2 a binary term for hot-wet and cool-dry seasons representing a typical divide of Malawi’s climate over months of November–April and May–October [8], respectively (Additional file 1: Fig. S1).
Likelihood estimation
To fit the Markov model, the likelihood is constructed as the product of probabilities of transition between observed states, over all individuals and observation times , assuming that sampling times are ignorable, e.g. the fact that a particular observation is made at a certain time does not implicitly give information about the value of that observation.
where each is the entry of the transition probability matrix at row and column evaluated at time . The likelihood is maximised under a log scale to compute estimates of using Bound Optimisation By Quadratic Approximation (BOBYQA) algorithm implemented by msm R package [26, 27].
Results
Participant and sample description
At baseline, 65 individuals were enrolled in each group of HIV-, ALWHIV on ART < 3 m, and ALWHIV on ART > 1y, totalling 195 participants of whom 5.1% and 26.2% carried VT and NVT, respectively. One hundred and one adults (51.8%) were females, 25.6% lived with at least two children < 5y, and 41.6% were in low SES. The median participant age was 33 (interquartile range [IQR]: 25–37, range: 18–45), and pneumococcal carriage density was 10,720 CFU/ml (IQR: 1005–82,075). We estimated carriage prevalence by dividing the number of positive samples by the number of swabs taken per visit, HIV status and/or ART group. The baseline prevalence of pneumococcal NVT and VT carriage was generally higher for ALWHIV on ART > 1y (33.8% and 7.7%) compared to ALWHIV on ART < 3 m (24.6% and 3.1%) or HIV- adults (20.0% and 4.6%). Likewise, the baseline median pneumococcal carriage density was higher for ALWHIV on ART > 1y (13,400 CFU/ml; IQR: 520–67,838) compared to ALWHIV on ART < 3 m (9548 CFU/ml; IQR 2387–247,900) or HIV- adults (8208 CFU/ml, IQR: 1884–149,494) (Table 1).
Table 1.
Baseline characteristics of adults without HIV (HIV-), adults living with HIV (ALWHIV) on ART < 3 months (m), and ALWHIV on ART > 1 year (y), who were recruited during in a pneumococcal nasopharyngeal swabbing study in Blantyre, Malawi, between September 2021 and December 2023
| Description | All participants | HIV- adults | ALWHIV on ART < 3 m | ALWHIV on ART > 1y |
|---|---|---|---|---|
| 195, n (%) | N = 65, n (%) | N = 65, n (%) | N = 65, n (%) | |
| Pneumococcal serotype group | ||||
| Non-carriers | 134 (68.6) | 49 (75.4) | 47 (72.3) | 38 (58.5) |
| Non-vaccine-serotypes (NVT) | 51 (26.2) | 13 (20.0) | 16 (24.6) | 22 (33.8) |
| Vaccine-serotypes (VT) | 10 (5.1) | 3 (4.6) | 2 (3.1) | 5 (7.7) |
| Sex | ||||
| Male | 94 (48.2) | 34 (52.3) | 27 (41.5) | 33 (50.8) |
| Female | 101 (51.8) | 31 (47.7) | 38 (58.5) | 32 (49.2) |
| Age group (years) | ||||
| Median age (IQR) | 33 (25–37) | 33 (26–38) | 34 (25–37) | 34 (25–37) |
| 18–33 years | 99 (50.8) | 35 (53.8) | 32 (49.2) | 32 (49.2) |
| 34–44 years | 96 (49.2) | 30 (46.2) | 33 (50.8) | 33 (50.8) |
| Number of children in the house | ||||
| One child | 145 (74.4) | 51 (78.5) | 47 (72.3) | 47 (72.3) |
| Two or more children | 50 (25.6) | 14 (21.5) | 18 (27.7) | 18 (27.7) |
| Pneumococcal density groups | ||||
| Median pneumococcal density (IQR) (CFU/ml) | 10,720 (1005–82,075) | 8208 (1884–149,494) | 9548 (2387–247,900) | 13,400 (520–67,838) |
| Low | 33 (54.1) | 9 (56.3) | 10 (55.6) | 14 (51.9) |
| High | 28 (45.9) | 7 (43.8) | 8 (44.4) | 13 (48.1) |
| Social economic status | ||||
| Low | 79 (41.6) | 22 (35.5) | 47 (74.6) | 42 (64.6) |
| High | 111 (58.4) | 40 (64.5) | 16 (25.4) | 23 (35.4) |
| Absolute CD4 count, cells/mm3 (median, confidence intervals [95% CI]) | 456 (415,561) | 541 (511, 621) | ||
| Categorised CD4 count | ||||
| ≤ 250 cells/mm3 | 15 (23) | 5 (7.7) | ||
| > 250 cells/mm3 | 50 (77) | 60 (92.3) | ||
| Viral load (HIV copies/ml) | ||||
| < 1000 | 8 (12.3) | 1 (1.5) | ||
| < 40 | 13 (20.0) | 4 (6.2) | ||
| ≥ 1000 | 12 (18.5) | 4 (6.2) | ||
| Not detected | 32 (49.2) | 56 (86.1) | ||
VT: refers to a group of serotypes targeted by 13-valency pneumococcal conjugate vaccine (PCV13)
NVT: refers to a group of serotypes not targeted by PCV13
IQR: interquartile range with first and third quartile
CFU/ml: colony forming unit per millilitre
ART: antiretroviral therapy
Cut off for age groups is based on overall median age of 33 years old
Cut off for pneumococcal density groups is based on overall median carriage density of 10,720 CFU/ml
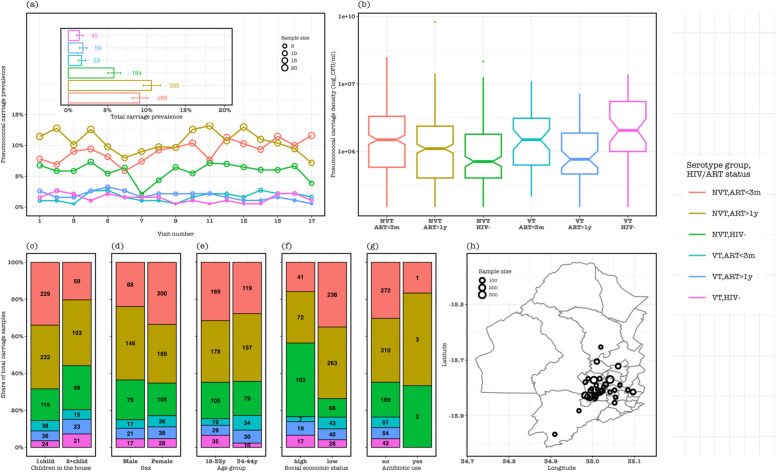
During the follow-up visits, NVT carriage prevalence was mostly highest in ALWHIV on ART > 1y (range: 7.2–13.2%) than in ALWHIV on ART < 3 m (5.9–11.6%) or HIV- adults (2.1–7.3%), whereas VT carriage prevalence remained similar in the three groups at 0.5–2.7%. For aggregated samples across all visits, NVT carriage prevalence remained higher in ALWHIV on ART > 1y (10.6%, 95% confidence intervals [CI]: 9.6–11.8) than ALWHIV on ART < 3 m (9.1%, 95% CI: 8.2–10.2) or HIV- adults (5.8%, 95% CI: 5.0–6.7). Among NVT carriers, the median carriage density was higher among ALWHIV on ART > 1y than HIV- adults. In contrast, the median carriage density was higher among ALWHIV on ART < 3 m than ALWHIV on ART > 1y carrying either VT or NVT. In addition, NVT samples from ALWHIV on ART > 1y dominated among those who lived with at least two children < 5y (35.5%), who were 18–33 years (33.3%), from low SES (38.7%), and did not use antibiotics (34.5%). Conversely, NVT samples from ALWHIV on ART < 3 m were highest among females (33.6%) (Fig. 1).
Fig. 1.
Participant demographic and epidemiologic characteristics of follow-up samples stratified by vaccine-serotype (VT) and non-VT (NVT) carriage and potential risk factors. a The prevalence of pneumococcal carriage in all samples at each sampling visit stratified by serotype group and human immunodeficiency virus (HIV) status, with an insert showing pneumococcal carriage prevalence of samples aggregated across all visits. b Distribution of pneumococcal carriage density in HIV- adults, adults living with HIV (ALWHIV) on antiretroviral therapy (ART) at most 3 months and at least 1 year. The share of all pneumococcal carriage stratified by serotype group and HIV/ART status among c adults living with 1 child or at least 2 children < 5y, d males or females, e 18–33 years or 34–44 years, f low or high social economic status, and g antibiotic use. h The map shows Blantyre district with circular points on the map indicating the residential location of the adults from whom the nasopharyngeal samples were collected during the study. The size of the circular point is proportion to the number of samples collected in adults from that location. Overall, the map indicates that samples were mostly collected within the high-density informal settlements of urban Blantyre
Pneumococcal carriage acquisition dynamics
The probability that NVT carriage would next be acquired in a non-carrier was generally higher than VT carriage (82.9%, 95% CI: 78.3–86.7% vs 17.1%, 95% CI: 13.4–21.7%). Thus, among ALWHIV on ART > 1y, ALWHIV on ART < 3 m, and HIV-, we respectively estimated the annual acquisition episodes of 5.9 (95% CI: 4.3–7.9), 6.0 (95% CI: 4.4–7.9), and 5.0 (95% CI: 3.8–6.8) for overall carriage, 6.2 (95% CI: 4.4–8.2), 6.0 (95% CI: 4.1–8.4), and 5.0 (95% CI: 3.5–6.9) for NVT carriage, and 0.69 (95% CI: 0.31–1.57), 0.42 (95% CI: 0.19–1.01), and 0.78 (95% CI: 0.40–1.70) for VT carriage.
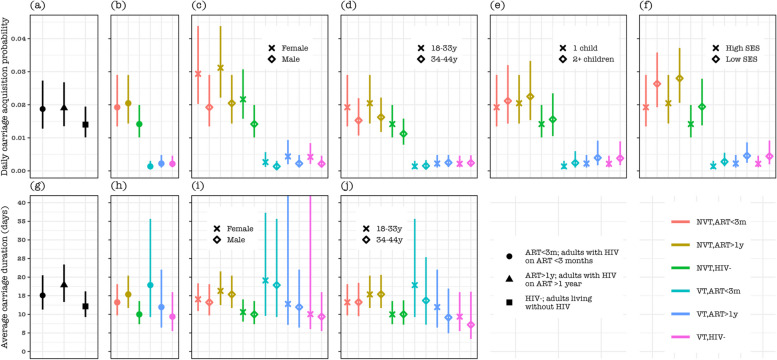
In a multivariate analysis, the pneumococcal acquisition rate was higher among females vs males of overall carriage (hazard ratio [HR]: 1.64, 95% CI: 1.262–2.12), NVT (HR: 1.53, 95% CI: 1.17–2.01), and VT (HR: 1.96, 95% CI: 1.11–3.49), among low vs high SES of overall carriage (HR: 1.47, 95% CI: 1.12–1.94), NVT (HR: 1.38, 95% CI: 1.03–1.83), and VT (HR: 2.06, 95% CI: 1.13–3.77), among adult living with 2 + vs 1 child < 5y of VT (HR: 1.78, 95% CI: 1.05–3.01), and among ALWHIV on ART > 1y than HIV- of NVT (HR: 1.43, 95% CI: 1.01–2.02) (Fig. 2, Table 2, Additional file 1: Table S1). Cut off for age groups is based on the median age of 33 years old VT: serotypes targeted by 13-valency pneumococcal conjugate vaccine (PCV13) NVT: serotypes not targeted by PCV13 ART: antiretroviral therapy HIV-: adults living without human immunodeficiency virus ALWHIV: adults living with human immunodeficiency virus
Fig. 2.
Pneumococcal carriage acquisition probability and duration by serotype group and human immunodeficiency virus (HIV) infection status among potential risk groups. Daily pneumococcal carriage acquisition probability for a overall carriage, and carriage stratified by vaccine-serotype group and HIV status among b all participants, c females or males, d adults aged 18–33 or 34–44 years old (y), e adults living with 1 child or at least 2 children in the house, and f adults in low or high social economic status (SES). Pneumococcal carriage duration in days for g overall carriage, and carriage stratified by vaccine-serotype group and HIV status among h all participants, i females or males, and j adults aged 18–33 or 34–44 years old (y)
Table 2.
The effect of each considered risk factor on pneumococcal acquisition and clearance rates estimated from the Markov model using data from a longitudinal nasopharyngeal swabbing study conducted in Blantyre, Malawi, between September 2021 and December 2023
| Description | HR (95% CI)a | HR (95% CI)a | HR (95% CI)a |
|---|---|---|---|
| Total carriage | VT carriage | NVT carriage | |
| Daily pneumococcal carriage acquisition | |||
| HIV/ART status | |||
| HIV- | Reference | Reference | Reference |
| ALWHIV ART < 3 months | 1.33 (0.95–1.86) | 0.62 (0.30–1.25) | 1.35 (0.94–1.92) |
| ALWHIV ART > 1 year | 1.34 (0.97–1.87) | 1.03 (0.52–2.01) | 1.43 (1.01–2.02)b |
| Sex | |||
| Male | Reference | Reference | Reference |
| Female | 1.64 (1.262–2.12)* | 1.96 (1.11– 3.49)* | 1.53 (1.17–2.01)b |
| Age group | |||
| 18–33 years | Reference | Reference | Reference |
| 34–44 years | 0.86 (0.66–1.12) | 1.13 (0.65–1.97) | 0.79 (0.60–1.04) |
| Number of under 5y children in the house | |||
| One child | Reference | Reference | Reference |
| Two or more children | 1.06 (0.81–1.38) | 1.78 (1.05–3.01)* | 1.10 (0.84–1.45) |
| Social economic status (SES) | |||
| High | Reference | Reference | Reference |
| Low | 1.47 (1.12–1.94)* | 2.06 (1.13–3.77)* | 1.38 (1.03–1.83)b |
| Daily pneumococcal carriage clearance | |||
| HIV/ART status | |||
| HIV- | Reference | Reference | Reference |
| ALWHIV ART < 3 months | 0.80 (0.59–1.10) | 0.53 (0.25–1.10) | 0.76 (0.54–1.05) |
| ALWHIV ART > 1 year | 0.68 (0.50–0.92)* | 0.79 (0.41–1.50) | 0.65 (0.47–0.90)b |
| Sex | |||
| Male | Reference | Reference | Reference |
| Female | 0.97 (0.75–1.24) | 0.93 (0.54–1.60) | 0.94 (0.72–1.23) |
| Age group | |||
| 18–33 years | Reference | Reference | Reference |
| 34–44 years | 1.05 (0.82–1.35) | 1.30 (0.72–2.35) | 1.00 (0.77–1.29) |
SES Social economic status is based on possession index, calculated as a sum of positive responses for household ownership of each of one of 15 different functioning items: watch, radio, bank account, iron (charcoal), sewing machine (electric), mobile phone, CD player, fan (electric), bednet, mattress, bed, bicycle, motorcycle, car, and television
aHR refers to hazard ratio of the incidence or clearance rates
bStatistically significant at 95% confidence intervals (95% CI)
Pneumococcal carriage duration dynamics
The average overall carriage duration was slightly higher among ALWHIV on ART > 1y (17.9 days, 95% CI: 13.7–23.6) compared to ALWHIV on ART < 3 m (15.2 days, 95% CI: 11.2–20.4) or HIV- adults (12.2 days, 95% CI: 9.2–16.1). In a stratified analysis, the average carriage duration was comparable between VT (9.4 days, 95% CI: 5.5–16.0) and NVT (9.9 days, 95% CI: 7.3–13.6) HIV- carriers. However, it was lower for NVT (13.2 days, 95% CI: 9.7–18.1) than VT (17.9 days, 95% CI: 9.3–35.7) in ALWHIV on ART < 3 m carriers, and higher for NVT (15.4 days, 95% CI: 11.7–20.4) than VT (11.9 days, 95% CI: 6.4–22.0) in ALWHIV on ART > 1y carriers.
In a multivariate analysis, pneumococcal carriage clearance was slower among ALWHIV on ART > 1y compared to HIV- adults for overall carriage (hazard ratio [HR]: 0.68, 95% CI: 0.50–0.92) and NVT carriage (HR: 0.65, 95% CI: 0.47–0.90), and comparable between ALWHIV on ART < 3 months and HIV- adults for overall carriage (0.80, 95% CI: 0.59–1.10) and NVT (0.76, 95% CI: 0.54–1.05) (Fig. 2, Table 2, Additional file 1: Table S2).
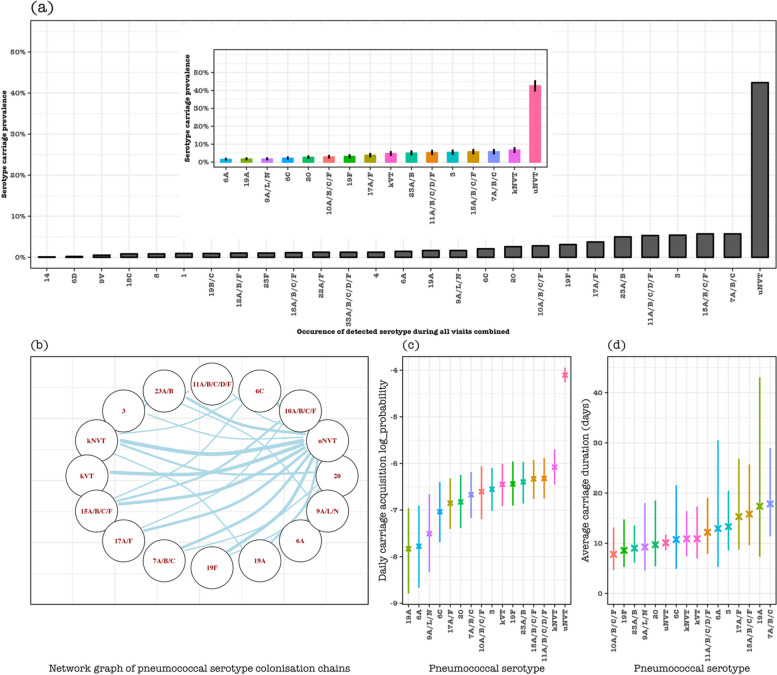
Pneumococcal serotype-specific carriage dynamics
In all adults, the sampling frequency of identified pneumococcal serotypes ranged from n = 1 (0.01%) for serotype 14 to n = 55 (5.7%) for serogroup 15 or serotype 7A/B/C, with n = 410 (42.5%) of NVT with unknown serotype (uNVT), e.g. NVT not assigned a specific serotype, being the largest samples. The overall serotype carriage dynamics without stratifying by HIV status showed that serotypes 3 (0.14%, 95% CI: 0.09–0.23) and 19F (0.16%, 95% CI: 0.10–0.26) among PCV13 serotypes, and serogroup 15 (0.18%, 95% CI: 0.12–0.27), serogroup 11 (0.18%, 95% CI: 0.12–0.28) and 23A/B (0.17%, 95% CI: 0.10–0.26) among non-PCV13 serotypes generally had high daily acquisition probability compared to other serotypes or serogroups. On the other hand, serotypes 19A (17.4 days, 95% CI: 7.3–43.1), 3 (13.3 days, 95% CI: 8.6–20.5) and 6A (12.9 days, 95% CI: 5.3–30.5) among PCV13 serotypes, and 7A/B/C (17.8 days, 95% CI: 11.4–28.9), serogroup 15 (15.8 days, 95% CI: 9.6–25.7), and 17A/F (15.0 days, 95% CI: 8.7–26.8) among non-PCV13 serotype were carried the longest. Co-colonisation of pneumococcal serotypes or serogroup (colonisation chains) was more frequent among NVT (e.g. between NVT with known serotypes [kNVT] and uNVT) than between VT and NVT, with the highest colonisation chains estimated between uNVT and serogroup 15 or kNVT (Fig. 3, Additional file 1: Table S3).
Fig. 3.
Pneumococcal serotype-specific carriage dynamics in considered serotypes with relative high sampling frequency. a Prevalence of each serotype in all samples, with ‘uNVT’ representing unknown non-PCV13 serotypes because they were not included in the serotyping assay which could only identify up to 23 serotypes including all VT. Insert in a is the carriage prevalence of each serotype or serogroup with a relatively high sample frequency, where ‘kVT’ represents known PCV13 serotypes with very low sample frequency (1, 4, 9 V, 14, 18C, and 23F), and ‘kNVT’ represents non-PCV13 serotypes with known serotypes with very low sample frequency (22A/F, serogroup 33 and 18, 12A/B/F, 19B/C, 8, and 6D). b Network diagram showing the acquisition of a serotype replacing a specific serotype in a colonisation chain. The size of the edges reflects the pairs of serotype transition events in the colonisation chain that occur more likely than expected, and the node represents the serotype or serotype group or vaccine-serotype group. c Daily pneumococcal carriage acquisition probability under a log scale and d daily average pneumococcal serotype carriage duration
Discussion
We have used multi-state Markov models to disentangle pneumococcal serotype carriage dynamics in ALWHIV and HIV- adults in a mature infant PCV13 programme in Malawi. We estimate substantial acquisitions of VT and NVT carriage in females and those living under low socioeconomic status. High VT acquisitions among adults living with at least two children < 5y in the house and NVT acquisitions among ALWHIV on ART > 1y are also estimated. On the other hand, prolonged durations of NVT carriage are estimated among ALWHIV on ART > 1y. Residual PCV13 serotypes 19F and 3 are highly acquired, whereas 19A, 3, and 6A are prolongedly carried, although non-PCV13 serotypes remain dominant in circulation among adults. Our findings unravel pneumococcal carriage dynamics among ALWHIV and provide baseline estimates for assessing future pneumococcal vaccine impact in ALWHIV. These results suggest that a PCV strategy in ALWHIV with expanded serotype coverage may be warranted to tackle the remaining preventable burden of pneumococcal carriage and subsequent disease in ALWHIV.
Pneumococcal carriage prevalence has previously been reported to be higher among ALWHIV on ART compared to those not on ART in rural Malawi [8]. Our study shows a similar higher prevalence of pneumococcal carriage in ALWHIV on ART > 1y than those on ART < 3 m or HIV- adults. Follow-up studies are required to investigate the biological factors for the increased pneumococcal prevalence in individuals who have been on ART for an extended period compared to those who recently started treatment. We further show that this elevated carriage in ALWHIV on ART > 1y is likely influenced by frequent acquisitions and prolonged carriage duration of NVT serotypes.
Antibiotic use is sometimes associated with individual carriage reduction [28], but its role was not assessed in this study due to limited data points on antibiotic uptake. Nonetheless, the baseline and follow-up density of pneumococcal carriage remained comparable between HIV groups. Thus, it remains unclear whether the slow NVT clearance is linked to reported cotrimoxazole or penicillin-resistant pneumococci among ALWHIV in this setting [29]. If indeed the reported drugs select for resistant NVT, it may suggest that colonisation of resistant NVT pneumococci in ALWHIV may be inefficiently cleared at the mucosal level, leading to prolonged duration of pneumococcal carriage. However, causal links of prolonged pneumococcal carriage among ALWHIV need further investigation from laboratory measures.
Children < 5y remain the major reservoir of pneumococcal carriage transmission in the era of PCV13 in this setting and elsewhere [15, 16, 25, 30]. Since female adults are more likely to interact with younger children due to cultural and parental roles, social mixing is highly intensive between children and females compared to male adults in this setting [31], likely resulting in higher carriage acquisition risk in females than males consistent with our findings in this study. Furthermore, household spread of pneumococcus is usually influenced by higher household density [25, 32, 33], and having more younger children in the house who are a major reservoir of pneumococcal carriage transmission increases the risk of pneumococcal carriage acquisition [3]. Similarly, higher pneumococcal carriage acquisitions in low than high SES households, as shown here and in previous studies in this setting [3], is likely related to poor living conditions, including poor ventilation and overcrowding. However, fine-scale household pneumococcal carriage dynamics, including quantifying the contribution of different household members to pneumococcal carriage transmission, remain a gap to be addressed in this setting.
Serotype-specific pneumococcal carriage acquisition and clearance estimates reported in our study have implications for the choice of PCV strategy in ALWHIV in this setting. PCV13 serotypes still in circulation underscore inadequate herd immunity from the infant PCV13 programme [15, 16] and suggest that ALWHIV remains at high risk of preventable pneumococcal carriage and subsequent disease [17]. Thus, providing direct PCV protection to ALWHIV or indirect protection by switching to a new infant PCV schedule that substantially improves herd immunity among ALWHIV is urgently needed [18]. The high presence of NVT implies that ALWHIV have the additional risk of pneumococcal disease that may not be prevented by PCV13, necessitating the need for assessing the impact of a newer infant or ALWHIV PCV products with expanded serotype coverage. Of note, serotypes 1 and 5 cause most pneumococcal invasive disease in children in this setting [34], yet were not isolated in adults in this study reflecting that serotypes circulating in carriage do not usually match those in disease as reported by others [35]. Moreover, the extent to which serotypes circulation in adults influence those in children and vice versa remains to be quantified. Thus, the choice of a PCV strategy partly needs to account for the complex interaction between at risk age groups, PCV serotype coverage, and the distribution in serotype carriage and disease in this setting [36].
Our study did not explicitly account for simultaneous carriage of multiple serotypes because latex agglutination was used for serotyping a single bacterial colony [29]. Absence of multiple serotype detection may have biased downward on acquisition rates by missing acquisition events of new serotype while detecting resident serotype and carriage duration by failing to detect serotype when another dominant serotype is present [2]. Another limitation of this study is the lack of serotyping data for all the NVT serotypes. Follow-up studies should use molecular assays or whole-genome sequencing approaches to reliably detect the carriage of multiple serotypes within an individual [37]. Insufficient data points propelled us to combine the carriage of some serotypes targeted or not targeted by PCV13 to estimate serotype dynamics. Although the baseline samples for PCV13 and non-PCV13 serotypes were relatively small, carriage dynamics at baseline were informed by stable rates estimated during the study follow-up where samples were relatively large. The distribution of serotypes in healthy carriers is needed to evaluate PCV impact on invasive disease [19], and our study provides baseline estimates of serotype distribution, acquisition, and clearance at vaccine-serotype group and serotype-specific levels, for assessing future PCV impact in ALWHIV.
Conclusions
The disproportionately high pneumococcal carriage prevalence in ALWHIV on ART > 1y is mostly due to high acquisition and prolonged duration of NVT. Our study provides baseline estimates of pneumococcal serotype dynamics for comparison when new PCV strategies are implemented directly in ALWHIV or indirectly in infants.
Supplementary Information
Additional file 1: Fig. S1 Susceptible-infected-susceptible (SIS) Markov model of pneumococcal carriage dynamics among Malawian adults living with and without human immunodeficiency virus (HIV) between 2021 and 2023. Table S1 Daily acquisition probability of vaccine-serotype (VT) and non-vaccine-serotype (NVT) pneumococcal carriage among adults living with and without HIV estimated from a Markov model. Table S2 Pneumococcal carriage duration (days) of vaccine-serotype (VT) and non-vaccine-serotype (NVT) among adults living with and without HIV estimated from a Markov model. Table S3 Daily pneumococcal serotype carriage acquisition probability and duration (days) of carriage of each serotype among ALWHIV and adult without HIV estimated from a Markov model.
Acknowledgements
The authors thank all community study participants, and the study staff for their support and co-operation during the study.
Authors’ Twitter handles
Twitter handles: @kjambo (KCJ), @JoePhiriMLW (JP), @deusthindwa (DT), @danielavaccines (DMF).
Abbreviations
- NP
Nasopharynx
- ALWHIV
Adults living with human immunodeficiency virus
- ART
Antiretroviral therapy
- HIV
Human immunodeficiency virus
- PCVs
Pneumococcal conjugate vaccines
- PCV13
13-Valent pneumococcal conjugate vaccine
- VT
Vaccine serotype
- NVT
Non-vaccine serotype
- IPD
Invasive pneumococcal disease
- NHSRC
Malawi National Health Sciences Research Ethics Committee
- WHO
World Health Organisation
- SES
Socioeconomic status
- SIS
Susceptible-infected-susceptible
- CFU
Colony forming units
- IQR
Interquartile range
- CI
Confidence interval
- HR
Hazard ratio
- uNVT
Unknown non-vaccine type
- kNVT
Known non-vaccine type
Authors’ contributions
Conceptualization; JP, LS, DT, KCJ Data curation; LS, LM, DT Formal analysis; DT Funding acquisition; KCJ Investigation; LS, LM, DT, KCJ Methodology; JP, CG, LS, DT, KCJ Project administration; JP, KCJ Resources; KCJ Software; DT Supervision; LS, JP, KCJ Validation; KCJ Visualization; DT Writing—original draft; JP, LS, DT, KCJ Writing—review & editing; JP, LS, LM, NM, AK, MK, TK, EL, PK, KM, CC, DMF, DT, KCJ.
Funding
This work was supported by an African Research Leader (ARL) award (MR/T008822/1) to KCJ. This ARL award is jointly funded by the UK Medical Research Council (MRC) and the UK Foreign Commonwealth and Development Office (FCDO) under the MRC/FCDO Concordat agreement and is also part of the EDCTP2 programme supported by the European Union. A Wellcome Strategic award number 206545/Z/17/Z supports MLW. The funders were not involved in the design of the study; in the collection, analysis, and interpretation of the data; and in writing the manuscript. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funders.
Availability of data and materials
An R script that was used to analyse the datasets is available in the GitHub repository https://github.com/deusthindwa/markov.model.pneumococcus.hiv.malawi.
Declarations
Ethics approval and consent to participate
Nasomune study nasopharyngeal (NP) samples were obtained from each Malawian adult through written consent. Study ethics approval was granted by the Malawi National Health Sciences Research Ethics Committee (NHSRC) (21/24/2680) and the Liverpool School of Tropical Medicine Research Ethics (21–035) in accordance with the Declaration of Helsinki. Written informed consent to participate was obtained from all of the participants in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Joseph Phiri and Lusako Sibale contributed equally to this work.
Deus Thindwa and Kondwani Jambo contributed equally to this work.
Contributor Information
Deus Thindwa, Email: deus.thindwa@gmail.com.
Kondwani Jambo, Email: kondwani.jambo@lstmed.ac.uk.
References
- 1.Zhang L, Li Z, Wan Z, Kilby A, Kilby JM, Jiang W. Humoral immune responses to Streptococcus pneumoniae in the setting of HIV-1 infection. Vaccine. 2015;33(36):4430–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipsitch M, Abdullahi O, D’Amour A, Xie W, Weinberger DM, Tchetgen Tchetgen E, Scott JA. Estimating rates of carriage acquisition and clearance and competitive ability for pneumococcal serotypes in Kenya with a Markov transition model. Epidemiology. 2012;23(4):510–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thindwa D, Mwalukomo TS, Msefula J, Jambo KC, Brown C, Kamng’ona A, Mwansambo C, Ojal J, Flasche S, French N, et al. Risk factors for pneumococcal carriage in adults living with HIV on antiretroviral therapy in the infant pneumococcal vaccine era in Malawi. AIDS. 2022;36(14):2045–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wahl B, O’Brien KL, Greenbaum A, Majumder A, Liu L, Chu Y, Lukšić I, Nair H, McAllister DA, Campbell H, et al. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: global, regional, and national estimates for 2000–15. Lancet Glob Health. 2018;6(7):e744–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Aalst M, Lotsch F, Spijker R, van der Meer JTM, Langendam MW, Goorhuis A, Grobusch MP, de Bree GJ. Incidence of invasive pneumococcal disease in immunocompromised patients: a systematic review and meta-analysis. Travel Med Infect Dis. 2018;24:89–100. [DOI] [PubMed] [Google Scholar]
- 6.Harries AD, Ford N, Jahn A, Schouten EJ, Libamba E, Chimbwandira F, Maher D. Act local, think global: how the Malawi experience of scaling up antiretroviral treatment has informed global policy. BMC Public Health. 2016;16(1):938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health (MOH), Malawi. Malawi Population-based HIV Impact Assessment 2020- 2021 (MPHIA 2020-2021): Final Report. Lilongwe: MOH, Malawi; 2022.
- 8.Heinsbroek E, Tafatatha T, Phiri A, Ngwira B, Crampin AC, Read JM, French N. Persisting high prevalence of pneumococcal carriage among HIV-infected adults receiving antiretroviral therapy in Malawi: a cohort study. AIDS. 2015;29(14):1837–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi YH, Andrews N, Miller E. Estimated impact of revising the 13-valent pneumococcal conjugate vaccine schedule from 2+1 to 1+1 in England and Wales: a modelling study. PLoS Med. 2019;16(7): e1002845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flasche S, Lipsitch M, Ojal J, Pinsent A. Estimating the contribution of different age strata to vaccine serotype pneumococcal transmission in the pre vaccine era: a modelling study. BMC Med. 2020;18(1):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mvula H, Heinsbroek E, Chihana M, Crampin AC, Kabuluzi S, Chirwa G, Mwansambo C, Costello A, Cunliffe NA, Heyderman RS, et al. Predictors of uptake and timeliness of newly introduced pneumococcal and rotavirus vaccines, and of measles vaccine in rural Malawi: a population cohort study. PLoS ONE. 2016;11(5): e0154997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsega A, Hausi H, Chriwa G, Steinglass R, Smith D, Valle M. Vaccination coverage and timely vaccination with valid doses in Malawi. Vaccine Reports. 2016;6:8–12. [Google Scholar]
- 13.Immunisation schedules - Africa. Vaccines for Africa. https://health.uct.ac.za/vacfa/about-vaccines/immunization-schedules-africa.
- 14.Swarthout TD, Henrion MYR, Thindwa D, Meiring JE, Mbewe M, Kalizang’Oma A, Brown C, Msefula J, Moyo B, Mataya AA, et al. Waning of antibody levels induced by a 13-valent pneumococcal conjugate vaccine, using a 3 + 0 schedule, within the first year of life among children younger than 5 years in Blantyre, Malawi: an observational, population-level, serosurveillance study. Lancet Infect Dis. 2022;22(12):1737–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lourenco J, Obolski U, Swarthout TD, Gori A, Bar-Zeev N, Everett D, Kamng’ona AW, Mwalukomo TS, Mataya AA, Mwansambo C, et al. Determinants of high residual post-PCV13 pneumococcal vaccine-type carriage in Blantyre, Malawi: a modelling study. BMC Med. 2019;17(1):219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swarthout TD, Fronterre C, Lourenco J, Obolski U, Gori A, Bar-Zeev N, Everett D, Kamng’ona AW, Mwalukomo TS, Mataya AA, et al. High residual carriage of vaccine-serotype Streptococcus pneumoniae after introduction of pneumococcal conjugate vaccine in Malawi. Nat Commun. 2020;11(1):2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bar-Zeev N, Swarthout TD, Everett DB, Alaerts M, Msefula J, Brown C, Bilima S, Mallewa J, King C, von Gottberg A, et al. Impact and effectiveness of 13-valent pneumococcal conjugate vaccine on population incidence of vaccine and non-vaccine serotype invasive pneumococcal disease in Blantyre, Malawi, 2006–18: prospective observational time-series and case-control studies. Lancet Glob Health. 2021;9(7):e989–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thindwa D, Pinsent A, Ojal J, Gallagher KE, French N, Flasche S. Vaccine strategies to reduce the burden of pneumococcal disease in HIV-infected adults in Africa. Expert Rev Vaccines. 2020;19(11):1085–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Flasche S, Le Polain de Waroux O, O’Brien KL, Edmunds WJ. The serotype distribution among healthy carriers before vaccination is essential for predicting the impact of pneumococcal conjugate vaccine on invasive disease. PLoS Comput Biol. 2015;11(4):e1004173. [DOI] [PMC free article] [PubMed]
- 20.Molesworth AM, Ndhlovu R, Banda E, Saul J, Ngwira B, Glynn JR, Crampin AC, French N. High accuracy of home-based community rapid HIV testing in rural Malawi. J Acquir Immune Defic Syndr. 2010;55(5):625–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Health MMo. Malawi guidelines for clinical management of HIV in children and adults. Lilongwe: Malawi Ministry of Health; 2018.
- 22.Satzke C, Turner P, Virolainen-Julkunen A, Adrian PV, Antonio M, Hare KM, Henao-Restrepo AM, Leach AJ, Klugman KP, Porter BD, et al. Standard method for detecting upper respiratory carriage of Streptococcus pneumoniae: updated recommendations from the World Health Organization Pneumococcal Carriage Working Group. Vaccine. 2013;32(1):165–79. [DOI] [PubMed] [Google Scholar]
- 23.Swarthout TD, Gori A, Bar-Zeev N, Kamng'ona AW, Mwalukomo TS, Bonomali F, Nyirenda R, Brown C, Msefula J, Everett D et al: Evaluation of pneumococcal serotyping of nasopharyngeal-carriage isolates by latex agglutination, whole-genome sequencing (PneumoCaT), and DNA microarray in a high-pneumococcal-carriage-prevalence population in Malawi. J Clin Microbiol 2020;59(1). [DOI] [PMC free article] [PubMed]
- 24.Gritzfeld JF, Cremers AJ, Ferwerda G, Ferreira DM, Kadioglu A, Hermans PW, Gordon SB. Density and duration of experimental human pneumococcal carriage. Clin Microbiol Infect. 2014;20(12):O1145-1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thindwa D, Wolter N, Pinsent A, Carrim M, Ojal J, Tempia S, Moyes J, McMorrow M, Kleynhans J, Gottberg AV, et al. Estimating the contribution of HIV-infected adults to household pneumococcal transmission in South Africa, 2016–2018: a hidden Markov modelling study. PLoS Comput Biol. 2021;17(12): e1009680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jackson C. Multi-state models for panel data: the msm package for R. J Stat Softw. 2011;38(8):1–28. [Google Scholar]
- 27.Powell M. The BOBYQA algorithm for bound constrained optimization without derivatives; 2009.
- 28.Coulibaly B, Sie A, Kiemde D, Dembele N, Compaore A, Dabo O, Dah C, Ouermi L, Cevallos V, Lebas E, et al. Pneumococcal carriage and antibiotic resistance in children younger than 5 years in Nouna District, Burkina Faso. Am J Trop Med Hyg. 2020;103(2):684–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sibale L, Phiri J, Mitole N, Kalata N, Nyazika T, Kalirani A, Khwiya M, Sagawa G, Thindwa D, Swarthout TD, et al. Frequent shedding of multi-drug resistant pneumococci among adults living with HIV on suppressive antiretroviral therapy in Malawi. Medrxiv. 2022. Pre-print.
- 30.Chaguza C, Senghore M, Bojang E, Lo SW, Ebruke C, Gladstone RA, Tientcheu PE, Bancroft RE, Worwui A, Foster-Nyarko E, et al. Carriage dynamics of pneumococcal serotypes in naturally colonized infants in a rural African setting during the first year of life. Front Pediatr. 2020;8: 587730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thindwa D, Jambo KC, Ojal J, MacPherson P, Dennis Phiri M, Pinsent A, Khundi M, Chiume L, Gallagher KE, Heyderman RS, et al. Social mixing patterns relevant to infectious diseases spread by close contact in urban Blantyre, Malawi. Epidemics. 2022;40:100590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melegaro A, Choi Y, Pebody R, Gay N. Pneumococcal carriage in United Kingdom families: estimating serotype-specific transmission parameters from longitudinal data. Am J Epidemiol. 2007;166(2):228–35. [DOI] [PubMed] [Google Scholar]
- 33.Melegaro A, Gay NJ, Medley GF. Estimating the transmission parameters of pneumococcal carriage in households. Epidemiol Infect. 2004;132(3):433–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirolos A, Swarthout TD, Mataya AA, Bonomali F, Brown C, Msefula J, Bar-Zeev N, Iroh Tam PY, Alaerts M, Bilima S, et al. Invasiveness potential of pneumococcal serotypes in children after introduction of PCV13 in Blantyre, Malawi. BMC Infect Dis. 2023;23(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brueggemann AB, Griffiths DT, Meats E, Peto T, Crook DW, Spratt BG. Clonal relationships between invasive and carriage Streptococcus pneumoniae and serotype- and clone-specific differences in invasive disease potential. J Infect Dis. 2003;187(9):1424–32. [DOI] [PubMed] [Google Scholar]
- 36.Colijn C, Corander J, Croucher NJ. Designing ecologically optimized pneumococcal vaccines using population genomics. Nat Microbiol. 2020;5(3):473–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Knight JR, Dunne EM, Mulholland EK, Saha S, Satzke C, Tothpal A, Weinberger DM: Determining the serotype composition of mixed samples of pneumococcus using whole-genome sequencing. Microb Genom 2021;7(1). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Fig. S1 Susceptible-infected-susceptible (SIS) Markov model of pneumococcal carriage dynamics among Malawian adults living with and without human immunodeficiency virus (HIV) between 2021 and 2023. Table S1 Daily acquisition probability of vaccine-serotype (VT) and non-vaccine-serotype (NVT) pneumococcal carriage among adults living with and without HIV estimated from a Markov model. Table S2 Pneumococcal carriage duration (days) of vaccine-serotype (VT) and non-vaccine-serotype (NVT) among adults living with and without HIV estimated from a Markov model. Table S3 Daily pneumococcal serotype carriage acquisition probability and duration (days) of carriage of each serotype among ALWHIV and adult without HIV estimated from a Markov model.
Data Availability Statement
An R script that was used to analyse the datasets is available in the GitHub repository https://github.com/deusthindwa/markov.model.pneumococcus.hiv.malawi.