Abstract
Background
Epilepsy remains a significant public health concern in Tanzania, with affected individuals enduring stigma, whether through actions or perceptions. Myths, misunderstandings, and misconceptions about epilepsy have persisted due to a multitude of factors. Here, we assessed attitudes and perceptions toward epilepsy in Mahenge.
Methods
A cross-sectional study utilising a mixed-methods approach was undertaken in eight villages in the Ulanga district of Mahenge, integrating a semi-structured questionnaire and focus group discussions (FGDs). The questionnaire involved 778 community members, and 15 FGDs were conducted (seven groups with people with epilepsy and eight without). Descriptive statistics, chi-square, and logistic regression were used for quantitative analysis, while we used NVivo version 14 for thematic analysis of qualitative data.
Results
Of 778 participants, over half were women (425, 54.6%) with a median age of 41 years (IQR: 30–55) and most had completed primary education (79.9%). The majority of participants were aware of epilepsy (96.8%), yet they displayed low knowledge (51%), negative attitudes (45.5%), and perceptions (42.1%) towards the disorder. A low level of understanding was significantly associated with negative attitudes (Adjusted Odds Ratio [AOR] = 1.89, 95%CI: 1.41–2.53) and perceptions (AOR = 3.22, 95%CI: 2.05–5.04) towards epilepsy. In the qualitative analysis, often hereditary factors and infections were named as causes of epilepsy, along with misconceptions involving witchcraft and divine punishment. There was also a misconception about the contagiousness of epilepsy. Traditional healers were often the initial point of treatment. Epilepsy-related stigma was evident, with individuals with epilepsy facing derogatory labels, social isolation, and barriers to education. Lastly, there was a lack of understanding regarding a possible association between epilepsy and onchocerciasis.
Conclusions
Despite high awareness of epilepsy, there is insufficient understanding, negative attitudes, and perceptions, including misconceptions and stigma about this neurologic condition. Community-based education programmes are essential for promoting proper healthcare-seeking behaviour and dispelling myths.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20108-5.
Keywords: Attitudes, Perceptions, Epilepsy, Stigma, Onchocerciasis, Mahenge, Tanzania
Background
Epilepsy remains a prevalent neurological condition, impacting over 50 million individuals globally [1]. The majority of people with epilepsy, around 80%, live in low- and middle-income countries [1]. While its causes are diverse and not fully elucidated, studies have highlighted brain infections, severe head trauma, and perinatal factors as primary risk factors for epilepsy in these settings [1–3]. Parasitic infections like onchocerciasis, neurocysticercosis, cerebral malaria, echinococcosis, and toxoplasmosis have been linked to epilepsy in endemic regions [2, 3].
A high prevalence of epilepsy has been reported in regions where onchocerciasis is prevalent, particularly with suboptimal onchocerciasis elimination programmes [4–6]. The term “onchocerciasis-associated epilepsy” (OAE) was introduced to describe this connection in onchocerciasis endemic areas [7]. Globally, it is estimated that over 381,000 individuals are affected by OAE, presenting with various phenotypes, such as the nodding and nakalanga syndromes [8, 9].
Studies across five African nations, Tanzania, Kenya, Uganda, South Africa, and Ghana, showed epilepsy prevalence rates ranging from 7 to 15 cases per 1000 individuals [3]. Tanzanian studies have reported epilepsy prevalence ranging from 2.2 to 37.1/1,000 people, with prevalence in rural areas higher than in urban areas [10–12]. Onchocerciasis-endemic foci, notably Ulanga (Mahenge), are of significant interest due to previous reports of an association between onchocerciasis and epilepsy, including nodding syndrome [13–16]. The exact mechanism by which onchocerciasis could trigger epilepsy remains unclear [17]. Mahenge is one of Tanzania’s eight onchocerciasis foci, with the condition being highly prevalent since the 1960s [18, 19]. In this area, a peculiar head-nodding syndrome, accompanied by seizures and psychotic episodes among children with epilepsy, was first reported in 1965 [20, 21]. Subsequent studies from Mahenge have highlighted a mounting epilepsy burden alongside persistent onchocerciasis transmission [14, 15].
People with epilepsy encounter psychological, intellectual, physical, and social constraints, potentially leading to long-lasting disabilities and in severe cases, fatal incidents such as drowning, burns, sudden death or suicide [22, 23]. Despite its significant impact, epilepsy is often misunderstood and stigmatised due to persistent misunderstanding, negative attitudes, and perceptions [24, 25]. A 2019 socio-anthropological study in Mahenge focused on the knowledge, attitudes, and perceptions surrounding epilepsy. The investigation uncovered misconceptions about the causes, a lack of awareness regarding the association between onchocerciasis and epilepsy, instances of discrimination and stigmatisation, and a lack of educational opportunities [26]. The study was not designed to quantify to what extent these factors persisted in this community. We now aim to quantify the magnitude/levels of community awareness, knowledge, attitudes, and perceptions toward epilepsy in the Ulanga district. The findings may serve as a basis for developing a community-based epilepsy awareness campaign, which could be incorporated into the ongoing onchocerciasis control programme.
Materials and methods
Study setting
The setting was the Ulanga district in the Morogoro region. The district is bordered to the east by the Lindi Region, to the south by the Ruvuma Region, and to the north and west by the Kilombero District [27]. Ulanga district covers an area of 24,460 square kilometres divided into 59 villages, with an approximate population of 265,000 [27, 28]. The district is mountainous with fast-flowing rivers favouring the breeding of Simulium damnosum s.l, a vector for onchocerciasis. The economic activities of Ulanga include small-scale farming, animal husbandry, and mining. The Ulanga district was selected due to the high prevalence of epilepsy and onchocerciasis despite more than 25 years of ongoing community-directed treatment with ivermectin (CDTI) [14, 15, 29].
Study design
This community-based cross-sectional study was conducted between August and September 2023 using concurrent triangulation mixed data collection methods.
Study population
The population consisted of Mahenge residents who were 18 years or older, able to communicate, and willing to participate in the study.
Sample size and sampling procedure
Quantitative
The sample size for the quantitative survey was estimated using the infinite population formula for proportion, (n = z2P(100-P)/ε2) [30]. In this formula, n is the minimum required sample size; z is the standard normal deviate, which is 1.96 for a 95% confidence level; P is the proportion of the exploratory variables, set at 50% to yield the maximum sample size given a 5% type one error rate; and ε denotes the margin of error, set at 5%. We considered a design effect of 2 and a 10% non-response rate to account for heterogeneity between the study villages. The total sample size was 845 community members.
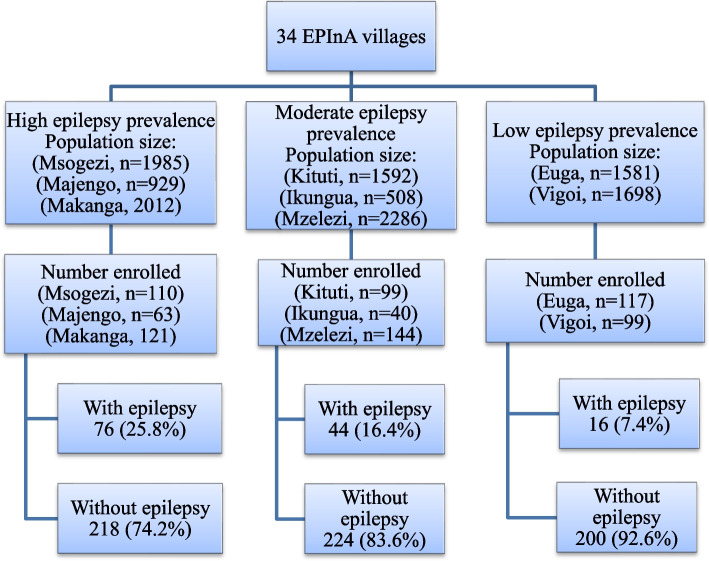
We used the multistage sampling technique, described in detail in Fig. 1. Before sampling, the villages were stratified based on onchocerciasis and epilepsy, which in this area are endemic to high, moderate, and low. Then, eight villages (three from high endemicity, three from moderate, and two from low) were randomly selected. In each of the selected villages, a total population was obtained to determine the total number of participants for recruitment per selected village. At the village level, households where participants live were chosen randomly, with the village with more residents contributing to a higher number of participants and vice versa. 778 community members were recruited. Two of the villages selected (Msogezi and Mzelezi) were involved in previous studies, including an epilepsy surveillance system [14].
Fig. 1.
Flowchart of sampling procedures
Qualitative
The eight villages sampled for the quantitative survey were selected purposefully for the qualitative part. Two FGDs were conducted in each of the selected villages, with participants grouped based on their epilepsy status; one group comprised individuals with epilepsy, while the other group included those without epilepsy to ensure freedom of expression during the discussions. Between 8 and 12, either males or females were selected for each FGD.
Data collection
Quantitative
A structured questionnaire was used to collect data among study participants. Data were collected electronically on tablets and computers through the open-source software Open Data Kit (ODK) [https://opendatakit.org/]. The questionnaire had four sections: socio-demographic, awareness and knowledge, attitudes, and perceptions toward epilepsy. Data were collected in Kiswahili. English and Kiswahili versions of the questionnaire are supplied as additional files 1 and 2.
Qualitative
The interview guide, comprised of open-ended questions, was formulated to explore the respondents’ knowledge, attitudes, and perceptions toward epilepsy in the community. The guide had six sections exploring general health problems affecting the Mahenge community, information about epilepsy and onchocerciasis, knowledge, attitudes, and perceptions about epilepsy, and recommendations for improving onchocerciasis and epilepsy services in Mahenge. Fifteen FGDs (seven with people with epilepsy and eight with people without epilepsy) were held in the eight selected villages at their village offices in Kiswahili. The FGDs lasted about 45 min to an hour, and with the participant’s consent, the FGDs were audio-taped. Data collection stopped upon reaching saturation point, as repetitive information emerged frequently. Participant study numbers replaced names to maintain confidentiality. English and Kiswahili versions of the interview guide are provided as additional files 3 and 4.
Quality control
The questionnaire was pre-tested among the 25 community members in Mahenge, and the interview guide was pre-tested in two FGDs, each with people with and without epilepsy in Vigoi village. Pre-testing aimed to check the flow of the questions and participants’ understanding of the questions. The results of pre-testing were used to improve the tools before data collection.
Data management and analysis
Quantitative
Cleaned data were exported into STATA version 17 (Stata Corp Inc., TX, USA) and R. version 4.0.3 (R Core Team 2020, Vienna, Austria) for analysis. The categorical variables were summarised using descriptive statistics into frequencies, which were reported as proportions with associated 95% confidence intervals (95%CI). In contrast, continuous variables were summarised using either means (with 95%CI) or medians (with interquartile range [IQR]). We used Pearson’s chi-square test to compare proportions between groups, and its p-values were employed with a 5% significance level.
Eleven questions with 34 correct responses were used to measure knowledge and then analysed using a scoring scale. After assigning one score for correct answers and zero for incorrect ones, the sum of responses were obtained and categorised into two groups of knowledge scores: low knowledge (corresponding to scores equal to or below the median) and high level of knowledge for scores above the median.
Attitudes and perceptions were assessed using thirteen-items with a five-point Likert scale. Cronbach’s alpha statistic determined the reliability of the scores in assessing attitudes and perceptions, where the assessment of items fitted in the model was done and excluded variables that were found with low correlations with others to improve Cronbach’s alpha value. For every participant, cumulative scores ranging from 13 to 65 points were computed for the attitude and perception items. Then, the median attitude scores were used to categorise attitudes and perceptions into positive (scores above the median) and negative attitudes/perceptions otherwise.
Univariate and multivariate logistic regression analyses were employed to assess the predictors for KAP. Independent variables with a p-value < 0.25 in the univariate analysis were included in the multivariate analysis. The backward elimination method was used to determine the minimal model with the best fit, while comparisons of the models were done using the loglikelihood ratio test. Variables with p-values < 0.05 were deemed statistically significant, and the estimates with corresponding 95%CI indicated the strength of the association.
Qualitative
The qualitative data analysis was conducted using the thematic framework approach with NVivo 14 (QSR International Pty Ltd., Cardigan, UK). Initially, VPM, ISM, PFM, and RK transcribed the audio data verbatim to obtain a textual format. Subsequently, the investigators (VPM and PFM) read the transcripts multiple times to familiarise themselves. The transcripts were then imported into NVivo, where information was coded inductively to generate initial codes and patterns among the codes were identified and merged to form themes and subthemes. These themes were subsequently reviewed and compared with the dataset to ensure their significant data representation. Lastly, the themes were defined and labelled.
Definition of key terms
Awareness was defined as the extent to which community members are informed about epilepsy or have heard about it, regardless of their depth of understanding. Knowledge, in the context of epilepsy, was defined as the actual understanding or familiarity possessed by community members, representing the depth and accuracy of information. Community members with a knowledge score at or above the median, indicating a deeper and more accurate understanding of epilepsy, were defined as having high knowledge. Conversely, those with scores below the median, reflecting a less comprehensive or accurate understanding, were described as having low knowledge. Attitude was referred to as individuals’ feelings and beliefs towards epilepsy, with negative attitudes defined as biased or discriminatory beliefs, feelings, or behaviours held by individuals or communities toward people with epilepsy. Perception was defined as individuals’ interpretations or subjective views of epilepsy, with negative perceptions referred to as misconceptions, stereotypes, and stigmatising views leading to discrimination and social exclusion.
Results
Quantitative survey
Socio-demographic characteristics of the study participants
Seven hundred seventy-eight people participated, with a median age of 41 years (interquartile range (IQR) of 30–55), achieving a response rate of 92.1% (778/845). Females comprised 54.6% of the participants. The majority (79.9%) of the participants had completed primary school education and were engaged in farming (Table 1).
Table 1.
Socio-demographic characteristics of the study participants (n = 778)
| Variable | n (%) | 95% CI |
|---|---|---|
| Sex | ||
| Males | 353 (45.4) | 41.8–48.9 |
| Females | 425(54.6) | 51.1–58.2 |
| Age (years) | 41, (30–55)a | |
| 18–35 (Young adults) | 301 (38.7) | 35.3–42.2 |
| 36–55 (Middle-aged adults) | 292 (37.5) | 34.1–41.0 |
| ≥ 56 (Older) | 185 (23.8) | 20.8–26.9 |
| Education level | ||
| Never attended school | 69 (8.9) | 7.0–11.1 |
| Primary school | 622 (79.9) | 77.0–82.7 |
| Secondary school | 68 (8.7) | 6.9–10.9 |
| Post-secondary school | 19 (2.4) | 1.5–3.8 |
| Marital status | ||
| Married | 165 (21.2) | 18.4–24.2 |
| Single | 157 (20.2) | 17.4–23.2 |
| Divorced/separated | 39 (5.0) | 3.6–6.8 |
| Cohabiting | 336 (43.2) | 39.8–46.8 |
| Widow(er) | 81 (10.4) | 8.4–12.8 |
| Occupation | ||
| Farmer | 660 (84.8) | 82.6–87.1 |
| Business/Petty business | 65 (8.24) | 6.5–10.5 |
| Employed | 19 (2.3) | 1.4–3.6 |
| Others | 35 (4.5) | 3.2–6.2 |
| Residency (years) | 33 (20–50)a | |
| ≤ 17 | 163 (20.9) | 18.1–24.0 |
| ≥ 18 | 121 (79.1) | 76.0–81.9 |
| Villages per epilepsy prevalence | ||
| Low (Euga and Vigoi) | 216 (27.8) | 24.6–31.1 |
| Moderate (Kituti, Ikungua andMzelezi) | 268 (34.4) | 31.1–37.9 |
|
High (Msogezi, Majengo and Makanaga) |
294 (37.8) | 34.4–41.3 |
aInterquartile range (IQR)
Awareness of epilepsy among participants
Table 2 presents variables associated with participant’s awareness of epilepsy. Of the 778 respondents in the questionnaire survey, 753 (96.8%) were aware of epilepsy, of which around two-thirds, 510 (67.7%), had received epilepsy information from within their communities, friends, or personal experience from the community/family members affected by the disease. Other significant sources of information were community healthcare workers 216 (28.7%), health facilities 183 (24.3%), and mass media, which contributed to 139 (18.5%) (Table 2).
Table 2.
Awareness of epilepsy among participants
| Variable | n (%) |
|---|---|
| Heard of epilepsy (n = 778) | |
| Yes | 753 (96.8) |
| Source of information | |
| Health facility (n = 753) | 183 (24.3) |
| Mass media (n = 753) | 139 (18.5) |
| Community health workers (n = 753) | 216 (28.7) |
| Community, households/friends (n = 753) | 510 (67.7) |
| Had a member of the family with epilepsy (n = 753) | |
| Yes | 136 (18.1) |
| Relationship with family members with epilepsy (n = 136) | |
| Myself | 11 (8.1) |
| Child | 49 (36.0) |
| Parent | 6 (4.4) |
| Sibling/relative | 41 (30.1) |
| Other relatives | 19 (14.0) |
| Others | 10 (7.3) |
Knowledge of epilepsy among participants
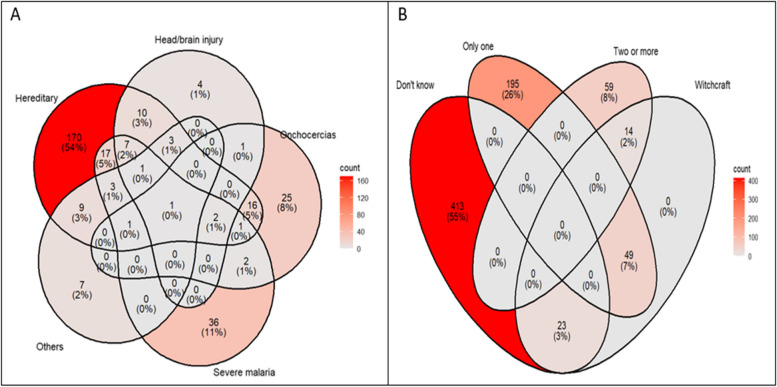
Table 3 presents epilepsy knowledge among participants. The most common causes of epilepsy mentioned were hereditary, 238 (31.6%), severe malaria/febrile convulsion 70 (9.3%), onchocerciasis 49 (6.5%), and head/brain injury 29 (3.9%), Fig. 2A. Witchcraft was mentioned as a cause of epilepsy by 86 (11.4%) participants, making this the second most common attributed cause in these communities. More than half of the participants, 436/753 (57.9%) did not know any of the correct causes of epilepsy, while only 9.7% (73/753) of them knew at least two causes of epilepsy, Fig. 2B.
Table 3.
Knowledge of epilepsy among participants
| Variable | n (%) |
|---|---|
| Causes of epilepsy (each out of 753) | |
| Hereditary | 238 (31.6) |
| Severe malaria/febrile convulsion | 70 (9.3) |
| Onchocerciasis | 49 (6.5) |
| Witchcraft | 86 (11.4) |
| Don’t know | 413 (54.8) |
| Symptoms of epilepsy (each out of 753) | |
| Loss of consciousness plus (foaming, tongue biting, incontinency) | 548 (72.8) |
| Shaking/trembling of part of the body for a short period, but unable to control | 144 (19.1) |
| Head nodding | 44 (5.8) |
| Experiences unusual smells, sounds, or visual hallucinations | 3 (0.4) |
| Changes behaviour | 60 (8.0) |
| Don’t know | 182 (24.2) |
| Epilepsy is an infectious disease (n = 753) | |
| Yes | 165 (21.9) |
| No | 368 (48.9) |
| Don’t know | 220 (29.2) |
| Onchocerciasis causes epilepsy (n = 753) | |
| Yes | 109 (14.5) |
| No | 177 (23.5) |
| Don’t know | 469 (62.0) |
| The most vulnerable population at risk of developing OAE (each out of 753) | |
| Children | 114 (15.4) |
| Adolescents and young adults | 964 (12.7) |
| Adults and Elders | 80 (10.6) |
| Other (pregnant women, any age group, those who do not take ivermectin) | 81 (10.8) |
| Don’t know | 473 (62.8) |
| Epilepsy is treatable (n = 753) | |
| Yes | 391 (51.9) |
| No | 225 (29.9) |
| Don’t know | 137 (18.2) |
| Method of treatment (each out of 391) | |
| Traditional treatment (Herbal remedies or/and traditional healers) | 101 (25.8) |
| Modern treatment | 342 (87.5) |
| Don’t know | 01 (0.3) |
| Ivermectin for onchocerciasis treatment helps to reduce the incidences of OAE (n = 753) | |
| Yes | 192 (25.5) |
| No | 50 (6.6) |
| Don’t know | 511 (67.9) |
| Seizure management (each out of 753) | |
| Keep the individual in a safe place to avoid injury | 374 (49.7) |
| Lay the person on his/her side to enable smooth breathing while unconscious | 244 (32.4) |
| Consult a health facility if an individual remains unconscious for ≥ 5 min | 117 (15.5) |
| Others | 42 (5.6) |
| Don’t know | 233 (30.9) |
| OAE is a preventable disease (n = 753) | |
| Yes | 156 (20.7) |
| No | 73 (9.7) |
| Don’t know | 524 (69.6) |
| Methods of OAE prevention (each out of 156) | |
| Preventive chemotherapy (use of ivermectin treatment) | 156 (99.3) |
| Avoid being bitten by blackflies | 14 (9.0) |
Fig. 2.
Venn diagrams showing participants with correct knowledge of the possible causes of epilepsy A and the distribution of overall participants' knowledge of the causes of epilepsy (B). Don’t know represents participants who did not know any of the right causes of epilepsy; witchcraft represents participants who perceived epilepsy to be caused by witchcraft or superstition, while those indicated as one and two or more represent those who knew one or more causes of epilepsy. Colour intensity increases with the count
Loss of consciousness with foaming at the mouth, tongue biting, and incontinence were the most common symptoms mentioned by most of the participants, 548 (72.8%). A small proportion (20.7%) knew OAE could be prevented, with ivermectin treatment being the most recognised preventive measure (99.3%), Table 3.
Factors associated with low levels of knowledge of epilepsy
The median knowledge score was 4, ranging from 0 to 16. Of 384 individuals (51%) were categorised as having low knowledge (with scores ranging from 0 to 4), while the rest had high levels.
Low knowledge was associated with age, with individuals aged 36–55 having a 30% lower odds of low knowledge, while those aged 56 and above had a 24% lower odds compared to the 18–35 age group. Females had a slightly higher odds ratio of having low knowledge compared to males (OR = 1.35, 95%CI: 0.997–2.178, p = 0.057). Participants from villages involved in epilepsy surveillance had a lower odds ratio of lower knowledge (p = 0.001). In comparison, participants from the villages with a moderate epilepsy prevalence showed a trend of higher odds ratio of low knowledge (p = 0.052) than those villages with low prevalence. Other variables with significant effects were education and marital status, where widow(er) had a higher odds ratio of low knowledge than married participants, Table 4.
Table 4.
Factors associated with low knowledge in univariate and multivariate models
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| cOR (95%CI) | P-value | aOR (95%CI) | P-value | |
| Age group | ||||
| 18–35 | Ref | Ref | ||
| 36–55 | 0.705 (0.507—0.98) | 0.038 | 0.57 (0.395—0.822) | 0.003 |
| 56 + | 0.764 (0.527—1.109) | 0.157 | 0.466 (0.292—0.743) | 0.001 |
| Sex | ||||
| Males | Ref | Ref | ||
| Females | 1.485 (1.113—1.982) | 0.007 | 1.348 (0.991—1.834) | 0.057 |
| Villages per epilepsy prevalence | ||||
| Low | Ref | Ref | ||
| Moderate | 1.576 (1.09—2.277) | 0.016 | 1.473 (0.997—2.178) | 0.052 |
| High | 1.139 (0.796—1.629) | 0.476 | 0.896 (0.61—1.316) | 0.576 |
| Epilepsy surveillance | ||||
| No surveillance | Ref | Ref | ||
| Available | 0.61 (0.456—0.815) | 0.001 | 0.604 (0.446—0.819) | 0.001 |
| Education level | ||||
| Never attended school | Ref | Ref | ||
| Primary | 0.581 (0.342—0.988) | 0.045 | 0.522 (0.301—0.908) | 0.021 |
| Secondary | 0.306 (0.15—0.623) | 0.001 | 0.202 (0.092—0.444) | < 0.001 |
| Post-secondary school | 0.107 (0.028—0.408) | 0.001 | 0.088 (0.022—0.359) | 0.001 |
| Family member with epilepsy | ||||
| Yes | Ref | |||
| No | 1.257 (0.866—1.823) | 0.229 | ||
| Marital status | ||||
| Married | Ref | Ref | ||
| Single | 1.45 (0.925—2.274) | 0.105 | 1.182 (0.727—1.921) | 0.501 |
| Divorced/Separated | 1.177 (0.585—2.371) | 0.648 | 0.96 (0.463—1.991) | 0.912 |
| Cohabiting | 1.009 (0.691—1.471) | 0.965 | 0.766 (0.506—1.159) | 0.207 |
| Widow(er) | 1.957 (1.12—3.42) | 0.018 | 1.894 (1.019—3.521) | 0.044 |
| Stay period | ||||
| 0–17 years | Ref | |||
| 18 + years | 1.235 (0.869—1.755) | 0.24 | ||
Attitudes toward epilepsy
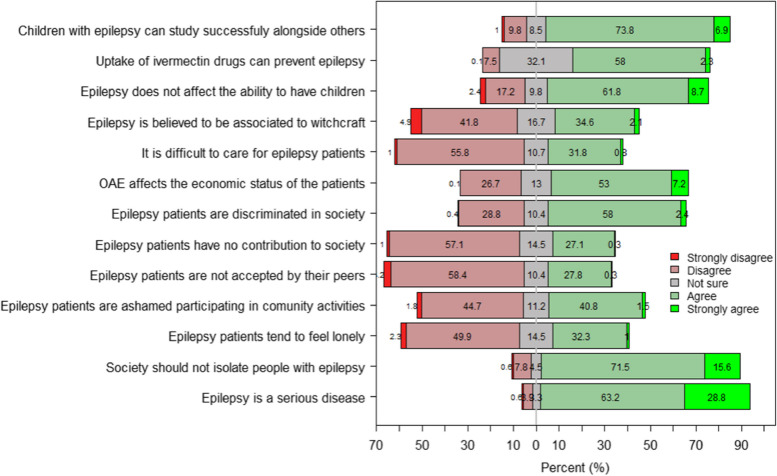
Of the 778 participants, 92% perceived epilepsy as a bad disease, and 27.4% thought that people with epilepsy could not contribute to society. More than half agreed that people with epilepsy are discriminated against in society (60%), and 33.3% agreed that people with epilepsy are lonely and mistreated by the community. 37% of participants agreed that there was an association between epilepsy and witchcraft (Fig. 3).
Fig. 3.
Distribution of scores for items used to assess attitudes toward epilepsy. The score distribution was skewed to the right of the x-axis, showing that more participants agreed with the statements rather than disagreed. A score of zero on the x-axis indicated neutrality
Cronbach’s alpha statistic for attitude was 0.67, which indicates that the reliability was within the acceptable range. Of 778 participants, 424 (54.5%) had positive attitudes toward epilepsy.
Table 5 shows that although several variables were significantly associated with negative attitudes towards people with epilepsy, only three variables in the multivariate model remained significant, which included marital status, where single participants had a higher odds ratio of negative attitudes (p = 0.029) than married participants. The odds ratio for negative attitudes was more than 50% in communities living in the villages with a moderate and high epilepsy prevalence (p ≤ 0.06) when compared to villages with a low prevalence. Communities with low knowledge had a higher odds ratio of negative attitudes (p < 0.001).
Table 5.
Factors associated with negative attitudes in univariate and multivariate models
| Variable | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| cOR | P-value | aOR | P-value | ||
| Age group (years) | |||||
| 18–35 | Ref | ||||
| 36–55 | 0.92 (0.67—1.28) | 0.628 | |||
| ≥ 56 | 0.90 (0.63—1.31) | 0.588 | |||
| Sex | |||||
| Males | Ref | ||||
| Females | 1.15 (0.86—1.53) | 0.339 | |||
| Education level | |||||
| Never attended school | Ref | ||||
| Primary school | 0.88 (0.54—1.45) | 0.621 | |||
| Secondary school | 0.68 (0.34—1.33) | 0.261 | |||
| Post-secondary school | 0.47 (0.16—1.39) | 0.175 | |||
| Marital status | |||||
| Married | Ref | Ref | |||
| Single | 1.77 (1.14—2.76) | 0.012 | 1.65 (1.05—2.60) | 0.029 | |
| Divorced/separated | 0.99 (0.48—2.02) | 0.970 | 0.94 (0.45—1.95) | 0.867 | |
| Cohabiting | 1.29 (0.88—1.88) | 0.191 | 1.24 (0.84—1.83) | 0.272 | |
| Widow(er) | 1.62 (0.95—2.77) | 0.079 | 1.48 (0.85—2.55) | 0.163 | |
| Occupation | |||||
| Peasant | Ref | ||||
| Business/Petty business | 0.67 (0.4—1.13) | 0.13 | |||
| Employed | 0.57 (0.21—1.54) | 0.27 | |||
| Others (from informal sectors) | 0.96 (0.49—1.9) | 0.91 | |||
| Residency (years) | |||||
| ≤ 17 years | Ref | ||||
| > 17 years | 1.04 (0.73—1.47) | 0.836 | |||
| Villages per epilepsy prevalence | |||||
| Low | Ref | Ref | |||
| Moderate | 1.52 (1.05—2.18) | 0.025 | 1.43 (0.98—2.08) | 0.061 | |
| High | 1.55 (1.08—2.21) | 0.017 | 1.55 (1.08—2.23) | 0.019 | |
| Epilepsy surveillance | |||||
| No epilepsy | Ref | ||||
| Available | 0.92 (0.69—1.23) | 0.582 | |||
| Family member with epilepsy | |||||
| No | Ref | ||||
| Yes | 1.19 (0.82—1.73) | 0.355 | |||
| Knowledge score | |||||
| High | Ref | ||||
| Low | 1.95 (1.46—2.60) | < 0.001 | 1.89 (1.41—2.53) | < 0.001 | |
Perceptions towards epilepsy
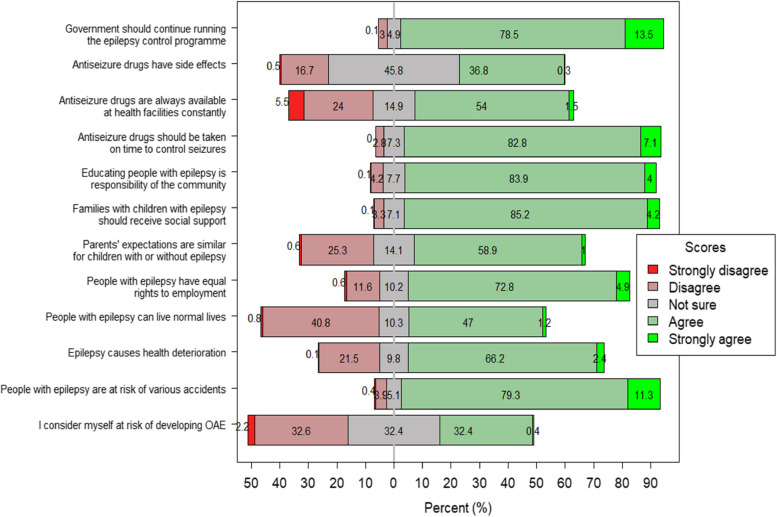
Of 778 participants, 35% disagreed that they were at risk of developing epilepsy, 91% perceived people with epilepsy to be at higher risk of accidents, and 69% perceived them as having deteriorating health conditions. About 42% of participants perceived that people with epilepsy could not live a normal life, while 60% agreed that parental expectations were similar for children with and without epilepsy (Fig. 4).
Fig. 4.
Distribution of scores for items used to assess perception toward epilepsy. The score distribution was skewed to the right of the x-axis, showing that more participants agreed with the statements. A score of zero on the x-axis indicated neutrality
Out of the 13 items collected, 12 were used in Cronbach’s test. The alpha improved from 0.59 to 0.62, just above the lower margin of acceptable reliability (0.61–0.70). Overall, the proportion of people with negative perceptions towards people with epilepsy was 42.1% (95%CI: 38.8–45.6).
Table 6 shows variables significantly associated with negative perceptions in the univariate. Following adjustment for confounders, three variables remained statistically significantly associated with negative perceptions, whereby being single, cohabiting, and widow(er) were associated with a low odds ratio of negative perceptions compared to married. The higher odds ratio of negative perceptions were observed in the villages with a high prevalence (p < 0.001) compared to villages with a lower prevalence. Communities with low knowledge of epilepsy had a higher odds ratio of negative perceptions of epilepsy (p < 0.001) (Table 6).
Table 6.
Factors associated with negative perceptions in univariate and multivariate models
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| cOR | P-value | aOR | P-value | |
| Age group (years) | ||||
| 18–35 | Ref | |||
| 36–55 | 0.96 (0.61—1.5) | 0.850 | ||
| ≥ 56 | 1.16 (0.71—1.9) | 0.557 | ||
| Sex | ||||
| Males | Ref | |||
| Females | 1.12 (0.76—1.66) | 0.564 | ||
| Education level | ||||
| Never attended school | Ref | |||
| Primary school | 0.54 (0.3—0.97) | 0.039 | ||
| Secondary school | 0.47 (0.19—1.14) | 0.093 | ||
| Post-secondary school | 0.36 (0.08—1.72) | 0.200 | ||
| Marital status | ||||
| Married | Ref | Ref | ||
| Single | 0.56 (0.33—0.97) | 0.039 | 0.46 (0.26—0.81) | 0.008 |
| Divorced/separated | 0.73 (0.31—1.72) | 0.473 | 0.61 (0.25—1.5) | 0.285 |
| Cohabiting | 0.32 (0.19—0.52) | < 0.001 | 0.28 (0.16—0.46) | < 0.001 |
| Widow(er) | 0.4 (0.19—0.84) | 0.016 | 0.3 (0.14—0.66) | 0.003 |
| Occupation | ||||
| Peasant | Ref | |||
| Business/Petty business | 0.74 (0.34—1.6) | 0.447 | ||
| Employed | 0.31 (0.04—2.36) | 0.259 | ||
| Others (from informal sectors) | 1.32 (0.56—3.1) | 0.522 | ||
| Residency (years) | ||||
| ≤ 17 years | Ref | |||
| > 17 years | 1.4 (0.84—2.35) | 0.195 | ||
| Villages per epilepsy prevalence | ||||
| Low | Ref | Ref | ||
| Moderate | 1.46 (0.83—2.55) | 0.187 | 1.41 (0.79—2.52) | 0.245 |
| High | 2.31 (1.37—3.9) | 0.002 | 2.65 (1.53—4.57) | < 0.001 |
| Epilepsy surveillance | ||||
| No epilepsy | Ref | |||
| Available | 0.98 (0.66—1.45) | 0.910 | ||
| Family member with epilepsy | ||||
| No | Ref | |||
| Yes | 1.35 (0.78—2.34) | 0.281 | ||
| Knowledge score | ||||
| High | Ref | |||
| Low | 2.96 (1.92—4.57) | < 0.001 | 3.22 (2.05—5.04) | < 0.001 |
Qualitative study
Socio-demographic characteristics of respondents
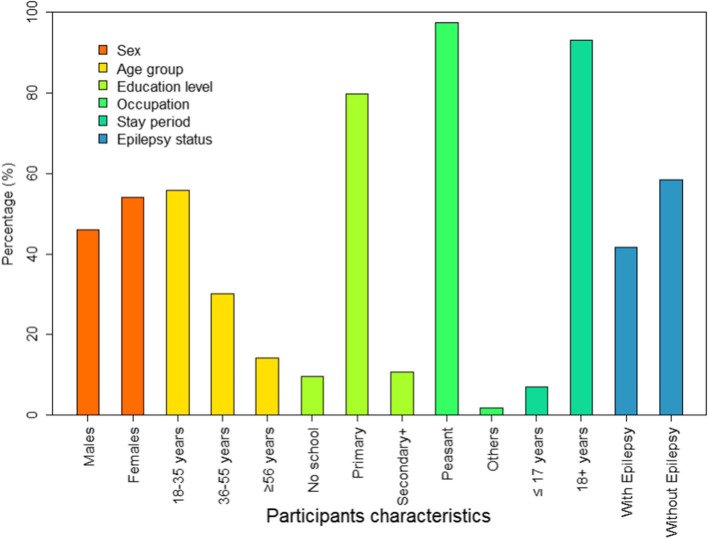
One hundred and thirteen people participated in the 15 FGDs, with 42% of those living with epilepsy, Fig. 5.
Fig. 5.
Socio-demographic characteristics of the study participants in FGDs
Five major themes emerged from the fifteen FGDs.
Theme one: awareness of public health issues in Ulanga
Common diseases and reasons for endemicity in Ulanga district
In the initial theme, which focused on prevalent diseases in the district and how people obtain information about them, epilepsy and onchocerciasis emerged as the most frequently discussed conditions affecting the community in most FGDs across all villages. These were followed by infections, primarily malaria, which was mentioned by respondents from Majengo, Msogezi, and Ikungua, with and without epilepsy. Respondents across all the villages with a high to low prevalence cited heredity and witchcraft as reasons for the high prevalence. At the same time, onchocerciasis was attributed to the abundance of blackflies and malaria to the abundance of mosquitoes.
Source of information regarding endemic diseases in Ulanga district
In discussions on the sources of information about epilepsy, participants brought up additional sources not covered in the questionnaire survey, including sensitisation meetings held within villages and educational sessions conducted at the Mahenge epilepsy clinic.
One of the respondents pointed out:
“Usually, such information comes from the Mahenge Epilepsy clinic. If you visit the clinic and ask, they will let you know, and they provide sessions and make specific announcements at the clinic for people with epilepsy. For instance, they might announce that medications have arrived and are ready for collection.” (R1-FGD, Person without epilepsy, male, 60 years old, from Euga village)
People with epilepsy stated acquiring information about their condition, particularly regarding medications, during clinic visits for prescription refills. In Majengo village, where onchocerciasis is highly prevalent, participants reported receiving information about the disease from community drug distributors (CDDs).
Theme two: knowledge of epilepsy
Understanding of epilepsy (causes, symptoms, treatment, and its association with onchocerciasis)
The findings of the quantitative survey mirrored those of the qualitative study. Hereditary factors and infections emerged as commonly cited causes of epilepsy. In FGDs, respondents who didn’t have epilepsy from Makanga, Kituti, and Euga villages highlighted the significance of hereditary factors, noting that they believe these contribute to the presence of epilepsy across generations within families. Misconceptions from people living with epilepsy were identified, such as viewing epilepsy as a disease from God, linked to witchcraft, and associated with contact with animals. At the same time, the incest relationship was mentioned by people living without epilepsy in Vigoi.
One of the respondents reported.
“While it is acknowledged that epilepsy can be inherited, people often incorporate superstitious beliefs. It seems as though there is a consensus emerging around this notion due to the high burden of epilepsy. This is also why, when seizures occur in young children or adults, instead of seeking medical help, they often end up consulting traditional healers.” (R5-FGD, Persron without epilepsy, male, 29 years old, from Majengo village)
Concerning epilepsy symptoms, they were thoroughly discussed with the participants in all FGDs, mirroring the findings from the questionnaire survey. During FGDs, respondents living without epilepsy in high (Msogezi) and moderate (Mzelezi) onchocerciasis transmission villages mentioned head nodding as an epilepsy symptom. Respondents did not say this in the questionnaire survey. In discussions regarding the link between onchocerciasis and epilepsy, the majority of FGDs expressed uncertainty about an association, citing the distinct symptoms and treatment methods of the two diseases, with some respondents declaring they do not know. Despite this scepticism, a minority of respondents living without epilepsy from three villages of Msogezi, Mzelezi, and Vigoi acknowledged the potential association, particularly emphasising the preventive effect of regular ivermectin uptake in preventing OAE.
There has been a notable misconception in people living with and without epilepsy across all villages about epilepsy transmission, with some believing the disorder to be contagious, potentially transmitted through inhaling flatus, sexual intercourse, saliva, urine, faeces, and coming into contact with the blood of individuals with epilepsy. Similarly, there were misunderstandings regarding the treatment of epilepsy, with some respondents living with epilepsy attributing it to traditional and spiritual forms of healing. Consequently, seeking treatment from traditional healers and spiritual leaders has often been the initial course of action.
One of the respondents reported.
“For epilepsy resulting from bewitchment, traditional healers are available to provide treatment, resulting in complete recovery. However, for the other type of epilepsy, there is no full recovery. If one has been bewitched, they receive effective treatment.” (R2-FGD, Person without epilepsy, male, 59 years old, from Vigoi village)
Respondents living with epilepsy expressed a belief that epilepsy is untreatable. They based this on their prolonged use of medications without seeing significant improvement in their condition, with some still experiencing seizures.
Theme three: attitudes toward epilepsy
The stigma related to epilepsy
During discussions with groups of individuals without epilepsy, it was often mentioned that no discrimination, stigmatisation, or isolation of people with epilepsy was present. They reported treating them like any other individuals, offering support during seizure attacks, assisting with the uptake of antiseizure medications (ASMs), and aiding in daily tasks.
One of the respondents reported.
“Individuals with epilepsy are not subjected to mistreatment by their neighbours; instead, they are cared for and supported. Even if a person’s relative is absent, the community assists and rescues them, especially when they encounter seizures in water. The community demonstrates bravery in rescuing individuals from the water and bringing them safely ashore. Upon receiving news of such incidents and arriving at the scene, one often finds that the individuals have already been rescued. We are sincerely grateful for their actions.” (R9-FGD, Person without epilepsy, female, 39 years old, from Ikungua village)
Respondents who have epilepsy across all the villages stated that they are subjected to derogatory labels such as “crazy” or “mentally ill,” facing discrimination and social exclusion. They are marginalised in social activities, including village meetings, where they are denied opportunities to voice their opinions. They experience isolation from social matters and lack support from community members.
One of the respondents reported.
“We often experience discrimination and mistreatment, as if this condition makes us less of a person. For instance, people label us as mentally ill immediately after mentioning epilepsy. Even in meetings, we are not listened to. When someone with epilepsy tries to speak up, everyone assumes we are mentally disturbed, so there is no value given to what we say. Additionally, in the community, we are not allowed to hunt for animals because seizures can happen to us at any time. This lack of recognition and acceptance in the community can be hurtful to us.” (R5-FGD, Person with epilepsy, male, 24 years old, from Mzelezi village)
Theme four: perceived difficulties of living with epilepsy
Lack of ASMs
During the discussions, the respondents reported the absence of ASMs in their dispensaries and the delayed arrival of medications as crucial challenges, leading to seizure exacerbation. They elaborated that purchasing medicines from local pharmacies is unaffordable due to high prices.
One of the respondents reported.
“The challenges we face include a shortage of medication in dispensaries, coupled with delays in its delivery. Patients frequently endure waiting periods when their medication supply is exhausted due to its unavailability, leading to more seizures. Hence, the government must prioritise ensuring an ample supply of medication.” (R2-FGD, Person without epilepsy, male, 70 years old, from Euga village)
Low socioeconomic status
Respondents who did not have epilepsy reported that having a family member with epilepsy affects household income, as expenses for medication and caregiving add up, potentially reducing the household’s overall financial resources. Respondents with epilepsy reported that if the individual with epilepsy is the breadwinner, their ability to earn and support the family is often compromised due to the challenges posed by frequent seizures.
One of the respondents reported.
“Epilepsy significantly interrupts our daily lives due to frequent episodes of unconsciousness that can impede our participation in activities aimed at enhancing our livelihoods. For example, individuals may be reluctant to engage in farming or gardening due to the fear of experiencing seizures and potentially falling into the water.” (R1-FGD, Person with epilepsy, female, 35 years old, from Mzelezi village)
The transportation expenses incurred when collecting ASMs at the Mahenge epilepsy clinic
Respondents living with epilepsy from Mzelezi reported that they are required to pick up the medication from the Mahenge epilepsy clinic, which means they have to incur transportation costs. As a result, if they don’t have the funds for transportation, they often end up walking long distances or do not go to collect the medication, hence continuing to suffer from seizure attacks.
Consequences of seizures such as injuries and death
During FGDs, respondents without epilepsy highlighted that they have observed frequent seizures can lead to different types of harm for those with epilepsy. They mentioned instances such as drowning during activities like working, bathing, or fetching water from water sources, as well as getting burns while cooking. They pointed out that seizures can sometimes be life-threatening, especially if the person experiencing them is left unattended, highlighting the significance of avoiding leaving them unattended.
One of the respondents reported.
“Living with epilepsy can be challenging, and there is a risk of falling into dangerous areas. Falling into the water, on fire, or onto rocks can lead to serious injuries or even death. In the case of such an incident, time is of the essence; if the person is found quickly, there is a chance they can be saved. However, if the person is alone, the chances of survival are low.” (R5-FGD, Person without epilepsy, male, 68 years old, from Vigoi village)
Denied access to education opportunities
The respondents without epilepsy in most of the villages pointed out that a large number of people with epilepsy are unable to complete their education, particularly if their condition begins while they are still in school. Parents and guardians tend to refrain from enrolling their children in school if they have epilepsy, even if they have attained school age, because of the risks and concerns associated with their condition.
One of the respondents reported.
“In my opinion, some parents refrain from sending their children to school out of fear. They worry that if any problem arises at school, their child may face severe consequences. For instance, if an issue occurs in water, and the child is with classmates who lack the skills to help, it could lead to a fatal outcome.” (R2-FGD, Person without epilepsy, male, 29 years old, from Makanga village)
Theme five: recommendations from FGDs regarding strategies to mitigate epilepsy
Ensuring a sufficient supply of ASMs and timely availability
Most respondents living with epilepsy emphasised the importance of addressing the burden of epilepsy in Ulanga by urging the government to ensure an adequate ASM supply in health facilities to avoid stockouts.
One of the respondents reported.
“I would request the government to take into consideration the situation of people like us who have low socioeconomic status, as we are the most vulnerable and often ignored. Our need for ASMs is significant. Without them, we’re forced to pay very expensive, sometimes as much as one thousand shillings (equivalent to 0.38$) for a single pill. When faced with such dilemmas, like today, when I lack even basic items like salt at home, I have to choose whether to purchase a month’s supply of medication, leaving my family eating food without salt. Therefore, I would like to request the government to prioritise delivering these medications to us, ensuring coverage for both epilepsy and onchocerciasis conditions, as their timely arrival will significantly alleviate our health burdens. My humble request to the government is to take our plight seriously.” (R2-FGD, People with epilepsy, male, 38 years old, from Majengo village)
Provision of health education on epilepsy
The respondents, living with or without epilepsy across the villages with high to low burden, proposed the necessity for health education, emphasising the importance of providing comprehensive information about epilepsy, including covering treatment and management. The respondents from Mzelezi, Majengo, and Makanga suggested that community drug distributors could offer this education during the mass distribution of ivermectin for control of onchocerciasis.
Discussion
The reduction of the epilepsy burden is contingent on high awareness, adequate knowledge, positive attitudes, and positive perceptions. Our findings suggest a considerable degree of epilepsy understanding in Mahenge, presumably due to the epilepsy endemicity, with some villages carrying an epilepsy burden up to four times higher than the national average [11, 14, 31, 32]. The high epilepsy awareness results from various sources of information, including sensitisation meetings held in villages as mentioned in FGDs, sessions broadcasted on Radio Ulanga, firsthand observations of family members or neighbours who have epilepsy, and the presence of a local epilepsy clinic for over 60 years. Similarly, studies elsewhere have demonstrated a high epilepsy awareness within communities where individuals know someone with the condition [25, 33–35]. Despite this high awareness, in some studies, insufficient understanding of epilepsy has been observed among the general population [25, 34, 36].
In qualitative findings, participants demonstrated a strong familiarity with onchocerciasis and malaria as prevalent diseases in the Ulanga community alongside epilepsy. This awareness likely stems from the diseases’ longstanding endemic status in the region since the 1960s, coupled with ongoing interventions like community-directed treatment with ivermectin [18]. Despite epilepsy being recognised widely in Mahenge’s focus, a significant portion of the population living with and without epilepsy lacks a thorough understanding of the condition, primarily because of less well-established health education programmes tailored to close the gap of knowledge in the primary health workers and the community on epilepsy. The misconceptions observed originate from the lack of comprehensive understanding—for example, the misconceptions that witchcraft can cause epilepsy and epilepsy can be effectively treated with traditional medicine—and have led many individuals to seek assistance from traditional healers as their first point of contact. This pattern is not seen in Mahenge alone [26], but across other sub-Saharan countries [37–39]
The symptoms of epilepsy were widely mentioned and discussed in the questionnaire survey and qualitative discussion. The thorough understanding likely stems from the disease’s longstanding presence within their families and community, where individuals have observed seizures experienced by relatives or neighbours. A subgroup of participants lacked knowledge about how to manage seizures, thereby increasing the potential for injury, accidents, complications, and even life-threatening situations for those experiencing seizures. Similarly, in a study conducted in Mahenge in 2019, participants had a strong understanding of the symptoms of epilepsy compared to other aspects of knowledge [26].
Despite the high prevalence of onchocerciasis in the Mahenge focus and ongoing epilepsy research, there remains a lack of awareness among community members about the connection between the two, as revealed by the questionnaire survey and focus group discussions. Similary, onchocerciasis was mentioned infrequently as a cause of epilepsy, even though the study was conducted in an area where the disease is highly endemic, indicating a gap in community knowledge. This knowledge gap could impact efforts to enhance bi-annual ivermectin treatment for onchocerciasis control and prevent OAE incidences. These findings align with studies conducted in countries where onchocerciasis is endemic [40, 41]. Villages under epilepsy surveillance (Mzogezi and Mzelezi) had lower odds of having low knowledge about epilepsy and OAE compared to other villages. Qualitative evidence supports this, indicating that some individuals in surveillance villages significantly understood OAE and nodding syndrome.
The observed improvement of knowledge in villages under surveillance is due to the impact of the four-year-long surveillance associated with health education programmes [29]. Not statistically significant, but villages under epilepsy surveillance experienced an 8% reduction in negative attitudes and a 2% decrease in negative perceptions regarding epilepsy.
Participants aged 36 years and older and those who attained at least a primary education also had lower odds of having low knowledge of epilepsy. This phenomenon might speculate that individuals with primary education and above have greater access to educational materials and resources that cover various health topics, including epilepsy. The older participants, mainly those aged 36 years and above, likely accumulated more life experiences with epilepsy and encountered more information related to it over time. The findings of this study are in agreement with findings from similar studies, which showed individuals with high education levels had better knowledge about epilepsy compared to those with low levels of education [42, 43].
In sub-Saharan Africa, including in Tanzania, epilepsy is among the conditions associated with significant stigma [26, 33, 44, 45]. People living with epilepsy in Mahenge encounter stigma, and discrimination and are subjected to derogatory labels, leading to their exclusion from community activities and opportunities. These negative attitudes significantly impact their emotional and psychological well-being. The community’s stigma surrounding epilepsy prevents affected individuals from disclosing their symptoms or seeking assistance promptly, leading to delays in diagnosis and treatment initiation. This reluctance also discourages them from accessing medical care or following treatment plans, potentially elevating the risk of seizure-related injuries and complications while diminishing their overall quality of life. This underlines the necessity for community interventions aimed at the reduction of stigma associated with epilepsy. Studies conducted in Mahenge and similar contexts have demonstrated that negative attitudes contribute to individuals with epilepsy being denied their rights to education, employment, and marriage [26, 46–48].
People who were single and resided in villages with a high prevalence of epilepsy were more likely to have negative attitudes toward epilepsy. This could be because unmarried individuals, who are often younger, might have had fewer chances to interact with people with epilepsy, unlike those in relationships or married who may have a partner or child with epilepsy. It is, though, essential to recognise that negative attitudes and perceptions toward epilepsy are multifaceted and can vary significantly among individuals regardless of their marital status.
Participants residing in a village with a high prevalence of epilepsy were more likely to have negative attitudes and negative perceptions. This may stem from their frequent exposure to epilepsy-related challenges, including the suffering, discrimination, and isolation experienced by affected individuals, thereby perpetuating negative attitudes and perceptions within these communities. Negative attitudes and perceptions towards epilepsy can significantly impact the quality of life and well-being of people living with epilepsy, as well as impede efforts to promote awareness, acceptance, and support for those affected [49].
A low level of knowledge was the catalyst for negative attitudes and perceptions in this study. Inadequate knowledge about epilepsy leads to misconceptions, which in turn foster fear, stigma, social exclusion, and obstacles to accessing proper healthcare. These results are in line with previous studies in areas where epilepsy is prevalent [33, 50, 51]. Lastly, the findings revealed the unavailability of ASMs in local dispensaries as a significant challenge faced by individuals living with epilepsy. The absence of ASMs in dispensaries could lead to inadequate management of seizures, thereby impacting the quality of life for those affected [52]. Steady access and adequate availability of ASMs in Mahenge are paramount.
Study limitations
The study has several limitations. Firstly, there was a risk of social desirability bias influencing respondents’ answers, although participants were assured that their responses would not have negative consequences. Secondly, the study relied on insights from respondents rather than direct observation within the community, potentially limiting the depth of understanding. Utilising an ethnographic approach could have provided richer insights. Interviewer bias in the quantitative survey was a concern due to the involvement of multiple interviewers. We sought to mitigate this risk by training interviewers before data collection and having all interviewers participate in piloting to minimise bias.
Conclusions and recommendations
Despite high awareness of epilepsy, many individuals had insufficient knowledge coupled with negative attitudes and perceptions toward the condition. Additionally, there was limited knowledge regarding the association between onchocerciasis and epilepsy. There were misconceptions concerning the causes, transmission, and management of epilepsy combined with epilepsy-related stigma. These factors could potentially affect appropriate health-seeking behaviour, although it’s noteworthy that in certain villages, people with epilepsy were not stigmatised. Lastly, the challenges faced by people living with epilepsy included the unavailability of ASMs in local dispensaries and being denied access to education.
We propose that the government, through the Ministry of Health, establish a community-based epilepsy education programme across Tanzania. This programme should provide comprehensive education about epilepsy, including its potential association with onchocerciasis, aiming to change negative attitudes and perceptions and address misconceptions and stigma associated with epilepsy. Ideally, this programme would include schoolchildren embedding learning about epilepsy at a young age. In addition, the government should ensure a consistent and sufficient supply of ASMs in Mahenge. The Ministry of Health should establish an outreach epilepsy care programme aimed at delivering vital services, such as medication, support, and education, to individuals with epilepsy who face challenges accessing traditional healthcare services. The Ministry of Education should create a safe and inclusive environment for children with epilepsy in schools. Collaborating with the Ministry of Health, the Ministry of Education should provide proper training to teachers and school staff on how to support students with epilepsy and respond to seizures effectively. This will create a safer learning environment and encourage children with epilepsy to enrol and stay in schools.
Supplementary Information
Acknowledgements
The authors extend their gratitude to the Ulanga community members who took part in this research, as well as to community leaders for their efforts in mobilising participants, and to the data collectors for their assistance in data collection. Special appreciation is also extended to the Epilepsy Pathway Innovation in Africa (EPInA) project and its team for their support in completing this work.
Abbreviations
- ASMs
Antiseizure Medications
- CDTI
Community Directed Treatment with Ivermectin
- FGDs
Focus Group Discussions
- KAP
Knowledge, Attitudes, and Perceptions
- OAE
Onchocerciasis Associated Epilepsy
Author’s contributions
Conceptualisation: VPM, WK, DB, CRN, and BPM. Data curation: VPM, ISM, DB, and BPM. Formal analysis: VPM, PFM, and BPM. Funding acquisition: CRN and AS. Investigation: VPM, WK, ISM, DB, CRN and BPM. Methodology: VPM, WK, ISM, DB, CRN, and BPM. Writing – original draft: VPM and BPM. Writing – review & editing: VPM, WK, ISM, PFM, DB, REK, HK, HFH, WM, AS, JWS, RC, SM, CRN and BPM, EPInA Study Group. All authors have read and approved the final version of the manuscript.
Funding
This research was commissioned by the National Institute for Health Research (grant number NIHR200134) using Official Development Assistance (ODA) funding. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health and Social Care.
Availability of data and materials
The corresponding author will provide the datasets used in/or analysed during the current work upon reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the National Institute of Medical Research Ethics Committee (NIMR/HQ/R.8a/Vol.IX/3582). Written informed consent was obtained from all participants. Illiterate participants were informed verbally about the study, and then their fingerprints and a witness’s signature were printed on the form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bruno P. Mmbando, Email: b.mmbando@yahoo.com
EPInA Study Group:
Dan Bhwana, Henrika Kimambo, William Matuja, Arjune Sen, Sloan Mahone, Charles R. Newton, Albert Akpalu, Anthony Godi, Bruno Mmbando, Cynthia Sottie, Damazo T. Kadengye, Daniel Mtai Mwanga, Daniel Nana Yaw Abankwah, David McDaid, Dorcas Muli, Emmanuel Darkwa, Frederick Murunga Wekesah, Gergana Manolova, Gershim Asiki, Herieth Hyera, Helen Cross, Isolide Sylvester, Josemir Sander, Mary Bitta, Mercy Atieno, Neerja Chowdhary, Neerja Chowdhary, Patrick Adjei, Pendo Faustine, Peter Otieno, Richard Walker, Ryan Wagner, Sabina Asiamah, Samuel Iddi, Simone Grassi, Sonia Vallentin, Stella Waruingi, Symon Kariuki, Tarun Dua, Thomas Kwasa, Timothy Denison, and Vivian Mushi
References
- 1.WHO. Epilepsy. Available from: https://www.who.int/news-room/fact-sheets/detail/epilepsy. Accessed 3 Feb 2024.
- 2.Kamuyu G, Bottomley C, Mageto J, Lowe B, Wilkins PP, Noh JC, et al. Exposure to multiple parasites is associated with the prevalence of active convulsive epilepsy in sub-Saharan Africa. PLoS Negl Trop Dis. 2014;8(5):e2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ngugi AK, Bottomley C, Kleinschmidt I, Wagner RG, Kakooza-Mwesige A, Ae-Ngibise K, et al. Prevalence of active convulsive epilepsy in sub-Saharan Africa and associated risk factors: cross-sectional and case-control studies. Lancet Neurol. 2013;12(3):253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boussinesq M, Pion SDS, Demanga-Ngangue, Kamgno J. Relationship between onchocerciasis and epilepsy: a matched case-control study in the Mbam Valley, Republic of Cameroon. Trans R Soc Trop Med Hyg. 2002;96(5):537–41. [DOI] [PubMed] [Google Scholar]
- 5.Pion SDS, Kalser C, Boutros-Toni F, Cournil A, Taylor MM, Meredith SEO, et al. Epilepsy in Onchocerciasis Endemic Areas: Systematic Review and Meta-analysis of Population-Based Surveys. PLoS Negl Trop Dis. 2009;3(6):461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colebunders R, Hendy A, Mokili JL, Wamala JF, Kaducu J, Kur L, et al. Nodding syndrome and epilepsy in onchocerciasis endemic regions: Comparing preliminary observations from South Sudan and the Democratic Republic of the Congo with data from Uganda. BMC Res Notes. 2016;9(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaiser C, Pion SDS, Boussinesq M. Case-control studies on the relationship between onchocerciasis and epilepsy: systematic review and meta-analysis. PLoS Negl Trop Dis. 2013;7(3):e2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vinkeles Melchers NVS, Mollenkopf S, Colebunders R, Edlinger M, Coffeng LE, Irani J, et al. Burden of onchocerciasis-associated epilepsy: First estimates and research priorities. Infect Dis Poverty. 2018;7(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Föger K, Gora-Stahlberg G, Sejvar J, Ovuga E, Jilek-Aall L, Schmutzhard E, et al. Nakalanga Syndrome: Clinical Characteristics, Potential Causes, and Its Relationship with Recently Described Nodding Syndrome. PLoS Negl Trop Dis. 2017;11(2):e0005201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stelzle D, Schmidt V, Ngowi BJ, Matuja W, Schmutzhard E, Winkler AS. Lifetime prevalence of epilepsy in urban Tanzania – A door-to-door random cluster survey. eNeurologicalSci. 2021;24:100352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rwiza HT, Kilonzo GP, Haule J, Matuja WBP, Mteza I, Mbena P, et al. Prevalence and Incidence of Epilepsy in Ulanga, a Rural Tanzanian District: A Community-Based Study. Epilepsia. 1992;33(6):1051–6. [DOI] [PubMed] [Google Scholar]
- 12.Greter H, Mmbando B, Makunde W, Mnacho M, Matuja W, Kakorozya A, et al. Evolution of epilepsy prevalence and incidence in a Tanzanian area endemic for onchocerciasis and the potential impact of community-directed treatment with ivermectin : a cross-sectional study and comparison over 28 years. BMJ Open. 2018;8(3):17188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.König R, Nassri A, Meindl M, Matuja W, Kidunda AR, Siegmund V, Bretzel G, Löscher T, Jilek-Aall L, Schmutzhard E, Winkler AS. The role of Onchocerca volvulus in the development of epilepsy in a rural area of Tanzania. Parasitology. 2010;137(10):1559–68. [DOI] [PubMed] [Google Scholar]
- 14.Bhwana D, Mmbando BP, Dekker MC, Mnacho M, Kakorozya A, Matuja W, et al. Clinical presentation of epilepsy in six villages in an onchocerciasis endemic area in Mahenge. Tanzania Epileptic Disord. 2019;21(5):425–35. [DOI] [PubMed] [Google Scholar]
- 15.Mmbando BP, Suykerbuyk P, Mnacho M, Kakorozya A, Matuja W, Hendy A, et al. High prevalence of epilepsy in two rural onchocerciasis endemic villages in the Mahenge area, Tanzania, after 20 years of community-directed treatment with ivermectin. Infect Dis Poverty. 2018;7(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dusabimana A, Nelson J, Fodjo S, Ndahura MM, Mmbando BP, Jada SR, et al. Surveillance for Onchocerciasis-Associated Epilepsy and OV16 IgG4 Testing of Children 6–10 Years Old Should Be Used to Identify Areas Where Onchocerciasis Elimination Programs Need Strengthening. Pathogens. 2022;11(3):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colebunders R, Njamnshi AK, Menon S, Newton CR, Hotterbeekx A, Preux PM, et al. Onchocerca volvulus and epilepsy: A comprehensive review using the Bradford Hill criteria for causation. PLoS Negl Trop Dis. 2021;15(1):e0008965. 10.1371/journal.pntd.0008965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neglected Tropical Diseases Control Programme in Tanzania. The Global Onchocerciasis Network for Elimination Webinar -Tanzania Oncho Elimination Updates. 2022. Accessed 4 Feb 2024.
- 19.Mwaiko GL, Mtoi RS, Mkufya AR. Onchocerciasis prevalence in Tanzania. Cent Afr J Med. 1990;36(4):94–6. [PubMed] [Google Scholar]
- 20.Jilek-Aall L, Jilek W, Miller JR. Clinical and genetic aspects of seizure disorders prevalent in an isolated African population. Epilepsia. 1979;20(6):613–22. [DOI] [PubMed] [Google Scholar]
- 21.Aall-Jilek LM. Epilepsy in the Wapogoro tribe in Tanganyika. Acta Psychiatr Scand. 1965;41(1):57–86. [Google Scholar]
- 22.Adamolekun B, Mielke JK, Ball DE. An evaluation of the impact of health worker and patient education on the care and compliance of patients with epilepsy in Zimbabwe. Epilepsia. 1999;40(4):507. [DOI] [PubMed] [Google Scholar]
- 23.Mugumbate J, Mushonga J. Myths, perceptions, and incorrect knowledge surrounding epilepsy in rural Zimbabwe: A study of the villagers in Buhera District. Epilepsy Behav. 2013;27(1):144–7. [DOI] [PubMed] [Google Scholar]
- 24.Sanya EO, Salami TAT, Goodman OO, Buhari OIN, Araoye MO. Perception and attitude to epilepsy among teachers in primary, secondary and tertiary educational institutions in middle belt Nigeria. Trop Doct. 2005;35(3):153–6. [DOI] [PubMed] [Google Scholar]
- 25.Bain LE, Awah PK, Takougang I, Sigal Y, Ajime TT. Public awareness, knowledge and practice relating to epilepsy amongst adult residents in rural Cameroon - case study of the fundong health district. Pan Afr Med J. 2013;14:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mmbando BP, Bhwana DK, Massawe IS, Magili P, Mahone S, Makunde W, et al. Community knowledge, attitudes, and practices regarding epilepsy in Mahenge, Tanzania: A socio-anthropological study in an onchocerciasis-endemic area with a high prevalence of epilepsy. Epilepsy Behav. 2022;128:108568. [DOI] [PubMed] [Google Scholar]
- 27.Ulanga District Council, Morogoro, TZ. Climate Zone, Monthly Averages, Historical Weather Data. Available from: https://tcktcktck.org/tanzania/morogoro/boma-ya-ulanga. Accessed 5 Feb 2024.
- 28.National Bureau of Statistics. The United Republic of Tanzania 2022 Population and Housing Census distributed by Administrative Areas. Ministry of Finance. 2023. Available at: https://www.nbs.go.tz/statistics/topic/census-2022. Accessed 23 Mar 2024.
- 29.Bhwana D, Amaral LJ, Mhina A, Hayuma PM, Francis F, Siewe Fodjo JN, Mmbando BP, Colebunders R. Impact of a bi-annual community-directed treatment with ivermectin programme on the incidence of epilepsy in an onchocerciasis-endemic area of Mahenge, Tanzania: A population-based prospective study. PLoS Negl Trop Dis. 2023;17(6):e0011178. 10.1371/journal.pntd.0011178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Enderlein, Daniel G, Wayne W. Biostatistics — A Foundations for Analysis in the Health Sciences. Wiley & Sons, New York—Chichester—Brisbane—Toronto—Singapore, 6th ed. 1995, 780 S., ISBN 0–471–58852–0. Biometrical J. 1995;37(6):744–744. [Google Scholar]
- 31.Dent W, Helbok R, Matuja WBP, Scheunemann S, Schmutzhard E. Prevalence of active epilepsy in a rural area in South Tanzania: a door-to-door survey. Epilepsia. 2005;46(12):1963–9. [DOI] [PubMed] [Google Scholar]
- 32.Hunter E, Rogathi J, Chigudu S, Jusabani A, Jackson M, McNally R, et al. Prevalence of active epilepsy in rural Tanzania: A large community-based survey in an adult population. Seizure. 2012;21(9):691–8. [DOI] [PubMed] [Google Scholar]
- 33.Adewumi T, Oladipo E, Adewuya AO. Public perception and attitude towards people living with epilepsy in Nigeria. Epilepsy Behav. 2020;106:107033. [DOI] [PubMed] [Google Scholar]
- 34.Macit C, Clark PM, Taner N, Bingol C, Mercanoglu G, Yuksel G. A survey on awareness, knowledge, and attitudes toward epilepsy in an urban community in Turkey. Niger J Clin Pract. 2018;21(8):979–87. [DOI] [PubMed] [Google Scholar]
- 35.Al-Hayani MM, Kobeisy SA, Allebdi KS, Al Hajari SH, Alluhibi WS, Al-Yahyawi NY, et al. Epilepsy awareness among Rabigh Province residents in Saudi Arabia: A cross-sectional survey study. Neurosciences. 2022;27(4):221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Molla A, Mekuriaw B, Habtamu E, Mareg M. Knowledge and attitude towards epilepsy among rural residents in southern Ethiopia: a cross-sectional study. BMC Public Health. 2021;21(1):420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raimon S, Lakwo TL, Sebit WJ, Siewe Fodjo JN, Alinda P, Carter JY, et al. “Slash and Clear”, a Community-Based Vector Control Method to Reduce Onchocerciasis Transmission by Simulium sirbanum in Maridi, South Sudan: A Prospective Study. Pathog (Basel, Switzerland). 2021;10(10):1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keikelame MJ, Swartz L. ’ A thing full of stories’: Traditional healers’ explanations of epilepsy and perspectives on collaboration with biomedical health care in Cape Town. Transcult Psychiatry. 2015;52(5):659–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaddumukasa M, Nalubwama H, Kaddumukasa MN, Lhatoo S, Sewankambo N, Katabira E, et al. Barriers to epilepsy care in Central Uganda, a qualitative interview and focus group study involving PLWE and their caregivers. BMC Neurol. 2019;19(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dolo H, Mandro M, Wonya’ Rossi D, Ngave F, Fraeyman J, Siewe JN, et al. Community perceptions of epilepsy and its treatment in an onchocerciasis endemic region in Ituri, Democratic Republic of Congo. Infect Dis Poverty. 2018;7(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Colebunders R, Siewe FJN, Hotterbeekx A. Onchocerciasis-Associated Epilepsy, an Additional Reason for Strengthening Onchocerciasis Elimination Programs. Trends Parasitol. 2017;34(3):208–16. [DOI] [PubMed] [Google Scholar]
- 42.Legesse E, Nigussie T, Kebede Y, Aman M, Chaka M, Tilahun D. What is the community’s knowledge and understanding regarding epilepsy? Epilepsy knowledge and its determinants among residents of Debub Bench District, Bench Sheko Zone, Southwest Ethiopia, 2019: a cross-sectional study. BMJ Open. 2022;12(1):e052480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teferi J, Shewangizaw Z. Assessment of knowledge, attitude, and practice related to epilepsy: A community-based study. Neuropsychiatr Dis Treat. 2015;11:1239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Birbeck G, Chomba E, Atadzhanov M, Mbewe E, Haworth A. The social and economic impact of epilepsy in Zambia: a cross-sectional study. Lancet Neurol. 2007;6(1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Quereshi C, Standing HC, Swai A, Hunter E, Walker R, Owens S. Barriers to access to education for young people with epilepsy in Northern Tanzania: A qualitative interview and focus group study involving teachers, parents and young people with epilepsy. Epilepsy Behav. 2017;72:145–9. [DOI] [PubMed] [Google Scholar]
- 46.Magili PF, Kakoko DC, Bhwana D, Akyoo WO, Amaral LJ, Massawe IS, et al. Accessibility to formal education among persons with epilepsy in Mahenge Tanzania. Epilepsy Behav. 2023;148:109445. [DOI] [PubMed] [Google Scholar]
- 47.de Souza EA, Salgado PC. A psychosocial view of anxiety and depression in epilepsy. Epilepsy Behav. 2006;8(1):232–8. [DOI] [PubMed] [Google Scholar]
- 48.de Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav. 2008;12(4):540–6. [DOI] [PubMed] [Google Scholar]
- 49.Asnakew S, Legas G, Belete A, Tadele Admasu F, Demilie K, Alebachew Bayih W, et al. Knowledge and attitude of the community towards epilepsy in Northwest Ethiopia: A huge gap on knowledge and attitude of the community. Epilepsy Behav Rep. 2021;15:100422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaddumukasa M, Kaddumukasa MN, Buwembo W, Munabi IG, Blixen C, Lhatoo S, et al. Epilepsy misconceptions and stigma reduction interventions in sub-Saharan Africa, a systematic review. Epilepsy Behav. 2018;85:21–7. 10.1016/j.yebeh.2018.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shihata SS, Abdullah TS, Alfaidi AM, Alasmari AA, Alfaidi TM, Bifari AE, et al. Knowledge, perception, and attitudes toward epilepsy among medical students at King Abdulaziz University. SAGE Open Med. 2021;9:2050312121991248. 10.1177/2050312121991248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dorji T, Yangchen, Wangmo S, Tenzin K, Jamtsho S, Pema D, et al. Challenges in epilepsy diagnosis and management in a low-resource setting: An experience from Bhutan. Vol. 192, Epilepsy Research. 2023. 10.1016/j.eplepsyres.2023.107126. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The corresponding author will provide the datasets used in/or analysed during the current work upon reasonable request.