Abstract
Background
Exposure to ambient air pollution is a top risk factor contributing to the global burden of disease. Pregnant persons and their developing fetuses are particularly susceptible to adverse health outcomes associated with air pollution exposures. During pregnancy, the thyroid plays a critical role in fetal development, producing thyroid hormones that are associated with brain development. Our objective is to systematically review recent literature that investigates how prenatal exposure to air pollution affects maternal and fetal thyroid function.
Methods
Following the Navigation Guide Framework, we systematically reviewed peer-reviewed journal articles that examined prenatal exposures to air pollution and outcomes related to maternal and fetal thyroid function, evaluated the risk of bias for individual studies, and synthesized the overall quality and strength of the evidence.
Results
We found 19 studies that collected data on pregnancy exposure windows spanning preconception to full term from 1999 to 2020 across nine countries. Exposure to fine particulate matter (PM2.5) was most frequently and significantly positively associated with fetal/neonatal thyroid hormone concentrations, and inversely associated with maternal thyroid hormone concentrations. To a lesser extent, traffic-related air pollutants, such as nitrogen dioxide (NO2) had significant effects on fetal/neonatal thyroid function but no significant effects on maternal thyroid function. However, the body of literature is challenged by risk of bias in exposure assessment methods and in the evaluation of confounding variables, and there is an inconsistency amongst effect estimates. Thus, using the definitions provided by the objective Navigation Guide Framework, we have concluded that there is limited, low quality evidence pertaining to the effects of prenatal air pollution exposure on maternal and fetal thyroid function.
Conclusion
To improve the quality of the body of evidence, future research should seek to enhance exposure assessment methods by integrating personal monitoring and high-quality exposure data (e.g., using spatiotemporally resolved satellite observations and statistical modeling) and outcome assessment methods by measuring a range of thyroid hormones throughout the course of pregnancy.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12940-024-01116-9.
Keywords: Prenatal, Air pollution, Thyroid function, Fetal, Maternal
Introduction
Exposure to ambient air pollution is one of the top risk factors contributing to the global burden of disease and accounts for millions of deaths worldwide each year [1]. Long-term exposure to pollutants, such as particulate matter (PM), nitrogen dioxide (NO2), and ground-level ozone (O3), have an increasing impact on the public health burden associated with chronic disease outcomes, including ischemic heart disease, type 2 diabetes mellitus, chronic obstructive pulmonary disease (COPD), lung cancer, and others. While air pollution affects people of all ages and socioeconomic statuses, some vulnerable groups including pregnant persons, children, older adults, and those with preexisting health conditions experience an elevated risk of exposure to air pollution and thus, shoulder a greater burden of air pollution-related health consequences [2]. With an estimated 213 million pregnancies occurring annually and 99% of the world’s population breathing air that exceeds the World Health Organization’s (WHO) air quality limits [3], continuous exposure to air pollutants poses a serious health risk to pregnant persons and their children [4, 5].
The complex, multifaceted interactions through which air pollution affects human health, influences not only maternal health, but fetal, perinatal, and postnatal health of the parent/child pair. Maternal exposure to air pollution has been associated with complications during pregnancy including gestational hypertension, gestational diabetes mellitus, and preeclampsia [6]. Gestational exposures to air pollution have been linked with adverse birth outcomes such as preterm birth, low birth weight, and stillbirth [7, 8]; and are further connected to neurodevelopmental effects, effects on childhood respiratory function and lung development, and congenital heart defects [9–12]. In recent years, a growing body of literature has examined ways that air pollution affects thyroid function, which plays a critical role in fetal development.
During pregnancy, the thyroid produces a set of hormones that are associated with fetal brain development [13]. The thyroid is responsible for secreting two major hormones: thyroxine (T4) and triiodothyronine (T3), the release of which is controlled by thyroid- stimulating hormone (TSH) [14]. During the first trimester, the fetal thyroid gland is developing, causing the fetus to be dependent upon the maternal transfer of T4 [13, 15]. Fetal T4 production begins at the end of the first trimester and steadily increases until the end of the third trimester, therefore, thyroid hormone-dependent functions are driven by maternal thyroid hormones during the first two trimesters of gestation [13, 16]. Alterations in thyroid function and thyroid hormone ratios in pregnant persons can negatively impact a developing fetus, even contributing to cognitive deficits and reductions in the growth of the child [17, 18]. As such, it is important to consider the impacts of air pollution on thyroid function in both the pregnant person and their offspring, including during gestation and the early postnatal period, to identify underlying mechanisms contributing to endocrine disruption and provide an evidence base for protective guidance.
The mechanisms by which air pollutants disrupt the endocrine system have not been sufficiently characterized [19, 20]. However, environmental pollutants more broadly disrupt thyroid gland function through thyroid hormone synthesis, metabolism, secretion, and action; primarily by reducing circulating thyroid hormone levels or by disrupting hormone action. Furthermore, environmental pollutants affect the pituitary gland, TSH levels, and iodine absorption (important in thyroid hormone biosynthesis), and act as thyroid hormone receptor agonists [21–23]. Aside from fetal developmental defects that can arise from hormone fluctuations during pregnancy, disruptions to thyroid function have implications for thyroid-related autoimmune disorders and the development of conditions such as hyper- or hypothyroidism [24]. Altered thyroid function usually results from genetic predisposition coupled with environmental triggers, namely synthetic chemicals, organic water pollutants, and air pollutants [25, 26].
We conducted a systematic literature review to identify effects of prenatal air pollutants exposure on maternal and fetal thyroid function. Several reviews have investigated the association between air pollution exposure and a range of adverse birth outcomes [7, 9–12, 27]. One review examines air pollution effects on childhood endocrinologic disorders [28], and two examine air pollution effects on thyroid function generally [29, 30]; both of which have broad inclusive criteria for population and thyroid abnormalities yet conduct a very limited assessment of the effects of air pollutants on associated thyroid outcomes. Here, we advance upon these previous reviews by applying the rigorous Navigation Guide Framework [31] and focusing on prenatal exposure, resulting in a narrowed topical focus that includes more articles and a wider range of pollutants and thyroid outcomes.
Key reports that evaluate policy-relevant science to protect public health presently lack epidemiologic literature on prenatal air pollutant exposure and its impacts on maternal and fetal thyroid function. For example, the Environmental Protection Agency’s 2019 Integrated Science Assessment (ISA) for PM [32] mentions the potential impact of PM2.5 on biological pathways for pregnancy and birth outcomes, including effects on fetal thyroid function, in only one sentence citing two studies [33, 34], neither of which considers effects on maternal thyroid function. Results of our review may be useful to characterize important air pollution exposure windows during pregnancy and identify concentration-response relationships between prenatal air pollution exposure and adverse thyroid outcomes.
Methods
We conducted a systematic literature review using steps adapted from the Navigation Guide Framework described by Johnson et al. [31]: (1) specify the study question; (2) select the evidence; and (3) rate the quality and strength of evidence.
Development of study question
The objective of this systematic review is to answer the question: How does prenatal exposure to air pollution affect maternal and fetal thyroid function? A PECO (population, exposure, comparator, outcome) statement was developed containing the following components:
P [population]: pregnant women and fetuses exposed to higher levels of air pollution.
E [exposure]: ambient air pollution.
C [comparator]: pregnant women and fetuses exposed to lower levels of air pollution.
O [outcome]: maternal and fetal thyroid outcomes.
For the purposes of this systematic review, we additionally considered studies that collected outcome assessment measures of neonates when the measurements of thyroid function were recorded shortly after delivery and air pollution exposure was still assigned during the prenatal period; these studies were considered for inclusion as the exposure assessment is focused on the gestational experience and the measurement of thyroid function in the near-immediacy after birth provides some insight into fetal thyroid functioning [35].
Evidence selection
Search terms and methods
We used the following search terms to identify admissible literature: prenatal (OR before birth OR pregnant OR pre-birth OR in utero OR gestational OR trimester) AND air pollution (OR nitrogen oxide OR nitrogen dioxide OR particulate matter OR fine particulate matter OR ozone OR traffic-related) AND thyroid (OR endocrine OR thyroid function OR hypothyroidism OR hyperthyroidism OR congenital hypothyroidism OR thyroxine OR triiodothyronine OR thyroid stimulating hormone OR thyrotropin). We conducted a first search on February 22 and 26, 2022 and an updated search on January 25, 2024 using four databases: PubMed [36], Scopus [37], ProQuest Environmental [38], and Cochrane Reviews [39]. We hand-vetted all reference lists for included studies to incorporate studies that may have been missed in the initial search. Complete lists of search terms and records retrieved for each database during the two search periods are included in Tables S1 and S2.
Study selection
Included papers must have been peer-reviewed, published in English, and published from 2017 to the date the search was carried out to be considered in the final analysis. All search results were exported to Covidence [40]. We first screened titles and abstracts for inclusion criteria, and then reviewed the non-excluded articles in full text. Following full-text review, we excluded studies if they examined animal and not human populations; did not include the outcome, exposure, or population of interest; or did not present novel data. Additionally, we excluded Review, Narrative, or Perspective papers. Two authors (C.O. and E.J.C.) independently screened and reviewed articles for inclusion or exclusion and met to decide on final selection. A third author (S.C.A.) adjudicated if the two authors could not come to a consensus.
When referencing specific results of manuscripts included in this review, we adopt the language used by those manuscripts (e.g., women, females, mothers). In our broader discussions on the implications of such work, we have chosen to use gender-inclusive terms (e.g., pregnant persons, parent, etc.).
Rate the quality and strength of evidence
We evaluated the quality and strength of the evidence by: (1) assessing the “risk of bias” of individual studies, following Johnson et al. [31]; (2) evaluating the quality of evidence across the selected studies; and (3) rating the strength of the evidence across the breadth of studies.
Risk of bias assessment
We used the Risk of Bias instrument described by Johnson et al. [31]. Two authors (C.O. and E.J.C.) independently analyzed the risk of bias for each included study and met to decide on final bias designations. A third author (S.C.A.) adjudicated if the two authors could not come to a consensus. Each risk of bias domain was assigned as “low risk,” “probably low risk,” “probably high risk,” “high risk,” or “unclear risk” (not enough information given to provide a clear designation of risk). We applied a protocol which outlined specific instructions and designations for each bias classification to ensure consistency in interpretation (Table S3).
Quality of evidence
We used three ratings to synthesize the overall quality of evidence: (1) “high;” (2) “moderate;” and (3) “low.” We first assigned an initial “moderate” quality rating to the encompassing body of evidence. We then considered evaluation factors via “downgrades” and “upgrades” (Table S4). Possible ratings ranged from 0 (no change from “moderate” quality); -1 (one-level downgrade); -2 (two-level downgrade); +1 (one-level upgrade); or + 2 (two-level upgrade).
Strength of evidence
We rated the overall strength of the body of evidence based on a combination of four considerations: (1) quality of evidence (described in previous section); (2) direction of the effect estimate; (3) confidence in the effect estimate; and (4) other compelling data attributes that may affect the conclusion. We compared the results of the strength of evidence rating to definitions specified in the Johnson et al. [31] Navigation Guide for “sufficient evidence of toxicity,” “limited evidence of toxicity,” “inadequate evidence of toxicity,” or “evidence of lack of toxicity” (Table S5).
Results
Included studies
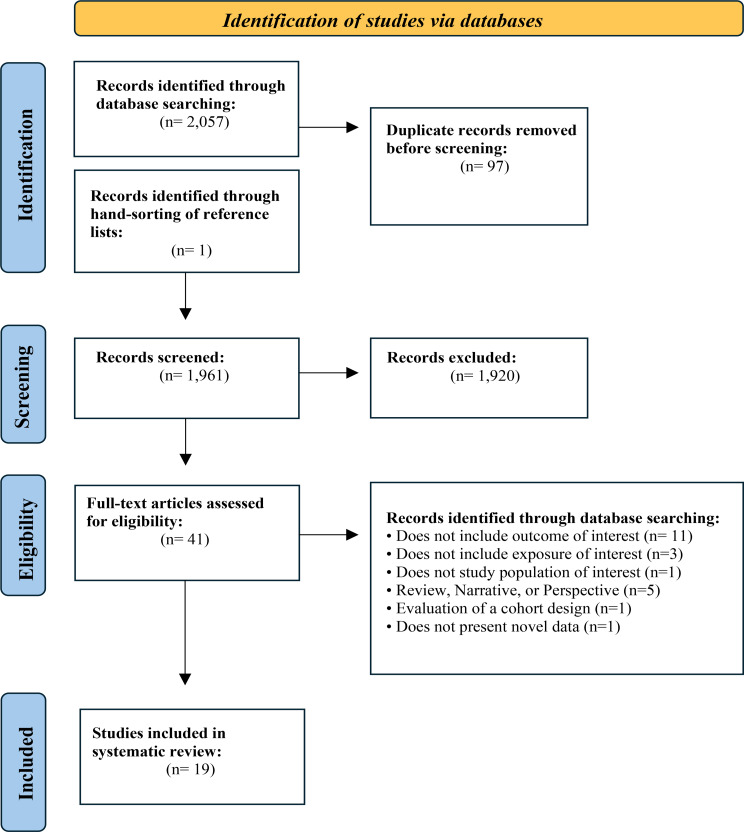
Our search recovered 2,057 unique records, and we added one paper identified through hand-vetting the reference lists of each article (Fig. 1). After removing duplicates, we screened 1,961 papers and assessed 41 full-text articles for eligibility. Of these 41 articles, 22 were excluded for the following reasons: did not include outcome of interest (11 excluded); did not include exposure of interest (3); Review, Narrative, or Perspective article (5); did not examine the study population of interest (1); was an evaluation of a cohort design (1); and did not present novel data (1).
Fig. 1.
PRISMA Diagram of the literature search and screening process
The included studies encompassed nine countries (Belgium, China, France, Greece, Iran, Israel, Netherlands, Spain, United States) and 736,808 individuals, plus two studies that analyzed 367 cities for which a total sample size was not provided (Table 1). The studies ranged in air pollutants measured (e.g., PM2.5, NOx, bound metals, etc.) and thyroid outcomes measured (e.g., fluctuations in hormones [TSH, T3, T4], congenital hypothyroidism, hypothyroxinemia). Data collection ranged from 1999 to 2020, and exposure windows ranged from preconception to full pregnancy term.
Table 1.
Descriptive information for all 19 included studies
| Study | Study design | Location | Sample size | Air pollutants measured | Study duration | Thyroid outcome measured | Exposure window |
|---|---|---|---|---|---|---|---|
| Chamot et al. [41] | Regional Registry Analysis | Picardy Region, France | 6,249 | PM2.5, PM10 | 2021 | TSH (neonatal) | Third trimester |
| Ghassabian et al. [42] | Multi-Cohort Analysis | Amsterdam, Netherlands (ABCD) | 9,931 total | PM2.5, PM10, NO2, NOx, PM2.5−10, PM2.5absorbance | 2003–2004 | TSH, hypothyroxinemia (maternal) | First trimester |
| Rotterdam, Netherlands (Generation R) | PM2.5, PM10, NO2, NOx, PM2.5−10, PM2.5absorbance | 2002–2006 | |||||
| Spain (INMA) | PM2.5, PM10, NO2, NOx, PM2.5−10, PM2.5absorbance | 2003–2008 | |||||
| Crete, Greece (Rhea) | PM2.5, PM10, PM2.5−10, PM2.5absorbance | 2007–2008 | |||||
| Massachusetts, United States (Project Viva) | PM2.5, NO2 | 1999–2002 | |||||
| Gong et al. [43] | Prospective Cohort | Henan Province, China | 1,049 | PM2.5, PM10 | 2017–2019 | FT4, TSH (maternal) | First trimester |
| Harari-Kremer et al. [44] | Historical Cohort Study | Israel | 696, 461 |
PM2.5, PM10 − 2.5, NO2, NOx |
2009–2015 | CHT (neonatal) | Full pregnancy |
| Howe et al. [45] | Retrospective Cohort | California, United States | 2,050 | PM2.5, PM10, NO2, O3, NOx | 1994–1997 | TT4 (neonatal) | Full pregnancy |
| Ilias et al. [46] | Retrospective Cohort | Athens, Greece | 293 | PM2.5, PM10, NO2 | 2012–2018 | TSH (maternal) | Nine months preceding second and third trimesters |
| Irizar et al. [47] | Prospective Cohort | Gipuzkoa, Spain | 463 pairs | PM2.5, NO2 | 2006–2008 | TT4 (neonatal) | Full pregnancy |
| Janssen et al. [33] | Birth Cohort | Limburg, Belgium | 499 pairs | PM2.5 | 2010–2014 | FT3, FT4, FT4/FT3 ratio, TSH (maternal and fetal) | Third trimester |
| Li et al. [48] | Birth Cohort | Wuhan, China | 551 | PM2.5 | 2013–2015 | FT3, FT4, FT4/FT3 ratio, TSH (maternal) | Preconception; First Trimester |
| Nourouzi & Chamani [49] | Birth Cohort | Isfahan City, Iran | 200 | PM2.5, CO | 2019–2020 | TSH (fetal) | Full pregnancy |
| Qi et al. [50] | National Database Analysis | China | 367 cities (30 provinces) | SO2, CO, NO2, O3 | 2014–2015 | CHT (neonatal) | Full pregnancy |
| Qiu et al. [51] | Retrospective Cohort | Jinhua, China | 2,528 | PM2.5, PM10, SO2, CO, NO2, PM2.5-bound metals [Al, As, Be, Cr, Pb, Mn, Ni, Se, Tl, Ba] | 2018 | FT3, FT4, FT4/FT3 ratio, TSH (maternal) | First trimester |
| Shang et al. [52] | National Database Analysis | China | 30 provinces | PM2.5, PM10 | 2014–2015 | CHT (neonatal) | Full pregnancy |
| Sun et al. [53] | Retrospective Case-Control | Beijing, China | 3,180 (795 cases, 2,385 controls) | PM2.5, PM10 | 2012–2020 | Hypothyroidism (maternal) | Preconception and early pregnancy |
| Wang et al. [54] | Prospective Birth Cohort | Nanjing, China | 433 pairs | PM2.5, OM, BC, SO42−, NO3−, NH4+, soil dust | 2014–2015 | FT4 (maternal), TSH (maternal and neonatal) | First trimester |
| Zeng et al. [55] | Birth Cohort | Guiyu and Haojiang, China | 204 pairs | PM2.5 | 2011–2012 | FT4, FT3, TSH (fetal) | Full pregnancy |
| Zhang et al. [56] | Prospective Birth Cohort | Wuhan, China | 921 | PM2.5, PM10 | 2013–2014 | FT4, FT3, FT4/FT3 ratio, TSH (maternal) | First trimester |
| Zhao et al. [57] | Cohort Study | Shanghai, China | 8,077 | PM2.5, NO2 | 2014–2015 | FT4, TSH, hypothyroxinemia (maternal) | First and second trimester |
| Zhou et al. [58] | Prospective Birth Cohort | Shanghai, China | 1,060 pairs | PM2.5, 17 inorganic constituents above 50% detection rate (Na, Al, Si, P, S, Cl, K, Ca, Ti, V, Cr, Mn, Fe, Ni, Cu, Zn, Pb) | 2016–2018 | FT4, FT3, FT4/FT3 ratio, TSH (maternal) | Early pregnancy |
Abbreviations: TSH, thyroid stimulating hormone; FT3, triiodothyronine; FT4, thyroxine; CHT, congenital hypothyroidism; TT4, total thyroxine; PM2.5, particulate matter of 2.5 microns; PM10, particulate matter of 10 microns; PM2.5−10, particulate matter of 2.5–10 microns; NO2, nitrogen dioxide; O3, ozone; NOx, nitrogen oxides; CO, carbon monoxide; SO2, sulfur dioxide; As, arsenic; Be, beryllium; Cr, chromium; Mn, manganese; Se, selenium; Tl, thallium; Ba, barium; Na, sodium; Al, aluminum; Si, silicon; P, phosphorous; S, sulfur; Cl, chlorine; K, potassium; Ca, calcium; Ti, titanium; V, vanadium; Fe, iron; Ni, nickel; Cu, copper; Zn, zinc; Pb, lead; OM, organic matter; BC, black carbon; SO42−, sulfate; NO3−, nitrate; NH4+, ammonium
Measuring exposure
The studies used a diverse range of methods to measure exposure (Table S6). Of the 19 studies, 12 used residential geocoding to improve spatial accuracy of exposure estimates (all except 37–43). Four studies utilized fixed-monitoring networks within their locality [46, 50–52], 12 studies used modeling (e.g., land-use regression, dispersion) or machine learning methods [33, 41, 43, 44, 44, 48, 49, 53–58], and three studies used a combination of fixed-monitoring network data and pollutant modeling [42, 45, 47]. Two studies used particle sampling, including high volume aerosol and radial passive sampling [47] and filter capture of particulates [51]; and one study conducted personal monitoring on a sub cohort group of their study population [58].
PM2.5 was the pollutant measured most frequently, incorporated in 18 of the 19 included studies (all except 40). Nine studies incorporated exposure estimates for PM10 [41–43, 45, 46, 51–53, 56] and eight studies used exposure estimates for NO2 [42, 44–47, 50, 51, 57]. Additionally, two studies included measurements of PM2.5- bound metals and inorganic constituents [51, 58] and one study assessed six constituents of PM2.5 (i.e., OM, BC, SO42−, NO3−, NH4+, soil dust) [54]. Other pollutants measured in the studies included coarse particulate matter (PM2.5−10), ozone (O3), nitrogen oxides (NOx), sulfur dioxide (SO2), and carbon monoxide (CO).
Exposure windows
Studies varied with respect to exposure windows. Five studies assessed exposure during the first trimester only [42, 43, 51, 54, 56], no studies assessed exposure during second trimester only, two studies assessed exposure during third trimester only [33, 41], and seven studies assessed exposure during the full gestation period [44, 45, 47, 49, 50, 52, 55]. Three studies looked at exposure during the period prior to gestation, known as preconception [46, 48, 53].
Measuring outcome
Included studies measured TSH, FT4, FT3, FT4/FT3 ratio, TT4, hypothyroxinemia, hypothyroidism, and congenital hypothyroidism (CHT) in either pregnant women [42, 43, 46, 48, 51, 53, 56–58], their fetuses [49, 55], their neonates [41, 44, 45, 47, 50, 52], or as a paired analysis of both maternal and fetal/neonatal outcomes [33, 54]. Studies defined hypothyroxinemia as FT4 concentrations in the lower 2.5th to 5th percentile (or < 12.25 pg/L) of the population despite a normal TSH level [42, 57], hypothyroidism as TSH concentrations > 4 mU/L and FT4 concentrations below the lower limit of the reference range (0.93–1.70 ng/dL) [53], and congenital hypothyroidism as a concentration of TSH higher than 10–20 µIU/ml in double testing and confirmed diagnosis by a pediatric endocrinologist based on serum thyroid function tests [44, 50, 52].
For studies solely measuring thyroid outcomes in fetal/neonatal populations (Table S6), newborn heel-prick was the method used most frequently, employed in four studies [41, 44, 45, 47], followed by cord blood collection in two studies [49, 55], and whole-blood collection in two studies [50, 52]. Sample collection time frames ranged from immediately after delivery [49] to within seven days after birth [50, 52]. Most studies collected samples within 72 h after birth [41, 44, 45, 47].
For studies solely measuring thyroid outcomes in maternal populations (Table S6), blood samples were collected in six of the studies [43, 48, 51, 56–58] and maternal serum was sampled in one study [42]. Ilias et al. [46] identified women who were diagnosed with hypothyroidism during pregnancy and retrospectively analyzed air quality data during their gestation period. Sample collection time frames ranged from within the first 14 weeks of pregnancy [42, 51, 53, 58] to second trimester [43, 46, 57].
Janssen et al. [33] and Wang et al. [54] assessed outcomes in mother-child pairs (Table S6). Janssen et al. [33] used umbilical cord blood samples for the fetal population, collected immediately after delivery, and blood samples for the maternal population, collected one day after delivery. Wang et al. [54] utilized newborn heel-prick samples to assess neonatal thyroid function, collected within 72 h after birth, and maternal serum samples collected during the second trimester.
Maternal and fetal/neonatal thyroid function
TSH
Main study findings for each study including whether there was evidence of altered maternal or fetal/neonatal thyroid function, the outcome assessed, and the directionality of the association can be found in Table 2. Of the outcomes examined, TSH levels were evaluated most frequently, in 13 of the 19 studies (all except 39,40,42,45,48,54). Of the studies that assessed prenatal air pollution exposure and maternal TSH levels, two studies found a positive association with PM2.5 [46, 58] and seven studies found no association with PM2.5 [33, 42, 43, 48, 51, 56, 57]. Five studies found no association with PM10 [42, 43, 46, 51, 56] and four studies found no statistically significant association with NO2 exposure [42, 46, 51, 57]. Of the studies that assessed prenatal air pollution exposure to PM2.5 and fetal/neonatal TSH levels, results were mixed: three studies found a positive association [41, 49, 55], one study found an inverse association [33], and one study found no association [54].
Table 2.
Main findings for each study including whether there was evidence of altered maternal or fetal/neonatal thyroid function, the outcome assessed, and the directionality of associations with air pollution exposure
| Study | Evidence of altered maternal thyroid function | Evidence of altered fetal/neonatal thyroid function | Outcome assessed/directionality of association |
|---|---|---|---|
| Chamot et al. [41] | -- | Yes | ↑ Increased exposure to PM2.5 and PM10 was associated with an increase in TSH concentration |
| Ghassabian et al. [42] | Yes | -- |
↑ Increased exposure to PM2.5 was associated with increased odds of hypothyroxinemia ⦸ No statistically significant association between exposure to PM10, PM2.5-10, PM2.5absorbance, NO2, and NOx and odds of hypothyroxinemia or high TSH concentration. No statistically significant association between exposure to PM2.5 and odds of high TSH concentration |
| Gong et al. [43] | Yes | -- |
↑ Increased exposure to PM2.5 and PM10 was associated with an increase in FT4 concentration ⦸ No statistically significant association between exposure to PM2.5 and PM10 and TSH concentration |
| Harari-Kremer et al. [44] | -- | Yes |
↑ Increased exposure to NO2 and NOx was associated with increased odds of developing CHT ⦸ No statistically significant association between exposure to PM2.5 and PM10-2.5 and odds of developing CHT |
| Howe et al. [45] | -- | Yes |
↑ Increased exposure to PM2.5 and PM10 was associated with increased TT4 concentration ⦸ No statistically significant association between NO2, O3, or NOx and TT4 concentration |
| Ilias et al. [46] | Yes | -- |
↑ Increased exposure to PM2.5 was associated with increased logTSH concentration ⦸ No statistically significant association between exposure to PM10 and NO2 and TSH concentration |
| Irizar et al. [47] | -- | Yes |
↑ Increased exposure to PM2.5 was associated with increased TT4 concentration ⦸ No statistically significant association between exposure to NO2 and TT4 concentration |
| Janssen et al. [33] | No | Yes |
↓ Increased exposure to PM2.5 was associated with decreased fetal TSH, FT4, and FT4/FT3 ratio concentrations ↑ Increased exposure to PM2.5 was associated with increased fetal FT3 concentration ⦸ No statistically significant associations between exposure to PM2.5 and maternal FT4, FT3, FT4/FT3 ratio, or TSH concentrations |
| Li et al. [48] | Yes | -- |
↑ Increased exposure to PM2.5 was associated with increased FT3 concentration ↓ Increased exposure to PM2.5 was associated with decreased FT4 and FT4/FT3 ratio concentration ⦸ No statistically significant associations between exposure to PM2.5 and TSH concentration |
| Nourouzi & Chamani [49] | -- | Yes | ↑ Increased exposure to PM2.5 and CO was associated with increased TSH concentration |
| Qi et al. [50] | -- | Yes |
↑ Increased exposure to O3 and NO2 was associated with an increased risk of CHT ⦸ No statistically significant association between exposure to SO2 and CO and risk of CHT |
| Qiu et al. [51] | Yes | -- |
↑ Increased exposure to PM2.5-bound Ba was associated with increased FT4 concentration. Increased exposure to PM2.5-bound Be and Mn were associated with increased FT3 concentration. Increased exposure to PM2.5-bound As, Cr, Se, Tl, and Ba were associated with increased FT4/FT3 ratio concentration ↓ Increased exposure to CO, NO2, and PM2.5-bound Be, Pb, Mn, and Ni were associated with decreased FT4 concentration. Increased exposure to PM2.5, PM10, CO, SO2, and PM2.5-bound As, Cr, Se, and Tl were associated with decreased FT3 concentration. Increased exposure to PM2.5-bound Al, Be, Pb, Mn, and Ni were associated with decreased FT4/FT3 ratio concentration ⦸ No statistically significant associations were observed between exposure to any of the pollutants and TSH concentration |
| Shang et al. [52] | -- | Yes |
↑ Increased exposure to PM2.5 was associated with an increased risk of CHT ⦸ No statistically significant association between exposure to PM10 and risk of CHT |
| Sun et al. [53] | Yes | -- | ↑ Increased exposure to PM2.5 and PM10 (particularly 60 days preconception – month of conception) was associated with increased risk of hypothyroidism |
| Wang et al. [54] | Yes | No |
↓ Increased exposure to PM2.5 was associated with decreased maternal FT4 concentration. Increased exposure to PM2.5 components (BC and NH4+) was associated with decreased maternal FT4 concentration ⦸ No statistically significant association between exposure to PM2.5 and its components and neonatal TSH concentration |
| Zeng et al. [55] | -- | Yes |
↑ Increased exposure to PM2.5 was associated with higher odds of abnormal fetal TSH concentration ⦸ No statistically significant association between exposure to PM2.5 and odds of abnormal fetal FT3 or FT4 concentration |
| Zhang et al. [56] | Yes | -- |
↓ Increased exposure to PM2.5 was associated with decreased FT4 and FT4/FT3 ratio concentration ⦸ No statistically significant association was found between exposure to PM2.5 and FT3 and TSH concentration. No statistically significant association was found between PM10 and any of the thyroid hormones measured |
| Zhao et al. [57] | Yes | -- |
↑ Increased exposure to PM2.5 was associated with an increased risk in hypothyroxinemia ↓ Increased exposure to PM2.5 (particularly in the second trimester) and NO2 (particularly in the first trimester) was associated with decreased FT4 concentration ⦸ No statistically significant association was found between PM2.5 and NO2 and TSH concentration. There was no statistically significant association found between NO2 and risk of hypothyroxinemia |
| Zhou et al. [58] | Yes | -- |
↑ Increased exposure to PM2.5 was associated with increased TSH concentration. Increased exposure to constituent Al and Si was associated with increased FT4 concentration ↓ Increased exposure to PM2.5 was associated with decreased FT4 and FT4/FT3 ratio concentration. Increased exposure to Zn was associated with decreased FT4 concentration. Increased exposure to K, Mn, and Zn weas associated with decreased FT4/FT3 ratio concentration ⦸ No statistically significant association was found between PM2.5 and inorganic constituents and FT3 concentration |
Symbols: –, not evaluated; ↑, positive association; ↓, inverse association; ⦸, no statistically significant association
TT4
Two studies evaluated prenatal exposure to air pollution and neonatal total thyroxine (TT4) measure, and both observed a positive association between increases in PM2.5 exposure and higher TT4 levels [45, 47]. The same studies also observed no significant association with NO2.
FT3
Results were not congruent amongst studies that assessed PM2.5 exposure and maternal FT3 levels. Three studies found no association [33, 56, 58], one study found a positive association [48], and one study found an inverse association [50]. Results were similarly inconsistent amongst studies that assessed PM2.5 and fetal FT3 concentrations: one study found positive association [33], and one study found no association [55].
FT4
Free thyroxine (FT4) levels were examined in nine studies [33, 43, 48, 51, 54–58]. Similar to the results of FT3, there was inconsistency amongst findings. In studies that evaluated PM2.5 exposure and changes to maternal FT4 concentrations, one study found a positive association [43], five studies found an inverse association [48, 54, 56–58], and one study found no association [33]. In studies that evaluated PM2.5 exposure and changes to fetal FT4 concentrations, one study found an inverse association [33], and one study found no association [55].
CHT and hypothyroxinemia
Additionally, CHT was investigated in three studies [44, 50, 52] and maternal hypothyroxinemia was evaluated in two studies [42, 57]. For studies that evaluated CHT: two studies found a positive association between NO2 exposure and odds of developing CHT [44, 50], one study observed a positive association between PM2.5 exposure and risk of CHT, as well as no statistically significant association between PM10 and CHT [52], and one study found no association between PM2.5−10 exposure and odds of developing CHT [44]. For studies that evaluated maternal hypothyroxinemia: both found a positive association between increased exposure to PM2.5 and increased odds of hypothyroxinemia as well as no association between exposure to NO2 and odds of hypothyroxinemia [42, 57].
FT4/FT3 ratio
Air pollution exposure and its effect on the FT4/FT3 ratio was explored in five studies [33, 48, 51, 56, 58]. Of the studies that looked at the association between PM2.5 exposure and the FT4/FT3 ratio concentrations in maternal samples, results differed. Two studies found no association [33, 51], and three studies found an inverse association [48, 56, 58]. Only one study assessed the FT4/FT3 ratio in fetal samples [33]; authors found a significant inverse association between increased PM2.5 exposure and decreased FT4/FT3 ratio concentration in cord blood.
Critical windows of exposure
Of the seven studies that assessed exposure during the full gestation period, three identified critical windows of exposure based on evidence of a significant association [44, 45, 47]. Harari-Kremer et al. [44] identified the third trimester as a sensitive window for exposure to NO2 and NOx and associated odds of CHT. Howe et al. [45] identified gestation months 3–7 (strongest association observed at month five) as critical for exposure to PM2.5 and effects on TT4 concentration, and gestation months 1–8 (strongest effect observed at month one) as critical for exposure to PM10 and effects on TT4 concentration. Irizar et al. [47] identified three windows of sensitivity for PM2.5 exposure and effects on TT4 concentration: the preconception period, gestation weeks 12–17, and gestation weeks 31–37. The remaining four studies that assessed the full gestation period focused their analysis on the spatial aspects of exposure [49] or on the level of exposure [50, 52, 55], and therefore did not assess critical windows of exposure.
Risk of bias assessment
The included studies had a moderate risk of bias. All studies were rated as ‘low risk’ or ‘probably low risk’ for selective outcome reporting, conflict of interest, recruitment strategy, and other biases (Fig. 2). Almost all of the studies were determined to have an ‘unclear’ level of risk for blinding due to the insufficiency of evidence provided to make a clear designation of risk. Risk of bias for exposure assessment was determined as ‘high risk’ for almost all studies (63%), as the methods were deemed not robust (e.g., did not geocode to participant residence, did not address participant mobility, or only used fixed-site monitoring). All studies were rated as ‘probably high risk’ of bias for exposure assessment at the start due to the inability of studies to account for the full exposure profile, including exposures at work, during travel, etc. All studies were rated as ‘high risk’ or ‘probably high risk’ for confounding as it is anticipated that the lack of accounting for important potential confounders is expected to introduce some bias. All studies were rated ‘probably high risk’ of bias for confounding at the start due to the inability to adjust for pollutants not included in the studies’ analysis, including PM2.5-bound endocrine disruptors, polychlorinated biphenyls, heavy metals, and others, that could be associated with air pollution and thyroid function. Additionally, if a study did not account for two or more of the important potential confounders listed in Table S3, a ‘high risk’ designation was assigned.
Fig. 2.
Risk of bias designations for each included study. Table S7 includes the rationale for the designations for each study
Quality of the body of evidence
We assessed the quality of the body of evidence using the upgrading and downgrading factors described in Table S4. This approach was only applied to studies that evaluated exposure to PM2.5 because this was the pollutant addressed in nearly all studies (95%). Other pollutants were not included as evaluative factors in enough studies to be able to assess the quality of evidence across the body of literature. Generally, the studies were individually assigned a moderate risk of bias, as ‘low risk’ or ‘probably low risk’ was assigned for most bias categories, and ‘high risk’ or ‘probably high risk’ was similarly assigned for exposure assessment and confounding biases.
The findings across studies were inconsistent, resulting in a -2 downgrading of the evidence. For example, there were incongruent relationships in three or more pollutant and outcome pairs in similar populations (e.g., three studies found no association between PM2.5 exposure and FT3 concentration, one study found a positive association between increased PM2.5 exposure and increased FT3 concentration, and one study found an inverse association between increased PM2.5 exposure and decreased FT3 concentration). There was a consistent positive concentration-response in ten or more of the studies which resulted in a + 2 upgrading of the quality of evidence. Notably, Howe et al. [45] and Irizar et al. 47] identified a positive association between increases in exposure to PM2.5 and increases in neonatal TT4 levels, and Ghassabian et al. [42] and Zhao et al. [57] observed a positive relationship between increased exposure to PM2.5 and odds of developing hypothyroxinemia. Because we upgraded the body of literature based on concentration-response relationships and downgraded based on inconsistency of the data across studies and risk of bias, we deemed the overall quality of evidence to be “Low” (Table 3).
Table 3.
Ratings and rationale for downgrading and upgrading factors applied to studies that evaluated PM2.5, and overall quality of the body of evidence. Table S8 presents effect estimates and confidence intervals for the group of studies that evaluated PM2.5
| Factor | Rating | Rationale |
|---|---|---|
| Downgrading factors | ||
| Risk of bias | -1 | The reviewers conclude that there is a moderate, but not substantial, risk of bias across the included studies |
| Indirectness | 0 | The included studies directly assessed the population, exposure, and outcome of interest |
| Inconsistency | -2 | There was inconsistency in results within similar populations in more than three pollutant/outcome pairs |
| Imprecision | 0 | Included studies had adequate sample sizes and confidence intervals were not considered wide (all reported 95% confidence intervals) |
| Publication bias | 0 | The reviewers found no indication of publication bias. The search was extensive and comprehensive and there is no reason to believe that studies were missing from the body of evidence |
| Upgrading factors | ||
| Large magnitude of effect | 0 | The estimated effects across studies were not considered to be large |
| Concentration-response | +2 | Relationships between concentration and response were identified in ten or more studies |
| Confounding minimizes effect | 0 | The reviewers did not find evidence to suggest that residual confounding or additional biases would reduce effect estimates |
| Overall rating of quality of evidence: | Low Quality Evidence | Low = -1: -1 downgrade for risk of bias; -2 downgrade for inconsistency amongst pollutant effects on thyroid outcomes; and + 2 upgrade for concentration-response relationship. |
Strength of the body of evidence
Our strength of the body of evidence considerations included the quality of the body of evidence, direction of the effect estimate, confidence in the effect estimate, and other compelling attributes of the data. The overall quality of the body of evidence was rated as low based on the upgrading factor of concentration-response relationships and the downgrading factors of inconsistency in results and risk of bias. Based on our analysis and interpretation of the evidence, we conclude that there is limited evidence of an association between prenatal air pollution exposure and maternal and fetal thyroid function. Chance, bias, and confounding cannot be ruled out with reasonable confidence as the relationship is constrained by inconsistency of findings across individual studies. As more research is made available, it is possible that the observed effect could change.
Discussion
We conducted a systematic review of human population health studies to examine evidence for associations between prenatal air pollution exposure and maternal and fetal thyroid outcomes. We found limited evidence for associations based on 19 studies examining a range of air pollutants (PM2.5, PM10, PM2.5−10, NO2, O3, NOx, CO, SO2, PM2.5-bound metals and inorganic constituents, OM, BC, SO42−, NO3−, NH4+, soil dust) and maternal and fetal/neonatal thyroid outcomes (congenital hypothyroidism, hypothyroxinemia, hypothyroidism, FT3, FT4, TT4, TSH, and FT4/FT3 ratios). The overall risk of bias across the studies was rated as moderate and the quality of the body of evidence was rated as low.
Among the pollutants, PM2.5 was most consistently and significantly associated with differences in fetal/neonatal and maternal thyroid hormone concentrations, with 17 (89%) of the included studies finding an association. To a lesser extent, traffic-related air pollutants, such as NO2 had significant effects on thyroid outcomes. There was less evidence to support that exposure to other air pollutants, such as PM10, NOx, CO, SO2, O3, and others, contributed to alterations in thyroid hormone levels in both pregnant persons and their children. In terms of health outcomes, we found positive associations between increased exposure to PM2.5 and higher odds of hypothyroxinemia and increased neonatal TT4 concentration [42, 45, 47, 57]. Additional studies found a positive association between increased exposure to NO2 and odds of congenital hypothyroidism [44, 50]. Associations between air pollution and TSH, FT4, FT3, and the FT3/FT4 ratio levels were inconsistent.
Directional effect differences associated with PM2.5-bound metals may be in part due to the underlying biological mechanisms in exposure-response pathways [59–61]. Prior research has shown that exposure to air pollution contributes to alterations in maternal thyroid function through mechanisms such as hormone synthesis, transport, metabolism, and gene regulation [62]. And, some research, including from some studies incorporated in this review, has suggested that air pollutants disrupt fetal or neonatal hormone concentrations through changes in enzymes associated with hormone synthesis, the obstruction of hormone metabolism, or by impeding the placental transfer of thyroid hormones from mother to fetus [33, 44, 45]. Aside from the effect that different pollutants and pollutant-bound metals may have on hormones, differences in the directional associations of thyroid hormone concentrations may at least be in part explained by the point of gestation at which the serum or blood sample was taken. For example, the FT4/FT3 ratio is a metabolic indicator of how well the body is able to convert the T4 hormone to the T3 hormone [63]. As mentioned previously, depending on the gestational time frame, the fetus is either more or less dependent on the maternal production of T4 [13, 15, 16]. Thus, differences in gestational sampling windows across the studies, coupled with biological process differences in exposure-response pathways, may explain some of the variation in thyroid hormone concentration findings.
At the time of this review, a critical window of exposure for air pollution and effects on maternal and fetal thyroid function has not been established. Critical windows, also referred to as sensitive periods, are representative of developmental periods when an organism is susceptible to changes in response to environmental stimuli, and thus are important to characterize to better understand the underlying biological mechanisms that contribute to adverse outcomes [64]. Results from this review support the need for further research that aims to identify critical windows of exposure to better understand how air pollution affects the biological processes that contribute to altered thyroid functioning.
The findings of this review support findings from other reviews not included in this analysis, suggesting that prenatal exposure to air pollution may be associated with altered thyroid functioning in pregnant persons and their fetuses/neonates. Liu et al. [29] conducted a pooled analysis of a subgroup of included studies that assessed pregnancy exposure windows (primarily in the first trimester), finding that PM2.5 was associated with an inverse relationship with FT4 concentration; in our review, one study found a positive association, six studies found an inverse association, and two studies found no statistically significant association. Rohani et al. [30], a preprint, non-peer reviewed article, conducted a pooled assessment for maternal hypothyroxinemia and found that exposure to PM2.5 was associated with increased odds of maternal hypothyroxinemia but exposure to NO2 was not; this is consistent with findings of our review.
Location was the primary driver of exposure and was indicative of types of pollutants analyzed (PM10, PM2.5, NO2, NOx, O3, and others), exposure assessment methods used, and level of exposure. For example, Harari-Kremer et al. [44] was only able to capture NO2 and NOx exposure data for a subset of 54% of their study population due to data availability. Spatial variability in level of exposure may be attributed to residential proximity to high emitting sources of air pollutants, such as highways. While exposure profiles were characterized by geocoding to residential address in twelve (63%) studies, geocoding to residential zip code in one study, and assigned based on proximity to fixed-site monitoring data in the remaining six studies, this does not capture the full exposure profile and does not characterize internal dose. The large portion of included studies that were conducted in China (11 of 19; or 58%), where pollutant concentrations were higher than in studies conducted in other parts of the world, could have affected study results (e.g. if the exposure-response relationship is non-linear).
The outcomes related to thyroid function evaluated in these studies are known to be multifactorial and complex. Alterations to maternal thyroid function can be associated with factors such as autoimmunity, iodine deficiency, and physical characteristics such as high body mass index (BMI) [65]. Assessing thyroid hormone function during pregnancy can be further complicated due to the natural hormonal and physiological changes that pregnant persons undergo, as well as stress put on the maternal thyroid during this time [66]. The compilation of the results from studies included in this review present some evidence that in addition to the aforementioned associations, prenatal exposures to air pollution may contribute to adverse outcomes related to maternal and fetal thyroid function. Though there was heterogeneity in findings amongst several pollutant and outcome pairs in similar populations, we consider any alterations in thyroid hormone levels (both increases and decreases) as adversely impactful due to established implications such as fetal neurodevelopmental defects, and the development of thyroid-related autoimmune disorders and conditions (e.g., hyperthyroidism).
This review had several strengths. Including studies from multiple countries, some of which have very large sample sizes (e.g., hundreds of thousands of people) provides a global perspective to both exposure and outcome; establishing that adverse maternal and fetal/neonatal thyroid outcomes are not isolated to air pollution exposures in a particular region but occur globally. Furthermore, studies included in this analysis measured health outcomes objectively (either pulled from medical records or registries, or collected and analyzed during the study period), which limited outcome related self-report bias in the analyses. However, there are several important limitations of this review. Including articles only written in English may have omitted important results from additional studies, though multiple studies from non-English speaking countries were included. The primary limitation of this review stems from the breadth of pollutants, outcomes, and populations in included studies, which prohibited us from being able to draw comparative conclusions across the body of literature. For example, we were only able to consider upgrading and downgrading factors for PM2.5 due to the limited number of studies that addressed other pollutants, and were unable to look at the quality of evidence for fetal, neonatal, and maternal thyroid function separately; it would be reasonable expect that additional literature could increase comparability and elucidate differences in direction and magnitude of effect estimates for individual air pollutant and thyroid outcome combinations in distinct populations. Additionally, a limiting factor in the body of literature is that few studies address important confounding factors that are associated with air pollution and/or thyroid hormone outcomes; some studies collected covariate information through self-reported questionnaires, which could introduce bias.
Because there is some possibility that differences in study outcomes are driven by the diverse approaches used to measure exposures and outcomes across the body of literature, future research should seek to enhance both exposure and outcome assessment to reduce potential sources of study heterogeneity and obtain more robust conclusions. Exposure assessment methods could be improved by conducting personal monitoring, which is considered the gold standard of exposure assessment, though this could pose cost and logistical constraints that lead to reduced sample size or study periods. While ground monitoring stations offer an accurate picture of exposure at the earth’s surface, they only do so for the area in the immediate vicinity. Because these stations are oftentimes spatially distant, and in some regions of the world nonexistent, satellite remote sensing data and modeling tools offer an opportunity to fill in gaps in exposure estimates. Therefore, we strongly recommend that future work integrate satellite, model, and monitor pollutant datasets to establish exposure profiles. Outcome assessment methods can be improved by measuring multiple thyroid hormones (TT4, FT4, FT3, TSH) and measuring outcomes in both the pregnant person and their offspring. The thyroid system is extremely complex, and even more challenging to study during pregnancy due to the changes that it undergoes during this time, therefore, the thorough collection of measurements would be helpful to understand the intricacies of exposure and outcome during this critical period. Additionally, this research could be enhanced by evaluating both exposure and outcome throughout term pregnancy, as opposed to only evaluating at points in time or during specific trimesters to provide a more complete picture of how the thyroid is affected during gestation and explore whether critical exposure windows exist for exposure to air pollution and altered thyroid function. Thus, we recommend future studies leverage longitudinal designs as opposed to cross-sectional evaluations; thyroid disorders tend to develop over longer periods of prolonged stress and therefore a cross-sectional approach may miss the full spectrum of, and the individual variability of, air pollution exposures and associated thyroid outcomes.
Conclusion
While a significant portion of included studies in this review present findings that suggest prenatal exposure to air pollutants may affect maternal and fetal/neonatal thyroid function, using the objective framework of the Navigation Guide we found the body of evidence to be both limited and low quality. The findings from this review, specifically prenatal exposure to PM2.5 and its association with altered maternal and fetal/neonatal thyroid function, add to the growing body of literature on how air pollution affects pregnant persons and their developing fetuses. Future research should seek to enhance exposure and outcome assessment methods to reduce study heterogeneity and gain a better understanding of the nuanced complexities between prenatal exposure to air pollution and thyroid function. Furthermore, future research should focus on establishing critical windows of exposure to air pollution and associated impacts on thyroid function.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Dr. Lance Price, Mr. Paul Levett, and Meredith Clemons for their guidance and instruction. Dr. Jordan Kuiper and Dr. Robert Canales are also acknowledged and thanked for their helpful insights.
Abbreviations
- PM
Particulate matter
- NO2
Nitrogen dioxide
- O3
Ozone
- COPD
Chronic obstructive pulmonary disease
- WHO
World Health Organization
- T4
Thyroxine
- T3
Triiodothyronine
- TSH
Thyroid-stimulating hormone
- PM2.5
Particulate matter of 2.5 microns
- ISA
Integrated Science Assessment
- PECO
Population, Exposure, Control, Outcome
- NOx
Nitrogen oxides
- FT3
Free triiodothyronine
- FT4
Free thyroxine
- TT4
Total thyroxine
- CHT
Congenital hypothyroidism
- PM10
Particulate matter of 10 microns
- PM2.5−10
Particulate matter of 2.5–10 microns
- CO
Carbon monoxide
- SO2
Sulfur dioxide
- As
Arsenic
- Be
Beryllium
- Cr
Chromium
- Mn
Manganese
- Se
Selenium
- Tl
Thallium
- Ba
Barium
- Na
Sodium
- Al
Aluminum
- Si
Silicon
- P
Phosphorous
- S
Sulfur
- Cl
Chlorine
- K
Potassium
- Ca
Calcium
- Ti
Titanium
- V
Vanadium
- Fe
Iron
- Ni
Nickel
- Cu
Copper
- Zn
Zinc
- Pb
Lead
- OM
Organic matter
- BC
Black carbon
- SO42−
Sulfate
- NO3−
Nitrate
- NH4+
Ammonium
- LUR
Land-use regression
Author contributions
C.O. conceived of the study, conducted the analysis, and was responsible for drafting the manuscript. E.J.C. conducted the literature review, evaluated risk of bias and strength and quality of the evidence, and contributed to manuscript writing. S.C.A. and S.M. reviewed the analysis and contributed to the manuscript writing. All authors read and approved the final manuscript.
Funding
We thank the George Washington University Milken Institute School of Public Health for supporting this project.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Brauer M, Roth GA, Aravkin AY, Zheng P, Abate KH, Abate YH et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. The Lancet [Internet]. 2024 May [cited 2024 Jun 28];403(10440):2162–203. https://linkinghub.elsevier.com/retrieve/pii/S0140673624009334 [DOI] [PMC free article] [PubMed]
- 2.Health Effects Institute. State of global air 2024 [Internet]. https://www.stateofglobalair.org/resources/report/state-global-air-report-2024
- 3.WHO global air. quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Executive summary [Internet]. p. 4. https://iris.who.int/bitstream/handle/10665/345334/9789240034433-eng.pdf [PubMed]
- 4.Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann [Internet]. 2014 Sep [cited 2024 Jun 29];45(3):301–14. 10.1111/j.1728-4465.2014.00393.x [DOI] [PMC free article] [PubMed]
- 5.World Health Organization. Billions of people still breathe unhealthy air: new WHO data [Internet]. 2022 [cited 2024 Jun 13]. https://www.who.int/news/item/04-04-2022-billions-of-people-still-breathe-unhealthy-air-new-who-data
- 6.Bai W, Li Y, Niu Y, Ding Y, Yu X, Zhu B et al. Association between ambient air pollution and pregnancy complications: A systematic review and meta-analysis of cohort studies. Environ Res [Internet]. 2020 Jun [cited 2024 Aug 20];185:109471. https://linkinghub.elsevier.com/retrieve/pii/S0013935120303649 [DOI] [PubMed]
- 7.Bekkar B, Pacheco S, Basu R, DeNicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open [Internet]. 2020 [cited 2024 Jun 28];3(6):e208243–e208243. https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2767260 [DOI] [PMC free article] [PubMed]
- 8.Kuehn L, McCormick S. Heat Exposure and Maternal Health in the Face of Climate Change. Int J Environ Res Public Health [Internet]. 2017 Jul 29 [cited 2024 Jun 29];14(8):853. https://www.mdpi.com/1660-4601/14/8/853 [DOI] [PMC free article] [PubMed]
- 9.Hehua Z, Qing C, Shanyan G, Qijun W, Yuhong Z. The impact of prenatal exposure to air pollution on childhood wheezing and asthma: a systematic review. Environ Res [Internet]. 2017 Nov [cited 2024 Jun 29];159:519–30. https://linkinghub.elsevier.com/retrieve/pii/S0013935117313841 [DOI] [PubMed]
- 10.Hu CY, Huang K, Fang Y, Yang XJ, Ding K, Jiang W et al. Maternal air pollution exposure and congenital heart defects in offspring: a systematic review and meta-analysis. Chemosphere [Internet]. 2020 Aug [cited 2024 Jun 29];253:126668. https://linkinghub.elsevier.com/retrieve/pii/S0045653520308614 [DOI] [PubMed]
- 11.Korten I, Ramsey K, Latzin P. Air pollution during pregnancy and lung development in the child. Paediatr Respir Rev [Internet]. 2017 Jan [cited 2024 Jun 29];21:38–46. https://linkinghub.elsevier.com/retrieve/pii/S1526054216300823 [DOI] [PubMed]
- 12.Volk HE, Perera F, Braun JM, Kingsley SL, Gray K, Buckley J et al. Prenatal air pollution exposure and neurodevelopment: a review and blueprint for a harmonized approach within ECHO. Environ Res [Internet]. 2021 May [cited 2024 Jun 29];196:110320. https://linkinghub.elsevier.com/retrieve/pii/S0013935120312172 [DOI] [PMC free article] [PubMed]
- 13.Burrow GN, Fisher DA, Larsen PR. Maternal and fetal thyroid function. N Engl J Med [Internet]. 1994 Oct 20 [cited 2024 Jun 28];331(16):1072–8.10.1056/NEJM199410203311608 [DOI] [PubMed]
- 14.Brent GA. Mechanisms of thyroid hormone action. J Clin Invest [Internet]. 2012 Sep 4 [cited 2024 Jun 28];122(9):3035–43. http://www.jci.org/articles/view/60047 [DOI] [PMC free article] [PubMed]
- 15.De Morreale G, Obregon M, Escobar Del Rey F. Role of thyroid hormone during early brain development. Eur J Endocrinol [Internet]. 2004 Nov 1 [cited 2024 Jun 28];U25–37. https://academic.oup.com/ejendo/article/151/Supplement_3/U25/6694487 [DOI] [PubMed]
- 16.Contempré B, Jauniaux E, Calvo R, Jurkovic D, Campbell S, De Escobar GM. Detection of thyroid hormones in human embryonic cavities during the first trimester of pregnancy. J Clin Endocrinol Metab [Internet]. 1993 Dec [cited 2024 Jun 28];77(6):1719–22. 10.1210/jcem.77.6.8263162 [DOI] [PubMed]
- 17.Korevaar TIM, Muetzel R, Medici M, Chaker L, Jaddoe VWV, De Rijke YB et al. Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: a population-based prospective cohort study. Lancet Diabetes Endocrinol [Internet]. 2016 Jan [cited 2024 Jun 29];4(1):35–43. https://linkinghub.elsevier.com/retrieve/pii/S2213858715003277 [DOI] [PubMed]
- 18.Medici M, Timmermans S, Visser W, De Muinck Keizer-Schrama SMPF, Jaddoe VWW, Hofman A et al. Maternal thyroid hormone parameters during early pregnancy and birth weight: the generation R study. J Clin Endocrinol Metab [Internet]. 2013 Jan [cited 2024 Jun 29];98(1):59–66. 10.1210/jc.2012-2420 [DOI] [PubMed]
- 19.Tanda M, Piantanida E, Lai A, Lombardi V, Dalle Mule I, Liparulo L et al. Thyroid autoimmunity and environment. Horm Metab Res [Internet]. 2009 Jun [cited 2024 Jun 29];41(06):436–42. http://www.thieme-connect.de/DOI/DOI?10.1055/s-0029-1215568 [DOI] [PubMed]
- 20.Prummel M, Strieder T, Wiersinga W. The environment and autoimmune thyroid diseases. Eur J Endocrinol [Internet]. 2004 May 1 [cited 2024 Jun 29];150(5):605–18. https://academic.oup.com/ejendo/article/150/5/605/6694370 [DOI] [PubMed]
- 21.Brent GA, Braverman L, Zoeller T. Thyroid health and the environment. thyroid [Internet]. 2007 Sep [cited 2024 Jun 28];17(9):807–9. https://www.liebertpub.com/doi/10.1089/thy.2007.1514 [DOI] [PubMed]
- 22.Pearce EN, Braverman LE. Environmental pollutants and the thyroid. Best Pract Res Clin Endocrinol Metab [Internet]. 2009 Dec [cited 2024 Jun 29];23(6):801–13. https://linkinghub.elsevier.com/retrieve/pii/S1521690X0900075X [DOI] [PubMed]
- 23.Zoeller TR, Dowling ALS, Herzig CTA, Iannacone EA, Gauger KJ, Bansal R. Thyroid hormone, brain development, and the environment. Environ Health Perspect [Internet]. 2002 Jun [cited 2024 Jun 29];110(suppl 3):355–61. 10.1289/ehp.02110s3355 [DOI] [PMC free article] [PubMed]
- 24.Murthy MB, Murthy BK. Thyroid disruptors and their possible clinical implications. Indian J Pharmacol. 2012;44(4):542–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burek CL, Talor MV. Environmental triggers of autoimmune thyroiditis. J Autoimmun [Internet]. 2009 Nov [cited 2024 Jun 28];33(3–4):183–9. https://linkinghub.elsevier.com/retrieve/pii/S0896841109001152 [DOI] [PMC free article] [PubMed]
- 26.Tomer Y, Huber A. The etiology of autoimmune thyroid disease: a story of genes and environment. J Autoimmun [Internet]. 2009 May [cited 2024 Jun 29];32(3–4):231–9. https://linkinghub.elsevier.com/retrieve/pii/S0896841109000341 [DOI] [PMC free article] [PubMed]
- 27.Hu CY, Gao X, Fang Y, Jiang W, Huang K, Hua XG et al. Human epidemiological evidence about the association between air pollution exposure and gestational diabetes mellitus: systematic review and meta-analysis. Environ Res [Internet]. 2020 Jan [cited 2024 Jun 29];180:108843. https://linkinghub.elsevier.com/retrieve/pii/S0013935119306401 [DOI] [PubMed]
- 28.Heo YJ, Kim HS. Ambient air pollution and endocrinologic disorders in childhood. Ann Pediatr Endocrinol Metab [Internet]. 2021 Sep 30 [cited 2024 Jun 29];26(3):158–70. http://e-apem.org/journal/view.php?doi=10.6065/apem.2142132.066 [DOI] [PMC free article] [PubMed]
- 29.Liu J, Zhao K, Qian T, Li X, Yi W, Pan R et al. Association between ambient air pollution and thyroid hormones levels: a systematic review and meta-analysis. Sci Total Environ [Internet]. 2023 Dec [cited 2024 Jun 29];904:166780. https://linkinghub.elsevier.com/retrieve/pii/S0048969723054050 [DOI] [PubMed]
- 30.Rohani F, Rezayat AA, Rohani B, Liaghat A, Najafi S, Jafari N et al. Air pollution and thyroid abnormalities: systematic review and meta-analysis [Internet]. 2023 [cited 2024 Jun 29]. https://www.researchsquare.com/article/rs-3021590/v1
- 31.Johnson PI, Sutton P, Atchley DS, Koustas E, Lam J, Sen S et al. The navigation guide—evidence-based medicine meets environmental health: systematic review of human evidence for PFOA effects on fetal growth. Environ Health Perspect [Internet]. 2014 Oct [cited 2024 Jun 29];122(10):1028–39. 10.1289/ehp.1307893 [DOI] [PMC free article] [PubMed]
- 32.U.S. EPA. Integrated science assessment (ISA) for particulate matter [Internet]. 2019 Dec. https://assessments.epa.gov/risk/document/&deid=347534
- 33.Janssen BG, Saenen ND, Roels HA, Madhloum N, Gyselaers W, Lefebvre W et al. Fetal thyroid function, birth weight, and in Utero exposure to fine particle air pollution: a birth cohort study. Environ Health Perspect [Internet]. 2017 Apr [cited 2024 Jun 29];125(4):699–705. 10.1289/EHP508 [DOI] [PMC free article] [PubMed]
- 34.Lavigne E, Ashley-Martin J, Dodds L, Arbuckle TE, Hystad P, Johnson M et al. Air pollution exposure during pregnancy and fetal markers of metabolic function: the MIREC study. Am J Epidemiol [Internet]. 2016 May 1 [cited 2024 Jun 29];183(9):842–51. 10.1093/aje/kwv256 [DOI] [PMC free article] [PubMed]
- 35.Seth A, Rashmi M, Bhakhri B, Sekri T. Neonatal thyroid screening: Relationship between cord blood thyroid stimulating hormone levels and thyroid stimulating hormone in heel prick sample on 4th to 7th day-of-life. Indian J Endocrinol Metab [Internet]. 2014 [cited 2024 Sep 11];18(1):125. 10.4103/2230-8210.126599 [DOI] [PMC free article] [PubMed]
- 36.PubMed [Internet]. https://pubmed.ncbi.nlm.nih.gov/
- 37.Scopus [Internet]. https://www-scopus-com.proxygw.wrlc.org/search/form.uri?display=basic#basic
- 38.ProQuest Environmental [Internet]. https://www.proquest.com/
- 39.Cochrane Reviews [Internet]. https://www.cochranelibrary.com/
- 40.Covidence. [Internet]. https://www.covidence.org
- 41.Chamot S, Al-Salameh A, Petit P, Bonneterre V, Cancé C, Decocq G et al. Does prenatal exposure to multiple airborne and tap-water pollutants increase neonatal thyroid-stimulating hormone concentrations? Data from the Picardy region, France. Sci Total Environ [Internet]. 2023 Dec [cited 2024 Jun 29];905:167089. https://linkinghub.elsevier.com/retrieve/pii/S0048969723057169 [DOI] [PubMed]
- 42.Ghassabian A, Pierotti L, Basterrechea M, Chatzi L, Estarlich M, Fernández-Somoano A et al. Association of exposure to ambient air pollution with thyroid function during pregnancy. JAMA Netw Open [Internet]. 2019 Oct 16 [cited 2024 Jun 29];2(10):e1912902. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2752988 [DOI] [PMC free article] [PubMed]
- 43.Gong Y, Zhao Y, Zhang X, Zhao X, Chang H, Huang J et al. Ambient particulate matter, maternal thyroid function, and birth weight: a mediation analysis. Ecotoxicol Environ Saf [Internet]. 2023 Oct [cited 2024 Jun 29];264:115420. https://linkinghub.elsevier.com/retrieve/pii/S0147651323009247 [DOI] [PubMed]
- 44.Harari-Kremer R, Calderon-Margalit R, Korevaar TIM, Nevo D, Broday D, Kloog I et al. Associations between prenatal exposure to air pollution and congenital hypothyroidism. Am J Epidemiol [Internet]. 2021 Dec 1 [cited 2024 Jun 29];190(12):2630–8. https://academic.oup.com/aje/article/190/12/2630/6310595 [DOI] [PubMed]
- 45.Howe CG, Eckel SP, Habre R, Girguis MS, Gao L, Lurmann FW et al. Association of prenatal exposure to ambient and traffic-related air pollution with newborn thyroid function: findings from the children’s health study. JAMA Netw Open [Internet]. 2018 Sep 14 [cited 2024 Jun 29];1(5):e182172. http://jamanetworkopen.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2018.2172. [DOI] [PMC free article] [PubMed]
- 46.Ilias I, Kakoulidis I, Togias S, Stergiotis S, Michou A, Lekkou A et al. Atmospheric pollution and thyroid function of pregnant women in Athens, Greece: a pilot study. Med Sci [Internet]. 2020 Apr 4 [cited 2024 Jun 29];8(2):19. https://www.mdpi.com/2076-3271/8/2/19. [DOI] [PMC free article] [PubMed]
- 47.Irizar A, Txintxurreta A, Molinuevo A, Jimeno-Romero A, Anabitarte A, Álvarez JI et al. Association between prenatal exposure to air pollutants and newborn thyroxine (T4) levels. Environ Res [Internet]. 2021 Jun [cited 2024 Jun 29];197:111132. https://linkinghub.elsevier.com/retrieve/pii/S0013935121004266 [DOI] [PubMed]
- 48.Li J, Liao J, Hu C, Bao S, Mahai G, Cao Z et al. Preconceptional and the first trimester exposure to PM2.5 and offspring neurodevelopment at 24 months of age: Examining mediation by maternal thyroid hormones in a birth cohort study. Environ Pollut [Internet]. 2021 Sep [cited 2024 Jun 29];284:117133. https://linkinghub.elsevier.com/retrieve/pii/S0269749121007156 [DOI] [PubMed]
- 49.Nourouzi Z, Chamani A. Characterization of ambient carbon monoxide and PM 2.5 effects on fetus development, liver enzymes and TSH in Isfahan City, central Iran. Environ Pollut [Internet]. 2021 Dec [cited 2024 Jun 29];291:118238. https://linkinghub.elsevier.com/retrieve/pii/S0269749121018200 [DOI] [PubMed]
- 50.Qi C, Shang L, Yang W, Huang L, Yang L, Xin J et al. Maternal exposure to O3 and NO2 may increase the risk of newborn congenital hypothyroidism: a national data-based analysis in China. Environ Sci Pollut Res [Internet]. 2021 Jul [cited 2024 Jun 29];28(26):34621–9. 10.1007/s11356-021-13083-6 [DOI] [PMC free article] [PubMed]
- 51.Qiu L, Shen W, Ye C, Wu J, Zheng S, Lou B et al. Association of exposure to PM2.5-bound metals with maternal thyroid function in early pregnancy. Sci Total Environ [Internet]. 2022 Mar [cited 2024 Jun 29];810:151167. https://linkinghub.elsevier.com/retrieve/pii/S0048969721062458 [DOI] [PubMed]
- 52.Shang L, Huang L, Yang W, Qi C, Yang L, Xin J et al. Maternal exposure to PM2.5 may increase the risk of congenital hypothyroidism in the offspring: a national database based study in China. BMC Public Health [Internet]. 2019 Dec [cited 2024 Jun 29];19(1):1412. 10.1186/s12889-019-7790-1 [DOI] [PMC free article] [PubMed]
- 53.Sun Q, Chen Y, Ye F, Liu J, Liu D, Ao B et al. Association of hypothyroidism during pregnancy with preconception and early pregnancy exposure to ambient particulate matter. Environ Sci Pollut Res [Internet]. 2023 Jul 12 [cited 2024 Jun 29];30(37):88084–94. 10.1007/s11356-023-28683-7 [DOI] [PMC free article] [PubMed]
- 54.Wang X, Liu C, Zhang M, Han Y, Aase H, Villanger GD et al. Evaluation of maternal exposure to PM 2.5 and its components on maternal and neonatal thyroid function and birth weight: a cohort study. Thyroid [Internet]. 2019 Aug [cited 2024 Jun 29];29(8):1147–57. 10.1089/thy.2018.0780 [DOI] [PubMed]
- 55.Zeng Z, Xu X, Wang Q, Zhang Z, Meng P, Huo X. Maternal exposure to atmospheric PM2.5 and fetal brain development: Associations with BAI1 methylation and thyroid hormones. Environ Pollut [Internet]. 2022 Sep [cited 2024 Jun 29];308:119665. https://linkinghub.elsevier.com/retrieve/pii/S026974912200879X [DOI] [PubMed]
- 56.Zhang X, Huels A, Makuch R, Zhou A, Zheng T, Xia W et al. Association of exposure to ambient particulate matter with maternal thyroid function in early pregnancy. Environ Res [Internet]. 2022 Nov [cited 2024 Jun 29];214:113942. https://linkinghub.elsevier.com/retrieve/pii/S0013935122012695 [DOI] [PubMed]
- 57.Zhao Y, Cao Z, Li H, Su X, Yang Y, Liu C et al. Air pollution exposure in association with maternal thyroid function during early pregnancy. J Hazard Mater [Internet]. 2019 Apr [cited 2024 Jun 29];367:188–93. https://linkinghub.elsevier.com/retrieve/pii/S0304389418312263 [DOI] [PubMed]
- 58.Zhou Y, Zhu Q, Wang P, Li J, Luo R, Zhao W et al. Early pregnancy PM2.5 exposure and its inorganic constituents affect fetal growth by interrupting maternal thyroid function. Environ Pollut [Internet]. 2022 Aug [cited 2024 Jun 29];307:119481. https://linkinghub.elsevier.com/retrieve/pii/S0269749122006959 [DOI] [PubMed]
- 59.Kassotis CD, Iwanowicz LR, Akob DM, Cozzarelli IM, Mumford AC, Orem WH et al. Endocrine disrupting activities of surface water associated with a West Virginia oil and gas industry wastewater disposal site. Sci Total Environ [Internet]. 2016 Jul [cited 2024 Jun 29];557–558:901–10. https://linkinghub.elsevier.com/retrieve/pii/S0048969716305356 [DOI] [PubMed]
- 60.Liu Y, Chen H, Zhang L, Zhang T, Ren X. The association between thyroid injury and apoptosis, and alterations of Bax, Bcl-2, and Caspase-3 mRNA/Protein expression induced by nickel sulfate in wistar rats. Biol Trace Elem Res [Internet]. 2020 May [cited 2024 Jun 29];195(1):159–68. 10.1007/s12011-019-01825-0 [DOI] [PubMed]
- 61.Rezaei M, Javadmoosavi SY, Mansouri B, Azadi NA, Mehrpour O, Nakhaee S. Thyroid dysfunction: how concentration of toxic and essential elements contribute to risk of hypothyroidism, hyperthyroidism, and thyroid cancer. Environ Sci Pollut Res [Internet]. 2019 Dec [cited 2024 Jun 29];26(35):35787–96. 10.1007/s11356-019-06632-7 [DOI] [PubMed]
- 62.Di Ciaula A, Bonfrate L, Noviello M, Portincasa P. Thyroid function: a target for endocrine disruptors, air pollution and radiofrequencies. Endocr Metab Immune Disord Drug Targets [Internet]. 2023 Jul [cited 2024 Aug 20];23(8):1032–40. https://www.eurekaselect.com/196304/article [DOI] [PubMed]
- 63.Derakhshan A, Shu H, Peeters RP, Kortenkamp A, Lindh CH, Demeneix B et al. Association of urinary bisphenols and triclosan with thyroid function during early pregnancy. Environ Int [Internet]. 2019 Dec [cited 2024 Jun 29];133:105123. https://linkinghub.elsevier.com/retrieve/pii/S0160412019319361 [DOI] [PubMed]
- 64.Burggren WW, Mueller CA. Developmental critical windows and sensitive periods as three-dimensional constructs in time and space. Physiol Biochem Zool [Internet]. 2015 Mar [cited 2024 Jun 28];88(2):91–102. 10.1086/679906 [DOI] [PubMed]
- 65.Delitala AP, Capobianco G, Cherchi PL, Dessole S, Delitala G. Thyroid function and thyroid disorders during pregnancy: a review and care pathway. Arch Gynecol Obstet [Internet]. 2019 Feb [cited 2024 Jun 28];299(2):327–38. 10.1007/s00404-018-5018-8 [DOI] [PubMed]
- 66.McNeil AR, Stanford PE. Reporting thyroid function tests in pregnancy. Clin Biochem Rev. 2015;36(4):109–26. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.