Abstract
Background
Persons with disabilities (PwDs) experience various adverse sexual and reproductive health (SRH) outcomes. However, there is a paucity of evidence on the strategies to improve their SRH outcomes. This study, therefore, used a pluralistic approach to explore PwDs and healthcare providers’ (HPs) perspectives on how to improve the SRH of PwDs in Ghana.
Methods
In-depth interviews were conducted with 62 purposively selected stakeholders (37 PwDs and 25 HPs) in the Kumasi Metropolis and Offinso North District. The data was subjected to reflexive thematic analysis.
Results
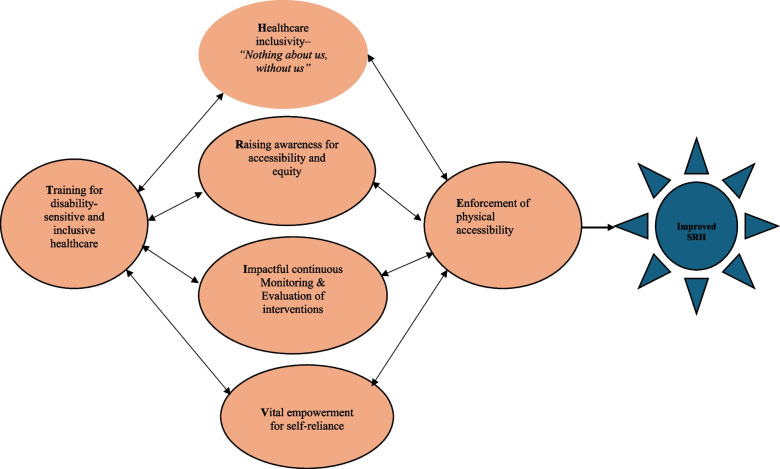
Six major themes were generated from the data: Training for disability-sensitive and inclusive healthcare, Healthcare inclusivity – ‘nothing about us, without us’, Raising awareness for accessibility and equity, Impactful continuous monitoring and evaluation, Vital empowerment for self-reliance and Educating for disability-inclusive healthcare environment.
These recommendations were synthesised to develop the THRIVE model–a comprehensive data driven framework from stakeholders that emphasises the importance of factors such as Training for disability-sensitive and inclusive healthcare, Healthcare inclusivity – ‘nothing about us, without us’, Raising awareness for accessibility and equity, Impactful continuous monitoring and evaluation, Vital empowerment for self-reliance and Enforcement of physical accessibility to improve their SRH outcomes.
Conclusion
Using the evidence based THRIVE model could facilitate the development and strengthening of existing interventions and policies including the disability Act 715 to improve the SRH access and outcomes of PwDs in Ghana and other low-and middle-income countries.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12939-024-02269-2.
Keywords: Disability, Ghana, Outcomes, Recommendations, Sexual and reproductive health
Background
Globally, there are over one billion individuals living with disabilities, constituting 16% of the world's population [1]. Disability is more prevalent in low- and middle-income countries (LMICs) [1]. The interplay of factors including childhood diseases, limited access to healthcare, high rates of injuries, limited access to rehabilitation services and poverty are some of the major contributing factors [2–4]. Persons with disabilities (PwDs) encounter challenges and barriers in various aspects of life due to lower income, limited education, unemployment, and accessibility issues [5]. These barriers encompass political, health, economic, environmental, cultural, personal, and social dimensions, with the latter involving stigma and discrimination [6, 7]. These barriers are interconnected and contribute to overall poor health including sexual and reproductive health (SRH) [8]. Available evidence indicates that the complicated nature of the challenges faced by PwDs make them susceptible to adverse SRH outcomes including sexual exploitation or abuse [9, 10], unintended pregnancies [11], and sexually transmitted infections (STIs) [12].
Considering these fundamental causes of disparities, it is essential to formulate practical recommendations or strategies aimed at enhancing access to SRH care for PwDs, thereby improving their overall well-being. This holds particular significance as evidence suggests that proposing recommendations or strategies integrating the needs of PwDs could effectively mitigate health disparities, thus warranting the designation of a primary research priority in LMICs [13, 14]. The SRH of PwDs has garnered significant global attention, as reflected in major international documents such as the United Nations (UN) Convention on the Rights of Persons with Disabilities (UNCRPD). It mandates governments to ensure access to SRH services for PwDs [15]. Additionally, Sustainable Development Goals (SDG) 3.7 and 5.6 aim to achieve universal access to SRH [16] for all including PwDs.
In response to the UN mandate, Ghana which is a LMIC country in West Africa enacted policies such as the passage of the Disability Act 715 in 2006 [17], addressing the health needs of PwDs and their overall well-being. This Act mandates that the Ministry of Health formulates policies ensuring free general and specialist medical care, rehabilitative care, and suitable assistive devices for individuals with severe disabilities [17]. Additionally, the government introduced a national health insurance scheme (NHIS) to enhance healthcare affordability, broadening access to basic healthcare for all residents, including those with disabilities [18]. Despite these policies, evidence indicates that practical implementation remains problematic, as interactions between PwDs and the healthcare system often result in access barriers, including insufficient services, financial constraints, inaccessible facilities and equipment, and negative provider attitudes [13, 18–22].
Prior research in Ghana has improved our understanding of the factors affecting PwDs access to SRH [8, 13, 18–23]. These studies have mainly focused on perspectives from healthcare providers (HPs) or PwDs in general, for the aim of enhancing healthcare provision for the broader disability population in Ghana [24]. However, there is limited research specifically addressing recommendations from key stakeholders–both service providers (HPs) and service users (PwDs) to enhance SRH delivery for this population [24, 25]. The existing studies often have limitations in scope, such as focusing on high-income countries [25] or having restricted breadth [24]. A critical step to improving SRH outcomes for PwDs is fostering shared decision-making, whereby HPs who are charged with provision of healthcare and the PwDs who are the end users are both involved in the decision-making process in relation to appropriateness and timeliness of medical treatment that meet the unique needs of PwDs. Hence, it is important to build upon previous research by utilising recommendations proffered by these stakeholders to develop effective strategies that enhance SRH delivery for PwDs. In addition, health policy and systems research should prioritise ‘people-centredness’, particularly emphasising the most vulnerable, when providing systematic recommendations to policymakers for addressing equity and social justice [26, 27].
This study seeks to address the gaps in the literature with the following aims: a) to explore stakeholders views regarding strategies or recommendations to improve SRH outcomes for PwDs and b) to synthesise the recommendations to develop a conceptual model [28]. Deepening the knowledge of both service users’ and providers’ recommendations can address health disparities and enhance healthcare quality for PwDs in Ghana and similar LMICs. Addressing these aims is quintessential to inform how SRH policies for PwDs should be designed and implemented to achieve better SRH outcomes. This aligns with the objectives of SDG 3.7 and 5.6, which emphasises universal health coverage, access to quality health, and equity in healthcare as crucial for sustainable development [16].
Methods
Ethics
This study obtained ethical clearance from three institutional review committees: the Ghana Health Service (GHS) Ethics Review Committee (GHS-ERC: 005–0621), the Komfo Anokye Teaching Hospital (KATH) (KATH-IRB/RR/101/21), and the James Cook University (JCU) Human Research Ethics Committee (H8531). Additionally, official approval was granted by the Regional Health Directorate in Kumasi and the Offinso North District Health Directorate in Akumadan, as well as by leaders of two disability organisations in these settings. The study prioritised the confidentiality of all participants’ information and data. Before administering the research instrument, each participant received a comprehensive document outlining the study's objectives, emphasising the significance of confidentiality, and highlighting the potential benefits of participation. Participants were informed of the voluntary nature of their involvement and their right to withdraw from the project at any point. Furthermore, participants were assured that their data would be used exclusively for academic purposes and that their identities would remain undisclosed to third parties. Both written and verbal informed consents were obtained from all participants.
Study area and design
This study was conducted in the Kumasi Metropolis and Offinso North district in the Ashanti Region of Ghana as part of a broader research project on the impact of health policies and interventions on the sexual and reproductive health outcomes of PwDs in the Ashanti region, with relevant findings published elsewhere [21, 22]. Employing a descriptive qualitative study design [29] and a pluralistic framework, the research aimed to explore the perspectives and experiences of stakeholders, including HPs and PwDs, regarding the strategies to improve the SRH outcomes. The pluralistic approach involved synthesising the viewpoints of PwDs and HPs to reach common elements in the data on strategies for improving the SRH of PwDs [30, 31]. The study adhered to the Consolidated Criteria for Reporting Qualitative Studies (COREQ) guidelines (Appendix 1).
Target population and sample
This study involved 62 participants, comprising 25 HPs and 37 PwDs. Participant were selected purposively, encompassing the identification of individuals representing the population through a pre-interview survey [21, 22]. Specifically, HPs comprised doctors, nurses and midwives while PwDs comprised those with visual impairment and physical disabilities [21, 22]. Principles of data saturation guided the sample size determination [32].
Data collection
Trained female research assistant (RA) and the first author (AS) conducted all the in-depth interviews in English and Twi in various locations including, disability resource centres, participants’ homes, and health facilities, and at times convenient to each participant and the interviewer. The interview guides have been attached as appendices (Appendix 2 and 3). Each interview was digitally recorded with the consent of the participants. Field notes were taken during and after each interview recording non-verbal cues and researcher reflections. Probes were repeatedly used to elicit detailed information or clarification of certain concepts used by the participants. The interviews lasted an average of 65 min.
Data analysis
After conducting interviews, the first author (AS) and the RA translated and transcribed the interviews that were conducted in Twi into English. Cross-language methodological consideration were considered [33]. For example, both AS and the RA are fluent in Twi and also experienced translators. These transcripts were also cross-referenced with the original audio recordings to ensure alignment. The data was analysed thematically [28, 34, 35] using NVivo version 12 (QSR International, Ltd., Daresbury Cheshire, UK). Specifically, transcripts were carefully reviewed, noting, and highlighting significant points to identify codes. AS initiated "grouping of codes into themes" stage, with input from KMR and TIE, who held frequent discussions to refine the structure and direction. In the third stage, the research team identified grouped themes into thematic networks. Subsequently, in the fourth stage, further exploration of thematic networks for relationships was done by the team, establishing connections. The next stage involved the development of a conceptual model linking the conceptual findings in the thematic network to the research question [28]. The team collaboratively identified and reached consensus on relevant quotes related to the themes. Ultimately, verbatim quotes, along with relevant demographic information (e.g., sex, age, type of health worker, type of disability, and district), were used to represent the themes from the data.
Results
Demographic characteristics of participants
The study included 62 participants, comprising 37 PwDs (22 males and 15 females) with ages ranging from 21 to 60 years. Most of the PwDs were from the Kumasi Metropolis (n = 24), belonged to the Akan ethnic group (n = 31), identified as Christians (n = 34), and were married (n = 19). Thirteen were from the Offinso North district (n = 13). Twenty-five HPs were included in the study (16 females and 9 males). Their ages ranged from 28 to 60 years. Nine were from the Offinso North district and 16 were from Kumasi metropolis. Work experience spanned from 1 to 40 years.
Themes generated from data
This section of the study presents the recommendations that stakeholders (HPs and PwDs) suggested as strategies to improve the SRH outcomes among PwDs in Ghana. Six themes were derived from the data, and these are discussed in the next section. The themes were: Training for disability-sensitive and inclusive healthcare, Healthcare inclusivity – ‘nothing about us, without us’, Raising awareness for accessibility and equity, Impactful continuous monitoring and evaluation, Vital empowerment for self-reliance and Enforcement of physical accessibility to improve their SRH outcomes. These themes were used to develop the THRIVE model (Fig. 1).
Fig. 1.
Conceptual model–THRIVE to improve sexual and reproductive health outcomes for persons with disability
Development and description of the THRIVE model
Morgan [36] defined models as “systematic depictions of the relationships among a set of concepts”, serving as a bridge between themes and higher-level theories in qualitative research (p.340). Themes represent significant patterns within data, aiding interpretation, while theories explain why themes are related as depicted in the model [36] (p.339). Tolley et al. [37] characterised conceptual models as “integrated assumptions drawing on substantive theories to define a problem in a specific setting or context. These models guide research domains and questions, or they may emerge from the analysis as a means of synthesising qualitative data” (p.39). Similarly, Börner et al. [38] stated that, “a model is a systematic description of an object or phenomenon sharing characteristics with its real-world counterpart and supporting detailed investigation, supporting theory creation. Models serve to simplify real-world complexity and provide generalisable representations for practical solutions, advancing knowledge [39].
Framework on the other hand is defined as a synthesised set of components and variables used to address real-world problems, serving as the lens through which issues are deduced and resolved [40]. Its development starts with the assumption of a problem and involves applying various methods, models, or theories for resolution. Imenda [40] thus argues that the synthesis may be called a model or conceptual framework, which essentially represents an ‘integrated’ way of looking at a problem (p.189). Hence, model and framework would be used interchangeably in this study.
A review of the literature showed that existing models and frameworks on strategies to improve access to healthcare and SRH outcomes among PwDs is scarce [25, 41]. The few existing ones were done in countries such as the United States of America [25] or Guatemala [41]. These previous models were also limited in scope. For instance, the model by Hashemi et al. [41] solicited the views of only PwDs, however, to foster effective delivery of health services, the recommendations from both service providers and receivers are indispensable [25]. These factors propelled the development of the multidimensional THRIVE model. In this current study the THRIVE model (Fig. 1) is a complex interrelated model developed based on the themes generated from stakeholders’ recommendations on strategies to improve the SRH outcomes of PwDs.
THRIVE is an acronym representing the themes from the data. In this conceptual model, each sphere “O” signifies a recommendation, with the star “*” symbolising the outcome–improved SRH. The arrows “ ↔ ” depict the multidirectional influence among themes, illustrating potential overlaps and mutual influence. The model suggests that despite distinct themes, its components are interconnected. The influence of the components may vary due to PwDs socio-demographic characteristics, social conditions, health system characteristics and responsiveness, and perceived severity of health conditions and treatment necessity [41]. According to the model, to improve the SRH outcomes of PwDs, six factors could be considered. These include Training for disability-sensitive and inclusive healthcare, Healthcare inclusivity – ‘nothing about us, without us’, Raising awareness for accessibility and equity, Impactful continuous monitoring and evaluation, Vital empowerment for self-reliance and Enforcement of physical accessibility. Detailed description of these factors and the various quotes from the participants are presented in the subsequent section of this paper.
Theme 1: training for disability- sensitive and inclusive healthcare
The first theme that was generated from the data was disability sensitive and inclusive healthcare training as a prominent strategy for enhancing SRH outcomes of PwDs. Specifically, both HPs and PwDs emphasised the necessity of integrating disability-related topics into health training institutions, including sign language, and offering regular refresher training to HPs.
“… Ghana Health Service should give training to nurses on sign languages so that they can communicate with persons living with disability–Hearing impaired. They can teach them common signs on vomiting, headache,and STI issues. Ghana Health Service from time to time should conduct workshops for health care providers on sign languages and ways to provide support for person living with disability. We need proper training on how to handle people with disability, because they are also part of us, and we must handle them with care. The health administration and management should also educate their staff on how to handle and take care of people with disability”. [Doctor, Kumasi, Male, 28 years]
A significant proportion of PwDs underscored the pivotal role of education and training in fostering a deeper understanding of the needs of PwDs. They advocated for clear instructions on medication usage, emphasising that HPs cannot rely on follow-up at home to ensure proper adherence. This highlights the importance of effective communication strategies and the provision of accessible information to all patients.
“Healthcare providers should be trained about inclusiveness. As I am blind [visually impaired], if I am pregnant and I come to the facility, they should know how to care for me. Sometimes, they don’t indicate how you should take the medicines. Because they are not going to follow up at home to see how I am taking the medications, they have to be courteous to provide clear information". [Visually Impaired, Offinso, Female, 51 years]
“I think there should be a disability training for them [HPs] whereby they will be trained on disability issues. In Ghana, 26 categories of disabilities have been identified and I’m sure if they are trained on all these categories, they will be able to work on it. Some are the visually impaired, the hearing impaired, the deaf blind, the multiple disability, etc. Some of them I cannot pronounce off head”. [Visually Impaired, Kumasi, Male, 31 years]
Moreover, both HPs and PwDs described the significance of sign language training to facilitate effective communication and the provision of high-quality SRH care for patients with hearing impairments. Some participants also shared that such training would contribute to the prioritisation of PwDs within healthcare facilities whenever they seek medical care.
“…As I said the disability is in forms, so if we empower all the health care workers in their various areas they will put in their best. If we check all these things and everybody perform their duty well, you know most often we do assessment, ideally, I have to work at the ANC, but I can’t do it, because when the child is born and there is something they didn’t pick from there I will pick from there and continue. The teachers who are expert in sign language should conduct training for nurses and teach them sign language on sexual reproductive health like how to say penis or your penis or vagina is itching you. It is quite complicated because there is no single word for sexual and reproductive health”. [ Nurse, Kumasi, Female, 59 years]
“I think that people in general should be made to understand the needs and rights of PwDs. There are times that when you go to the hospital, some people will allow you to be prioritised. But there are others who will never allow you to see the health professionals before they do. And so, if they are made to understand that we are vulnerable and have special needs, then it will increase our health-seeking behaviour”. [Physically Disabled, Offinso, Female, 60 years]
Furthermore, PwDs emphasised that this training is vital for cultivating empathy, compassion, and addressing stereotypes through the virtues of patience, tolerance, and respectful care. They emphasised the fundamental need for HPs to be consistently available and attentive to their needs, highlighting a lack of trust that arises from past experiences of deception or neglect. They also connected this neglect and mistrust to harmful influence of traditional beliefs and misconceptions surrounding disabilities and how deeply ingrained societal attitudes can exacerbate the challenges faced by PwDs.
"The healthcare providers should always be ready to attend to us and assist us all the time. Sometimes because we cannot see they will lie to us that they have done the thing for us but in a real sense they have not. And the traditional beliefs and misconceptions that we are disabled because of our bad deeds or others is what is fuelling this". [Visually Impaired, Kumasi, Male, 45 years]
"Sometimes, some of the healthcare providers disrespect us. Therefore, it is important for the government to invest in education for the service providers on how to provide respectful care to us". [Visually Impaired, Offinso, Female, 33 years]
Theme 2: healthcare inclusivity – ‘nothing about us, without us’
The second recommendation that the stakeholders, especially all the PwDs, made was the need to ensure that PwDs are included in the design and development of policies, particularly those related to SRH, to help them fully benefit from these policies. Previous studies have noted the low level of inclusiveness of PwDs in policy development [42, 43]. The participants emphasised the importance of active engagement and participation of PwDs in the development of policies and programs that directly affect their lives.
“How can you formulate a policy without those who will benefit from it? It is not logical. So, it should be like ‘nothing about us, without us’. So, they need to involve us and get to know of our needs so that they can allocate the available resources to meet our needs. If they cannot involve all of us, they should involve the leaders of the disability unions”. [Visually Impaired, Kumasi, Male, 38 years]
Elaborating on this, some of the participants indicated the need to actively involve the National Council of Disability–a mouthpiece for PwDs established from the recommendations of the 2006 National Disability Act [17].
“They should make sure that the National Council of Disability should be a lead…because there should not be nothing about us, without us–you can’t decide for us if you don’t consult us. You are not in our shoes, and you are looking at it from your own perspective, how can you advocate well for that person. Even if you are empathising with someone, you will but will not understand what is actually in it". [Visually Impaired, Kumasi, Male, 31 years]
Other PwDs expressed this differently as follows:
"There is an adage that says, ‘the one closer to his fire is the person who best knows how hot the fire is.' This means that PwDs should be actively involved in the healthcare policies that are made for us". [Visually Impaired, Offinso, Male 49 years].
Similarly, another PwD said, "There is a saying that 'he who is sitting by the fire knows best how hot it is.' Meaning we as PwDs should play an active role in the development of policies and legislations that are about us. If they don't include us, they can’t develop policies that directly meet our needs". [Visually Impaired, Kumasi, Male 45 years].
These quotes aptly convey the principle of meaningful inclusion in policymaking and serve as a metaphorical reminder of the importance of involving PwDs in the formulation of healthcare policies and interventions that directly affect their SRH lives. Some HPs also shared their views as follows:
“With respect to inclusion, we should make sure PwD are included in every policy or programmes carried out by government because you can’t initiate a program for the disabled and ignore or reject their opinions and contributions. If you do so, then the policies cannot be implemented well so it’s good to include persons with disabilities in each and every policy government seeks to formulate for them because it will make them have ownership of that policy and will abide by them as their motto goes “nothing about us, without us”.[Nurse, Kumasi, Male, 42 years]
Participants also discussed that involving PwDs in policy development is not just about token representation but genuine engagement, where their voices and concerns are taken seriously.
“There is the need for policy makers to include PwDs in the development of policies and programmes. If they include us in programme development, we can let them know our pressing concerns when it comes to SRH issues as well as other issues. For instance, for the health insurance, we could have told them that due to our circumstance, they have to make all healthcare services free for PwDs. ‘There is a saying that the one who scrubs your back is the one who knows what is on your butt’. Like how you have called me today to ask about our issues, if they do more of that by including us in policy development, it will go a long way to help all of us. So, we plead that the policy makers remember to include us during the policy and intervention developments”. [Visually Impaired, Offinso, Male, 55 years]
Theme 3: raising awareness for accessibility and equity
Another major theme arising from the data concerning the improvement of SRH outcomes among PwDs pertains to creating awareness to dispel misconceptions and enhance accessibility and equity. This theme encompassed sub-issues involving community and national-level education and awareness initiatives regarding SRH for PwDs. Furthermore, all stakeholders underscored the critical role of cultivating positive attitudes and raising awareness about disability-related issues within the broader population, recognizing this as a pivotal measure for improving SRH outcomes for PwDs. Given the prevailing stigmatisation and discrimination encountered by PwDs, participants advocated for the promotion of positive attitudes within both the public and the healthcare system to facilitate equitable access to SRH services.
“If you are aware of your rights and the SRH services available to you as a PwD, then you are likely to use the services. So, I think that should be improved. Also, because of our culture, we have a lot of misconceptions about disability, especially intellectual disability. So, the community members should be educated to understand that disabled people are not taboos or spiritual beings. It is so bad that you cannot become a chief or work with traditional authority. That is why people had a challenge when the Minister for Chieftaincy [Formal Minister] was a PwD. There is total stigmatisation nationwide. That is why if you are not careful, your partner will leave you”. [Visually Impaired, Offinso, Male, 55 years]
“Awareness should be created among people that disability has got nothing to do with spirituality... it is as a result of something that brings about the disability. Parents should not hide their children because of the stigma so that they will also have equal access to education, healthcare, and other things. When all these things are put in place, it will help a lot". [Nurse, Kumasi, Female, 46 years]
Educational strategies encompassed community outreach programs, the dissemination of information through social media platforms, and engagement with community radio stations to educate the public about the rights and capabilities of PwDs in freely expressing their sexual desires and accessing SRH services.
"…Yeah, awareness like I said if there is public education about people with disability. Sometimes the stigma alone doesn’t even let some of us come out so if through some of the government institutions like the National Commission for Civic Education can educate the public this will be good via social media platforms, and engagement with community radio stations to educate the public...". [Visually Impaired, Kumasi, Male, 25 years]
Participants also discussed the impacts of misconceptions that PwDs are asexual, thus hindering their access to and the provision of SRH services by HPs. To address this challenge, participants also recommended conducting additional research to generate empirical evidence challenging the existing stigma and discrimination against PwDs, as well as advocating for disaggregated data due to the heterogeneity among PwDs.
"I don’t know how many people have conducted research on sexual and reproductive health among persons with disability in Ghana or somewhere else... delve more into SRH of PwDs in Ghana to help improve their reproductive health and health in general". [Nurse, Kumasi, Female, 46 years]
“Researchers should not sit at one place and do the research; they should go to the field because when you sit somewhere, you will not get the real information. When they are taking the data, it should be disaggregated by the various categories of disability and sub-groups because our needs are different”. [Visually Impaired, Kumasi, Female, 45 years]
Theme 4: impactful continuous monitoring and evaluation
Another recommendation from stakeholders was the need for continuous quality improvement. Specifically, participants indicated the need for monitoring and evaluation of existing policies and interventions. Participants also discussed the need to establish a system for tracking and assessing the performance of certain interventions, such as the national health insurance scheme, particularly in terms of improving access to quality SRH services for PwDs. Furthermore, participants shared that continuous monitoring and evaluation would lead to accountability and efficiency in healthcare policy implementation. Other participants also discussed the need for policy modifications.
“It all boils down to the implementation. If the government really wants the policy to work, they will make sure that the people who are supposed to carry out the interventions will check them. For instance, if the government wants the disability common fund to be effective, it is about the evaluation. He should check and demand reports from the various district giving them vivid reports …meaning the government is in control but if people spend the money and nothing is done to them then it means the government is not doing much. So, the monitoring, the officials must be checked and to give a good report about the various policies and interventions”. [Visually Impaired, Kumasi, Male, 25 years]
“Monitoring is also important because interventions like the national health insurance scheme have been problematic because of the paper system. You have to send a lot of papers to different people. This sometimes lead to loss of critical data for planning. But the computerization of the system will make services much effective because it becomes very easy to monitor and evaluate the system”. [Midwife, Offinso, Female, 34 years]
Other participants discussed the need to modify some of the existing policies and interventions, specifically the national health insurance scheme.
“… That would be terrific. As PwDs we have serious challenges with our finances. And so, having a special health insurance for PwDs is a brilliant way for us to get access to healthcare. We only wish that research and data collected about PwDs and their experiences would be taken into consideration in the development of policies and programs for us”. [Physically Disabled, Offinso, Female, 33 years]
“There should be a reproductive health policy targeting PwDs in that hospitals would be able to establish some unit or under the public health unit singularly for them, but the current policy is not benefiting them although access to health services has improved over time with NHIS policy, its making health affordable for them. Even though there are existing reproductive policies in Ghana, I think that there must be one for people with disability and must be institutionalized”. [Nurse, Male, Kumasi, 33 years]
Theme 5: vital empowerment for self-reliance
Another important recommendation was the need for vital empowerment for PwDs to ensure self-reliance. Various support mechanisms were suggested by both PwDs and HPs. These include economic empowerment and support programs. Specifically, participants suggested the need for job opportunities and skills development, and business support, strengthening disability organizations and support from non-governmental organisations (NGOs), providing assistive devices, and delivering free SRH services to PwDs. Participants discussed that most PwDs are not economically sound due to their inability to work, hence the need for job creation and skills development for PwDs. Some HPs also indicated that they need more economic support to provide SRH services to PwDs.
“The thing is that most PwDs do not work as such, they are poor. Therefore, if you really want to make an impact and get us to use SRH services, then we have to be helped to get work to do. That will make us economically self-reliant, and we will be able to use these SRH services any time that we want. Most people go about begging because they don’t have any work to do. In such instances, the SRH needs are not really important to them”. [Physically Disabled, Offinso, Male, 35years]
“But I think if they have that particular support from the government in the district [common fund], they can take part of it to also focus on reproductive health of people with disability. We need more money to do more, a classical example is someone we have identified as vulnerable; the vulnerability sometimes comes in economic sense. If, the person is able to go and come or have something in their hands [economically independent], they are least expected to be abused or sexually assaulted, so if we have more funds and more resources then we can train some of these people and set them up adequately”. [NGO official–Nurse, Kumasi, Male, 30 years]
It was also discussed that to ensure PwDs’ grievances are heard then it is prudent to strengthen disability organisations to adequately lobby for them. Participants discussed the need for the government to actively support and empower organizations representing PwDs to effectively advocate for their rights and needs.
“These groups are there but their voices are not heard so if the government can provide them like we have the federation and the government will allow us to express ourselves through the leadership of these groups so that it will not be that we are only talking and no one is listening so the government must also help strengthen our groups so that when we speak, it will not be like it is just noise. So if the government will be committed, it will help strengthen these institutions or leadership of these groups”. [Visually Impaired, Kumasi, Male, 25 years]
“I am not sure of the objectives of forming the disability organisations but I think that, maybe it is there to support them. It is there to hear their plea, it’s there to show some the way and all that, so if the groups are supposed to be working then if they want funding, they should be given the requisite funding to effectively carry out their mandate as head of organization or as some organization supporting their members, if they need funds, they should be given and it should be adequate”. [NGO official–Nurse, Kumasi, Male, 30 years]
Theme 6: enforcement of physical accessibility
All stakeholders emphasised that the majority of healthcare facilities lack accessibility for PwDs, underscoring the need to draw increased attention to these facilities and make them disability-friendly. While most PwDs highlighted challenges related to the physical infrastructure, HPs also stressed the necessity of ensuring that all services and equipment are tailored to accommodate the needs of PwDs. The unanimous recommendation, therefore, was to enhance the disability-friendliness of healthcare facilities through renovations or strict adherence to the guidelines outlined in the Disability Act 715 [17], which mandates accessible infrastructure for PwDs in public spaces and facilities. Such disability-friendly public spaces should encompass the installation of ramps, spacious restroom facilities, and the provision of adequate space within providers' offices to accommodate wheelchair users.
“In terms of delivery of SRH services, a health facility which will be conducive for persons with disabilities must also be considered. So, accessing sexual and reproductive health will help me to know which health facility is accessible for me when I am in that condition. In 2006, we passed the Disability Act. New public or health facilities have been coming up and still, they are not accessible so we are still advocating that hospitals should be disability-friendly”. [Visually Impaired, Kumasi, Female, 45 years]
“When they are building hospitals, I think it’s the last thing on their mind. There’s nothing for persons with disabilities. Even where the wheelchair will pass, there's nothing like that in most facilities so I think all these factors should be included. Our big men up there or the government have to make sure that whenever they are establishing any of these health facilities, they should make sure that people with disabilities are part of whatever they are planning, whatever they are programming so that it makes it easier for them because if the person comes and the person is not comfortable, or the person finds it difficult to access, they won’t even come back again”. [Doctor, Kumasi, Female, 32 years]
Discussion
This qualitative study employed a pluralistic approach to explore stakeholders’ recommendations on strategies to improve SRH access and outcomes among PwDs in Ghana. The stakeholders suggested several multipronged measures. These included Training for disability-sensitive and inclusive healthcare, Healthcare inclusivity – ‘nothing about us, without us’, Raising awareness for accessibility and equity, Impactful continuous monitoring and evaluation, Vital empowerment for self-reliance and Enforcement of physical accessibility to improve their SRH outcomes. These recommendations are synthesised to develop a conceptual model called THRIVE. The synthesis of the model components against previous evidence is discussed in the subsequent sections below.
Training for disability- sensitive and inclusive healthcare
Both PwDs and HPs shared the need to provide more education on disability-related issues to HPs. Previous studies in the USA [25], Zimbabwe [44], Senegal [45], Uganda [26], Guatemala [46], Ghana [24], and scoping reviews [6, 47] have emphasised the need to ensure that HPs are well-trained to care for PwDs. Several participants expressed their opinions on integrating education and training through formal or informal methods into both existing and new programs. They deliberated on targeted strategies to improve HPs knowledge and training. These strategies included sign language training and intensification, workshops, refresher courses and integrating disability training into healthcare curricula. Some participants also emphasised the need to train PwDs as HPs to ensure that they are also part of the care delivery systems [24, 44, 46–50].The findings, therefore, imply the need to institute mandatory training for HPs on disability-related issues and the intensification and strengthening of sign language instruction in various health training institutions [24, 44, 47–50]. Furthermore, there could be refresher training at various intervals, such as quarterly training. Also, as argued by Dassah et al. [24] basic training on disability issues could be a core criterion to fulfill before appointments or promotions are granted to HPs.
Healthcare inclusivity – ‘nothing about us, without us’
Previous studies in Ghana have shown that there is a low level of inclusiveness of PwDs in SRH policies [43, 51]. In this current study, both PwDs and HPs strongly advocated for the development of more inclusive SRH policies and interventions that meet the unique needs of PwDs. This reiterates the "nothing about us, without us" framework of disability organisations [52]. The reference to this document encapsulates a fundamental principle in disability rights advocacy. It emphasises that policies should not be developed for PwDs without their active participation and input. Inclusion in the policymaking process allows PwDs to provide valuable insights and ensure that policies align with their real-world experiences. Other PwDs also argued that even if it is impossible to include everyone in the policy formulation process, it is critical to include their leaders, such as the Ghana Blind Union, the Federation of the Disabled and National Council of Disability to facilitate inclusive policymaking. This approach recognises the diversity within the disability community and the importance of engaging with different groups to capture a wide range of perspectives. In addition to this, the universal health coverage agenda of the SDGs also strongly advocates for leaving no one behind. Previous studies [26, 44, 53, 24] have also argued for the inclusion of PwDs in policies and interventions aimed at improving their SRH. Similar findings have also been reported by Dassah et al in Ghana [24].
Raising awareness for accessibility and equity
One of the main recommendations the participants shared was the need to educate PwDs and community members via appropriate channels, including radio and community engagements, to reduce stigma and discrimination associated with disability. In addition, participants discussed the need to conduct more studies with PwDs and provide disability-disaggregated data for evidence-based practice and policy implementation. Awareness creation about the importance of accessing SRH services among PwDs was also discussed. Previous studies have reported similar ways to ensure appropriate SRH care and service delivery to PwDs [44, 45, 53]. The need to educate community members about disability reinforces the pervasiveness of stigma against PwDs, which subsequently impacts PwDs’ use of SRH services. Therefore, if more awareness is created and stigma is reduced, it could motivate PwDs to use SRH services, ultimately improving their SRH outcomes [44, 53].
Impactful continuous monitoring and evaluation
Another important narrative the participants shared was the need for continuous quality improvement. Specifically, participants emphasised the importance of monitoring and evaluating implemented policies and programs to ensure that they are fit for purpose. Some participants specifically highlighted the need to ensure that tailored policies meeting the needs of PwDs are implemented. Others also argued for the need to implement special policies regarding the health accessibility of PwDs. In addition, the participants discussed that when the implemented policies and programs, such as the NHIS, are continuously evaluated, they will provide evidence of whether indeed PwDs are benefiting from them or not. These findings are consistent with previous studies in the USA [25] and Uganda [26, 54]. Torsha et al. [55] and WHO report on health equity for PwDs [1] argued that a structured monitoring and evaluation system should be in place to assess whether PwDs are benefiting from health policies and interventions, and this should be done by a competent authority. These views emphasise that monitoring and evaluation are essential tools to gauge the success and effectiveness of healthcare initiatives, including those aimed at benefiting PwDs. It also implies that through this, accountability and evidence-based decision-making in healthcare policy development, healthcare areas needing improvement and optimal resource allocation can help improve the SRH outcomes of PwDs.
Vital empowerment for self-reliance
One of the primary recommendations discussed by participants pertained to support for PwDs, encompassing both formal and informal assistance to improve self-reliance. Formal support includes economic aid, the provision of free SRH services, distribution of assistive devices, opportunities for skill development, and the reinforcement of disability organisations [44]. The role of NGOs in enhancing PwDs’ access to SRH services was also discussed. Harvey [53] proposed that to ensure adequate provision of SRH services for PwDs, collaboration is essential. Policies should consider cost reduction and/or the provision of financial assistance to individuals with disabilities for SRH and transportation. Enhanced cooperation between the health, finance, education, and infrastructure sectors in LMICs is warranted.
According to the WHO and World Bank [56], approximately 50% of individuals with disabilities lack the financial means to access healthcare, rendering them 50% more susceptible to severe health-related financial burdens arising from both direct and indirect healthcare costs. Given these findings, the achievement of SDG three may face significant challenges if PwDs continue to be underserved [41, 57]. Therefore, the recommendation to provide financial support to PwDs represents a positive step forward. This underscores the importance of effectively implementing and strengthening existing interventions in Ghana, such as the Disability Common Fund and the NHIS [52].
Enforcement of physical accessibility
Another major recommendation the participants shared was the need to enforce physical access to infrastructure and services. This aligns with previous studies [6, 24] in many LMICs that call for the provision of disability-friendly infrastructure and services to improve SRH health accessibility and care. For example, previous studies have found that PwDs experience various infrastructural barriers in their quest to access SRH services in Ghana [8, 21, 22] and other parts of the world [6, 58]. PwDs sometimes navigate these barriers through assistance from caregivers, which sometimes leads to a breach in confidentiality when accessing SRH services [21]. This calls for an urgent need to ensure that health facilities and SRH services, in general, are accessible to various categories of PwDs. The finding on the need for disability-friendly healthcare facilities reiterates the importance of ensuring that the provisions of Disability Act 715 regarding accessible buildings are strictly implemented [24]. Furthermore, it would be prudent to conduct a nationwide study in major healthcare facilities to assess the extent of health infrastructural friendliness to PwDs. Based on this, a costed action plan or implementation plan can be developed to determine the resources required to address this issue. Disability-friendly health facility principles can then be developed and publicly displayed in relevant areas within every hospital [58].
Implications for policy and practice
The THRIVE model, developed from this study, serves as a blueprint for enhancing the delivery and accessibility of SRH services for PwDs. Its implementation could potentially lead to improved SRH outcomes for PwDs. The findings highlight a notable disparity between stakeholders’ experiences and the provisions outlined in various policy documents aimed at supporting SRH access for PwDs in Ghana. Consequently, these findings offer valuable insights for the development, monitoring, and revision of existing policies and interventions aimed at enhancing the SRH of PwDs. For instance, while Disability Act 715 contains provisions related to medical treatment, healthcare professional training, and access to public places and services [17], these provisions have not been effectively translated into practice. In addition, the NHIS has also been ineffective to adequately take off the financial burden and out of pockets payment related to health cost. Both HPs and PwDs emphasised the importance of disability-friendly health facilities and services. Further research that incorporates the perspectives of policymakers is recommended to address these discrepancies.
Strength and limitations
The major strengths of this study include the utilisation of a pluralistic approach [30, 31] and a qualitative study design to facilitate a comprehensive exploration of both service users’ and providers’ perspectives, offering valuable insights. The synthesis of the study findings [28] to develop the THRIVE model is also a key strength of the study. However, it should be noted that the study did not incorporate the viewpoints of policymakers. Additionally, it is important to recognise that social desirability biases may have influenced the expressed views in the study. Furthermore, the study was conducted exclusively in two settings in the Ashanti region of Ghana, warranting caution when considering the transferability of the study findings to other settings. Some of the interviews were conducted in Twi, hence the need to translate them to English. It is possible that some of the meanings might have been lost during the translation process [33].
Conclusion
Employing a pluralistic approach, this study explored the perceptions of HPs and PwDs regarding the strategies to improve SRH outcomes of PwDs. These perspectives led to the development of the THRIVE model–a comprehensive framework that emphasises the importance of factors such as Training for disability-sensitive and inclusive healthcare, Healthcare inclusivity – ‘nothing about us, without us’, Raising awareness for accessibility and equity, Impactful continuous monitoring and evaluation, Vital empowerment for self-reliance and Enforcement of physical accessibility to improve their SRH outcomes. Using the evidence based THRIVE model could facilitate the development and strengthening of existing interventions and policies including the disability Act 715 to improve the SRH access and outcomes of PwDs in Ghana and other LMICs.
Supplementary Information
Acknowledgements
We acknowledge the study participants for their participation in the study. We also appreciate the research assistants' contribution to the data collection. We would also like to acknowledge JCU for PhD research scholarship for the first author–Abdul-Aziz Seidu.
Abbreviations
- COREQ
Consolidated criteria for reporting qualitative research
- GHS
Ghana Health Service
- GSS
Ghana Statistical Service
- JCU
James Cook University
- KATH
Komfo Anokye Teaching Hospital
- NHIS
National Health Insurance Scheme
- PwDs
Persons with disabilities
- RAs
Research Assistants
- SRH
Sexual and reproductive health
- UN
United Nations
- HPs
Healthcare providers
- WHO
World Health Organization
Authors’ contributions
Conceptualisation: A.S., B.S.M.-A., K.M.-R., A.E.O.M.-A. and T.I.E.; writing—original draft preparation, A.S.; writing—review and editing, A.S., B.S.M.-A., K.M.-R., A.E.O.M.-A. and T.I.E.; supervision, B.S.M.-A., K.M.-R., A.E.O.M.-A. and T.I.E.; funding acquisition, A.S and T.I.E. All authors approved it for publication. All authors have read and agreed to the published version of the manuscript.
Funding
The study did not receive any funding.
Availability of data and materials
The dataset is available upon reasonable request from the corresponding authors (A.S and T.I.E).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from three institutional review committees: the Ghana Health Service (GHS) Ethics Review Committee (GHS-ERC: 005–0621), the Komfo Anokye Teaching Hospital (KATH) (KATH-IRB/RR/101/21), and the James Cook University (JCU) Human Ethics Committee (H8531). The study also received approval from the Regional Health Directorate in Kumasi and the Offinso North District Health Directorate in Akumadan, as well as from the heads of two disability organisations in these districts. Furthermore, the study ensured the anonymity and confidentiality of the participants. Prior to administering the study instrument, a document explaining the study objectives, anonymity and confidentiality, and benefits of participation was provided to the participants. They were also informed that their involvement was voluntary and that they could withdraw from the project at any time devoid any repercussions. They were also assured that their data would be used only for academic purposes and that their identities would not be disclosed to anyone. Both written and verbal informed consents were obtained from all participants. The investigations were performed according to Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abdul-Aziz Seidu, Email: abdulaziz.seidu@jcu.edu.au.
Theophilus I. Emeto, Email: theophilus.emeto@jcu.edu.au
References
- 1.WHO. Global report on health equity for persons with disabilities. Geneva: WHO; 2022. p. 1–312. [Google Scholar]
- 2.Banks LM, Kuper H, Polack S. Poverty and disability in low-and middle-income countries: a systematic review. PLoS ONE. 2017;12(12):e0189996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bright T, Kuper H. A systematic review of access to general healthcare services for people with disabilities in low and middle income countries. Int J Environ Res Public Health. 2018;15(9):1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low-and middle-income countries. Int J Environ Res Public Health. 2018;15(10):2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Bank. Disability inclusion. World Bank; 2018. https://www.worldbank.org/en/topic/disability. Accessed 20 Oct 2023.
- 6.Nguyen A. Challenges for women with disabilities accessing reproductive health care around the world: a scoping review. Sex Disabil. 2020;38(3):371–88. [Google Scholar]
- 7.World Health Organization. International classification of functioning, disability and health. Geneva: WHO; 2001.
- 8.Badu E, et al. Enablers and barriers in accessing sexual and reproductive health services among visually impaired women in the Ashanti and Brong Ahafo regions of Ghana. Reprod Health Matters. 2018;26(54):51–60. [DOI] [PubMed] [Google Scholar]
- 9.Mailhot AA, et al. Sexual violence against persons with disabilities: a meta-analysis. Trauma Violence Abuse. 2022;23(4):1330–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tenaw Z, Gari T, Gebretsadik A. Sexual violence and associated factors among reproductive-age females with disabilities in central Sidama National Regional State, Ethiopia: a multilevel analysis. BMC Womens Health. 2023;23(1):353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tenaw Z, Gari T, Gebretsadik A. Unintended pregnancy and its associated factors among women with disabilities in central Sidama National Regional State, Ethiopia: a multilevel analysis. BMC Pregnancy Childbirth. 2023;23(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parekh T, Gimm G, Kitsantas P. Sexually transmitted infections in women of reproductive age by disability type. Am J Prev Med. 2023;64(3):393–404. [DOI] [PubMed] [Google Scholar]
- 13.Dassah E, et al. ‘When I don’t have money to buy the drugs, I just manage’.—Exploring the lived experience of persons with physical disabilities in accessing primary health care services in rural Ghana. Soc Sci Med. 2018;214:83–90. [DOI] [PubMed] [Google Scholar]
- 14.Tomlinson M, et al. Research priorities for health of people with disabilities: an expert opinion exercise. Lancet. 2009;374(9704):1857–62. [DOI] [PubMed] [Google Scholar]
- 15.UN. Convention on the rights of persons with disabilities. New York: United Nations; 2006. [DOI] [PubMed] [Google Scholar]
- 16.UN, Transforming our world: The 2030 agenda for sustainable development. New York: United Nations; 2015. [Google Scholar]
- 17.Republic of Ghana. Disability Act 715, Ghana. Accra: Ghana Publishing Press; 2006.
- 18.Badu E, et al. Financial access to healthcare among persons with disabilities in the Kumasi Metropolis, Ghana. Disabil CBR Inclusive Dev. 2015;26(2):47–68.
- 19.Badu E, Opoku MP, Appiah SC. Attitudes of health service providers: The perspective of people with disabilities in the Kumasi Metropolis of Ghana. Afr J Disab. 2016;5(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dassah E, et al. Healthcare providers’ perspectives of providing primary healthcare services to persons with physical disabilities in rural Ghana. Prim Health Care Res Develop. 2019;20:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seidu AA, et al. “God is my only health insurance”: a mixed-methods study on the experiences of persons with disability in accessing sexual and reproductive health services in Ghana. Front Public Health. 2023;11:1232046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seidu A-A, et al. “Sex Should Not Be Part of the Lives of Persons with Disabilities, but They Are Human Beings Too”: Perceptions of Healthcare Providers and Factors Affecting Service Delivery in Ghana. Healthcare. 2023;11(7):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Badu E, et al. Knowledge and sources of accessing sexual and reproductive health information among visually impaired women in Ghana. BMC Res Notes. 2019;12(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dassah E, et al. Health care providers’ and persons with disabilities’ recommendations for improving access to primary health care services in rural northern Ghana: A qualitative study. PLoS ONE. 2022;17(9):e0274163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McClintock HF, et al. Health care access and quality for persons with disability: Patient and provider recommendations. Disabil Health J. 2018;11(3):382–9. [DOI] [PubMed] [Google Scholar]
- 26.Mac-Seing M, et al. The intersectional jeopardy of disability, gender and sexual and reproductive health: experiences and recommendations of women and men with disabilities in Northern Uganda. Sex Reprod Health atters. 2020;28(2): 1772654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheikh K, George A, Gilson L. People-centred science: strengthening the practice of health policy and systems research. Health Res Policy Syst. 2014;12(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1(3):385–405. [Google Scholar]
- 29.Bradshaw C, Atkinson S, Doody O. Employing a qualitative description approach in health care research. Glob Qual Nurs Res. 2017;4:2333393617742282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hall JE. Pluralistic evaluation: a situational approach to service evaluation. J Nurs Manag. 2004;12(1):22–7. [DOI] [PubMed] [Google Scholar]
- 31.Hart E. The use of pluralistic evaluation to explore people’s experiences of stroke services in the community. Health Soc Care Community. 1999;7(4):248–56. [DOI] [PubMed] [Google Scholar]
- 32.Saunders B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Squires A. Methodological challenges in cross-language qualitative research: a research review. Int J Nurs Stud. 2009;46(2):277–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 35.Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18(3):328–52. [Google Scholar]
- 36.Morgan DL. Themes, theories, and models. Qual Health Res. 2018;28(3):339–45. [DOI] [PubMed] [Google Scholar]
- 37.Tolley EE, et al. Qualitative methods in public health: a field guide for applied research. John Wiley & Sons; 2016.
- 38.Börner K, et al. An introduction to modeling science: Basic model types, key definitions, and a general framework for the comparison of process models. In: Models of science dynamics: Encounters between complexity theory and information sciences. Springer; 2011. p. 3–22.
- 39.Rashid HS. A theoretical model of industrial accidents investigations: a conceptualization of the mental processes that trigger and control investigative activities. Theor Issu Ergon Sci. 2023;25(5):1–25.
- 40.Imenda S. Is there a conceptual difference between theoretical and conceptual frameworks? J Soc Sci. 2014;38(2):185–95. [Google Scholar]
- 41.Hashemi G, et al. How do people with disabilities in three regions of Guatemala make healthcare decisions? A qualitative study focusing on use of primary healthcare services. PLOS Glob Public Health. 2023;3(2): e0000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mprah WK, Anafi P, Sekyere FO. Does disability matter? Disability in sexual and reproductive health policies and research in Ghana. Int Q Community Health Educ. 2014;35(1):21–35. [DOI] [PubMed] [Google Scholar]
- 43.Seidu A-A, et al. Level of inclusiveness of people with disabilities in Ghanaian health policies and reports: a scoping review. Disabilities. 2021;1(3):257–77. [Google Scholar]
- 44.Rugoho T, et al. NGOs and the Promotion of the sexual and reproductive rights of girls and young women with disabilities in Zimbabwe. Soc Policy Soc. 2023;1–13. 10.1017/S1474746422000641.
- 45.Soule O, Sonko D. Examining access to sexual and reproductive health services and information for young women with disabilities in Senegal: a qualitative study. Sex Reprod Health Matters. 2022;30(1): 2105965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hashemi G, et al. Healthcare stakeholders’ perspectives on challenges in the provision of quality primary healthcare for people with disabilities in three regions of guatemala: a qualitative study. Int J Environ Res Public Health. 2023;20(19):6896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rotenberg S, et al. Disability training for health workers: a global evidence synthesis. Disabil Health J. 2022;15(2):101260. [DOI] [PubMed] [Google Scholar]
- 48.Havercamp SM, et al. What should we teach about disability? National consensus on disability competencies for health care education. Disabil Health J. 2021;14(2):100989. [DOI] [PubMed] [Google Scholar]
- 49.Rugoho T, Maphosa F. Challenges faced by women with disabilities in accessing sexual and reproductive health in Zimbabwe: the case of Chitungwiza town. Afr J Disab. 2017;6(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shakespeare T, Kleine I. Educating health professionals about disability: a review of interventions. Health Soc Care Educ. 2013;2(2):20–37. [Google Scholar]
- 51.Kwadwo W, Anafi P, Sekyere FO. Does disability matter? Disability in sexual and reproductive health policies and research in Ghana. Int Q Community Health Educ. 2014;35(1):21–35. [DOI] [PubMed] [Google Scholar]
- 52.Opoku MP, Nketsia W. ‘Nothing about us, without us’: Voices of leaders of disabled people’s organisation in management of disability fund. Soc Sci Human Open. 2021;4(1): 100160. [Google Scholar]
- 53.Clare Harvey. Evidence Brief: How is the sexual health of men and women with physical disabilities in low- and middle- income countries promoted? Disability Evidence Portal. 2021. 10.13140/RG.2.2.26387.35363.
- 54.Mac-Seing M, et al. Policy implementation challenges and barriers to access sexual and reproductive health services faced by people with disabilities: an intersectional analysis of policy actors’ perspectives in post-conflict Northern Uganda. Int J Health Policy Manag. 2022;11(7):1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Torsha N, et al. Disability-friendly healthcare at public health facilities in Bangladesh: a mixed-method study to explore the existing situation. BMC Health Serv Res. 2022;22(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.WHO and World Bank. World report on disability. Geneva: WHO; 2011. p. 1–350. [Google Scholar]
- 57.Hashemi G, Kuper H, Wickenden M. SDGs, Inclusive health and the path to universal health coverage disability and the global south. Disab Glob South. 2017;4(1):1088–111. [Google Scholar]
- 58.Ganle JK, et al. Barriers facing persons with disability in accessing sexual and reproductive health services in sub-Saharan Africa: a systematic review. PLoS ONE. 2020;15(10): e0238585. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset is available upon reasonable request from the corresponding authors (A.S and T.I.E).
No datasets were generated or analysed during the current study.