Abstract
Background:
Symptoms of emotional and physical stress near death may be related to previous experiences of trauma.
Objective:
To investigate current evidence regarding the following: (1) Is previous trauma identified in people who are dying, and if so, how? (2) How is previous trauma associated with the experience of death/dying in people with or without cognitive impairment? and (3) What palliative care interventions are available to people with previous trauma at the end of life?
Design:
This integrative review was conducted per Whittemore and Knafl’s guidelines, which involves a stepped approach, specifically (1) problem identification, (2) literature search, (3) data evaluation, (4) data analysis and (5) presentation.
Methods:
This integrative review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. Electronic databases were searched in August 2021 and updated in August 2023. The articles were quality appraised, and narrative data were analysed using Grounded Theory (GT).
Results:
Of 1310 studies screened, 11 met the inclusion criteria (four qualitative and seven quantitative) conducted in Australia, Canada, Japan and the United States; and American studies accounted for 7/11 studies. Eight were focused on war veterans. Descriptive studies accounted for the majority, with only two publications testing interventions. Re-living trauma near death has additional features to a diagnosis of post-traumatic stress disorder alone, such as physical symptoms of uncontrolled, unexplained acute pain and this distress was reported in the last weeks of life.
Conclusion:
This study proposes that re-living trauma near death is a recognisable phenomenon with physical and psychological impacts that can be ameliorated with improved clinical knowledge and appropriate management as a new GT. Further research is needed to enable past trauma identification at the end of life, and trauma-informed safe interventions at the end of life are an urgent need.
Keywords: end-of-life care, identifying past trauma, increased suffering, trauma, trauma-informed palliative care
Introduction
Most people have experienced traumas across their life course, but little is known about how this may affect their experience of dying. Trauma is a psychological response to an incident or series of incidents or set of conditions that are experienced by an individual as physically or emotionally harmful or life-threatening. 1 Experiencing trauma has the potential to cause long-lasting adverse effects on the person’s functioning including mental, physical, social, emotional and spiritual well-being. 1 Causative events may include conflicts and exposure to violence, sexual violence, Adverse Childhood Experiences (ACE), fires, floods and earthquakes.1,2 In a collective summary of WHO World Mental Health Surveys in 24 countries, 70% of respondents reported experiencing trauma, with an average of 3.2 experiences per person. 3 Trauma-informed health care has developed in response to the need to provide safe access to care for trauma survivors that do not re-traumatise them.4–6
Meyerson et al. and Ganzel highlight that it is essential to be aware of the impact that trauma can have on the dying experience as trauma experiences are common and are part of the personal biographies of many people receiving palliative care.4,5 To date, trauma-informed care is not usual practice in palliative care delivery.4,5,7 Dying patients may live and die with increased chronic pain and suffering and may be re-traumatised at the end of life.4,5,8 Early palliative care has been shown to improve quality of life and mood significantly, 9 be associated with less aggressive care at the end of life and increased survival. 9 Currently, there is a gap in knowledge in providing trauma-informed palliative care,4,5,10 and in part, this may be due to a lack of recognition and understanding of dying patients with known or unknown past trauma, including those with previous post-traumatic stress disorder (PTSD).
The experience of trauma during the lifespan can progress to PTSD, a psychological disorder that occurs post-trauma. 2 PTSD can present in the following ways: intrusive symptoms, persistent avoidance, negative changes to cognition and mood, and hyperarousal/hypervigilance.1,2 Life stressors like physical and cognitive decline in older adults can result in PTSD relapse or worsening symptoms, including subjective re-experiencing of trauma.11,12 In other cases, people can experience delayed onset of PTSD and have symptoms for the first time in later life.12,13 Past trauma is also known to be missed or misinterpreted at the end of life, particularly when people are dying with cognitive impairment, delirium, dementia, pain and anxiety.4,5,14,15 Symptoms can represent first-time emergence and re-emergent experiences of trauma.5,7,12,13
Most people who experience trauma do not develop PTSD; pooled global estimates of the lifetime prevalence of PTSD are around 3.6% with a significant inter-country variation. 3 Prevalence rates of PTSD are significantly higher in conflict-affected populations. Pooled estimates in meta-analyses of conflicted-affected populations have been found to range from 15.3% to 30.6%.11,16 Trauma involving interpersonal violence, particularly sexual violence, is highly associated with PTSD development. 2
Trauma exposure adversely and disproportionally affects vulnerable members of society, including women and girls, ethnic minorities, Indigenous peoples, socioeconomically disadvantaged people and those living in areas of conflict.1,2,16,17 Women have twice the lifetime risk of developing PTSD than males, as they have a higher incidence of being victims of violence, sexual abuse and rape. 2 Trauma also has a heightened impact on children with exposure to traumatic events in childhood increasing the lifelong impacts of that and any subsequent trauma. 2 Trauma survivors often live with chronic pain, have a more significant number of medical diagnoses and report more physical and emotional ill-health than those who have not experienced trauma.8,18,19 Despite the commonality of trauma experiences, diagnosing PTSD can be complex when past trauma has not been disclosed or indeed identified. 2
A better understanding of end-of-life experiences for trauma survivors is needed, whether they have been diagnosed with PTSD, have had a history of PTSD or have had no known PTSD diagnosis.4,7,20 Improving our understanding of current experiences and practice is necessary to develop patient-centred trauma-informed care. This end-of-life care needs to be suitable for those diagnosed with PTSD, those undiagnosed who have symptoms of PTSD and those with first-time emergent or re-emergent experiences of trauma.5,7,12,13
Methods
Aim
This integrative review addressed the following research questions: (1) Is previous trauma identified in people who are dying, and if so, how? (2) How is previous trauma associated with the experience of death/dying in people with or without cognitive impairment? and (3) What palliative care interventions are available to people with previous trauma at the end of life?
Design
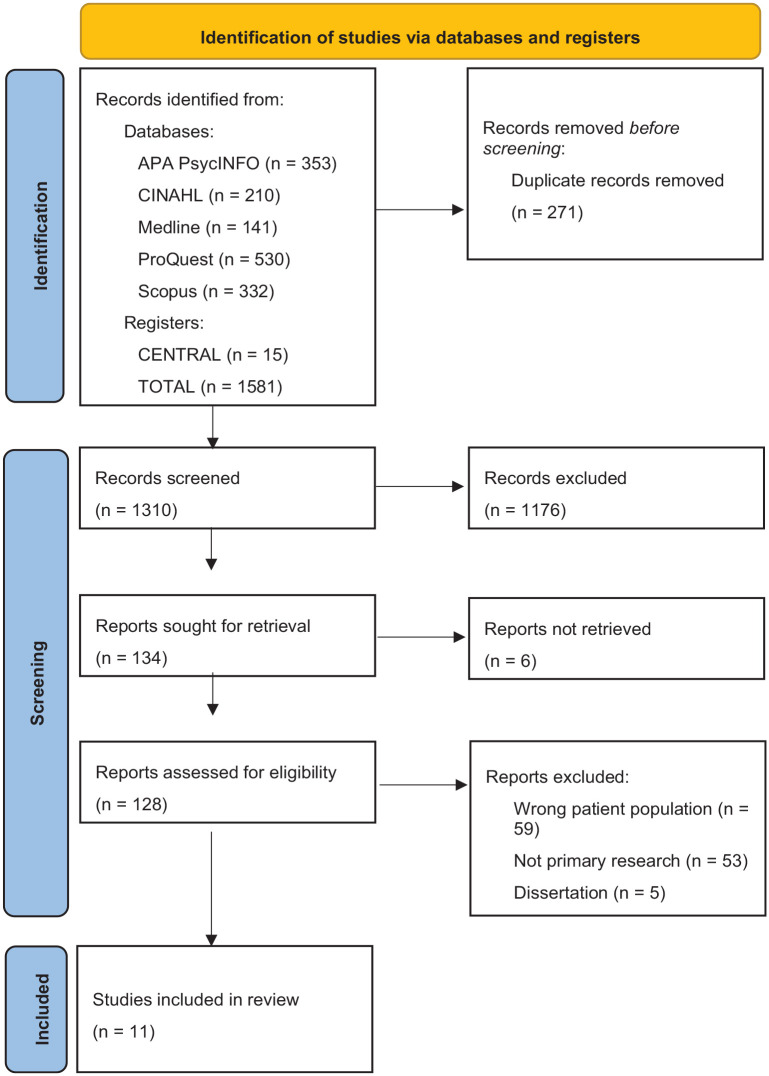
This integrative review was conducted in accordance with Whittemore and Knafl’s guidelines, 21 which involves a stepped approach specifically (1) problem identification, (2) literature search, (3) data evaluation, (4) data analysis and (5) presentation. 21 A convergent integrative review was appropriate as the outcome measures of the included studies were heterogeneous and included qualitative, quantitative and mixed-methods research studies. 21 A convergent integrated approach critically synthesises all extracted data from quantitative and qualitative studies. 21 For quantitative studies, this involved qualitising the quantitative data to be used in the narrative interpretation.7,22 The review protocol was registered with PROSPERO CRD42021225037 and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Figure 1). 23
Figure 1.
Search outcomes PRISMA. 23
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Definition of PTSD
PTSD was the term used to describe trauma responses in most papers. Although some of the papers were conducted using earlier Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 2 diagnostic criteria, all share the elements of trauma exposure, hyper-regulation, avoidance, mood disturbance and functional impact. Studies were included if they defined PTSD using DSM-IV and DSM-5 Criteria, 2 see Table 1.
Table 1.
Diagnostic and Statistical Manual of Mental Disorders-5 criteria. 7 .
| Criterion | Description | Specific example |
|---|---|---|
| A | Exposure to stressor | Direct exposure, witnessing trauma, learning of a trauma, repeated or extreme indirect exposure to aversive details |
| B | Intrusive symptoms | Recurrent memories, traumatic nightmares, dissociative reactions (flashbacks), psychological distress at traumatic reminders and marked physiological reactivity to reminders |
| C | Persistent avoidance | Trauma-related thoughts or feelings, trauma-related external reminders such as people, places or activities |
| D | Negative alterations in cognition and mood | Dissociative amnesia, persistent negative beliefs and expectations, persistent distorted blame of self or others for causing trauma, negative trauma-related emotions: fear, horror, guilt, shame and anger. Diminished interest in activities, detachment and estrangement from others, inability to experience positive emotions |
| E | Alterations in arousal and reactivity | Irritability and aggressive behaviour, self-destructive and reckless behaviour, hypervigilance, exaggerated startle, problems concentrating, sleep disturbances |
| F | Duration | Must experience criteria B, C, D and F for more than a month |
| G | Functional significance | Impairment in social, occupational or other domains |
| H | Exclusion | Not attributed to medication, substance use or other illness |
Search methods
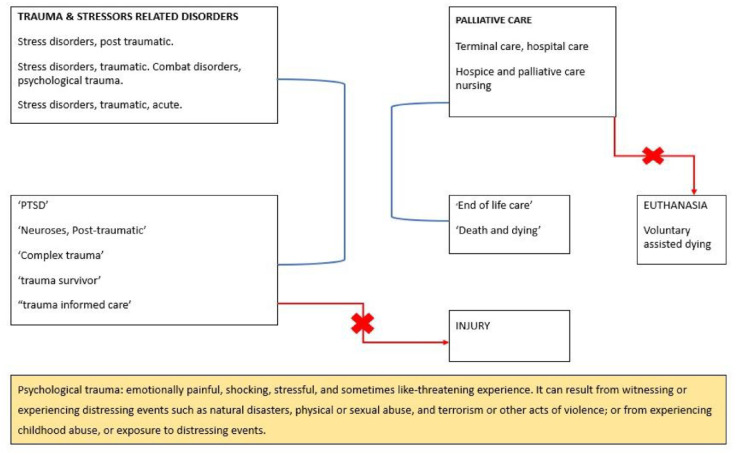
Five electronic databases (APA PsycINFO, CINAHL, Medline, ProQuest and Scopus) and the Cochrane trial register, CENTRAL, were last searched in August 2023 using keywords and subject headings to capture the concepts of trauma- and stressor-related disorders, palliative care and dying. The search strategy was inclusive of identifying all relevant studies over the preceding 20 years. An expert medical librarian developed the search strategy. See Supplemental Appendix 1 for the entire record of database searches. Following the search, all studies were imported into Covidence systematic review software for independent screening by the reviewers according to predetermined inclusion/exclusion criteria (Figure 2). 24 Four reviewers screened titles and abstracts, and four reviewers screened the full-text selected studies.
Figure 2.
Inclusion and exclusion criteria.
Data extraction
Data extracted from included studies comprised study aims, methods, samples and key findings, which are represented in the article matrix table (Table 2). 25
Table 2.
Article matrix table.
| Author and year, country, study design | Study aim | Methods | Participants/sample | Data collection | Key findings relevant to re-living trauma near death |
|---|---|---|---|---|---|
| Akechi et al. (2004), Japan, Quantitative | To determine the prevalence of ADs, MD and PTSD among terminally ill cancer patients. | Multivariate logistical regression analysis on the determinant of psychological distress: diagnosed with an AD, MD or PTSD. Factors include patient characteristics including age, sex, education, marital status, employment status, household size, living alone, cancer site, time since initial diagnosis, past cancer therapy, current medication and religion. |
A total of 209 cancer patients registered with the PCU participated in the baseline assessment. Of them, 85 participated in the follow-up study to assess longitudinal changes in performance status and physical symptoms. | Clinical interviews and questionnaires were utilised prospectively with consecutive cancer patients at two timepoints: (1) outpatient appointment visit after registration with PCU (baseline) and (2) follow-up 1 week post-admission to the inpatient PCU. | Results show lower performance status (proxy by patient’s Karnofsky score), concern about being a burden to others and lower satisfaction with social support were significantly associated with psychological distress at baseline. At follow-up, a higher Hospital Anxiety Depression Scale at baseline was a significant predictor for the subsequent presence of ADs and/or MD. Results suggested that factors underlying psychological distress at the end of life are multifactorial. However, none of the patients were identified to have PTSD. |
| Alici et al. (2010), USA, Quantitative | To define the frequency of PTSD-related symptoms near the end of life among veterans. To describe the impact of these symptoms on veterans and their family members. |
The FATE survey assessed their perceptions of the quality of the care of the deceased and what they received during the patient’s last month of life. Three symptoms were analysed in relation to the patient’s comfort (pain, dyspnoea), and PTSD-related symptoms (persistent re-experience of the traumatic event, persistent avoidance of the stimuli associated with the trauma and increased arousal as per DSM IV) in the last month of life. |
Family members of 524 deceased American veterans, who died in one of five veterans’ affairs medical centres and their affiliated nursing homes and clinics in the USA. | Participants were contacted by phone and were asked about demographics and then filled in a retrospective survey at least 6 weeks after the death of the veteran. | 17% (N = 89) of family members reported that the patient experienced PTSD-related symptoms in the last month of life. Of them, 28% ‘always’ experienced discomfort. And 71% (N = 63) had no previous PTSD diagnosis. Families were more likely to report PTSD-related symptoms if they had a previous diagnosis of PTSD, but they otherwise had similar characteristics to other patients in terms of age, gender, site of death and ethnicity. In the full sample, patients were more likely to experience pain (81%) and dyspnoea (77%) than PTSD-related symptoms, but families reported that PTSD-related symptoms made the patient more uncomfortable than dyspnoea, but not more uncomfortable than pain. Patients with pain or dyspnoea were more likely to experience PTSD-related symptoms. Families of patients dying with PTSD-related symptoms were more likely to report having unmet emotional needs than patients without PTSD-related symptoms. They were also more likely to report worse communication with providers in the patient’s last month of life, less attention to dignity and well-being, and overall less satisfaction with care received. |
| Bickel et al. 2019 USA Quantitative |
To determine whether veterans with PTSD have increased end-of-life healthcare utilisation or medication use and to examine predictors of medication administration. | Secondary analysis of data from a stepped-wedge RTC, design implementation trial to improve end-of-life care for VA inpatients. Outcome variables were collected via direct chart review. | 5341 dying Veterans with or without a diagnosis of PTSD across six VA facilities. | Data were collected when Veterans attended the Emergency room, hospitalisations and received medication administration in the last 7 days of life. | Of the 5341 veterans included in the analysis, 1946 (36.4%) had at least one psychiatric illness and 468 (8.76%) had a diagnosis of PTSD. Those with a diagnosis of PTSD had increased end-of-life care health utilisation and increased antipsychotic administration in the final days of life. This suggests veterans with PTSD have a greater symptom burden at the end of life and have the potential of increased risk of terminal delirium, hospitalisation and use of more medication at the end of life. Psychiatric co-morbidities were more prevalent for veterans with a diagnosis of PTSD. |
| Casarett et al. (2019), USA and Canada, Quantitative | To determine the relative contributions of THCs and CBD among patients’ self-ratings of efficacy for common palliative care symptoms. | This is an electronic record-based retrospective cohort study, where logistic regression with bootstrapped confidence intervals (CIs) with standard errors clustered to account for multiple observations by each patient. Analyses were conducted using a series of parametric and non-parametric tests. | Palliative care patients who were registered on the national Canadian patient portal with a total sample of 2431 patients. | Data were sourced from the Strainprint™ mobile app which is a medical outcomes tracker providing medical cannabis users a means of tracking changes in symptoms as a function of different doses and types of cannabis. | The use of THC was associated with marked improvement in symptoms including PTSD-related flashbacks. After adjusting for dose, age and gender, the odds of achieving at least three-point improvement in neuropathic pain, insomnia and depressive symptoms from an increasing THC concentration (measured by THC/CBD ratio) were 3.58 (95% CI: 1.33–9.68), 2.93 (95% CI: 1.75–4.91) and 1.63 (95% CI: 1.07–2.47), respectively. However, the corresponding odds for PTSD flashback (1.43) were not statistically significant at the 5% level (95% CI: 0.60–3.41). While THC fails to provide specific benefits in managing PTSD symptoms at the end of life, it can be used to improve symptoms of re-living trauma near death such as acute pain, depression and insomnia. |
| Feldman et al. (2013), USA, Qualitative | To explore the application of the SPPC model based on psychosocial palliative care philosophy using a case study. To provide concrete guidance to providers regarding the management of PTSD at the end of life in diverse palliative care settings. |
Three cases were examined in which the SPPC model was utilised. | Outpatient and SPC inpatient unit care settings within a medium-sized VA Medical that had a palliative care consultancy. Three patients in two distinct palliative care settings within a medium-sized Veteran Affairs Medical Centre. |
Three veteran case studies from admitted patients were used. | The SPPC model is an effective alternative therapeutic approach that focuses on the quality of life for veterans with PTSD at the end of life. There is clinical support for this using case examples; however, to date, research has not tested its efficacy or effectiveness. The paper highlighted that trauma survivors may have a distrust of medical providers. Staff can find it difficult when trauma survivors avoid palliative care treatments. Delirium, hallucinations and pain are common when PTSD is identified. Veterans who have survived trauma and had a cancer diagnosis can experience intense pain and unexplained pain at the end of life. They also experienced conflation of PTSD symptoms such as sleep disturbances, nightmares and intrusive thoughts about combat experiences. |
| Kaiser et al. (2021), USA, Qualitative | This project aimed to evaluate: - Do hospice and palliative care providers/staff observe PTSD symptoms in veterans at the end of life? - If so, how are symptoms like and different from existing DSM-5 criteria for PTSD? |
Content analysis was used on focus group data with a mixed deductive and inductive approach to coding anonymised data. | Hospice and palliative care clinicians caring for military veterans at the end of life N = 92. The data comprise nurses (42.4%), social workers (16.3%), chaplains (13.0%), physicians (4.3%), program directors/managers (often nurses by training) (18.5%), others (e.g. volunteer coordinator, volunteers (4.4%) and unknown (1.1%). | Data were collected through 10 focus groups of clinicians. Six open-ended questions about trauma and PTSD using a traditional focus group format. General questions followed by specific prompts. | 92 clinicians reported on their experiences of veterans with PTSD and described that veterans with PTSD had Increased symptom burden at the end of life. Different trauma exposures led to different symptom intensities. The example found in this article; Vietnam-era veterans had increased suffering at the end of life when compared to other war eras. ‘Existential issues, especially in a Vietnam-era vet where they weren’t seen as heroes, so their PTSD has gone undiagnosed and unspoken’. This is the only article in this review to link PTSD and related symptoms at the end of life to dementia. ‘It shows up in dementia – re-enacting trauma, often mixed with delirium’. ‘Clinicians described forms of agitation, restlessness, pain, and delirium which seemed to interact with PTSD symptoms of hyperarousal. “A lot more difficulties sleeping at night that wasn’t so prevalent in their daily life – now it starts to emerge”’. ‘Clinicians . . . described emotions or emotion-related behaviours, such as crying, grief, moral injury, isolation, stoicism, and strained relationships with family. Although these emotions are not specifically named in DSM5-5 in this category, they may comprise additional presentations in the context of hospice and palliative care’. Trauma-related avoidance behaviours can hinder communication and care. Trust issues compound this. |
| Kelly-Cook et al. (2016), USA, Quantitative | To evaluate the clinical impact of palliative care in the treatment of terminally ill Vietnam veterans with a history of PTSD vs those without PTSD, as it pertains to medications for symptom control at the end of life. | Retrospective study that analysed data obtained from electronic medical records (EMR) of a tertiary VA hospital. The data consist of patient demographics and characteristics of the study including clinical laboratory and history of events. Participants with PTSD vs the non-PTSD participants (control group) were analysed. | The total sample was 176: Participants with PTSD was 39, and the control group (participants without PTSD) was 137. | Retrospective data collection was investigators used CPRS (VA’s EMR system) for palliative care consults. | Lifetime prevalence of PTSD was noted in 22% of this study population, while 27% had a diagnosis of insomnia, 30% had a diagnosis of anxiety, 44% had a history of alcohol-related substance abuse and 47% had a history of substance abuse other than alcohol. Results showed that there is a significant association between the diagnosis of PTSD and the medications needed at the end of life. 72% of PTSD participants received some form of PTSD medication (collective use of benzodiazepines, antipsychotics, antidepressants and hypnotics) at the end of life vs 40% of the non-PTSD group (p = 0.0005). However, when broken down into individual drug components, there was no statistically significant association between the diagnosis of PTSD and the need for benzodiazepines (p = 0.4413) and antipsychotics (p = 0.1016). Furthermore, there was a significant correlation between the diagnosis of PTSD and the need for antidepressants (59% of PTSD population vs 27% of non-PTSD population; p = 0.0002) and hypnotics (38% of PTSD population vs 18% of non-PTSD population; p = 0.0085) at the end of life. |
| Kutney-Lee et al. (2021), USA, Quantitative | To examine demographic and clinical characteristics, and EOL healthcare utilisation and quality indicators among Vietnam-era Veterans who died as inpatients in VA Medical Centres. Also a contemporaneous comparison to Veterans of the WWII/Korean War-eras to identify the presence of any clinically meaningful differences. | Retrospective pilot using medical records from VA decedents examined clinical characteristics, healthcare utilisation and EOL quality indicators for Vietnam-era Veterans who died in VA inpatient settings between fiscal years 2013 and 2017. In addition, bereaved family surveys were used to identify and develop best practices for improving hospice care for this population. Descriptive statistics were calculated to examine differences in patient and facility characteristics by war era. Robust logistic and linear regression models were used to compare EOL process measures and utilisation measures by war era. | This study had participants from two places: (1) a larger sample of nearly all acute, Community Living Centres and inpatient hospice unit descendants that was used to examine demographics and clinical characteristics, and end of life, process and utilisation measures (N = 87,526), and a (2) smaller sample of descendants with complete BFS data (N = 39,296). | BFS data and VA medical records obtained from the Corporate Data Warehouse (VA’s clinical, administrative and financial data repository) for Veterans who died as inpatients across 146 VA Medical Centres nationwide for fiscal years 2013–2017. | The percentage of Veterans with ‘high disability’ priority status was significantly higher in the Vietnam-era (44.9% vs 34.2%). Although Vietnam-era Veterans were younger, they carried a significantly higher comorbidity burden than Veterans from earlier eras, including mental health and substance use disorders. 33% of Vietnam-era Veterans had a diagnosis of depression, compared to 23.5% Veterans from prior eras. After accounting for age and survey nonresponses, slightly lower scores were observed for Vietnam-era Veterans compared to WWII/Korean War-era Veterans for PTSD symptom management at the EOL (82.6% vs 90.9%, p < 0.001). Alcohol abuse was nearly five times higher among Vietnam-era Veterans compared to WWII/Korean War-era Veterans (24.0% vs 5.7%), while PTSD was three times higher (16.5% vs 5.7%). Drug abuse was also more common among Vietnam-era Veterans (11.8% vs 2.0%). When comparing EOL care utilisation and process measures by war era, Vietnam-era Veterans had significantly more outpatient visits (55.8 vs 50.4, p < 0.001) and days in hospital (72.3 vs 53.2, p < 0.001) in the last year of life compared to prior war eras. Compared to WWII/Korean War-era Veterans, fewer Vietnam-era Veterans received a palliative care consultation in the last 90 days of life (70.4% vs 72.0%, p < 0.01), whereas higher proportions of Vietnam-era Veterans died in a Community Living Centres (i.e. VA nursing homes) setting (18.1% vs 15.8%, p < 0.001). |
| O’Connor et al. (2014), Australia, Qualitative | To understand the palliative care needs of veterans at the end of life. The study specifically set out to - Investigate distinctive aspects of a veteran’s EOL care, - Determine whether the needs of dying veterans were being met and - Compare these aspects between veterans and non-veterans. |
A small qualitative exploratory study designed to examine the home-based palliative care needs of veterans as they face the end of their life, to highlight their needs in comparison with non-veterans. All analyses were undertaken manually by the researchers; the descriptive data were comparatively analysed and the qualitative data thematically analysed, and then both were compared and contrasted between veteran and non-veteran records. | 10 deceased veterans and 10 deceased non-veterans were drawn from the palliative care service’s patient database in 2009. | The data were sourced from the medical record on-site, utilising a template specifically developed for this study. | Avoidance behaviours were seen more ‘“a number of veterans expressed anxiety about prognosis”; one was reluctant to use services, preferring to be “left alone to die.” Nursing notes made reference to depression: “He declined counselling, psychology assessment and antidepressants”’ (V7). ‘Frustration and anxiety were evident in a number of veterans records; one indicated frustration waiting for a diagnosis; another worried about prognosis saying he would “be safer in a palliative care unit” and was too fatigued to think about it anymore’ (VA1). A veteran was ‘frustrated and anxious’, insisting on staying in his home alone, resisting moving to his daughters’ home alone, resisting moving to his daughters’ home so he could remain independent ‘to the end’ (V1). |
| Prince-Paul et al. (2016), USA, Qualitative | This study aims to explore: - The meaning of important life events and life review within the context of being a veteran; - To discover if and how emotions may be associated with these memories and - To understand if the military experience shaped or influenced these memories. |
A phenomenological, hermeneutic, qualitative study was planned to advance the understanding and meaning of being a veteran enrolled in home hospice care. All interviews were transcribed verbatim and analysis was guided by the Giorgi method as outlined by Omery. The Giorgi method of analysis consisted of five steps: each transcript was read to get a sense of the whole; individual constituents of the experience were identified; coding was based on emerged categories and identification of essential meanings; and new data were compared and contrasted until themes emerged. The final step of the analysis involved the synthesis and integration of the various themes into a description of the phenomenon that was enriched with illuminating parts of the text. Preliminary analysis involved open coding, or the assignment of labels to words or phrases representing key categories. Analysis within and across the interviews resulted in the identification of recurring themes. |
15 adult terminally ill veterans who resided in their private homes in a community setting were purposively selected from a large, non-profit hospice program in the Midwestern United States. | Data were collected using in-depth voice recorded semi-structured interviews. An interview guide, developed by the PI, was used to aid in the facilitation of the interview. Only one participant screened positive for PTSD, according to the PC-PTSD instrument; this individual decided to continue with the full interview. |
Five themes emerged that described the meaning of being a veteran enrolled in home hospice care: limited opportunities, broken relationships, obligation, military service as a life influence – not definition and lack of fear/acceptance of death. Theme 1. Limited opportunities Theme 2. Broken relationships ‘My childhood and relationships with my mom and dad were terrible. . .cause her and I didn’t get along. . .that affected me more than my entire war time. . .I joined the [branch]. . .I went to kiss my mother and hug her about 5 in the evening before I left. . .“go to hell”. . .she said in Slovak. I’ll never forget that’ ‘My dad was a big alcoholic and he didn’t support us or nothing, you know. When I got back from Vietnam, I got married and obviously that didn’t turn out so good either’ ‘The VA never informed us of anything, so I got mad and says if this is how the government works, I don’t want no part of it. So I quit getting it’ ‘I have seen them [VA] one time, but they’re not very helpful. . .I don’t think I could rely on them. . . and then it takes so long to wait to be there anyways. . .’ Theme 3. Obligation Theme 4. Life influence not definition ‘The happiest day of my life was when I got outa Vietnam. . .I was an alcoholic though. . .’ Theme 5. Lack of fear/acceptance of death ‘I’ve covered the bases. . .I know I’m dying. . .I tell people I’m not afraid of being dead. . .everyone does that’ ‘I want to get out of here. . .I want to go. . .I have no regrets. . .I don’t need anything. . .I am just a regular guy who is ready to die’ ‘If you get the impression that I am totally at peace, I am. . . enjoy life as you get it. When you got it, enjoy life cause it’s really . . .it’s really too short. That’s been said a million times, it’s too short, and there’s really nothing to worry about’. |
| Roth et al. (2013), Canada, Quantitative | This study examines: - Predictors of PTSD-related symptoms in patients requiring palliative care; - Assess whether anxiety, depression, pain catastrophizing and pain anxiety mediate the relationship between pain interference and PTSD-related symptoms; and - Evaluate the relationship of these variables on pain interference and PTSD-related symptoms in a multiple mediator model. |
Hierarchical multiple regressions were used to examine HADS-Anxiety, HADS-Depression, PCS and PASS-20 scores as predictors of PCL-C scores; and mediation analyses were used to test the effect of HADS-Anxiety, HADS-Depression, PCS and PASS-20 on the relationship between BPI-SF interference and PCL-C. | A total of 100 cancer patients at one of two palliative care sites completed the questionnaires after providing written informed consent. 89 of them were completed in the presence of the study investigator, and the remaining 11 participants completed the questionnaires independently. | In addition to the survey, demographic and disease-related data, including age, sex, marital status, cancer diagnosis, stage of cancer at date of diagnosis and current stage of diagnosis, were extracted directly from participants’ medical record. | Only pain anxiety and pain catastrophizing emerged as significant mediators of the relationship between pain interference and PTSD-related symptoms. After being entered in a multiple mediator model, pain anxiety emerged as the strongest mediator. They found that pain anxiety strengthen the positive relationship between pain interference and PTSD symptoms. The findings of the present study reveal that pain and PTSD-related symptoms are important concerns in palliative care, and that pain must be addressed to best meet the needs of this population. |
AD, adjustment disorder; BFS, bereaved family survey; BPI-SF, Brief Pain Inventory–Short Form; CBD, cannabidiol; CPRS, Computerized Patient Record System; EOL, end of life; FATE, Family Assessment of Treatment at End-of-life; HADS, Hospital Anxiety and Depression Scale; KPS, Karnofsky Performance Status; MD, major depression; MMSE, Mini-Mental State Examination; PASS-20, Pain Anxiety Symptoms Scale-20; PC-PTSD, primary care post-traumatic screen; PCL-C, PTSD Checklist–Civilian Version; PCS, Pain Catastrophizing Scale; PCU, Palliative Care Unit; PTSD, post-traumatic stress disorder; RTC, randomised control trial; SPCC, Stepwise Psychosocial Palliative Care; THC, tetrahydrocannabinols; USA, United States; VA, Veteran Affairs; vs, versus.
Data analysis
Strauss and Corbin’s approach to coding was used within Grounded Theory (GT) methodology to analyse the narrative data.26,27 Historically, the integrative review method 21 and GT methodology 28 have been used successfully to build nursing knowledge and inform research, practice and policy initiatives. The ATLAs.ti 23 Computor-Aided Qualitative Data Analsis software was used to support data analysis. 27 Three stages of coding were applied, guided by GT methodological traditions. 26 Firstly, open coding was used to fracture the data to distinguish ‘basic conceptual units’ found in the data and organises codes into categories. 29 Once the codes were categorised, axial coding was applied to the data. This step takes the categorised codes and creates a mechanism through which interactions among them can be worked out. 29 Drawing on the data and constant comparison helps ensure the proposed connections demonstrate sustained resonance under interrogation. 29 After axial coding had clarified core categories linked to subcategories, selective coding builds ‘a conceptual framework from which to generate the new GT’ (p. 129) 29 was applied to the data. Networks represented the relationships developed using constant comparison 27 as an essential step demonstrating the transparency of interpretations.
Results
Description of studies
A total of 1581 studies were identified by database searching and exported to Covidence software for removing duplicates (n = 271) and screening (Table 2 – Article matrix table). Around 1176 studies were removed after title and abstract screening due to being out of scope. The full texts of the remaining 136 studies were then screened, and reasons were provided for exclusion. The full-text versions of six publications were not available from any source, including directly from publishers or libraries. As a result, they were excluded. A total of 11 studies were included: four qualitative designs included in-depth interviews, 30 a case study, 31 retrospective data extraction from the clinical record, 32 and an observational study using focus groups and qualitative content analysis. 33 Seven were quantitative in design, including a medical record review,34–37 prospective38,39 and retrospective 40 clinical cohort studies. The studies were conducted in Australia (n = 1), 32 Canada (n = 1), 39 Japan (n = 1) 38 and the United States (n = 7). One study used a medical outcomes tracker and could not provide details of the participant’s country of origin. 40
This review represents 96,505 participants. The sample size varied widely across the studies (from three participants in a case study, 31 to 87,526 in a 5-year study using national hospital datasets). 36 Seven studies included participants with diagnosed PTSD31,33–37,39 and four inferred the existence of PTSD based on responses or clusters of symptoms.30,32,38,40 Of the 11 studies, eight were focused on war veterans, which addressed trauma-informed palliative care for veterans,30–37 pharmaceutical treatment for those with and without PTSD, 40 a comparison of end-of-life care for veterans of the Vietnam War and World War 1/Korean War34,36 and veterans descendants, including bereaved family’s perceptions. 37 One study explored clinicians’ perceptions of end-of-life care for veterans. 33 Three studies were not focused on veterans; one study investigated the self-reported impact of medicinal cannabis on palliative care symptoms, including PTSD-related intrusive symptoms such as flashbacks, 40 one examined psychological distress among cancer patients, 38 and the third explored the relationship between pain and PTSD symptoms in palliative care. 39 Only two studies explored interventions.31,40 Feldman et al. 31 undertook a case series evaluation of a three-step graded intervention process for a veteran population. Casarett et al. 40 studied the self-reported benefits of medical cannabis for common palliative care symptoms, including flashbacks, pain, insomnia and dyspnoea, in a retrospective analysis of a medical outcome tracker for medicinal cannabis users.
Quality appraisal
The Quality Appraisal for primary studies assessed the risk of bias in the included studies. Overall, the methodological quality of retained studies was fair. Quality appraisal was conducted using the Mixed Methods Appraisal Tool (MMAT) Hong et al. (2018). 25 (Table 3).
Table 3.
Results of Quality Appraisal of primary studies.
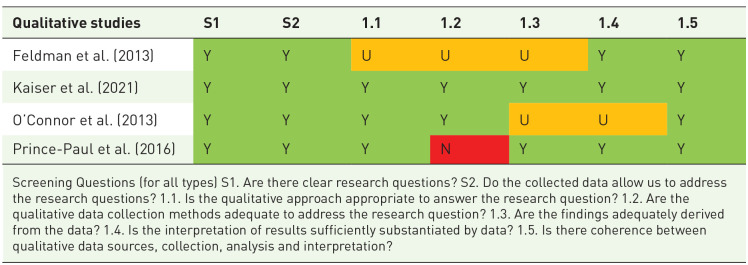
|
Screening Questions (for all types) S1. Are there clear research questions? S2. Do the collected data allow us to address the research questions? 1.1. Is the qualitative approach appropriate to answer the research question? 1.2. Are the qualitative data collection methods adequate to address the research question? 1.3. Are the findings adequately derived from the data? 1.4. Is the interpretation of results sufficiently substantiated by data? 1.5. Is there coherence between qualitative data sources, collection, analysis and interpretation?
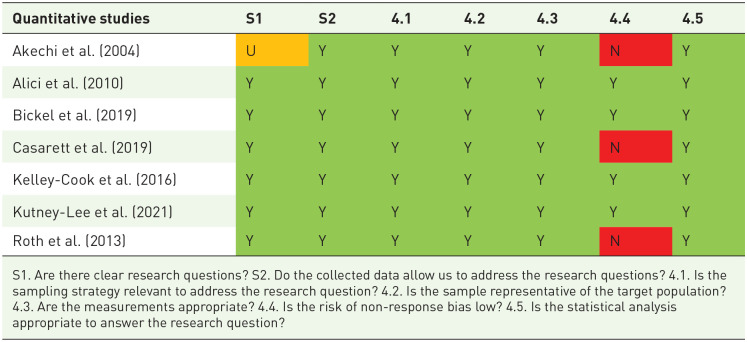
|
S1. Are there clear research questions? S2. Do the collected data allow us to address the research questions? 4.1. Is the sampling strategy relevant to address the research question? 4.2. Is the sample representative of the target population? 4.3. Are the measurements appropriate? 4.4. Is the risk of non-response bias low? 4.5. Is the statistical analysis appropriate to answer the research question?

|
Three levels of assessment quality scores

|
Narrative results
The GT developed from this review is as follows: Re-living trauma near death is a recognisable phenomenon with additional physical and psychological impacts that can be ameliorated with improved clinical knowledge and appropriate management.
This theory is supported by three core categories (Table 4). (1) Additional features help clinicians identify patients who are re-living trauma near death; (2) re-living trauma happens in the last weeks of life and is associated with increased healthcare needs and can include cognitive impairment; and (3) experiences of end-of-life care can be improved for trauma survivors who are re-living trauma near death. Each of the core categories will now be presented, with supporting concepts developed during the data extractions and narrative analysis of the original studies.
Table 4.
Grounded Theory: Re-living trauma near death is a recognisable phenomenon with additional physical and psychological impacts that can be ameliorated with improved clinical knowledge and appropriate management.
| Core Category 1. Additional features help clinicians identify patients who are re-living trauma near death | ||
|---|---|---|
| Subcategories | Codes | |
| 1. Impact on end-of-life physical symptoms | a. Increased acute pain and dyspnoea | - ‘JT’s cancer was advanced, and he reported intense uncontrolled pain’. (Feldman et al.,
31
p. 237) - ‘HJ’s pain was related to his radiation treatment. He reported that his pain rating was 10 out of 10 and typically ranged from 8 to 10’. (Feldman et al., 31 p. 238) - ‘Therefore, pain anxiety emerged as the strongest mediator of the relationship between BPI-SF [Brief Pain inventory–Short Form] interference and PCL-C [PTSD Checklist–Civilian version] scores’. (Roth et al., 39 p. 187) - ‘Although PTSD-related symptoms were common in this sample, patients were much more likely to have pain. . . . families also said that PTSD-related symptoms caused discomfort less often than pain did (1.79 vs. 1.93; sign rank test, P < 0.001). Patients with pain were more likely to experience PTSD-related symptoms’. (Alici et al., 37 p. 510) - ‘[Family members] reported that the patient experienced PTSD-related symptoms . . .Of these, 28% (n 1⁄4 25/89) “always” experienced discomfort. Those patients who had PTSD-related symptoms were similar to other patients with respect to age, gender, site of death, and the patient’s and respondent’s ethnicity (Table 1)’. (Alici et al., 37 p. 510) - ‘Although PTSD-related symptoms were common in this sample, patients were much more likely to have. . . . dyspnea . . . . families reported that PTSD-related symptoms made the patient uncomfortable more often than dyspnea did . . . . patients with dyspnea were more likely to experience PTSD-related symptoms . . . .’ (Alici et al., 37 p. 510) |
| 2. Intensification of PTSD-related symptoms and disorders | a. Persistent avoidance, resistance to care and mistrust of authority |
- ‘“JT” [patient], a 65-year-old male veteran. . .. .had been diagnosed with lung cancer and was refusing all further care, which included palliative care . . . In team meetings, his physicians shared concerns about refusal of all further medical care. . .Staff members experienced significant emotional reactions to JT, including frustration and anger’. (Feldman et al.,
31
p. 237) - ‘. . . . be safer in a palliative care unit’, and was ‘too fatigued to think about it anymore’ [Veteran 1 medical record]. (Feldman et al., 31 p. 138) - ‘Because the patient was unwilling to engage with most members of the treatment team directly, the psychologist engaged with the team on his behalf. First, he shared the diagnosis of PTSD with the PCCT (palliative Care Consultancy Team). Psycho-education was provided to the team regarding various ways PTSD can complicate end-of-life care, many of which were exhibited by JT, including anxiety and anger, poor medical adherence. . .’. (Feldman et al., 31 p. 237) - ‘A number of veterans expressed anxiety about their prognosis; one was reluctant to use services, preferring to be “left alone to die.” Nursing notes made reference to depression: “He declined counseling, psychosocial assessment and anti-depressants” (V7). Two male veterans refused to speak with counselors or nurses, preferring to let their wives or children “have those conversations” (V10). One veteran expressed a desire to stop treatment, but there was no ensuing reference to withdrawing treatment’. (O’Connor et al., 32 p. 135) - ‘Although avoidance is a symptom of PTSD, some clinicians described observing the opposite of avoidance in some of their veteran patients. Namely, clinicians described in some veterans an eagerness to share stories, a desire to connect with others from the military, or a sense of pride in one’s military service. In some instances, this eagerness to share applied to staff but not family’. (Kaiser et al., 33 p. 5) - ‘In the present study, Cronbach’s alpha for the total score and fear of pain, cognitive anxiety, escape/avoidance behaviors, and physiological symptoms of anxiety subscale scores’. (Roth et al., 39 p. 184) - ‘he didn’t trust his medical providers. He stated, “I know they are not telling me everything and I think they are hiding something from me about my condition”’. (Feldman et al., 31 p. 238) - ‘TR reported distrust of his medical providers regarding his prognosis. As mentioned in the previous case discussion, although trust issues are not necessary for a diagnosis of PTSD, they are common in trauma-exposed veterans’. (Feldman et al., 31 p. 240) - ‘Trust issues makes it difficult for them to want to open up’. (Kaiser et al., 33 p. 4) - ‘Several participants highlighted a sense of mistrust and lack of fulfillment of promises, critical transgressions of relationships, of the VA health system’. (Prince-Paul et al., 30 p. 5) - ‘Psychoeducation regarding various ways PTSD can complicate end-of-life care, many of which were exhibited by JT, including anxiety and anger, poor medical adherence, difficulty engaging in direct problem-focused communication regarding care, and distrust of authority. This information also was documented in his chart for future providers’. (Feldman et al., 31 p. 237) - ‘The therapist also shared with the doctor that PTSD may be interfering with the patient’s ability to trust medical providers. The therapist offered to directly facilitate a conversation between the patient and physician about the listed questions’. (Feldman et al., 31 p. 240) |
| b. Intrusive symptoms and alterations in arousal and reactivity | - ‘Hospice and palliative care clinicians observed symptoms aligning with all four symptom clusters of PTSD: re-experiencing, avoidance, negative alternations of cognition and mood, hyperarousal, . . .. For the latter two clusters, clinician observations revealed numerous potential additional presentations of symptoms in the hospice and palliative care setting’. (Kaiser et al.,
33
p. 3) - ‘. . .particularly irritability or angry outbursts, hypervigilance, and sleep disturbance. Clinicians were less likely to report exaggerated startle response or concentration problems. (Kaiser et al., 33 p. 5) - ‘A lot more difficulties sleeping at night that wasn’t so prevalent in their daily life – now starts to emerge’. (Kaiser et al., 33 p. 5) - ‘When asked about psychological symptoms, HJ, indicating recently experiencing what he called “hallucinations,” difficulty sleeping due to nightmares, intrusive thoughts about combat experiences, flashbacks, a tendency to isolate himself from others, and intense anxiety whenever reminded of his experiences in the military. He was seen by a psychiatrist who determined that his hallucinations were related to a combination of analgesic and psychiatric medications. Adjustments to his medication regimen quickly alleviated these hallucinations, though the other symptoms persisted’. (Feldman et al., 31 p. 238) - ‘Furthermore, TR was having difficulty sleeping due to nightmares and intrusive thoughts about his military combat experience. The patient scored within the clinical range for depression and PTSD on the GDS and PTSD Symptom Checklist-Military Version (PCL-M)’. (Feldman et al., 31 p. 240) - ‘Psychiatric co-morbidities were statistically more prevalent in veterans with PTSD, 36% with anxiety disorders and 21.4% with major depressive disorder’. (Bickel et al., 35 p. 507) - ‘Lifetime prevalence of PTSD was noted in 22% of this study population, while 27% had a diagnosis of insomnia, 30% had a diagnosis of anxiety. . . . . . Lifetime diagnosis of PTSD was positively associated with a past medical history of insomnia, other sleep disorder diagnoses (such as obstructive sleep apnea or restless leg syndrome), anxiety, depression. . .’. (Kelley-Cook et al., 34 p. 629) |
|
| c. Re-living trauma near death can coexist with dementia and cognitive impairment |
- ‘Clinicians infrequently reported observing physiological reactions to trauma reminders. Clinicians noted that re-experiencing sometimes occurred in tandem with dementia or delirium. Examples as observed by clinicians include:• “Hallucinations that can be tied back to service” • “Flashbacks” • “It shows up in dementia – reenacting trauma, often mixed with delirium”’ (Kaiser et al.,
33
p. 4) - ‘It shows up in dementia – reenacting trauma, often mixed with delirium’. (Kaiser et al., 33 p. 3) ‘. . . He was seen by a psychiatrist who determined that his hallucinations were related to a combination of analgesic and psychiatric medications. Adjustments to his medication regimen quickly alleviated these hallucinations, though the other symptoms persisted’. (Feldman et al., 31 p. 238) |
|
| d. Related disorders including substance use disorder |
- ‘“HJ,” a 65-year-old Caucasian, single male, was refer – red to the Palliative Care Unit for pain management. He was diagnosed with squamous cell carcinoma and was receiving chemotherapy and radiation. He had a history of type II diabetes, COPD, congestive heart failure, and PTSD, as well as current tobacco use and previous substance abuse’. (Feldman et al.,
31
p. 237) - ‘Some had attempted to mend past transgressions with the help of the Twelve Steps of Alcoholic Anonymous. . . .I think it would of been worse though without the military. . . it makes you shape yourself up a little. . . .the whole time I was influenced by it. . . . I’d probably still be living with my mother without it. . . but here I am now. . . in my own house. . . even though I am dying I have this wonderful spouse, I can take care of my car, and I have my family’. (Prince-Paul et al., 30 p. 7) - ‘Lifetime prevalence of PTSD was noted in 22% of this study population, . . . . . .44% had a history of alcohol-related substance abuse, and 47% had a history of substance abuse other than alcohol. . . Lifetime diagnosis of PTSD was positively associated with . . .. . . . alcohol abuse’. (Kelley-Cook et al., 34 p. 629) |
|
| Core Category 2. Re-living trauma near death requires increased health care utilisation | ||
| Subcategory | Codes | |
| 1. Last weeks of life | a. Increased health care utilisation at the end of life including increased medications in the last weeks/days of life. |
- ‘Participants with PTSD diagnosis were more likely to be followed by outpatient mental health than those participants without PTSD (P < .0001)’. (Kelley-Cook et al.,
34
p. 679) - ‘Patients with PTSD had significantly more VA hospital admissions and ER visits than those without PTSD (admissions: PTSD 2.8, no PTSD 2.4, p < 0.0001; ER visits: 3.2 vs 2.5, p < 0.0001)’. (Bickel et al., 35 p. 507) - ‘During the final admission, for veterans with PTSD, there was a trend towards any ICU use (49.6% vs 42.7%, p = 0.004), but deaths in the medical or cardiac ICU were less likely’ (Bickel et al., 35 p. 507). - ‘There were no statistically significant differences noted in length of stay or use of invasive treatments’. (Bickel et al., 35 P. 507) - ‘The rates of admission to health care facilities varied with five veterans admitted once, four admitted twice, and one admitted 3 times in the last 2 years of their lives. In the non-veteran sample, there was no medical record for two, three had one admission, and five had two admissions in the 2 years prior to death’. (O’Connor et al., 32 p. 136) - ‘The use of health care professionals and services varied between the veterans and non-veterans, with almost all veterans seeing five or more. In contrast, almost all non-veterans saw five or less’. (O’Connor et al., 32 p. 137) - ‘Patients with PTSD were more likely to have received an opioid, benzodiazepine, or an antipsychotic at any time during the last 7 days of life and were also more likely to have received each medication class in both the last 48 h of life and in the time period from 49 h to 7 days before death’. (Bickel et al., 35 p. 507) - ‘There were no statistically significant differences noted in length of stay or use of invasive treatments. However, there were significant differences in administration of symptom-relieving medications in the last 7 days of life’. (Bickel et al., 35 p. 507) - ‘In this pilot study’s population, there is a significant association between the diagnosis of PTSD and the medications needed at the EOL’. (Kelley-Cook et al., 34 p. 679) - ‘Roughly, 72% of PTSD participants were receiving some form of PTSD medication (collective use of benzodiazepines, antipsychotics, antidepressants, and hypnotics) at the EOL versus 40% of the non-PTSD group (P 1⁄4 .0005). . .. . .Furthermore, there was a significant correlation between the diagnosis of PTSD and the need for antidepressants (59% of PTSD population vs 27% of non-PTSD population) (P 1⁄4 .0002) and hypnotics (38% of PTSD population vs 18% of non-PTSD population) (P 1⁄4 .0085) at the EOL’. (Kelley-Cook et al., 34 p. 630) - ‘Patients with PTSD were more likely to have received an opioid, benzodiazepine, or an antipsychotic at any time during the last 7 days of life and were also more likely to have received each medication class in both the last 48 h of life and in the time period from 49 h to 7 days before death. . .. . .’. (Bickel et al., 35 p. 507) - ‘[Family members] reported that the patient experienced PTSD-related symptoms . . .. . .Of these, 28% . . . “always” experienced discomfort. . .Seventeen percent of family members. . . reported that the patient experienced PTSD-related symptoms in the last month of life’. (Alici et al., 37 p. 510) - ‘Patients with PTSD were more likely to have received an opioid, benzodiazepine, or an antipsychotic at any time during the last 7 days of life and were also more likely to have received each medication class in both the last 48 h of life and in the period from 49 h to 7 days before death’. (Alici et al., 37 p. 510) |
| Core Category 3. Experiences of end-of-life care can be improved for trauma survivors who are re-living trauma near death. | ||
| Subcategory | Codes | |
| 1. Palliative care for trauma survivors | a. Unmet needs of trauma survivors, their families and palliative care staff | ‘“A lot of families don’t understand what PTSD is or what is going on when the behavior changes”. . . “Not enough education for everyone on PTSD” [Palliative care staff]’. (Kaiser et al.,
33
p. 6) - ‘Family members of patients who had PTSD-related symptoms were more likely to report that they had unmet needs for emotional support in the patient’s last month of life. . .. Families who reported PTSD-related symptoms had lower (worse) scores on the VA quality survey compared with those who did not. . .. . .’. (Alici et al., 37 p. 510) - ‘Family members . . .. . .They also were more likely to report worse communication with providers and less attention to the patient’s dignity and well-being. . . . In addition, family members of patients with PTSD-related symptoms reported less satisfaction overall with the care received. . . .’ (Alici et al., 37 p. 510) - ‘Families who reported PTSD-related symptoms had lower (worse) scores on the VA quality survey compared with those who did not’. (Alici et al., 37 p. 510) - ‘None of the patients were referred to the psychiatry division during the study period’. (Akechi et al., 38 p. 1961) - ‘ . . . some clinicians included observations about the needs of veterans’ family members. These responses differed from observations of estrangement from families, . . .instead relating to needs and responses of family members when their veterans neared EOL.• “A lot of families don’t understand what PTSD is or what is going on when the behavior changes” • “[We see a] dynamic with families – strain, families don’t understand what’s going on. Sometimes vets open up to chaplain (who is a Navy vet) and family gets upset that their family member doesn’t talk to them” • “Not enough education for everyone on PTSD”’. (Kaiser et al., 33 p. 6) - ‘Approach or engagement with military memories. Military cohort issues Family support issues • Pride • Telling stories • Meaning making • Negative homecoming/lack of recognition • Family as reporters • Families need support • Family emotions • Family knowledge of PTSD’. (Kaiser et al., 33 p. 5) - ‘In team meetings, his physicians shared concern about his refusal of all further medical care. Staff members experienced significant emotional reactions to JT, including frustration and anger. Furthermore, they were uncertain about how to communicate with him to address his medical needs’. (Feldman et al., 31 p. 237) - ‘. . . some clinicians included observations about the needs of veterans’ family members. . .. . .’. (Kaiser et al., 33 p. 6) - ‘PTSD education and resource needs, Clinicians indicated interest in learning about PTSD assessment, how to effectively communicate with veterans who share memories or have difficulty with PTSD symptoms, and how best to support family members’. (Kaiser et al., 33 p. 6) - ‘Clinicians also expressed interest in learning more about military cohort differences, military culture, and the impact of substance use disorders, moral injury, and military sexual trauma’. (Kaiser et al., 33 p. 6) |
| 2.Enablers of better EOL care for trauma survivors | a. Receiving palliative care |
- ‘Among patients with PTSD-related symptoms, those who received a palliative care consult (n 1⁄4 49) had lower ratings of discomfort because of those symptoms . . .. (Alici et al.,
37
p. 510) - ‘. . .palliative care services could reduce his present suffering and provide an alternative care option’. (Feldman et al., 31 p. 237) |
| b. Benefits of medication for symptom management |
- ‘Of the six symptoms, response was associated with increased THC:CBD ratio for neuropathic pain. . ., insomnia. . ., and depressive symptoms. . . Increased THC:CBD ratio was not associated with a greater response of post-traumatic stress disorder (PTSD)-related flashbacks . . . or anorexia. . . The response for anxiety symptoms was not significant . . ., but showed an inverted U-shaped curve, with maximal benefit at a 1:1 ratio (50% THC). (Casarett et al.,
40
p. 1180) - ‘Pre-use symptom severity varied from 5.90 (depressive symptoms) to 7.19 (insomnia) and post use severity ranged from 2.21 (anxiety symptoms) to 3.45 (neuropathic pain). The smallest reductions were seen for neuropathic pain (42.2% had at least a three-point reduction) and the largest for PTSD-related flashbacks (78.1%) (Table 1). Across symptoms, THC percentage ranged from 70.5% (neuropathic pain) to 94.9% (insomnia) and ranged from *0% to 100%. (Casarett et al., 40 p. 1181) - ‘Several symptoms were very sensitive to increasing THC:CBD ratios. For instance, response increased with increasing THC:CBD ratio for neuropathic pain . . . and insomnia. . . . There was a smaller positive association for depressive symptoms. . . . (Casarett et al., 40 p. 1182) - ‘About 71% and 78% of the patient cohort experienced at least 3-point improvement in insomnia and PTSD-related flashbacks, respectively, while only 42% of the cohort experienced similar improvement in neuropathic pain. After adjusting for THC/Cannabidiol (CBD) ratio, dose, age and gender, the odds of achieving at least 3-point improvement in neuropathic pain and insomnia were 3.58 and 2.93,. . .respectively. However, the odds ratio for PTSD flashback was not statistically significant. . .’. (Casarett et al., 40 p. 1181). |
|
| c. Application of the Stepwise Psychosocial Palliative Care model | ‘. . . His daughter and wife agreed to inform staff if they were not going to be present so [that] staff could make more frequent visits. Leaving the television on and closing the door to his room were identified as ways to decrease traffic noise [Staff in VA Medical Centre]’. (Feldman et al.,
31
p. 240) - ‘His primary physician and other staff members then utilized these strategies, allowing them to clarify information and build rapport. After such rapport was built, the physician then further utilized these strategies to engage in a discussion regarding his medical care, through which the patient gained trust in the physician, was open to learning about care options, and ultimately decided to be discharged to his home with the support of home hospice care’. (Feldman et al., 31 p. 237) - ‘In this case, the goal was to help with staff/doctor–patient communication. This education led to a collaborative problem-solving discussion that enabled all team members to generate and acquire practical solutions for use with JT’. (Feldman et al., 31 p. 237) - ‘focus on a variety of cognitive-behavioral techniques, she also provided information on the nature of PTSD from a CBT perspective, focusing on the connections between thoughts, feelings, and behaviors. This explanation helped to render his symptoms more predictable, lowering his anxiety somewhat. To further address his anxiety, calm (diaphragmatic) breathing, and thought stopping were introduced. These techniques were explained, demonstrated, and practiced with the patient’. (Feldman et al., 31 p. 239) |
|
PTSD, post-traumatic stress disorder.
Additional features help clinicians identify patients who are re-living trauma near death
This category revealed additional features that were not explained by a diagnosis of PTSD that may assist clinicians in identifying patients who may be re-living trauma near death.30–36,38,39 Re-living trauma near death may represent a specific expression of PTSD-related symptoms, including a combination of specific intrusive symptoms, hyperarousal, avoidance, and negative cognitive and emotional symptoms associated with PTSD. Additional features included increased end-of-life physical symptoms that have a co-relationship with trauma exposure. Included symptoms are unexplained severe pain or dyspnoea, intensification of PTSD-related presentations including avoidance behaviours, negative cognitive symptoms leading to mistrust, hyperarousal and related sleep disorders. These symptoms were described as reflecting a late emergence of trauma symptoms, or an increasing intensity of pre-existing trauma symptoms for the dying person.
Impact on end-of-life physical symptoms
Increased acute pain and dyspnoea
Physical symptoms such as acute pain and dyspnoea are not included in PTSD-related diagnostic criteria but were described as potential features of re-living trauma near death. Three of the included studies provided evidence that re-living trauma near death was associated with increased acute pain.31,37,39 Feldman et al. 31 described a new approach to treatment for individuals with PTSD at the end of life and identified three veterans with a diagnosis of terminal cancer admitted to a palliative care inpatient unit who experienced newly uncontrolled pain. They documented relationships between PTSD-related symptoms and acute pain crises. Emotional and physical pain were connected, with nightmares resulting in worsening pain crises the following morning. 31 Roth et al. 39 found that patients with a terminal cancer diagnosis transitioning to palliative care experienced co-occurrence of physical pain and emotional response to pain including PTSD symptoms. When patients worried about or feared cancer pain, their PTSD-related symptoms were triggered. 39 This interaction of pain symptoms was further emphasised in a separate study of family members’ perceptions of the frequency and impact of PTSD-related symptoms in veterans at end-of-life. 37 They found that pain had a bidirectional relationship with PTSD. Trauma affected the extent of pain reported by patients, and patients with pain experienced more symptoms of PTSD than those without pain. 37
Alici et al. 37 found that increased distress with dyspnoea was an additional feature of re-living trauma near death. There was also a bidirectional relationship between dyspnoea and PTSD-related symptoms. 37 Dyspnoea increased PTSD symptoms such as anxiety, and these symptoms adversely affected dyspnoea. This observation was a significant finding, as dyspnoea, along with pain, are symptoms that can cause high levels of distress for those dying. 37 Although PTSD-related symptoms were common at the end of life, family members reported that pain and dyspnoea occurred more frequently, 37 though, in comparison with PTSD symptoms, the pain was more likely to be rated as having a more significant impact than dyspnoea symptoms.
Intensification of PTSD-related symptoms and disorders
PTSD-related features of intrusive symptoms, persistent avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity were intensified when re-living trauma near death. 33 The presence of other factors such as substance use disorders, mood, anxiety disorders, risky behaviours and self-harm increased PTSD symptoms for trauma survivors. 33
Persistent avoidance, resistance to care and mistrust of authority
Mistrust of others is not included in the PTSD diagnostic criteria; however, it is a feature of re-living trauma near death. Four of the included studies31–33,39 showed evidence of avoidance behaviour that reduced access to palliative care at end-of-life. In an Australian retrospective study, O’Connor et al. 32 compared the home-based palliative care needs of 10 veterans to 10 non-veterans facing dying and found that some veterans avoided conversations with clinicians. 32 Two male veterans were reluctant to engage with services and avoided interventions like counselling, psychosocial assessment and antidepressant medication. 32 One veteran was unwilling to access services and expressed a wish to be ‘left alone to die’ (p. 138). 32 Similarly, Roth et al. 39 found that when PTSD-related symptoms were triggered by cancer pain, avoidance behaviours and psychological symptoms increased. Kaiser et al. 33 found that resistance to care was a feature of re-living trauma near death and was common in dying veterans. In their case studies evaluating the Stepwise Psychosocial Palliative Care (SPPC) model, Feldman et al. 31 found that one veteran with terminal cancer ‘coped with stressful topics by avoiding them’ (p. 240). Feldman et al. 31 also found that clinicians in the palliative care inpatient unit found it challenging to accept when patients declined medical care. Staff experienced emotional reactions like anger and frustration when a 65-year-old veteran with lung cancer refused all future care, including palliative care. 31 Notably, the male veteran previously referred to had not disclosed his history of trauma. When he refused care, including palliative care, the psychologist did a chart audit of his medical record, and a history of PTSD was identified. 31 This then initiated the trauma-informed palliative care SPPC model, which improved his symptom management.
Three of the included studies provided evidence of mistrust of medical providers and authority.30,31,33 Kaiser et al. 33 and Feldman et al. 31 found that palliative care clinicians perceived that trust issues impeded veterans’ engagement. Several interviewees in the study by Prince-Paul et al. 30 emphasised their mistrust and experience of unfulfilled promises by the United States Department of Veterans Affairs. O’Connor et al. 32 found that frustration and anxiety were evident in the records of several deceased Australian veterans. One veteran worried about his prognosis and stated that he would feel safer in an inpatient palliative care unit and that he did not have the energy to think about it anymore. 32
On occasion, some patients addressed trauma through increased engagement. Kaiser et al. 33 found that some clinicians reported the opposite of avoidance, describing veterans as being eager to share stories about medals and certificates and connect with others from the military. Other American war veterans chose to be cared for in the hospice programme as they felt the comradery and increased dignity of dying with their fellow servicemen. Others were proud of being veterans and liked to talk about their experiences. 33
Intrusive symptoms and alterations in arousal and reactivity
Four studies30,31,33,35 found that participants experienced increased sleep disturbance and increased psychological distress. Prince-Paul et al. 30 found exposure to ACE was associated with an increased risk of further trauma exposure later in life. In their study of the views of clinicians, Kaiser et al. 33 noted that some dying veterans had additional trauma-related presentations that aligned with traditional PTSD symptom clusters. Moral injury, family avoidance with or without fractured relationships, and isolation aligned with negative alterations in cognition and mood, pain, agitation, restlessness, cognitive issues and risky behaviours aligned with hyperarousal. 33
A retrospective study authored by Kelley-Cook et al. 34 compared the use of benzodiazepines, hypnotics, antidepressants and antipsychotic medications for terminally ill veterans with a history of PTSD (n = 28) to those without PTSD (n = 55). PTSD-related symptoms were often associated with a history of insomnia and other sleep disturbances such as obstructive sleep apnoea and restless leg syndrome. 34 In their national study of health care utilisation and medication use at the end of life, Bickel et al. 35 found that veterans with PTSD, compared to veterans without PTSD, were more likely to be prescribed antipsychotic medication, potentially increasing their risk of terminal delirium.
Re-living trauma near death can coexist with dementia and cognitive impairment
Two of the included studies described links between re-living trauma near death and cognitive impairment. Kaiser et al. 33 found a link between re-living trauma near death and dementia. Clinicians in this study reported observations in people who had dementia or cognitive impairment at the end of life that are consistent with re-living traumatic events. 33 Re-experiencing trauma can co-occur with dementia and delirium. 33 Palliative care clinicians included in focus groups described forms of agitation, restlessness and delirium, which were thought to be hyperarousal symptoms of PTSD. 33 There can be an iatrogenic relationship between re-living trauma and cognitive and perceptual impairment. 31 Feldman et al. 31 described the case of one veteran who experienced end-of-life hallucinations that were caused by a combination of antipsychotics and pain relief.
Related conditions, including substance use disorder
Co-morbid psychiatric disorders and substance use disorders were described in the reviewed research. In a study of 5341 veterans receiving end-of-life care in US-based Veteran Administration hospitals, 36.5% of veterans with PTSD also had anxiety disorders, compared to 12.5% without diagnosed PTSD; 21.4% of veterans with PTSD and 4.8% of those without PTSD had major depressive disorder. 35 Substance use disorder is not included in the DSM-5 criteria for the diagnosis of PTSD. 2 The clinicians in the study by Kaiser et al. 33 cited substance use disorder as a potential additional presentation for dying veterans who are trauma survivors. In Bickel et al.’s 35 national study, alcohol abuse was reported among 10.7% of veterans with PTSD and 3.4% of those without PTSD; 11.8% had a drug-use disorder (excluding nicotine and alcohol) compared with 2.9% of veterans without PTSD. In their pilot study, Kelley-Cook et al. 34 compared terminally ill Vietnam veterans with or without PTSD at the end of life and found that 44% of veterans with a history of PTSD had a history of alcohol-related substance abuse, and 47% had a history of substance abuse other than alcohol.
Kelly-Cook et al. 34 proposed that medication use for people with PTSD is likely to differ from those without PTSD, reflecting their greater vulnerability to re-experiencing and other PTSD symptoms. Kutney-Lee et al. 36 studied terminally ill Vietnam veterans and compared them to dying veterans from World War 2 and the Korean War campaigns and found that alcohol abuse rates among Vietnam-era veterans were five times that of other veterans.
In the interview study by Prince-Paul et al., 30 one veteran at the end of life commented that he tried to heal past transgressions by attending Alcoholics Anonymous. Another talked about being an alcoholic when he returned from the Vietnam War. 30
Re-living trauma near death requires increased healthcare utilisation
Increased healthcare utilisation and medications in the last weeks of life
Two of the included studies34,35 found that patients re-living trauma near death had increased health care utilisation and use of end-of-life medication in the last days/weeks of life. When comparing Vietnam veterans with or without PTSD, Kelley-Cook et al. 34 found that veterans with PTSD were more likely to attend outpatient mental health services. They also found that there was a significant association between a diagnosis of PTSD and increased use of antidepressants and hypnotic medication at the end of life. 34 Bickel et al. 35 found that American veterans with PTSD did have increased healthcare utilisation and medication use in the final 12 months of life. Healthcare use included significantly more United States Department of Veterans Affairs hospital admissions and emergency room visits, longer stays and an increased use of invasive treatments. 35 The latter may have reflected the fact that the cohort with PTSD was younger than the cohort without PTSD (mean age 65.4 and 70.1 years, respectively). 35 Significantly, the cohort with PTSD also received increased symptom-relieving opioids, benzodiazepines and antipsychotic medications within the last 48 h and the last 7 days of life. This suggests that trauma survivors have increased symptoms and suffering at the end of life and thus require more medication to manage these symptoms. 35
In the included studies, there was evidence of symptoms increasing for people who were re-living trauma near death. Alici et al. 37 found that family members reported observing symptoms of PTSD and pain in the last months of life. Furthermore, they discovered that in the last month of life, these descriptions of re-living trauma seemed to be associated with decreased comfort. 37 O’Connor et al., 32 who compared veterans to non-veterans and their health utilisation at the end of life, found that rates of hospitalisation varied among the 20 participants. Veterans, however, had more hospital admissions and had more significant contact with health professionals than their non-veteran counterparts. 32
Experiences of end-of-life care can be improved for trauma survivors who are re-living trauma near death
Five of the included studies provide evidence that trauma survivors and their families have unmet needs at the end of life.31,33,35,37,38 Alici et al. 37 found that family members were more likely to have unmet needs when their loved one was a veteran with PTSD. Family members reported that the clinician’s communication was poorer and that they paid less attention to the patient’s dignity. Family members also described ‘less satisfaction’ with their overall care delivery. Kaiser et al. 33 found that clinicians observed unmet needs from family members caring for veterans at the end of life and recommended education about PTSD at the end of life for families, providers and veterans. 33
Akechi et al. 38 found that none of the patients were referred to a psychiatrist during the study period despite 16.3% of participants having an adjustment disorder at baseline, highlighting this as an unmet need. Feldman et al. 31 found that palliative care staff had unmet educational needs as they were uncertain how to communicate with patients who refused care, including palliative care. Kaiser et al. 33 found that clinicians wanted more education and resources to understand PTSD at the end of life better. Clinicians wanted to learn how to identify past trauma, improve assessment skills, communication skills, symptom management and support family members. 33
Enablers of better end-of-life care for trauma survivors
Receiving palliative care
Palliative care seemed to be effective when it was available and provided.31,37 Feldman et al. 31 and Alici et al. 37 both reported the benefit of clinical palliative care services for dying veterans with PTSD. Alici et al. 37 surveyed family members of veterans who had died in a United States Department of Veterans Affairs hospital; family members of people with PTSD symptoms reported that those who had received a palliative care consult had lower ratings of discomfort due to PTSD-related symptoms.
Four included studies31,33,37,40 suggested further benefits of trauma-informed palliative care. Kaiser et al. 33 found that some clinicians expressed interest in learning more about trauma and its effects on dying veterans. In the same study, hospice and palliative care clinicians spoke about the importance of identifying past trauma and suggested universal screening be used to increase the chance of identification. 33 Alici et al. 37 found that family members identified PTSD-related symptoms more quickly if a diagnosis of PTSD had been made. However, since 63 of the 89 patients observed to have PTSD-related symptoms did not have a previous PTSD diagnosis, family members were sometimes left having to puzzle out symptoms without a frame for understanding them. 37
Benefit of medications for symptom management
There was a lack of evidence of specific pharmacotherapies that could support trauma survivors as they die, and all studies were observational. The only medication studied in relation to PTSD-related flashbacks at the end of life was cannabis. Using an internationally used self-report app connected to a portal, Casarett et al. 40 explored the relative contribution of tetrahydrocannabinol (THC) and cannabidiol (CBD) to patients’ self-rating of efficacy for common palliative care symptoms. They chose to look at common palliative care symptoms such as neuropathic pain, anorexia, anxiety symptoms, depression symptoms, insomnia and PTSD-related flashbacks. 40 Higher doses of THC, relative to CBD, were associated with a marked improvement in symptoms, including PTSD-related flashbacks. 40 The findings from this study have increased relevance to this review as both increased pain31,37,39 and sleep disturbances31,33,34 have been identified as additional features of re-living trauma near death, both of which cannabis was effective in managing. 40
Application of the SPCC model
There was a notable lack of palliative care interventions for those who are re-living trauma near death. Only one specific palliative care intervention for trauma survivors was identified. Feldman et al. 31 derived case-study-informed evidence that supports the pilot of the SPPC model. 31 This model reportedly improves access to effective palliative care for dying veterans with PTSD. Feldman’s model of care is based on palliative care philosophy and recognises that assessing for trauma can re-traumatise, so the first two steps are trauma sensitive rather than directly trauma treating. 31 The model has three stages or steps. Stage 1 ‘Palliate Immediate Discomfort and Provide Social Supports’. If this is ineffective, the clinicians must progress to Stage 2, ‘Provide Psychoeducation and Enhance Coping Skills’. If this stage is ineffective, clinicians progress to Stage 3, ‘Treat Specific Trauma Issues’. 31 In the case studies used to explore this model, environmental changes could reduce the triggering of PTSD-related symptoms. 31 One Veteran’s PTSD-related symptoms were triggered by traffic noise. His TV was always left on to combat this, and his door was shut. 31
Discussion
This study reveals new synthesised knowledge regarding the identification of trauma experiences near death. Findings should be interpreted with caution, as only 11 studies met the inclusion criteria. This review has highlighted that re-living trauma near death is a recognisable phenomenon with physical and psychological impacts30–40 that can be ameliorated with improved clinician knowledge30,33–37,39 and appropriate management.30,31,33–37,40 Additional features that are not included in a diagnosis of PTSD, such as intense unexplained acute pain,31,37,39 can help clinicians identify patients who are re-living trauma near death. These additional features that can occur in the last weeks of life are associated with increased healthcare utilisation and increased use of end-of-life medications and may coexist with cognitive and perceptual impairment.33–37 Additional features also include refusing all care, including palliative care, as an avoidance and mistrust response and staff-splitting behaviours.5,31
The positive interventions highlighted that stepwise communication was effective when trauma survivors had limited time to live, were fatigued or were unwilling to engage in trauma therapy, but this was a single case study with only three participants. 31 Elsewhere, Meyerson et al. 5 discussed trauma-informed care approaches in palliative care settings again for dying patients who were too fatigued or unwilling to engage in trauma therapy at this time in their lives. Meyerson et al. 5 provide examples of how trauma-informed hospice and palliative care can ameliorate distress and PTSD symptoms at the end of life. They provide recommendations for all palliative care teams on how to elicit and respond to a history of trauma. 5 If palliative care teams are not aware of a history of trauma, they may not pick up on contextual cues, and appropriate referrals may not be made, resulting in increased suffering and a delay in both curative treatment and palliative care. 5
To date, trauma-informed care is not the usual practice in palliative care delivery.4,5,7,10 Timely palliative care has been shown to improve quality of life and mood significantly 9 ; patients experience less aggressive care at the end of life and survive longer. 9 Yet, dying patients who have experienced trauma may live and die with increased chronic pain, severe unexplained acute pain and increased suffering and may be re-traumatised at the end of life.4,5,8,31,37,39 As has been discussed, the use of palliative care in general seems helpful for people re-living trauma at the end of life, as specific approaches show promise. Stepwise communication was effective when trauma survivors had limited time to live, were fatigued or were unwilling to engage in trauma therapy, but this was a single case study with only three participants. 31
Multiple knowledge gaps impede clinical responses to the challenge of care provision for people re-living trauma at the end of life. Clinicians are not adequately trained in how to provide trauma-informed palliative care. 10 There is also a lack of awareness of the commonality of trauma experiences and PTSD in dying patients.4,5,20 Lastly, there is incomplete knowledge of the significant impact that trauma has on dying experiences.4,5 These issues likely exacerbate palliative care teams not adequately seeking a history of trauma in their patients, missing contextual cues and opportunities for appropriate referrals, and resulting in increased suffering and delays in care-focused responses to these issues. 5 A lack of awareness, screening tools, trauma-informed practices and related specific educational interventions contribute to the unmet needs in clinical practice for this high-risk patient group.14,20
Our review highlights other significant gaps in the literature regarding re-living trauma near death in relation to specific populations and essential outcomes. Current published research concentrates on trauma-affected North American male war veterans.30,31,33–37 Studies including women and girls, who are twice as likely to have a history of trauma, are urgently needed.1,2 Indigenous populations, including those from Australia, are often trauma survivors and at risk of developing multiple related co-morbidities.2,17,41–46 These issues, and the pervasive inequity of care provision that many minority groups face, compound the challenges of understanding and meeting needs relating to trauma experiences at the end of life.2,17,41–46 Additionally, the impact of trauma causes other than war and combat requires attention. 2 There is also a lack of understanding about predictive risk factors for re-living trauma near death: for example, are certain types of trauma experiences associated with increased risk of re-living trauma near death? Does a diagnosis of PTSD during the life course increase the risk of re-living trauma near death? Does psychological therapy for PTSD decrease risks, and does a dementia diagnosis increase your chance of re-living trauma near death?
This review also demonstrates the challenges of understanding and responding to trauma experiences at the end of life when these experiences are complicated by other co-morbid conditions. The impacts of ageing and disability on trauma experiences at the end of life are poorly understood. Ageing and its predictable association with reduced mobility and increased disability can decrease a sense of control and increase stress for older people who are trauma survivors. 14 Reduced mobility and increased disability can also lead to feelings of vulnerability that lead to re-emergence or exacerbation of PTSD symptoms. 5 Cognitive impairments such as delirium, and dementia or even the heightened distress of physical pain at the end of life may also lead to mental health issues, including PTSD being overlooked or under-appreciated. 14 In 2021, the leading cause of death for Australian adult females was dementia. 46 However, people with dementia and cognitive impairment continue to be under-represented in end-of-life care research and the receipt of specialist palliative care.30,38,39,47–50 The link between trauma and the development of cognitive impairment like dementia highlights the urgent need to understand better the coexistence of these issues near dying.43,45 The more intense trauma experienced, the greater the risk of developing dementia later in life.4,43,45 Whether this relationship also affects the risks of re-living trauma near death remains unknown. As noted by Kaiser et al., 33 re-living trauma near death can coexist with dementia and/or delirium. The typical exclusion of people with cognitive impairment from end-of-life research needs to be urgently redressed to better understand the impacts of the emerging links between these issues in this vulnerable population, and determine the most appropriate clinical responses to their needs.
Implications for research
Firstly, there is an urgent need to fill research gaps, including how to identify re-living trauma near death for those with or without cognitive impairment. Currently, a validated tool has not been developed and tested for assessing trauma history for patients at the end of life.4,5,37 Secondly, there is an urgent need to fill education and knowledge gaps for clinicians to provide evidence-based trauma-informed practice to support trauma survivors as they die. Prospective studies are needed in the last weeks of life to capture re-living trauma near death.
Implications for practice
This review highlighted that a range of presentations, in conjunction with a known or suspected history of trauma, can be interpreted as ‘trauma cues’ as a constructive clinical activity to better meet patient needs by identifying re-living trauma near death. The ‘trauma cues’ identified in this review include acute severe unexplained pain and dyspnoea.31,39
Limitations of articles included in the review
The research followed a clear and transparent review process, but there are several limitations to point out. Only 11 studies met the inclusion criteria for this review, which identifies that this is an emerging focus for clinicians and researchers. The study designs were heterogeneous, qualitative and quantitative, with participant numbers ranging from 3 to 8752. Findings should be interpreted with caution as only 5/11 had a low risk of bias,33–37 and the majority of participants were war veterans (8/11)30–37 mostly from North America (7/11).30,31,33–37 All 11 studies used PTSD either directly (7/11)31,33–37,39 or indirectly (4/11).30,32,38,40 Only two were intervention studies (graded communication and medical cannabis).31,40
Paradigmatic factors confound attempts to draw coherent conclusions. Most of the studies were conducted in America, and subjects were mostly male military veterans; therefore, possible cultural differences may not be evident. In this review, prospective studies excluded participants with cognitive impairment. None of the studies addressed the experiences of people who did not speak the country’s majority language.
The studies draw strongly on record reviews in veteran hospitals. Most of the studies were descriptive, and few engaged with the experiences of consumers; few interviewed persons dying or undertook case or ethnographic analyses of dying people. As most of the studies were of veterans, most were of older men. Few studies explored interventions.
Conclusion
The findings suggest that re-living trauma near death has additional features that a diagnosis of PTSD cannot explain. These additional features include physical symptoms of severe unexplained pain and dyspnoea, exacerbation of PTSD symptoms even in the absence of a prior PTSD diagnosis, and this happens in the last weeks of life. Further examination that can apprise past trauma identification and trauma-informed interventions is urgently needed to reduce suffering at the end of life for trauma survivors. This examination needs to include participants from all trauma types, including participants with cognitive impairment and women.
Supplemental Material
Supplemental material, sj-docx-1-pcr-10.1177_26323524241277851 for Re-living trauma near death: an integrative review using Grounded Theory narrative analysis by Nikki Johnston, Michael Chapman, Jo Gibson, Catherine Paterson, Murray Turner, Karen Strickland, Wai-Man Liu, Christine Phillips and Kasia Bail in Palliative Care and Social Practice
Supplemental material, sj-docx-2-pcr-10.1177_26323524241277851 for Re-living trauma near death: an integrative review using Grounded Theory narrative analysis by Nikki Johnston, Michael Chapman, Jo Gibson, Catherine Paterson, Murray Turner, Karen Strickland, Wai-Man Liu, Christine Phillips and Kasia Bail in Palliative Care and Social Practice
Acknowledgments
None.
Footnotes
ORCID iDs: Nikki Johnston  https://orcid.org/0000-0003-3057-0787
https://orcid.org/0000-0003-3057-0787
Murray Turner  https://orcid.org/0000-0001-6326-8707
https://orcid.org/0000-0001-6326-8707
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Nikki Johnston, Faculty of Health, University of Canberra, Building 10, 11 Kirinari Street, Bruce, Australia, ACT Health Directorate, Canberra, ACT, Bruce, ACT 2617, Australia; Synergy Nursing and Midwifery Research Centre, Australia; Centre of Ageing Research and Translation, University of Canberra, Bruce, ACT, Australia.
Michael Chapman, Palliative and Supportive Care, Canberra Health Services, Garran, ACT, Australia; School of Medicine and Psychology, Australian National University, Canberra, ACT, Australia; Palliative Care Research Service, Canberra Health Services, Garran, ACT, Australia.
Jo Gibson, Faculty of Health, University of Canberra, Bruce, ACT, Australia.
Catherine Paterson, College of Nursing and Health Sciences, Flinders University, Adelaide, SA, Australia; Central Adelaide Local Health Network, Adelaide, SA, Australia; Robert Gordon University, Aberdeen, Scotland, UK.
Murray Turner, Faculty of Health, University of Canberra, Bruce, ACT, Australia.
Karen Strickland, School of Nursing and Midwifery, Edith Cowan University, Joondalup, WA, Australia; School of Clinical Sciences, Faculty of Health and Environmental Sciences, Auckland University of Technology, Auckland.
Wai-Man Liu, Research School of Finance, Actuarial Studies and Statistics, Australian National University, Canberra, ACT, Australia.
Christine Phillips, School of Medicine and Psychology, Australian National University, Canberra, ACT, Australia.
Kasia Bail, Faculty of Health, University of Canberra, Bruce, ACT, Australia; Synergy Nursing and Midwifery Research Centre, ACT Health Directorate, Canberra, ACT, Australia; Centre of Ageing Research and Translation, University of Canberra, Bruce, ACT, Australia.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Nikki Johnston: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Visualisation; Writing – original draft; Writing – review & editing.
Michael Chapman: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Supervision; Writing – original draft; Writing – review & editing.
Jo Gibson: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Supervision; Writing – original draft; Writing – review & editing.
Catherine Paterson: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Validation; Writing – original draft; Writing – review & editing.
Murray Turner: Conceptualisation; Formal analysis; Investigation; Methodology; Software; Writing – original draft; Writing – review & editing.
Karen Strickland: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Wai-Man Liu: Conceptualisation; Data curation; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Christine Phillips: Conceptualisation; Formal analysis; Investigation; Methodology; Writing – original draft; Writing – review & editing.
Kasia Bail: Conceptualisation; Formal analysis; Investigation; Methodology; Supervision; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Substance Abuse and Mental Health Services Administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014. [Google Scholar]
- 2. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers 2015; 1: 15057. [DOI] [PubMed] [Google Scholar]
- 3. Koenen KC, Ratanatharathorn A, Ng L, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med 2017; 47: 2260–2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ganzel BL. Trauma-informed hospice and palliative care. Gerontologist 2018; 58: 409–419. [DOI] [PubMed] [Google Scholar]
- 5. Meyerson JL, O’Malley KA, Obas CE, et al. Lived experience: a case-based review of trauma-informed hospice and palliative care at a Veterans Affairs Medical Center. Am J Hosp Palliat Med 2023; 40: 329–336. [DOI] [PubMed] [Google Scholar]
- 6. Raja S, Hasnain M, Hoersch M, et al. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health 2015; 38: 216–226. [DOI] [PubMed] [Google Scholar]
- 7. Feldman DB, Vyjeyanthi S, periyokoil MD. Posttraumatic Stress Disorder at End of Life. Journal of Palliative Medicine 2006; 9: 213-218. [DOI] [PubMed] [Google Scholar]
- 8. Asmundson GJG. The emotional and physical pains of trauma: contemporary and innovative approaches for treating co-occurring PTSD and chronic pain. Depress Anxiety 2014; 31: 717–720. [DOI] [PubMed] [Google Scholar]
- 9. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med 2010; 363: 733–742. [DOI] [PubMed] [Google Scholar]
- 10. Feldman DB. Stepwise psychosocial palliative care: a new approach to the treatment of posttraumatic stress disorder at the end of life. J Soc Work End Life Palliat Care 2017; 13: 113–133. [DOI] [PubMed] [Google Scholar]
- 11. Charlson F, van Ommeren M, Flaxman A, et al. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet 2019; 394: 240–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Horesh D, Solomon Z, Zerach G, et al. Delayed-onset PTSD among war veterans: the role of life events throughout the life cycle. Soc Psychiatry Psychiatr Epidemiol 2011; 46: 863–870. [DOI] [PubMed] [Google Scholar]
- 13. Hiskey S, Luckie M, Davies S, et al. The emergence of posttraumatic distress in later life: a review. J Geriatr Psychiatry Neurol 2008; 21: 232–241. [DOI] [PubMed] [Google Scholar]
- 14. Eleff A, Shloush M. Post-traumatic stress disorder and end-of-life care: a well-being review. Am J Hosp Palliat Med 2023; 40: 945–948. [DOI] [PubMed] [Google Scholar]
- 15. Glick DM, Cook JM, Moye J, et al. Assessment and Treatment Considerations for Post Traumatic Stress Disorder at End of Life. Am J Hosp Palliat Care 2018; 35: 1133–1139. 2018/02/22. DOI: 10.1177/1049909118756656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Steel Z, Chey T, Silove D, et al. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 2009; 302: 537–549. [DOI] [PubMed] [Google Scholar]
- 17. Healing Foundation. Working with the Stolen Generations: understanding trauma. Providing effective aged care services to Stolen Generations survivors. Australia. https://healingfoundation.org.au/working-stolen-generations/ (2023, accessed 7 August 2023).
- 18. Probst DR, Wells-Di Gregorio S, Marks DR. Suffering compounded: the relationship between abuse history and distress in five palliative care domains. J Palliat Med 2013; 16: 1242–1248. [DOI] [PubMed] [Google Scholar]
- 19. Fishbain DA, Pulikal A, Lewis JE, et al. Chronic pain types differ in their reported prevalence of post-traumatic stress disorder (PTSD) and there is consistent evidence that chronic pain is associated with PTSD: an evidence-based structured systematic review. Pain Med 2017; 18: 711–735. [DOI] [PubMed] [Google Scholar]
- 20. Riss T. A case report of posttraumatic stress disorder at the end of life. Wiener medizinische Wochenschrift 2022; 172: 184–188. [DOI] [PubMed] [Google Scholar]
- 21. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs 2005; 52: 546–553. [DOI] [PubMed] [Google Scholar]
- 22. Nzabonimpa JP. Quantitizing and qualitizing (im-)possibilities in mixed methods research. Methodol Innovations 2018; 11: 205979911878902. [Google Scholar]
- 23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 2021; 18: e1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Veritas Health Innovation. Covidence systematic review software, www.covidence.org (2023, accessed 12 August 2023).
- 25. Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract 2018; 24: 459–467. [DOI] [PubMed] [Google Scholar]
- 26. Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. Thousand Oaks, CA: SAGE Publications, 1998. [Google Scholar]
- 27. Flick U. An introduction to qualitative research. 7th ed. London: SAGE, 2023. [Google Scholar]
- 28. Mills J, Bonner A, Francis K. The development of constructivist grounded theory. Int J Qual Method 2006; 5: 25–35. [Google Scholar]
- 29. Thorne S. Interpretive description: qualitative research for applied practice. 2nd ed. New York: Routledge, 2016. [Google Scholar]
- 30. Prince-Paul M, Peereboom K, Daly BJ. Confronting mortality: Narratives of military veterans enrolled in home hospice care. Journal of Hospice & Palliative Nursing 2016; 18: 219–226. 2016/07/12. DOI: 10.1097/NJH.0000000000000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Feldman DB, Sorocco KH, Bratkovich KL. Treatment of posttraumatic stress disorder at the end-of-life: application of the Stepwise Psychosocial Palliative Care model. Palliat Support Care 2014; 12: 233–243. [DOI] [PubMed] [Google Scholar]
- 32. O’Connor M, Brennan B, Bloomer MJ, et al. Vulnerability at the end of life: Australian veterans requiring home-based palliative care. Home Health Care Manage Pract 2014; 26: 134–2140. [Google Scholar]
- 33. Kaiser AP, O’Malley K, Moye J, et al. Hopsice and palliative care clinicians’ perceptions of posttraumatic stress disorder at end-of-life in military veterans. Prog Palliat Care 2021; 2021: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kelley-Cook E, Nguyen G, Lee S, et al. Medication needs vary for terminally ill vietnam era veterans with and without a diagnosis of PTSD. Am J Hosp Palliat Care 2016; 33: 625–632. [DOI] [PubMed] [Google Scholar]
- 35. Bickel KE, Kennedy R, Levy C, et al. The relationship of post-traumatic stress disorder to end-of-life care received by dying veterans: a secondary data analysis. J Gen Intern Med 2020; 35: 505–2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kutney-Lee A, Smith D, Griffin H, et al. Quality of end-of-life care for Vietnam-era Veterans: implications for practice and policy. Healthcare 2021; 9: 100494. [DOI] [PubMed] [Google Scholar]
- 37. Alici Y, Smith D, Lu HL, et al. Families’ perceptions of veterans’ distress due to post-traumatic stress disorder-related symptoms at the end of life. J Pain Symptom Manage 2010; 39: 507–514. [DOI] [PubMed] [Google Scholar]
- 38. Akechi T, Okuyama T, Sugawara Y, et al. Major depression, adjustment disorders, and post-traumatic stress disorder in terminally ill cancer patients: associated and predictive factors. J Clin Oncol 2004; 22: 1957–1965. [DOI] [PubMed] [Google Scholar]
- 39. Roth ML, St Cyr K, Harle I, et al. Relationship between pain and post-traumatic stress symptoms in palliative care. J Pain Symptom Manage 2013; 46: 182–191. [DOI] [PubMed] [Google Scholar]
- 40. Casarett DJ, Beliveau JN, Arbus MS. Benefit of tetrahydrocannabinol versus cannabidiol for common palliative care symptoms. J Palliat Med 2019; 22: 1180–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Anderson E, Twiggs C, Goins RT, et al. Nephrology and palliative care providers’ beliefs in engaging American Indian patients in palliative care conversations. J Palliat Med 2022; 25: 1810–1817. [DOI] [PubMed] [Google Scholar]
- 42. Woods JA, Newton JC, Thompson SC, et al. Indigenous compared with non-Indigenous Australian patients at entry to specialist palliative care: Cross-sectional findings from a multi-jurisdictional dataset. PloS one 2019; 14: e0215403-e0215403. DOI: 10.1371/journal.pone.0215403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang TY, Wei HT, Liou YJ, et al. Risk for developing dementia among patients with posttraumatic stress disorder: a nationwide longitudinal study. J Affect Disord 2016; 205: 306–310. [DOI] [PubMed] [Google Scholar]
- 44. Walls ML, Gonzalez J, Gladney T, et al. Unconscious biases: racial microaggressions in American Indian health care. J Am Board Fam Med 2015; 28: 231–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Desmarais P, Weidman D, Wassef A, et al. The interplay between post-traumatic stress disorder and dementia: a systematic review. Am J Geriatr Psychiatry 2020; 28: 48–60. [DOI] [PubMed] [Google Scholar]
- 46. Ahmadi N, Hajsadeghi F, Mirshkarlo HB, et al. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol 2011; 108: 29–33. [DOI] [PubMed] [Google Scholar]
- 47. Zestcott CA, Spece L, McDermott D, et al. Health care providers’ negative implicit attitudes and stereotypes of American Indians. J Racial Ethn Health Disparities 2021; 8: 230–236. [DOI] [PubMed] [Google Scholar]
- 48. Australian Government and Australian Institute of Health and Welfare. Deaths in Australia life expectancy and death, https://www.aihw.gov.au/reports/life-expectancy-deaths-inAustralia/contents/summary (2023, accessed 10 August 2023).
- 49. Walshe C, Todd C, Caress A, et al. Patterns of access to community palliative care services: a literature review. J Pain Symptom Manage 2009; 37: 884–912. [DOI] [PubMed] [Google Scholar]
- 50. Parker D, Lewis J, Gourlay K. Palliative Care and Dementia. A report for Dementia Australia, prepared in collaboration with Palliative Care Australia. Sydney: Dementia Australia, 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pcr-10.1177_26323524241277851 for Re-living trauma near death: an integrative review using Grounded Theory narrative analysis by Nikki Johnston, Michael Chapman, Jo Gibson, Catherine Paterson, Murray Turner, Karen Strickland, Wai-Man Liu, Christine Phillips and Kasia Bail in Palliative Care and Social Practice
Supplemental material, sj-docx-2-pcr-10.1177_26323524241277851 for Re-living trauma near death: an integrative review using Grounded Theory narrative analysis by Nikki Johnston, Michael Chapman, Jo Gibson, Catherine Paterson, Murray Turner, Karen Strickland, Wai-Man Liu, Christine Phillips and Kasia Bail in Palliative Care and Social Practice