Graphical abstract
Some relevant key messages from the first presentation of the 2024 ESC Guidelines for the management of elevated blood pressure (BP) and hypertension.
Keywords: Hypertension, Cardiovascular prevention, Treatment
On August 30, 2024, during the European Society of Cardiology (ESC) congress in London, the new ESC Guidelines for the management of elevated blood pressure (BP) and hypertension were officially presented and offered to the whole cardiovascular community. This 2024 guideline [1], developed by a multidisciplinary task-force, updated the 2018 ESC/ESH guidelines on the management of arterial hypertension [2], using the most robust contemporary evidence, and were mainly aimed at providing new simplified classification of BP, as far as at outlining processes for the diagnosis, evaluation, and management of individuals with elevated BP and hypertension.
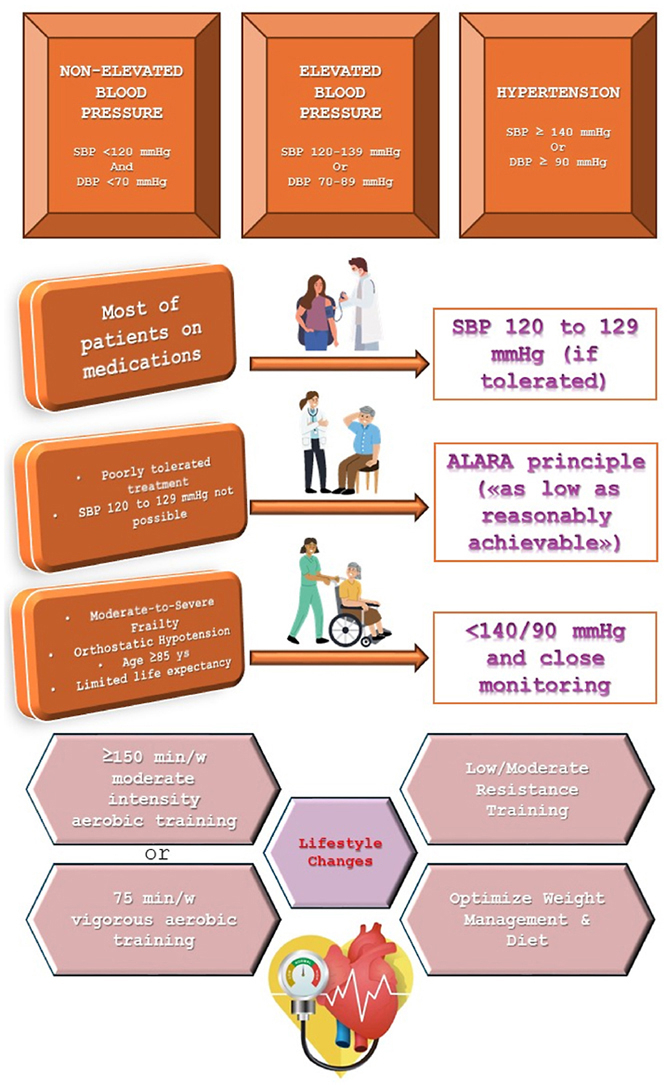
By taking a look on new and revised recommendations, one could get the impression that “between tradition and innovation” may represent the motto of the congress presentation and of guidelines themselves. Indeed, guidelines continue to define hypertension as a systolic BP of at least 140 mmHg and a diastolic BP of at least 90 mmHg, and now include a new category, i.e. elevated BP. This is defined as a systolic BP of 120 mmHg–139 mmHg or a diastolic BP of 70 mmHg–89 mmHg, with strong related recommendation to perform cardiovascular risk assessment to guide treatment, particularly in patients with a BP of at least 130/80 mmHg. From now, we're simply advised to consider 3 categories for BP classification, i.e. non-elevated (<120/70 mmHg), elevated (120 mmHg–139 mmHg/70 mmHg–89 mmHg), and hypertension (≥140/90 mmHg), hopefully to better qualify those patients needing active and optimized treatment. Frequent citation of media after the ESC symposium was as follows: “This new category of elevated BP recognizes that people do not go from normal blood pressure to hypertensive overnight," John William McEvoy, chair of the guidelines task-force, said. "It is, in most cases, a steady gradient of change, and different subgroups of patients — for example, those at a higher risk of developing cardiovascular disease — could benefit from more intensive treatment before their BP reaches the traditional threshold of hypertension." In this perspective, the continuum of cardiovascular risk and prevention activities, as far as the need for tailored intervention, seem to be strongly reaffirmed.
Concerning treatment goals, the 2024 guidelines recommend a more aggressive BP target, since additional evidence are now available confirming the results of the SPRINT trial [3]. The new systolic BP target of 120 mmHg–129 mmHg for most patients receiving antihypertensive medications, if tolerated, represents a major change from the 2018 “130 mmHg” target, and is now more in line with the American guidelines [4]. Another major change is the modification of the 2018 I/A recommendation to target systolic BP to a range of 130–139 mmHg in older patients aged ≥65 years, now converted in a more lenient <140 mmHg target to be considered in pre-treatment, symptomatic, orthostatic hypotension and/or age ≥85 years (IIa/C), as far as in clinically significant, moderate to severe frailty, and/or limited predicted lifespan (IIb/C). Also in this case Europe and America are closer than ever: the absence of tight age cutoffs in both guidelines reduce barriers to treatment and, overall, may favour a more tailored approach based on structured evaluation of conditions such as frailty. On a personal note, and either based on pragmatism of real world experience, easier said than done: everyone knows that in clinical practice it's often hard to estimate life expectancy in an elderly and/or multimorbid patients and that, even before categorization between “light”, “moderate”, or “severe”, the first problem is to appropriately consider frailty per se. Future guidelines on when and how patients with elevated BP or hypertension should be evaluated for frailty are awaited.
Apart from target definition, someone might wonder whether these 2024 ESC guidelines mark the final overcoming of the “stepwise approach” recommended in 2021 ESC guidelines on cardiovascular disease prevention in clinical practice [5]. As is well known, these guidelines recommended an on-treatment systolic BP target of 130–139 mmHg as the first step and then—based on patient preferences, risk, and frailty—to proceed to a systolic BP target of <130 mmHg as the second step. Making a bold statement, new guidelines clearly state that the 2021 approach “will not be considered reasonable to those who follow the updated 2024 ESC recommendations”, and that “it is well established that an on-treatment systolic BP of 135 mmHg is not optimal relative to more intensive control”. Anyway, the stepwise approach probably was not as widespread as due, since many cardiologists seem to prefer an intensive and rapidly performed treat-to-target approach.
A final commentary could be inspired by “new” suggested lifestyle changes, particularly the updated recommendation of 75 min of vigorous intensity aerobic exercise per week over 3 days as an alternative to the previous recommendation of at least 30 min of moderate dynamic exercise on 5–7 days/week, to be complemented with low- or moderate-intensity resistance training two to three times a week. That's doesn't feel especially new, since anyone working in the field of cardiovascular rehabilitation and prevention knows that high intensity exercise – especially in form of aerobic interval training with equivalent energy expenditure to endurance training – could be considered in selected patients, and that resistance/strength training is a fundamental complementary tool to improve cardiovascular prognosis [6]. Moreover, as the case of frailty, this clear sentence doesn't run out all questions, since it's not always intuitive to identify intensity domains for aerobic and strength training, especially in clinical settings with no possibility to provide direct testing. Hopefully, having included this topic among major caveats of guidelines will give more emphasis on non-pharmacologic treatments – surely less impressive than modern invasive procedures such as renal denervation, now considered in 2024 guidelines for patients with resistant hypertension – but probably much more feasible and cost-effective.
CRediT authorship contribution statement
Marco Ambrosetti: Conceptualization, Supervision, Validation, Writing – original draft, Writing – review & editing. Monica Loguercio: Writing – original draft, Writing – review & editing. Luigi Maresca: Writing – original draft, Writing – review & editing. Chiara Meloni: Writing – original draft, Writing – review & editing. Daniela Zaniboni: Writing – original draft, Writing – review & editing.
Handling editor: D Levy
References
- 1.McEvoy J.W., McCarthy C.P., Bruno R.M., Brouwers S., Canavan M.D., Ceconi C., Christodorescu R.M., Daskalopoulou S.S., Ferro C.J., Gerdts E., Hanssen H., Harris J., Lauder L., McManus R.J., Molloy G.J., Rahimi K., Regitz-Zagrosek V., Rossi G.P., Sandset E.C., Scheenaerts B., Staessen J.A., Uchmanowicz I., Volterrani M., Touyz R.M., ESC Scientific Document Group 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur. Heart J. 2024 Aug;30 doi: 10.1093/eurheartj/ehae178. Epub ahead of print. PMID: 39210715. [DOI] [PubMed] [Google Scholar]
- 2.Williams B., Mancia G., Spiering W., Agabiti Rosei E., Azizi M., Burnier M., Clement D.L., Coca A., de Simone G., Dominiczak A., Kahan T., Mahfoud F., Redon J., Ruilope L., Zanchetti A., Kerins M., Kjeldsen S.E., Kreutz R., Laurent S., Lip G.Y.H., McManus R., Narkiewicz K., Ruschitzka F., Schmieder R.E., Shlyakhto E., Tsioufis C., Aboyans V., Desormais I., Authors/Task Force Members 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of Cardiology and the European society of hypertension: the task force for the management of arterial hypertension of the European society of Cardiology and the European society of hypertension. J. Hypertens. 2018 Oct;36(10):1953–2041. doi: 10.1097/HJH.0000000000001940. Erratum in: J Hypertens. 2019 Jan;37(1):226. doi: 10.1097/HJH.0000000000002017. PMID: 30234752. [DOI] [PubMed] [Google Scholar]
- 3.Sprint Research Group, Wright JT Jr, Williamson J.D., Whelton P.K., Snyder J.K., Sink K.M., Rocco M.V., Reboussin D.M., Rahman M., Oparil S., Lewis C.E., Kimmel P.L., Johnson K.C., Goff D.C., Jr., Fine L.J., Cutler J.A., Cushman W.C., Cheung A.K., Ambrosius W.T. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2015 Nov 26;373(22):2103–2116. doi: 10.1056/NEJMoa1511939. Epub 2015 Nov 9. Erratum in: N Engl J Med. 2017 Dec 21;377(25):2506. doi: 10.1056/NEJMx170008. PMID: 26551272; PMCID: PMC4689591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whelton P.K., Carey R.M., Aronow W.S., Casey D.E., Jr., Collins K.J., Dennison Himmelfarb C., DePalma S.M., Gidding S., Jamerson K.A., Jones D.W., MacLaughlin E.J., Muntner P., Ovbiagele B., Smith S.C., Jr., Spencer C.C., Stafford R.S., Taler S.J., Thomas R.J., Williams KA Sr, Williamson J.D., Wright J.T., Jr. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2017;71(6):e13–e115. doi: 10.1161/HYP.0000000000000065. Epub 2017 Nov 13. Erratum in: Hypertension. 2018 Jun;71(6):e140-e144. doi: 10.1161/HYP.0000000000000076. PMID: 29133356. [DOI] [PubMed] [Google Scholar]
- 5.Visseren F.L.J., Mach F., Smulders Y.M., Carballo D., Koskinas K.C., Bäck M., Benetos A., Biffi A., Boavida J.M., Capodanno D., Cosyns B., Crawford C., Davos C.H., Desormais I., Di Angelantonio E., Franco O.H., Halvorsen S., Hobbs F.D.R., Hollander M., Jankowska E.A., Michal M., Sacco S., Sattar N., Tokgozoglu L., Tonstad S., Tsioufis K.P., van Dis I., van Gelder I.C., Wanner C., Williams B., ESC National Cardiac Societies; ESC Scientific Document Group ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021;42(34):3227–3337. doi: 10.1093/eurheartj/ehab484. Erratum in: Eur Heart J. 2022 Nov 7;43(42):4468. doi: 10.1093/eurheartj/ehac458. PMID: 34458905. [DOI] [PubMed] [Google Scholar]
- 6.Hansen D., Abreu A., Ambrosetti M., Cornelissen V., Gevaert A., Kemps H., Laukkanen J.A., Pedretti R., Simonenko M., Wilhelm M., Davos C.H., Doehner W., Iliou M.C., Kränkel N., Völler H., Piepoli M. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: why and how: a position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022 Feb 19;29(1):230–245. doi: 10.1093/eurjpc/zwab007. Erratum in: Eur J Prev Cardiol. 2023 Dec 22:zwad397. doi: 10.1093/eurjpc/zwad397. PMID: 34077542. [DOI] [PubMed] [Google Scholar]


