Abstract
Background and objective
Deciduous teeth portray less pain sensitivity in comparison to permanent teeth. Conventional vitality tests depend on the stimulation of nerve fibers. Loss of sensory function due to trauma can result in negative responses. Unpleasant painful stimuli may lead to apprehensiveness and require behavior management in children. This study is a genuine attempt to compare pulp oxygen saturation levels of deciduous posterior teeth clinically or radiographically diagnosed as reversible pulpitis (RP), irreversible pulpitis (IRP), and pulpal necrosis (PN) with healthy teeth using a pulse oximeter with probes in preoperative and postoperative conditions.
Methods
A total of 120 deciduous posterior teeth from participants aged 4–9 years were evaluated using random stratified sampling, divided into four groups with 30 teeth each based on clinical and radiological interpretation—group I: noncarious (NC) (control group); group II: RP; group III: IRP; group IV: PN. Teeth from children meeting the inclusion criteria were recorded and examined. The data obtained were sent for statistical analysis.
Results
A significant difference in pulp oxygenation rates was observed between teeth with pulpal pathologies and healthy teeth in both preoperative and postoperative conditions.
Interpretation and conclusion
Pulpal diseases cause a reduction in oxygen saturation of the pulp vasculature, thereby affecting the vitality of the tooth. The pulse oximeter used in the neonatal intensive care unit (ICU) was suitable for determining SpO2% in children.
Clinical significance
Pedodontists face challenges in making diagnoses because children may provide false-positive or false-negative responses to stimuli or questions. Pulse oximetry is a boon as it is highly efficient, can be used chairside, is completely atraumatic, and eco-friendly.
How to cite this article
Betal SK, Singh S, Dasgupta B. Analysis of the Pulp Oxygenation Rate by Pulse Oximeter in Children with Pulpal Diseases. Int J Clin Pediatr Dent 2024;17(5):576-579.
Keywords: Healthy tooth, Irreversible pulpitis, Pulpal necrosis, Pulse oximeter, Reversible pulpitis, SpO2%
Introduction
Dental pulp is housed in the center of each tooth and consists of connective tissues, nerves, and blood vessels. The average lifespan of deciduous pulp, functioning in the oral cavity, is about 8–8.3 years.1 Deciduous teeth portray less pain sensitivity in comparison to permanent teeth resulting from differences in the number or innervations of the neural component such as Raschkow plexus.1 The pulp of primary teeth is composed of a less dense network of myelinated fibers. Moreover, nerve fibers are rarely found in the calcified structure of deciduous teeth.1
Pulp vitality is of great importance for diagnosing pulpal diseases and planning treatment with a good prognosis. The pulp-dentin complex is richly innervated by sensory fibers, predominantly A-delta and C fibers. Most vitality tests in everyday practice, such as the electric pulp test or thermal pulp test, depend on stimulating these nerve fibers.2 Electrical pulp testing excites C fibers, whereas thermal sensitivity testing primarily excites A-delta fibers. Loss of sensory function within the pulp results in negative responses to thermal and electrical pulp sensitivity testing, which is common in traumatic injuries.3 Sensitivity tests are perceived as unpleasant and occasionally painful stimuli, which may lead to cooperation problems and require behavior management in the pediatric population.4
The evaluation of the blood supply is the most certain determinant of pulp vitality which is performed by pulse oximetry. It is a physiometric, objective method based on spectrophotometry and photoplethysmography3 that reads the oxygenation rate (SpO2%) of the pulp by its vascular supply. It is a noninvasive and user-friendly device. One arm of the device sensor consists of light emitting diodes (red light: 640 nm and infrared light: 900 nm). Light transmission occurs through the arteries of the pulp and is received by a photodetector on the other arm. Oxygenated hemoglobin and deoxygenated hemoglobin flowing through the vasculature absorb the emitted red and infrared light. The pulsatile changes in blood flow cause fluctuations in absorption, which determine the oxygen saturation of arterial blood (Fig. 1).5
Fig. 1:
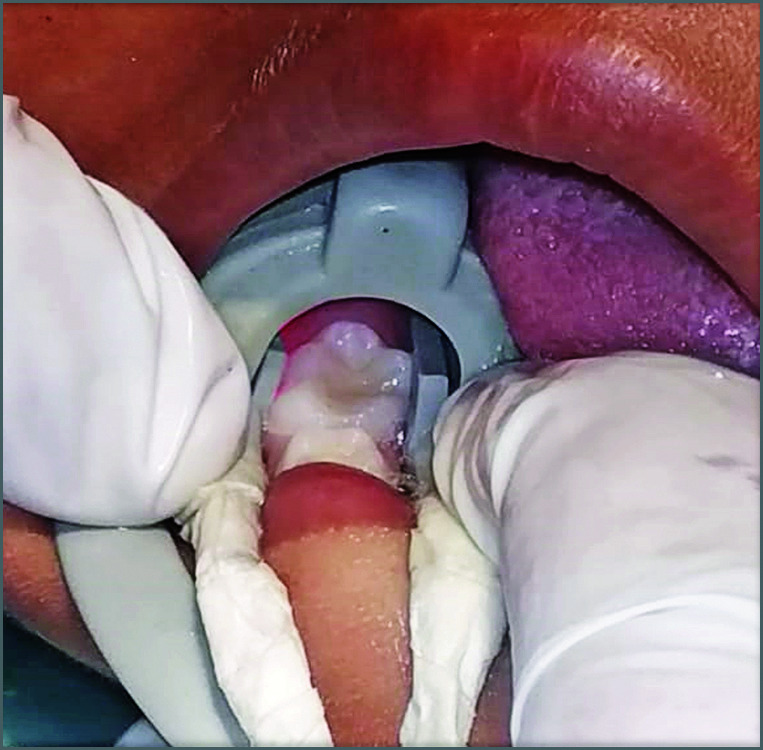
Placement of the probe on the teeth
A normal person has 15 gm of hemoglobin in each 100 mL of blood, and each gram transports 1.34 mL of oxygen, resulting in 20 mL of oxygen in 100 mL of blood. With proper monitoring, changes in oxygen saturation of pulpal blood flow can be detected using a pulse oximeter. This method can be utilized to detect pulpal inflammation or pulpal necrosis (PN) in teeth.6 The pulse oximeter has proven to provide very accurate results by measuring pulp oxygenation rates and providing SpO2%, which is used to diagnose pulpal inflammation and determine the mode of treatment.
There is a plethora of literature focusing on the efficacy of pulse oximetry in measuring oxygen saturation levels of vital, nonvital, and immature permanent teeth. It is established that pulse oximetry is a significant and trustworthy vitality testing device compared to electric pulp testers and thermal pulp testers.2
Studies were also conducted to assess pulp oxygen saturation levels in permanent teeth with various types of pulpal inflammations.2 However, there is no concrete data available showing the differences in stages of pulp inflammation in deciduous teeth using a pulse oximeter. Hence, this study is a genuine attempt to compare pulp oxygen saturation levels of deciduous posterior teeth diagnosed clinically or radiographically as reversible pulpitis (RP), irreversible pulpitis (IRP), and PN with carious teeth using pulse oximeter probes.
Aims and Objectives
To assess the pulp oxygenation level of different inflamed deciduous teeth.
To correlate the pulpal oxygenation rate with various inflammatory pulpal conditions.
To analyze the difference in pulp oxygenation rates between teeth with pulpal pathologies and healthy teeth.
To analyze the difference in pulp oxygenation rates between teeth with pulpal pathologies in preoperative and postoperative conditions.
To determine the potential use of the pulse oximeter used in neonatal intensive care unit (ICU) for checking pulpal SpO2 values in deciduous molars.
Methods of Data Collection
A total of 120 deciduous posterior teeth from participants aged 4–9 years were evaluated using stratified sampling, divided into four groups of 30 teeth each based on clinical and radiological interpretation.
Group I— NC: Non carious molars (Control Group).
Group II—RP: Molars presenting reversible pulpitis.
Group III—IRP: Molars presenting irreversible pulpitis.
Group IV—PN: Molars presenting pulpal necrosis.
Inclusion Criteria
Children aged 4–9 years who were cooperative (rating 3 and 4 on the Frankl scale).
Children with NC posterior teeth, carious posterior teeth with pulpal disease, teeth with periapical abscess or sinus opening, and nonvital teeth.
Children with informed parental consent.
Exclusion Criteria
Children with mental and physical disabilities.
Children suffering from systemic disorders.
Teeth affected by dental trauma.
Children undergoing orthodontic treatment.
Children presenting with extraoral swelling.
Methodology
Participants aged 4–9 years with carious deciduous posterior teeth were selected using a stratified sampling procedure.
A total of 120 posterior teeth were categorized into four groups based on the extent of caries progression clinically and radiographically.
Medical and dental histories were recorded, and oral prophylaxis was performed for every participant.
Children were given time to relax and interact with investigators to achieve full cooperation during data collection.
Preoperative Reading
The probes of the pulse oximeter were placed on the sample teeth.
Three readings shown by the pulse oximeter were recorded at intervals of 30 seconds each.
After recording, the required treatment procedures were carried out for teeth with pulpal pathologies.
Postoperative Reading
After the required treatment procedure, three postoperative readings were recorded on the sample tooth with pulpal pathology at intervals of 30 seconds each.
Further treatment procedures, if required, were carried out afterward.
All the collected data were subjected to statistical analysis.
Results and Discussion
A pediatric dentist faces challenges in the clinic when making diagnoses and determining prognosis. In such cases, diagnostic tools for pulp diseases are invaluable. Various tools are utilized to accurately diagnose pathology, assess pulp vitality, and determine treatment methods. Despite numerous technological advancements available today, they can be unreliable when used on children, often yielding false negative findings due to the child's inability to respond consistently.
A more recent idea is the pulse oximeter, which detects the amount of oxygen in the blood as it flows through blood arteries. According to Goho's writings,6 the tooth's vascularity has a direct impact on the pulp's vitality. If only the neural component of the pulp is injured, it may test as nonvital even when the vasculature is intact. This situation commonly occurs with newly damaged teeth. Unlike vascular tissue, pulp nerve fibers are more resistant to necrosis. Testing the neural response alone using heat or electric methods may also yield false-positive results if only the pulp vasculature is compromised. Assessing oxygen saturation levels with pulse oximetry provides a proven, noninvasive, direct, and entirely objective approach for evaluating vascular health.7
The probes of the Nellcor GE OxiMax Open “Y” type SpO2 sensor were attached to the probe holder designed for use in neonatal ICUs. They were then positioned on the tooth surface in accordance with the literature.
Jubran8 emphasized that the accurate measurement of SpO2% is influenced by the specific probes attached to a pulse oximeter. Ear probes typically provide a more accurate average on the screen and are more responsive to variations in blood oxygen saturation. Calil et al. and Goho's higher SpO2 results compared to Sharma et al. and Bargrizan et al. could be explained by the fact that they employed ear probes.6,9–11
Our research is in close approximation to Shahi et al.12 and Mazumdar et al.13 Shahi et al.12 found that pulse oximetry can be utilized as a standard procedure for determining the vitality of the pulp in primary, young permanent and mature permanent teeth. Mazumdar et al.13 also mentioned that a pulse oximeter can not only distinguish between vital and nonvital teeth, but it can also predict the severity of pulpal inflammation. This study also demonstrated that there was no correlation between pulpal and systemic oxygen saturation rates. With rising pulpal inflammation, there was a decline in pulpal oxygen saturation.
Pulse oximetry, dual-wavelength spectrophotometry, and laser Doppler flowmetry are techniques used to measure pulpal blood flow. Dual-wavelength spectrophotometry has been examined only in laboratory settings, where it detects the presence of hemoglobin in blood but does not measure blood circulation.5 Laser Doppler flowmetry is unfortunately not practical for dental practices because it takes around an hour to create recordings.14 It is not reproducible, expensive, and the probe moves around uncontrollably. When compared to heat tests, cold tests, and electric pulp tests, the diagnostic accuracy with a pulse oximeter was shown to be much greater, according to Janani et al.'s analysis.15
Analysis of variance (ANOVA) was used to determine the significance of oxygen saturation among all groups in pre- and posttreatment conditions (Table 1), showing the comparison of pulp oxygenation levels among all study groups before treatment. The mean and standard deviation for each group were as follows: group I (NC) was 95.4 ± 0.7; group II (RP) was 91.5 ± 1.35; group III (IRP) was 89.3 ± 1.26; group IV (PN) was 86.9 ± 1.92. The derived F-value is 200.3, indicating that the test is highly significant. Pulp oxygenation levels in each pathological condition are observed to be reduced compared to healthy teeth and to each other, as the pathology affects the vasculature of the tooth. Table 2 shows multiple pairwise comparisons of pulp oxygenation levels before treatment between different study groups using Tukey's post hoc test, with group I (NC), group II (RP), group III (IRP), and group IV (PN). Comparisons among the four groups in the preoperative condition resulted in a highly significant evaluation, with a p-value < 0.001.
Table 1:
Comparison of pulp oxygenation level among all the study groups before the treatment using ANOVA test
| Serial number | Study groups | Pulp oxygenation level before treatment (mean ± SD) | F-value | p-value |
|---|---|---|---|---|
| 1. | Group I (NC): Molars without any caries (control group) | 95.4 ± 0.7 | 200.3 | 0.000 (p < 0.001) very highly significant |
| 2. | Group II (RP): Molars for the RP | 91.5 ± 1.35 | ||
| 3. | Group III (IRP): Molars for the IRP | 89.3 ± 1.26 | ||
| 4. | Group IV (PN): Molars for the PN | 86.9 ± 1.92 |
Table 2:
Multiple pairwise comparison of pulp oxygenation level before treatment between different study groups using Tukey's post hoc test
| Serial number | Group | Compared with | p-value after applying Tukey's post hoc test |
|---|---|---|---|
| 1. | Group I (NC) | Group II (RP) | 0.000 (p < 0.001) [Vickers hardness scale (VHS)] |
| Group III (IRP) | 0.000 (p < 0.001) (VHS) | ||
| Group IV (PN) | 0.000 (p < 0.001) (VHS) | ||
| 2. | Group II (RP) | Group I (NC) | 0.000 (p < 0.001) (VHS) |
| Group III (IRP) | 0.000 (p < 0.001) (VHS) | ||
| Group IV (PN) | 0.000 (p < 0.001) (VHS) | ||
| 3. | Group III (IRP) | Group I (NC) | 0.000 (p < 0.001) (VHS) |
| Group II (RP) | 0.000 (p < 0.001) (VHS) | ||
| Group IV (PN) | 0.000 (p < 0.001) (VHS) | ||
| 4. | Group IV (PN) | Group I (NC) | 0.000 (p < 0.001) (VHS) |
| Group II (RP) | 0.000 (p < 0.001) (VHS) | ||
| Group III (IRP) | 0.000 (p < 0.001) (VHS) |
Table 3 shows the comparison of pulp oxygenation level among all the study groups after the treatment using ANOVA test where mean and standard deviation (SD) for group I (NC) is 95.4 ± 0.7; group II (RP) is 89.6 ± 1.09; group III (IRP) is 0.000 ± 0.000; group IV (PN) is 0.000 ± 0.000. Derived F-value is 204351.8 and as per result, the test is very highly significant. In postoperative condition also, there is reduction in the oxygen saturation of RP in comparison to the healthy tooth. In cases of group III and group IV, the valuation is zero as pulpectomy procedure is already performed as the pulps were already extirpated. Table 4 shows multiple pairwise comparison of pulp oxygenation level before treatment between different study groups using Tukey's post hoc test where group I (NC), group II (RP) in comparison to the other three groups provide a very highly significant result. Group III (IRP) and group IV (PN) in comparison to group I (NC) and group II (RP) provide very highly significant result but on comparison group III (IRP) to group IV (PN) and group IV (PN) to group III (IRP) provides a nonsignificant result as after pulpectomy procedure there is no vasculature present in the pulp chamber.
Table 3:
Comparison of pulp oxygenation level among all the study groups after the treatment using ANOVA test
| Serial number | Study groups | Pulp oxygenation level after treatment (mean ± SD) | F-value | p-value |
|---|---|---|---|---|
| 1. | Group I (NC): Molars without any caries (control group) | 95.4 ± 0.7 | 204351.8 | 0.000 (p < 0.001) very highly significant |
| 2. | Group II (RP): Molars for the RP | 89.6 ± 1.09 | ||
| 3. | Group III (IRP): Molars for the IRP | 0.000 ± 0.000 | ||
| 4. | Group IV (PN): Molars for the PN | 0.000 ± 0.000 |
Table 4:
Multiple pairwise comparison of pulp oxygenation level before treatment between different study groups using Tukey's post hoc test
| Serial number | Group | Compared with | p-value after applying Tukey's post hoc test |
|---|---|---|---|
| 1. | Group I (NC) | Group II (RP) | 0.000 (p < 0.001) (VHS) |
| Group III (IRP) | 0.000 (p < 0.001) (VHS) | ||
| Group IV (PN) | 0.000 (p < 0.001) (VHS) | ||
| 2. | Group II (RP) | Group I (NC) | 0.000 (p < 0.001) (VHS) |
| Group III (IRP) | 0.000 (p < 0.001) (VHS) | ||
| Group IV (PN) | 0.000 (p < 0.001) (VHS) | ||
| 3. | Group III (IRP) | Group I (NC) | 0.000 (p < 0.001) (VHS) |
| Group II (RP) | 0.000 (p < 0.001) (VHS) | ||
| Group IV (PN) | 1.00 (p > 0.05) [not significant (NS)] | ||
| 4. | Group IV (PN) | Group I (NC) | 0.000 (p < 0.001) (VHS) |
| Group II (RP) | 0.000 (p < 0.001) (VHS) | ||
| Group III (IRP) | 1.00 (p > 0.05) (NS) |
Our study yielded highly significant results in each category of comparison among oxygen saturation levels in pre- and post-condition pulpal inflammation, as well as in comparisons of oxygen saturation levels among each group.
Conclusion
Significant differences in pulp oxygenation rates were observed between teeth with pulpal pathologies and healthy teeth in both preoperative and postoperative conditions. There was also a notable decrease in oxygen saturation when pathological conditions were compared to healthy teeth. Comparing RP, IRP, and PN, a decreased value of SpO2% was evident. The pulse oximeter used in the neonatal ICU was effective in determining SpO2% levels.
With this study, we conclude that pulpal diseases lead to a reduction in oxygen saturation in the vasculature of the pulp, thereby affecting the vitality of the tooth. In the pediatric population, pulse oximetry proves to be beneficial as it is completely atraumatic and environmentally friendly in nature.
Orcid
Sumit Kumar Betal https://orcid.org/0009-0001-8862-7486
Swati Singh https://orcid.org/0009-0004-1768-3140
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Rapp R, Avery JK, Stracham DS. The distribution of nerves in human primary teeth. Anat Rec. 1967;159:89–103. doi: 10.1002/ar.1091590113. [DOI] [PubMed] [Google Scholar]
- 2.Anusha B, Madhusudhana K, Chinni SK, et al. Assessment of pulp oxygen saturation levels by pulse oximetry for pulpal diseases—a diagnostic study. J Clin Diag Res. 2017;11(9):ZC36–ZC39. doi: 10.7860/JCDR/2017/28322.10572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Setzer FC, Katoka SH, Natrielli F, et al. Clinical diagnosis of pulp inflammation based on pulp oxygenation rates measured by pulse oximetry. J Endod. 2012;38(7):880–883. doi: 10.1016/j.joen.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 4.Pozzobon MH, de Sousa Vieira R, Alves AMH, et al. Assessment of pulp blood flow in primary and permanent teeth using pulse oximetry. Dent Traumatol. 2011;27:184–188. doi: 10.1111/j.1600-9657.2011.00976.x. [DOI] [PubMed] [Google Scholar]
- 5.Gopikrishna V, Tinagupta K, Kandaswamy D. Evaluation of efficacy of a new custom-made pulse oximeter dental probe in comparison with the electrical and thermal tests for assessing pulp vitality. J Endod. 2007;33:411–414. doi: 10.1016/j.joen.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Goho C. Pulse oximetry evaluation of vitality in primary and immature permanent teeth. Pediatr Dent. 1999;21:125–127. [PubMed] [Google Scholar]
- 7.Noblett WC, Wilcox LR, Scamman F, et al. Detection of pulpal circulation in vitro by pulse oximetry. J Endod. 1996;22(1):1–5. doi: 10.1016/S0099-2399(96)80226-3. [DOI] [PubMed] [Google Scholar]
- 8.Jubran A. Pulse oximetry. Crit Care. 1999;3(2):R11–R17. doi: 10.1186/cc341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bargrizan M, Ashari MA, Ahmadi M, et al. The use of pulse oximetry in evaluation of pulp vitality in immature permanent teeth. Dent Traumatol. 2016;32:43–47. doi: 10.1111/edt.12215. [DOI] [PubMed] [Google Scholar]
- 10.Sharma DS, Mishra S, Banda NR, et al. In vivo evaluation of customized pulse oximeter and sensitivity pulp tests for assessment of pulp vitality. J Clin Ped Dent. 2019;43(1):11–15. doi: 10.17796/1053-4625-43.1.3. [DOI] [PubMed] [Google Scholar]
- 11.Calil E, Caldeira CL, Gavini G, et al. Determination of pulp vitality in vivo with pulse oximetry. Int Endod J. 2008;41:741–746. doi: 10.1111/j.1365-2591.2008.01421.x. [DOI] [PubMed] [Google Scholar]
- 12.Shahi P, Sood P B, Sharma A, et al. Comparative study of pulp vitality in primary and young permanent molars in human children with pulse oximeter and electric pulp tester. Int J ClinPediatr Dent. 2015;8(2):94–98. doi: 10.5005/jp-journals-10005-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mazumdar P, Bhattacharya S. An in vivo study on the reliability of using a modified pulse oximeter for chair side determination of pulpal inflammatory status. Res Sq. 2022:1–20. doi: 10.21203/rs.3.rs-1866007/v1. [DOI] [Google Scholar]
- 14.Polat S, Er K, Polat NT. Penetration depth of laser Doppler flowmetry beam in teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1):125–129. doi: 10.1016/j.tripleo.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Janani K, Ajitha P, Sandhya R, et al. Efficiency of new custom-made pulse oximeter sensor holder in assessment of actual pulp status. J Family Med Prim Care. 2020;9:3333–3337. doi: 10.4103/jfmpc.jfmpc_73_20. [DOI] [PMC free article] [PubMed] [Google Scholar]


