Abstract
Background
We aimed to ascertain the current state of and needs for virtual reality (VR)-based simulation training in the care of adult respiratory patients. Learning to care for patients with infectious respiratory disease is crucial in nurses’ practical education. Thus, studies on the state of VR-based simulation-training are required.
Methods
We used an explanatory sequential mixed-methods design. The sample included 122 new nurses at two advanced general hospitals and five educators at a nursing college. The educational needs of virtual reality-based simulation education were measured by the tool developed in this study. Research data were collected from August 31 to September 26, 2022. Quantitative data were subjected to a descriptive analysis, while qualitative data were subjected to content analysis.
Results
The new nurses in this study had a mean age of 24.51 years and total clinical experience of 11.18 months; 82.8% of the participants had experience in adult respiratory patient care, and 94.3% were aware of the need for this training. In the qualitative data analysis of six new nurses, all participants had experience with simulation training and were aware of its need. Moreover, all participants wanted repeated VR-based simulation training using real clinical cases. Regarding the qualitative data analysis of five nursing college educators, most of them had experience providing and receiving simulation training, and they were aware of its need in caring for respiratory patients. They reported the need for VR learning spaces that reflect the clinical environment, alongside sufficient duration and frequency of learning. Our findings could help develop simulation training programs for nursing students to assist adult respiratory patients.
Conclusions
We provide a basis for developing VR-based simulation training for respiratory care by studying the current state of and demand for nurses’ VR-based simulation training. The results can contribute to improving the quality of nursing for adult respiratory patients.
Keywords: Virtual reality, Simulation training, Nursing students, Education
Background
The World Health Organization [1] declared the need to reassess the efficacy of previous methods and to implement a paradigm shift in the education of public health workers. In particular, nursing students require both theoretical and specialized practical education. Theoretical knowledge about various diseases and practical clinical skills includes core competencies [2], which nursing students acquire through general education in nursing colleges. Specialized practical education includes education in practice rooms at school and clinical education in the field; various teaching methods can be combined with practical education, including simulation training.
When caring for diverse patients in clinical settings, nurses must display critical problem-solving abilities and holistic thinking. Multidisciplinary interventions involving cooperation with fellow nurses and other medical personnel are thus necessary and require good communication and teamwork. However, emphasis on the awareness of patient safety and rights in the modern medical field limits students’ ability to practice direct nursing and other nursing skills in real clinical situations. Further, with the onset of the coronavirus disease (COVID-19) pandemic in January 2020, severe restrictions regarding practical education in clinical environments and practice rooms [3, 4] were imposed at nursing colleges in South Korea. Quarantine guidelines, such as social distancing, prompted a shift to revolutionary teaching methods from traditional ones, which became insufficient for holding classes and following curricula [5].
Restricted practical instruction negatively impacts nursing students’ education [3]. During the COVID-19 pandemic, many nursing colleges in South Korea responded to the limitations on practical teaching by implementing various alternative methods, including clinical practice in school and online practical content like vSim® for Nursing (Laerdal Medical & Wolters Kluwer Health) [6]; simulation training played a key role in this process [4]. Advances in simulation training designed to closely resemble real clinical environments have allowed students to gain repeated, indirect practical experience in a safe learning environment at school. Simulation training includes partial models, role-playing, high-fidelity simulator, and standard patients (SPs). Recent advances in simulation training include integration with virtual reality (VR), augmented reality (AR), and mixed reality (MR). While simulation training at nursing colleges has traditionally used high-fidelity simulators, further advances have led to the emergence of VR-based simulation training with expanding applications [7, 8].
VR is defined as “the sum of the hardware and software systems that seek to perfect an all-inclusive, sensory illusion of being present in another environment” [9, p. 63]. VR provides an immersive three-dimensional experience capable of replicating reality with high fidelity or transporting users to entirely fictional environments [10]. VR also uses 360-degree video for detailed, accurate depictions that feel realistic, giving users the sensation of actually being in the place being depicted. VR is related to the concepts of AR and MR. AR, which is a subdomain of VR, is a computer graphics technique in which a set of virtual objects or information is generated and made to appear as if they were present within a real environment. Through AR, users can easily and immediately use diverse content according to the situation. By stimulating users’ vision, hearing, and proprioception, AR provides users with the most immersive experience of virtual worlds [11]. The use of AR in education provides learners with a sense of immersion. Its ability to let users view objects close-up has been utilized in diverse fields, including entertainment and education [11, 12]. Regarding higher education in the field of healthcare, VR and AR are used mostly for fire safety [13], medical education [14], and nursing education [15, 16], especially in practical learning. VR and AR are also used in biomedical science [17], biology, geology education [18], and art education [11] for purposes such as pathology VR, neuron tracing, vision VR, surgery, anatomy, and telemedicine. With AR being used more in education, the time is opportune for the systematic implementation and enhancement of practical education using these advanced technologies. However, in Korea, simulation education using VR is still in its beginning stages [19].
In 2021, the third leading cause of death in South Korea after cancer and cardiac disease, was pneumonia which is a representative infectious respiratory disease [20]. In nursing colleges, simulation training is based on various scenarios. Depending on the specific subdomain of nursing education, different patient scenarios have been developed and employed, including pediatric, maternity, adult, geriatric, community, and psychiatric nursing. Experts are warning of the possibility of infectious respiratory disease occurring in the future. Teaching students in adult nursing to care for patients with infectious respiratory disease can help them develop specific abilities they are likely to apply frequently in real clinical settings. Thus, the development of respiratory nursing education using simulation needs to be continued and strengthened.
In nursing education, VR-based practice is used for both curricular and extracurricular applications [4]. Moreover, it is expected to have strong applicability and educational efficacy in the future. Given their ability to improve nursing students’ learning attitudes, critical thinking [3], and clinical competence, simulation-based classes should continue to be studied and utilized in education [16]. Several previous studies have examined VR-based simulation: experiences of practical education using virtual and high-fidelity simulation [21]; effects on nursing competency [2]; problem-solving ability and nursing self-confidence [16]; effects on knowledge of the hospital environment, academic self-efficacy, learning immersion, satisfaction in education, and academic achievement [22]; and experiences of VR simulation practice [5]. Lee and Ryu also applied VR to develop a program to strengthen clinical decision-making ability for patients with respiratory problems, focusing on the measurement of oxygen saturation and oxygen therapy using a nasal cannula [21].
However, there is still a shortage of studies investigating the current state of and demand for VR-based simulation training for the care of respiratory patients by nursing students. Needs refer to the difference between the learner’s current level and the level to be reached [23]. Educational needs serve as an indicator that identifies the current level and desirable level of perception regarding a certain content; they can be considered a standard for judging the degree of educational requirements [24]. In order to develop a higher education program, an analysis of learner needs assessment must be conducted first. Thus, this study aimed to ascertain the current state of and needs for VR-based education in the care of adult respiratory patients among a group of new nurses working at two advanced general hospitals and a group of educators working at a nursing college. Our findings will provide data to support the development of VR-based training programs for nursing students in the care of adult respiratory patients.
Methods
Design
This study used an explanatory sequential mixed-methods design. Figure 1 depicts the research flowchart. This study followed a three-step process. First, we developed the educational need questionnaire through an extensive literature review. Second, we collected quantitative data using the developed questionnaire and supplemented it with qualitative insights obtained through personal interviews to ensure a comprehensive analysis. Lastly, we analyzed the needs assessment, synthesizing findings from both quantitative and qualitative data.
Fig. 1.
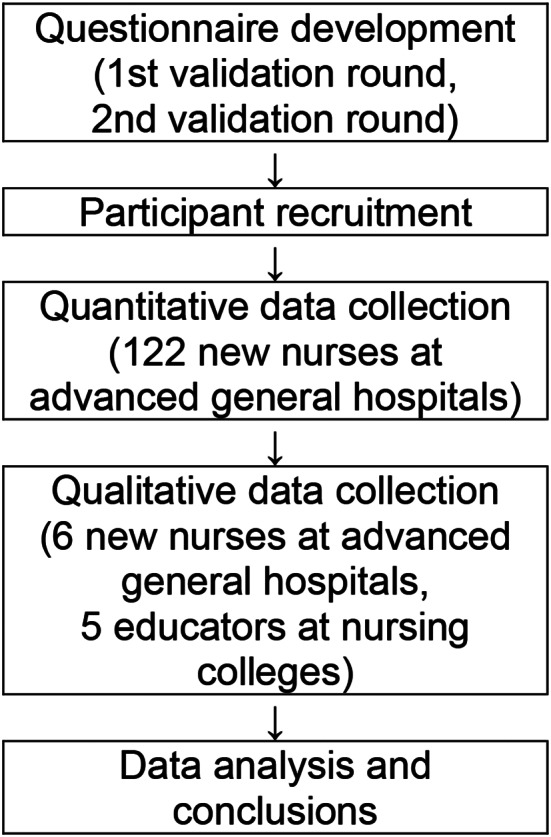
Research flowchart
Sampling and recruitment
There were two pools of participants. Quantitative and qualitative data were collected from new nurses recruited by convenience sampling at advanced general hospitals in two major cities (G— and S—). The two hospitals are representative tertiary hospitals in the capital and regional areas in Korea. These were selected to extract samples from the accessible population. In addition, qualitative data were also collected from educators working at a nursing college. The inclusion criterion for new nurses was having 2–24 months of experience, while that for educators was being a full-time teaching staff member at a four-year college with experience in simulation training.
Of the 128 new nurses who participated in quantitative data collection, six consented to qualitative data collection. Owing to incomplete responses or not meeting the inclusion criteria, six participants were excluded from quantitative data analysis; thus, 122 participants were included in the quantitative analysis. Qualitative data were collected from new nurses and nursing college educators using snowball sampling until saturation. Six new nurses and five educators were included in the final qualitative analysis.
Research instruments
For the participants’ general characteristics, sex, age, clinical experience, and current working department were assessed.
Educational experience
The participants’ educational experience was investigated using six questions developed by the researchers based on the previous research [4, 5, 15] asking the following: (1) whether the participants had experience of education in the care of adult respiratory patients, (2) the educational content, (3) educational methods, (4) source of information about the care of adult respiratory patients, (5) educational methods that participants thought were most effective, and (6) whether the participants thought that VR-based simulation training was necessary for nursing students.
Educational needs
Educational needs were measured using an instrument developed by the researchers. To investigate the needs for VR-based simulation training in the care of adult respiratory patients, a set of 47 preliminary questions was developed through a literature review [4, 5, 15, 23, 24]. The content validity was tested by a panel of three nursing college professors with ample experience of simulation training.
Based on the results of the first panel meeting, eight questions with a content validity index (CVI) < 0.7 were excluded after discussions between the researchers. Some questions were adjusted to convey a clearer meaning or resolve duplicated content. A second round of content validation was then conducted, and 32 questions were selected for the final questionnaire. The questions on educational needs were divided into three domains: overall respiratory care in adults, upper/lower respiratory disease, and core nursing skills. Each question was scored on a 5-point Likert scale from 1 (“completely unnecessary”) to 5 (“very necessary”), with higher scores indicating greater educational need. The content validity of the final instrument was demonstrated by CVI > 0.94, and the internal consistency of the instrument was demonstrated by Cronbach’s α = 0.917.
Data collection
Quantitative and qualitative data collection
Research data were collected from August 31 to September 26, 2022. After collecting quantitative data to investigate the experience of and needs for VR-based simulation training, qualitative data were collected for a more in-depth study. An online questionnaire was used for quantitative data collection, since the COVID-19 pandemic had forced advanced general hospitals in Korea to restrict outside access to the wards. Participants voluntarily read an explanation of the study online via recruitment notices. Only after signing the consent form were they asked to complete the questionnaire. Furthermore, participants were allowed to communicate with the researchers about any aspect of the study.
The interviews for qualitative data collection were conducted over the telephone using a semi-structured questionnaire. Using snowball sampling, six new nurses and five nursing college educators were interviewed before saturation. The mean time per interview per person was 25–30 min. The interview content was recorded after obtaining consent from the participants, and the researchers listened to the recordings multiple times to transcribe the content.
Researchers’ preparations for qualitative data analysis
Before the qualitative data analysis, the two researchers took a course on qualitative nursing research at a graduate school and also attended several workshops and special lectures held by the Korean Society of Qualitative Nursing Research.
Data analysis
The quantitative data were analyzed using IBM SPSS Statistics 29.0 (IBM Co., Armonk, NY, USA). The specific methods of analysis were as follows. General characteristics were analyzed using frequency, percentile, mean, and standard deviation; the responses to each question were subjected to multiple response analysis and frequency analysis. Qualitative data were subjected to the qualitative content analysis method of Krippendorff [25]. The content analysis included coding units of testimony, validating these units, and determining reliability between multiple expert coders [26]. The researchers transcribed the recorded interviews and then made notes and categorizations while repeatedly reading the content. The first stage of content analysis involved extracting significant meaning from the data, while the second stage involved categorizing the data.
Ethical considerations
This study was conducted after receiving approval from the Institutional Review Board of X University (1041465-202205-HR-001-14). Official written approval for data collection was obtained from the heads of nursing at the two hospitals participating in the study. The quantitative survey was only conducted on participants who consented to participate via a recruitment notice. All participants were informed that they could ask the researchers questions at any time during the study. The validity, reliability, and risk of generalization were considered continually throughout qualitative data collection. All participants were sent a small gift voucher as a token of appreciation.
Results
Quantitative data analysis
Participants’ general characteristics
Table 1 presents the new nurses’ general characteristics. There were 109 female (89.3%) and 13 male (10.7%) nurses. Their mean age was 24.51 ± 1.91 years, with most participants being in their twenties (n = 119, 97.5%). The mean total clinical experience was 11.18 ± 5.84 months, and the most common bracket was 2–12 months (n = 64, 52.5%). The mean clinical experience in the present department was 10.54 ± 5.77 months, and 2–12 months was the most common bracket (n = 73, 59.8%).
Table 1.
Participants’ general characteristics (N = 122)
| Characteristics | Category | n | (%) | Mean ± SD |
|---|---|---|---|---|
| Sex | Male | 13 | 10.7 | |
| Female | 109 | 89.3 | ||
| Age (years) | 20–29 | 119 | 97.5 | 24.51 ± 1.91 |
| 30–39 | 3 | 2.5 | ||
| Total clinical experience (months) | 2–12 | 64 | 52.5 | 11.18 ± 5.84 |
| 12–24 | 58 | 47.5 | ||
| Clinical experience in the present department (months) | 2–12 | 73 | 59.8 | 10.54 ± 5.77 |
| 12–24 | 49 | 40.2 | ||
| Experience of adult respiratory patient care | Yes | 101 | 82.8 | |
| No | 21 | 17.2 | ||
| Educational contenta | Definitions and causes of diseases | 93 | 20.6 | |
| Clinical symptoms | 95 | 21.1 | ||
| Diagnostic methods | 82 | 18.2 | ||
| Treatment | 88 | 19.5 | ||
| Nursing | 93 | 20.6 | ||
| Source of informationa | Hospital website | 26 | 13.5 | |
| National public institution website | 49 | 25.5 | ||
| Mass media | 12 | 6.3 | ||
| YouTube and social media | 82 | 42.7 | ||
| Other | 23 | 12.0 | ||
| Previously experienced educational methodsa | In-person lectures | 82 | 41.2 | |
| Remote lectures (live) | 24 | 12.1 | ||
| Remote lectures (recorded) | 35 | 17.6 | ||
| Practice | 54 | 27.1 | ||
| Other | 4 | 2.0 | ||
| Most effective educational methods of the adult respiratory patient care | In-person lectures | 16 | 13.1 | |
| Remote lectures (live) | 1 | 0.8 | ||
| Remote lectures (recorded) | 7 | 5.8 | ||
| Simulation-based practical education | 68 | 55.7 | ||
| Core nursing skills practical education | 29 | 23.8 | ||
| Other | 1 | 0.8 | ||
| Perception of the need for VR-based simulation training | Necessary | 115 | 94.3 | |
| Unnecessary | 7 | 5.7 |
SD: Standard Deviation; VR: Virtual Reality
amultiple choice questions
Educational experience
Most participants had previous experience of adult respiratory patient care (n = 101, 82.8%), and the most common educational content was clinical symptoms (n = 95, 21.1%), followed by nursing (n = 93, 20.6%), definitions and causes of disease (n = 93, 20.6%), treatment (n = 88, 19.5%), and diagnostic methods (n = 82, 18.2%).
Among sources of information, YouTube and social media were the most common (n = 82, 42.7%), followed by the national public institution website (n = 49, 25.5%) and “other” (n = 23, 12.0%). “Other” specifically included specialist writings and academic papers.
Among previously experienced educational methods, in-person lectures were the most common (n = 82, 41.2%), followed by practice (n = 54, 27.1%), recorded lectures (n = 35, 17.6%), and live remote lectures (n = 24, 12.1%). The most effective method was reported to be simulation-based practical education (n = 68, 55.7%), and the “other” response (n = 1, 0.8%) included in-person lectures and practical education in parallel. Overall, 115 (94.3%) responded that VR-based simulation training was necessary whereas seven (5.7%) who considered it unnecessary (Table 1).
Educational needs
New nurses’ educational needs were analyzed in terms of overall educational needs for the adult respiratory system, upper respiratory disease, lower respiratory disease, and core nursing skills. Table 2 presents the results. The strongest needs in overall education for the adult respiratory system were clinical symptoms (4.59 ± 0.51), followed by patient nursing (ineffective breathing patterns [4.59 ± 0.54], gas exchange impairment [4.53 ± 0.56], and ineffective airway clearance [4.51 ± 0.62]). For upper/lower respiratory disease, the strongest needs were infectious disease (acute bronchitis, pneumonia, pulmonary tuberculosis, lung abscess [4.63 ± 0.53]), followed by respiratory insufficiency (acute respiratory insufficiency, acute dyspnea [4.49 ± 0.66]) and obstructive lung disease (bronchial asthma, chronic obstructive pulmonary disease, bronchial dilation, cystic fibrosis [4.48 ± 0.59]). For core nursing skills, the strongest needs were basic cardiopulmonary resuscitation (CPR) and defibrillation (4.74 ± 0.46), followed by intravenous fluids (including use of an infusion pump or syringe pump [4.69 ± 0.53]), pulse oximeter measurement and electrocardiogram (EKG) monitor use (4.62 ± 0.55), suction (4.58 ± 0.65), and vital signs measurement (4.51 ± 0.75).
Table 2.
Participants’ educational needs (N = 122)
| Categories | Contents | Min | Max | Mean ± SD |
|---|---|---|---|---|
| Overall educational needs for the adult respiratory system | Definitions and causes of disease | 2 | 5 | 4.27 ± 0.64 |
| Clinical symptoms | 3 | 5 | 4.59 ± 0.51 | |
| Diagnostic and testing methods | 3 | 5 | 4.34 ± 0.63 | |
| Treatment methods | 3 | 5 | 4.40 ± 0.56 | |
| Patient nursing (gas exchange impairment) | 3 | 5 | 4.53 ± 0.56 | |
| Patient nursing (activity intolerance) | 2 | 5 | 3.82 ± 0.82 | |
| Patient nursing (fatigue) | 2 | 5 | 3.54 ± 0.81 | |
| Patient nursing (ineffective breathing patterns) | 3 | 5 | 4.59 ± 0.54 | |
| Patient nursing (impaired spontaneous ventilation) | 3 | 5 | 4.34 ± 0.65 | |
| Patient nursing (ineffective airway clearance) | 3 | 5 | 4.51 ± 0.62 | |
| Upper respiratory disease | Infectious disease (influenza, rhinitis, sinusitis, pharyngitis, tonsillitis, adenoiditis, peritonsillar abscess, laryngitis, COVID-19) | 2 | 5 | 4.09 ± 0.70 |
| Neoplastic disease (head and neck cancer) | 2 | 5 | 3.51 ± 0.71 | |
| Multifactorial disorders (epistaxis, nasal polyps, intranasal foreign body, obstructive sleep apnea, vocal paralysis, vocal cord polyps/nodules, laryngeal edema, laryngeal foreign body, facial trauma) | 2 | 5 | 3.62 ± 0.76 | |
| Lower respiratory disease | Infectious disease (acute bronchitis, pneumonia, pulmonary tuberculosis, lung abscess) | 3 | 5 | 4.63 ± 0.53 |
| Interstitial lung disease (occupational lung disease, sarcoidosis, idiopathic pulmonary fibrosis) | 2 | 5 | 3.69 ± 0.81 | |
| Pulmonary vascular disease (pulmonary embolism, pulmonary hypertension, pulmonary heart disease) | 2 | 5 | 4.32 ± 0.71 | |
| Pleural disorders (pleural effusion, empyema) | 2 | 5 | 4.39 ± 0.66 | |
| Respiratory insufficiency (acute respiratory insufficiency, acute dyspnea) | 2 | 5 | 4.49 ± 0.66 | |
| Obstructive lung disease (bronchial asthma, chronic obstructive pulmonary disease, bronchial dilation, cystic fibrosis) | 3 | 5 | 4.48 ± 0.59 | |
| Neoplastic disease (lung cancer) | 2 | 5 | 4.07 ± 0.79 | |
| Trauma (pulmonary contusion, rib fracture, flail chest, pneumothorax, hemothorax) | 2 | 5 | 4.22 ± 0.70 | |
| Educational needs for core nursing skills | Vital signs measurement | 2 | 5 | 4.51 ± 0.75 |
| Oral administration | 1 | 5 | 3.94 ± 0.99 | |
| Intramuscular injection | 2 | 5 | 4.30 ± 0.80 | |
| Intravenous fluids (including use of an infusion pump or syringe pump) | 3 | 5 | 4.69 ± 0.53 | |
| Pulse oximeter measurement and EKG monitor use | 3 | 5 | 4.62 ± 0.55 | |
| Oxygen therapy using a nasal cannula | 2 | 5 | 4.42 ± 0.75 | |
| Suction | 2 | 5 | 4.58 ± 0.65 | |
| Basic CPR and defibrillation | 3 | 5 | 4.74 ± 0.46 | |
| Pain management | 2 | 5 | 4.04 ± 0.79 | |
| Sores management and fall prevention | 2 | 5 | 4.30 ± 0.74 | |
| Catheter management (JP or Hemovac) | 2 | 5 | 4.39 ± 0.65 |
EKG: electrocardiogram; CPR: cardiopulmonary resuscitation; JP: Jackson Pratt
Qualitative data analysis
Participants’ general characteristics
Of the six new nurses, five (83.33%) were women and one (16.67%) was men; all five educators (100%) were women (Table 3). The mean age of the participants was 24.67 ± 0.82 years for the new nurses and 44.60 ± 7.40 years for the educators. The mean total clinical experience was 10.67 ± 4.18 months for the new nurses and 92.20 ± 82.98 months for the educators. The current work departments of the new nurses were internal/surgical mixed ward (n = 3, 50.0%), traditional Korean medicine ward (neurology) (n = 1, 16.7%), emergency department (n = 1, 16.7%), and circulatory medicine department (n = 1, 16.7%). The educators’ current majors were pediatric nursing (n = 2, 40.0%), community nursing (n = 1, 20.0%), and adult nursing (n = 2, 40.0%; Table 3).
Table 3.
General characteristics and educational experience (N = 11)
| Categories | Sex | Age (years) | Total clinical career (months) | Work department or Nursing major |
|---|---|---|---|---|
| New nurses | Female | 25 | 14 | Internal/surgical mixed ward |
| Male | 26 | 16 | Internal/surgical mixed ward | |
| Female | 25 | 13 | Internal/surgical mixed ward | |
| Female | 24 | 6 | Traditional Korean medicine ward (neurology) | |
| Female | 24 | 7 | Emergency department | |
| Female | 24 | 8 | Circulatory medicine department | |
| Nursing college educators | Female | 49 | 238 | Pediatric nursing |
| Female | 39 | 80 | Community nursing | |
| Female | 35 | 37 | Adult nursing | |
| Female | 53 | 50 | Pediatric nursing | |
| Female | 47 | 56 | Adult nursing |
New nurses’ views on the state of education and educational needs
Theme 1: current state of education
Subtheme 1: experience of receiving education relating to patients with infectious respiratory disease (satisfactory in-person education)
Excluding one person working in a traditional Korean medicine ward, all participants reported experiences of education relating to patients with infectious respiratory disease. Educational methods mostly involved theory and practice in parallel. Satisfaction was high for in-person practical training, but not for online video education. Below, we list some excerpts from the data that reflect this subtheme.
I was grateful that our hospital explained what infection control guidelines there are, as well as practical information, like how to wear personal protective equipment (PPE), and how to use a ventilator or administer continuous renal replacement therapy (CRRT) (Participant A).
Two nurses who were responsible for training new nurses actually brought equipment with them and taught us thoroughly from setting the mode to priming; I liked that there were ample opportunities to learn and practice (Participant B).
Subtheme 2: experience of receiving simulation training (simulation training has both strengths and weaknesses)
All participants had experienced receiving simulation training before and after graduating from nursing college. Participants spoke positively about simulation training because it was gratifying, allowed indirect experience of real situations, and could foster cooperation with colleagues. Moreover, they indicated that the instructors provided positive feedback through the simulation training.
Nevertheless, the method had some shortcomings. For example, the nurse working at a traditional Korean medicine ward (neurology) was disappointed that the latest clinical equipment and materials were not used, while nurses who had used high-fidelity simulators were disappointed by the few number of sessions. Nurses who had received training using VR highlighted technical problems, such as buffering and blurry images. Below, we list some excerpts from the data that reflect this subtheme.
I remember when they actually brought in an actor so we could practice cases you might see in a clinical setting. I liked that I could see how I might cope with those scenarios after I become a nurse (Participant B).
I liked that I could learn about the work that real nurses do and how they can respond (Participant B).
I took part in a simulation where a baby was crying and the mother was complaining. I thought it was good to be able to embody, indirectly, the role of a nurse (Participant C).
During CPR education, we did a simulation with some teachers acting as doctors and others acting as nurses. I felt like we could never have too much of this (Participant A).
I liked that I could ask questions whenever I was curious and get an immediate answer (Participant D).
Unfortunately, the equipment they used for training was old. It would be good to get training with materials and equipment that were recently bought and a little more diverse (Participant D).
Theme 2: needs for VR-based simulation training in nursing
Subtheme 1: need for VR-based simulation training on respiratory care for adults
One of the participants reported that VR-based simulation training was necessary for nurses working in a directly related ward, but was not required for everybody. Other participants reported that VR-based simulation education for respiratory patients was necessary. Among them, one participant highlighted the need to accumulate clinical knowledge to prepare for clinical situations, such as those involving patients with respiratory problems like tuberculosis. One participant also mentioned that VR-based simulation education was important to protect oneself as a medical worker. Below, we list some excerpts from the data that reflect this subtheme.
Even if I work in a general ward, a patient could be admitted with, say tuberculosis. So, I think that I need to know the basics in order to protect myself (Participant C).
I think it’s necessary. First of all, I need to know about this so that I don’t negatively affect other patients. Also, I think the more clinical knowledge you have, the better it is for yourself (Participant F).
Subtheme 2: need for a realistic and detailed nursing education design (contents, methods, environment)
Essential educational content included routes of infection, patient care, treatment, patient education, and related core nursing skills such as suction, oxygen therapy, use of PPE, and managing medical waste materials from quarantined patients. In terms of educational methods, most participants favored in-person education. Regarding the educational environment, participants highlighted the need to use the latest equipment, and to ensure sufficient training duration and frequency. Below, we list some excerpts from the data that reflect this subtheme.
I would like the education content to include a detailed manual on how to manage different cases, using real case studies (Participant A).
The educational content should include types of infectious respiratory disease, care, treatment, and patient education (Participant A).
I would like training on how to handle an emergency situation with a patient who is short of breath (Participant C).
I think that suction is the most important, since there are lots of patients using a ventilator or Optiflow (i.e., Airvo™) (Participant E).
I think it would be better if they gave us more opportunities to repeat the training (Participant B).
Educators’ views on the state of education and educational needs
Theme 1: current state of education
Subtheme 1: diverse and satisfactory experiences of administering simulation training
The participants experienced administering training to children with respiratory problems using a high-fidelity simulator, newborn apnea, febrile children, pre-eclampsia patients, respiratory infectious disease, preoperative care for cholecystectomy patients, upper gastrointestinal bleeding patients, liver cirrhosis patient scenarios, and a home care scenario using SPs. All participants were generally satisfied with their experiences of running simulations. Below, we list some excerpts from the data that reflect this subtheme.
The scenarios I’ve run in the last four years include children with respiratory problems and women with pre-eclampsia (Participant G).
It was a scenario for the postoperative care of upper gastrointestinal bleeding patients (Participant I).
There were scenarios for managing newborn apnea and febrile children (Participant J).
It was very effective at engrossing and motivating the students (Participant H).
Subtheme 2: receiving simulation training that reflect its strengths and weaknesses
All participants had experience in receiving simulation training, mostly through remote methods. Participants received training through online videos or real-time Zoom calls, in the form of supplementary or continuing education. Satisfaction with training was generally good. Participants mentioned that VR-based training was more efficient than high-fidelity simulation owing to the lower cost of equipment. Participants who received training using a metaverse in real-time Zoom calls reported positive experiences of infant consultations in a home-visit scenario within a virtual space. They mentioned that this experience of receiving training helped them advise students. The negative aspects of receiving education included somewhat poor quality graphics in VR, and difficulties maintaining consistent learning speeds between students owing to discrepancies in adapting to the digital environment of the metaverse. Thus, the participants highlighted VR graphics as an area for improvement and also mentioned that combining VR with well-trained SPs could be effective. Below, we list some excerpts from the data that reflect this subtheme.
These methods could be cost-effective by exhibiting optimal efficacy while occupying minimal space. I got a positive impression, and I think this could be exceptionally effective if more diverse programs were offered (Participant G).
I think the technology needs to be refined a bit more, since the graphics and content were of poor quality, and students might find it boring (Participant J).
Theme 2: needs for VR-based simulation training in nursing
Subtheme 1: need for VR-based simulation training on respiratory care in adults
All participants responded that VR-based simulation training on respiratory care is essential. They highlighted the need for education on infectious respiratory patients, including novel infectious diseases. Below, we list some excerpts from the data that reflect this subtheme.
Since novel infectious diseases like COVID-19 will continue to emerge, it seems right to receive this type of education in order to prepare the necessary knowledge and practical competencies (Participant H).
I think this type of education is necessary, because it allows the learner to clearly experience the importance of infectious patient management in hospitals (Participant G).
Subtheme 2: need for a realistic and detailed nursing education design (contents, methods, environment) that reflects students’ needs
The participants each suggested educational content that they wanted to see included when designing VR-based simulation training for the care of adult respiratory patients. This content included basic nursing (anatomy, pathology), characteristic features of the disease, transmission routes and management protocols for different infectious diseases, and protective methods for medical personnel, including the use of PPE. In terms of educational methods, the participants did not distinguish between in-person and remote methods, stating that both could be used in parallel if necessary. Student safety and similarity to real clinical settings should be considered when designing the educational environment. Below, we list some excerpts from the data that reflect this subtheme.
First, when thinking of infectious respiratory diseases, we think of Middle East respiratory syndrome (MERS), severe acute respiratory syndrome (SARS), and now COVID-19. I would like to teach students about the similarities and differences between these three diseases. In the post-COVID-19 era, we should think about what we can do in the event of another infectious disease related to disaster (Participant G).
I think that it would be beneficial to experience many different simulation modules using diverse media (Participant H).
I think that we ought to prioritize education that ensures students’ safety, and that can sufficiently meet their needs and standards (Participant J).
I think it would be good to construct a scenario based on dealing with ventilators (Participant H).
I think it would be good to practice wearing Level D PPE (Participant H).
I think it would be good to include content on communicating with other types of medical personnel (Participant I).
There should be scenarios set in a negative pressure room and materials prepared for isolation of infectious respiratory patients (Participant K).
Discussion
This descriptive survey examined the current state of and demand for VR-based simulation training for nursing students. In the quantitative analysis of new nurses’ educational experiences, most participants reported that they perceived VR-based simulation training through in-person lectures as necessary. About half the participants reported that simulation training was an effective educational method. In the qualitative analysis, all participants experienced simulation training, with most having received it through an in-person format. They reported being satisfied with the simulation training as it allowed them to experience nursing indirectly and reflect on how they would cope in certain situations.
Brown et al. provided a VR program to advanced practice nurse students, who reported that the VR learning experience satisfied their educational needs, which is consistent with the results of our study [7]. Chau et al. reported that learning using high-fidelity simulators or VR could provide nursing students with a fulfilling educational experience [8]. Classes using VR can improve nursing students’ knowledge of hospital settings, educational satisfaction, and academic achievement [22], while VR-based simulation training using vSim® can improve the ability to perform nursing tasks, critical thinking tendencies, and self-efficacy [2]. Zaragoza-García et al. applied vSim® to nursing students in their final year and observed increased satisfaction and self-confidence among participants [6]. Moreover, learning using AR has positive effects on learning immersion, interest, and attitudes [3].
Thus, this study adds to existing evidence that VR-based simulation training has positive, useful effects on nursing students’ practical education. Considering the various advantages of simulation education using VR, it is necessary to make efforts to implement a realistic teaching and learning environment when designing education. Additionally, it is necessary to build a safe educational environment that takes into account temporary dizziness caused by learning in a virtual space. It is also necessary to provide training in advance on the use of VR devices and consider precautions. Since VR-based education relies on technical devices, instructors must anticipate potential delays due to technical problems or graphic resolution issues. Therefore, before starting the education, the instructor should recognize surrounding objects using the VR device and perform a calibration process to match the device to the subject’s eyes.
Needs assessments in medical education are often conducted using data gathered from surveys, structured personal interviews, observations of clinical practice, or peer review data [27]. In this study, we employed survey and personal interviews as part of a mixed-method approach. Among the educational needs of new nurses, our quantitative analysis showed strong needs relating to clinical symptoms of diseases, patient care (ineffective breathing patterns, impairment of gas exchange, ineffective airway clearance), and infectious respiratory diseases. Meanwhile, the core nursing skills that new nurses wanted to learn alongside simulation training for the care of respiratory patients were, in order of importance, basic CPR and defibrillation, intravenous fluid administration (including infusion pump use), pulse oximeter measurement and EKG monitor use, and suction. Among the six stages of the nursing process, the patient’s clinical symptoms should be collected as objective evidence in the first stage, and our results verified the nursing diagnosis that can be deduced most often in relation to respiratory patients.
The qualitative results also showed that new nurses wanted to receive detailed, realistic education about diseases, and there was an especially high demand for simulation training to prepare for emergency situations. Similarly, when Jung studied the practical educational needs of new operating theater nurses, participants reported a need for simulation training to improve their ability to cope in problematic situations [28]. In summary, these results demonstrate that new nurses’ educational needs include improvement in the ability to deal with the sudden worsening of a patient’s condition, suggesting that these findings could be applied proactively to nursing students’ education. Likewise, the core nursing skills that were found to have high relevance could be included as educational content when planning future simulation training in the care of respiratory patients for real nursing students. Zaragoza-García et al. also reported the need to add activities to improve technical skills [6].
In exploring the educational experiences of nursing college educators, we found that all participants had experienced both delivering and receiving simulation training. Most of the educators had received remote training and mentioned the poor quality of VR graphics and discrepancies between students in their ability to adapt to a digital setting as disappointing aspects of their experience. Nevertheless, they responded favorably to its potential to allow educators to experience nursing, albeit indirectly. Therefore, instructors need to check the resolution and clarity of graphics when using VR equipment. Jung and Chae also reported that their participants had ambivalent feelings about VR practice [15], while Seo and Jeong reported that theirs felt “tension” during a VR simulation of psychiatric nursing [29]. This demonstrates that learners can simultaneously experience interest and awkwardness regarding VR practice, suggesting several implications regarding the development of VR-based simulation training for learners. To induce the positive effects of VR-based training, it is important to provide a thorough explanation of VR before training. Moreover, trial runs requiring students to practice operating the equipment may help reduce ambivalence toward VR. In addition, when using VR, it is necessary to provide learners with breaks at regular intervals and prepare measures to reduce tension. A study by Takhdat et al. [30] showed that a brief pre-briefing mindfulness meditation practice mitigates student’s state-anxiety. Therefore, it is considered beneficial to include meditation when designing a VR based simulation program.
When the educators were asked about educational needs, all participants reported the need for VR-based simulation programs relating to the respiratory system. In terms of essential educational content, the participants mentioned the need for detailed content regarding different infectious respiratory diseases, inclusion of practice wearing PPE, construction of an environment that resembles real clinical settings, and consideration of student safety. According to Kolb’s experiential learning theory, learning is achieved through specific concrete experiences, reflecting observations, conceptualization of abstract thought, and active experimentation [31]. As an educational method, simulation training is a good representation of Kolb’s theory and can be a useful method in students’ learning experiences in nursing studies [32]. Lim also reported that VR-based simulation training improves performance in nursing tasks, and that students need to experience repeated, thorough practice through VR-based simulation training before they engage in real clinical practice [2]. As such, it is essential to develop programs that include detailed educational content, with a careful design that considers learning goals and student safety.
Nursing is a pragmatic study in which theory and practice should be incorporated. During the COVID-19 pandemic, practical education faced many obstacles. In-school practice requires a specific learning process using practice materials and props, wherein the educator provides a demonstration, and the students practice the process themselves before making corrections based on the educator’s feedback. In reality, clinical practice is often done entirely on-site in a clinical setting. Given the circumstances, some schools tried to replace clinical practice with practice in school. Even when practical education was provided in a real clinical setting, the experience was often limited, and nursing students experienced anxiety from the uncertainty of not knowing when their practical learning might be suspended [4]. For practical education in the post-COVID era, it will be important to develop new learning methods that integrate existing practice room classes, clinical practice, high-fidelity simulation, and VR by analyzing their educational effects when applied as part of real nursing programs.
This is consistent with what has been described so far: the contents show that most of the research subjects who participated in the qualitative data collection of this study responded positively because the simulation education experience allowed them to learn by linking theory and practice.
We derive the following implications for the future development of nursing students’ VR-based simulation training in the care of adult respiratory patients. First, educational programs need to be designed comprehensively, based on the NLN Jeffries Simulation Theory [33]. Previous educational research using AR found the need to diversify both educational subjects and learners [34] and proposed that programs should be designed carefully and in a multifaceted manner to meet the needs of learners. Given that multiple studies have mentioned the limitations of precise, integrated design and application [4, 7], it will be necessary to develop programs that include details, accurate techniques, settings, and content.
Second, AR-based educational content is classified into experiential, practical, cooperative, and communicational forms [34]; cooperative forms, wherein several learners work together to solve a task, could be utilized in practical education at nursing colleges. VR-based learning experiences, which enable the total immersion of the learner, could be a new strategy to provide engaging nursing instruction [7] and be an effective learning method for learners familiar with digital environments.
Third, when running a VR-based simulation training program, we propose the need for hybrid education using partial models in the case of nursing skills that require fine hand movements. The use of partial models will be even more useful when designing core nursing skills in simulation programs.
Fourth, given the importance of ethical awareness and professionalism, it will be necessary to construct programs that include digital ethical education as part of nursing education using VR and digital information [35]. No previous study applying VR-based simulation training as an intervention included considerations of digital ethics [5, 15,, 16]. When administering education using the latest equipment in the age of the fourth industrial revolution, it is necessary to consider education design, including student safety and the ethical attitude of nursing students when caring for virtual patients [36].
Limitations
This study had some limitations. First, because the data were collected from new nurses working at two advanced general hospitals, there may be limitations in generalizing the results. Second, since we collected data from nursing college educators with diverse clinical experience and specialist fields, the study must be repeated with a larger pool of participants. Third, the study must be repeated with quantitative and qualitative data from preceptors, who are responsible for teaching new nurses in clinical settings. Lastly, the data were collected using a developed tool and from online; there may be limitations in generalizing the results.
Conclusions
This study provides data to support the development of VR-based simulation training for nursing students on the care of respiratory patients. Given the educational experiences and needs of the participants, it will be important to develop comprehensive and customizable simulation programs that provide an educational environment that maximally resembles real clinical settings. When designing a simulation education program using VR for nursing students, it is crucial to develop an educational environment that carefully considers the safety of learners and incorporate a realistic clinical setting. Additionally, we recommend including digital ethics to enhance the quality of the simulation program.
Acknowledgements
The authors would like to express their gratitude to all the participants of the study.
Abbreviations
- AR
Augmented reality
- CPR
Cardiopulmonary resuscitation
- CRRT
Continuous renal replacement therapy
- CVI
Content validity index
- EKG
Electrocardiogram
- MERS
Middle East respiratory syndrome
- MR
Mixed reality
- PPE
Personal protective equipment
- SARS
Severe acute respiratory syndrome
- SP
Standard patient
- VR
Virtual reality
Author contributions
Conceptualization: MJ, ML; Data curation: MJ, ML; Formal analysis: MJ; Funding acquisition: MJ; Investigation: MJ, ML; Methodology: MJ, ML; Resources: MJ, ML; Supervision: MJ; Validation: MJ, ML; Visualization: MJ, ML; Writing – original draft: MJ, ML; Writing – review and editing: MJ, ML. All authors read and approved the final manuscript.
Funding
This study was supported by the National Research Foundation of Korea grant funded by the Korean government (No. 2022R1G1A1007923).
Data availability
The data used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kwangju Women’s University (1041465-202205-HR-001-14). Informed consent was obtained from all the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Global strategy on human resources for health: workforce 2030. 2016. https://apps.who.int/iris/bitstream/handle/10665/250368/9789241511131-eng.pdf. Accessed 27 Apr 2023.
- 2.Lim J. The effect of virtual reality simulation education on nursing process competency. J Digit Converg. 2021;19:401–9. 10.14400/JDC.2021.19.9.401. [Google Scholar]
- 3.Son HK. Effects of S-PBL in maternity nursing clinical practicum on learning attitude, metacognition, and critical thinking in nursing students: a quasi-experimental design. Int J Environ Res Public Health. 2020;17:7866. 10.3390/ijerph17217866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim KS, Park JM. Clinical practice experience including web-based simulation practice of nursing students during the COVID-19 pandemic. J Converg Inf Technol. 2022;12:81–93. [Google Scholar]
- 5.Lee SE, Chung SE. The experiences of virtual reality-based simulation in nursing students. J Converg Cult Technol. 2021;7(1):151–61. 10.17703/JCCT.2021.7.1.151. [Google Scholar]
- 6.Zaragoza-García I, Ortuño-Soriano I, Posada-Moreno P, Sánchez-Gómez R, Raurell-Torredà M. Virtual simulation for last-year nursing graduate students in times of Covid-19: a quasi-experimental study. Clin Simul Nurs. 2021;60:32–41. 10.1016/j.ecns.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown KM, Swoboda SM, Gilbert GE, Horvath C, Sullivan N. Curricular integration of virtual reality in nursing education. J Nurs Educ. 2023;1–10. 10.3928/01484834-20230110-01. [DOI] [PubMed]
- 8.Chau M, Arruzza E, Johnson N. Simulation-based education for medical radiation students: a scoping review. J Med Radiat Sci. 2022;69:367–81. 10.1002/jmrs.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biocca F, Levy MR. Communication in the age of virtual reality. Taylor & Francis; 2013.
- 10.Radianti J, Majchrzak TA, Fromm J, Wohlgenannt I. A systematic review of immersive virtual reality applications for higher education: design elements, lessons learned, and research agenda. Comput Educ. 2020;147:103778. 10.1016/j.compedu.2019.103778. [Google Scholar]
- 11.Kwon H, Morrill K. Virtual reality: immersive and situated art education with 360-Degree cameras, and augmented and virtual reality technology. Art Educ. 2022:75:27–32. 10.1080/00043125.2022.2053458
- 12.Suh D, Suh EA. Study on the development of AR content for promoting memory learning - nursing education learning content. J Ind Converg. 2021;19:79–85. 10.22678/jic.2021.19.1.079. [Google Scholar]
- 13.Chen H, Hou L, Zhang G, Moon S. Development of BIM, IoT and AR/VR technologies for fire safety and upskilling. Autom Constr. 2021;125:103631. 10.1016/j.autcon.2021.103631. [Google Scholar]
- 14.Robinson DA, Piekut DT, Hasman L, Knight PA. Cadaveric simulation training in cardiothoracic surgery: a systematic review. Anat Sci Educ. 2020;13:413–25. 10.1002/ase.1908. [DOI] [PubMed] [Google Scholar]
- 15.Jung H, Chae M. Experience the core fundamental nursing skills practice of nursing students using virtual reality. J Humanit Social Sci. 2020;11:703–16. 10.22143/hss21.11.4.51. [Google Scholar]
- 16.You Y, Yang B. The effects of virtual reality simulation scenario application on clinical competency, problem solving ability and nursing performance confidence. J Korea Acad-Ind Coop Soc. 2021;22:116–26. 10.5762/KAIS.2021.22.9.116. [Google Scholar]
- 17.Venkatesan M, Mohan H, Ryan JR, Schürch CM, Nolan GP, Frakes DH et al. (2021). Virtual and augmented reality for biomedical applications. Cell Rep Med. 2021;2(7):100348. 10.1016/j.xcrm.2021.100348 [DOI] [PMC free article] [PubMed]
- 18.Delgado-Rodríguez S, Carrascal Domínguez S, Garcia-Fandino R. Design, development and validation of an educational methodology using immersive augmented reality for STEAM education. J New Approaches Educ Res. 2023;12:19–39. 10.7821/naer.2023.1.1250. [Google Scholar]
- 19.Lee M, Han S, Choi J. Korea Armed Forces nursing academy cadets’ experience with virtual reality core nursing skills training program. Military Health Policy Res. 2023;41:32–47. 10.31148/kjmnr.2023.41.3.32. [Google Scholar]
- 20.Statistics Korea. 2021 Cause of death statistics. 2022. https://kostat.go.kr/board.es?mid=a10301060200&bid=218&act=view&list_no=420715. Accessed 27 Apr 2023.
- 21.Lee EH, Ryu SY. Analysis of the virtual simulation practice and high fidelity simulation practice training experience of nursing students: a mixed-methods study. J Korean Acad Soc Nurs Educ. 2021;27:227–39. 10.5977/jkasne.2021.27.3.227. [Google Scholar]
- 22.Kim MG, Kim HW. The effects of classes using virtual reality simulations of the hospital environment on knowledge of the hospital environment, academic self-efficacy, learning flow, educational satisfaction and academic achievement in nursing students. J Korean Acad Fundam Nurs. 2022;28:520–9. 10.7739/jkafn.2021.28.4.520. [Google Scholar]
- 23.Kaufman R, Fenwick W. Needs assessment: Concept and application. Educational Technology; 1979.
- 24.Borich GD. A needs assessment model for conducting follow-up studies. J Teach Educ. 1980;31(3):39–42. 10.1177/002248718003100310. [Google Scholar]
- 25.Krippendorff K. Content analysis: an introduction to its methodology. Sage; 2019.
- 26.Hayes AF, Krippendorff K. Answering the call for a standard reliability measure for coding data. Commun Methods Meas. 2007;1:77–89. 10.1080/19312450709336664. [Google Scholar]
- 27.Grant J. Learning needs assessment: assessing the need. BMJ: Br Med J. 2002;324:156–9. 10.1136/bmj.324.7330.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jung J. According to the clinical career of operating room nurses. Differences between job performance capability and needs for practical education. [Unpublished master’s thesis]. Seoul: Chung-Ang University; 2019.
- 29.Seo Y-S, Jeong CY. A qualitative content analysis of journals for psychiatric nursing virtual reality-based simulation in nursing students. J Korea Acad-Ind Coop Soc. 2022:23:217–26. 10.5762/kais.2022.23.11.217
- 30.Takhdat K, Rebahi H, Rooney DM, Babram MA, Benali A, Touzani S, … El Adib AR. The impact of brief mindfulness meditation on anxiety, cognitive load, and teamwork in emergency simulation training: a randomized controlled trial. Nurse Educ Today. 2024;132:106005. doi.org/10.1016/j.nedt.2023.106005. [DOI] [PubMed]
- 31.Kolb DA, Plovnick MS. The experiential learning theory of career development. Legare Street; 2022.
- 32.Kolb AY, Kolb DA. Learning styles and Learning spaces: enhancing Experiential Learning in Higher Education. Acad Manag Learn Educ. 2005;4:193–212. 10.5465/amle.2005.17268566. [Google Scholar]
- 33.Jeffries PR, Rodgers B, Adamson K. NLN Jeffries Simulation Theory: brief narrative description. Nurs Educ Perspect. 2015;36:292–3. 10.5480/1536-5026-26.5.292. [DOI] [PubMed] [Google Scholar]
- 34.Park S, Lee J. Domestic trends in research on education using augmented reality. J Learn-cent Curric Instr. 2020;20:1–23. 10.22251/JLCCI.2020.20.11.1. [Google Scholar]
- 35.Sedgwick M, Yanicki S, Harder N, Scott D. A scoping review of the integration of ethics education in undergraduate nursing high-fidelity human simulation‐based learning. J Clin Nurs. 2021;30:605–14. 10.1111/jocn.15552. [DOI] [PubMed] [Google Scholar]
- 36.Bang J, Park P. Metaverse R&D promotion strategy reflecting digital ethics and UX. J Broadcast Eng. 2022;27:703–17. 10.5909/JBE.2022.27.5.703. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used and analyzed during the current study are available from the corresponding author on reasonable request.


