Abstract
Background
Parenting a child with disabilities can feel isolating and overwhelming. Understanding the health challenges of parents with disabled children is essential for providing effective healthcare. This study aims to offer a comprehensive view of the health challenges faced by these parents by synthesizing existing literature from various perspectives.
Method
This scoping review conducted using the JBI scoping review method. Searches were performed on PubMed, Web of Science, Scopus, and Google Scholar databases spanning from 2014 to 2024. The initial search yielded 388 articles, with 24 articles undergoing qualitative assessment and data analysis via narrative synthesis.
Results
From the 24 selected articles, three health challenges were identified: physical, emotional, and social health challenges.
Conclusion
Parents of children with disabilities face intricate health challenges, including physical challenges like fatigue, musculoskeletal pain, and sleep issues. Additionally, they experience significant emotional strain, with symptoms of depression, anxiety, and hopelessness. Social isolation and stigma further compound these challenges. A collaborative approach involving healthcare professionals, policymakers, and support organizations can empower parents to thrive in their caregiving roles.
Keywords: Health, Caregiver burden, Parents, Disabled children
Introduction
The journey of parenting is a profound experience marked by love, joy, and challenges. However, for parents raising children with disabilities, the complexities of caregiving are magnified, impacting their physical, emotional, and social well-being [1–2].
Disability is a multifaceted concept encompassing a range of physical, intellectual, developmental, and mental health conditions that impact an individual’s functioning and participation in daily life. Parental health, in the context of caregiving for disabled children, refers to the physical, emotional, and social well-being of parents as they navigate the challenges and responsibilities associated with caring for their child [3–4].
Caring for a child with a disability presents unique challenges for families, often requiring substantial adjustments in their daily lives and can have various effects on their health [5].
The health challenges that families with disabled children faced are complex, varied and multifaceted issue and can have a significant impact on the family’s financial, emotional, and social well-being that requires attention from healthcare providers, policymakers, and society as a whole [6–7]. The stress of caring for a child with a disability can also lead to depression, anxiety, and marital conflict [8–10].
Research has shown that families with disabled children encounter numerous healthcare-related challenges, including accessing appropriate medical care due to inadequate insurance coverage, limited availability of specialized care, and high out-of-pocket costs [11], managing the financial costs of treatment, and navigating the complexities of the healthcare system. These challenges not only affect the well-being of parents but also have implications for the overall family dynamics and the quality of care provided to the disabled child. Moreover, the healthcare needs of children with disabilities are often intertwined with their social, emotional, and educational needs, which can further complicate the situation. Therefore, it is essential to understand the health challenges of families with disabled children and their healthcare needs and develop effective interventions to address these needs [6].
The healthcare needs of families with disabled children encompass a wide range of medical, psychological, and social support services [12]. These needs are further complicated by the financial burden, emotional stress, and time commitment associated with caring for a disabled child. Understanding and addressing these complex needs is crucial for providing comprehensive and effective healthcare for both the disabled child and their family [13].
Given the multifaceted nature of the healthcare needs of parents with disabled children, it is imperative to examine the existing literature and evidence-based practices in order to gain a comprehensive understanding of the challenges they face. By identifying the specific health challenges of these families, healthcare professionals, policymakers, and researchers can develop targeted interventions and support services to address these needs effectively. Only two reviews have examined the challenges faced by families with disabled children, both of which are old, and the study by Neely-Barnes, etal( 2008) is a simple review that did not examine all dimensions of health [14] and the focus of the Piškur etal( 2012) was not on evaluating the parents’ health [15] and the meta-analysis that investigated adverse health in parents of children with disabilities [16] only examined stress index’s health sub-domain in these people. This scoping review aims to provide a comprehensive view of the health challenges faced by parents of disabled children by synthesizing existing literature from diverse disciplinary perspectives.
Methods
This study is a scoping review of the health challenges of parents with disabled children based on the JBI Scoping Review Methodology Group’s methodological guidance [17] and the Prisma extension for scoping review (PRISMA-ScR) [18]. PubMed, Web of Science, Scopus, and Google Scholar databases were searched from January 2014 to February 2024 for English or Persian peer-reviewed articles that were relevant to the research question using qualitative or quantitative, or mixed methods approaches. Review articles also included in the study. However, we did not include various other types of publications, such as research protocols, commentaries, editorials, book chapters, conference abstracts, and other gray literatures. Articles that only addressed the health challenges of disabled children, or focused on other challenges, or studied parents with disabilities or studied the family health challenges during disasters or covid 19 situation were considered as exclusion criteria.
In order to explore the research question “What are the health challenges of parents with disabled children?“, the PECOT (Population, Exposure, Comparisons, Outcome and Time/type of study) method was utilized:
Population: Parents raising children with disabilities.
Exposure: child diagnosed with disabilities.
Comparisons: Parents of children without disabilities.
Outcomes: Health challenges faced by parents of children with disabilities (e.g., mental health, physical health, social well-being, etc.).
Time: January 2014 to February 2024.
Type of Study: Quantitative, qualitative, and mixed-methods studies and review articles.
Based on the PECOT elements, these search terms were used:
Population (P): parent* (parents, caregiver, mothers, fathers, parent-carer*) Or child* (children) Or disabilit* (disability, disabilities, Vision Disabilities, Mobility Disabilities, Auditory Disabilities, Neurological Disabilities, Cognitive Disabilities, Medical Disabilities, Psychological Disabilities, Developmental Disabilities) Or Impairment.
Outcome (O): health* (health, health challenges, well-being), physical health* (physical health, physical problems), mental health* (mental health, stress, anxiety, depression), social health* (social health, social isolation), burden* (burden of care, caregiver burden), quality of life*. We use Boolean operators (AND, OR, NOT) to combine our search terms effectively.
These terms were intentionally broad to ensure that a wide range of relevant articles were included and to ensure that the research team captured a wider range of findings, in accordance with the JBI Scoping Review Methodology.
All articles were screened based on the inclusion/exclusion criteria using the article title, and abstract. Concerns about eligibility for inclusion were addressed by reviewing the full texts in accordance with the methodological approach.
The Mixed Methods Appraisal Tool (MMAT) was used for the quality assessment of the articles [19].
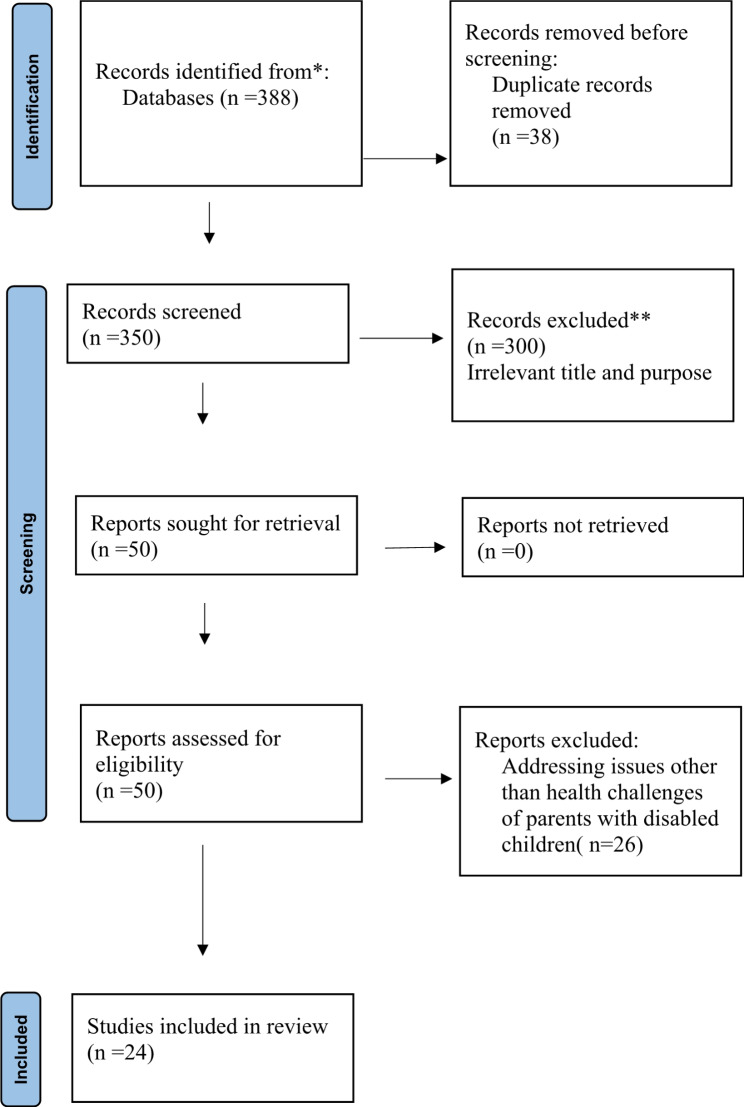
Two researchers (S.S and M.T) independently reviewed the articles for relevance and quality. In case of disagreement, the articles were reviewed by a third researcher (J.S). The final selection was 24 articles out of a total of 388 articles (Fig. 1).
Fig. 1.
PRISMA-SCR flow diagram
From the included studies, the title, authors, design, objectives, description of participants and results were extracted. (Table 1) Due to the diversity in study design, interventions, and outcome measures, the researchers analyzed the data narratively. The narrative synthesis method was employed to address the review question, evaluating various review papers, quantitative studies, and qualitative investigations. According to Popay et al. [20], this method involves formulating a theory of how the intervention works, synthesizing findings, exploring their relationships, and assessing their strength. It primarily relies on textual analysis to review and integrate results from multiple studies in alignment with the scoping review’s objectives.
Table 1.
Relevant studies summary
| code | Researcher, year of publication | Title | Country and study design | Research population/ sample size | Findings | Quality of evidence |
|---|---|---|---|---|---|---|
| 1 | Abdullah MM, et al. (2021) [28] |
Are parental depressive symptoms related to the sleep quality and physical activity of their children with developmental disabilities? |
USA, prospective study | 147 parents of children with developmental disabilities | Parents of children with above-average sleep problems had about twice the odds of depression, and parents of children with above-average exercise problems had about one-and-a-half times the odds. | V |
| 2 | Balbo N & Bolano D.(2024) [30] | Child disability as a family issue: a study on mothers’ and fathers’ health in Italy. | Italy, cross sectional study | 13 000 mothers and fathers (7000 families) of disabled children | Compared to parents of a healthy child, parents of a child with a disability report lower levels of general and mental health and well-being. | V |
| 3 | Bilsin E, et al. (2014) [33] | A review of the relationship between the needs of mothers who have hearing impairment children and their state-trait anxiety levels | Turkey, cross-sectional study | 87mothers who have hearing impairment children | The anxiety level of mothers with hearing impaired children increased negatively as their needs increased. | V |
| 4 | Björquist E, etal(2016) [38] | Parents’ Experiences of Health and Needs When Supporting Their Adolescents with Cerebral Palsy During Transition to Adulthood. | Sweden, qualitative study | 15 mothers and fathers to 10 adolescents with CP aged 17–18 years | Parents’ experiences are illustrated by the main theme “Friction blisters, chafing and healing during transition”. Five sub-themes described parents’ concerns, worries about what was to come, needs for support, coping strategies, and experiences of togetherness, in addition to grief and stress in life | III |
| 5 | Bourke-Taylor HM, et al. (2022) [21] | Fathers of children with a disability: health, work, and family life issues | Australia, mixed-methods study | 33 fathers in families raising children with disabilities | Fathers reported high levels of symptoms of depression (58%), anxiety (37%), and stress (61%). Fathers reported low participation in health-promoting activities less than weekly: planning health activities (58%); exercising alone (26%); social activities (3%); taking time to relax (16%). 64% were in full-time employment, although work was reported to be a challenge because of family responsibilities. Although service interactions were low and delegated to mothers, fathers described direct care of their children. | III |
| 6 | Brekke I & Alecu A. (2023) [31] | The health of mothers caring for a child with a disability: a longitudinal study | Norway, longitudinal study | Mothers and their children without disability, n = 1,574,328 Mild disability, n = 6,343 Complex disability, n = 14,229 | Mothers of children with disabilities are more likely than mothers of children without disabilities to be diagnosed with musculoskeletal conditions, depression, anxiety, insomnia, and migraine. The differences between the two groups of mothers diminish after adjustment for child, mother, and family characteristics, but remain significant for musculoskeletal disorders, depression, anxiety, and sleep disorders, although the absolute differences are modest. | V |
| 7 | Caicedo C. (2014) [27] | Families with special needs children: family health, functioning, and care burden | South Florida, USA, longitudinal study | 84 parents of children with special health care needs | Parents woke with physical fatigue, unable to do their favorite activities and with little energy to do housework or socialize. Cognitive problems with remembering and concentrating on tasks, worrying about the child’s medicines, therapies and side effects, and worrying about the child’s future and the effect of the child’s condition on other family members. Socially, they found it difficult to talk to others, including doctors and nurses, and felt isolated and that people did not understand their family situation. | V |
| 8 | Chen C, etal(2023) [23] | Parents of children with disability: Mental health outcomes and utilization of mental health services | Australia, Longitudinal Study | 4935 children with disability and their parents | At all child ages, parents of children with disabilities had a higher prevalence of mental health problems than parents of children without disabilities. Parents of disabled children aged 12 to 17 years had significantly higher mental health service utilization and costs than parents of nondisabled children (2-year cost differential=$86.37, 95% CI ($15.67-$157.07)). Among parents of children aged 4–11 years, however, these differences were not observed. | V |
| 9 | Coughlin MB& Sethares KA, (2017) [29] | Chronic Sorrow in Parents of Children with a Chronic Illness or Disability: An Integrative Literature Review | USA, integrative review | 19 studies from a literature search | Compared to fathers, mothers experience more intense chronic sorrow. Strong triggers for the resurgence of chronic sorrow are health crises and developmental milestones. | III |
| 10 | DiGiacomo M, et al. (2017) [25] | Experiences and needs of carers of Aboriginal children with a disability: a qualitative study | Australia, qualitative study | 16 mothers and 3 grandmothers of Aboriginal children aged zero-eight with disability | They described their experiences, including the challenges and enablers of care provision and access, the impact on their health and welfare, and the related economic and noneconomic costs of care. For lone caregivers, financial strain and social isolation were particularly prominent. | III |
| 11 | Gilson KM, et al. (2018) [24] | Supporting the mental health of mothers of children with a disability: Health professional perceptions of need, role, and challenges | Australia, qualitative study | 13 health professionals working with families of a child with a disability | Professionals were aware of mothers’ need for mental health support, but were not always clear about their roles and responsibilities in support of maternal mental health. Providers also struggled to respond to mothers’ mental health problems, were not always aware of the best strategies to promote mothers’ mental health, and encountered barriers that could be overcome with training and systemic change. | III |
| 12 | Gilson KM, et al. (2018) [22] | Mental health care needs and preferences for mothers of children with a disability | Australia, cross-sectional study | 294 mothers of children with a disability. | High rates of self-reported clinically significant depression (44%), anxiety (42%), and suicidality (22%) in the past 12 months were reported. High to very high levels of psychological distress were reported by nearly half (48%) of mothers. Only 58% of mothers attempted to access professional support, even though 75% felt they needed it. The main barriers to seeking help were caregiving responsibilities that made scheduling appointments difficult (45%) and not perceiving the mental health problem to be serious enough to require help (36%). Individual counseling was the most preferred type of support (66%). This was followed by professionally guided relaxation (49%) and mental health education (47%). | III |
| 13 | Hagerman TK, et al. (2022) [26] | The Mental and Physical Health of Mothers of Children with Special Health Care Needs in the United States | USA, National Survey |
102,341 children ages 0–17 including 23,280 CSHCN. |
Compared with non-CSHCN, moms of children with special health care needs were twice as likely to have poor mental and physical health (mental 10.3% versus 4.0%, p < 0.001; physical 11.9% versus 5.0%, p < 0.001). In regression models, an increase in the number of special health care needs and the severity of activity limitations were associated with significantly higher odds of poor maternal health. | V |
| 14 | Joung WJ. (2023) [41] | Phenomenological Study on the Lived Experiences of Mothers Caring for Their Pubescent Children with Developmental Disabilities | Korea, qualitative study | 9 mothers caring for pubescent children with developmental disabilities | The lived experiences of mothers who cared for adolescent children with DDs were grouped into four themes and nine sub-themes from 19 units of meaning (1) not being allowed to enjoy the growth of the child due to an imbalance in the rate of growth, (2) feeling ostracized along with the disabled child, (3) feeling like a slow and permanent expulsion from society, and (4) reorienting the direction and purpose of caregiving. | III |
| 15 | Kocherova OIu, (2014) [35] | Psychological features of mothers bringing up disabled children [Article in Russian] | Russia, survey | 60 mothers bringing up children of early age with infantile cerebral palsy and 50 mothers of children with compensation of perinatal affections of the central nervous system by the 1 life year | Mothers who raise handicapped children are more likely to suffer from emotional disturbances, have a negative attitude to divorce, and are less likely to assign a primary role in a family to their husbands. | V |
| 16 | Masefield SC, et al. (2021) [32] |
The Effects of Caring for Young Children with Developmental Disabilities on Mothers’ Health and Healthcare Use: Analysis of Primary Care Data in the Born in Bradford Cohort |
Bradford UK, Cohort |
477 caregivers of preschool disabled children and 7250 other mothers |
Caregiving mothers had higher odds of symptoms of psychological distress (odds ratio 1,24; 95% CI 1,01, 1,53), fatigue (1,42; 1,12, 1,80), and possibly headache and muscle pain (1,18; 0,97, 1,43). Despite the higher prevalence of symptoms, they were not more likely to use health care services and may be less likely to seek health care for psychological distress (0.64; 0.40, 1.02). There was a general association between socio-economic deprivation and poorer health. | V |
| 17 | Masulani-Mwale C, etal.(2016) [39] | Parenting children with intellectual disabilities in Malawi: the impact that reaches beyond coping? | Malawi, qualitative study | 10 focus group discussions and four in-depth interviews with parents who had children diagnosed with intellectual disability | There are a number of challenges associated with caring for children with intellectual disabilities. Parents have limited access to services for their children, let alone for their own mental health issues; they face stigma and discrimination; they have mental health problems as a result of being a caregiver; they have suicidal thoughts; and in some cases, have even been forced by neighbours to kill their disabled child. In order to cope with these problems, most of the parents cope through their spirituality. | III |
| 18 | Miodrag N, et al. (2015) [16] | Adverse health in parents of children with disabilities and chronic health conditions: a meta-analysis using the parenting stress index’s health sub-domain | USA, meta-analysis | 19 eligible studies. | Parents of children with DD/CHC reported higher PSI health problem scores, with a weighted mean effect size of 0.39 (95% CI = 0.23–0.55), compared with parents of children without DD/CHC. | V |
| 19 | Nazzal MS & Al-Rawajfah OM. (2017) [40] | Lived experiences of Jordanian mothers caring for a child with disability | Jordan, qualitative study | 7 mothers of children with disability | Four main themes emerged from the mothers’ experiences, including increased stigma, fear for the future, increased caregiving burden, and adjusting to the child’s disabilities. | III |
| 20 | Ranehov L & Håkansson C. (2019) [37] | Mothers’ experiences of their work as healthcare assistants for their chronic disabled child | Sweden, qualitative study |
9 mothers who had a child aged 8–17 years old with a cognitive or/and physical chronic disability. |
The mothers in the study had to be on call for their child at all times. They emphasized the physical and psychological health problems caused by their work situation. | III |
| 21 | Rizvi Jafree S, Burhan SK. (2020) [36] | Health challenges of mothers with special needs children in Pakistan and the importance of integrating health social workers | Pakistan, qualitative study | 21 mothers of special needs children |
Mothers faced significant and salient challenges in eight subcategories of mental health (constant stress due to structural failures, fear of social shame and avoidance of public exposure, fear of public assault, morbid feelings and anticipation of child’s death, acceptance of blame for child’s condition, and feelings of depression). Morbid feelings and anticipation of child’s imminent death, Acceptance of blame for child’s condition and feelings of depression, Anxiety about marriage of children with special needs Mood swings and erratic outbursts constant physical fatigue, migraine headaches and sleeplessness, muscular and joint pain or bone loss, hypertensive disorders, diabetes and nutrition problems, physical abuse and self-harm, consequences of contraception and hysterectomies). |
III |
| 22 | Whiting M. (2014) [7] | Children with disability and complex health needs: the impact on family life | UK, qualitative study | parents from 33 families that included one or more child with disabilities | Childhood disability has many impacts on the family. For the most part, these effects cannot be easily defined or described in the context of a particular “medical” diagnosis or prognosis. Many elements of impact seem unrelated to whether or not a child has a life-threatening or life-limiting condition, or whether or not a child requires specific medical equipment or ongoing care. | III |
| 23 | Xia C, et al. (2023) [10] | Depression and Associated Factors among Family Caregivers of Children with Disabilities: Analysis of Intergenerational Differences | China, cross-sectional study | 380 parents and 108 grandparents of children with disabilities | There was no statistical difference between parents (35.5%) and grandparents (32.4%) in the risk of depression. Child sleep problems (AOR = 1,751, 95%CI = 1,019, 3,008), harmonious family relationships (AOR = 0,694, 95%CI = 0,569, 0,846) and better accessibility (AOR = 0,742, 95%CI = 0,568, 0,970) were significantly associated with parental depression. Higher education (AOR = 4,108, 95%CI = 1,526, 11,057) and taking care of children with frequent mood changes (AOR = 2,242, 95%CI = 1,161, 4,329) were associated with higher risk of depression. Owning a home (AOR = 0.167, 95%CI = 0.031, 0.887), having a more cohesive family (AOR = 0.545, 95%CI = 0.297, 1.000), and having a more accessible home (AOR = 0.401, 95%CI = 0.185, 0.869) were associated with lower odds of depression. | V |
| 24 | Yilmaz G. (2020) [34] | Mothers with disabled children: needs, stress levels and family functionality in rehabilitation. | Turkey, cross-sectional study | 181 mothers with disabled children | Mothers were found to have high information needs, moderate stress levels, and moderate family functionality in rehabilitation. They concluded that mothers’ stress levels rose with increasing need, whereas their stress levels declined with increasing rehabilitation function. | V |
Results
Description of studies
The database search identified a total of 388 potentially relevant articles. After screening titles and abstracts, 50 potentially relevant articles were identified. All 50 articles were assessed at full-text level, resulting in 24 relevant articles for analysis.
Most of the articles that met the inclusion criteria were carried out in Australia [21–25] and the United States [26–30]. The results of the studies were analyzed based on the countries studied (European, African, Asian, American, and Australian countries). The results indicated no differences among the findings in the various countries. Twelve articles were quantitative studies [10, 22–23, 27, 28, 29, 31, 32, 33, 34, 35, 16], nine were qualitative studies [7, 24–25, 36, 37, 38, 39, 40, 41]. One article utilized a mixed methods approach [21], and two were review articles [9, 26]. (Table 1). All articles are of good quality. A total of 24 studies involving 1,717,852 parents have been included in this review. The reviewed studies consist of 3 on parents of children with developmental disabilities [29, 33, 41], 3 on parents of children with physical and intellectual disabilities [16–36, 38], 2 on parents of children with medical disabilities [27–28], 1 on parents of children with intellectual disabilities [39], 1 on parents of children with auditory disabilities [34], and others that cover parents of children with all types of disabilities (not specified) (7–10,16, 21–22, 24–25, 31–32, 35, 37, 40).
Analysis of the studies
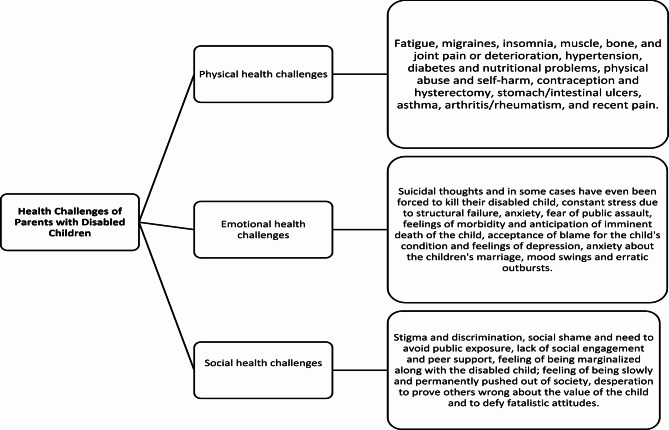
Results were categorized into three main groups: physical, emotional, and social health challenges (Fig. 2).
Fig. 2.
Findings based on narrative synthesis
Physical health challenges
This theme is about parents’ illnesses or impairments that are related to the care of their child with a disability and that affect the parents’ physical well-being or ability to function optimally. Among the 24 studies reviewed, 10 highlighted the challenges faced by parents in maintaining good physical health while caring for their disabled child [10, 21, 27, 28, 29, 31, 32, 33, 36–37].
One of the most common physical health challenges reported by parents in studies was poor physical health, often due to the stress and demands of caregiving [27, 31, 36–37]. Muscle, bone, and joint pain or deterioration were reported in several studies, highlighting the physical toll of long-term caregiving Parents experienced head and musculoskeletal pain, which could be attributed to the physical strain of caregiving tasks, such as lifting and maneuvering their child [32–33, 36].
Constant physical fatigue was another issue reported among parents. The demands of caregiving, coupled with emotional and mental stress, often left parents feeling exhausted and drained, affecting their ability to engage in daily activities [28, 33, 36].
Migraines were a significant concern for some parents, with studies indicating that the stress and emotional burden of caregiving could trigger or exacerbate migraine episodes [32, 36]. Insomnia and sleep problems were also reported, likely due to the overwhelming responsibilities and worries associated with caring for a disabled child [10, 29, 32].
Conditions such as hypertension and high blood pressure were also reported, possibly linked to chronic stress and lack of self-care opportunities for parents. Diabetes and nutritional issues were additional challenges faced by some parents, often exacerbated by the demands of caregiving and limited time for proper meal planning and self-care. Physical abuse and self-harm were alarming findings, suggesting that the stress and emotional strain of caregiving could lead to harmful coping mechanisms among some parents [36]. Overall, the severity of activity limitations due to physical health issues was a common theme, with many parents expressing frustration at being too tired to do the things they liked or needed to do, further impacting their overall well-being [21].
The use of contraception and hysterectomy were also discussed due to fear of deformities in future children and lack of time and money to have more children, further complicating their physical health challenges [36].
Emotional health challenges
This theme refers to difficulties or disruptions in parents’ emotional well-being and psychological resilience as a result of caring for their child with a disability. Of the 24 studies reviewed, 20 highlighted the profound emotional health challenges experienced by parents in this context [7, 10, 26, 21, 22, 23, 24, 28, 29, 30, 31, 32, 33, 34, 35, 16, 36, 38–39].
Depressive symptoms, including feelings of sadness, hopelessness, and low mood, were common among parents caring for children with disabilities. These symptoms often coincided with lower levels of mental health and increased levels of anxiety, creating a complex emotional burden for parents. Parents reported experiencing worry, sadness, and stress in their lives, and worried about what the future held for their child and themselves. Many felt frustrated, helpless, and hopeless in their caregiving role, leading to feelings of anger and ongoing stress symptoms [10, 21–22, 28, 29, 30, 32, 33, 34, 35, 36, 38].
Cognitive problems, such as difficulty remembering and concentrating on tasks, were also reported, likely due to the emotional burden of caregiving and concern for their child’s well-being [28].
The need for mental health support was a recurring finding in all 20 studies, as parents struggled with emotional disturbance, psychological distress, and anxiety about the future [7, 10, 26, 21, 22, 23, 24, 28, 29, 30, 31, 32, 33, 34, 35, 16, 36, 38–39].
Some reported suicidal ideation, including thoughts of harming their disabled child, highlighting the extreme psychological distress experienced by some parents [22, 39]. Parents faced the emotional burden of awaiting the death of their child, compounded by fears of public assault and morbid feelings. Despite the development of coping strategies, many parents continued to experience an increased perceived caregiving burden and struggled with feelings of guilt and blame for their child’s condition. Fear of social shaming and intense chronic sorrow added to the emotional challenges, making it difficult for parents to openly discuss their problems and needs with others, including health care professionals [23, 31, 16–36, 38].
Furthermore, the emotional issues were exacerbated by limited access to services for their children, let alone adequate support for their own psychological issues. This led to higher mental health service utilization and costs, as parents sought ways to manage their emotional well-being amidst challenging circumstances [39].
Social health challenges
Social health challenges refer to difficulties or barriers that parents of children with disabilities face in maintaining positive social interactions, relationships, and overall well-being in society. Of the 24 studies reviewed, 10 highlighted the social health challenges experienced by these parents [10, 21, 25, 33, 16–36, 39, 40–41].
Parents reported increased perceived stigma associated with having a child with a disability, resulting in low participation in social activities. Many parents felt socially isolated and marginalized, particularly when faced with financial strain and social isolation due to the demands of caregiving. Parents often had to avoid public exposure and be constantly on call for their child’s needs, which further limited their access to health services. They also experienced stigma and discrimination from society, which affected their ability to participate in health-promoting activities and to relax [21, 25, 28, 36, 39–41].
The economic and non-economic costs of caregiving contributed to the socioeconomic disadvantage of some parents, leading them to seek health care less frequently and to develop negative attitudes toward divorce, possibly due to the added complexity and responsibility of their situation [16, 33].
Feelings of being kicked out of society slowly and permanently were prevalent among parents, especially as they felt compelled to give the leading role in the family to the husband, leading to a lack of understanding of their family situation by others [41].
Despite these challenges, parents expressed desperation to prove others wrong about the value of their child and defy fatalistic attitudes. They also felt apprehensive about the marriage prospects of their special needs children, concerned about potential challenges and societal perceptions [36].
Mood swings and erratic outbursts were common among parents, reflecting the emotional turmoil and stress they experienced. However, some parents also reported experiences of cohesion within their support networks and a strong need for support from their communities and healthcare providers [10, 36].
Discussion
Parenting children with disability can be particularly challenging, especially when children have complex conditions. Parents may struggle to manage their child’s health and their own emotions, leading to poorer health outcomes for the family. This scoping review has shed light on the complex and multifaceted health challenges faced by parents raising children with disabilities. By synthesizing findings from 24 studies, we identified a significant burden experienced across physical, emotional, and social domains. The review included parents of children with a broad spectrum of disabilities.
The study supports the biopsychosocial model of health [42], which emphasizes the interconnectedness of biological, psychological, and social factors in health outcomes. The findings highlight the physical health problems (biological), emotional challenges (psychological), and social difficulties (social) faced by parents caring for children with disabilities. The findings are also consistent with caregiver strain theory [43], which suggests that the demands of caregiving can lead to physical, emotional, and social problems for caregivers. The findings describe the physical strain, emotional exhaustion, and social isolation experienced by parents.
The review is consistent with existing research [7, 10, 16, 21–41] that highlights the toll that caregiving can take on parents’ physical well-being. Fatigue, musculoskeletal pain, and sleep problems emerged as prominent concerns, likely due to the physical demands and chronic stress associated with caring for a child with a disability. Our findings also underscore the profound emotional impact of caregiving. Depressive symptoms, anxiety, hopelessness, and feelings of isolation were common among parents. The review highlights the significant social challenges that parents face. Social stigma, marginalization, and limited social interaction were consistently reported. These challenges may be exacerbated by feelings of guilt, social isolation, and limited access to support networks or health services. It’s important to note that these challenges can interact to create a vicious cycle. Chronic stress can exacerbate social isolation, which can make self-care even more difficult, leading to further emotional and physical challenges.
While the review is consistent with existing literature on specific challenges [7, 10, 16, 21–41], it does so with a broader scope that includes physical, emotional, and social dimensions. This holistic perspective provides a more comprehensive understanding of the multifaceted health burden experienced by parents.
The findings of this review have important implications for health care providers, policy makers, and support organizations. Recognizing the multifaceted health challenges experienced by parents is an important first step. Health care providers should be encouraged to screen for physical and mental health problems during routine check-ups. Policymakers could allocate resources to support services that address parents’ specific needs, such as affordable child care and mental health services. Support organizations could develop programs that promote social connections and provide education on coping mechanisms.
This scoping review provides valuable insights into health challenges of parents of children with disabilities and highlights the need for further research and tailored interventions.
By recognizing the multifaceted health challenges and addressing parents’ needs through targeted interventions, we can create a more supportive environment that empowers parents to raise their children with disabilities and promotes their own well-being. Further research is needed to identify and evaluate effective interventions to improve the health and well-being of these dedicated parents.
It is crucial to support parents of children with disabilities for their well-being. Parent Training Programs help parents develop skills and problem-solving approaches. Contextually-Appropriate and Culturally-Sensitive Interventions tailor interventions to the socio-economic settings and cultural context of the parents, train local community workers, and involve other parents with children with disabilities using community resources to provide parent training and support interventions. Positive, Proactive Approaches include resources, strategies, and evidence-based practices that support parents, educators, and families in meeting requirements and enhancing their health.
Limitations
The studies in this review included parents of children with a wide range of disabilities. The impact on parents may vary depending on the type and severity of the disability. In addition, exploring the coping mechanisms used by parents and the role of support networks may provide valuable insights and need to be evaluated in further studies.
This study covered and analyzed the articles of the last 10 years from 4 databases. Although it is approved by the JBI Scoping Reviews method, expanding the time frame and combining additional databases can increase the investigation of factors affecting the health of parents with disabled children.
Conclusion
This scoping review highlights the complex health challenges experienced by parents of children with disabilities. The findings highlight the physical toll of caregiving, with parents reporting fatigue, musculoskeletal pain, and sleep problems. These problems are likely due to the constant demands of caregiving and chronic stress. In addition, the report highlights the significant emotional toll on parents. Symptoms of depression, anxiety and hopelessness were common, highlighting the need for comprehensive mental health support. Social isolation and stigma were also identified as key challenges, potentially leading to feelings of marginalization and hindering access to health services. By promoting a collaborative approach involving healthcare professionals, policymakers and support organizations, we can create a more supportive environment that empowers parents to thrive in their caregiving roles.
Acknowledgements
This research is the outcome of a project at the Tarbiat Modares University and Health Metrics Research Center, Institute for Health Sciences Research, ACECR. We appreciate the staff of Tarbiat Modares University and ACECR.
Author contributions
S.S and M.T reviewed texts, designed research, collected and organized data, analyzed data, and prepared the article draft; they corrected the final version of the article. J.S, R.M.K, and R.R performed data analysis, collaborated on compiling the final report, reviewed the article, and corrected and approved its final version.
Funding
There is no specific grant for this research from any funding agency in the public, commercial or non -for- profit sectors.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval
N/A.
Patient and public involvement
Patients or the public were not involved in the research.
Patient consent for publication
Not applicable.
Province and peer review
Not commissioned; externally peer reviewed.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Billen RM, Sams J, Nordquist VM. A conceptual model of parenting children with disabilities. J Fam Stud. 2023;29(4):1781–803. 10.1080/13229400.2022.2085617 [Google Scholar]
- 2.Hodgkinson S, Clarke D. Parenting a child with disability: a review of research on parental stress. Child Youth Serv Rev. 2018;88:227–40. [Google Scholar]
- 3.World Health Organization. Disability. https://www.who.int/health-topics/disability#tab=tab_1[11.5.2024]
- 4.Sulaimani GH, Kamel S, Alotaibi G, Telmesani N. Quality of life among family caregivers of disabled children in Saudi Arabia. Cureus. 2023;15(7):e41320. 10.7759/cureus.41320. PMID: 37539394; PMCID: PMC10395756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moosa-Tayob S, Risenga PR. Challenges of caregivers providing care to children with disabilities at non-governmental organisations in Tshwane townships, South Africa. Afr J Disabil. 2022;11:930. 10.4102/ajod.v11i0.930. PMID: 35936924; PMCID: PMC9350488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Academies of Sciences, Engineering, and, Health M, and Medicine Division; Board on Health Care Services; Committee on Improving Health Outcomes for Children with Disabilities. Opportunities for Improving ProgramsServices for Children with Disabilities. Byers E, Valliere FR, Houtrow AJ, editors. Washington (DC): National Academies Press (US); 2018 May 11. PMID: 30088879. [PubMed]
- 7.Whiting M. Children with disability and complex health needs: the impact on family life. Nurs Child Young People. 2014;26(3):26–30. 10.7748/ncyp2014.04.26.3.26.e388. PMID: 24708336. [DOI] [PubMed]
- 8.McConnell D, Savage A. Stress and resilience among families caring for children with intellectual disability: expanding the research agenda. Curr Dev Disord Rep. 2015;2:100–9. 10.1007/s40474-015-0040-z [Google Scholar]
- 9.Park GA, Lee ON. The moderating effect of social support on parental stress and depression in mothers of children with disabilities. Occup Ther Int. 2022;2022:5162954. 10.1155/2022/5162954. PMID: 35359427; PMCID: PMC8938151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia C, Wei T, Tang Q, Zheng H, Chen G, Lu J. Depression and associated factors among family caregivers of children with disabilities: analysis of intergenerational differences. Healthc (Basel). 2023;11(19):2693. 10.3390/healthcare11192693. PMID: 37830730; PMCID: PMC10572526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adugna MB, Nabbouh F, Shehata S, Ghahari S. Barriers and facilitators to healthcare access for children with disabilities in low and middle income sub-saharan African countries: a scoping review. BMC Health Serv Res. 2020;20(1):15. 10.1186/s12913-019-4822-6. PMID: 31906927; PMCID: PMC6945633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tétreault S, Blais-Michaud S, Deschênes M, Beaupré P, Gascon P, Boucher H, N., Carrière M. How to support families of children with disabilities? An exploratory study of social support services. Child Family Social Work. 2012;19(3):272–81. 10.1111/j.1365-2206.2012.00898.x [Google Scholar]
- 13.Goudie A, Narcisse MR, Hall DE, Kuo DZ. Financial and psychological stressors associated with caring for children with disability. Fam Syst Health. 2014;32(3):280–90. 10.1037/fsh0000027. Epub 2014 Apr 7. PMID: 24707826; PMCID: PMC4315505. [DOI] [PMC free article] [PubMed]
- 14.Neely-Barnes SL, Dia DA. Families of children with disabilities: a review of literature and recommendations for interventions. J Early Intensive Behav Intervention. 2008;5(3):93–107. 10.1037/h0100425 [Google Scholar]
- 15.Piškur B, Beurskens AJ, Jongmans MJ, Ketelaar M, Norton M, Frings CA, Hemmingsson H, Smeets RJ. Parents’ actions, challenges, and needs while enabling participation of children with a physical disability. 2012;177. PMID: 23137071. [DOI] [PMC free article] [PubMed]
- 16.Kocherova OIu, Fil’kina OM, Dolotova NV, Malyshkina AI, Antysheva EN. Psychological features of mothers bringing up disabled children. Vestn Ross Akad Med Nauk. 2014;(5–6):98–101. Russian. 10.15690/vramn.v69i5-6.1051. PMID: 25558688. [DOI] [PubMed]
- 17.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126. 10.11124/JBIES-20-00167. PMID: 33038124. [DOI] [PubMed]
- 18.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 19.Hong QN, Fàbregues S, Bartlett G, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inform. 2018;34(4):285–91. [Google Scholar]
- 20.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M et al. Narrative synthesis in systematic reviews: a product from the ESRC methods programme. ESRC Methods Program. 2006;(2006):93.
- 21.Bourke-Taylor HM, Cotter C, Joyce KS, Reddihough DS, Brown T. Fathers of children with a disability: health, work, and family life issues. Disabil Rehabil. 2022;44(16):4441–51. Epub 2021 Apr 25. PMID: 33896319. [DOI] [PubMed] [Google Scholar]
- 22.Gilson KM, Davis E, Johnson S, Gains J, Reddihough D, Williams K. Mental health care needs and preferences for mothers of children with a disability. Child Care Health Dev. 2018;44(3):384–91. 10.1111/cch.12556. Epub 2018 Feb 12. PMID: 29430692. [DOI] [PubMed] [Google Scholar]
- 23.Chen C, Bailey C, Baikie G, Dalziel K, Hua X. Parents of children with disability: mental health outcomes and utilization of mental health services. Disabil Health J. 2023;16(4):101506. 10.1016/j.dhjo.2023.101506. Epub 2023 Jul 6. PMID: 37517905. [DOI] [PubMed] [Google Scholar]
- 24.Gilson KM, Johnson S, Davis E, Brunton S, Swift E, Reddihough D, Williams K. Supporting the mental health of mothers of children with a disability: health professional perceptions of need, role, and challenges. Child Care Health Dev. 2018;44(5):721–729. 10.1111/cch.12589. PMID: 30133770. [DOI] [PubMed]
- 25.DiGiacomo M, Green A, Delaney P, Delaney J, Patradoon-Ho P, Davidson PM, Abbott P. Experiences and needs of carers of aboriginal children with a disability: a qualitative study. BMC Fam Pract. 2017;18(1):96. 10.1186/s12875-017-0668-3. PMID: 29187141; PMCID: PMC5707922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miodrag N, Burke M, Tanner-Smith E, Hodapp RM. Adverse health in parents of children with disabilities and chronic health conditions: a meta-analysis using the parenting stress index’s health sub-domain. J Intellect Disabil Res. 2015;59(3):257–71. 10.1111/jir.12135. Epub 2014 Apr 24. PMID: 24762325. [DOI] [PubMed] [Google Scholar]
- 27.Hagerman TK, McKernan GP, Carle AC, Yu JA, Stover AD, Houtrow AJ. The mental and physical health of mothers of children with special health care needs in the United States. Matern Child Health J. 2022;26(3):500–10. 10.1007/s10995-021-03359-1. Epub 2022 Jan 24. PMID: 35072870. [DOI] [PubMed] [Google Scholar]
- 28.Caicedo C. Families with special needs children: family health, functioning, and care burden. J Am Psychiatr Nurses Assoc. 2014;20(6):398–407. 10.1177/1078390314561326. Epub 2014 Nov 26. PMID: 25428686. [DOI] [PubMed]
- 29.Abdullah MM, Neville RD, Donnelly JH, Lakes KD. Are parental depressive symptoms related to the sleep quality and physical activity of their children with developmental disabilities? Res Dev Disabil. 2021;119:104091. 10.1016/j.ridd.2021.104091. Epub 2021 Oct 9. PMID: 34634581. [DOI] [PubMed] [Google Scholar]
- 30.Coughlin MB, Sethares KA. Chronic sorrow in parents of children with a chronic illness or disability: an integrative literature review. J Pediatr Nurs 2017;37:108–16. 10.1016/j.pedn.2017.06.011. Epub 2017 Jul 24. PMID: 28751135. [DOI] [PubMed]
- 31.Balbo N, Bolano D. Child disability as a family issue: a study on mothers’ and fathers’ health in Italy. Eur J Public Health. 2024;34(1):79–84. 10.1093/eurpub/ckad168. PMID: 37798136; PMCID: PMC10843958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brekke I, Alecu A. The health of mothers caring for a child with a disability: a longitudinal study. BMC Womens Health. 2023;23(1):639. 10.1186/s12905-023-02798-y. PMID: 38037017; PMCID: PMC10688054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masefield SC, Prady SL, Sheldon TA, et al. The effects of caring for young children with developmental disabilities on mothers’ health and healthcare use: analysis of primary care data in the born in Bradford cohort. J Dev Phys Disabil. 2022;34:67–87. 10.1007/s10882-021-09789-7 [Google Scholar]
- 34.Bilsin E, Çuhadar D, Göv P. A review of the relationship between the needs of mothers who have hearing impairment children and their state-trait anxiety levels. J Pediatr Nurs. 2015;30(1):254–61. Epub 2014 Jul 31. PMID: 25131517. [DOI] [PubMed]
- 35.Yilmaz G. Mothers with disabled children: needs, stress levels and family functionality in rehabilitation. Scand J Caring Sci. 2020;34(2):524–32. 10.1111/scs.12783. Epub 2019 Nov 20. PMID: 31747083. [DOI] [PubMed] [Google Scholar]
- 36.Rizvi Jafree S, Burhan SK. Health challenges of mothers with special needs children in Pakistan and the importance of integrating health social workers. Soc Work Health Care. 2020;59(6):408–429. 10.1080/00981389.2020.1781738. PMID: 32614737. [DOI] [PubMed]
- 37.Ranehov L, Håkansson C. Mothers’ experiences of their work as healthcare assistants for their chronic disabled child. Scand J Occup Ther. 2019;26(2):121–34. Epub 2018 Jul 8. PMID: 29983089. [DOI] [PubMed] [Google Scholar]
- 38.Björquist E, Nordmark E, Hallström I. Parents’ experiences of health and needs when supporting their adolescents with cerebral palsy during transition to adulthood. Phys Occup Ther Pediatr. 2016;36(2):204–16. Epub 2015 Dec 7. PMID: 26642865. [DOI] [PubMed] [Google Scholar]
- 39.Masulani-Mwale C, Mathanga D, Silungwe D, Kauye F, Gladstone M. Parenting children with intellectual disabilities in Malawi: the impact that reaches beyond coping? Child Care Health Dev. 2016;42(6):871–80. 10.1111/cch.12368. Epub 2016 Jul 15. PMID: 27416799. [DOI] [PubMed] [Google Scholar]
- 40.Nazzal MS, Al-Rawajfah OM. Lived experiences of Jordanian mothers caring for a child with disability. Disabil Rehabil. 2018;40(23):2723–33. Epub 2017 Jul 18. PMID: 28715919. [DOI] [PubMed] [Google Scholar]
- 41.Joung WJ. Phenomenological study on the lived experiences of mothers caring for their pubescent children with developmental disabilities. Asian Nurs Res (Korean Soc Nurs Sci). 2023;17(4):226–34. 10.1016/j.anr.2023.09.001. Epub 2023 Sep 14. PMID: 37716423. [DOI] [PubMed] [Google Scholar]
- 42.Papadimitriou G. The biopsychosocial model: 40 years of application in psychiatry. Psychiatriki. 2017;28(2):107–110. Greek, Modern, English. 10.22365/jpsych.2017.282.107. PMID: 28686557. [DOI] [PubMed]
- 43.Liu Z, Heffernan C, Tan J. Caregiver burden: a concept analysis. Int J Nurs Sci. 2020;7(4):438–45. 10.1016/j.ijnss.2020.07.012. PMID: 33195757; PMCID: PMC7644552. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.