Abstract
The Covid-19 pandemic challenged health care delivery systems worldwide. Many acute care hospitals in communities that experienced surges in cases and hospitalizations had to make decisions such as rationing scarce resources. Hospitals serving low-income communities, communities of color, and those in other historically marginalized or vulnerable groups reported the greatest operational impacts of surges. However, cross-institutional collaborations within jurisdictions offer unique opportunities to prevent or mitigate health disparities in resource utilization and access to care. In January 2020, in response to the emerging coronavirus epidemic, the San Francisco Department of Public Health (SFDPH) and local hospital and health systems partners convened to align and coordinate medical surge planning and response. Adopting a governance structure of mutual accountability and transparency, the San Francisco Health Systems Collaborative guided local medical and public health response in the areas of medical surge, vaccination administration, testing, and therapeutics. Four principles guided the collaborative response: (1) shared priorities, (2) clear governance and accountability, (3) data transparency, and (4) operational coordination. High-level priorities established included protecting vulnerable people, protecting health care workers, and maintaining health system capacity. The governance structure consisted of three layers: local hospital and health systems’ CEOs coordinating with SFDPH executives; hospital chief medical and nursing officers coordinating high-level surge capacity assessments and mitigation plans; and local clinical operational managers working with public health response operational leaders to coordinate scarce resource utilization. Fluctuating with the tempo of the disease indicators and medical surge, governance and coordination were maintained through a tiered meeting and reporting system. Data visibility and transparency were key principles facilitating operational decision-making and executive-level coordination of resources, including identifying additional surge bed capacity for use systemwide, as well as ensuring efficient and equitable vaccine distribution through implementation of five mass-vaccination sites with prioritized access for vulnerable communities. Applying these four principles of shared priorities, accountability, transparency, and operational coordination and pragmatism helped the public health and individual hospital systems make contributions to the overall response that were aligned with their unique strengths and resources. Publication here represents the first official public use of the name San Francisco Health Systems Collaborative (which had served as the term used internally to refer to the group) and the first time codifying this structure. Through this coordination, San Francisco achieved one of the lowest Covid-19 death rates and had one of the highest vaccination and booster rates, compared with rates across California or the United States. Similar principles and implementation methods can be adopted by other health jurisdictions for future emergency outbreak response.
The Covid-19 pandemic strained health care delivery systems globally, leading to resource shortages and necessitating stringent public health measures, such as shelter-in-place orders and reduced routine care. Hospitals faced challenges in rationing scarce resources and transferring critically ill patients to institutions with available resources.1–3 Additionally, the pandemic exacerbated existing health disparities affecting historically disadvantaged and underresourced groups, including communities of color and low-income populations. These populations had higher burden of disease and case mortality and lower access to therapeutics and vaccinations.4–8 Similar disparities were observed in San Francisco, with higher Covid-19 case rates and hospitalizations among Black or African American and Hispanic or Latino/a individuals residing in low-income neighborhoods.9,10 This report describes a notably close and multifaceted collaboration among large private and public health care delivery systems and local governmental agencies in San Francisco to implement a coordinated, high-impact response to the Covid-19 pandemic.
Methods
Study Design
This is a retrospective, descriptive account of a collaborative effort of independent health care systems and a public health department involving the design, implementation, and quality improvement efforts of a response coordinated across multiple institutions during the height of the Covid-19 pandemic. Following a narrative description of the intervention’s structure and operating principles, outcomes reported include qualitative and quantitative data and feedback regarding application of the principles. This study was deemed exempt from full institutional review by the University of California San Francisco (UCSF) Institutional Review Board.
Setting
San Francisco, California, is a city and county of approximately 800,000 residents, with a prepandemic daytime population of more than 1 million.11,12 As a cultural and commercial hub of the San Francisco Bay Area (population greater than 7 million), the city of San Francisco hosts a number of acute care hospitals operating within multicounty entities with regional patient membership: Dignity Health, Kaiser Permanente, Sutter Health, and UCSF Health. In addition, several large entities serving the San Francisco community include Chinese Hospital, a Veterans Administration Health Care System hospital, a number of Federally Qualified Health Centers, and the San Francisco Health Network (SFHN), which is the health care delivery system operated by the San Francisco Department of Public Health (SFDPH).
More than 96% of San Franciscans have health insurance, and approximately 80% hold private health insurance.13 The local health care facilities, including large health systems and hospitals, routinely collaborate with each other and across the region to share information for the purpose of disaster preparedness and response. Collaboration occurs through regular meetings of CEOs of hospitals, monthly preparedness meetings and exercises coordinated by the SFDPH’s unit for Public Health Emergency Preparedness and Response, and the local emergency medical system agency. The latter two groups also manage mutual aid allocation for the county in the setting of regional acute disaster situations (e.g., wildfires, earthquakes, etc.). Additionally, the chief nursing officers (CNOs) from each major hospital meet periodically to share updates.
In January 2020, SFDPH initiated its emergency response and incident command system to monitor the evolving outbreak of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Wuhan, China. Although much was unknown about the potential magnitude of impact of the virus locally, San Francisco’s public health and health care delivery system leaders took the opportunity to draw on past emergency preparedness efforts to enhance monitoring and contingency planning. To augment existing hospital surge frameworks, SFDPH and the San Francisco Hospital Council (CEOs’ group) assigned chief medical officers (CMOs) and CNOs from acute care hospitals to assess surge capacity and existing plans and to develop a comprehensive Covid-19 hospital surge plan for the city. As the pandemic unfolded and its impacts were felt in San Francisco in the subsequent months, the health systems and SFDPH collaborated on various aspects of response, including sharing information; adapting operations based on federal, state, or local health orders; accessing Covid-19 response resources; and managing Covid-19 vaccination, testing, and therapeutic resources.
Principles of the Health Systems Collaborative
Four principles have guided the San Francisco Health Systems Collaborative (HSC) efforts: (1) shared objectives, (2) disciplined governance, (3) data transparency, and (4) a commitment to operational collaboration. Although this report is a retrospective review of the structure and outcomes of the HSC, these four principles, and the operational and communication norms that reinforced them, were periodically explicitly named, discussed, and negotiated in the regular meetings of the different collaborative cohorts. Below, we elaborate upon these principles and describe examples of each in the work of the HSC.
Principle 1. Shared Objectives
In addition to establishing the four guiding principles, in March 2020, SFDPH defined five top strategic priorities for the Covid-19 response: (1) protect vulnerable populations, (2) protect health care workers, (3) mitigate transmission, (4) optimize surge, and (5) expand capacity for testing.14,15 These priorities were communicated with internal and external stakeholders across the city to identify opportunities for collaboration and alignment among public, private, and community-based entities. In the earliest days of the response, the HSC focused efforts on objectives number 2 (protect health care workers) and number 4 (optimize surge) through coordination of personal protective equipment resource distribution and mutual aid and through intentional and collaborative surge planning, as described below. As conditions evolved and advancements for Covid-19 therapeutics and vaccines materialized, the HSC shifted its aims to address additional objectives focused on ensuring continuous and equitable distribution for both. These objectives were reaffirmed by the CEO council agreements and detailed processes for how to actualize such distributions that were negotiated and implemented by the CMOs and operational councils, as detailed below.
Principle 2. Disciplined Governance Structures
The HSC operates within a four-tiered governance structure, drawing on decades of formal and informal coordination between organizations. As described above, prior to January 2020, three key forums facilitated information sharing and collaboration among hospitals and the SFDPH: the Hospital Council, comprising CEOs from local hospitals; the local Healthcare Coalition for Disaster Preparedness, comprising emergency preparedness coordinators; and hospital CNO communications. Before 2020, there were few formal gatherings of the chief medical or operational leaders of the local hospitals, and outpatient or ambulatory leaders from affiliated health systems were not regularly involved in disaster preparedness efforts. However, despite being business competitors, health systems leaders demonstrated a willingness to more closely collaborate on pandemic-related issues within this supportive structure. Working norms within the tiered groups were established, emphasizing data-driven decision-making, sharing updates and challenges, identifying opportunities for collaboration, and building trust by dispelling misinformation and rumors. Based on their regular meeting cadence, representatives from each group could report up to their chief executives so that system and city leaders would have up-to-date information on collective efforts. In addition to regular check-ins for each cohort, the HSC members also conducted an after-action review at the end of the federal emergency declaration to capture key learnings and inform future work. Table 1 provides a visual representation of this governance structure.
Table 1.
Tiered Governance Structure of San Francisco Health Systems Collaborative
| Domains | Department of Public Health | Health Care Delivery Systems | Examples |
|---|---|---|---|
| • Leadership • Local Policy |
Director of Health and Health Officer (Director of Population Health) | Hospital Council (CEOs) | • Overall resource commitments and
authority • Memoranda of understanding for operational collaboration • Feedback on local policies |
| • Medical Surge • Hospital Response |
San Francisco Health Network CMO and CNO | CMOs and CNOs | • Proposed surge triggers and
hospital-based operational levers (e.g., clinic or operating room
reductions outside of health orders) • Detailed resource allocation (e.g., remdesivir or nirmatrelvir) |
| • Operations • System Access |
Covid-19 operational leaders (population health, ambulatory care, hospital) | Operational executives (chief operations officers, chief pharmacy executives, ambulatory care leaders) | • Vaccine site operations (hours
staffing, community referrals, vaccine product
distribution) • Testing access expansions • Alternative Care site pathways and operations |
| • Preparedness Planning • Regional Resource Requests |
Public health emergency preparedness and response | Hospital emergency management teams | • Medical surge plan reviews, feedback,
and additional systemwide supports/gap closure • Scarce resource requests to region/mutual aid (vaccine or medication surplus requests, outbreak resource requests) |
This table shows the four primary work groups of the San Francisco Health Systems Collaborative, their domains of responsibility, and examples of the nature of work or decision-making at each level of collaboration. CMO = chief medical officer, CNO = chief nursing officer. Source: The authors
Principle 3. Data Transparency
Early on, the Hospital Council recognized the urgency of the public health threat posed by Covid-19, and its members made a commitment to share hospital bed utilization and surge capacity data with SFDPH to aid in operational planning, including the development of surge plans. Initially, data were shared in biweekly meetings, then daily, by manual hospital polling. Subsequently, the state and local health department implemented formal requirements for all acute care hospitals to share data on general and critical care utilization metrics and, later, on patient- and organizational-level data on vaccinations and testing.16
Similar to other health jurisdictions at national, state, and local levels, the SFDPH relied on epidemiologic disease surveillance and timely data visualization during the Covid-19 pandemic. These efforts aimed to enhance the understanding of disease conditions among public health leaders and the general public, as well as to improve timely decision-making and adjustments.17 The members of the HSC and SFDPH used public dashboards as well as more detailed internal operational analyses and prediction models to monitor impacts of the disease and progress toward shared goals. These goals included preserving hospital capacity, establishing and lifting public health orders, and tracking whether the distribution of vaccinations was as equitable and efficient as planned. HSC member organizations committed to sharing timely organizational data related to Covid-19 operations with SFDPH. Data-sharing procedures adhered to privacy and compliance standards and underwent legal review, sometimes facilitated by state or local health orders. In cases where the data contained sensitive business intelligence (e.g., exact number of staff assigned to a site, percentage of insured patients seen, or exact number of vaccinations administered per organization per site), it was shared with the larger group only in aggregated form (e.g., combined doses administered, population-level vaccination progress by age, race or ethnicity, or zip code).
Principle 4. Operational Collaboration
Building upon the preceding three principles, the final principle focused on fostering operational coordination to achieve the shared population health objectives. Health system leaders collaborated with one another and public health personnel to align their operational plans in a manner that would enhance resource efficiency and equity citywide. By sharing both high-level and detailed operational plans for Covid-19 response, organizations ensured the presence of complementary rather than duplicative services distributed geographically throughout the city, enhancing access for historically underserved communities. Initial operational plans were developed by each organization and subsequently reviewed by SFDPH for both individual and collective impact relative to stated goals (efficiency and equity). Feedback to each organization was provided and operational adjustments negotiated between each individual organization and SFDPH. The level of collaboration fluctuated with the surging and waning demands of the pandemic, both in terms of time intensity and degree of operational coordination — at times requiring daily information sharing or operational coordination and at others weekly or monthly touchpoints to ensure continued program alignment. This collaboration was fundamentally introduced and regularly reinforced through frequent reporting within the tiered governance structures and interpersonal development of work group norms (e.g., agreed-upon communication practices and data review) described above. However, standardization of key features of the interorganizational collaboration was also formally reinforced through strategic use of local health orders as well as monitoring of both collective and individual health system performance related to these orders.
Results
Applications
The HSC members applied the shared principles described above to a number of use cases for a robust operational response. We describe those applications and key features here.
Application 1. Hospital Surge Capacity and Responding to Local and Regional Needs
Starting in January 2020, San Francisco hospitals began reviewing and updating their acute care surge plans in response to the evolving Covid-19 crisis. By March 2020, CMOs and CNOs aligned surge plans to enhance overall city capacity. Hospitals established standardized surge indicators and triggers that specified the countermeasures to be implemented at different levels of patient volume (e.g., opening surge units and reducing or pausing outpatient procedures). Additionally, hospital leaders identified and designated a dedicated Covid-19 surge unit at one of the facilities that could be opened swiftly for patient transfers.18 Local academic partners at University of California Berkeley and San Francisco developed prediction models for hospital bed utilization in different disease dynamics, against which these surge plans could be tested and then tracked during surges.17 As has been reported elsewhere, these prediction models helped to inform public health policy and decision-making following the initial swift and decisive regional shelter-in-place orders that helped to maintain hospital inpatient capacity.15,17
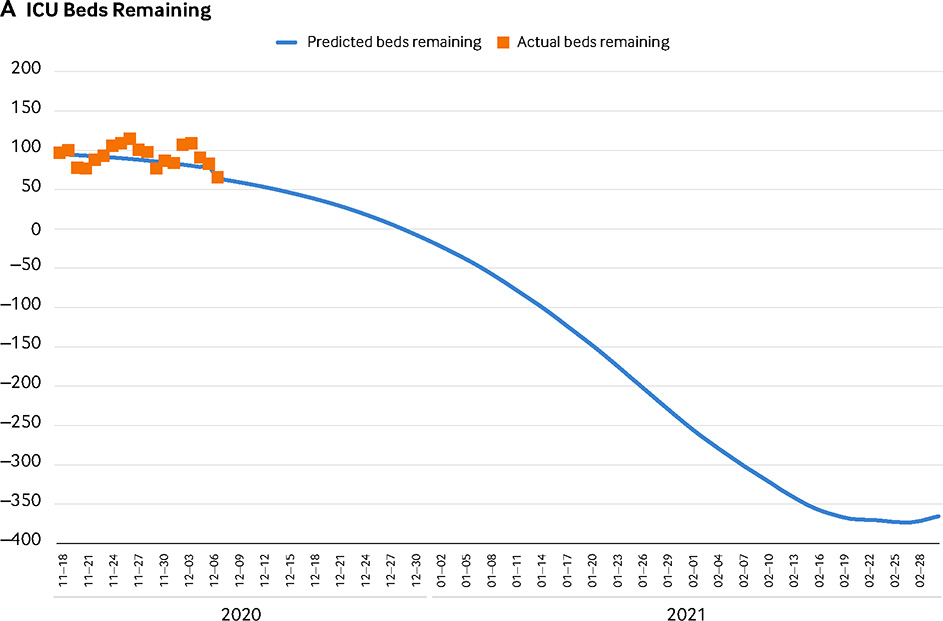
Disease dynamics — including community-level Covid-19 positivity rates and rate of new hospital admissions as well as remaining acute care bed capacity — influenced the timing of both health order implementation or cessation (e.g., for modified shelter-in-place and elective surgery restrictions). Additionally, hospitals relied on established and updated predetermined thresholds of remaining bed capacity to trigger modification of internal hospital policies or smoothing of elective procedures. The CMO and CNO groups were responsible for negotiating the updated thresholds together and with the health department and aligning and adhering to these surge plans. Examples of hospital surge capacity tracking for both ICU beds (Figure 1, Part A) and acute care beds (Figure 1, Part B), with the potential impact of elective procedure cancellations and delays, are provided.
FIGURE 1. ICU and Acute Care Bed Capacity Tracking: Projected Surge Model Versus Daily Actuals.
(A) This graph shows an example of ICU bed capacity and compares the projected surge model with the daily actual remaining capacity. The blue line indicates the predicted remaining ICU beds in San Francisco based on the median projection of Covid-19–positive cases that will need ICU-level hospitalization for data inputs as of December 10, 2020. The orange squares indicate the actual values mapped against that projection. This graph shows that on December 30, 2020, we anticipated running out of ICU beds, and if conditions remained unchanged, we would have run out of all additional surge beds opened up to accommodate the surge on February 8, 2021. (B) This graph shows an example of acute care bed capacity, comparing the projected surge model with the daily actual remaining capacity. The blue line indicates the predicted remaining non-ICU or acute care beds in San Francisco based on the median projection of Covid-19–positive cases that would need acute care–level hospitalization for data inputs as of December 10, 2020. The orange squares indicate the actual values mapped against that projection. This graph shows that on January 9, 2021, we anticipated running out of acute care beds. If nonemergency or prescheduled procedures were cancelled, the estimated date of running out of beds would be extended to January 15, 2021. If conditions remained unchanged, we would run out of all additional beds opened up to accommodate the surge on January 29, 2021, and we would anticipate a deficit of 60 surge acute care beds on February 20, 2021.
Source: The authors
NEJM Catalyst (catalyst.nejm.org) © Massachusetts Medical Society
Hospital surge plan alignment was applied to support response operations for several local and regional surges. Similar to other regions, the initial surge of patients with Covid-19 in San Francisco in April 2020 disproportionately affected lower-income communities and communities of color. A testing study conducted in the Mission neighborhood, where a majority of residents identify as Latino/a/x and household occupancy is higher than in other neighborhoods, revealed a test positivity rate 20 times higher than the citywide average.19 This disparity was reflected in the early Covid-19 hospitalization data, with Zuckerberg San Francisco General Hospital (ZSFG), the SFDPH-operated safety-net hospital located in the same neighborhood where the study was conducted, managing a high proportion of patients with Covid-19 in the first wave of the pandemic.
However, by leveraging citywide data, hospital CMOs and CNOs were able to facilitate transfers between facilities if census levels approached capacity. Because of the relatively low incidence of Covid-19 disease in San Francisco during surges compared with other metropolitan areas (for example, Covid-19 case incidence in San Francisco in December 2020 was approximately 18 new cases per week per 100,000 people compared with 44 new cases per week per 100,000 in the United States),20 interfacility transfers only had to be initiated a few times, with fewer than five patients identified for transfer per any given surge period; all patients meeting transfer criteria consented to transfer following standard procedures. Insurance status was not identified as a barrier to transfer. A concurrent city program used daily census data to direct ambulance patients with respiratory syndromes to hospitals with the highest remaining inpatient capacity.21 The planning for this physician-directed ambulance-management pilot program had begun prior to the Covid-19 pandemic to address issues relating to rising ambulance patient offload delays but was adapted at the start of the pandemic to incorporate hospital Covid-19 census data into hospital destination decisions.
Additionally, during the first several months of the pandemic, in response to hospital needs to free up lower-acuity admission space, the emergency medical services system created a transport hub to facilitate patient discharges to isolation and quarantine hotels that had been established by the city for monitoring lower-acuity patients with Covid-19 without the ability to isolate or those with high-risk medical conditions who were experiencing homelessness. These public health interventions helped to maintain hospital capacity in San Francisco during early Covid-19 surges.22 Finally, daily sharing of census data through the state-mandated process meant that San Francisco hospital systems were able to support surge response for regional outbreaks across California, including those affecting a local federal prison and a distant, low-resource county.23,24
Application 2. Scarce Resource Allocation, Medical Countermeasures, Therapeutics, and Vaccinations
Throughout the pandemic, the entities within the HSC had multiple opportunities to collaborate on the distribution of medical countermeasures, ranging from intravenous and oral therapeutics to mass-vaccination campaigns. Early in 2020, the CMO council of the HSC had established shared best practices for the allocation of scarce resources, following national and state guidelines for critical resource usage during times of contingency and crisis care.25–27 Within a few months, the HSC member organizations had the opportunity to apply these locally agreed-upon guidelines to practice for specific operational efforts.
The first opportunity for distributing Covid-19 therapeutics arose in May 2020 following the Emergency Use Authorization of remdesivir for the treatment of hospitalized or high-risk individuals. However, due to surges in other parts of the country, allocations to San Francisco were significantly limited.28 To ensure equitable and efficient distribution based on local disease dynamics, the HSC CMO council participated in weekly polling, applying their aligned scarce resource plans to request doses proportional to their most critically ill patients. Next, in December 2021 and January 2022, during the surge of the Omicron variant of SARS-CoV-2, a limited supply of antivirals became available for outpatient management. Once again, SFDPH relied on the HSC to facilitate the rapid distribution of a significant portion of the initial doses of ritonavir-boosted nirmatrelvir (Paxlovid) and molnupiravir to high-risk individuals presenting in ambulatory, ED, or inpatient settings within these health systems. Simultaneously, efforts were made to ensure that doses were accessible to community clinics. In addition to aligning prescribing practices, several organizations ensured open-access appointments for all San Franciscans, regardless of their primary health care affiliation or insurance, preserving capacity at sites dedicated to the underinsured and uninsured.
Application 3. Mass-Vaccination Campaign
The HSC and SFDPH engaged in extensive coordination efforts for the Covid-19 vaccination campaign, covering both the initial and subsequent booster campaigns. HSC and SFDPH leaders established core principles of efficiency and equity, with a goal of achieving a throughput capacity of at least 10,000 vaccines per day collectively and administering 900,000 vaccinations by April 30, 2021. Regular coordination meetings were held between HSC and SFDPH operational leaders, with a frequency of up to three times per week during peak times, to align strategies and resources needed for implementation of low-barrier access protocols.
“The chief medical officer and chief nursing officer groups were responsible for negotiating the updated thresholds together and with the health department and aligning and adhering to these surge plans.”
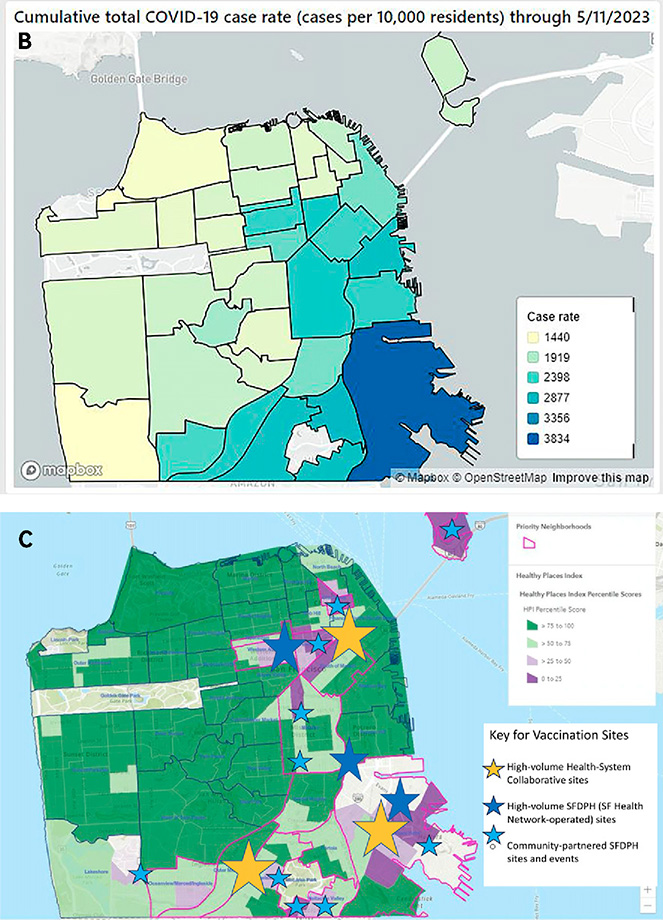
To ensure efficiency and speed, three high-volume mass-vaccination sites were designed and opened in January and February 2021.29 Each site was operated through collaboration of one of three regional health systems (Kaiser Permanente, Sutter Health, and UCSF Health) with the City and County of San Francisco (CCSF). The health care systems provided vaccine allocations, staffing, documentation, and medical equipment, whereas CCSF took care of site selection, maintenance, and logistic needs. Other HSC members, such as Dignity Health (Common Spirit) and Chinese Hospital, also participated in the mass-vaccination campaign by contributing staff to these sites and through on-campus vaccination clinics. Each of the high-volume sites aimed to maintain a capacity of more than 1,000 vaccines per day per site, some with individual capacity of up to 8,000 per day. Site locations were strategically chosen based on high Covid-19 case rates, historical health disparities, and barriers to health care access as indicated by the Healthy Places Index (HPI) model used by the California Department of Health.10 Additionally, the SFHN, the health care delivery arm of SFDPH, opened two mass-vaccination sites on the campuses of their hospital (ZSFG) and a primary care clinic (Southeast Family Health Center). Collectively, these five high-volume sites could administer more than 15,000 doses per day, occasionally facilitating reallocations to prevent dosage gaps during times of scarcity.
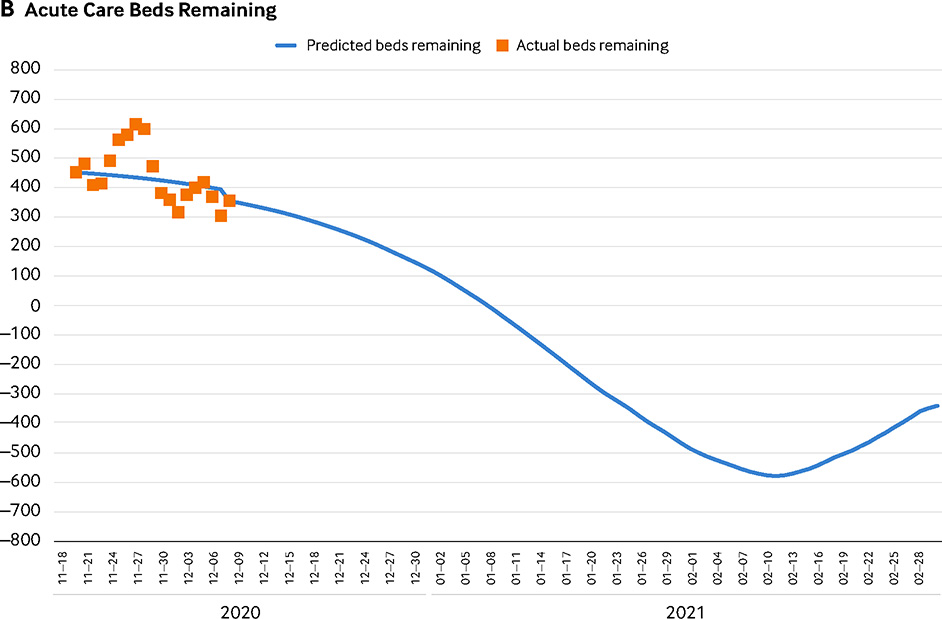
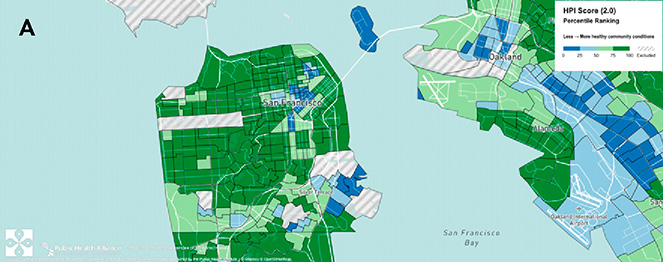
To further address the objective of equitable access, the HSC implemented strategies to provide low-barrier access to vaccines for underserved communities. These strategies included prioritized appointments and pop-up vaccination events for those with limited access to online scheduling or traditional sites. Events included locations such as community fairs, churches, senior affordable housing developments, and behavioral health day programs. Some organizations established ongoing partnerships within historically underserved communities.30–33 Additionally, the larger health care systems’ focus on administering high-volume sites allowed SFDPH to concentrate its operations on communities with the greatest barriers to access. This involved establishing a system of semipermanent neighborhood-based vaccination sites, hosting more than 200 smaller-volume pop-up community events, and deploying mobile teams to reach long-term care facilities, people experiencing homelessness, and homebound individuals.34,35 Figure 2, Part A and Figure 2, Part B illustrate the geographic distribution of the high-volume mass-vaccination sites and SFDPH neighborhood-based sites across the city compared with the HPI score. Figure 2, Part C depicts a geographic representation of the CCSF, with overlays of both social vulnerability factors and the operational response to ensure equitable access to vaccinations.
FIGURE 2. San Francisco County Healthy Places Index by Census Tract, Cumulative Covid-19 Case Rate by Neighborhood, and Vaccination Efforts Focused on the Most Heavily Impacted Communities.
(A) The Healthy Places Index (HPI) is a composite score of 25 community characteristics that affect health (such as housing, income, pollution, etc.). With a range of 0–100, a higher score indicates more healthy community conditions. This figure shows that although most of the communities are dark green, putting them in the top 75th percentile nationally, several communities fall below the 50th and 25th percentiles. The data supporting this figure are from 2020 through April 2022. (B) This map shows the cumulative total Covid-19 case rate (cases per 10,000 residents) through May 11, 2023. The highest rates are nearly three times greater than the lowest rates. Note that when comparing these rates with the Healthy Places Index scores, it is evident that areas with greater healthy community conditions had lower Covid-19 infection rates. (C) This geographic representation of the City and County of San Francisco, with overlays of both social vulnerability factors and the operational response of activity from January 2021 through May 2023, shows the distribution of vaccination sites of varying volume capacities and operated by different entities including members of the San Francisco Health Systems Collaborative as well as by the San Francisco Department of Public Health (SFDPH). The balance of large-volume mass-vaccination sites mostly operated by health systems allowed SFDPH to focus resources on highly impacted communities, including several large- and moderate-volume vaccination sites in partnership with community organizations.
Source: The authors, with information and permission from Public Health Alliance of Southern California and using Mapbox OpenStreetMap services
NEJM Catalyst (catalyst.nejm.org) © Massachusetts Medical Society
As the vaccination campaign progressed beyond the initial phase, the HSC operations cohort shifted its focus to sustainable models of population-based outreach and vaccination. High-volume vaccination sites were closed by July 2021, and health care systems collaborated with the SFDPH by sharing their plans for ensuring ongoing access to Covid-19 services and meeting anticipated surges in demand for testing and vaccines. Health care systems incorporated vaccinations into primary care and specialty care settings, and some established campus-based mass-vaccination sites capable of administering more than 500 vaccines per day. This planning and infrastructure enabled the HSC and SFDPH to rapidly expand operations in response to the arrival of the Omicron surge in late 2021 and for subsequent booster campaigns, as emerging evidence highlighted the importance of additional vaccine doses to mitigate the impact of the disease.36,37
Outcomes
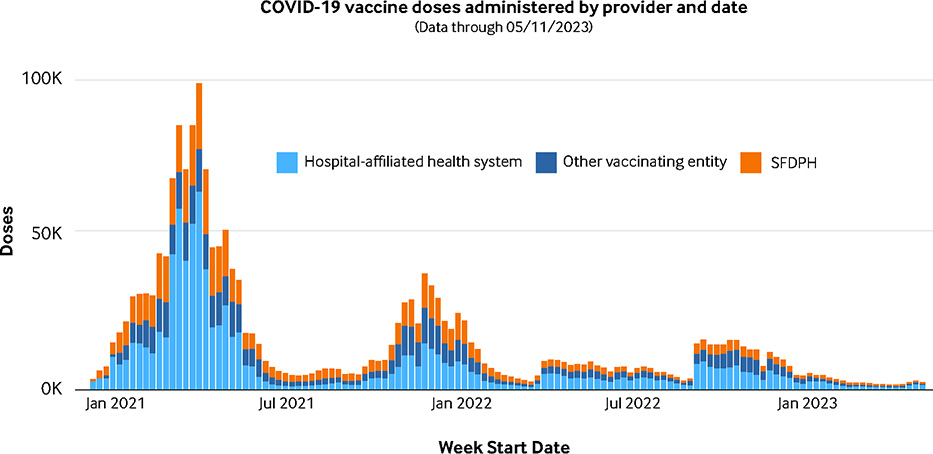
Over the first 3years of the Covid-19 pandemic (through December 31, 2022) San Francisco experienced a death rate from Covid-19 of approximately 14 per 100,000, compared with the California statewide death rate of approximately 30 per 100,000 and the United States rate of 70 per 100,000 for the same time period.38,39 Throughout the response, San Francisco maintained greater than 10% hospital bed capacity across the city (Figure 1, Part A and Figure 1, Part B) and, as described above, this capacity allowed for assisting with other regional hospital surges. Through May 11, 2023, the end of the Public Health Emergency Declaration in the United States, San Francisco had administered more than 1.9 million doses of Covid-19 vaccines, of which SFDPH has administered 28%, and other large health systems had administered 48% (Figure 3).
FIGURE 3. San Francisco County Covid-19 Vaccine Administration by Vaccinating Entities over Time.
Administration of Covid-19 vaccinations was shared among San Francisco Health Systems Collaborative participants, as shown in this graph of weekly doses by date and provider type. The bulk of doses (48%) was provided by hospitals and health systems, followed by the San Francisco Department of Public Health (SFDPH; 28%), and other entities (24%), which includes organizations such as Chinese Hospital, a Veterans Administration Health Care System, and Federally Qualified Health Centers.
Source: The authors
NEJM Catalyst (catalyst.nejm.org) © Massachusetts Medical Society
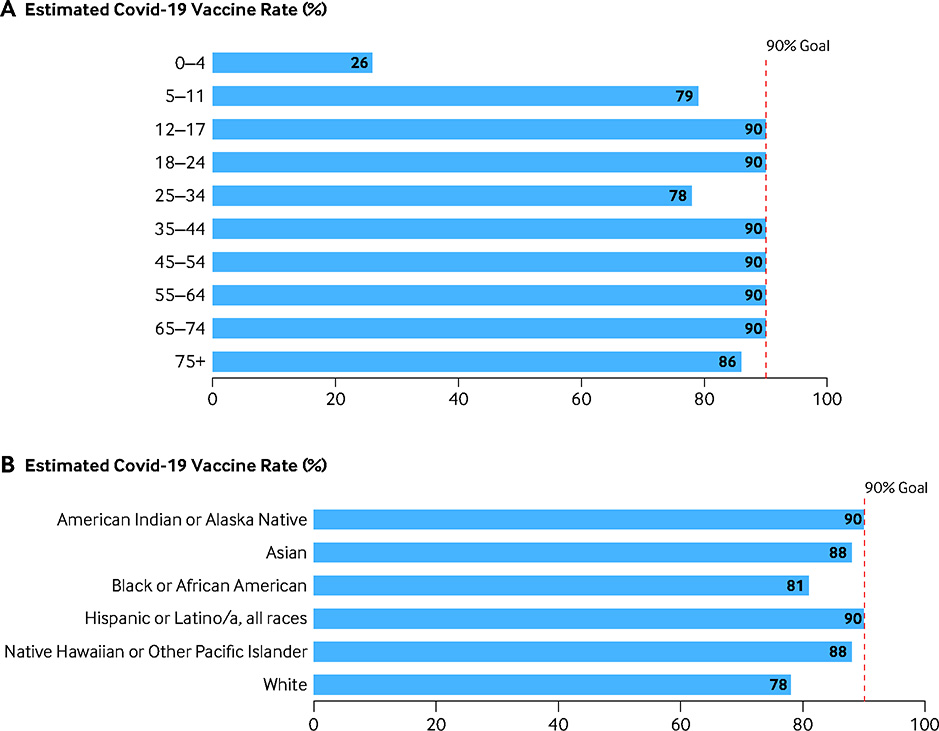
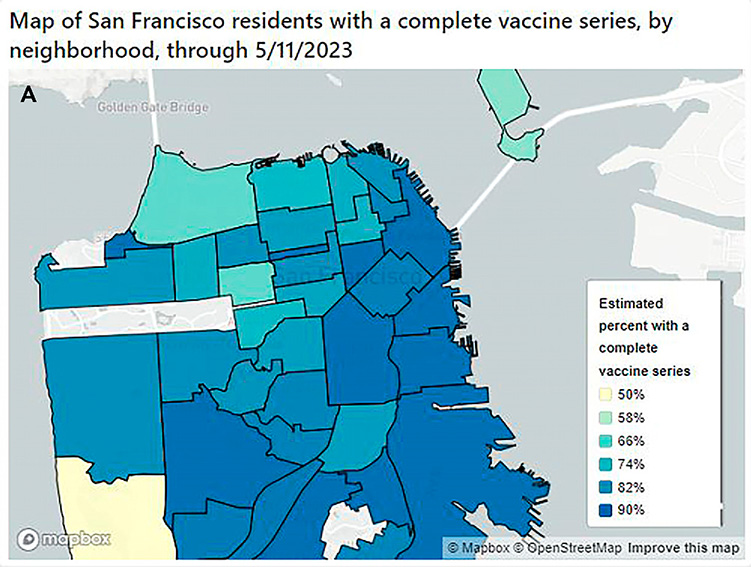
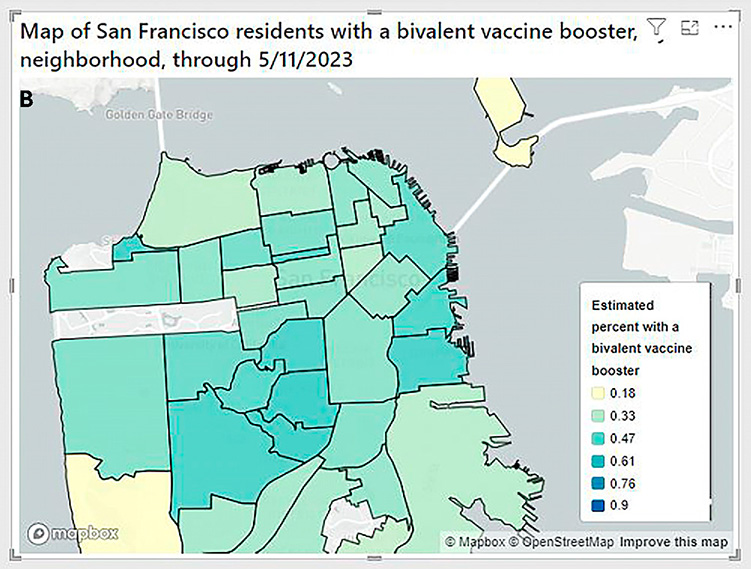
These vaccination rates represent more than 90% of the total population receiving the primary Covid-19 vaccination series and 40% bivalent booster dose, compared with U.S. rates of 81% and 17%, respectively. For the primary vaccination campaign, San Francisco was one of the first cities in the United States to reach the milestone of 90% in June 2022. Additionally, San Francisco’s vaccination campaign is notable for one of the lowest rates of disparities by age, race, ethnicity, and neighborhood. For example, San Francisco’s vaccination rates among people who identify as Black or those who identify as Hispanic across all age groups routinely exceeded state and national averages by 10 to 20 percentage points in both the primary series and booster campaigns.40–42 Vaccination rates by subgroups and geography are shown in Figure 4, Part A, Figure 4, Part B, Figure 5, Part A, and Figure 5, Part B.
FIGURE 4. Estimated Percentage of Residents with a Complete Covid-19 Vaccine Series, by Age and Race or Ethnicity, Through May 11, 2023.
(A) The efforts of the San Francisco Health Systems Collaborative contributed to high Covid-19 vaccination rates across most age groups, with 6 of 10 segments achieving the Collaborative’s target of 90%. Completion of the vaccine series is defined as completion of the first dose. Follow-up booster vaccination is not included. (B) The efforts of the San Francisco Health Systems Collaborative contributed to high Covid-19 vaccination rates across all age groups, ranging from 78% to 90%. Completion of the vaccine series is defined as completion of the first dose. Follow-up booster vaccination is not included.
Note: The red dotted line represents the goal of achieving a 90% complete Covid-19 vaccination rate.
Disclaimer: Population information is from the 2020 American Community Survey (ACS) 5-year estimates. The U.S. Census Bureau provides these data. We use these data to estimate the percent of each SF group that is up to date on their Covid-19 vaccinations. The ACS estimates the number of residents in each age group based on a survey of residents. Estimates may not be precise, especially for groups with smaller populations. If the true population is larger than the estimate we use, then the true vaccination rate will be lower than what we report here. This is likely true for groups that show a larger number of vaccine recipients than estimated residents. As a result, the percent of residents who are up to date is only an estimate and percentages will not be reported above 90%. </p/>Source: The authors, with data from: DataSF. SFDPH Reporting - Demographics Population Estimates. Updated June 12, 2024. Accessed June 26, 2024. https://data.sfgov.org/Economy-and-Community/SFDPH-reporting-demographics-population-estimates/cedd-86uf/about_data.
NEJM Catalyst (catalyst.nejm.org) © Massachusetts Medical Society
FIGURE 5. Estimated Percentage of San Francisco Residents with a Complete Covid-19 Series and with a Covid-19 Booster, by Neighborhood, Through May 11, 2023.
(A) This map shows the estimated percentage of San Francisco residents with a complete Covid-19 series, by neighborhood. Throughout the 41 neighborhoods within San Francisco, completion of the Covid-19 vaccination series varied from approximately 50% up to 90%. Factors that may influence the rate are those associated with the Healthy Places Index (Figure 3). Completion of the vaccine series is defined as completion of the first dose. Follow-up booster vaccination is not included. (B) This map shows the estimated percentage of San Francisco residents with a bivalent Covid-19 booster, by neighborhood. Throughout the 41 neighborhoods within San Francisco, completion of the Covid-19 bivalent booster varied from approximately 18% up to 90%. Factors that may influence the rate are those associated with the Healthy Places Index (Figure 3). Completion of the bivalent booster is defined as completion of one or more of the booster options after the initial complete Covid-19 vaccine series.
Disclaimer: Population information is from the 2020 American Community Survey (ACS) 5-year estimates. The U.S. Census Bureau provides these data. We use these data to estimate the percent of each SF group that is up to date on their COVID-19 vaccinations. The ACS estimates the number of residents in each age group based on a survey of residents. Estimates may not be precise, especially for groups with smaller populations. If the true population is larger than the estimate we use, then the true vaccination rate will be lower than what we report here. This is likely true for groups that show a larger number of vaccine recipients than estimated residents. As a result, the percent of residents who are up to date is only an estimate and percentages will not be reported above 90%.
Source: The authors, using Mapbox OpenStreetMap services, with data from: DataSF. SFDPH Reporting - Demographics Population Estimates. Updated June 12, 2024. Accessed June 26, 2024. https://data.sfgov.org/Economy-and-Community/SFDPH-reporting-demographics-population-estimates/cedd-86uf/about_data
NEJM Catalyst (catalyst.nejm.org) © Massachusetts Medical Society
In addition to quantitative outcome data regarding San Francisco’s Covid-19 performance metrics, quantitative and qualitative data were reviewed through the after-action survey process regarding HSC membership feedback on overall structure, process, and lessons learned. An anonymous survey (see Appendix) was distributed to all members of the HSC group (executive leaders, operations leaders, clinical leaders, emergency preparedness leaders, etc.). Additionally, facilitated after-action discussions were conducted by each cohort to provide feedback to SFDPH on future preparedness directions. Of the anonymous survey participation, 11 participants, who reported representing four of the HSC organizations, participated in the 12-question survey, with varying degrees of individual question response because all were optional.
However, survey responses were shared in the group discussions to prompt conversation and additional qualitative feedback during review sessions. Survey data assessed HSC’s adherence to the four principles of collaboration outlined and reinforced through the work group structures. Overall, the majority of HSC work group participants who responded to the survey question, six of seven (86%), reported that the group was effective or very effective in defining its vision and objectives. Additionally, six of six (100%) respondents reported that the group used data effectively or very effectively to inform decisions. These findings were reinforced in the group discussions. One area of constructive feedback noted in the survey and in group discussions was that the group should have more intentionally oriented new members to the overall mission and objectives of the group following leadership transitions. Additionally, many members noted the preference for more emphasis on areas of consensus to the response approach rather than health orders (e.g., legal requirements to participate or to share data).
Discussion
Health care delivery systems play a critical role in responding to and managing pandemics and public health emergencies. In this study, we examined the functional norms and impacts of a proactive collaboration model between private health care delivery systems and a local government’s department of public health during a public health emergency. This governance structure and clinical operational partnership effectively ensured desirable population-level health outcomes for access to care, infection rate, immunization, and mortality across a diverse metropolitan community. However, there is a paucity of data or reporting on interorganizational collaborations between hospitals or health care systems enacting collective responses to Covid-19. In fact, previous reports from the first wave of Covid-19 in New York City highlighted significant disparities in hospitalizations and death rates among different socioeconomic and racial or ethnic groups due to the siloed nature of health care delivery and inequitable access to care based on income and insurance.43,44
Similarly, in multiple Covid-19 waves across the United States, different hospitals reported varying degrees of crowding or operational impacts based on payer mix.45–48 In contrast, during Arizona’s first wave of Covid-19, a collaborative public–private response demonstrated that regional and local coordination and state policies and programs could facilitate resource sharing among health systems to help mitigate potential bed shortages.49 Similarly, the San Francisco HSC found that collective action on the organizational level appeared to be associated with reduced inequities of strain among individual hospitals. Additionally, the HSC’s experience underscored the finding that visibility into citywide and regional hospitalization trends could help support timely preparations for and mitigation of institutional impacts of Covid-19.
San Francisco’s collaborative response was facilitated by public health policies and practices. However, health orders alone do not explain the degree of sustained alignment of both mission and operations across health care delivery systems. We have posited that four core principles that defined purpose, governance, data accessibility, and working norms helped to drive success in terms of measurable Covid-19 outcomes. Based on the current paucity of literature examining the intersection of health orders with organizational principles such as collaboration, it is difficult to differentiate which portion of San Francisco’s success was attributable to the mandatory versus voluntary aspects of collaboration, including the governance, relational, and operational norms established and periodically reaffirmed by the tiered work groups. However, without informational and operational alignment reinforced by the four principles we describe here, we hypothesize that health orders alone — without active coordination of response — would have led to less-efficient deployment of resources and likely magnification of health disparities in access to Covid-19 resources. Given the voluntary aspects of a large portion of each organization’s participation in the collaborative (relative to the health orders that supported specific data transparency), there was no comprehensive way to determine the degree to which each organization adhered to the four principles at all points in time. However, the qualitative assessments provided by the after-action process provided some measure of shared validation of the model for collaboration.
Although literature on health care delivery and public health systems during the Covid-19 pandemic is still emerging, some reports do document strategies employed by health systems to address fluctuating clinical operational needs. The Incident Command System and Hospital Incident Command System (HICS) were used by various health systems to organize and track operational objectives, facilitating rapid communication, operational alignment, and resource allocation.50–53 The HSC member organizations reported similar efficiencies in using HICS. Additionally, several health care delivery systems reported on use of the Lean management system (Lean) at varied phases of pandemic response: from creating and operating a field hospital for surge, to managing the supply chain, to ensuring operational area alignment.54–56 Because Lean is commonly used across many hospital and health care delivery systems, personnel familiar with its principles could easily apply Lean tools to pandemic-related initiatives. The San Francisco HSC and SFDPH incorporated Lean principles into coordination and alignment efforts, such as patient level-loading and scaling vaccination pods. As highlighted in existing literature describing applications of Lean management in health care, the HSC member organizations both individually and as a collective benefited from aligning to core principles, regular data review to inform decision-making, and incorporating feedback from the front line and patients into solution design.
Looking Ahead
As discussed above, the HSC identified opportunities to codify best practices for collaboration to address health emergencies facing the broader population, even if they do not rise to the level of a global pandemic with a novel virus. The chance to test both the operational systems of collaboration and the benefits of tiered governance and data-informed strategies came sooner than anticipated in the setting of the mpox outbreak. During this response, many health systems expanded on existing community-facing Covid-19 response infrastructure to offer low-barrier and open access to mpox vaccines on their campuses, at community events, and in mobile clinics.57,58 Currently, the HSC and SFDPH are evaluating mechanisms to maintain and strengthen both situational awareness and ongoing collaborative efforts to address population health disparities in nonemergency times. For example, HSC operational leaders provided assistance through their patient care and population health leads to address the general pediatric vaccination gap that was exacerbated by the Covid-19 pandemic; also, additional informational and operational best practices are underway for innovations in prevention and treatment of sexually transmitted infections, including HIV. Although there is little literature to suggest lasting strategies for ongoing alignment between public health and health care delivery entities, the experiences and lessons learned in the San Francisco model described here may provide a framework for other local health jurisdictions and health care systems to use in disaster preparedness and response, as well as other population health initiatives. The extent of this future alignment and coordination locally will, in part, depend on variation and urgency of future public health threats. However, the existing work group structures and relationships, including periodic meetings of most cohorts, provide a foundation for the design and operationalization of future coordinated response efforts.
Limitations
There are several limitations to generalizability of the principles and findings described here. This is a report describing the processes adopted by stakeholders operating within one local health jurisdiction. Because this was a descriptive account conducted retrospectively, it cannot account for the impacts of other environmental confounders, including local public health or governmental policy (e.g., timing of shelter-in-place orders, community attitudes toward public health measures, etc.). Additionally, we could not fully quantify the degree of resource investment of individual organizations (relative to available assets) to collaborative efforts. Moreover, organizations may have at times reduced resource commitments based on internal factors. Additionally, SFDPH is unusual for a public health department in that it has both health care delivery and traditional public health functions. Furthermore, San Francisco as a community experienced both strong public and political support for pandemic response efforts. Despite its relatively small geographic size (just about 47 square miles), San Francisco has a number of private health systems operating with robust infrastructures within the city. Although this is not unique for a metropolitan center, the degree to which traditional competitors collaborated may not be easily replicated in another market. The near-universal health insurance coverage of San Francisco’s population (about 97%) removed a potentially significant barrier to collaboration, including for patient transfers. Finally, San Francisco’s long history of robust public health response to HIV and public–private–community partnerships in those efforts may have also facilitated the degree of interorganizational collaboration observed.
The Covid-19 experience shows us that health care delivery systems and public health collaborations can be effective in achieving population health outcomes during an emergency and may provide a framework for ongoing preparedness and response for future time-limited events and longer-term public health campaigns. A governance structure that is supported by principles of shared objectives, clear governance and accountability, data transparency, and commitment of operational expertise can help to enhance equitable and efficient population health initiatives.
“The Health Systems Collaborative identified opportunities to codify best practices for collaboration to address health emergencies facing the broader population, even if they do not rise to the level of a global pandemic with a novel virus.”
Supplementary Material
Where to Start.
For a public health system or group of health care delivery organizations interested in building such a collaborative, our experience indicates that there are several factors that can help to facilitate success:
Building and/or strengthening collaborative relationships:
Relying on preexisting organizational relationships is helpful, but it is not essential to initiating a coalition. Although the participants of the San Francisco HSC had enjoyed several decades of loose collaboration — through emergency preparedness efforts, as well as quarterly, industry-level touchpoints of chief executives — commitment to more in-depth collaboration deepened in the setting of a complex, real-world problem. Furthermore, once the problem is identified, reflection on and outlining the organizing principles for collaboration and supporting with governance and operating structures to reinforce those principles can, in itself, strengthen collaboration and foster closer working relationships among peers.
Flexible but reinforcing governance structures:
Recognize that a different type of governance and authority may be needed for response to any particular problem at hand. A flexible governance structure that maintains some connections and touchpoints between peers during times of routine challenge and complexity could be intensified during issues of higher volatility, complexity, and uncertainty. Additionally, some organizational members may be more (or less) participatory than others based on their available resources or organizational culture. Therefore, a tiered governance structure with both vertical and horizontal lines of communication between coordinating entities can help ensure feasible and continued engagement at the levels needed for the particular problem at hand, given the resources available.
Clear principles of engagement:
As we shared in this article, establishing up-front (or as early as possible) the guiding principles of engagement can help to inspire and maintain ongoing collaboration. Four specific principles were essential to our collaborative and would likely benefit other such responses: shared priorities and objectives; clear and disciplined governance and communication; a commitment to data transparency for information relevant to the problem at hand; and operational and resource coordination and alignment, denoting a commitment to share more than data or high-level concerns but to ensure sweat equity among organizations invested in collective action.
Acknowledgments
We acknowledge additional past and present members of the San Francisco Health Systems Collaborative as well as other partners in this work, including but not limited to the following individuals and organizations: The Hospital Council of Northern and Central California, San Francisco Department of Emergency Management, DataSF, SFDPH IT, San Francisco Controller’s Office, The San Francisco Human Services Agency, Michon Coleman, Tomas Arag on, Andrew Holcolmb, Joanna Omi, Craig Vercruysse, Lisa Winston, Gabe Ortiz, Eric Raffin, Jeff Scarafia, Neda Ratanawongsa, Laura Krehbiel, Colten Strickland, Seth Pardo, Jonathan Fuchs, Isela Ford, Aaron Yen, Oscar Macias, Katy Tang, Blake Gregory, Rachel Stern, Darpun Sachdev, Lisa Golden, Vincent Fuqua, Jackie McCright, Andrew Felix, Alice Kassinger, Emily Vontsolos, Reyna McKinnon, Michelle Littlefield, Helen McLendon, Nancy Milholland, Jason Lally, Blake Valenta, Tania Jogesh, Monica Kendrick, Dionne Miller, Jamie Rant, Anastasiya Nazarova, Daniel Woody, Zina Kay-Moore, Katie Taquino, Yvan Vizcardo, Allen Sia, Jonathan Volk, Brad Hare, Thea Thompson, Susan Smith, Gina Intinarelli, Sarah Doernberg, Kim Rhoads, Diane Havlir, Carina Marquez, Margot Kushel, Malcolm John, Maya Petersen, Joshua Schwab, Kristen Bibbins-Domingo, Arthur Reingold, Eric Goosby, George Rutherford. The San Francisco Community Clinic Consortium, and many other clinical and operational leaders and team members at the San Francisco Department of Public Health, the City and County of San Francisco, Chinese Hospital of San Francisco, Common Spirit/Dignity Health, Sutter Health and California Pacific Medical, Kaiser Permanente, University of California San Francisco (UCSF) Health, the Veterans Administration Medical Center of San Francisco, Laguna Honda Hospital, the San Francisco Campus for Jewish Living, and Kentfield Hospital.
*. San Francisco Health Systems Collaborative Additional Members:
Roland Pickens, Terry Dentoni, Gillian Otway, Andrea Turner, Lann Wilder, Charles Fann, Jenna Bilinski, Tosan Boyo, Anna Robert, Carol Taniguchi, Jeff Schmidt, Merjo Roca, Hali Hammer, Ellen Chen, Blake Gregory, Hallie Randel-Schreiber, David Stier, George Han, Mariecar Dela Cruz, Gino Cifolelli, Amy Ovadia, Radha Rai, Michael Phillips, Troy Williams, Albert Yu, Ayanna Bennett, Jeff Critchfield, Mary Ellen Carroll, Adrienne Bechelli, Linda Yeung, Ronald Groepper, Tarek A. Salaway, Guy Chicoine, Peggy Sugar, Scott Keech, Natalie Roesler, Sunitha Dharman, Michael Machado-Morrow, Ian McLachlan, Theophilus Little, Bridget Williams, Abhishek Dosi, Hamila Kownacki, Warren Browner, James Benney, Jennifer Ma, Katherine Weiland, Kiren Rizvi Jafry, Kate Baust, Robert Nordgren, Kathy Sforzo, Jian Zhang, Antonia Lendaris, Gina Yam, Daryn Kumar, David Klein, Kecia Kelly, Ruth Perry, Charlene Battaglia, Kim Brown Smith, Brandie Kolta, Suresh Gunasekaran, Mark Laret, Sheila Antrum, Shelby Decosta, Joshua Adler, Erin Carrera, Kim Murphy, Art Dominguez, Judie Boehmer, Jonathan Hutchinson, Katherine Yang, Wayne Little, Stephanie Kang, Jeanette Cavano, Kelsey Waier, Kevin Dugan, Francine Sneddon, Jia F. Li, Elfega Nunez, Robert Walters, and Mary Connick.
Note: Publication here represents the first official public use of the name San Francisco Health Systems Collaborative, which had served as the term used internally to refer to the group.
Footnotes
Disclosures: Mary P. Mercer, Lukejohn Day, Maria Ansari, Elizabeth Kwan, Desi Kotis, Valerie Caplan, Trang Quyen Nguyen, Christopher Lee, Matthew Smith, Andrea G. Tenner, Baljeet Sangha, Tiffany Rivera, Kenpou Saelee, Claire Horton, Adrienne Green, Vernon Giang, Bruce Ovbiagele, Justin Quock, Todd LeVine, Jonathan Sears, Amabel Chow, Ellie Schafer, Eleanor Morse, John Brown, Elizabeth Connelly, Jim Marks, Wayne Enanoria, Susan Ehrlich, Susan Philip, Naveena Bobba, and Grant Colfax have nothing to disclose.
Contributor Information
Mary P. Mercer, Chief of Medical Staff, Zuckerberg San Francisco General Hospital, San Francisco, California, USA; Former Covid-19 Vaccine Section Chief and Covid-19 Health Systems Deputy Director, San Francisco Department of Public Health, San Francisco, California, USA; Director, Emergency Medical Services and Disaster Medicine Section, University of California San Francisco Department of Emergency Medicine, San Francisco, California, USA; Professor of Emergency Medicine, University of California San Francisco School of Medicine, San Francisco, California, USA.
Lukejohn Day, Chief Medical Officer, University of California San Francisco Health System, San Francisco, California, USA; Former Chief Medical Officer, Zuckerberg San Francisco General Hospital, San Francisco Department of Public Health, San Francisco, California, USA; Professor of Medicine, University of California San Francisco School of Medicine, San Francisco, California, USA.
Maria Ansari, Chief Executive Officer and Executive Director, The Permanente Medical Group Inc., Oakland, California, USA; President and Chief Executive Officer, Mid-Atlantic Permanente Medical Group, Rockland, Maryland, USA; Co-Chief Executive Officer, The Permanente Federation, Oakland, California, USA; Former Physician in Chief, Kaiser Permanente Medical Group, San Francisco, California, USA.
Elizabeth Kwan, Former Covid-19 Vaccine Logistics Branch Director, San Francisco Department of Public Health, San Francisco, California, USA; Associate Professor of Emergency Medicine, University of California San Francisco School of Medicine, San Francisco, California, USA.
Desi Kotis, Chief Pharmacy Executive, UCSF Health, San Francisco, California, USA; Associate Dean and Faculty Member, UCSF School of Pharmacy, San Francisco, California, USA.
Valerie Caplan, Data Visualization & Reporting Team Manager, Center for Data Science, San Francisco Department of Public Health, San Francisco, California, USA.
Trang Quyen Nguyen, Epidemiologist, Applied Research, Community Health Epidemiology, and Surveillance Branch Population, Health Division, San Francisco Department of Public Health, San Francisco, California, USA.
Christopher Lee, Epidemiologist, San Francisco Department of Public Health, San Francisco, California, USA.
Matthew Smith, Analytics Engineer, DataSF, Office of the City Administrator, San Francisco, California, USA; Former Principal Analyst, San Francisco Department of Public Health, San Francisco, California, USA.
Andrea G. Tenner, Director of Public Health Emergency Preparedness and Response, San Francisco Department of Public Health, San Francisco, California, USA; Associate Clinical Professor, Emergency Medicine, University of California San Francisco School of Medicine, San Francisco, California, USA.
Baljeet Sangha, System Chief Operating Officer and Deputy Director, San Francisco Department of Public Health, San Francisco, California, USA.
Tiffany Rivera, Deputy Director, Public Health Emergency Preparedness and Response, San Francisco Department of Public Health, San Francisco, California, USA.
Kenpou Saelee, Program Coordinator, Emergency Preparedness, San Francisco Department of Public Health, San Francisco, California, USA.
Claire Horton, Vice President and Associate Chief Medical Officer, National Medicaid Program, Kaiser Permanente National Health Plan and Hospitals, Oakland, California, USA; Former Chief Medical Officer, San Francisco Health Network, San Francisco Department of Public Health, San Francisco, California, USA.
Adrienne Green, Professor of Medicine, University of California San Francisco School of Medicine, San Francisco, California, USA; CEO, San Francisco Campus for Jewish Living, San Francisco, California, USA.
Vernon Giang, Chief Medical Executive, California Pacific Medical Center, Sutter Health, San Francisco, California, USA.
Bruce Ovbiagele, Chief of Staff, San Francisco Veterans Affairs Health Care System, San Francisco, California, USA.
Justin Quock, Chief, Department of Internal Medicine, Chinese Hospital, San Francisco, California, USA.
Todd LeVine, Chief Medical Officer, Dignity Health/CommonSpirit, San Francisco, California, USA.
Jonathan Sears, Senior Lean Specialist, California Department of Health, Sacramento, California, USA; Former Covid-19 Vaccine Branch Director, San Francisco Department of Public Health, San Francisco, California, USA.
Amabel Chow, Special Projects Manager, San Francisco Department of Emergency Management, San Francisco, California, USA; Former Covid-19 Vaccine Branch Operations Lead, San Francisco Department of Public Health, San Francisco, California, USA.
Ellie Schafer, Former Program Coordinator, Covid-19 Vaccine Branch Operations, San Francisco Department of Emergency Management, San Francisco, California, USA.
Eleanor Morse, Program Coordinator, San Francisco Department of Public Health, San Francisco, California, USA; Former Covid-19 Vaccine Branch Logistics Unit Deputy, San Francisco Department of Public Health, San Francisco, California, USA.
John Brown, Medical Director, San Francisco Emergency Medical Services Agency, San Francisco Department of Public Health, San Francisco, California, USA; Clinical Professor of Emergency Medicine, University of California San Francisco Medical School, San Francisco, California, USA.
Elizabeth Connelly, Kaizen Promotion Office, Predictive Analytics Fellow, Zuckerberg San Francisco General Hospital, San Francisco, California, USA; Former Covid-19 Advanced Planning Branch Director, San Francisco Department of Public Health, San Francisco, California, USA.
Jim Marks, Professor of Anesthesiology, University of California San Francisco School of Medicine, San Francisco, California, USA; Former Chief of Performance Excellence, Zuckerberg San Francisco General Hospital, San Francisco Department of Public Health, San Francisco, California, USA.
Wayne Enanoria, Chief Science Officer, Santa Clara County Department of Public Health, San Jose, California, USA; Assistant Professor, Epidemiology & Biostatistics, University of California San Francisco School of Medicine, San Francisco, California, USA; Former Director of Applied Research Community Health Epidemiology and Surveillance (ARCHES), San Francisco Department of Public Health, San Francisco, California, USA.
Susan Ehrlich, CEO, Zuckerberg San Francisco General Hospital, San Francisco, California, USA; Professor of Medicine, University of California San Francisco School of Medicine, San Francisco, California, USA.
Susan Philip, Health Officer, City and County of San Francisco, San Francisco, California, USA; Director, Population Health Division, San Francisco Department of Public Health, San Francisco, California, USA.
Naveena Bobba, Deputy Director of Health, San Francisco Department of Public Health, San Francisco, California, USA.
Grant Colfax, Director of Health, City and County of San Francisco, San Francisco, California, USA.
References
- 1.Farrell TW, Francis L, Brown T, et al. Rationing limited healthcare resources in the COVID-19 era and beyond: ethical considerations regarding older adults. J Am Geriatr Soc 2020;68:1143–9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7267288/ 10.1111/jgs.16539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gershengorn HB, Holt GE, Rezk A, et al. Assessment of disparities associated with a crisis standards of care resource allocation algorithm for patients in 2 US hospitals during the COVID-19 pandemic. JAMA Netw Open 2021;4:e214149 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7980099/ https://doi.org/10.1001/jamanetworkopen.2021.4149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hick JL, Hanfling D, Wynia M. Hospital planning for contingency and crisis conditions: crisis standards of care lessons from COVID-19. Jt Comm J Qual Patient Saf 2022;48:354–61 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8828442/ https://doi.org/10.1016/j.jcjq.2022.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simon P, Ho A, Shah MD, Shetgiri R. Trends in mortality from COVID-19 and other leading causes of death among Latino vs white individuals in Los Angeles County, 2011–2020. JAMA 2021;326:973–4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8290334/ https://doi.org/10.1001/jama.2021.11945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez DA, Hinson JS, Klein EY, et al. SARS-CoV-2 positivity rate for Latinos in the Baltimore-Washington, DC region. JAMA 2020;324:392–5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7303900/ https://doi.org/10.1001/jama.2020.11374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and white patients with Covid-19. N Engl J Med 2020;382:2534–43 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7269015/ https://doi.org/10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kriss JL, Hung MC, Srivastav A, et al. COVID-19 vaccination coverage, by race and ethnicity — National Immunization Survey Adult COVID Module, United States, December 2020–November 2021. MMWR Morb Mortal Wkly Rep 2022;71:757–63 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9181054/ https://doi.org/10.15585/mmwr.mm7123a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boehmer TK, Koumans EH, Skillen EL, et al. Racial and ethnic disparities in outpatient treatment of COVID-19 — United States, January–July 2022. MMWR Morb Mortal Wkly Rep 2022;71:1359–65 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9620572/ https://doi.org/10.15585/mmwr.mm7143a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.City and County of San Francisco. COVID-19 Data and Reports. Accessed February 15, 2024. https://www.sf.gov/resource/2021/covid-19-data-and-reports. [Google Scholar]
- 10.Public Health Alliance of Southern California. Welcome to the Healthy Places Index. 2022. Accessed October 1, 2023. https://www.healthyplacesindex.org/. [Google Scholar]
- 11.United States Census Bureau. Quick Facts. San Francisco County, California. Population Estimates, July 1, 2023. (V2023). Accessed June 30, 2023. https://www.census.gov/quickfacts/sanfranciscocountycalifornia. [Google Scholar]
- 12.United States Census Bureau. Census Bureau Reports 265,000 Workers Commute into San Francisco County, Calif., Each Day. March 5, 2013. Accessed June 30, 2023. https://www.census.gov/newsroom/archives/2013-pr/cb13-r22.html. [Google Scholar]
- 13.City and County of San Francisco. City Performance Scorecards. Health Insurance Coverage. Accessed October 1, 2023. https://sfgov.org/scorecards/public-health/health-insurance-coverage. [Google Scholar]
- 14.Hung DY, Rundall TG, Lee J, Khandel N, Shortell SM. Managing through a pandemic: a daily management system for COVID-19 response and recovery. J Healthc Manag 2022;67:446–57 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9640242/ https://doi.org/10.1097/JHM-D-21-00319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aragón TJ, Cody SH, Farnitano C, et al. Crisis decision-making at the speed of COVID-19: field report on issuing the first regional shelter-in-place orders in the United States. J Public Health Manag Pract 2021;27(Suppl 1):S19–28 https://journals.lww.com/jphmp/fulltext/2021/01001/crisis_decision_making_at_the_speed_of_covid_19_.5.aspx https://doi.org/10.1097/PHH.0000000000001292. [DOI] [PubMed] [Google Scholar]
- 16.California Department of Public Health. Respiratory Virus Dashboard Updated May 22, 2024. Accessed October 1, 2023. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/Respiratory-Viruses/RespiratoryDashboard.aspx. [Google Scholar]
- 17.Sachdev DD, Petersen M, Havlir DV, et al. San Francisco’s citywide COVID-19 response: strategies to reduce COVID-19 severity and health disparities, March 2020 through May 2022. Public Health Rep 2023;138:747–55 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10323495/ https://doi.org/10.1177/00333549231181353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moench M Inside a Dedicated Covid Unit. San Francisco Chronicle. Updated April 9, 2020. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/Inside-SF-s-first-coronavirus-hospital-unit-15183217.php. [Google Scholar]
- 19.Chamie G, Marquez C, Crawford E, et al. Community transmission of severe acute respiratory syndrome coronavirus 2 disproportionately affects the Latinx population during shelter-in-place in San Francisco. Clin Infect Dis 2021;73(Suppl 2)S127–35 https://academic.oup.com/cid/article/73/Supplement_2/S127/5895337 https://doi.org/10.1093/cid/ciaa1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVID-19 stats: COVID-19 incidence, by age group — United States, March 1–November 14, 2020. MMWR Morb Mortal Wkly Rep 2021;69:1664 https://www.cdc.gov/mmwr/volumes/69/wr/mm695152a8.htm?s_cid=mm695152a8_w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bains G, Breyre A, Seymour R, et al. Centralized ambulance destination determination: a retrospective data analysis to determine impact on EMS system distribution, surge events, and diversion status. West J Emerg Med 2021;22:1311–6 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8597692/ https://doi.org/10.5811/westjem.2021.8.53198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fuchs JD, Carter HC, Evans J, et al. Assessment of a hotel-based COVID-19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Netw Open 2021;4:e210490 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7926291/ https://doi.org/10.1001/jamanetworkopen.2021.0490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moench M Coronavirus Patients from Overwhelmed Imperial County Fill Bay Area Hospital Beds. San Francisco Chronicle. Updated July 8, 2000. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/Coronavirus-patients-from-overwhelmed-Imperial-15395397.php. [Google Scholar]
- 24.Moench M San Quentin’s Coronavirus Outbreak Strains Marin, Bay Area Hospitals. San Francisco Chronicle. Updated July 7, 2000. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/San-Quentin-s-coronavirus-outbreak-strains-Bay-15392385.php. [Google Scholar]
- 25.California Department of Public Health. Crisis Care Continuum. January 21, 2021. Accessed October 1, 2023. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Crisis-Care-Continuum.aspx. [Google Scholar]
- 26.Centers for Disease Control and Prevention. COVID-19: Strategies to Mitigate Healthcare Personnel Staffing Shortages. Updated September 23, 2022. Accessed October 1, 2023. https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staff-shortages.html. [Google Scholar]
- 27.Alfandre D, Sharpe VA, Geppert C, et al. Between usual and crisis phases of a public health emergency: the mediating role of contingency measures. Am J Bioeth 2021;21:4–16 https://www.tandfonline.com/doi/full/10.1080/15265161.2021.1925778 https://doi.org/10.1080/15265161.2021.1925778. [DOI] [PubMed] [Google Scholar]
- 28.Fimrite P, Morris JD. UCSF Medical Workers Question Federal Distribution of COVID-19 Medicine. San Francisco Chronicle. May 8, 2000. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/UCSF-medical-workers-question-federal-15255699.php. [Google Scholar]
- 29.Thadni T SF to Open Three Mass Vaccination Sites with Hopes of Giving at Least 10,000 Vaccinations a Day. San Francisco Chronicle. January 15, 2021. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/S-F-to-open-three-mass-vaccination-sites-with-15874635.php. [Google Scholar]
- 30.Kushel M, DiPietro, Watts B. Bringing Covid-19 Vaccines to High Risk Populations—Like Those Who Are Homeless—Requires a Tailored Approach. The BMJ Opinion. March 22, 2021. Accessed October 1, 2023. https://blogs.bmj.com/bmj/2021/03/22/bringing-COVID-19-vaccines-to-high-risk-populations-like-those-who-are-homeless-requires-a-tailored-approach. [Google Scholar]
- 31.Fields J, Gutierrez JR, Marquez C, et al. Community-academic partnerships to address Covid-19 inequities: lessons from the San Francisco Bay Area. NEJM Catalyst. June 23, 2021. Accessed February 16, 2024. https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0135. [Google Scholar]
- 32.Peng J, Marquez C, Rubio L, et al. High likelihood of accepting COVID-19 vaccine in a Latinx community at high SARS-CoV-2 risk in San Francisco. Open Forum Infect Dis 2021;8:ofab202 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8083232/ https://doi.org/10.1093/ofid/ofab202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weng Y, Lu D, Bollyky J, et al. ; on Behalf of The California Pandemic Consortium. Race-ethnicity and COVID-19 vaccination beliefs and intentions: a cross-sectional study among the general population in the San Francisco Bay area. Vaccines (Basel) 2021;9:1406 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8705240/ https://doi.org/10.3390/vaccines9121406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stern RJ, Rafferty HF, Robert AC, et al. Concentrating vaccines in neighborhoods with high COVID-19 burden. NEJM Catalyst. April 6, 2021. Accessed February 16, 2024. https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0056. [Google Scholar]
- 35.Marquez C, Kerkhoff AD, Naso J, et al. A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among Latinx populations: from theory to practice. PLoS One 2021;16:e0257111 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8452046/ https://doi.org/10.1371/journal.pone.0257111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fagan K ‘This Is What Equity Looks Like’: Roving Teams Deliver COVID Vaccines Around S.F.’s Tenderloin. San Francisco Chronicle. Updated September 5, 2022. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/Tenderloin-COVID-vaccine-SF-17396467.php. [Google Scholar]
- 37.Vaziri A Second COVID Bivalent Booster Shots Set to Roll Out. Here’s What You Need to Know. San Francisco Chronicle. Updated April 19, 2023. Accessed October 1, 2023. https://www.sfchronicle.com/health/article/bivalent-covid-booster-cdc-walensky-faq-17906389.php. [Google Scholar]
- 38.Centers for Disease Control and Prevention. COVID-19 Mortality Overview: Provisional Death Counts for COVID-19. Last reviewed September 12, 2023. Accessed October 1, 2023. https://www.cdc.gov/nchs/covid19/mortality-overview.htm. [Google Scholar]
- 39.San Francisco Government. COVID-19 Deaths: COVID-19 Deaths in San Francisco, Including New and Cumulative Totals. Accessed October 1, 2023. https://sf.gov/data/COVID-19-cases-and-deaths#total-cases-and-deaths.
- 40.Lin R-G II, Money L, Greene S. San Francisco Bay Area’s COVID Death Rate Was Among the Lowest in the Nation. Here’s Why. Los Angeles Times. November 27, 2023. Accessed December 4, 2023. https://www.latimes.com/california/story/2023-11-27/san-franciscos-covid-death-rate-was-among-lowest-in-nation. [Google Scholar]
- 41.KFF. KFF COVID-19 Vaccine Monitor. Accessed December 4, 2023. https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard. [Google Scholar]
- 42.California Department of Public Health. COVID-19 Vaccination Data. Updated February 2, 2024. Accessed December 4, 2023. https://covid19.ca.gov/vaccination-progress-data/. [Google Scholar]
- 43.Chokshi DA, Katz MH. Emerging lessons from COVID-19 response in New York City. JAMA 2020;323:1996–7 https://jamanetwork.com/journals/jama/fullarticle/2766403 https://doi.org/10.1001/jama.2020.7310. [DOI] [PubMed] [Google Scholar]
- 44.Powell T, Chuang E. COVID in NYC: what we could do better. Am J Bioeth 2020;20:62–6 https://www.tandfonline.com/doi/full/10.1080/15265161.2020.1764146 https://doi.org/10.1080/15265161.2020.1764146. [DOI] [PubMed] [Google Scholar]
- 45.Piscitello GM, Kapania EM, Miller WD, Rojas JC, Siegler M, Parker WF. Variation in ventilator allocation guidelines by US state during the coronavirus disease 2019 pandemic: a systematic review. JAMA Netw Open 2020;3:e2012606 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767360 https://doi.org/10.1001/jamanetworkopen.2020.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cavallo JJ, Donoho DA, Forman HP. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic — planning for the nth patient. JAMA Health Forum 2020;1:e200345 https://jamanetwork.com/journals/jama-health-forum/fullarticle/2763353 https://doi.org/10.1001/jamahealthforum.2020.0345. [DOI] [PubMed] [Google Scholar]
- 47.Aron JA, Bulteel AJB, Clayman KA, et al. Strategies for responding to the COVID-19 pandemic in a rural health system in New York state. Healthc (Amst) 2021;9:100508 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8055183/ https://doi.org/10.1016/j.hjdsi.2020.100508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tangcharoensathien V, Bassett MT, Meng Q, Mills A. Are overwhelmed health systems an inevitable consequence of Covid-19? Experiences from China, Thailand, and New York State. BMJ 2021;372:n83 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8896039/ https://doi.org/10.1136/bmj.n83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Feldman SL, Mayer PA. Arizona health care systems’ coordinated response to COVID-19—“In It Together.” JAMA Health Forum 2020;1:e201064 https://jamanetwork.com/journals/jama-health-forum/fullarticle/2769929 https://doi.org/10.1001/jamahealthforum.2020.1064. [DOI] [PubMed] [Google Scholar]
- 50.Maurer ML. Leading a hospital Incident Command System during a global pandemic. J Emerg Manag 2021;18:183–7 https://wmpllc.org/ojs/index.php/jem/article/view/2917 https://doi.org/10.5055/jem.0555. [DOI] [PubMed] [Google Scholar]
- 51.Hartnett J, Houston KD, Rose SJ. Augmentation of a hospital Incident Command System to support continued waves of the COVID-19 pandemic. J Healthc Leadersh 2022;14:191–201 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9700468/ https://doi.org/10.2147/JHL.S372909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaye AD, Cornett EM, Kallurkar A, et al. Framework for creating an incident command center during crises. Best Pract Res Clin Anaesthesiol 2021;35:377–88 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8428470/ https://doi.org/10.1016/j.bpa.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holtzclaw T, Newman SD, Dwyer M, Simpson J, Goodwin T. Coronavirus disease 2019 in the emergency department: establishing an interprofessional Incident Command System. J Emerg Nurs 2022;48:477–83 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9249398/ https://doi.org/10.1016/j.jen.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tapia-Conyer R, Valdez-Vázquez RR, Lomelín-Gascín J, Saucedo-Martínez R, Martinez-Juarez LA, Gallardo-Rincón H. Rapid establishment of a dedicated COVID-19 hospital in Mexico City during a public health crisis. Hosp Pract 2021;50:183–7 https://www.tandfonline.com/doi/full/10.1080/21548331.2021.2017644 https://doi.org/10.1080/21548331.2021.2017644. [DOI] [PubMed] [Google Scholar]
- 55.Smith IM, Bayliss E. Recovering staff, recovering services: massive-online support for recovering a paediatric service using Lean and compassionate communication. BMJ Open Qual 2022;11:e001914 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9234906/ https://doi.org/10.1136/bmjoq-2022-001914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lanza-León P, Sanchez-Ruiz L, Cantarero-Prieto D. Kanban system applications in healthcare services: a literature review. Int J Health Plann Manage 2021;36:2062–78 https://onlinelibrary.wiley.com/doi/10.1002/hpm.3276 https://doi.org/10.1002/hpm.3276. [DOI] [PubMed] [Google Scholar]
- 57.Ho C SF to Get More Than 4,000 Doses of Monkeypox Vaccine Next Week. San Francisco Chronicle. July 15, 2022. Accessed October 1, 2023. https://www.sfchronicle.com/bayarea/article/More-monkeypox-vaccine-on-the-way-federal-health-17308378.php#photo-22706546. [Google Scholar]
- 58.Ho C SF Says Clinic Is Out of Monkeypox Vaccine, Will Be Closed Tuesday. San Francisco Chronicle. August 10, 2022. Accessed October 1, 2023. https://www.sfchronicle.com/bayarea/article/S-F-says-clinic-is-out-of-monkeypox-vaccine-17328129.php. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.