Abstract
Onconephrology, an emerging discipline nestled at the intersection of nephrology and oncology, has experienced remarkable growth over the past 15 years. This evolution has been punctuated by pivotal events, including establishing the American Society of Onconephrology, dedicated forums, and journals, highlighting its increasing significance. The clinical landscape of onconephrology is diverse, encompassing AKI in patients with cancer, toxicity from anticancer treatments, and a spectrum of electrolyte disorders, necessitating close collaboration between nephrologists and oncologists. However, trainees and mentors encounter various challenges surrounding its status as a distinct subspecialty. To overcome these barriers, there is a pressing need for streamlined training pathways, enhanced interdisciplinary collaboration, and targeted research efforts to elucidate the effect of onconephrology on patient outcomes. By addressing these challenges head-on, the field of onconephrology can continue its trajectory of growth and better serve patients with cancer with complex kidney needs.
Keywords: cancer, health policy, nephrology, onconephrology
Introduction
The subspecialty of onconephrology has rapidly evolved over the past 15 years, marked by significant milestones and advancements. Onconephrologists, pioneers in this field, continuously adapt to the ever-changing landscape of anticancer therapies and their effect on kidney health. This dynamic journey has been shaped by pivotal moments, reflecting the growing recognition and commitment to advancing onconephrology. The American Society of Nephrology (ASN) and the establishment of the American Society of Onconephrology (ASON) in 2022 played a pivotal role in this evolution. They acknowledged the importance of onconephrology and paved the way for dedicated forums and educational initiatives.
As the landscape of onconephrology continues to evolve, it becomes imperative to address the challenges and opportunities facing this thriving field. Collaborative efforts between nephrologists and oncologists are essential for effectively identifying and managing kidney disease in patients with cancer, leading to the formation of multidisciplinary care teams. However, several challenges hinder the progress of onconephrology training, ranging from a need for more centralized application processes to limited opportunities for trainees interested in this field.
In this comprehensive overview, we delve into the current status of onconephrology fellowship training, the challenges faced by trainees and mentors, and potential interventions to overcome these obstacles. By exploring the rich history, clinical scope, and future directions of onconephrology, we aim to inspire further advancements and collaborations in this field of nephrology.
History of Onconephrology
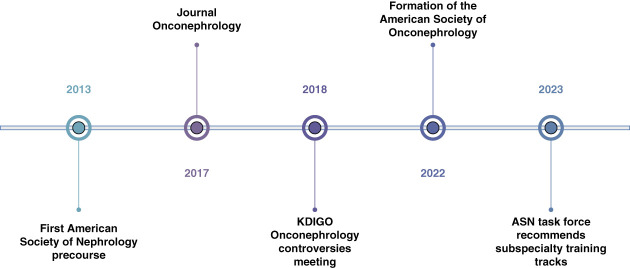
The subspecialty of onconephrology has witnessed remarkable growth since its inception approximately 15 years ago. Onconephrologists remain at the forefront of knowledge, continually adapting to new anticancer therapies and comprehending their effect on the kidneys. Over the past decade, pivotal milestones have shaped this dynamic field. The ASN recognized the importance of onconephrology and allowed for the establishment of a dedicated forum group, and in 2013, the inaugural ASN precourse was introduced. The same year nephrology self-assessment program dedicated the January 2013 issue for Cancer and the Kidneys, followed by an online ASN Onconephrology curriculum in 2016 that was updated in 2023. Subsequently, in 2017, the creation of the Journal of Onco-Nephrology marked a significant advancement in academic discourse. The momentum continued in 2018 with the first Kidney Disease Improving Global Outcomes onconephrology controversies meeting in Milan, Italy, fostering critical discussions and collaborations. These collective endeavors culminated in establishing the ASON in 2022, underscoring the growing recognition and commitment to advancing the field.1 Since its creation, ASON has championed numerous initiatives to propel the field forward. These include hosting annual onconephrology symposiums, organizing virtual educational conferences, fostering partnerships with international societies to facilitate knowledge exchange and collaboration, providing mentorship opportunities, and facilitating multicenter research collaborations. Figure 1 summarizes important events in the history of onconephrology.
Figure 1.
Onconephrology event time line. ASN, American Society of Nephrology; KDIGO, Kidney Disease Improving Global Outcomes.
Onconephrology Clinical Scope
The clinical scope of the field is broad because the relationship between cancer and kidneys is bidirectional. AKI stands as a prevalent concern, prompting frequent consultations among patients with cancer. The risk of AKI hovers between 17% and 27% within the initial 5 years after diagnosis, with critically ill individuals facing the highest susceptibility.2 AKI exerts a profound negative effect on patients with cancer, affecting their eligibility for treatment, increasing mortality rates, and dimming overall prognosis.3 With the advances in cancer treatment, patients have prolonged survivorship, and we are now encountering multiple patients with CKD and ESKD on renal replacement therapies. CKD itself is associated with decreased survival in patients with cancer. In a retrospective study of 8223 patients with cancer, the incidence of CKD was 12.8%; CKD in patients with cancer was associated with a higher risk of death, with an adjusted hazard ratio of 1.12 for eGFR of 30 to<60 ml/min per 1.73 m2 (95% confidence interval, 1.01 to 1.26; P = 0.04) and 1.75 for patients with an eGFR <30 ml/min per 1.73 m2 (95% confidence interval, 1.32 to 2.32; P < 0.001).4 Accurate adjustments in chemotherapy dosages in patients with CKD and cancer become imperative to achieve adequate efficacy in treating cancer. Moreover, onconephrologists navigate a diverse spectrum of electrolyte disorders arising from cancer and anticancer treatments, with hyponatremia,5 hyperkalemia,6 hypercalcemia,7 and hypomagnesemia8 among the most prevalent. Table 1 summarizes the clinical scope of onconephrology.
Table 1.
Clinical scope of onconephrology
| AKI in patients with cancer |
| CKD in patients with cancer |
| BP disorder from chemotherapy |
| Electrolyte disorders of malignancy |
| Tumor lysis syndrome |
| Multiple myeloma–related kidney disease |
| Secondary glomerular diseases from malignancy or related to cancer treatment |
| Stem cell transplant–related kidney diseases |
| CAR-T-cell therapy–related kidney disorders |
| Chemotherapy dosing adjustments to kidney disease |
| Kidney disease after nephrectomy |
| Paraproteinemias |
| Anticancer drug–related nephropathies |
CAR, chimeric antigen receptor.
Collaborative care between oncologists and nephrologists is essential for effectively identifying and managing kidney disease in patients with cancer. This has led to the formation of multidisciplinary teams, with onconephrologists being an integral pillar of the care team. Providing care for such intricate patients requires an active and mutually collaborative relationship among specialties. In large cancer centers, the onconephrologist expertise is valuable in complex cases, such as chimeric antigen receptor (CAR)-T-cell administration in ESKD, high risk of chemotherapy-induced tumor lysis syndrome, and AKI in post-stem cell transplant patients, among other scenarios.
Nephrology Training Status and Reimagining Nephrology Training
Over the past decade, interest in nephrology as a career hit a low point, resulting in fewer applicants and an increase in unfilled positions. Many nephrology programs fill empty positions through the post-match scramble process. However, in the most recent match for 2023, there was a 7% increase in matched candidates compared with the previous year.9
In response to declining interest in nephrology and a limited applicant pool, the ASN proactively established a task force in April 2022. The primary objective of this task force was to reshape the future landscape of nephrology training comprehensively. This task force gathered input from various stakeholders, including individuals with kidney diseases, fellows, program directors, division chiefs, private practice nephrologists, and dialysis organization leaders. Their collective insights provided invaluable perspectives on the challenges and opportunities facing nephrology training. Currently, nephrology trainees have minimal exposure to onconephrology during their 2-year training despite encountering cases involving malignancies, chemotherapy toxicity, and electrolyte disorders in patients with cancer. As the field of nephrology continues to evolve rapidly, the demand for nephrology providers equipped with the required knowledge, skills, values, and attitudes to deliver high-quality care to patients with cancer with kidney diseases is increasing. The ASN task force made ten recommendations.10 Among these recommendations is “establishing individualized pathways to meet career goals,” which emphasizes the opportunities for trainees to explore advanced specialized care, including onconephrology, during their second year of training. Recognizing this imperative, augmenting exposure to onconephrology, and introducing a structured teaching curriculum within nephrology training programs become crucial. By doing so, we are addressing the existing gaps in training and potentially stimulating greater interest and engagement among aspiring nephrologists, enhancing interest in the subspecialty.
The Current Status of Onconephrology Fellowship Training
The ASON lists six training onconephrology programs in the United States and Canada:
Mayo Clinic, Rochester, MN.
MD Anderson Cancer Center, Houston, TX.
Memorial Sloan Kettering Cancer, New York, NY.
University Health Network, Toronto, Canada.
North Shore University Hospital, Hempstead, NY.
University of Pennsylvania, Philadelphia, PA.
All these programs offer a dedicated onconephrology training year after the completion of a 2-year nephrology fellowship. The training is both inpatient and outpatient clinical training, in addition to an expectation for research performed during dedicated rotations. Research dedicated time varies between 4 and 24 weeks, depending on the training program.11
Several models of training are used, with most of the programs using a mixture of the following: integration of the onconephrology trainee with the inpatient oncology team, outpatient elective with oncology specialists (e.g., stem cell transplant, myeloma, transfusion medicine, and others), dedicated onconephrology outpatient clinic, and dedicated inpatient onconephrology consult services. The time allocation for each of these different clinical rotations varies. It is notable that both Northwell Health/North Shore University Hospital and the University of Pennsylvania offer onconephrology training in a combined track with glomerular disease.
The scope of training is quite similar between all six programs with a focus on12
Chemotherapy: dosing and kidney adverse events.
Management of CKD in patients with malignancy and cancer survivors.
Monoclonal gammopathy of renal significance.
Glomerular disease associated with malignancy and stem cell transplantation.
These training programs have been successful in graduating onconephrology fellows who are expanding the field through their clinical and research expertise. During a 4-year period, onconephrology fellows from four training programs presented more than 45 abstracts and published more than 40 articles.11
After their dedicated training, the graduating onconephrology fellows are helping the establishment of onconephrology as a nephrology subspecialty by decreasing the skepticism of their nephrology colleagues regarding this field. More recently, the “ASN Task Force, the Future of Nephrology” mentioned onconephrology as an emerging subspecialty training track and recommended “embracing” subspecialization and “adjusting” the training models to better support subspecialization.10
Challenges Faced by Onconephrology Trainees and Mentors
As pioneers of the field, both mentors and trainees in onconephrology are experiencing a multitude of challenges that are slowing the forward progress of this subspecialization track (summary in Table 2).
Table 2.
Summary of challenges and some suggestions on how to address it
| Challenges | Suggestions |
|---|---|
| Onconephrology application process | • Add onconephrology to the subspecialty track by the ASN • Add information about the application process on the ASON website (e.g., deadline, visa requirement) |
| Restriction around the immigration status of the interested trainee | • Work with the leader of nephrology advocacy groups to introduce immigration exception for a trainee on the nephrology subspecialty track • Seek institutional and philanthropic funding for onconephrology training |
| Limited multidisciplinary rounds for training | • Carve out an onconephrology consult service • Collaboration with other institutions to supplement the lecture series and introduce frequent case discussion forum attended by a nephrologist and an oncologist |
| Dedifferentiation of onconephrology as a stand-alone subspecialty | • Mandate specialized training in CAR-T-cell therapy and explore the possibility of performing this therapy by onconephrologists • Mandate specialized training in clone-directed therapy and explore the possibility of performing this therapy by onconephrologists • Prioritize training in immune-related adverse effects, oncopharmacology and transplant oncology |
| Requirement for an extra year of training | • An integrated onconephrology training track within the 2-yr nephrology training is feasible especially for a trainee seeking clinical skills • Combining onconephrology training with palliative care or glomerular disease can be offered to a trainee who elect for an extra year of postnephrology fellowship |
| Uncertainty of the job prospects | • Mentoring on the structure of an onconephrology clinic • Research focused on the financial effect of onconephrology expertise |
ASN, American Society of Nephrology; ASON, American Society of Onconephrology; CAR, chimeric antigen receptor.
Lack of a centralized training application:
Onconephrology training is advertised on the ASON and the individual institutional websites. The ASN website does not include onconephrology training in the subspecialized training pathways.
Suggested interventions:
The main web search destination for subspecialty training remains the ASN and the subspecialty society websites, ASON in the case of onconephrology. The ASN is embracing subspecialization and can start listing onconephrology as a training track and refer applicants to the ASON and the individual training programs for information regarding the application process.
The information on the ASON website and individual training program can be more comprehensive: the application deadline, salary, and, more importantly, the restrictions around the applicant's immigration status.
Limited opportunities for interested nephrology trainees with exchange visitor (e.g., J-1) or temporary worker (e.g., H-1B) immigrationstatus.
Because the onconephrology fellowship is not Accreditation Council for Graduate Medical Education accredited, some training programs require the trainee to be employed under the title of instructor and some require the trainee to treat patients independently and thus be eligible for state medical license. These requirements disqualify up to a quarter of nephrology fellows from applying to onconephrology because of the incompatibility of the immigration status like exchange visitor (e.g., J-1) or temporary worker (e.g., H-1B).13
Suggested interventions:
Navigating immigration requirements is not unique to the onconephrology subspecialty and requires joining forces with the leader of ASN, the National Kidney Foundation, and the Renal Physicians Association to create a plan for a comprehensive solution.
Funding through institutional and philanthropic grants can help overcome the financial restraints.
Limited multidisciplinary clinical space for onconephrology training.
Onconephrology is a new subspecialty, and most institutions do not have a prespecified inpatient consult service. To create the training space for onconephrologists, the trainees are integrated, during their clinical rotation, with the inpatient oncology teams.
Suggested interventions:
Training programs can work within their institutions to carve out a dedicated onconephrology consult service staffed by the general nephrology fellows under the supervision of the onconephrology fellow and/or faculty. The rotation with the oncology team is still essential and can be scheduled during mandatory elective weeks built into the curriculum.
Collaboration across institutions in the form of webinars and remote presentations, with a specific focus on case-based presentations, will supplement the medical knowledge for onconephrology trainees. An alternative is to supplement the clinical training by a remote training, such as the GlomCon (https://www.glomcon.org/) initiative for glomerular diseases.
Support and engage with initiatives that are creating onconephrology resources, such as the Onconephrotoxins Library Collaboration (https://www.olic-app.info/). Onconephrotoxins Library Collaboration is a comprehensive database of nephrotoxins that is focused on oncology products and is continuously updated.
Skepticism regarding the scope and status of onconephrology as a stand-alone nephrology subspecialty.
The diagnostic tools and therapeutic skills used by onconephrologists are similar and within the scope of a trained nephrologist. Some nephrologists, especially those practicing in medical centers with a large oncology population, are familiar with onconephrology patients and are skeptical about onconephrology as a subspecialty. This skepticism is understandable and expected to fade away as the field grows and becomes progressively differentiated.
Suggested interventions:
More work is needed to align the onconephrology curriculum across institutions and introduce mandatory onconephrology training in specific oncologic therapies that are outside the scope of a general nephrologist, such as immunotherapy, clone-directed therapy, stem cell transplantation, and CAR-T-cell therapy.
Explore potential training of onconephrologists in the administration of CAR-T-cell therapy for autoimmune disease. CAR-T-cell therapy is emerging as a therapeutic tool in autoimmune kidney disease, mainly lupus nephritis.14 An onconephrologist comfortable counseling and/or treating patients with CAR-T-cell therapy can certainly claim a differentiating skill.
Other potential differentiating skills is in oncopharmacology (chemotherapy drug dosing in patients with CKD and those receiving KRT) and oncology in kidney transplant recipients (focused on adverse effects associated with chemotherapy and immunotherapy).
The need for an additional training year: The current training opportunities are more compatible with the needs of trainees looking for clinical academic or research careers. The training pathways need diversification beyond the current additional year of training after finishing the nephrology fellowship.
Suggested interventions:
Create an onconephrology training track integrated within the 2-year nephrology training. The current ACGME nephrology requirement is for only 12 months of clinical experience, which opens the opportunity for focused training during the “other 12 months.” It is reasonable to expect that, with some adjustments to the other 12 months, a nephrology trainee can develop advanced clinical expertise in onconephrology. This training track fulfills the need for an onconephrologist looking for a clinical career.
Combining onconephrology training with other emerging or established subspecialty training, palliative care or glomerular disease is a realistic field for a combined training track: Glomerular disease uses oncologic therapeutic tools like chemotherapy, targeted therapy and immunotherapy with CAR-T-cell therapy. Monoclonal gammopathy or renal significance is within the spectrum of glomerular disease and onconephrology. Palliative care can also be combined with onconephrology because patients with oncology frequently require palliative services during their disease journey, and when kidney disease becomes the main comorbidity, a combined knowledge of nephrology, palliative care, and oncology fields is very helpful.
Uncertainty around job prospects: Most nephrology trainees will end up practicing in private practice, and most onconephrology patients are treated in private practice.13 Private practice is a highly undifferentiated nephrology job; the current payment model disincentivizes taking care of patients with complex kidney diseases, all this makes onconephrology training less attractive when looking for a job.
Future suggestions:
In addition to the clinical training, the trainee should be mentored regarding models of care delivery that are viable in private practice to overcome the challenges of nephrology payment models (e.g., the structure of onconephrology clinic: workflow for urgent onconephrology consult, creating a mixed panel of patients with high complexity (e.g., AKI, thrombotic microangiopathy and immunotherapy toxicity) and less complexity (e.g., post-chemotherapy CKD, uro-oncology patients). Trained onconephrologists should expect that their practice will include some work outside the scope of onconephrology training, such as outpatient dialysis to balance the relative value unit generation.
Additional research focused on the financial effect of employing a trained onconephrologist is needed: The effect of onconephrology expertise in quickly resolving kidney questions leading to more rapid resumption of oncology therapy can be financially appealing to institutions with a large number of patients with cancer.
Conclusion
Over the past 15 years, onconephrology has become an established nephrology subspecialty. Its scope is expanding and becoming increasingly differentiated from general nephrology. Training of onconephrology is offered by a limited number of institutions with a diverse training model. Efforts to align curriculums, clarify the application process, and additional funding can address training challenges. Additional challenges need collaboration between institutions and advocacy groups to assist with the immigration requirements and research in the financial benefits of onconephrology subspecialization.
Disclosures
Disclosure forms, as provided by each author, are available with the online version of the article at http://links.lww.com/KN9/A555.
Funding
None.
Author Contributions
Conceptualization: Abdallah S. Geara.
Methodology: Macro Bonilla.
Writing – original draft: Macro Bonilla, Abdallah S. Geara.
Writing – review & editing: Macro Bonilla, Abdallah S. Geara.
References
- 1.Rashidi A Jhaveri KD Workeneh BT, et al. The path toward the creation of the American Society of Onco-Nephrology (ASON). J Onco Nephrol. 2022;6(1-2):3–5. doi: 10.1177/23993693221079647 [DOI] [Google Scholar]
- 2.Gupta S, Gudsoorkar P, Jhaveri KD. Acute kidney injury in critically ill patients with cancer. Clin J Am Soc Nephrol. 2022;17(9):1385–1398. doi: 10.2215/CJN.15681221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Can W, Rong L, Lixia L. Incidence and risk factors of acute kidney injury in patients with malignant tumors: a systematic review and meta-analysis. BMC Cancer. 2023;23(1):1123. doi: 10.1186/s12885-023-11561-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Na SY Sung JY Chang JH, et al. Chronic kidney disease in cancer patients: an independent predictor of cancer-specific mortality. Am J Nephrol. 2011;33(2):121–130. doi: 10.1159/000323740 [DOI] [PubMed] [Google Scholar]
- 5.Workeneh BT, Jhaveri KD, Rondon-Berrios H. Hyponatremia in the cancer patient. Kidney Int. 2020;98(4):870–882. doi: 10.1016/j.kint.2020.05.015 [DOI] [PubMed] [Google Scholar]
- 6.Ratanasrimetha P, Workeneh BT, Seethapathy H. Sodium and potassium dysregulation in the patient with cancer. Adv Chronic Kidney Dis. 2022;29(2):171–179. doi: 10.1053/j.ackd.2022.01.003 [DOI] [PubMed] [Google Scholar]
- 7.El-Hajj Fuleihan G Clines GA Hu MI, et al. Treatment of hypercalcemia of malignancy in adults: an endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2023;108(3):507–528. doi: 10.1210/clinem/dgac621 [DOI] [PubMed] [Google Scholar]
- 8.Bonilla M, Workeneh BT, Uppal NN. Hypomagnesemia in patients with cancer: the forgotten ion. Semin Nephrol. 2022;42(6):151347. doi: 10.1016/j.semnephrol.2023.151347 [DOI] [PubMed] [Google Scholar]
- 9.Pivert KA. First Look: AY 2023 Match; 2022. Accessed June 1, 2024. https://data.asn-online.org/posts/ay_2023_match [Google Scholar]
- 10.Rosenberg ME Anderson S Farouk SS, et al. Reimagining nephrology fellowship education to meet the future needs of nephrology: a report of the American Society of Nephrology task Force on the Future of Nephrology. Clin J Am Soc Nephrol. 2023;18(6):816–825. doi: 10.2215/CJN.0000000000000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Latcha S Kala J Kitchlu A, et al. An extra year of Onco-Nephrology fellowship training is required for the subspecialty: PRO. J Onco Nephrol. 2020;5(1):31–34. doi: 10.1177/2399369320965578 [DOI] [Google Scholar]
- 12.Jhaveri KD, Agarwal S, Kenar D, Jhaveri SA. Onco-nephrology, an extra year of training: where do we stand? J Onco Nephrol. 2020;5(1):39–41. doi: 10.1177/2399369320973044 [DOI] [Google Scholar]
- 13.Pivert K. ASN Data Subcommittee. Reports on the ASN Nephrology Fellow Survey 2019–2022; 2023. [Google Scholar]
- 14.Mackensen A Muller F Mougiakakos D, et al. Anti-CD19 CAR T cell therapy for refractory systemic lupus erythematosus. Nat Med. 2022;28(10):2124–2132. doi: 10.1038/s41591-022-02017-5 [DOI] [PubMed] [Google Scholar]