To the Editor: Appropriate sleep patterns are essential for human health. Investigating the associations between sleep duration and coronary heart disease (CHD) across populations will enhance our comprehension of the relationship between lifestyle and disease, and provide valuable guidance for developing preventive strategies against CHD. Previous studies have been conducted in this field. However, their results have been inconsistent due to the heterogeneous methodologies, study populations, and social factors. Notably, most of the studies examining sleep-associated CHD risk have been conducted in Japan, Europe, and China, whereas limited research is centered on this issue in US populations. More importantly, in recent years, there have been changes in people’s sleep patterns and the susceptibility factors of diseases. It is necessary to conduct new investigations to provide fresh evidence on the impact of sleep duration on CHD. We studied sleep patterns in US adults aged 20 years and over using the National Health and Nutrition Examination Survey (NHANES) database from 2005 to 2018. Our goal was to understand how sleep duration relates to CHD, with a focus on variations among distinct subgroups.
We analyzed sleep characteristics in a sample of 39,551 adults, representing 223.7 million Americans. In examining the relationship between sleep duration and CHD, we selected patients with complete data, totaling 15,923 individuals for our analysis. The NHANES is a major program of the National Center for Health Statistics (NCHS) designed to assess the health and nutritional status of the US population. The NCHS Ethics Review Board approved all NHANES protocols, and all participants provided written informed consent. Thus, additional ethical approval is unnecessary for our study.
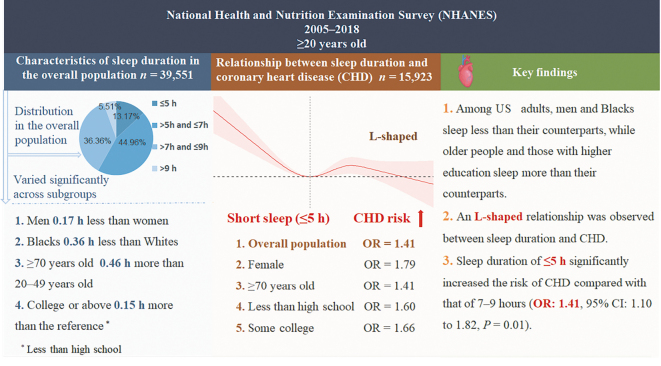
On the basis of previous studies, we categorized the estimated total daily sleep duration into four mutually exclusive groups (≤5 h, >5 h and ≤7 h, >7 h and ≤9 h [which was used as the reference], and >9 h).[1] The most common sleep duration was >5 h and ≤7 h (17,782/39,551, 44.96%), and the least common (2181/39,551, 5.51%) was >9 h. The other groups (≤5 h and >7 h and ≤9 h) had proportions of 13.17% (5208/39,551) and 36.36% (14,380/39,551), respectively. Relative to females, males had fewer hours of sleep (mean difference, 0.17 h; P <0.0001). Relative to White participants, Black participants had less sleep (0.36 h; P <0.0001), while Mexican American participants had more (0.11 h; P = 0.02). Those aged 70 years or over slept 0.46 h longer on average than those aged 20–49 years (P <0.0001). College graduates slept 0.15 h more than those whose education was less than high school (P <0.0001) [Figure 1].
Figure 1.
An overview of the distribution of sleep duration in US adults, the association of sleep duration with CHD in various subgroups, and summarization of the key findings. CI: Confidence interval; OR: Odds ratio; US: United States.
We used linear regression to obtain means and to compare sleep duration in these four subgroups. A multivariable logistic regression model was used to explore the association between sleep duration and CHD, and a restricted cubic spline (RCS) curve was used to describe the shape of the relationship of the above two variables. In the minimally adjusted models, we adjusted for age, sex, educational attainment, and race. The fully adjusted models added body mass index (BMI), use of hypnotics, smoking status (current/former vs. never), drinking status (drinker vs. non-drinker), history of diabetes and hypertension, and diagnosis of hyperlipidemia and depression. A P-value <0.05 is considered statistically significant. The data were analyzed, and visual plots were generated utilizing the R programming language v4.3.2 (https://www.r-project.org/), an open-source language for statistical computing. It’s maintained by the R Foundation, based in Vienna, Austria, and can be downloaded from CRAN.
In fully adjusted analyses, short duration of sleep (≤5 h) was associated with a significantly higher risk of CHD compared with >7 h and ≤9 h (odds ratio [OR]: 1.41; 95% confidence interval [CI]: 1.10–1.82, P = 0.01), independent of several potential confounders. When it comes to the trend test, the reference is ≤5 h; there was a non-linear trend between sleep duration and CHD in the fully adjusted model (adjusted for age, sex, race, educational attainment, smoking status, drinking status, hypnotics, BMI, depression, hypertension, hyperlipidemia, and diabetes mellitus [DM]; P for trend value = 0.08) [Supplementary Table 1, http://links.lww.com/CM9/C139]. Cubic spline analysis revealed a non-linear L-shaped relationship of sleep duration with risk of CHD [Supplementary Figure 1, http://links.lww.com/CM9/C139]. The forest plot shows the OR (95% CI) of sleep duration and risk of CHD at the subgroup level (sex, age, education attainment, and race) after adjusting for potential confounders. Compared with >7 h and ≤9 h (reference), a sleep duration of ≤5 h significantly increased the risk of CHD in women (OR: 1.79, 95% CI: 1.21–2.67), those aged ≥70 years (OR: 1.41, 95% CI: 1.00–1.99), those received less than high school education (OR: 1.60, 95% CI: 1.02–2.51), and those received some college education (OR: 1.66, 95% CI: 1.01–2.72). No significant differences were observed in the other groups [Supplementary Figure 2, http://links.lww.com/CM9/C139].
Our study presented three significant findings. First, among US adults, males and Blacks slept less than their counterparts, while older adults and those with higher education tended to have longer sleep duration. Second, there was an inverse relationship between short sleep duration and CHD among the study population. However, we have not observed any association between long sleep duration and CHD. After adjusting for multiple confounding factors, the conclusion still held, indicating that the regression model we constructed was stable. Third, we found that the association between short sleep duration and CHD was significant among females, individuals aged 70 years or above, and those with educational level less than high school or some college.
The National Sleep Foundation recommends >7 h and ≤9 h of sleep for adults (18–64 years) and 7–8 h for older adults (≥65 years).[2] However, changing socioeconomic factors have heavily influenced sleep patterns in the US in recent years. In our study, more than half of the population slept <7 h, and interestingly, subgroup analysis showed heterogeneity in the association between sleep duration and CHD across different populations.
In the analysis stratified by sex, short sleep duration (≤5 h) was associated with risk of CHD among women; whereas in men, the association was weak and not statistically significant. This conclusion is consistent with previous studies, including a large cohort study which suggested that the hazard ratio of myocardial infarction among women sleeping ≤5 h was greater than in men.[3] A complex combination of adverse social, economic, and environmental conditions can disadvantage Black people within the overall population.[4] These may lead them to get less sleep and this is seen in our study: 20.77% (1774/8542) of Blacks and 14.39% (547/3802) of Hispanics had sleep duration of no more than 5 h, while for White people, this was 10.75% (1770/16,472). Correspondingly, in this short sleep category, CHD risk was higher in Blacks and Mexican Americans than in Whites. This suggests that minority populations in the US experience more prevalent short sleep and are more adversely affected by it. We found that older adults (≥70 years) are more vulnerable to short sleep, which may indicate impaired sleep generation rather than reduced need, potentially elevating cardiovascular risks, as prior research suggests.[5] In our study, people with less-than-a-high-school education background had the shortest sleep duration, while college graduates or above had the longest. Educational attainment is particularly important for sleep in adulthood. This is possibly because those with lower-level education are more likely to face poor socioeconomic status (SES), graveyard shifts, or insufficient sleep health knowledge. Evidence has shown that low education is a causal risk factor in the development of CHD;[6] however, there is no evidence that sleep duration mediates this relationship. Our model observed that short sleep increased the risk of CHD in those with low education, but this phenomenon was also observed in those with some college education. Therefore, it does not suggest that the effect of sleep duration on CHD differs by education level.
Our study’s strength lies in providing novel insights into the relationship between sleep duration and CHD, coupled with an analysis of the variations in this association across distinct subgroups. Nonetheless, several limitations merit attention. Relying on NHANES questionnaire data for population sleep patterns introduces subjective elements, potentially affecting accuracy in distinguishing bedtime from sleep onset and precisely quantifying nap durations and frequencies. However, in large population studies, having each participant complete polysomnography (PSG) is not feasible. Moreover, given its cross-sectional design, this study is inherently limited to establishing associations between sleep duration and CHD, precluding definitive conclusions about causality. Finally, our study on sleep–CHD relations lacked direct SES analysis (income, education, occupation)—core health equity factors. Proxy variables (education, race) inadequately reflect SES’s diverse effects on sleep and cardiac health, complicating interpretation of its role. Cautious inference is essential given the SES assessment gap. Future work should use standardized SES metrics to clarify its intricate impact, deepening mechanistic understanding.
In conclusion, our study shows that there are significant racial and sex differences in sleep status in the US, and short sleep duration is associated with a high risk of CHD in women and people over 70 years old. Further longitudinal studies are needed to investigate their temporal causality and the underlying mechanisms of sleep characteristics associated with CHD. The association between long sleep duration and CHD needs to be further examined, considering the relatively low prevalence of long sleep duration.
Funding
The study was supported by the Chongqing Talent Program (No. CQYC20210303360).
Conflicts of interest
None.
Supplementary Material
Footnotes
Dan Deng and Wanxiang Zheng contributed equally to this work.
How to cite this article: Deng D, Zheng WX, Liu YH, Qian GZ, Bao XY, Chen YX, Zhu JF, Qu XL, Zhang ZH. Associations between sleep and coronary heart disease: Findings from NHANES database (2005–2018). Chin Med J 2024;137:2381–2383. doi: 10.1097/CM9.0000000000003291
References
- 1.Kim CW Chang Y Zhao D Cainzos-Achirica M Ryu S Jung HS, et al. Sleep duration, sleep quality, and markers of subclinical arterial disease in healthy men and women. Arterioscler Thromb Vasc Biol 2015;35:2238–2245. doi: 10.1161/atvbaha.115.306110. [DOI] [PubMed] [Google Scholar]
- 2.Hirshkowitz M Whiton K Albert SM Alessi C Bruni O DonCarlos L, et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015;1:233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Meisinger C, Heier M, Löwel H, Schneider A, Döring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: The MONICA/KORA Augsburg cohort study. Sleep 2007;30:1121–1127. doi: 10.1093/sleep/30.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Javed Z Haisum Maqsood M Yahya T Amin Z Acquah I Valero-Elizondo J, et al. Race, racism, and cardiovascular health: Applying a social determinants of health framework to racial/ethnic disparities in cardiovascular disease. Circ Cardiovasc Qual Outcomes 2022;15:e007917. doi: 10.1161/circoutcomes.121.007917. [DOI] [PubMed] [Google Scholar]
- 5.Mander BA, Winer JR, Walker MP. Sleep and human aging. Neuron 2017;94:19–36. doi: 10.1016/j.neuron.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tillmann T Vaucher J Okbay A Pikhart H Peasey A Kubinova R, et al. Education and coronary heart disease: Mendelian randomisation study. BMJ 2017;358:j3542. doi: 10.1136/bmj.j3542. [DOI] [PMC free article] [PubMed] [Google Scholar]