Abstract
Takayasu arteritis is a rare vasculitis of the aorta and its branches. Here, we present a teenaged athlete with coronary arteritis and pyoderma gangrenosum, the youngest person whose case is described in the literature. She received immune modulation and percutaneous coronary intervention, with subsequent in-stent restenosis and cardiac arrest requiring coronary artery bypass grafting.
Key Words: autoimmune, coronary artery bypass, percutaneous coronary intervention, vascular disease
Graphical Abstract

A 16-year-old high-dynamic sport athlete was prescribed isotretinoin for nodulocystic acne on her chest and back. During this treatment, her skin lesions spread to her hip and thigh. A dermatologist diagnosed acne fulminans and prescribed doxycycline, prednisone, topical corticosteroids, and later clarithromycin. A transthoracic echocardiogram (TTE) was requested by the family to rule out cardiac toxicity from clarithromycin, and she was referred to the cardiology service. At initial evaluation, the result of a review of systems was negative for cardiac and systemic symptoms during competitive play. Physical examination revealed a 13 × 5 cm tender, oval, erythematous lesion with a 4 × 6 cm central clearing and weeping edges on her left flank (Figure 1) in a well-appearing teenaged girl with normal vital signs. She had 2 similar smaller lesions on her back and scarring on her chest from healed lesions.
Learning Objectives
-
•
To understand the risks of PCI in Takayasu arteritis.
-
•
To recognize that pyoderma gangrenosum can be associated with Takayasu arteritis.
-
•
To demonstrate that Takayasu arteritis can present in adolescents with minimal cardiac symptoms despite significant coronary stenosis.
Figure 1.
Left Flank Skin Lesion
Noted on presentation, confirmed to be pyoderma gangrenosum.
Past Medical History
She had no significant past medical history.
Differential Diagnosis
The differential diagnosis included infection, inflammatory conditions such as lupus, IgG4 disease, sarcoidosis, cutaneous malignancy, vasculitides, or drug reactions.
Investigations
TTE showed trivial aortic regurgitation with an eccentric jet suggestive of an aortico–left ventricular tunnel (Figure 2). A computed tomographic angiogram showed severe narrowing of the left main coronary artery (LMCA) ostium and aortic root thickening suggesting aortitis (Figure 3). She was admitted to the cardiology service at our center for further evaluation. A coronary angiogram showed 70% narrowing of the LMCA ostium (Figure 4, Video 1) with otherwise normal coronary arteries. Treadmill stress testing demonstrated 2- to 3-mm upsloping ST-segment depression in the inferolateral leads at 14 minutes of exercise. She was asymptomatic at maximal heart rate. A magnetic resonance angiogram (MRA) showed circumferential wall thickening, fibrosis, and edema of the thoracic and abdominal aorta, left common carotid, left renal, and superior mesenteric artery (Figure 5). Her sedimentation rate was 23 mm/h (reference: <25), and serum C-reactive protein was elevated at 1.6 mg/dL (reference: <1.0). Analysis of a punch biopsy specimen from her thigh lesion showed reticular dermal fibrosis and mild perivascular inflammation diagnosed as pyoderma gangrenosum.
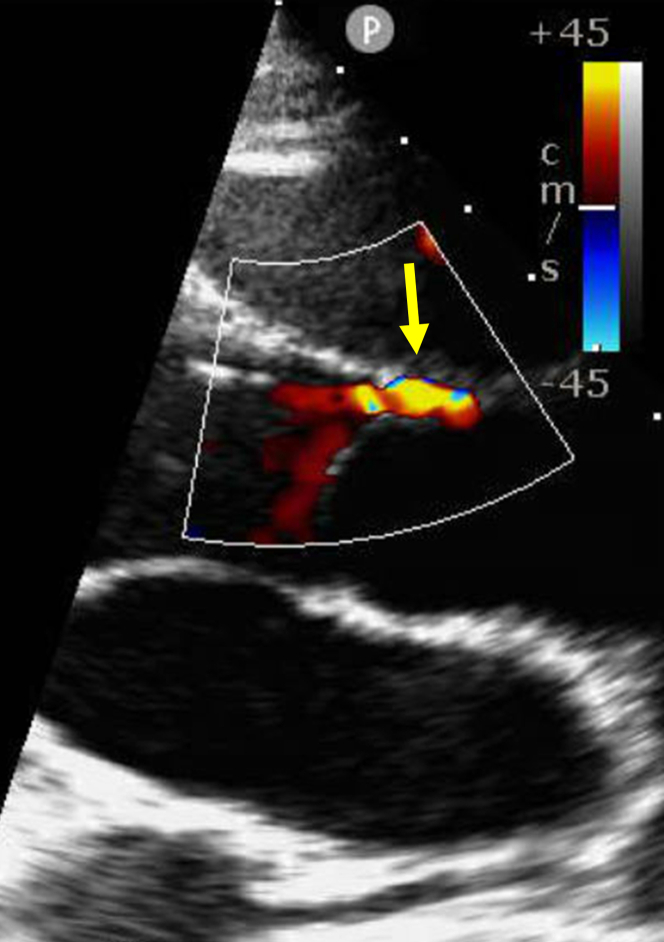
Figure 2.
Transthoracic Echo Parasternal View of the Aortic Valve Mid-Diastole
Yellow arrow shows an eccentric jet of aortic regurgitation suggestive of aorto–left ventricular tunnel.
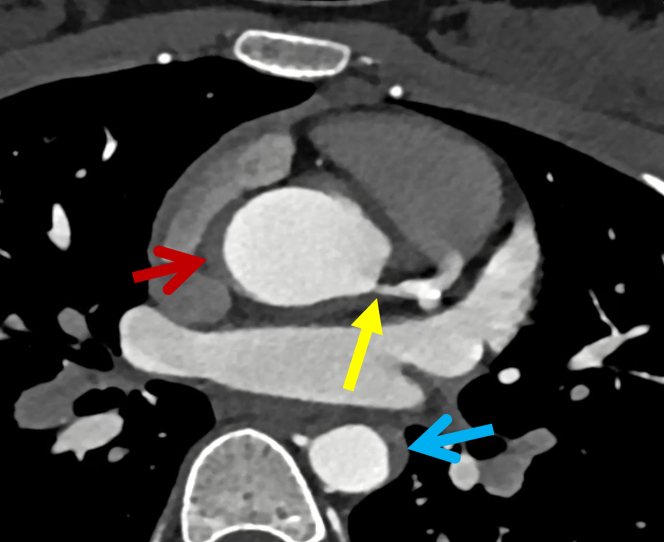
Figure 3.
Cardiac Computed Tomographic Angiogram
Axial view showing stenosis of the left main coronary artery (yellow arrow), wall thickening in the aortic root (red arrow), and descending aorta (blue arrow).
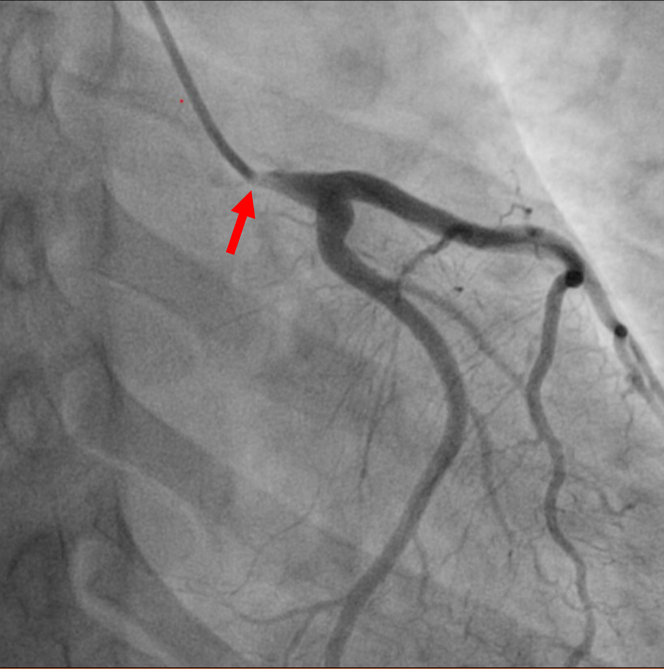
Figure 4.
Coronary Angiogram
View shows 70% narrowing at the ostium of the left main coronary artery (red arrow).
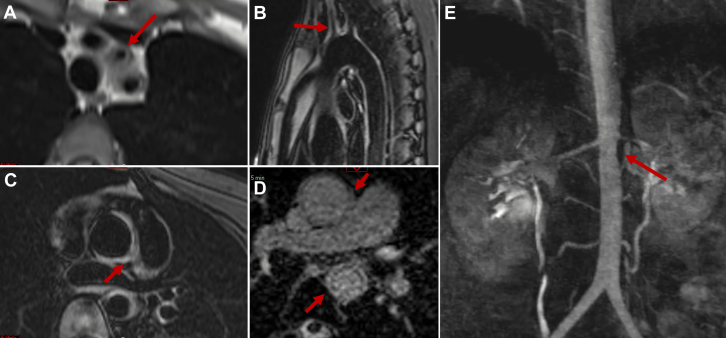
Figure 5.
Magnetic Resonance Angiography
Dark blood images show (A) diffuse narrowing of the proximal left coronary artery, (B) edema in the wall of the proximal ascending and descending aorta, (C) edema in the aortic root and left main coronary artery ostium, (D) gadolinium enhancement in the ascending and descending aorta and peri-aortic tissue, and (E) narrowing of the juxtarenal aorta and left renal artery.
Management
The patient received a diagnosis of Takayasu arteritis and pyoderma gangrenosum. After a multidisciplinary review, coronary artery bypass grafting (CABG) was recommended after a short course of immune modulating therapy to avoid grafting during the acute inflammatory stage. She was treated with aspirin, clopidogrel, metoprolol succinate, and 3 days of high dose methylprednisolone and was discharged with a regimen of weekly methotrexate, daily prednisone, dual antiplatelet therapy (DAPT), and metoprolol with strict restrictions on competitive sports. She tapered off prednisone during 5 months and transitioned to infliximab with an increased methotrexate dose to treat arteritis and pyoderma. With therapy, her pyoderma lesion resolved, and an interval MRA demonstrated stable coronary stenosis. She was subsequently seen at another center, was transitioned to weekly tocilizumab, and underwent percutaneous coronary intervention (PCI) 8 months after initial presentation. Two overlapping drug-eluting stents were placed in the LMCA with the proximal stent projecting into the aortic lumen. She was discharged with DAPT for 6 months and cleared for competitive play following normal stress test results at the other institution.
One month after discontinuation of DAPT, she experienced chest pain following a sports match and subsequently experienced cardiac arrest. Emergency medical services administered defibrillation at the scene. She was transferred to our center with an ongoing LUCAS device (Stryker Medical) providing cardiopulmonary resuscitation in asystole. Following the return of spontaneous circulation, she was emergently administered veno-arterial extracorporeal membrane oxygenation. Coronary angiography showed an ostial occlusion of the LMCA stent (Video 2) which was opened with balloon angioplasty; atrial septostomy was also performed. She was admitted to the intensive care unit for targeted temperature management, norepinephrine and epinephrine infusions, and continuous renal replacement therapy. TTE showed left ventricular ejection fraction <10%. An Impella 5.5 (Abiomed) was placed by cardiac surgery. On day 4, she had an intact mental status and spontaneous movement of the upper extremities, but her lower extremities were flaccid and insensate. A neurology evaluation suspected spinal cord ischemia causing paraplegia, however, diagnostic magnetic resonance imaging was not performed because of the patient’s critical illness. On day 7, she underwent decannulation from extracorporeal membrane oxygenation. A myocardial viability study showed extensive hibernating myocardium in the anterior, septal, and lateral walls. On day 21, she underwent CABG with left internal mammary artery grafting of the left anterior descending artery, saphenous vein grafting to an obtuse marginal artery, and resection of the coronary stent projecting into the aortic lumen.
Discussion
Takayasu arteritis is a vasculitis of the aorta and its branches. Progressive inflammation of the vessel wall leads to thickening, fibrosis, and stenosis.1 Occasionally, it is associated with pyoderma gangrenosum.2 In 1990, the American College of Rheumatology published 6 diagnostic criteria including age at onset, presence of claudication, decreased brachial artery pulses, upper extremity blood pressure discrepancies, presence of bruits, and angiographic abnormalities.3 The diagnosis in our patient was challenging because she was largely asymptomatic and presented at a young age.
This case report illustrates the youngest presentation of Takayasu arteritis with concurrent pyoderma gangrenosum and coronary involvement described in the literature. There are no consensus guidelines on the management of Takayasu arteritis; individual patient factors guide treatment. Our patient was at high risk for sudden cardiac death given her severe LMCA stenosis. Her family opted for PCI over CABG.
Data are limited on the long-term outcomes of PCI versus CABG in Takayasu arteritis with coronary involvement. Two retrospective cohort studies demonstrated statistically significant higher rates of restenosis4 and of major adverse cardiac events5 with PCI, suggesting that CABG is the ideal management. However, subgroup analysis in another study showed comparable outcomes between PCI and CABG if there was no active inflammation.6 Coronary artery involvement consists mostly of stenosis or occlusion of the coronary ostia, as in our patient.7 PCI has led to in-stent restenosis and higher rates of revascularization versus CABG during active inflammation.8 In a similar case with involvement of the LMCA ostium, a patient who had undergone PCI with a cobalt-chromium PICO stent (AMG) to the LMCA required multiple repeated revascularizations and eventually experienced an anterior ST-elevation myocardial infarction requiring emergent CABG.9 The underlying mechanism of inflammation and vascular stenosis differs in Takayasu arteritis versus atherosclerosis, which may explain why outcomes are worse with PCI. In our patient, projection of the coronary stent into the aortic root may have created a prothrombotic nidus. She experienced in-stent restenosis 1 month after discontinuing DAPT, which suggests that longer-term therapy may have been beneficial.
Follow-Up
After CABG, TTE showed persistent left ventricular ejection fraction <20%, and a HeartMate 3 left ventricular assist device was implanted (Abbott Cardiovascular). At this writing, she remains paraplegic. Diagnostic magnetic resonance imaging is not possible because of incompatibility with her Heartmate device. She was discharged on day 66 and is undergoing intensive rehabilitation.
Conclusions
Takayasu arteritis can present with pyoderma gangrenosum in adolescents without obvious cardiac symptoms despite significant coronary artery stenosis. With coronary involvement, CABG is preferred because PCI risks in-stent restenosis with potentially fatal outcomes.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Coronary Angiography
Angiogram demonstrating ostial left main coronary artery stenosis.
Aortic Root Injection
Angiogram demonstrating ostial occlusion of left main coronary artery stent.
References
- 1.Johnston S.L., Lock R.J., Gompels M.M. Takayasu arteritis: a review. J Clin Pathol. 2002;55:481–486. doi: 10.1136/jcp.55.7.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhowmick K., Roongta R., Dey S., et al. Refractory Takayasu arteritis with recurrent pyoderma gangrenosum: a therapeutic challenge with case-based review. Clin Rheumatol. 2023;42:1469–1477. doi: 10.1007/s10067-023-06506-x. [DOI] [PubMed] [Google Scholar]
- 3.Arend W.P., Michel B.A., Bloch D.A., et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990;33:1129–1134. doi: 10.1002/art.1780330811. [DOI] [PubMed] [Google Scholar]
- 4.Wang H., Zhang Y., Shen Z., Fang L., Liu Z., Zhang S. Comparing the effects of different management strategies on long-term outcomes for significant coronary stenosis in patients with Takayasu arteritis. Int J Cardiol. 2020;306:1–7. doi: 10.1016/j.ijcard.2020.02.051. [DOI] [PubMed] [Google Scholar]
- 5.Yang Y., Tian T., Yang K., et al. Outcomes of percutaneous coronary intervention and coronary artery bypass grafting in patients with Takayasu arteritis. Int J Cardiol. 2017;241:64–69. doi: 10.1016/j.ijcard.2017.02.041. [DOI] [PubMed] [Google Scholar]
- 6.Wang X., Dang A., Lv N., et al. Long-term outcomes of coronary artery bypass grafting versus percutaneous coronary intervention for Takayasu arteritis patients with coronary artery involvement. Semin Arthritis Rheum. 2017;47:247–252. doi: 10.1016/j.semarthrit.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Sun T., Zhang H., Ma W., et al. Coronary artery involvement in Takayasu arteritis in 45 Chinese patients. J Rheumatol. 2013;40:493–497. doi: 10.3899/jrheum.120813. [DOI] [PubMed] [Google Scholar]
- 8.Cobilinschi C.O., Gradinaru E., Saulescu I., et al. Refractory Takayasu's arteritis with severe coronary involvement: case report and literature review. J Clin Med. 2023;12(13):4394. doi: 10.3390/jcm12134394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee H.K., Namgung J., Choi W.-H., et al. Stenting of the left main coronary artery in a patient with Takayasu's arteritis. Korean Circ J. 2011;41:34–37. doi: 10.4070/kcj.2011.41.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronary Angiography
Angiogram demonstrating ostial left main coronary artery stenosis.
Aortic Root Injection
Angiogram demonstrating ostial occlusion of left main coronary artery stent.