Abstract
Spontaneous coronary artery dissection (SCAD) is an increasingly recognized cause of acute myocardial infarction. We examine 4 atypical presentations of SCAD. These cases highlight treatment course and outcomes for patients with SCAD who do not present with acute coronary syndrome.
Key Words: acute coronary syndrome, dissection, fibromuscular dysplasia, myocardial infarction
Graphical Abstract

Spontaneous coronary artery dissection (SCAD) is an emerging cause of myocardial infarction, most often affecting middle-aged women. SCAD is usually defined as causing acute coronary syndrome (ACS), including unstable angina, ST-segment elevation myocardial infarction (STEMI), non–ST-segment elevation myocardial infarction (NSTEMI), and/or cardiac arrest.1 Potentiating the already challenging diagnosis and management of SCAD, atypical presentations pose risks to patients and challenge those clinicians who care for them. Here we describe 4 patients with SCAD who presented with angina or ischemia without myocardial injury.
Take-Home Messages
-
•
A rare subset of patients with SCAD presents with angina or ischemia but without myocardial injury.
-
•
If SCAD is suspected, invasive coronary angiography with or without intracoronary imaging is the gold standard technique to confirm the diagnosis, thereby guiding treatment.
Case 1
A 61-year-old woman with a history of hypertension and hyperlipidemia presented to her internist with 4 months of exertional chest pain and dyspnea. Her resting blood pressure was elevated (152/90 mm Hg), and her heart rate was 59 beats/min. The electrocardiogram was normal. On stress echocardiogram, she exercised for <4 minutes and stopped because of dyspnea. Echocardiography at peak stress showed anteroapical hypokinesis consistent with mid-distal left anterior descending (LAD) artery ischemia. She was referred for cardiology consultation.
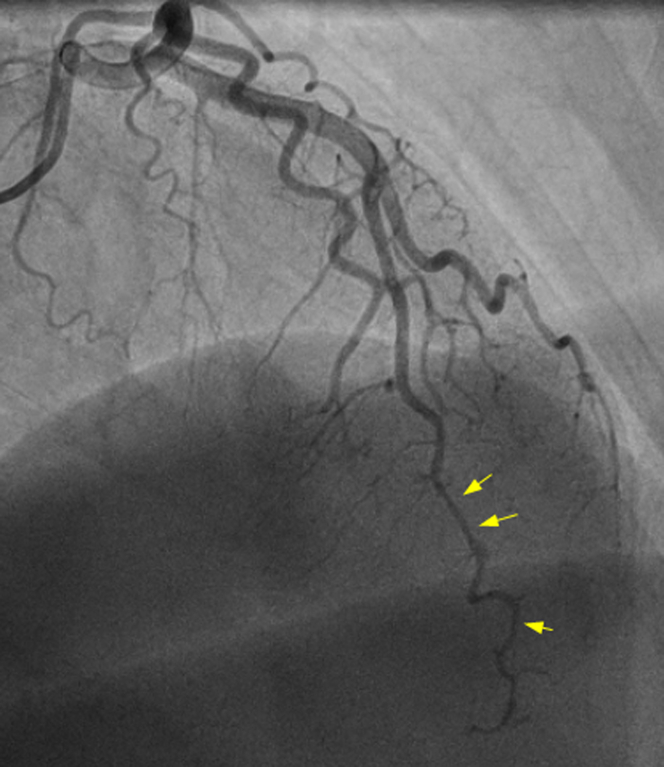
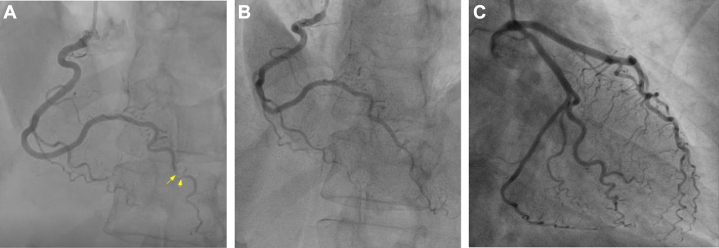
However, worsening chest pain and dyspnea prompted her to seek evaluation at the emergency department (ED). Symptoms were partially relieved with aspirin and nitroglycerin. Her blood pressure was mildly elevated (138/82 mm Hg), and her heart rate was 60 beats/min. Blood testing revealed normal serial troponin levels. Coronary angiography demonstrated distal LAD artery dissection with TIMI flow grade 2 to 3 (Figure 1, Video 1).
Figure 1.
Spontaneous Coronary Artery Dissection of the Left Anterior Descending Artery
Coronary angiography showed left anterior descending artery spontaneous coronary artery dissection (arrows).
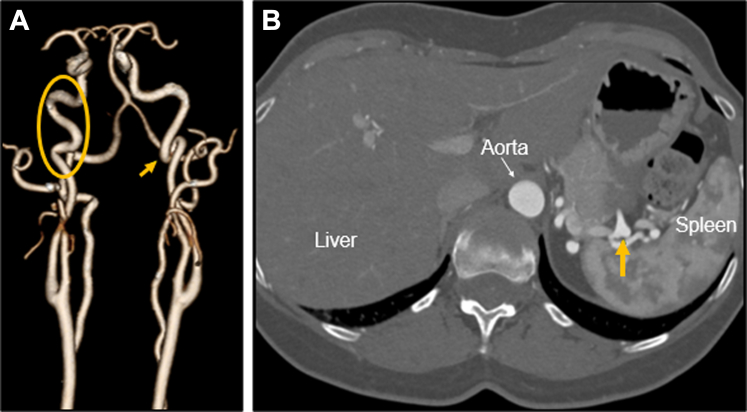
The patient was managed conservatively. Within 1 week of dismissal, she returned to the ED with dizziness and nausea. For those symptoms, magnetic resonance angiography did not show acute stroke or cervical arterial dissection. Troponin levels and the echocardiogram were normal. Subsequent comprehensive computed tomography angiography (CTA) showed an “S”-shaped curvature of both distal internal carotid arteries and a splenic artery aneurysm (Figures 2A and 2B). Repeat coronary angiography performed at 4 months for persistent exertional dyspnea showed improved appearance of the dissection.
Figure 2.
Arteriopathy
Comprehensive computed tomography angiography showed (A) “S”-shaped (oval) and coiled (arrow) curvature of the distal internal carotid arteries and (B) splenic artery aneurysm (arrow).
Case 2
A 57-year-old healthy woman presented to the ED with chest pain and dyspnea following vigorous exercise lasting 15 to 20 minutes from exercise cessation. She had attributed 2 previous similar episodes to anemia. Her resting blood pressure was elevated (161/118 mm Hg), and her heart rate was 62 beats/min.
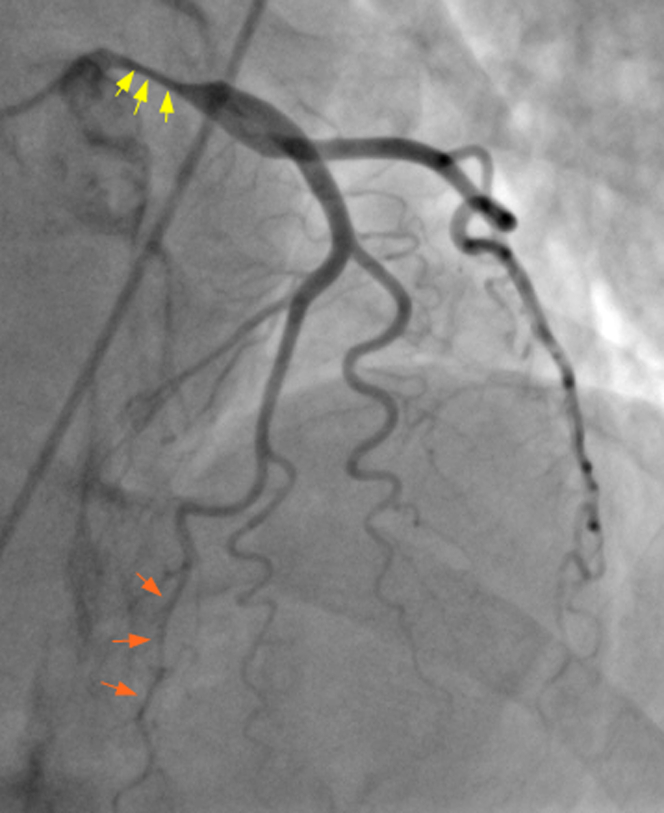
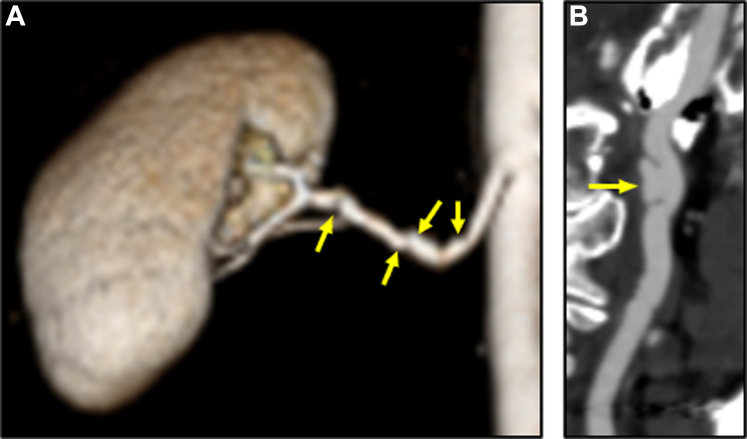
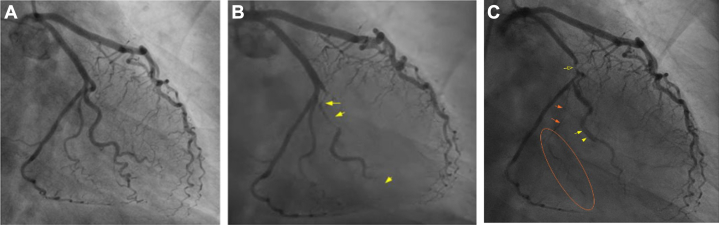
The electrocardiogram demonstrated T-wave inversions in leads V5 and V6. Her serial troponin levels increased slightly but remained within the normal laboratory limits (initial, <0.010 ng/mL; secondary, 0.015 ng/mL; final, 0.023 ng/mL [laboratory normal reference, <0.030 ng/mL]). The patient was referred for a stress echocardiogram by the ED clinician because of the “classic angina story.” The echocardiogram demonstrated a drop in ejection fraction from ∼60% at rest to ∼40% during peak stress, with regional wall motion abnormalities (RWMAs) in the territory of the LAD artery. Coronary angiography showed severe left main artery dissection with TIMI flow grade 3, likely LAD artery SCAD, and coronary artery tortuosity (Figures 3 and 4, Video 2). She was sent for emergency coronary artery bypass grafting, including a left internal mammary artery–to–LAD artery and saphenous vein graft to the obtuse marginal (OM) coronary artery. Comprehensive CTA revealed fibromuscular dysplasia (FMD) in the renal, carotid, and vertebral arteries and bilateral internal carotid pseudoaneurysms (Figures 5A and 5B). She participated in cardiac rehabilitation and experienced persistent exertional dyspnea. Three months following surgery, echocardiography showed a left ventricular ejection fraction of 59% without RWMA.
Figure 3.
Spontaneous Coronary Artery Dissection of the Left Main Artery
Coronary angiography showed left main spontaneous coronary artery dissection (yellow arrows) and likely spontaneous coronary artery dissection hematoma of the left anterior descending artery (orange arrows).
Figure 4.
Interval Worsening of the Left Main Spontaneous Coronary Artery Dissection
Coronary angiography showed worsening of the left main spontaneous coronary artery dissection (circle).
Figure 5.
Renal Artery Fibromuscular Dysplasia and Carotid Arteriopathy
Comprehensive computed tomography angiography showed (A) fibromuscular dysplasia of the renal artery (arrows) and (B) right internal carotid arteriopathy (arrow).
Case 3
A 55-year-old woman with a history of hyperlipidemia developed exertional chest pain during light exercise. She reported this to her physician and underwent stress echocardiography, which showed stress-induced hypokinesis of the septal wall. Coronary angiography showed stenosis of the right posterior descending (RPDA) and coronary artery tortuosity (Figures 6A to 6C, Video 3). The stenosis was thought to be atherosclerosis and was treated with a single drug-eluting stent (Figures 6A to 6C). She recovered without incident; however, on retrospective review of her images, the stenosis was likely RPDA SCAD.
Figure 6.
Spontaneous Coronary Artery Dissection of the Right Posterior Descending Artery
Coronary angiography showed (A) right posterior descending artery spontaneous coronary artery dissection (arrows), which was treated by (B) percutaneous coronary intervention with a single drug-eluting stent, and (C) coronary tortuosity.
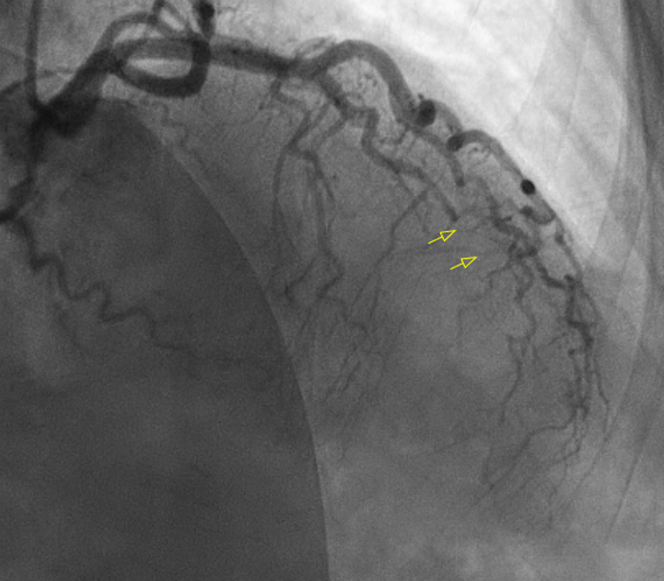
Four years later, she developed acute chest discomfort with elevated troponin levels. She underwent coronary angiography for NSTEMI, which showed a dissection of the first OM (OM1) artery (Figures 7A to 7C, Video 4). Percutaneous intervention was attempted but unsuccessful. Nine days later, she experienced recurrent chest pain and unstable angina with progression of the dissection into the second OM and left circumflex arteries on repeat coronary angiography (Figures 7A to 7C, Video 5). This was treated conservatively. Six months following her second dissection, she presented with acute chest pain, elevated troponin levels, and STEMI. Coronary angiography showed LAD artery SCAD occlusion extending into the first diagonal artery (Figure 8). Her previous dissections had almost entirely healed. She was monitored and treated conservatively. Comprehensive CTA demonstrated FMD in the iliac, renal, and carotid arteries. She has since recovered without recurrent chest pain for the past 5 years.
Figure 7.
Spontaneous Coronary Artery Dissection of the First Obtuse Marginal Coronary Artery With Progression
(A) Previously normal first obtuse marginal coronary artery. (B) Subsequent spontaneous coronary artery dissection of the first obtuse marginal (yellow arrows). (C) Progression of the spontaneous coronary artery dissection including the left circumflex (yellow open arrow), first obtuse marginal (yellow arrowheads), and second obtuse marginal artery (orange oval and arrows).
Figure 8.
Spontaneous Coronary Artery Dissection of the Left Anterior Descending Artery
Coronary angiography showed left anterior descending artery spontaneous coronary artery dissection (arrows), which extended into the first diagonal artery.
Case 4
A 67-year-old man with a history of hyperlipidemia presented to the ED with intermittent chest pain for 1 week; the patient associated the onset of symptoms with a recent iron transfusion for anemia. His resting blood pressure was elevated (153/81 mm Hg), and his heart rate was 64 beats/min. The initial electrocardiogram showed no acute changes, and 3 serial troponin levels were normal. He was discharged with a stress echocardiogram to be completed within 48 hours.
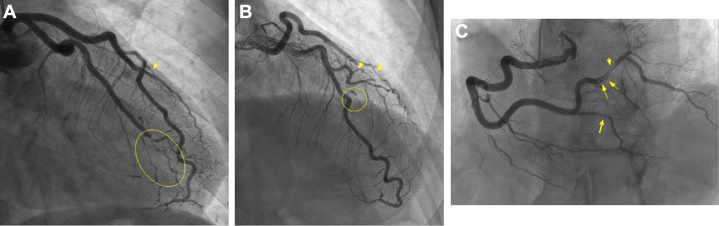
At peak exercise, the patient had horizontal ST-segment depressions in leads V3 and V4 with concurrent chest pain, but echocardiography showed no stress-induced RWMA. Following the stress study, he had persistent chest pain for which his physician recommended that he go to the ED. On arrival, his troponin levels were elevated. Coronary angiography showed SCAD of the OM1, third diagonal, and posterolateral coronary arteries (Figures 9A to 9C, Video 6, Video 7, Video 8) and coronary artery tortuosity. He was treated conservatively. CTA showed FMD of the right renal artery and bilateral carotid arteries (Figure 10). Additionally, a fusiform aneurysm with focal dissection of the celiac artery was noted. Over 3 months of follow-up, his chest pain gradually diminished.
Figure 9.
Multivessel Spontaneous Coronary Artery Dissection
(A to C) Coronary angiography showed spontaneous coronary artery dissection of the first obtuse marginal artery and branches (A, oval; B, arrows), diagonal artery (A, arrow; B, circle), the right posterior descending artery, and the right posterolateral artery (C, arrows).
Figure 10.
Carotid Artery Fibromuscular Dysplasia
Comprehensive computed tomography angiography showed fibromuscular dysplasia of the bilateral carotid arteries (arrow, arrowhead).
Discussion
SCAD is predominantly diagnosed in the context of ACS,1 and it is recognized as a potential cause of myocardial infarction with nonobstructive coronary arteries. The patients in this series exemplify SCAD as a cause of ischemia or angina without myocardial injury, likely from an evolving coronary hematoma or dissection. These cases also highlight an uncommon presentation of SCAD in the absence of ACS, which may contribute to delayed or missed diagnosis. Moreover, the absence of traditional cardiovascular risk factors, younger age, female sex, and symptoms attributed to nonischemic causes may lessen the likelihood of timely diagnosis and treatment.
Symptoms experienced by some patients align with the ischemia/angina with nonobstructive coronary arteries classification, consistent with the hypothesis that the cause of pain is more complex than simply obstruction of epicardial coronary blood flow. Rather, other mechanisms such as coronary vasospasm or endothelial and microvascular dysfunction may account for persistent symptoms in some patients.
Invasive coronary angiography is the gold standard diagnostic study to identify SCAD but is not an initial diagnostic test for patients presenting solely with chest pain.2 For instance, all patients underwent coronary angiography only after showing evidence of ischemia on noninvasive stress testing. For patient 2, the timely SCAD diagnosis facilitated critical surgical intervention. Conservative management with medications and monitoring remains a common treatment strategy, especially because SCAD vessels often heal with time. There are minimal data on which medications are most effective, although a small observational study suggested the benefit of beta-blockers.3 Additionally, another observational study has implied fewer adverse outcomes during the first year after SCAD among those patients treated with single vs dual antiplatelet therapy.4
Potentially, some coronary artery dissections are never detected because anginal symptoms and ischemia may not always lead to coronary imaging in the absence of ACS.2 Because dissections frequently heal,5 it is conceivable that some patients may have complete clinical resolution of their dissection without a diagnosis being made, thus affecting our understanding of the incidence, prevalence, and natural history of SCAD.
Conclusions
These cases highlight the importance of characterizing SCAD as a cause of angina without myocardial injury. Further awareness of SCAD presentation will facilitate proper treatment and counseling, which differ for patients with SCAD compared with other causes of ACS or angina. Invasive coronary angiography should be used when there is a suspicion of SCAD, for proper diagnosis and management.
Funding Support and Author Disclosures
Dr Tweet has received support from National Heart, Lung, and Blood Institute award 1K23HL155506. The authors also acknowledge support from SCAD Research, Inc.
Acknowledgments
The authors thank the patients in this case series for their permission and participation in SCAD research.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
SCAD of the LAD Artery
Coronary angiography showed a type 2 left anterior descending (LAD) spontaneous coronary artery dissection (SCAD) hematoma.
SCAD of the LM Artery
Coronary angiography showed left main (LM) spontaneous coronary artery dissection (SCAD) and left anterior descending artery spontaneous coronary artery dissection.
SCAD of the RPDA
Coronary angiography showed right posterior descending artery (RPDA) spontaneous coronary artery dissection (SCAD) before percutaneous coronary intervention with a single drug-eluting stent.
SCAD of the OM1 Coronary Artery
Coronary angiography showed first obtuse marginal (OM1) spontaneous coronary artery dissection (SCAD).
Interval Worsening of (SCAD
Coronary angiography showed spontaneous coronary artery dissection (SCAD) progression including the first obtuse marginal and extending into the left circumflex and second obtuse marginal arteries.
SCAD of the OM1 and Diagonal Arteries
Coronary angiography showed spontaneous coronary artery dissection (SCAD) of the first obtuse marginal (OM1) and diagonal arteries.
SCAD of the OM1 and Diagonal Arteries
Coronary angiography showed spontaneous coronary artery dissection (SCAD) of the first obtuse marginal (OM1) and diagonal arteries.
SCAD of the Right Posterolateral and Posterior Descending Arteries
Coronary angiography showed spontaneous coronary artery dissection (SCAD) of the right posterolateral and right posterior descending arteries.
References
- 1.Hayes S.N., Tweet M.S., Adlam D., et al. spontaneous coronary artery dissection: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76:961–984. doi: 10.1016/j.jacc.2020.05.084. [DOI] [PubMed] [Google Scholar]
- 2.Writing Committee. Gulati M., Levy P.D., et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187–e285. doi: 10.1016/j.jacc.2021.07.053. [DOI] [PubMed] [Google Scholar]
- 3.Saw J., Humphries K., Aymong E., et al. Spontaneous coronary artery dissection: clinical outcomes and risk of recurrence. J Am Coll Cardiol. 2017;70:1148–1158. doi: 10.1016/j.jacc.2017.06.053. [DOI] [PubMed] [Google Scholar]
- 4.Cerrato E., Giacobbe F., Quadri G., et al. Antiplatelet therapy in patients with conservatively managed spontaneous coronary artery dissection from the multicentre DISCO registry. Eur Heart J. 2021;42:3161–3171. doi: 10.1093/eurheartj/ehab372. [DOI] [PubMed] [Google Scholar]
- 5.Hayes S.N., Kim E.S.H., Saw J., et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation. 2018;137:e523–e557. doi: 10.1161/CIR.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SCAD of the LAD Artery
Coronary angiography showed a type 2 left anterior descending (LAD) spontaneous coronary artery dissection (SCAD) hematoma.
SCAD of the LM Artery
Coronary angiography showed left main (LM) spontaneous coronary artery dissection (SCAD) and left anterior descending artery spontaneous coronary artery dissection.
SCAD of the RPDA
Coronary angiography showed right posterior descending artery (RPDA) spontaneous coronary artery dissection (SCAD) before percutaneous coronary intervention with a single drug-eluting stent.
SCAD of the OM1 Coronary Artery
Coronary angiography showed first obtuse marginal (OM1) spontaneous coronary artery dissection (SCAD).
Interval Worsening of (SCAD
Coronary angiography showed spontaneous coronary artery dissection (SCAD) progression including the first obtuse marginal and extending into the left circumflex and second obtuse marginal arteries.
SCAD of the OM1 and Diagonal Arteries
Coronary angiography showed spontaneous coronary artery dissection (SCAD) of the first obtuse marginal (OM1) and diagonal arteries.
SCAD of the OM1 and Diagonal Arteries
Coronary angiography showed spontaneous coronary artery dissection (SCAD) of the first obtuse marginal (OM1) and diagonal arteries.
SCAD of the Right Posterolateral and Posterior Descending Arteries
Coronary angiography showed spontaneous coronary artery dissection (SCAD) of the right posterolateral and right posterior descending arteries.