Abstract
During the past century, there have been major developments in the medical and surgical treatment of cardiovascular disease (CVD). These advancements have resulted in more people surviving initial events and having reduced length of stay in hospital; consequently, there is an increasing number of people in need of ongoing and lifelong cardiovascular risk management. The physical and emotional effects of living with CVD are ongoing with broad challenges ranging from the individual to system level. However, post-discharge care of people with coronary disease continues to follow a 50-year-old cardiac rehabilitation model which focuses on the sub-acute phase and is of a finite in duration. The aim of this paper is to consider the concept of supporting survivors to live well with CVD rather than ‘rehabilitating’ them and propose factors for consideration in reframing secondary prevention towards optimizing cardiovascular health. We discuss deeply-held potential considerations and challenges associated with the concept of supporting survivors achieve optimal cardiovascular health and live well with CVD rather than ‘rehabilitating’ them. We propose the concept of 5 x P’s for reframing traditional cardiac rehabilitation towards the concept of cardiovascular health for survivors beyond ‘rehabilitation’. These include the need for personalization, processes, patient-centered care, parlance, and partnership. Taken together, consideration of challenges at the systems and population level will ultimately improve engagement with secondary prevention as well as outcomes for all people who need it.
Subject terms: Cardiology, Health care
Introduction
Cardiovascular disease (CVD), including coronary heart disease (CHD) and stroke, relentlessly continues to be the greatest cause of mortality and disease burden across the globe1. Based on 2019 data, approximately one-third of global fatalities were attributable to CVD, which equates to almost 18 million deaths1. Importantly, among survivors of an acute coronary event, one in four experience at least one emergency hospital admission for CVD within 2 years2. Moreover, evidence recently showed that leading CVD risk factors significantly increased the risk of poor outcomes in those infected with coronavirus disease 2019 (COVID-19)3. In this context, the global CVD crisis that has persisted for decades has decreased human resiliency in the face of other health challenges, such as viral pandemics.
During the past century, there have been major developments in CVD management in terms of how a diagnosis is made, how arteries are revascularized, particularly in coronary vasculature, and the breadth and effectiveness of available medications for people with CVD4. These advancements have resulted in more people surviving initial events and having reduced length of stay in hospital3; consequently, there is an increasing number of people in need of ongoing and lifelong cardiovascular risk management5. As such, international groups and organizations have identified improved secondary prevention as an global priority6,7. In addition, the impact of receiving a diagnosis of CVD or surviving a heart attack is traumatic and life-changing8. The physical and emotional effects of living with CVD9 are ongoing with broad challenges ranging from the individual to system level10.
Global health systems are facing an escalating challenge. The combination of an aging population and decreased population resiliency due to unhealthy lifestyle behaviors coupled with medical advancements means more people are living longer with heart disease and its sequelae11. Increasing numbers of survivors are in need of ongoing care and support to make sustained change, minimize disability, and reduce risk of recurrent events. The concept of survivorship, where the focus is on promoting health and wellbeing beyond diagnosis and treatment, is well recognized in cancer care and research12. In contrast, post-discharge care of coronary disease continues to follow a 50-year-old cardiac rehabilitation model which focuses on the sub-acute phase, is finite in duration5,13 and lacks systems for improving the model based on consumer input14. The aim of this paper is to consider the concept of supporting survivors to live well with CVD rather than ‘rehabilitating’ them and propose factors for consideration in reframing secondary prevention towards optimizing cardiovascular health.
Cardiac rehabilitation
Cardiac rehabilitation is a comprehensive secondary prevention model of care which is proven to mitigate the health and economic burden of CVD15,16. Cardiac rehabilitation programs deliver individualized, inter-professional care, including: clinical assessment, structured exercise training, patient and family education, cardiovascular risk factor management (e.g., smoking cessation advice where indicated and optimization of medications to control lipids and blood pressure) and psychosocial counseling17. The traditional model of cardiac rehabilitation is internationally accepted as comprising several sequential phases17–19. Phase 1 typically focuses on inpatient mobilization and introductory information but in recent years has been pared back to early discharge and changes in medical care. Phase 2 has traditionally been the primary focus – delivered by outpatient hospital-based programs run in groups attending for approximately six to 12 weeks18. Phase 3 is known as a maintenance phase of four to six months duration where people living with CVD continue their exercise and risk factor modification routine while returning to their regular life and work20. Programs vary somewhat in terms of dose and comprehensiveness21, likely impacted by several factors, including funding models within a given system22.
A large body of scientific research has highlighted the benefits of cardiac rehabilitation for those who attend23–26. These benefits include reduced risk of subsequent myocardial infarction, a modest reduction in all-cause mortality, and a considerable reduction in all-cause hospital admissions along with associated healthcare costs, increased functional/exercise capacity, and improved quality of life up to 12 months23–26. Evidence has highlighted the importance of comprehensive programs that manage multiple risk factors are most effective in terms of reducing all-cause mortality26.
Unfortunately, while major international guidelines strongly recommend cardiac rehabilitation for all with CVD27–31, research consistently shows that survivors have unacceptably poor rates of referral (30% of eligible)32, attendance (9% of eligible) and completion (<5% of all eligible)33. Further, the use of evidence-based medications and lifestyle improvements typically decline within six months34,35 of an acute event and are rarely sustained36,37. Contributing issues include that, historically consumers have not been involved in the reporting and design of cardiac rehabilitation programs. Health systems continue to be under-resourced leading to cardiac rehabilitation programs falling between the cracks of acute and primary care. Research in this area has also been under-funded and lacking national and international unity38. Global groups such as the International Council of Cardiovascular Prevention and Rehabilitation (ICCPR; www.globalcardiacrehab.com) and SOLVE-CHD (www.solvechd.org.au/) are collaborating to inform the conversation through unity and capacity building, but the challenge is complex and requires an interdisciplinary solution38.
Understanding the historical context of cardiac rehabilitation
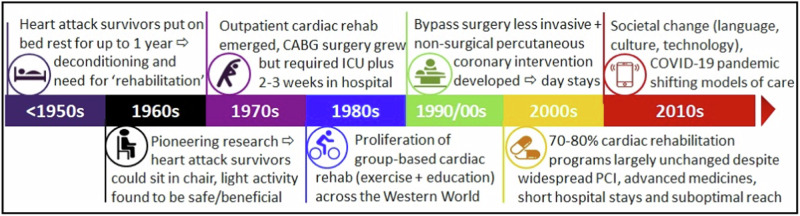
Exploring the origins of cardiac rehabilitation provides insight into why current programs are structured as they are and why programs have been slow to adapt to the evolving needs of patients living with CVD and societal expectations5. These changes include significant shifts in culture, language, and diversity, substantial advancements in the medical and surgical management of CVD, and the rapid expansion of technology availability and capability (Fig. 1)5. Exploring the beginnings of cardiac rehabilitation informs our understanding of why current programs are designed as they are and how this has failed to adapt with changed needs of societies5.
Fig. 1. Historical context underscores the need for reform5.
PCI, percutaneous coronary intervention.
Modern-day cardiac ‘rehabilitation’ was born at a time when bed rest and physical inactivity were recommended for people after a heart attack39. In the mid and late 20th century, survivors of heart attacks did require ‘rehabilitation’ - the timeline is detailed elsewhere but is represented schematically here in Fig. 15. To summarize, despite being designed more than 60 years ago40, the traditional model of cardiac rehabilitation is still followed by 70-80% of programs globally in today’s vastly different societal and medical contexts13,40. That is, cardiac rehabilitation largely continues to follow a ’one size fits all’ service-oriented model rather than a patient or survivor centered approach. Historically, programs have also been exercise-focussed with more contemporary literature highlighting the importance of comprehensive prevention with emphasis on behavioral approaches to address lifestyle as well as other pharmacotherapy for addressing clinical risk factors26. Taken together, programs lack flexibility and choice for people with CVD and hence their needs and preferences are not always paramount. Historical underpinnings are ultimately contributing to the sub-optimal referral, reach, participation and completion reflecting the need to reimagine cardiac rehabilitation service delivery in the 21st century.
The numbers do not add up
Globalization (including migration) has resulted in economic development along with greater need to manage equity and diversity both within and between countries. For example, individuals who do not speak the language of the country in which they live, those who live in rural and remote geographical areas, those with socioeconomic disadvantage, people from culturally diverse backgrounds and women remain under-represented in cardiac rehabilitation10. International guidelines recommend all eligible people should be offered and participate in a cardiac rehabilitation program27–31. However, the numbers do not add up.
Based on existing resources, if all eligible people referred to traditional cardiac rehabilitation took up the opportunity to participate, health systems would not be able to meet the demand. For example, recent data from Europe suggests that cardiac rehabilitation programs lack around 3.5 million places annually40. In the United States of America, the Million Hearts initiative has set a national target of increasing cardiac rehabilitation participation from 20% to 70%41, which based on current case numbers would roughly represent an additional 1.7 million participants annually.
Although costs vary within and between countries, it is globally estimated a traditional program costs $US945 per person (calculated based on purchasing power parity)22. To meet the above stated targets, the increased participation in Europe (3.5 million participants x $US945) and the USA (1.7 million participants x $US945) would conservatively cost an estimated $US3.3 billion (~€3.02 billion) and $US1.6 billion (approximately €1.47 billion) respectively to implement. Although these costs are likely to be an underestimate in contemporary healthcare they nevertheless highlight the cost of delivering traditional cardiac rehabilitation to all who are eligible around the world. Despite documented cost benefits of cardiac rehabilitation in its traditional form42, it is unlikely international governments will have the funding to pay for such costs upfront despite hope of a return on investment in the following 5-10 years. Robust long-term research also lacking in this area.
When considered in this way, the upfront funding requirements, of traditional cardiac rehabilitation, for societies and governments are unrealistic within contemporary health budgets being highly unlikely to be in a position to deliver scale-up. Furthermore, these financial challenges are significantly greater in low and middle-income countries. Ultimately, it appears unfeasible to offer traditional group-based and in-person cardiac rehabilitation at scale to all people who are eligible. Financial constraints also highlight the need for modernization, greater flexibility, and potential expansion of innovative and virtual models for supporting CVD survivors in managing their life-long cardiovascular risk. Consideration of the concept of ‘proportionate universalism’ could be considered relevant where consideration of how systems could balance care among and between people who need it most also help address equity but also balance cost and availability43,44.
Shifting the framing from ‘rehabilitation’ to ‘cardiovascular health’
The ‘cancer’ care and research community has embraced the importance of survivorship care with the aim of supporting people with cancer to participate fully in life in a meaningful way for the long term45. This need has arisen due to increasing cancer incidence rates (mainly resulting from an aging population and unhealthy lifestyle behaviors), earlier detection, and improved treatments and ongoing cardiovascular health46. Survivorship care in this area has a focus on strengths, a sense of vitality, living well and living a full life47. The same phenomena are occurring in relation to the number of people living with CVD. However, post-discharge care for people with CVD continues to focus on the above outlined time-limited ‘rehabilitation’ model5,40. Moreover, risk factors and secondary prevention recommendations to prevent recurrence are common to cancer and CVD48,49.
Survivorship care for people post-cancer has a focus on living well and promotes physical activity, a healthy diet and weight management, and recommended immunizations for survivors via care coordination that ensures all needs are addressed45. Associated strategies include appropriate screening, evaluation/assessment and treatment of contributing factors, education and counseling along with appropriate referrals47. These concepts are remarkably similar to those proposed in the Secondary Prevention for All in Need (SPAN) framework previously published in relation to CVD50. In SPAN, it is proposed that all people with CVD receive an assessment, education and personalized risk factor management along with follow-up with flexibility in format and duration50. At the same time, there are increasing calls for flexibility via virtual options for CVD prevention to achieve the preventive quadrella of referral, reach, participation and completion5,7,10,51,52. With this in mind, we propose the concept of lifelong cardiovascular health rather than a period of ‘rehabilitation’.
Some of the challenges for optimizing and maintaining cardiovascular health among people with CVD include the need for longer term support and care rather than a time-limited traditional rehabilitation program. This is embedded in the language and terminology used ubiquitously in the field, namely “rehabilitation”. This terminology itself is problematic because it conflicts with the concept of ongoing cardiovascular health or survivorship. However, current terminology is heavily embedded around the world including with international and country-specific cardiac rehabilitation organizations, clinician expectations and healthcare funders52. To enhance cardiovascular health, programs should strive to be more responsive to personal needs and preference to optimize patient-centredness of care14,53. Research has repeatedly found, in cardiology and other areas of health, that patient-reported outcomes and experience are inextricably linked with mortality rates, clinical effectiveness and safety53–55. More systematic collection of data, including patient-reported measures, would enable capitalization on opportunities through data science to facilitate improved care by enabling the identification of gaps, benchmarking and opportunities for better health.
Five x P’s for consideration in reframing ‘cardiac rehabilitation’
Although, traditional cardiac rehabilitation remains beneficial for those who attend, improvements require greater continuity in care, flexibility, and consideration of financial feasibility at a population level. To work towards reframing, we suggest that consideration of the below five ‘P’s’ (1) personalization, (2) processes and systems, (3) patient-centered care, (4) parlance, and (5) partnership and unity (Box 1).
Box 1 Proposed 5 x P’s for reframing cardiac rehabilitation.
1. Personalization
Consideration of approaches that embed personalization and flexibility into service delivery. The use of more personalized and digital support programs offers an opportunity to absorb some of the increasing diversity and patient load. For example, varied settings and models such as community, home-based approaches, and hybrid approaches with personalized education and management support based on the need and preference of people living with CVD. This includes consideration of multimorbidity where care is focused on the ‘whole’ person rather than the disease itself. In particular, digital strategies can offer light-touch solutions that have the potential to extend reach of programs10 and support for people with CVD in the longer term in the most cost-effective way56.
2. Processes and systems
Enhancing and implementing processes and systems for capturing and using data would enable a connected health system with built-in quality improvement systems. Current cardiac rehabilitation programs frequently lack the infrastructure and systems that support the collection and use of data for potential quality improvement, with many programs still using paper-based record-keeping57. Expanding access to streamlined and electronic data collection would offer an opportunity to leverage programs improvements and reach and ultimately ensure better care is offered to more people. Such data could subsequently be used to ensure ongoing preventive care is comprehensive and reaches all those who can potentially benefit. Data would help improve care for those who are eligible and participate but also identify those people who are falling through the ‘cracks’.
3. Patient-centered
Ensuring care is provided in a way that benefits people who need it in the best way to help them access it and achieve optimal outcomes. Flexibility service delivery along with collection of patient-reported measures with consumer involvement in program redesign would potentially facilitate these improvements. Improving patient-centered care and enhancing involvement and input would enable improved services in terms of quality and meaningfulness and for expanded programs beyond the traditional length of time to provide more lifelong cardiovascular health and support14,50,53–55.
4. Parlance
Parlance where the language and terminology used in the field of cardiac rehabilitation presents challenges. Progressing challenging conversations about terminology from ‘rehabilitation’ to the concept of cardiovascular health and life-long preventive care5. On balance, although a period of ‘rehabilitation’ is beneficial for some people with CVD, a more life-long and multifaceted prevention approach is needed for all if we are to reduce the CVD burden at the population level. As has been previously recommended this could include a universal definition and classification of preventive ‘rehabilitation’52.
5. Partnership and unity
Striving for stronger partnership and global unity with the common goal of optimizing cardiovascular health. Partnerships include consumers, stakeholders, policy-makers, clinicians, researchers to name a few. In terms of global unity, the ICCPR are working to understand and identify evidence-practice gaps from a global perspective with a focus on low-resource settings40,58. By bringing together the global cardiac rehabilitation community, more unity and sharing of challenges as well as collaboration on strategic directions can be achieved.
Conclusion
In this paper, we share deeply held potential considerations and challenges associated with the concept of supporting survivors to achieve optimal cardiovascular health and live well with CVD rather than ‘rehabilitating’ them. We emphasize the importance of modernization and the escalating demands required to meet current and projected expanding needs within financial limits. Furthermore, highlighting the importance of contemporary models of cardiac rehabilitation are being developed to better align with other treatments, changing societies, and technological advancements. We propose the concept of 5 x P’s for reframing traditional cardiac rehabilitation towards the concept of cardiovascular health for survivors beyond ‘rehabilitation’. These include the need for personalization, processes, patient-centered care, parlance, and partnership. Taken together, consideration of challenges at the systems and population level will ultimately improve engagement with secondary prevention as well as outcomes for all people who need it.
Acknowledgements
J.R. is funded by a National Health and Medical Research Council (NHMRC) Investigator Grant (GNT2007946). A.O. is supported by an NHMRC Emerging Leader 2 Fellowship (2009295). K.H. and E.T. are supported by NHMRC Emerging Leader Fellowships (GNT1196724 and GNT2017450, respectively). S.G., M.H., G.C. and L.Z. are funded by NHMRC Synergy Grant SOLVE-CHD postdoctoral fellowships (APP1182301). I.G. is funded through a Health Research Board Ireland Collaborative Doctoral Award 2019 (CDA-2019-001). R.S.T. has led and received research funding for trials of CR past and present and is currently Director of Cochrane cardiac rehabilitation review programme. No funding organisation had a role in the content or preparation of the manuscript.
Author contributions
J.R., R.G., S.L.G. conceived the manuscript. J.R., D.C., E.E.T., G.L.M.G., D.W., T.B. drafted the manuscript. J.R., A.M., M.H., S.G., A.O., I.G., A.B., R.S.T., R.A., C.J., D.W., S.L.G. contributed to development of recommendations and considerations for reframing. J.R., G.K.C., L.Z., K.H., C.J. contributed to literature synthesis. J.R., R.G., A.M., D.C., M.H., S.G., A.O., G.K.C., L.Z., E.E.T., G.L.M.G., I.G., K.H., A.B., T.B., R.S.T., R.A., C.J., D.W., S.L.G. (all authors) reviewed and approved the final manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Cardiovascular Diseases Factsheet. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (Accessed on 7th March 2024)
- 2.Redfern, J. et al. Impact of cardiac rehabilitation on 3 year outcomes amongst patients after acute coronary syndrome: (ACS) SNAPSHOT ACS follow-up study. Eur. Heart J.41, ehaa946.3108 (2020). [Google Scholar]
- 3.Warren-Gash, C. et al. Severe COVID-19 outcomes by cardiovascular risk profile in England in 2020: a population-based cohort study. Lancet Reg. Health Eur.27, 100604 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ades, P. A. Cardiac rehabilitation and secondary prevention of coronary heart disease. N. Engl. J. Med.345, 892–902 (2001). [DOI] [PubMed] [Google Scholar]
- 5.Redfern, J. et al. Historical context of cardiac rehabilitation: learning from the past to move to the future. Front. Cardiovasc. Med.9, 842567 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Redfern, J. Chow C on behalf of Secondary Prevention Alliance. Secondary prevention of coronary heart disease in Australia: a blueprint for reform. Med. J. Aust.198, 70–71 (2013). [DOI] [PubMed] [Google Scholar]
- 7.Laranjo, L. et al. World Heart Federation Roadmap for secondary prevention of cardiovascular disease: 2023 update. Glob. Heart19, 8 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roth, G. A. et al. Global and regional patterns in cardiovascular mortality From 1990 to 2013. Circ132, 1667–1678 (2015). [DOI] [PubMed] [Google Scholar]
- 9.Stewart, M. J., Hirth, A. M., Klassen, G. & Makrides, L. Wolf H. Stress, coping, and social support as psychosocial factors in readmissions for ischaemic heart disease. Int J. Nurs. Stud.34, 151–163 (1997). [DOI] [PubMed] [Google Scholar]
- 10.Beatty, A. L. et al. A new era in cardiac rehabilitation delivery: research gaps, questions, strategies, and priorities. Circulation147, 254–266 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan, M. A. et al. Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus12, e9349 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Denlinger, C. S. et al. Survivorship: introduction and definition. Clinical practice guidelines in oncology. J. Natl Compr. Canc. Netw.12, 34–45 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Briffa, T. et al. An integrated and coordinated approach to preventing recurrent coronary heart disease events in Australia: a policy statement. Med J. Aust.190, 683–686 (2009). [DOI] [PubMed] [Google Scholar]
- 14.Redfern, J., Briffa, T., Ellis, E. & Freedman, S. Choice of secondary prevention improves risk factors after acute coronary syndrome: one year follow-up of the CHOICE: randomised controlled trial. Heart95, 468–475 (2009). [DOI] [PubMed] [Google Scholar]
- 15.Taylor, R. S., Dalal, H. M. & McDonagh, S. T. J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol.19, 180–194 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oldridge, N. & Taylor, R. S. Cost-effectiveness of exercise therapy in patients with coronary heart disease, chronic heart failure and associated risk factors: A systematic review of economic evaluations of randomized clinical trials. Eur. J. Prev. Cardiol.27, 1045–1055 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Grace, S. L. et al. Cardiac rehabilitation delivery model for low-resource settings: an international council of cardiovascular prevention and rehabilitation consensus statement. Prog. Cardiovasc Dis.59, 303–322 (2016). [DOI] [PubMed] [Google Scholar]
- 18.Balady, G. J. et al. American heart association exercise, cardiac rehabilitation, and prevention committee, the council on clinical cardiology; American heart association council on cardiovascular nursing; American heart association council on epidemiology and prevention; American heart association council on nutrition, physical activity, and metabolism; American association of cardiovascular and pulmonary rehabilitation. core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American heart association exercise, cardiac rehabilitation, and prevention committee, the council on clinical cardiology; the councils on cardiovascular nursing, epidemiology and prevention, and nutrition, physical activity, and metabolism; and the American association of cardiovascular and pulmonary rehabilitation. Circulation115, 2675–2682 (2007). [DOI] [PubMed] [Google Scholar]
- 19.Chaves, G. et al. Cardiac rehabilitation dose around the globe: variation and drivers. Circ. Cardiovasc. Qual. Outcomes13, e005453 (2020). [DOI] [PubMed] [Google Scholar]
- 20.Chowdhury, M. et al. The effects of maintenance cardiac rehabilitation: a systematic review and meta-analysis with a focus on sex differences. Heart Lung50, 504–524 (2021). [DOI] [PubMed] [Google Scholar]
- 21.Kotseva, K. et al. EUROASPIRE III: a survey on the lifestyle, risk factors and use of cardioprotective drug therapies in coronary patients from 22 European countries. Eur. J. Cardiovasc. Prev. Rehabil.16, 121–137 (2009). [DOI] [PubMed] [Google Scholar]
- 22.Moghei, M. et al. Funding sources and costs to deliver cardiac rehabilitation around the globe: drivers and barriers. Int. J. Cardiol.276, 278–286 (2019). [DOI] [PubMed] [Google Scholar]
- 23.Dibben, G. et al. Exercise-based cardiac rehabilitation for coronary heart disease. Coch. Database Syst. Rev. 10.1002/14651858.CD001800.pub4. 2021) [DOI] [PMC free article] [PubMed]
- 24.Taylor, R. S. et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am. J. Med.116, 682–692 (2004). [DOI] [PubMed] [Google Scholar]
- 25.Candelaria, D., Randall, S., Ladak, L. & Gallagher, R. Health-related quality of life and exercise-based cardiac rehabilitation in contemporary acute coronary syndrome patients: a systematic review and meta-analysis. Qual. Life Res.29, 579–592 (2020). [DOI] [PubMed] [Google Scholar]
- 26.van Halewijn, G. et al. Lessons from contemporary trials of cardiovascular prevention and rehabilitation: a systematic review and meta-analysis. Int. J. Cardiol.232, 94–303 (2017). [DOI] [PubMed] [Google Scholar]
- 27.Amsterdam, E. et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol.64, e139–e228 (2014). [DOI] [PubMed] [Google Scholar]
- 28.Robert, A. et al. ESC Scientific Document Group, 2023 ESC Guidelines for the management of acute coronary syndromes: developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J.44, 3720–3826 (2023).37622654 [Google Scholar]
- 29.Lawton, J. S. et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol.79, 197–215 (2022). [DOI] [PubMed] [Google Scholar]
- 30.Canadian Association of Cardiovascular Prevention and Rehabilitation. Translating Knowledge into Action. 3rd edn. (Canadian Association of Cardiovascular Prevention and Rehabilitation, 2009).
- 31.Chew, D. P. et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med. J. Aust.205, 128–133 (2016). [DOI] [PubMed] [Google Scholar]
- 32.Redfern, J. et al. Prescription of secondary prevention medications, lifestyle advice and referral to rehabilitation among acute coronary syndrome (ACS) inpatients: results from a large prospective audit in Australia and New Zealand. Heart100, 1281–1288 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Astley, C. M. et al. The impact of cardiac rehabilitation and secondary prevention programs on 12-month clinical outcomes: a linked data analysis. Heart Lung Circ.29, 475–482 (2020). [DOI] [PubMed] [Google Scholar]
- 34.Chow, C. K. et al. Association of diet, exercise, smoking modification with risk of early cardiovascular events after ACS. Circulation121, 750–758 (2010). [DOI] [PubMed] [Google Scholar]
- 35.Kotseva, K. et al. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in 8 countries. Lancet373, 929–940 (2009). [DOI] [PubMed] [Google Scholar]
- 36.Petter, M., Blanchard, C., Kemp, K. A., Mazoff, A. S. & Ferrier, S. N. Correlates of exercise among coronary heart disease patients: review, implications and future directions. Eur. J. Cardiovasc. Prev. Rehabil.16, 515–526 (2009). [DOI] [PubMed] [Google Scholar]
- 37.Thomas, R. J. Cardiac rehabilitation - challenges, advances, and the road ahead. N. Eng. J. Med.390, 830–841 (2024). [DOI] [PubMed] [Google Scholar]
- 38.Gallagher, R. et al. Promotion And Advocacy For Secondary Prevention Of Cardiovascular Disease Through Cardiac Rehabilitation: The Iccpr Reach, Activities And Outcomes (World Non-Communicable Diseases Congress, 2023).
- 39.Dock, W. The evil sequelae of complete bed rest. J. Am. Med. Assoc.125, 1083–1085 (1944). [Google Scholar]
- 40.Turk-Adawi, K. et al. Cardiac rehabilitation availability and density around the globe. eClinicalMedicine13, 31–45 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beatty, A. L. et al. Million hearts cardiac rehabilitation think tank: accelerating new care models. Circ: Cardiovasc. Qual. Outcomes14, e008215 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shields, G. E. et al. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart104, 1403–1410 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marmot, M. Commentary: mental health and public health. Int J. Epidemiol.43, 293–296 (2014). [DOI] [PubMed] [Google Scholar]
- 44.Carey, G., Crammond, B. & De Leeuw, E. Towards health equity: a framework for the application of proportionate universalism. Int J. Equity Health14, 81 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chan, R. J. et al. Effectiveness and implementation of models of cancer survivorship care: an overview of systematic reviews. J. Cancer Surviv.17, 197–221 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Knox, J. B. L. The vitality of mortality: being-toward-death and long-term cancer survivorship. J. Med. Philos.45, 703–724 (2020). [DOI] [PubMed] [Google Scholar]
- 47.Tevaarwerk, A. et al. Survivorship, Version 1.2021. J. Natl Compr. Canc. Netw.19, 676–685 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Behrens, G. et al. Cancers due to excess weight, low physical activity, and unhealthy diet. Dtsch. Arztebl. Int.115, 578–585 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mehta, L. et al. Cardiovascular disease and breast cancer: where the entities intersect. A scientific statement from the American Heart Association. Circulation137, e30–e66 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Redfern, J., Maiorana, A., Neubeck, L., Clark, A. M. & Briffa, T. Achieving coordinated Secondary Prevention of coronary heart disease for All in Need (SPAN). Int J. Cardiol.146, 1–3 (2011). [DOI] [PubMed] [Google Scholar]
- 51.British Association for Cardiovascular Prevention and Rehabilitation. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation (4th edn). https://www.bacpr.org/__data/assets/pdf_file/0021/64236/BACPR-Standards-and-Core-Components-2023.pdf (Accessed 7 March 2024. 2023).
- 52.German, C. A. et al. Defining preventive cardiology: a clinical practice statement from the American Society for Preventive Cardiology. Am. J. Prev. Cardiol.12, 100432 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taherzadeh, G. et al. Patient-reported outcomes in cardiac rehabilitation: what do we know about program satisfaction? J. Cardiopulm. Rehabil. Prev.36, 230–239 (2016). [DOI] [PubMed] [Google Scholar]
- 54.Kotronoulas, G. et al. Value of the routine use of PROMs: systematic review. J. Clin. Oncol.32, 1480–1501 (2014). [DOI] [PubMed] [Google Scholar]
- 55.DeSalvo, K. B. et al. Mortality prediction with a single general self-rated health question. J. Gen. Intern. Med.21, 267–275 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Burn, E. et al. Cost-effectiveness of a text-message program for cardiovascular disease secondary prevention. Heart103, 893–894 (2017). [DOI] [PubMed] [Google Scholar]
- 57.Gallagher, R. et al. A National Survey of patient data capture, management, reporting practice in australian cardiac rehabilitation programs. Heart Lung Circ.32, 1361–1368 (2023). [DOI] [PubMed] [Google Scholar]
- 58.Grace, S. L. et al. International charter on cardiovascular prevention and rehabilitation: a call for action. J. Cardiopulm. Rehabil. Prev.33, 128–131 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]