Abstract
Introduction
In remote communities, maternal and child health is often compromised due to limited access to healthcare. Simultaneously, these communities historically rely greatly on traditional birth attendants (TBAs). However, optimal integration of these traditional methods with modern healthcare practices remains a topic of debate. We assessed the effect of maternal and child health training of traditional birth attendants on adverse pregnancy outcomes.
Methods
We conducted a systematic review and meta-analysis to answer the above research question. We independently screened studies using databases like PubMed, Scopus, and CENTRAL, extracted data, and assessed the study quality. Due to fewer original studies in this field, we considered both pre-post and between-group differences to assess the effect of differences. These were synthesised separately, assessed against a p-value function, and subjected to sensitivity analyses.
Results
We included six interventional studies. Training TBAs reduced the risk of perinatal mortality [0.69, 0.61–0.78] and 7-day neonatal mortality [0.65, 0.53–0.80] but not stillbirth [0.70, 0.39–1.26]. In randomized controlled trials, there is a lower risk of perinatal mortality [0.73, 0.67–0.79] and neonatal mortality [0.70, 0.62–0.80] but not stillbirth [0.81, 0.56–1.18] with trained traditional birth attendants. There are methodological concerns with most existing studies, including domains like allocation concealment.
Discussion
There is some evidence of the benefit of training TBAs, though of a low to very low certainty. Due to fewer studies, inconsistent estimates for different critical outcomes, and concerns with the existing studies, further well-designed studies can give more insights. They can also help optimize the contents of TBA training interventions.
Protocol
CRD42023412935 (PROSPERO).
Supplementary Information
The online version contains supplementary material available at 10.1007/s44197-024-00300-x.
Keywords: Traditional birth attendants, Tribal, Education, Skill, Maternal and child health, Equitable health access, Pregnancy
Introduction
Maternal health among tribals is a concern, as they often lack access to proper antenatal care, skilled birth attendants, and emergency obstetric services. This lack can lead to higher maternal mortality rates and complications during childbirth. Malnutrition and anaemia are also prevalent among tribal women, further exacerbating their health risks [1]. In the case of maternal and infant health care, these challenges can be particularly pronounced. The tribal population often resides in remote areas with limited access to healthcare facilities. This lack of accessibility can delay proper prenatal care, skilled birth attendance, and postnatal care [2]. Furthermore, cultural beliefs and practices within these communities may influence the utilization of healthcare services. Traditional methods and superstitions sometimes precede evidence-based medical practices, adversely affecting maternal and infant health outcomes [3]. In tribal communities, traditional birth attendants, often called Dais, are crucial in supporting women during pregnancy and childbirth. These skilled individuals have been serving their communities for generations, providing care and assistance to women during this transformative time [4]. During childbirth, a local traditional birth attendant assists the mother. They use their knowledge and experience to provide comfort measures, such as massage, positioning, and breathing techniques, to help ease the process of labour. They also ensure a clean and safe environment for delivery, using traditional practices and remedies to promote a smooth birth. In addition to their practical skills, traditional birth attendants also hold a significant cultural role within the community. They are respected members who carry the wisdom and traditions of their ancestors. Their presence during childbirth is seen to connect with the community's heritage and maintain cultural practices [5, 6]. However, it is important to note that the role of traditional birth attendants is evolving in many tribal communities. The traditional birth attendant's role has faced challenges and changes with the introduction of modern healthcare systems and the emphasis on skilled birth attendance. Some communities have transitioned to utilizing formal healthcare services for childbirth, while others continue to value the traditional birth attendant's expertise [7]. Traditional birth attendants, or TBAs, have long played a role in providing care during childbirth in many communities worldwide. However, the recognition and training of TBAs have been a subject of debate and evolution in maternal and child health [8]. In recent years, there has been a shift in global health policy towards promoting skilled birth attendance by trained healthcare professionals, such as midwives and doctors. This shift has led to a decrease in the formal training and recognition of TBAs in some regions. However, it is important to note that TBAs still play a significant role in providing care, particularly in areas with limited access to skilled birth attendants. In some countries, efforts were made to integrate TBAs into the formal healthcare system through training programs [9]. These programs aim to enhance the knowledge and skills of TBAs, ensuring that they can provide safe and effective care during childbirth. The training typically covers topics such as maternal and child health towards hygiene, infection prevention, recognizing complications, and making timely referrals to skilled healthcare providers [10, 11]. The training of TBAs varies across different regions and countries. Government health departments lead some training programs, while non-governmental organizations or community-based initiatives implement others. Training status for traditional birth attendants in maternal and child health care varies across regions and countries [12]. Efforts have been made to integrate TBAs into the formal healthcare system through training programs, but it is important to ensure that skilled birth attendance by trained healthcare professionals remains the primary focus for ensuring safe and effective childbirth care [13].
The requirement for an updated systematic review and meta-analysis (SRMA) on the impact of training Traditional Birth Attendants on adverse pregnancy outcomes stems from the importance of evidence-based practice in healthcare. As new studies are conducted and new evidence emerges, it is crucial to periodically review and synthesize the existing literature to ensure that our knowledge remains current and reliable.
In the case of training Traditional Birth Attendants, there has been ongoing interest in understanding the effectiveness of such interventions in improving pregnancy outcomes and reducing adverse events. By conducting an updated SRMA, researchers can systematically analyse the available evidence, including older and more recent studies, to assess the overall impact of training Traditional Birth Attendants on adverse pregnancy outcomes.
This process allows for a comprehensive evaluation of the benefits, limitations, and potential risks of training Traditional Birth Attendants. It helps to determine whether such interventions significantly reduce adverse events such as maternal and neonatal mortality, complications during childbirth, or other adverse outcomes. Furthermore, an updated SRMA can help identify gaps or inconsistencies in the existing literature, highlight areas requiring further research, and inform healthcare policies and practices. It provides a valuable tool for healthcare professionals, policymakers, and researchers to make informed decisions based on the most current and robust evidence.
Methods
Research Question and Selection Criteria
This SRMA answers the following research question: ‘What is the effect of training traditional birth attendants on adverse pregnancy outcomes?’ following the 2020 Preferred Reporting Items for Systematic Reviews and Meta-analyses(PRISMA) guidelines (Table S1). To answer this question, we systematically searched the literature and identified eligible articles based on the selection criteria defined using a PICO format (Table S2). We included all interventional studies assessing the effect of training traditional birth attendants on the risk ratios of all adverse pregnancy outcomes. For formal data synthesis, we only included the outcomes reported in two or more studies i.e., stillbirth, 7-day neonatal mortality, neonatal mortality, and perinatal mortality. We included both study designs—randomised controlled trials comparing training to no training, and pre-post single group interventional studies assessing training. Our primary outcome is risk ratio of stillbirth assessed before and after training. We registered the study at a publicly visible registry (PROSPERO), with the record ID CRD42023412935.
Systematic Search and Data Extraction
We systematically searched across three databases of published literature: PubMed, Scopus, and Cochrane Central Register of Controlled Trials, on 09.08.2023. RD prepared the search strategy for PubMed using MeSH terms, keywords, truncated terms and Boolean operators according to this extension to the PRISMA statement [14]. Another author(MAS) reviewed this as per the Peer Review of Electronic Search Strategies checklist [15]. Additionally, we included the grey literature via several preprint servers like Medrxiv, Biorxiv, Arxiv, and SSRN. A search in Google and Google Scholar supplemented this. We also reviewed clinical trial registries like ClinicalTrials.gov, International Clinical Trials Registry Platform(World Health Organisation), and Clinical Trials Registry–India. After this, we checked the references of eligible articles. Following this, we further searched by forward citation matching of the included articles. We sought the opinion of an expert in the field to identify other eligible articles. To achieve reproducibility, we have reported the search strategy across all three databases in Table S3.
After the systematic search and deduplication, two authors (RD & AR) reviewed the title and abstracts for eligibility. In case of any disagreement, the co-authors conversed to build consensus and decided on eligibility. A third independent reviewer's (KS) opinion was considered binding if conflict persisted. Potentially eligible studies went to the next step for full-text screening. Two authors (RD & AR) performed this. They followed a similar process with disagreements, and a third independent reviewer (PD) was the adjudicator.
The included reports were taken up for data extraction using a datasheet containing columns on bibliographic information, study characteristics, baseline data, information on intervention, control, outcome parameters, and other key details. Two authors (RD & AR) extracted data and followed a similar procedure. In case of conflict, they followed the opinion of an independent reviewer (PD).
Risk of Bias Assessment
Two independent authors (RD & AR) evaluated the quality of the selected studies for individual eligible outcomes. After answering signalling questions and assessing the risk of bias under five distinct domains, as recommended by the Cochrane Risk of Bias v2.0, the two assessors compared their findings [16]. In case of an inconsistency between them, they discussed it. If it persisted, they complied with the opinion of a third assessor (KS). This yielded an overall risk of bias for the outcomes in all these studies. The pre-post studies were assessed using an appropriate tool by National Institute of Health [17].
Statistical Analysis
The efficacy parameters are binary outcomes and are expressed as risk ratios. These were log-transformed and synthesised using the Mantel–Haenszel method [18]. These were then back-transformed in the visualisation for ease of interpretation.
For the assessment of heterogeneity, we used tau and tau-squared values. We used the restricted maximum likelihood estimator [19, 20] for estimating tau-squared and the Q-profile method [21] for determining the confidence interval of tau-squared. In addition, we used the I-squared [22], Q-test [23], and prediction interval [24] for estimating heterogeneity. These were considered for the assessment of heterogeneity.
For synthesis, we employed a fixed-effects or a random-effects model based upon the between-study heterogeneity using a threshold of 50% for I-squared. Along with this, we also demonstrated the prediction interval for the true outcomes. Given the current evidence, this gives us the expected range for results from future studies, and is more important for real-world application by epidemiologists and clinicians. We computed the prediction interval based on a t-distribution [25]. We constructed it only for outcomes with more than two studies.
The pooled estimate has been expressed using forest and drapery plots. Forest plots are the conventional and more commonly interpreted method of summarising the results from a meta-analysis. We have also included the details of the outcome parameter and meta-analytical methods in the plots for comprehensiveness and quicker interpretation. Drapery plots complement and add to the inference drawn from a forest plot [26]. The limitation of the former is that they only display the result at a single fixed threshold for the level of significance, usually p < 0.05. We can avoid this controversial sole reliance on a single level [27] and instead use p-value functions. This helps us visualise the results across a wide range of confidence intervals corresponding to diverse p-values. We can visualise the results across a range of significance values. Moreover, the studies are presented in a logical sequence, and the overall trend can be easily observed, along with assessing small-study effects and heterogeneity. The prediction interval could be computed only for those outcomes where more than two studies were present.
We could not use formal tools like the funnel plot and the corresponding Egger’s regression to assess small-study effects and publication bias because of less studies (< 10). The sensitivity analysis omitted each study once for outcomes with more than two studies. We then assessed the change in the pooled estimate. Sensitivity analysis was done in the form of leave-one-out meta-analyses omitting each study one by one and assessing the robustness of the results. We explored the moderation of pooled estimate by a quantitative predictor by performing meta-regression, and visualised it using a bubble plot.
We considered a p-value of 0.05 significant for the primary analysis. Analyses were done using meta [28], and metafor [29] packages in R(v4.2.1) [30]. We assessed evidence certainty using the grading of recommendations, assessment, development, and evaluation (GRADE) framework [31].
Ethical Statement
Ethical review is not applicable here since this is an SRMA of publicly available data.
Results
Study Selection
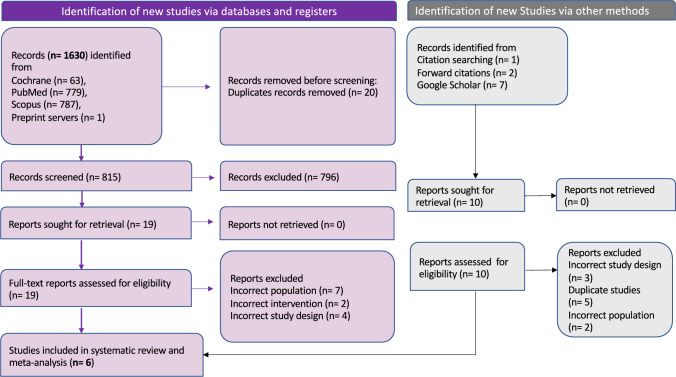
We can visualise the screening process via the PRISMA flowchart (Fig. 1). After a systematic search across three databases, following this search strategy (Table S3), we identified 1630 records. This study assessed the effect of training intervention on several professionals like physicians, nurses, TBAs, and others. TBAs only constituted 30%—40% of the study group, and the outcome data could not be retrieved separately for TBAs. So, we excluded this study [32]. This study assessed the effects of two different interventions using a factorial design. The effect of a community intervention with women’s groups has been studied here, and the effect of training the TBAs was planned to be released in a separate publication [33]. However, this could not be retrieved even after a detailed search and mailing the authors (see Figs. 2, 3 and 4).
Fig. 1.
PRISMA flow chart detailing the literature search, and providing reasons for exclusion of studies
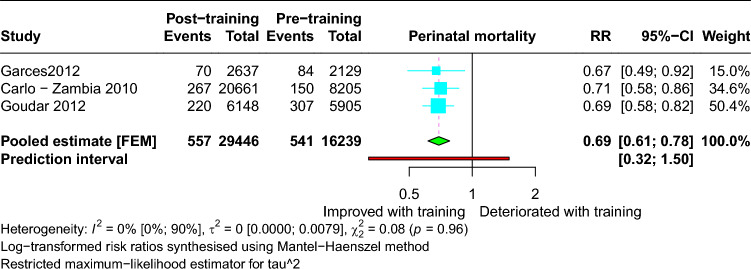
Fig. 2.
Forest plot showing the risk ratio of perinatal mortality with training of traditional birth attendants
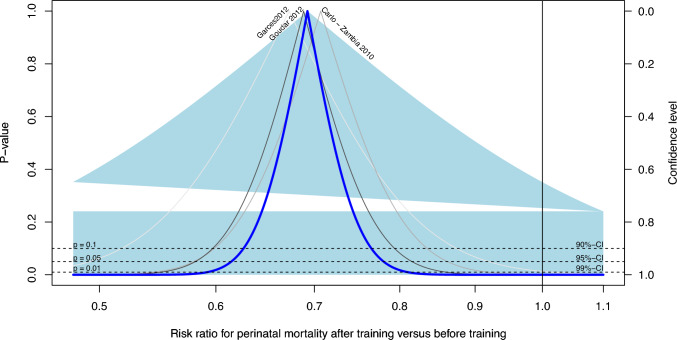
Fig. 3.
Drapery plot showing the ‘level of significance’–dependent variation in the risk ratio of perinatal mortality with training of traditional birth attendants
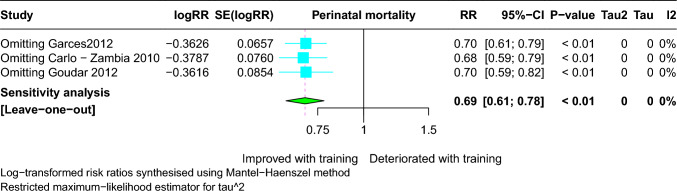
Fig. 4.
Leave-one-out meta-analysis for the risk ratio of perinatal mortality with training of traditional birth attendants
We finally included six studies for systematic review and quantitative synthesis [34–39] [Table 1]. The studies were conducted in several countries in Asia, Africa, and South America. We have summarized the detailed information in Table S4.
Table 1.
Pooled findings of the included studies (N = 6)
| Outcome | Study design | Pooled risk ratio (with 95% CI) | I2 | Model |
|---|---|---|---|---|
| Perinatal mortality | Pre-post studies (Trained versus untrained/less trained) | 0.69 (0.61–0.78) | 0% | Fixed-effects model |
| 7-day neonatal mortality | 0.65 (0.53–0.80) | 35% | Fixed-effects model | |
| Stillbirth | 0.70 (0.39–1.26) | 84% | Random-effects model | |
| Perinatal mortality | Randomised controlled trials (Before training versus after training) | 0.73 (0.67–0.79) | 100% | Fixed-effects model |
| Neonatal mortality | 0.70 (0.62–0.80) | 28% | Fixed-effects model | |
| Stillbirth | 0.81 (0.56–1.18) | 61% | Random-effects model |
Pooled Estimate
Training traditional birth attendants reduced the risk of perinatal mortality [RR: 0.69, 95% CI 0.61–0.78] post-training [Fig. 2]. The 95% prediction interval (95% PI) states the expected range into which the results of 95% of the future studies may lie, and is a more practical estimate. It is expected to give an effect size with the range of 0.32–1.50 in future studies.
Training traditional birth attendants also reduced the risk of 7-day neonatal mortality [RR: 0.65, 95% CI 0.53–0.80; 95% PI 0.08–5.81] post-training. However, the risk of stillbirth did not reduce significantly post-training [RR: 0.70, 95% CI 0.39–1.26; 95% PI 0.00–1036.89].
Trained traditional birth attendants compared to standard care showed a reduced risk of perinatal mortality [RR: 0.73, 95% CI 0.67–0.79] and neonatal mortality [RR: 0.70, 95% CI 0.62–0.80]. However, the risk of stillbirth [RR: 0.81, 95% CI 0.56–1.18] did not reduce significantly compared to usual care.
The drapery plots depict the individual study estimates and the pooled estimate alongside the shaded prediction interval [Fig. 3]. This is depicted against a range of significance thresholds. The thick blue lines shows that the risk reduction in neonatal mortality (after training), perinatal mortality (after training), and neonatal mortality (versus untrained) are all statistically significant even at a p-value as less as 0.01.
Heterogeneity and Small-Study Effects Assessment and Exploration
The pooled estimates had differing between-study heterogeneities as assessed by I2 and prediction interval and depicted in the respective forest plots. Since there is high between-study heterogeneity for risk of stillbirth [I2 = 84%, τ2 = 0.24 (0.03–12.03), Cochran’s Q: p < 0.01], we explored the relation with sample size. This was done using meta-regression, and visualised as a bubble plot. However, it did not moderate the pooled risk ratio (beta = 0, p = 0.16). We could not conduct a formal test for publication bias or small-study effects because of the low number of studies. The detailed outcome assessment for individual studies and heterogeneity estimates for each outcome can be checked in the respective forest plots.
Sensitivity Analysis
We conducted sensitivity analyses using leave-one-out meta-analyses for the outcomes with more than two studies [Fig. 4]. The effect of omitting each study one-by-one is depicted in Figs. S9–S11.
Risk of Bias
Amongst the randomised controlled trials, two studies were at a high risk of bias, while one had some concerns. In this study [37], the randomisation for the latter part of the control group is not clearly given. In another study [35], there is no information on allocation concealment. The detailed domain-wise quality assessment is given in Fig. S13. Amongst the pre-post studies, the study quality varied from moderate to low risk of bias. The question-wise detailed assessment is given in Table S5. The evidence certainty is provided in Table S6, with most outcomes providing effects of a low to very low certainty.
Discussion
We assessed the effect of maternal and child health training on traditional birth attendants. There is a decrease in the risk of early neonatal mortality, neonatal mortality, and perinatal mortality. However, there is no difference in the risk of stillbirth. This change indirectly suggests that these training modules help mitigate the reduction in the outcomes following delivery i.e., neonatal mortality. Although stillbirth is not reduced, the summary estimate of perinatal mortality shows a decline because of the neonatal parameter.
Several studies have explored the impact of maternal and child health training on traditional birth attendants (TBAs) on reducing the risk of perinatal mortality. TBAs are locally available individuals who provide childbirth and maternal care in many communities, particularly in areas with limited access to formal healthcare facilities [37]. Similarly, our findings show that training traditional birth attendants reduced the risk of perinatal mortality [RR: 0.69, 95% CI 0.61–0.78]. Post-training traditional birth attendants (TBAs) have proven effective in reducing perinatal and 7-day neonatal mortality risk. However, it appears that the training did not significantly impact stillbirth rates. Therefore, there is a need for TBAs' knowledge and abilities to be developed within acceptable limits by ongoing collaboration between TBAs and health systems [40]. As governments progress towards providing SBA to all women, the possible role of TBAs should be carefully considered. Although the data has limitations due to the research design, TBA training can enhance some newborn outcomes but does not affect mother mortality [41]. In India, because access to public healthcare is limited, the tribal health system faces challenges. Tribal health challenges differ due to the tribal populations' distinctive socio-cultural practices, rituals, customs, and languages [42]. Traditional birth attendants are very popular and highly influential in their tribal community. People prefer to take their help in maternal and child health. The TBA's psychological and socio-cultural support and community-wide access to mothers are believed to have contributed significantly to maternity and newborn health care. TBAs have an important role in improving maternal and newborn health, particularly in rural regions where they continue to be a vital force in delivering health and nutrition initiatives. One study shows that utilization of traditional birth attendant (TBA) services in a rural Local Government area with proper training of TBA can provide conventional and traditional maternity care that will translate into improved maternal and newborn health outcomes in relevant contexts [40]. The trained TBA adoption could positively influence the community members to handle and manage obstetric and neonatal complications [41].
There are several strengths to this manuscript. We have comprehensively covered a variety of evidence on the training of traditional birth attendants. We have followed it up with robust methodological and statistical steps to get accurate estimates. The limitation of this manuscript is tied down to the lack of enough well-designed interventional studies in this field. We have addressed this by covering several different research questions and synthesising them separately to get overall evidence. Training traditional birth attendants improved outcomes. However, there is a considerable scope for future research. There are very few studies, and further well-designed studies especially in the lower and middle- income countries can shed more light on the effectiveness of these training modules. The overall course content in these training packages can be further optimised to improve their effectiveness. As highlighted by the differential change in neonatal mortality and stillbirths, special attention should be paid to the neonatal components of training modules apart from the labour-related components. These can build an evidence base for good health and well-being with reduced inequality in the primary care for maternal and child health.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are thankful to the research team of the Centre of Excellence for Tribal Health, AIIMS, Jodhpur. The authors are extremely thankful to Dr. Naval Jit Kapoor, Additional Secretary, and the entire team of the Ministry of Tribal Affairs, Government of India, for their constant guidance and financial support. The authors acknowledge the National Workshop on Systematic Review and Meta-Analysis conducted by the Department of Pharmacology and Centre of Excellence for Tribal Health, AIIMS, Jodhpur.
Author Contributions
Study design: RD, MAS, PD, AR, PS, VV, KS. Data collection: RD, AR, MAS, PD. Data analysis: RD, MAS, ADG. Figures and tables: RD, PD, AR, ADG. Data interpretation: ADG, PS, VV, KS, SGD, KM. Initial manuscript writing: RD, AR, PD, SGD, KM. Critical inputs and final revision of the manuscript: All the authors Availability of the entire study Availability of the entire study data: All the authors.
Funding
None.
Data Sharing Statement
All data has been made available here and in the annexures.
Declarations
Conflict of Interest
The authors report no conflict of interest.
Ethics Approval
It is not applicable here since it is an SRMA of publicly available data.
Patient and Public Involvement Statement
It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
Footnotes
Rakhi Dwivedi and Muhammad Aaqib Shamim joint first authors and contributed equally.
Contributor Information
Pradeep Dwivedi, Email: dr.pradd99@gmail.com.
Kuldeep Singh, Email: kulpra@gmail.com.
References
- 1.Jose JA, Sarkar S, Kumar SG, et al. Utilization of maternal health-care services by tribal women in Kerala. J Nat Sci Biol Med. 2014;5:144–7. 10.4103/0976-9668.127314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nair H, Panda R. Quality of maternal healthcare in India: Has the National Rural Health Mission made a difference? J Glob Health. 2011;1:79–86. [PMC free article] [PubMed] [Google Scholar]
- 3.Omer S, Zakar R, Zakar MZ, et al. The influence of social and cultural practices on maternal mortality: a qualitative study from South Punjab. Pakistan Reprod Health. 2021;18:97. 10.1186/s12978-021-01151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhardwaj N, Yunus M, Hasan SB, et al. Role of traditional birth attendants in maternal care services—a rural study. Indian J Matern Child Health Off Publ Indian Matern Child Health Assoc. 1990;1:29–30. [PubMed] [Google Scholar]
- 5.Contractor SQ, Das A, Dasgupta J, et al. Beyond the template: the needs of tribal women and their experiences with maternity services in Odisha, India. Int J Equity Health. 2018;17:134. 10.1186/s12939-018-0850-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Musie MR, Mulaudzi MF, Anokwuru R, et al. Recognise and acknowledge us: views of traditional birth attendants on collaboration with midwives for maternal health care services. Int J Reprod Med. 2022;2022:9216500. 10.1155/2022/9216500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilunda C, Dallglio G, Scanagatta C, et al. Changing the role of traditional birth attendants in Yirol West, County South Sudan. PLoS ONE. 2017;12: e0185726. 10.1371/journal.pone.0185726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chi PC, Urdal H. The evolving role of traditional birth attendants in maternal health in post-conflict Africa: a qualitative study of Burundi and northern Uganda. SAGE Open Med. 2018;6:2050312117753631. 10.1177/2050312117753631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hernandez S, Oliveira JB, Shirazian T. How a training program is transforming the role of traditional birth attendants from cultural practitioners to unique health-care providers: a community case study in rural guatemala. Front Public Health. 2017;5:111. 10.3389/fpubh.2017.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garces A, McClure EM, Espinoza L, et al. Traditional birth attendants and birth outcomes in low-middle income countries: a review. Semin Perinatol. 2019;43:247–51. 10.1053/j.semperi.2019.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Traditional Birth Attendants. Geneva; 1992. https://iris.who.int/bitstream/handle/10665/38994/9241561505.pdf?sequence=1&isAllowed=y.
- 12.MacDonald ME. The place of traditional birth attendants in global maternal health: policy retreat, ambivalence and return. In: Wallace LJ, MacDonald ME, Storeng KT, editors. Anthropologies of global maternal and reproductive health: from policy spaces to sites of practice. Cham: Springer; 2022. [PubMed] [Google Scholar]
- 13.Ribeiro SD. Traditional Birth Attendance (TBA) in a health system: what are the roles, benefits and challenges: a case study of incorporated TBA in Timor-Leste. Asia Pac Fam Med. 2014;13:12. 10.1186/s12930-014-0012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rethlefsen ML, Kirtley S, Waffenschmidt S, et al. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 2021;10:39. 10.1186/s13643-020-01542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6. 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 16.RoB 2: a revised tool for assessing risk of bias in randomised trials | The BMJ. https://www.bmj.com/content/366/bmj.l4898. Accessed 21 Aug 2023 [DOI] [PubMed]
- 17.National Heart Lung and Blood Institute. Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group [National Heart Lung and Blood Institute web site]. 2014.
- 18.Robins J, Breslow N, Greenland S. Estimators of the Mantel-Haenszel variance consistent in both sparse data and large-strata limiting models. Biometrics. 1986;42:311–23. [PubMed] [Google Scholar]
- 19.Veroniki AA, Jackson D, Viechtbauer W, et al. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods. 2016;7:55–79. 10.1002/jrsm.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bias and efficiency of meta-analytic variance estimators in the random-effects model—Wolfgang Viechtbauer, 2005. https://journals.sagepub.com/doi/10.3102/10769986030003261. Accessed 21 Aug 2023
- 21.Viechtbauer W. Confidence intervals for the amount of heterogeneity in meta-analysis. Stat Med. 2007;26:37–52. 10.1002/sim.2514. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 23.Cochran WG. The Combination of Estimates from Different Experiments. Bioethics. 1954. 10.2307/3001666. [Google Scholar]
- 24.IntHout J, Ioannidis JPA, Rovers MM, et al. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6: e010247. 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc. 2009;172:137–59. 10.1111/j.1467-985X.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rücker G, Schwarzer G. Beyond the forest plot: The drapery plot. Res Synth Methods. 2021;12:13–9. 10.1002/jrsm.1410. [DOI] [PubMed] [Google Scholar]
- 27.Infanger D, Schmidt-Trucksäss A. P value functions: an underused method to present research results and to promote quantitative reasoning. Stat Med. 2019;38:4189–97. 10.1002/sim.8293. [DOI] [PubMed] [Google Scholar]
- 28.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60. 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viechtbauer W. Conducting meta-analyses in R with the metafor Package. J Stat Softw. 2010;36:1–48. 10.18637/jss.v036.i03. [Google Scholar]
- 30.Shamim MA, Gandhi AP, Dwivedi P, et al. How to perform meta-analysis in R: a simple yet comprehensive guide. The Evidence. 2023;1:93–113. 10.61505/evidence.2023.1.1.6. [Google Scholar]
- 31.Schünemann HJ, Neumann I, Hultcrantz M, et al. GRADE guidance 35: update on rating imprecision for assessing contextualized certainty of evidence and making decisions. J Clin Epidemiol. 2022;150:225–42. 10.1016/j.jclinepi.2022.07.015. [DOI] [PubMed] [Google Scholar]
- 32.Carlo WA, Goudar SS, Jehan I, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362:614–23. 10.1056/NEJMsa0806033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Azad K, Barnett S, Banerjee B, et al. Effect of scaling up women’s groups on birth outcomes in three rural districts in Bangladesh: a cluster-randomised controlled trial. The Lancet. 2010;375:1193–202. 10.1016/S0140-6736(10)60142-0. [DOI] [PubMed] [Google Scholar]
- 34.Kestler E, Ambrosio G, Hemming K, et al. An integrated approach to improve maternal and perinatal outcomes in rural Guatemala: a stepped-wedge cluster randomized trial. Int J Gynecol Obstet. 2020;151:109–16. 10.1002/ijgo.13262. [DOI] [PubMed] [Google Scholar]
- 35.Jokhio AH, Winter HR, Cheng KK. An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med. 2005;352:2091–9. 10.1056/NEJMsa042830. [DOI] [PubMed] [Google Scholar]
- 36.Goudar SS, Somannavar MS, Clark R, et al. Stillbirth and newborn mortality in India after helping babies breathe training. Pediatrics. 2013;131:e344-352. 10.1542/peds.2012-2112. [DOI] [PubMed] [Google Scholar]
- 37.Gill CJ, Phiri-Mazala G, Guerina NG, et al. Effect of training traditional birth attendants on neonatal mortality (Lufwanyama Neonatal Survival Project): randomised controlled study. BMJ. 2011;342: d346. 10.1136/bmj.d346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carlo WA, McClure EM, Chomba E, et al. Newborn care training of midwives and neonatal and perinatal mortality rates in a developing country. Pediatrics. 2010;126:e1064-1071. 10.1542/peds.2009-3464. [DOI] [PubMed] [Google Scholar]
- 39.Garcés A, McClure EM, Hambidge M, et al. Training traditional birth attendants on the WHO Essential Newborn Care reduces perinatal mortality. Acta Obstet Gynecol Scand. 2012;91:593–7. 10.1111/j.1600-0412.2012.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ebuehi OM, Akintujoye I. Perception and utilization of traditional birth attendants by pregnant women attending primary health care clinics in a rural Local Government Area in Ogun State, Nigeria. Int J Womens Health. 2012;4:25–34. 10.2147/IJWH.S23173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anono EL, Ochola S, Wawire S, et al. Community perceptions towards the new role of traditional birth attendants as birth companions and nutrition advocates in Kakamega County, Kenya. Matern Child Nutr. 2018;14(Suppl 1): e12578. 10.1111/mcn.12578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deb Roy A, Das D, Mondal H. The tribal health system in India: challenges in healthcare delivery in comparison to the global healthcare systems. Cureus. 2023;15: e39867. 10.7759/cureus.39867. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data has been made available here and in the annexures.