Abstract
Aim
Critically ill individuals may have left ventricular diastolic dysfunction (LVDD) which can prolong their intensive care unit (ICU) stay. The purpose of this study was to determine the prevalence of LVDD in critically ill adult patients requiring mechanical ventilation in ICU, the effect of LVDD on 28-day survival, and weaning from mechanical ventilation.
Methodology
A total of 227 adults who had been on mechanical ventilation for more than 48 hours in an ICU were recruited for this study. The study's parameters were recorded on the third day of mechanical ventilation using a low-frequency phased array probe. A simplified definition of LVDD in critically ill adults was utilized to determine the presence or absence of LVDD. Weaning failure and 28-day mortality were noted.
Results
The prevalence of LVDD in adults requiring mechanical ventilation in the ICU was found to be 35.4% (n = 79). Patients with LVDD had the odds of having a 28-day mortality increase by 7.48 (95% CI: 3.24–17.26, p < 0.0001). Patients with LVDD had the odds of having weaning failure increase by 5.37 (95% CI: 2.17–13.26, p = 0.0003).
Conclusion
Measures should be taken to detect critically ill adults with LVDD with systolic dysfunction or heart failure with preserved ejection fraction early so that their fluid balance, myocardial contractility, and afterload can be optimized to minimize their morbidity and mortality.
Highlights
Critically ill adults with LVDD may have adverse outcomes. Hence, protocol should be in place for diagnosing LVDD early in critically ill adults thereby, measures can be taken to minimize morbidity in those patients.
How to cite this article
Luitel B, Senthilnathan M, Cherian A, Suganya S, Adole PS. Prevalence of Diastolic Dysfunction in Critically Ill Patients Admitted to Intensive Care Unit from a Tertiary Care Hospital: A Prospective Observational Study. Indian J Crit Care Med 2024;28(9):832–836.
Keywords: Critically ill adults, Impaired relaxation, Left ventricular diastolic dysfunction, Prevalence, 28-day mortality, Weaning failure
Introduction
Critically ill individuals are more likely to develop hemodynamic instability, and this unstable hemodynamic state might eventually lead to multi-organ dysfunction. It frequently occurs after a period of physiological decline. The primary goal of current alert algorithms is to recognize circumstances that pose a threat to life.1 Hemodynamic monitoring is used to direct medical care toward curing or preventing organ failure as well as lowering morbidity and mortality. There are numerous invasive and non-invasive monitoring methods. Each of them has its own benefits and drawbacks. Nowadays, bedside transthoracic echocardiography (TTE) is one of the most adaptable diagnostic and therapeutic methods for monitoring individuals with hemodynamic instability. It has now become the go-to technique for quick, precise evaluation of heart function in the intensive care unit (ICU). While performing an echocardiographic evaluation on individuals who have diastolic dysfunction, one should look for signs of reduced left ventricular (LV) relaxation, decreased restoring forces, and increased diastolic stiffness, which will provide information on the disease's progression.
Left ventricular diastolic dysfunction (LVDD) is frequently overlooked, in contrast to systolic dysfunction (LVSD). Individuals with LVDD may have co-existing LV systolic dysfunction or normal systolic function (Heart Failure with Preserved Ejection Fraction [HFpEF]).2 It has been established that LVDD is a standalone risk factor for higher mortality in the ICU.3–6 Moreover, it is also a significant factor in delayed weaning from mechanical ventilation.7–10 There has not been any research on the prevalence of LVDD in the population of the Indian subcontinent. This study was designed with the primary objective as to study the prevalence of LVDD in adults requiring mechanical ventilation in ICU, and with secondary objectives as to study the effects of LVDD on 28-day survival and weaning failure.
Methodology
After obtaining approval from the IEC (Ref.no: JIP/ IEC/ 2021/ 0133), the study was registered in the Clinical Trial Registry-India (Reg.no: CTRI/2021/10/037633). Adult patients admitted to ICU requiring mechanical ventilation at least for 48 hours were recruited in this study (patients were recruited on the third day of mechanical ventilation). Patients with documented pre-existing mitral valvular lesions were excluded from this study. After obtaining informed written consent from the patient's legally acceptable representative, adult patients who had been on mechanical ventilation for more than 48 hours in the ICU were recruited for this study. On the first day of admission to the ICU, information about the patient's age, height, weight, gender, diagnosis, the reason they were put on a ventilator, and their acute physiology and chronic health evaluation (APACHE II) score were recorded. On the day of the study, a sequential organ failure assessment (SOFA) score was obtained. From the patient's history, prior medical records, and most recent investigations, it was possible to determine whether they had comorbid conditions like diabetes mellitus (DM), hypertension (HTN), coronary artery disease (CAD), dyslipidemia, congestive cardiac failure (CCF), chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), hepatic cirrhosis, and any arrhythmias. The patient's heart rate (HR), oxygen saturation (SpO2), systolic, diastolic, and mean arterial blood pressures (SBP, DBP, and MAP) were recorded just before the measurement of the study parameters. The attending intensivist made the decisions about the mechanical ventilation settings.
The study's parameters were recorded using a low-frequency phased array probe (1–5 mHz, My LabX5, Esaote, Genova, Italy). On the third day of mechanical ventilation in the CCU, during a stable hemodynamic window, the research parameters were recorded. In this study, a stable hemodynamic window is defined as the avoidance of fluid boluses or a change in the dose of a vasopressor or inotropic drug for at least 2 hours. An intensive care physician who has had experience in TTE for at least 1 year recorded the study parameters. An apical four-chamber (A4C) view was obtained by placing the echocardiographic probe over the apical impulse and keeping the probe horizontal with the orientation marker facing toward the left. In A4C view, pulse wave Doppler (PWD) sampling was obtained at the mitral valvular leaflet tips to obtain the E wave, which represents early passive diastolic filling, and the A wave, which results from atrial contraction. The deceleration time was obtained from the E wave. The machine calculated the E/A ratio. Tissue Doppler imaging (TDI) was utilized to measure mitral annular peak velocities. Tissue Doppler sampling was performed at the septal mitral annulus to obtain septal e’; it was performed in the lateral mitral annulus to obtain lateral e’. The machine calculated the average E/e’.11 The left atrial volume index (LAVI) was obtained by measuring its length and transverse diameter in A4C, or apical 2 chamber view, one to two frames prior to the opening of the mitral valve. Tricuspid regurgitation maximum velocity (TR Vmax) was obtained by placing the continuous wave Doppler (CWD) at the regurgitant jet area (located by color flow Doppler) in A4C view. The simplified definition of LVDD in critically ill adults was utilized to diagnose LVDD in this study.12 Patients with septal mitral annular velocity (septal e’) of less than 8 cmS−1 were categorized as LVDD and patients with septal e’ of >8 cmS−1 were considered as having normal LV diastolic function (Fig. 1). The findings from this study were shared with the treating doctors, and the decision to treat based on the findings from this study was left to their discretion. Weaning failure, in this study, was defined as the requirement of any form of ventilatory support within 48 hours of extubation. The patient's survival outcome at 28 days after recruitment in this study was noted. With an observed prevalence of 83% LVDD in critically ill adults in a study performed by Rolando et al.,13 the sample size has been calculated with an effect size of 1 and with absolute precision of 5%. The initial sample size was calculated as 207 and to compensate for the 10% dropouts, the final sample size had been calculated as 227.
Fig. 1.
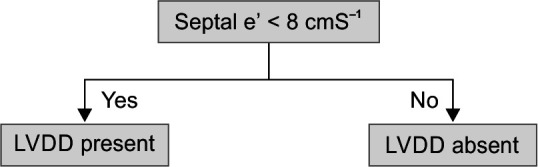
Simplified criteria for diagnosing LVDD in critically ill adults
LVDD, left ventricular diastolic dysfunction; Septal e’ velocity, septal mitral annular velocity
Results
Data was analyzed using SPSS for Windows version 20. The association between LVDD and 28-day mortality and weaning failure was analyzed with a chi-square test. Multivariate logistic regression was carried out to determine if the outcomes, “28-day mortality” and “weaning failure,” were influenced by independent variables. A total of 246 patients were screened for this study and 19 were excluded due to pre-existing mitral valvular lesions and unstable hemodynamics. Out of 227 recruited patients, 4 were withdrawn due to poor echogenic window (Fig. 2). Among the recruited patients, 56.5% were males and 43.5% were females. Recruited patients had a mean age of 43.2 ± 18.8 years, mean BMI of 23.3 ± 3.0 kg.m−2, mean APACHE-II of 22.8 ± 8.6, and mean SOFA score of 6.1 ± 2.5. Details of the primary etiology for which patients were admitted into the ICU were depicted as follows (Table 1).
Fig. 2.
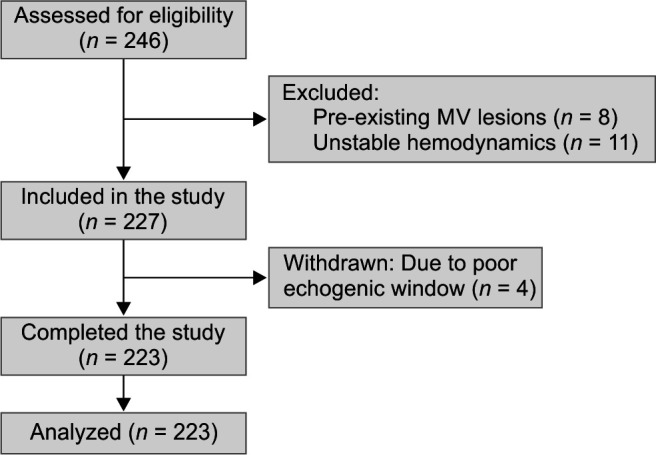
STROBE diagram of this study
Table 1.
Primary etiology for which patients were admitted to ICU
| Diagnosis | Number of patients (%) |
|---|---|
| Thoracic trauma | 11 (5.38%) |
| Abdominal trauma | 16 (10.31%) |
| Traumatic brain injury | 17 (7.62%) |
| Polytrauma (multiple bony injuries) | 19 (8.52%) |
| Acute coronary syndrome | 15 (6.72%) |
| Oxygenation failure | 27 (16.14%) |
| Ventilation failure | 14 (6.27%) |
| Immunological disorders | 9 (4%) |
| Pneumonia | 11 (4.93%) |
| Post-renal transplantation (due to systemic infections) | 3 (1.34%) |
| Organophosphorus poisoning | 17 (7.62%) |
| Snake bite | 5 (2.24%) |
| Meningitis | 18 (8.07%) |
| Guillain-Barre syndrome | 2 (0.89%) |
| Diabetic ketoacidosis | 7 (3.1%) |
| Hypokalemic periodic paralysis | 2 (0.89%) |
| Post-operative (esophagectomy, Whipple procedure, pheochromocytoma, gastrectomies) | 21 (9.41%) |
| Post-cardiac arrest | 7 (3.1%) |
| Anaphylactic shock | 2 (0.89%) |
The prevalence of LVDD in adults requiring mechanical ventilation in the ICU was found to be 35.4% (n = 79). The incidence of 28-day mortality among the patients with LVDD was found to be 35% (28 patients out of 79), while it was 7.64% (11 out of 144) in patients without LVDD which was statistically significant [Odds ratio (OR) 6.64; 95% confidence interval (CI): 3.08–14.32; p < 0.001]. Mean E/e’ in patients with LVDD was 7.88 ± 3.6 and 5.31 ± 1.43 in patients without LVDD, p < 0.001. Left ventricular filling pressures revealed a statistically significant difference as measured by E/e’ between patients who survived and died at 228 days [Mean E/e’ in patients with 28-day mortality was 7.89 4.22 vs 5.87 2.13 in patients who survived, p = 0.016]. The incidence of weaning failure among patients with LVDD was 25.32% (20 out of 79), while it was 6.94% (10 out of 144) in patients without LVDD (OR 4.54; 95% CI: 2.0–10.3); p < 0.001] and this was statistically significant.
Patients with LVDD had the odds of having a 28-day mortality increase by 7.48 [95% CI: 3.24 –17.26, p < 0.0001] (Table 2). Patients requiring vasopressors during ICU stay had the odds of having a 28-day mortality increase by 2.28 [95% CI: 1.04–4.99, p = 0.04]. Among patients with LVDD, 25 (31.6%) had LV systolic dysfunction and 54 (68.7%) had HFpEF.
Table 2.
Multivariate logistic regression for 28-day mortality as outcome
| Variables | Odds ratio | 95% Confidence interval | p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | 1.01 | 0.992 | 1.04 | 0.223 |
| APACHE II | 1.09 | 1.04 | 1.13 | 0.16 |
| Vasopressors need | 2.28 | 1.04 | 4.99 | 0.04* |
| Left ventricular diastolic dysfunction | 7.48 | 3.24 | 17.26 | <0.0001* |
*p < 0.05
Patients with LVDD had the odds of having weaning failure increase by 5.37 (95% CI: 2.17 left ventricular13.26, p = 0.0003) (Table 3).
Table 3.
Multivariate logistic regression for weaning failure as outcome
| Variables | Odds ratio | 95% Confidence interval | p-value | |
|---|---|---|---|---|
| Lower range | Upper range | |||
| Age | 1.02 | 0.992 | 1.04 | 0.202 |
| APACHE II | 1.11 | 1.06 | 1.16 | <0.0001 |
| Vasopressors need | 0.976 | 0.384 | 2.48 | 0.95 |
| Left ventricular diastolic dysfunction | 5.37 | 2.17 | 13.26 | 0.0003* |
*p < 0.05
Discussion
This study primarily aimed to determine the prevalence of LVDD in adults requiring positive pressure ventilation in the ICU. Left ventricular diastolic dysfunction was diagnosed with a simplified definition of LVDD in critically ill adults by Lanspa et al. Approximately one-third of the recruited patients in this study [79 (35.4%)] had LVDD. The prevalence of LVDD in several investigations that have been published in the literature has ranged from 10 to 84%. During the first 24 hours of their admission to critical care, Cavefors et al. performed echocardiograms on 218 patients, of whom 21 (10%) showed diastolic dysfunction and 35 (17%) had an indeterminate diastolic function.14 Gonzalez et al. conducted a retrospective study and found that 31% of recruited 223 patients in septic shock in a medical-surgical ICU were found to have LVDD which was similar to our study.5 In a prospective study by Pulido et al., TTE was performed within 24 hours of ICU admission for 106 patients with severe sepsis or septic shock.15 They discovered that 39 individuals (37%) had LV dysfunction. Rolando et al. performed 99 echocardiograms on 53 septic adults.13 83 percent had LVDD among them. Hong et al. found that 39 (24.1%) had LVDD among 162 critically ill patients with sepsis.16 According to Clancy et al., 20 (54%) of the 37 patients having severe sepsis or septic shock with normal systolic function studied on day 3 had diastolic dysfunction, and 6 (16%) had indeterminate diastolic dysfunction.17
One of the secondary objectives of this study was to study the incidence of 28-day mortality among patients with diastolic dysfunction. The incidence of 28-day mortality among the patients with LVDD was found to be 35% and it was 7.64% in patients without LVDD. The risk of 28 days mortality increased by 7.48 odds [95% CI: 3.24–17.26, p < 0.0001] in patients with LVDD. 2 echocardiography exams were performed on 262 adults with severe sepsis or septic shock and among them, 40.4% of patients with LVDD passed away while receiving hospital treatment, according to Landesberg et al.3 Gonzalez et al. studied the prognostic significance of LVDD in septic shock patients.5 Compared to their counterparts, non-survivors tended to have a larger percentage of LV diastolic dysfunction [28/78 (36%) vs 41/145 (28%]. Intensive care unit mortality was 48% among the 72 cancer patients who were admitted and had echocardiography within 48 hours of developing septic shock, according to Mourad et al.6 It was higher among those with diastolic dysfunction than among individuals without the condition, which was 71% vs 21% (p = 0.0001). Hong et al. found that LVDD was associated with mortality (Hazard ratio: 2.7; p = 0.047).16 A study by Sturgess et al. on 21 adults from an ICU. Echocardiography was performed within 72 hours of developing septic shock and demonstrated a hospital mortality of 29%.18
Notice that HFpEF attributes more than 50% of hospitalized patients with heart failure. Incidence of HFpEF increases with age, and comorbid conditions like hypertension, chronic kidney disease, atrial fibrillation, and obesity.19 Prevalence of HFpEF in ICU was 68.7% in this study.
Determining the prevalence of weaning failure among individuals with LVDD was the study's other secondary objective. In our study, weaning failure was defined as the requirement of ventilatory support within 48 hours of extubation. The incidence of weaning failure among patients with LVDD was 25.32% and it was 6.94% in patients without LVDD. The risks of weaning failure increased by 5.37 odds (95% CI: 2.17–13.26, p = 0.0003) in patients with LVDD. In a study by Papanikolaou et al., 50 critical care patients with no pre-existing heart conditions underwent echocardiography before and after spontaneous breathing trials (SBT) (pre-SBT/end-SBT, respectively).7 28 patients (or 56%) were unable to wean; of these, 23 had SBT failures, and 5 needed to be reintubated within 48 hours. Patients with LVDD at pre-SBT were associated with weaning failure (p = 0.01). By using Cox regression analysis, they observed that LVDD required the association of a positive fluid balance with age rather than being a solitary predictor of weaning failure. Moschietto et al. included 68 patients who were on positive pressure ventilation for >48 hours.9 The authors performed TTE before the SBT and 10 minutes after the commencement of the SBT. Left ventricular diastolic dysfunction was defined as annulus mitral velocity (e’) ≤8 cmS−1. 20 failed the weaning process. The cut-off value, obtained from receiver operating characteristics (ROC) curve analysis, to predict weaning failure gave a sensitivity and specificity of E/e’ ratio during SBT in predicting weaning failure as 75 and 95.8%, respectively. Hence, they concluded that measurement of the E/e’ ratio could predict weaning failure, and LVDD was strongly associated with weaning failure. A systematic review and meta-analysis that included 11 studies was carried out by Sanfilippo et al.10 Weaning failure was strongly associated with a lower e’ wave [standardized mean difference (SMD) = –1.22, 95% CI: (–2.33 to –0.11); p = 0.03], a greater E wave [SMD = 0.97, 95% CI: (0.29–1.65); p = 0.005], and a higher E/e’ ratio [SMD = 1.70, 95% CI: (0.78–2.62); p < 0.001]. They concluded that weaning failure was associated with parameters indicating worse LV diastolic function (E/e’, e’ wave, E wave) and increased LV filling pressure (E/e’ ratio).
This study had the following limitations. The echocardiography was performed by an intensivist with 1 year of experience and the acquired images were not counterchecked by an expert. The study parameters to diagnose LVDD were measured at only one-time point during this study. Cumulative fluid balance and cumulative vasopressor dose requirement of the recruited patients were not studied which could have been utilized to study the effect of these parameters on the survival outcome.
Conclusion
Adverse outcomes like 28-day mortality and weaning failure were high in critically ill adults with LVDD. Hence, measures should be taken to detect critically ill adults with LVDD with systolic dysfunction or HFpEF early. Their fluid balance, myocardial contractility, and afterload should be optimized to minimize their morbidity and mortality.
Orcid
Bipin Luitel https://orcid.org/0009-0001-8798-5978
Muthapillai Senthilnathan https://orcid.org/0000-0001-8418-5046
Anusha Cherian https://orcid.org/0000-0001-9017-5311
Srinivasan Suganya https://orcid.org/0000-0003-2953-3938
Prashant S Adole https://orcid.org/0000-0002-1692-3892
Footnotes
Source of support: JIPMER Intramural Grant Fund.
Conflict of interest: None
References
- 1.Huygh J, Peeters Y, Bernards J, Malbrain MLNG. Hemodynamic monitoring in the critically ill: An overview of current cardiac output monitoring methods. F1000Research. 2016:5. doi: 10.12688/f1000research.8991.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuznetsova T, Herbots L, López B, Jin Y, Richart T, Thijs L, et al. Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail. 2009;2:105–112. doi: 10.1161/CIRCHEARTFAILURE.108.822627. [DOI] [PubMed] [Google Scholar]
- 3.Landesberg G, Gilon D, Meroz Y, Georgieva M, Levin PD, Goodman S, et al. Diastolic dysfunction and mortality in severe sepsis and septic shock. Eur Heart J. 2012;33:895–903. doi: 10.1093/eurheartj/ehr351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bansal S, Varshney S, Shrivastava A. A prospective observational study to determine incidence and outcome of sepsis-induced cardiomyopathy in an intensive care unit. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med. 2022;26:798–803. doi: 10.5005/jp-journals-10071-24204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzalez C, Begot E, Dalmay F, Pichon N, François B, Fedou AL, et al. Prognostic impact of left ventricular diastolic function in patients with septic shock. Ann Intensive Care. 2016;6:36. doi: 10.1186/s13613-016-0136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mourad M, Chow-Chine L, Faucher M, Sannini A, Brun JP, de Guibert JM, et al. Early diastolic dysfunction is associated with intensive care unit mortality in cancer patients presenting with septic shock. Br J Anaesth. 2014;112:102–109. doi: 10.1093/bja/aet296. [DOI] [PubMed] [Google Scholar]
- 7.Papanikolaou J, Makris D, Saranteas T, Karakitsos D, Zintzaras E, Karabinis A, et al. New insights into weaning from mechanical ventilation: Left ventricular diastolic dysfunction is a key player. Intensive Care Med. 2011;37:1976–1985. doi: 10.1007/s00134-011-2368-0. [DOI] [PubMed] [Google Scholar]
- 8.Amarja H, Bhuvana K, Sriram S. Prospective observational study on evaluation of cardiac dysfunction induced during the weaning process. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med. 2019;23:15–19. doi: 10.5005/jp-journals-10071-23106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moschietto S, Doyen D, Grech L, Dellamonica J, Hyvernat H, Bernardin G. Transthoracic echocardiography with Doppler tissue imaging predicts weaning failure from mechanical ventilation: Evolution of the left ventricle relaxation rate during a spontaneous breathing trial is the key factor in weaning outcome. Crit Care Lond Engl. 2012;16:R81. doi: 10.1186/cc11339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanfilippo F, Di Falco D, Noto A, Santonocito C, Morelli A, Bignami E, et al. Association of weaning failure from mechanical ventilation with transthoracic echocardiography parameters: A systematic review and meta-analysis. Br J Anaesth. 2021;126:319–330. doi: 10.1016/j.bja.2020.07.059. [DOI] [PubMed] [Google Scholar]
- 11.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Lanspa MJ, Gutsche AR, Wilson EL, Olsen TD, Hirshberg EL, Knox DB, et al. Application of a simplified definition of diastolic function in severe sepsis and septic shock. Crit Care Lond Engl. 2016;20:243. doi: 10.1186/s13054-016-1421-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rolando G, Espinoza EDV, Avid E, Welsh S, Pozo JD, Vazquez AR, et al. Prognostic value of ventricular diastolic dysfunction in patients with severe sepsis and septic shock. Rev Bras Ter Intensiva. 2015;27:333–339. doi: 10.5935/0103-507X.20150057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavefors O, Ljung Faxén U, Bech-Hanssen O, Lundin S, Ricksten SE, Redfors B, et al. Isolated diastolic dysfunction is associated with increased mortality in critically ill patients. J Crit Care. 2023;76:154290. doi: 10.1016/j.jcrc.2023.154290. [DOI] [PubMed] [Google Scholar]
- 15.Pulido JN, Afessa B, Masaki M, Yuasa T, Gillespie S, Herasevich V, et al. Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shock. Mayo Clin Proc. 2012;87:620–628. doi: 10.1016/j.mayocp.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong JY, Shin J, Kim WY. Impact of left ventricular dysfunction and fluid balance on the outcomes of patients with sepsis. Eur J Intern Med. 2020;74:61–66. doi: 10.1016/j.ejim.2019.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Clancy DJ, Scully T, Slama M, Huang S, McLean AS, Orde SR. Application of updated guidelines on diastolic dysfunction in patients with severe sepsis and septic shock. Ann Intensive Care. 2017;7:121. doi: 10.1186/s13613-017-0342-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, et al. Prediction of hospital outcome in septic shock: A prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care Lond Engl. 2010;14:R44. doi: 10.1186/cc8931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e895–e1032. doi: 10.1161/CIR.0000000000001063. [DOI] [PubMed] [Google Scholar]


